Abstract
Objective
To characterize utilization of laser and incisional glaucoma surgery among Medicare beneficiaries from 2008–2016 and to compare utilization of these surgeries by glaucoma subspecialists versus nonspecialists.
Design
Retrospective, observational analysis.
Participants
1468035 Medicare beneficiaries who underwent ≥1 laser or incisional glaucoma surgery during 2008 to 2016.
Methods
Claims data from a 20% sample of enrollees in fee-for-service Medicare throughout the US were analyzed to identify all laser and incisional glaucoma surgeries performed during 2008–2016. We assessed utilization of traditional incisional glaucoma surgeries (trabeculectomy and glaucoma drainage implants (GDIs)) as well as microinvasive glaucoma surgeries (MIGS). Enrollee and procedure counts were multiplied by 5 to estimate utilization throughout all of Medicare. Using linear regression, we also compared trends in utilization of glaucoma surgeries among ophthalmologists we could characterize as glaucoma subspecialists and nonspecialists.
Main Outcome Measure
Numbers of laser and incisional glaucoma surgeries performed overall, and stratified by glaucoma subspecialist status
Results
The number of Medicare beneficiaries who underwent any glaucoma therapeutic procedure increased 10.6% from 218375 in 2008 to 241565 in 2016. The total number of traditional incisional glaucoma surgeries decreased 11.7% from 37225 in 2008 to 32885 in 2016 (p=0.02). By comparison, the total number of MIGS increased 426% from 13705 in 2012 (the first year there were codes available for these surgeries) to 58345 in 2016 (p=0.001). Throughout the study period, glaucoma subspecialists performed the majority of trabeculectomies (76.7% in 2008 and 83.1% in 2016) and GDIs (77.7% in 2008 and 80.6% in 2016). By comparison, many MIGS were performed by nonspecialists. The proportion of endocyclophotocoagulations, iStent insertions, goniotomies, and canaloplasties performed by subspecialists in 2016 were 22.0%, 25.2%, 56.9%, and 62.8%, respectively.
Conclusion
From 2008–2016 we observed a large shift in practice away from traditional incisional glaucoma surgeries to MIGS. While glaucoma subspecialists continue to perform the majority of traditional incisional glaucoma surgeries, many MIGS are performed by nonspecialists. These results highlight the importance of training residents how to properly perform MIGS and manage these patients during the perioperative period. Future studies should explore the impact of this shift in care on outcomes and costs.
Precis
Analyzing data on Medicare beneficiaries from 2008–2016, we found a substantial decrease in traditional glaucoma surgery utilization coupled with a marked increase in microinvasive glaucoma surgeries, many of which were performed by nonspecialists.
Introduction
Glaucoma is the leading cause of irreversible blindness worldwide, with more than 110 million persons estimated to have glaucoma by the year 2040.1 Management of glaucoma consists of lowering intraocular pressure (IOP), the only known modifiable risk factor, using ocular hypotensive medications, laser therapy, or various incisional surgical procedures. Over the past four decades, laser and incisional surgical management of glaucoma has evolved considerably. Laser trabeculoplasty has been shown to be a safe and effective initial therapy for glaucoma even ahead of topical medications for some patients.2–4 Likewise, the development of laser procedures such as endocyclophotcoagulation5–9 and refinement of transscleral diode cyclophotocoagulation, including micropulse delivery methods10–11 are permitting clinicians to be able to offer cycloablative procedures to patients earlier in the disease course.12–13 The Tube versus Trabeculectomy (TVT) study has provided support for the expanded use of glaucoma drainage implant (GDI) surgeries, including as a primary incisional surgical option for patients with glaucoma.14 Novel surgical procedures referred to as microinvasive glaucoma surgery (MIGS) have greatly expanded surgical options even further, permitting lowering of IOP by restoring aqueous outflow through the Schlemm’s canal or establishing flow to the suprachoroidal or subconjunctival spaces.15–16
Past research by Ramulu and colleagues looked at trends in utilization of laser and incisional glaucoma surgeries among Medicare enrollees between 1995 and 2004. They were the first to note an increase in GDI surgery coupled with a reduction in trabeculectomy procedures during this period.17 In a follow-up study by the same group, this time using Medicare data from 1994 to 2012, Arora and colleagues continued to demonstrate a rise in GDI surgery and a decline in trabeculectomy surgeries.18 To the best of our knowledge, we are unaware of any studies assessing utilization of laser and incisional glaucoma surgeries on large numbers of patients since 2012. Given the dramatically changing landscape of surgical options available to lower IOP since 2012, with the rapid rise in availability of MIGS, we sought to assess the extent by which traditional incisional glaucoma surgery utilization was affected by utilization of MIGS using Medicare claims data from 2008–2016. In addition, we sought to determine for each of the available laser and incisional glaucoma surgeries, whether they were being performed primarily by glaucoma subspecialists or nonspecialists.
Methods
Data Source
We used a Medicare claims dataset consisting of a nationally-representative 20% sample of all persons with Medicare Parts A, B and D health insurance coverage during January 1, 2008 to December 31, 2016. The database contains detailed records of all ocular and nonocular conditions based on International Classification of Disease, 9th Revision - Clinical Modification19 (ICD-9-CM) billing codes and all visits, diagnostic, and therapeutic procedures performed on the enrollees based on Current Procedural Terminology20 (CPT-4) codes. The database also contains information on demographics, type of health care provider for each encounter, and the amount paid for all services rendered. Researchers have used this database to study patients with glaucoma and other ocular conditions.21–22 The study was approved by the Institutional Review Board at the University of Michigan and adheres to the tenets of the Declaration of Helsinki. Since the data we had access to was de-identified before it was shared with us, it was impossible for us to seek informed consent from all of the enrollees. Due to the large number of eye care professionals caring for the Medicare enrollees in this study, it was also infeasible to consent all of the providers to study which procedures they performed on which patients.
Inclusion and Exclusion Criteria
We identified all laser and incisional glaucoma surgery claims during January 1, 2008 to December 31, 2016 for all beneficiaries in fee-for-service Medicare. The CPT-4 codes for the various laser and incisional glaucoma surgeries can be found in Online Table 1, available at http://aaojournal.org. Following similar methodology to Arora and colleagues, we identified CPT codes for all of the therapeutic glaucoma procedures they had studied and supplemented them with additional CPT codes for newer laser and incisional glaucoma surgeries that came out after their study had been published.18 Claims were excluded if they were rejected or not paid. We only considered therapeutic procedures performed by an ophthalmologist or optometrist in the 50 US states or the District of Columbia. Since the database we used had incomplete information about care rendered to patients in Medicare Advantage plans, we excluded these patients and the care they received from our analysis.
National Trends
Since our dataset was a 20% random sample, surgical procedure counts were multiplied by 5 to estimate the total number of each glaucoma therapeutic procedure performed in all of fee-for-service Medicare in a given year. Procedure volumes provided in the Results section represent extrapolated counts for the entire fee-for- service Medicare population. The number of each procedure performed in the cohort was evaluated annually from 2008 to 2016. A given beneficiary could undergo more than one of a given glaucoma therapeutic procedure or multiple different procedures in a given year and across years of enrollment in the plan.
For some analyses, we grouped incisional glaucoma surgeries into traditional incisional glaucoma surgeries versus MIGS. We classified trabeculectomy (trabeculectomy, trabeculectomy with Ex-PRESS shunt) and GDI surgery as traditional incisional glaucoma surgery. Canaloplasty, endocyclophotocoagulation, goniotomy, and iStent trabecular micro-bypass surgery were all classified as MIGS. For these analyses, transcleral diode cyclophotocoagulation was not classified as a traditional glaucoma surgery or a MIGS.
Distinguishing Glaucoma Subspecialists Versus Nonspecialists
The dataset we used categorizes health care providers by medical specialty but unfortunately does not capture which providers are subspecialists and which are not. As such, we devised methodology to identify glaucoma subspecialists by looking at the volume and types of surgeries they performed. First, we identified all ophthalmologists and optometrists in the database based on their unique National Provider Identification (NPI) number. Next, the number of traditional incisional glaucoma surgeries (trabeculectomy, trabeculectomy with Ex-PRESS, or GDI) performed by each ophthalmologist was counted and averaged over the number of years between when they first and last submitted a claim for one of these surgeries. We defined glaucoma subspecialists as ophthalmologists who performed ≥10 traditional incisional glaucoma surgeries annually that were billed to Medicare. Nonspecialists consisted of optometrists and ophthalmologists who performed at least one laser or incisional glaucoma surgery but fewer than 10 traditional incisional glaucoma surgeries annually. Eye care providers who performed no laser or incisional glaucoma surgeries at all were excluded. We assumed that most providers care for patients in Medicare as well as other health insurance plans and that the surgeries we are capturing for a given provider represent a subset of all procedures they performed in a given year so the total number of traditional incisional glaucoma surgeries performed by the providers we are classifying as glaucoma subspecialists are likely much higher than the 10 per year identified from our one data source.
In order to evaluate how our subspecialist classification methodology compared with documentation of glaucoma fellowship training status, we randomly selected 100 NPI numbers that were listed in the Medicare dataset for further review, stratified by the number of traditional incisional glaucoma surgeries they performed. For each of these cases, the NPI number was queried on the CMS NPI Registry Online Search Tool23 to ascertain the identity of the actual ophthalmologist or optometrist. One of the study authors (S.R.) used publicly available data on the internet, including practice website, American Glaucoma Society membership data, and online physician biographies to determine if the ophthalmologist had completed formal glaucoma fellowship training.
Analysis
Statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, North Carolina, USA) and the R computing environment version 3.6.3 (R Core Team, Vienna, Austria). Enrollee characteristics were summarized for the entire sample using means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. Counts of procedures were tabulated and graphed by year. Percentages of procedures performed by subspecialists were computed and graphed by year. Regression was used to assess the linear trends over time. We estimated the accuracy of our subspecialist classification rule using weighted methods for stratified random samples. To investigate the impact on our main results of possible subspecialist misclassification, we imputed (100 times) fellowship training status for all NPI based on the estimated positive and negative predictive value of our classification definition.
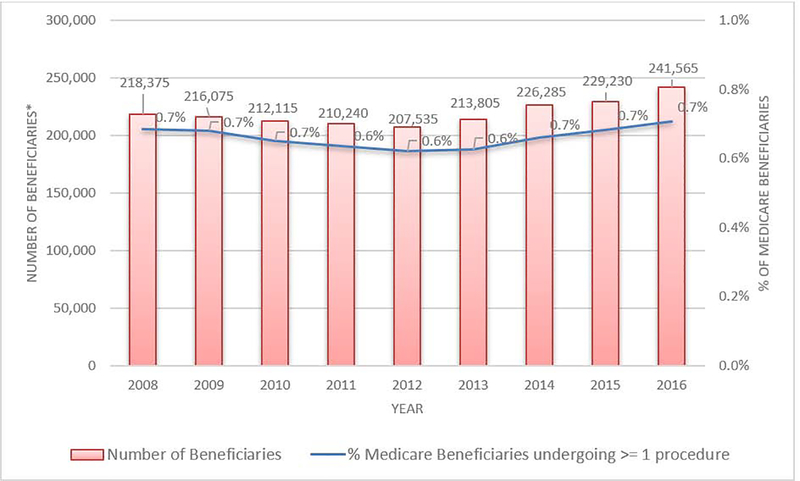
Results
There were 1468035 Medicare enrollees who underwent at least one laser or incisional glaucoma surgery during January 1, 2008 to December 31, 2016. The mean ± SD age of the enrollees in our cohort (those who had received at least one glaucoma therapeutic procedure) was 71.4 ± 2.3 years old in 2008. Our sample included 582475 (39.7%) males and included 1132670 (78.0%) whites, 194540 (13.4%) blacks, 44725 (3.1%) Asians, and 46105 (3.2%) Latinos. The number of enrollees in fee-for-service Medicare in our sample grew 9% from 35.0 million in 2008 to 38.3 million in 2016. The number of enrollees who underwent at least one glaucoma laser or incisional surgical procedure increased 10.6% from 218375 in 2008 to 241565 in 2016. (Figure 1)
Figure 1.
Overall Trends in Utilization of All Laser and Incisional Glaucoma Surgeries Among Medicare Enrollees from 2008 to 2016
*A given enrollee may be in Medicare for multiple years and may undergo surgeries in more than 1 year.
Red bar indicates the number of beneficiaries receiving ≥ 1 therapeutic glaucoma procedure. Blue bar captures the percentage of all beneficiaries in fee-for-service Medicare who received ≥ 1 therapeutic glaucoma procedure
First, we examined the validation of our glaucoma subspecialist classification methods. The number of providers we classified as glaucoma subspecialists and nonspecialists were 956 (26.8%) and 2603 (73.2%), respectively. From our NPI subset analysis, of the 50 providers with average number of traditional incisional glaucoma surgical procedures per year less than 10, the estimated proportion who demonstrated no evidence of being fellowship trained in glaucoma was 78.4% (95% confidence interval 66.4–90.4). Among the 50 providers with an average number of traditional incisional glaucoma surgeries of at least 10 per year, the estimated proportion who we could locate evidence that they were glaucoma fellowship trained was 81.6% (95% confidence interval 70.1–93.0). As such, with the methods we employed, we were able to accurately distinguish glaucoma subspecialists from nonspecialists for many of the eye care providers in the dataset.
The total number of therapeutic glaucoma procedures performed overall increased 14.7% from 294990 in 2008 to 338230 in 2016. The total number of traditional incisional glaucoma surgeries decreased 11.7% from 37225 in 2008 to 32885 in 2016 (p=0.02). By contrast, the total number of MIGS procedures increased 426% from 13705 in 2012 (the first year these procedures were captured in our dataset) to 58345 in 2016 (p=0.001). Table 1 shows the number of each laser and incisional glaucoma surgery performed each year from 2008–2016.
Table 1.
National Estimates of Common Laser and Incisional Glaucoma Surgeries Performed on Medicare Enrollees (2008–2016)
| Procedure | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|---|
| Laser Trabeculoplasty | 156185 | 153380 | 149735 | 144880 | 140940 | 142400 | 149165 | 150380 | 153865 |
| Trabeculectomy | 25610 | 25620 | 26145 | 24665 | 23370 | 22680 | 21730 | 20770 | 18925 |
| GDI | 11615 | 11270 | 12375 | 12675 | 13825 | 14825 | 14700 | 14315 | 13960 |
| Transcleral Diode Cyclophotocoagulation | 4450 | 3920 | 3885 | 3530 | 3495 | 3540 | 3745 | 4585 | 9510 |
| Endocyclophotocoagulation | 8775 | 10870 | 10725 | 10695 | 10815 | 10560 | 10535 | 10740 | 11275 |
| Iridectomy | 84850 | 84590 | 79665 | 83010 | 79055 | 82230 | 82150 | 79075 | 80720 |
| Iridoplasty | 3190 | 3260 | 3010 | 2995 | 2955 | 3115 | 2785 | 2785 | 2905 |
| Canaloplasty | 180 | 525 | 1275 | 1410 | 2445 | 1645 | 1130 | 1215 | 1615 |
| iStent | 0 | 0 | 0 | 10 | 350 | 8385 | 18460 | 29920 | 42635 |
| Goniotomy | 135 | 140 | 145 | 70 | 85 | 155 | 100 | 150 | 2715 |
| Trabeculectomy and GDI procedures | 37225 | 36890 | 38520 | 37340 | 37195 | 37505 | 36430 | 35085 | 32885 |
GDI = Glaucoma Drainage Implantation.
Procedure counts presented are estimates for all of fee-for-service Medicare (20% dataset values * 5).
Trabeculectomy numbers include those done with or without Ex-PRESS shunts.
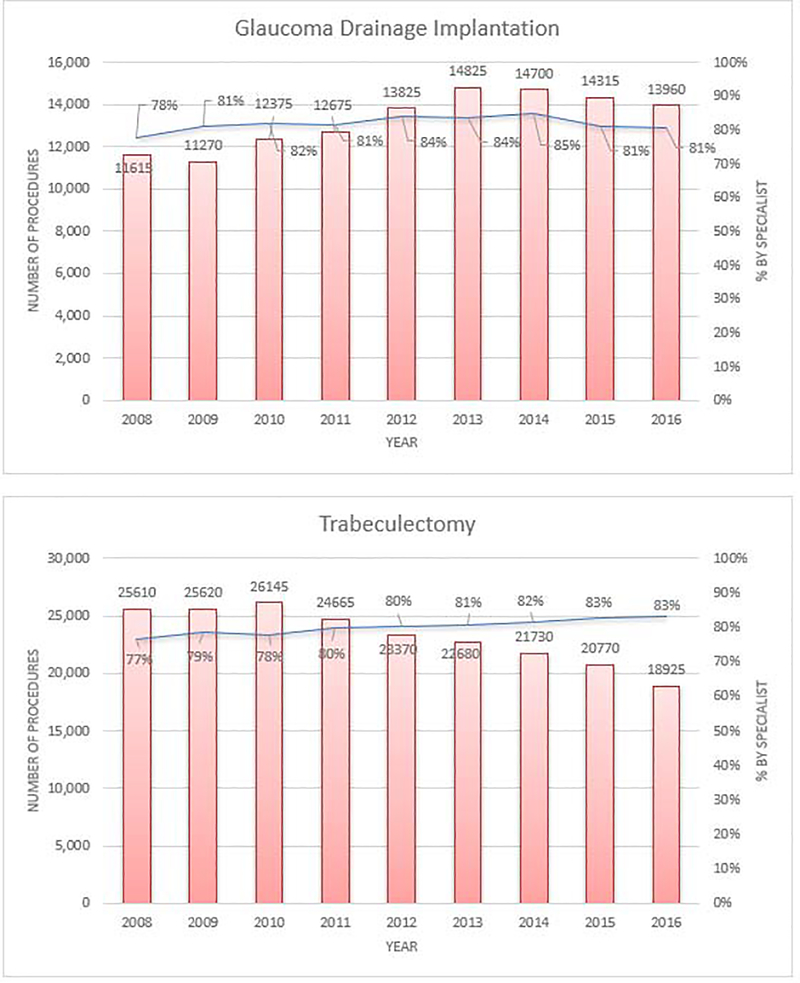
The overall number of trabeculectomies performed on fee-for-service Medicare enrollees decreased from 25610 in 2008 to 18925 in 2016 (p=0.0001). Glaucoma subspecialists performed more than three quarters of trabeculectomies each year and the proportions increased from 76.7% in 2008 to 83.1% in 2016 (p=0.0001). By comparison, the overall number of GDIs performed in Medicare beneficiaries increased 20.2% from 11615 in 2008 to 13960 in 2016 (p=0.003). Likewise, more than three quarters of these surgeries were performed by glaucoma subspecialists each year. There was no significant change in the proportion of GDI surgeries performed by glaucoma subspecialists from 2008 to 2016 (77.7% in 2008 versus 80.6% in 2016 (p=0.37). (Figure 2)
Figure 2.
Glaucoma Drainage Device Implantation and Trabeculectomy Volumes From 2008–2016 Among Glaucoma Subspecialists and Nonspecialists
Trabeculectomy volumes include those performed with or without Ex-PRESS shunts. Red bar indicates the number of beneficiaries receiving ≥ 1 of the surgery of interest in a given year. Blue bar captures the percentage of the surgery of interest that were performed by glaucoma subspecialists each year.
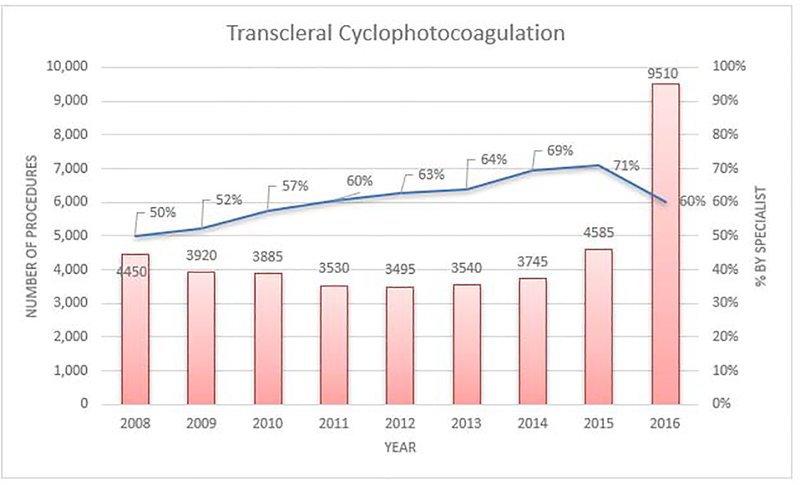
The overall number of transcleral diode cyclophotocoagulation and endocyclophotcoagulation procedures performed on Medicare enrollees increased 113.7% from 4450 in 2008 to 9510 in 2016 (p=0.15) and 28.5% from 8775 in 2008 to 11275 in 2016 (p=0.09), respectively. Although overall trends for cycloablation were not statistically significant from 2008 to 2016, the number of transcleral diode cyclophotocoagulation surgeries grew considerably (207%) in the last year we studied from 4585 in 2015 to 9510 in 2016. The proportion of transcleral diode cyclophotocoagulation surgeries performed by glaucoma subspecialists rose steadily from 49.9% in 2008 to 71.0% in 2015 but declined to 60.2% from 2015 to 2016 (p=0.008). (Figure 3) Each year, glaucoma subspecialists performed a relatively small percentage of the endocyclophotcoagulations (17.1% in 2008 and 22.0% in 2016) (p=0.0007).
Figure 3.
Transcleral Diode Cyclophotocoagulation Procedure Volume From 2008–2016 Among Glaucoma Subspecialists and Nonspecialists
Red bar indicates the number of beneficiaries receiving ≥ 1 of the surgery of interest in a given year. Blue bar captures the percentage of the surgery of interest that were performed by glaucoma subspecialists each year.
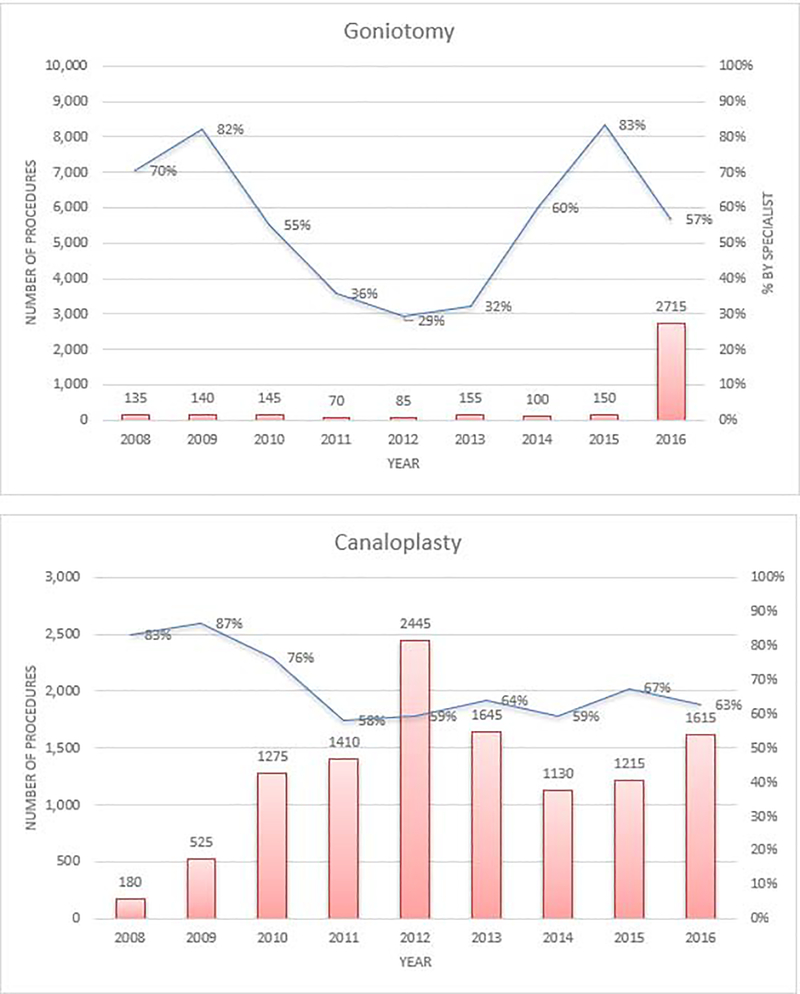
The overall number of goniotomies performed increased 1911% from only 135 in 2008 to 2715 in 2016 (p=0.13). (Figure 4) Most of this increase occurred from 2015 to 2016. The proportion of goniotomies performed by glaucoma subspecialists declined from 70.4% in 2008 to 56.9% in 2016 (p=0.80). Canaloplasty volume increased 797% from 180 in 2008 to 1615 in 2016 (p=0.13). (Figure 4) Glaucoma specialists performed 83.3% of canaloplasties in 2008 compared to only 62.8% in 2016 (p=0.02). The number of iStent trabecular micro-bypass (0191T, 0376T) procedures performed increased substantially from 350 in 2012 to 42635 in 2016 (p=0.0003). Glaucoma specialists performed only 29% of iStent trabecular micro-bypass procedures in 2012 and only 25.2% in 2016 (p=0.31).
Figure 4.
Goniotomy and Canaloplasty Procedure Volumes From 2008–2016 Among Glaucoma Subspecialists and Nonspecialists
Red bar indicates the number of beneficiaries receiving ≥ 1 of the surgery of interest in a given year. Blue bar captures the percentage of the surgery of interest that were performed by glaucoma subspecialists each year.
The number of laser trabeculoplasties performed on Medicare enrollees remained stable from 156185 in 2008 to 153865 in 2016 (p=0.62). The majority of laser trabeculoplasties were performed by nonspecialists (77% in 2008 and 71% in 2016) (p<0.0001). The number of iridotomies performed decreased slightly from 84850 in 2008 to 80720 in 2016 (p=0.09). Similar to laser trabeculoplasty, the majority of iridotomies were performed by nonspecialists (76.8% in 2016).
Finally, we performed simulations to determine whether our findings would change if the subset of glaucoma specialists and nonspecialists happened to get misclassified. We found the statistical significance of the each of the associations of MIGS, trabeculectomies, and GDIs with time were preserved in 94% or more of the subspecialist misclassification simulations.
Discussion
Using data from a nationally-representative sample of Medicare beneficiaries, we characterized longitudinal trends in laser and incisional glaucoma surgery utilization between 2008 to 2016 and sought to capture for each therapeutic procedure whether it was performed by a glaucoma subspecialist or a nonspecialist. We learned that there continues to be a decline in trabeculectomy surgery coupled with a rise in GDI surgeries from 2008–2016. The majority of these traditional incisional glaucoma surgeries (> 75% each year) are being performed by glaucoma subspecialists. Another important finding of our analyses was the marked rise in MIGS, many of which are being performed by nonspecialists.
Earlier research by Ramulu and colleagues captured trends in therapeutic glaucoma surgery utilization among Medicare beneficiaries from 1995 to 2004.17 A follow-up study by the same research group demonstrated trends in utilization of different laser and incisional glaucoma surgeries through 2012.18 These 2 prior studies identified a 14% decline in the total glaucoma procedures performed from the 1990s through 2012, despite a concurrent 5% increase in the number of Medicare Part B beneficiaries over this same time period.17,18 In our analyses, if we excluded the newer MIGS procedures, we also observed a modest decline (0.7%) in the total number of glaucoma procedures performed on Medicare enrollees from 2008–2016, despite a 9% increase in Medicare Part B beneficiaries during this time frame. However, once we account for MIGS surgeries— which started becoming popular in 2012, with rapid expansion from 2012 to 2016— there was actually a 14.7% increase in the total number of glaucoma procedures performed on Medicare beneficiaries. With the aging of the US population, the fact that glaucoma tends to disproportionately affect older patients24, coupled with the increased safety profile of some of these newer surgical options that are now available, along with a desire for patients to be on fewer topical IOP lowering medications, we expect to see continued rises in utilization of glaucoma therapeutic interventions in the years to come. It will be interesting to observe how the recent U.S. Food and Drug Administration approval and availability of injectable glaucoma medications will affect use of laser and incisional glaucoma surgeries.25
We found that approximately three quarters to four fifth of all traditional incisional glaucoma surgeries on Medicare beneficiaries were performed by glaucoma subspecialists. These trends remained relatively stable from 2008 through 2016. It is unsurprising that the majority of these surgeries are performed by glaucoma subspecialists, given some of the technical challenges of carrying out these surgeries, the need for antimetabolites and other intraoperative and postoperative interventions in many cases, and the importance of careful postoperative care and monitoring to ensure long term success of the procedure and manage any adverse events that may arise. Furthermore, with various IOP-lowering medications, lasers, and now MIGS as options, traditional incisional glaucoma surgeries are often performed on patients with more advanced disease, many of whom are under the care of a glaucoma subspecialist.
We did not expect to find that such a large proportion of MIGS are being performed by nonspecialists. While the safety profile of MIGS tends to be better than the more traditional incisional glaucoma surgeries26–27, the effectiveness of these procedures at lowering IOP requires a solid understanding of the anatomical landmarks of the angle structures by the surgeon to ensure proper placement of these devices. If many of these procedures are being performed by nonspecialists as our analyses are demonstrating, it highlights the importance of ensuring that ophthalmology residents obtain sufficient training in slit-lamp gonioscopy to properly identify angle structures and comfort performing gonioscopy in the operating room. Prior research on Medicare enrollees with glaucoma found that very few of them had any record of undergoing this important diagnostic procedure.28,29 Improper placement of MIGS can lead to damage to the corneal endothelium, ineffective lowering of IOP, and other adverse effects.30 Other reasons for the rise in utilization of MIGS among nonspecialists include the ability to often perform these procedures in conjunction with cataract surgery, indications for use of these surgeries in patients with mild to moderate glaucoma, many of whom are managed by nonspecialists, and a desire for some nonspecialists to market themselves as being early adopters to surgical innovations.31 Declines in reimbursement for phacoemulsification may also have incentivized some nonspecialists to offer MIGS in conjunction with phacoemulsification to make up for some of the lost revenue.
We found approximately a five percent decline in laser iridotomy volume from 2008 through 2016. This may be attributable to more widespread use of cataract surgery instead of iridotomy for patients with narrow angles and concomitant cataracts. Additionally, the increasing interest and popularity of refractive cataract surgery over the study period may have limited some patients from progressing to denser cataracts that can cause crowding of the angle, and this may have also influenced laser iridotomy volume. Unlike the past studies which revealed a rise in utilization of laser trabeculoplasty17–18, in the present analyses, laser trabeculoplasty volume was relatively stable. This may reflect the more widespread availability and utilization of MIGS procedures as an alternative to laser trabeculoplasty.
Study Limitations
Our study had several limitations. First, our study sample were limited to enrollees in fee-for-service Medicare. It is uncertain whether the findings generalize to patients with other types of health insurance, those who are uninsured, or those residing outside of the US. Second, the CPT-4 codes for some of the newer MIGS (Cypass microstent (Alcon, Fort Worth, TX), Hydrus microstent (Ivantis, Irvine, CA) and Xen Gel Stent (Allergan, Irvine, CA) were not device specific at the time of our data collection. As such, we were unable to capture utilization of these 3 MIGS devices. Future studies should be able to track utilization of these procedures along with the earlier MIGS that possessed their own unique CPT codes included in our analyses. Third, unfortunately our data source does not capture provider subspecialty designations. While the number of glaucoma subspecialists we identified in these analyses closely align with membership numbers for the American Glaucoma Society (Personal Communication with Carey Craig, Client Services Coordination, San Francisco Association of Management Services on July 22, 2019), we were only able to validate a sample of all of the NPIs to be certain that indeed these providers were glaucoma subspecialists. As such, we acknowledge that some nonspecialists may have been misclassified as glaucoma subspecialists and vice versa. Often the presence of measurement error (in this case misclassifying specialists as nonspecialists and vice versa) attenuates any differences between groups. Thus, the differences we are reporting between the subspecialists and nonspecialists are likely underestimates of the true differences that exist. Moreover, our simulation analyses revealed if some of the providers had been misclassified, it did not appreciably alter our study findings. New glaucoma taxonomy NPI associated codes that are beginning to become available have self-reported subspecialist designations but were unavailable at the time this data was captured by the Center for Medicare and Medicaid Services. Finally, in these analyses we excluded unpaid and rejected claims. Fewer than 10% of all claims for the procedures studied were unpaid or rejected. While there was a slightly greater percentage of rejected claims for patients undergoing procedures by nonspecialists relative to subspecialists, this difference was never larger than 2% in a given year so we doubt this affected our findings much.
Conclusion
In conclusion, this study captures trends in the utilization of laser and incisional glaucoma surgeries among Medicare enrollees from 2008–2016. It highlights the changing landscape of glaucoma surgery with a large shift away from the more traditional incisional glaucoma surgeries to rapid and widespread growth of MIGS. Unlike traditional glaucoma surgeries which are performed primarily by glaucoma subspecialists, we are observing that many MIGS are being performed by nonspecialists. Future research is needed to better understand how the changes we are observing are affecting patient outcomes and overall costs to Medicare.
Supplementary Material
Acknowledgments
Funding Support: American Glaucoma Society Mentoring for the Advancement of Physician Scientists (MAPS) Award 2018 (SR); University of Miami core grant P30EY014801 (DSG); Unrestricted grant from Research to Prevent Blindness, New York, NY (DSG, JDS); an unrestricted grant from Mr. and Mrs. Thorne B. Donnelley, Chicago, IL (DSG); the Maltz Family Endowment for Glaucoma Research, Cleveland, OH (DSG); Lighthouse Guild, New York, NY (JDS); National Eye Institute, Bethesda, MD R01 EY026641 (JDS); Dr. Beverley and Gerson Geltner Fund (JDS).
Footnotes
Financial Disclosure: Dr. Rathi serves as a consultant to Eyenovia. Dr. Greenfield serves as a consultant to Aerie Pharmaceuticals, Alcon, Allergan, Eyenovia, Galimedix, Pfizer and Quark Pharmaceuticals. Drs. Andrews and Stein have no relevant financial disclosures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014; 121:2081–2090. [DOI] [PubMed] [Google Scholar]
- 2.Katz LJ, Steinmann WC, Kabir A, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2012; 21(7):460–8. [DOI] [PubMed] [Google Scholar]
- 3.Li X, Wang W, Zhang X. Metaanalysis of selective laser trabeculoplasty versus topical medication in the treatment of open-angle glaucoma. BMC Ophthalmol. 2015;15:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong MO, Lee JW, Choy BN, et al. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol. 2015;60:1:36–50. [DOI] [PubMed] [Google Scholar]
- 5.Clement C Combining phacoemulsification with endoscopic cyclophotocoagulation to manage cataract and glaucoma. Clinical and Experimental Ophthalmology 2013;41:546–661. [DOI] [PubMed] [Google Scholar]
- 6.Lima F A Prospective, Comparative Study between Endoscopic Cyclophotocoagulation and the Ahmed Drainage Implant in Refractory Glaucoma. J Glaucoma. 2004;13:3. [DOI] [PubMed] [Google Scholar]
- 7.Lindfield D, Ritchie RW, Griffiths MF. Phaco-ECP: combined endoscopic cyclophotocoagulation and cataract surgery to augment medical control of glaucoma. BMJ Open. 2012;2:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kahook MY, Lathrop KL, Noecker RJ. One-site versus two-site endoscopic cyclophotocoagulation. J Glaucoma. 2007;16(6):527–530. [DOI] [PubMed] [Google Scholar]
- 9.Morales J, Al Qahtani M, Khandekar R, et al. Intraocular Pressure Following Phacoemulsification and Endoscopic Cyclophotocoagulation for Advanced Glaucoma: 1- Year Outcomes. Journal of Glaucoma. 2015. August;24(6):e157–62. [DOI] [PubMed] [Google Scholar]
- 10.Aquino MCD. Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Experiment Ophthalmol. 2015;43(1):40–46. [DOI] [PubMed] [Google Scholar]
- 11.Tan A, Chockalingam M, Aquino M, et al. Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Experiment Ophthalmol. 2010;38(3):266–272. [DOI] [PubMed] [Google Scholar]
- 12.Rotchford AP, Jayasawal R, Madhusudhan S, et al. Transscleral diode laser cycloablation in patients with good vision. Br J Ophthalmol. 2010;94(9):1180–1183. [DOI] [PubMed] [Google Scholar]
- 13.Egbert PR, Fiadoyor S, Budenz DL, et al. Diode laser transscleral cyclophotocoagulation as a primary surgical treatment for primary open-angle glaucoma. Arch Ophthalmol. 2001;119:345–350. [DOI] [PubMed] [Google Scholar]
- 14.Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the Tube versus Trabeculectomy study after five years of follow-up. Am J Ophthalmol. 2012; 153(5):789–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caprioli J, Kim J, Friedman D, et al. Special Commentary: Supporting Innovation for Safe and Effective Minimally Invasive Glaucoma Surgery. Ophthalmology. 2015;122(9):1795–1801. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed I MIGS and the FDA: What’s in a Name? Ophthalmology. 2015;122(9):1737–1739. [DOI] [PubMed] [Google Scholar]
- 17.Ramulu PY, Corcoran KJ, Corcoran SL, et al. Utilization of various glaucoma surgeries and procedures in Medicare beneficiaries from 1995 to 2004. Ophthalmology. 2007;114:2265–70. [DOI] [PubMed] [Google Scholar]
- 18.Arora KS, Robin AL, Corcoran KJ, Corcoran SL, Ramulu PY. Use of Various Glaucoma Surgeries and Procedures in Medicare Beneficiaries from 1994 to 2012. Ophthalmology. 2015; 122(8): 1615–1624. [DOI] [PubMed] [Google Scholar]
- 19.International classification of diseases, 9th revision, clinical modification: ICD-9-CM. 1996. [Salt Lake City, UT: ]: American Medical Association; Medicode. [Google Scholar]
- 20.CPT 2006. Chicago, IL: AMA Press; 2006. [Google Scholar]
- 21.Stein JD, Ayyagari P, Sloan FA, et al. Rates of glaucoma medication utilization among persons with primary open-angle glaucoma, 1992 to 2002. Ophthalmology. 2008;115(8):1315–9. [DOI] [PubMed] [Google Scholar]
- 22.Newman-Casey PA, Woodward MA, Niziol LM, Lee PP, De Lott LB. Brand Medications and Medicare Part D: How Eye Care Providers’ Prescribing Patterns Influence Costs. Ophthalmology. 2018;125(3):332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NPPES NPI Registry. Available at https://npiregistry.cms.hhs.gov. Accessed March 3, 2020.
- 24.Friedman DS, Wolfs RC, O’Colmain BJ, et al. Prevalence of Open-Angle Glaucoma Among Adults in The United States. Arch Ophthalmol. 2004;122(4):532–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allergan receives FDA approval for Durysta. Available at https://www.allergan.com/News/Details/2020/03/Allergan%20Receives%20FDA%20Approval%20for%20DURYSTA%20bimatoprost%20implant%20the%20First%20and%20Only%20Intracameral%20Biode; Accessed April 6, 2020.
- 26.Craven R, Katz J, Wells J, et al. Cataract surgery with trabecular mico-bypass stent implantation in patients with mild-to-moderate open-angle glaucoma and cataract: Two-year follow-up. J Cataract Refract Surg. 2012;38(8):1339–1345. [DOI] [PubMed] [Google Scholar]
- 27.Chen DZ, Sng CC. Safety and Efficacy of Microinvasive Glaucoma Surgery. J Ophthalmol 2017:3182935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coleman AL, Yu F, Evans SJ. Use of gonioscopy in medicare beneficiaries before glaucoma surgery. J Glaucoma. 2006:15(6):486–93. [DOI] [PubMed] [Google Scholar]
- 29.Fremont AM, Lee PP, Mangione CM, et al. Patterns of care for open-angle glaucoma in managed care. Arch Ophthalmol. 2003;121(6):777–783. [DOI] [PubMed] [Google Scholar]
- 30.Reiss G, Clifford B, Vold S, et al. Safety and Effectiveness of CyPass Supraciliary Micro-Stent in Primary Open-Angle Glaucoma: 5-Year Results from the COMPASS XT Study. Am J Ophthalmol. 2019;2018:219–225. [DOI] [PubMed] [Google Scholar]
- 31.Stein JD, Hanrahan BW, Comer GM, et al. Diffusion of technologies for the care of older adults with exudative age-related macular degeneration. Am J Ophthalmol. 2013; 155(4):688–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.