Abstract
Rural-urban differences in morbidity and mortality across the United States have been well documented and termed the “rural mortality penalty”. However, research studies frequently treat rural areas as homogeneous and often do not account for geospatial variability in rural health risks by both county, state, region, race, and sex within the United States.
Additionally, people living in the rural South of the US have higher rates of morbidity and mortality compared to both their urban counterparts and other rural areas. Of those living in southern rural communities, people of color experience higher rates of death and disease compared to white populations. Although there is a wealth of research that uses individual-level behaviors to explain rural-urban health disparities, there is less focus on how community and structural factors influence these differences. This review focuses on the “southern rural health penalty”, a term coined by the authors, which refers to the high rate of mortality and morbidity in southern rural areas in the USA compared to both urban areas and non-southern rural places. We use macrosocial determinants of health to explain possible reasons for the “southern rural health penalty”. This review can guide future research on rural health between southern and non-southern populations in the US and examine if macrosocial determinants of health can explain health disparities within southern rural populations.
Keywords: Rural, Macrosocial determinants of health, Rural mortality penalty, U.S. South, Race-specific mortality, Regional health disparities, Rural health
1. Introduction
1.1. Rural People Matter
While many rural Americans appear largely satisfied with their lives, they face persistent health disparities compared to people living in urban areas (NPR, 2018). Rural residents often struggle to access healthcare, while others experience high rates of disease and death (Cosby et al., 2019; Dwyer-Lindgren et al., 2017; Meit et al., 2014). Although there has been increasing national attention on rural health inequities, most research has focused on individual behaviors rather than community and structural influences on health. Additionally, research studies often treat rural areas as homogeneous and do not account for geospatial variability in rural health risks by both state, county, region, and race and sex within the United States. To understand and improve the health of rural Americans, research must examine structural and macrosocial determinants of health and assess how these factors interact to increase health risks in select rural areas.
The present review describes the history of the “rural-urban health divide” and how it has changed over time, with a focus on rural health disparities in southern US communities and differences in these disparities between races. We explore rural health challenges and summarize how they link to macrosocial determinants of health. The review concludes with suggested directions for future research that can inform our understanding of rural health disparities.
1.2. The Meaning of “Rural”
There are multiple definitions of “rural”, which leads to different estimates of the number of people living in rural areas (Smith et al., 2013). The federal government generally uses two organizations’ definitions of “rural”: The U.S. Census Bureau and the Office of Management and Budget (OMB), with the former stating that 20 percent of the US population is rural, and the latter estimating 15 percent is rural (Health Resources and Services Administration, 2017).
The various definitions of “rural” can make it difficult to understand specific rural health disparities, and to whom it applies (Smith et al., 2013). Additionally areas that are designated “rural” in one time period may be reclassified as “urban” in a subsequent time period, which makes it challenging to interpret rural mortality and morbidity trends over time (Cosby et al., 2019). It would be useful for researchers and the federal government to use one definition of “rural” to improve interpretations of mortality trends. In this review, we do not select one definition as different studies use various definitions of “rural”.
Despite different classifications, there are broad similarities between rural areas, including a decline in population, closure of health facilities, and increases in geographic distance to services, which lead to a widening gap in the morbidity and mortality rates between urban and rural populations (Meit et al., 2014).
1.3. Migration and Population Change in the US
Throughout the 20th century, many rural populations in the US declined as rural residents moved to cities for job opportunities. However, in the 1970s rural areas experienced an increase in population compared to urban areas. For the duration of the last century, rural and urban population change fluctuated (Bauer, 2010). Between 2000 and 2010, rural populations experienced increased growth, with wide variations among proportions of resident racial and ethnic groups. During this period, the Hispanic population has dramatically increased in rural and small town areas by 1.9 million or 46% (Housing Assistance Council, 2012). As of 2018, Non-Hispanic Whites comprise 80% of the rural population (Cromartie, 2018). Hispanics are the largest minority population in rural areas accounting for 9.0% of the rural population, blacks comprise 8% of the rural population, and Native Americans are the only minority group where a larger percentage lives in rural areas than urban areas (Cromartie, 2018). From 2013–2017, the population increase in rural areas was largely attributable to stable growth among Hispanic populations (Cromartie, 2018).
National trends in urban and rural population change masks local variations. While some rural areas may be experiencing population gains, other areas including the Midwest, Appalachia, the South, and the Northeast are experiencing persistent population loss due to declines in family farms and other job industries among other issues (Housing Assistance Council, 2011).
Moreover, many rural communities are experiencing an increase in populations over 65 years due to an aging population, influx of older individuals migrating to rural areas for retirement, and out-migration of younger residents (Cromartie, 2018). As rural areas continue to have larger populations of older populations, this increases the burden on the strained healthcare systems (Wakefield et al., 2004).
2. Rural Mortality Penalty in the US
Although contemporary data indicate that rural populations in the US experience higher rates of health concerns and mortality compared to their urban peers, this is a relatively recent trend (Cossman, James, & Wolf, 2016). During the Industrial Revolution in the eighteenth and nineteenth centuries, urban mortality exceeded rural mortality in the US (Cossman et al., 2016). The pattern of excess urban mortality has been termed the urban mortality penalty (Cossman et al., 2016).
High rates of mortality in urban areas was attributed to numerous reasons, including overcrowding, which led to rapid spread of infections and contagious disease; limited clean water and sewage disposal; and contaminated food and water (Haines, 2001). In contrast, rural residents lived farther from one another, which may have contributed to their overall lower mortality rate in that era (Haines, 2001). From the late nineteenth century onwards, public health improvements greatly reduced mortality rates across the US, which caused the urban mortality penalty to virtually disappear by the mid 20th century (Cossman et al., 2016; Haines, 2001).
2.1. Challenges with Tracking the Mortality Penalty Over Time
Research on the “rural mortality penalty” uses data from 1968 onwards, due to limited availability of earlier mortality data. In the United States, there are limited rigorous statistics for tracking mortality trends before the mid-20th century (Haines, 2001). Although the United States began conducting a regular census in 1790, most vital statistics were collected by local governments, which led to differences in how such information was collected and presented.
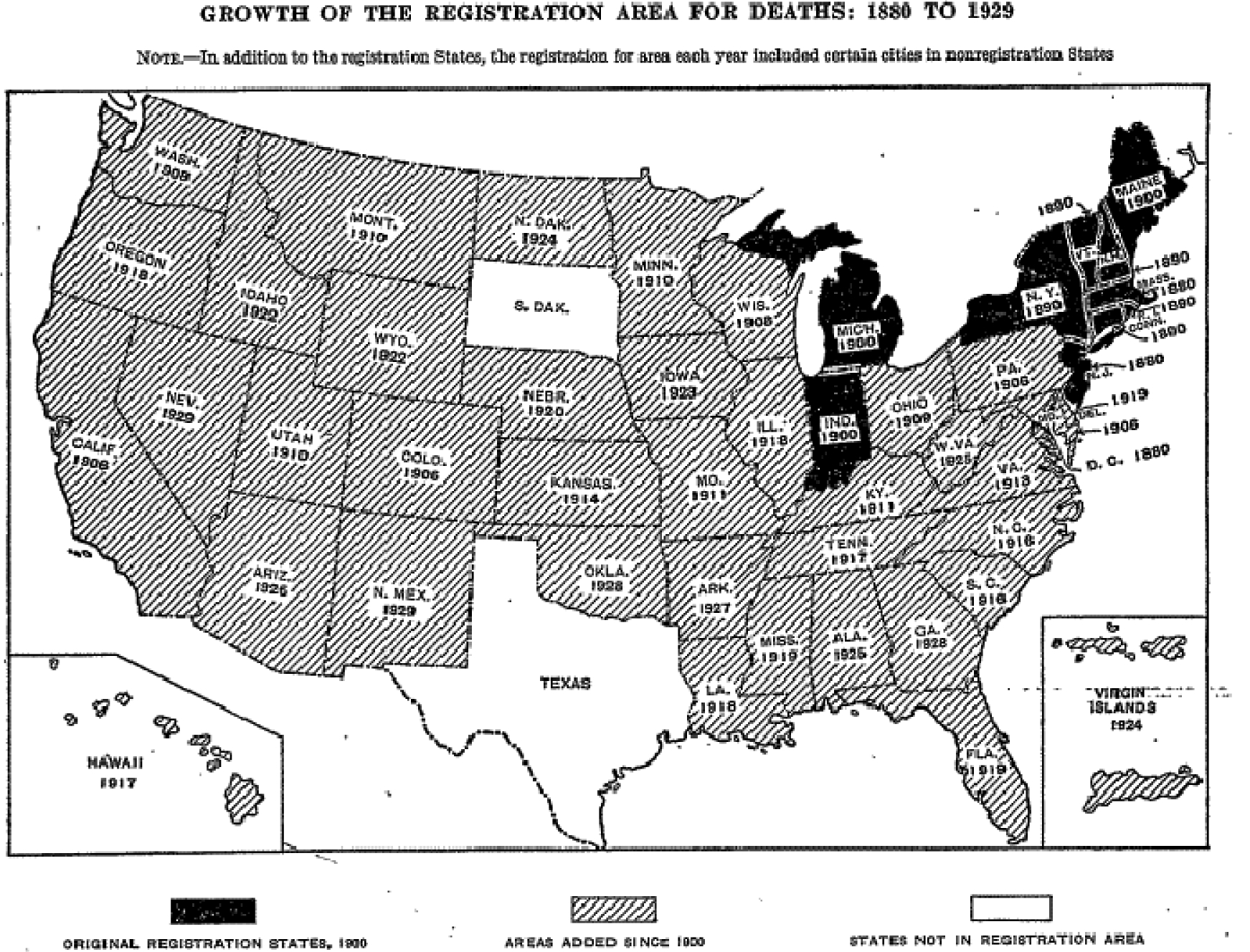
Additionally, the census data only included mortality statistics from US states that were “registration areas”, which did not represent the entire US (Haines, 2001; U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division., 1923). The first registration areas were established in 1890, and by 1929 most states were included in the census vital statistics (See Figure 1) (U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division., 1923).
Figure 1: Displays the growth of the registration area for deaths in the United States of America.
Some research on rural-urban mortality states that mortality rates between rural and urban areas were similar from the late 1940s until the 1980s when the rural mortality penalty began (Cossman, James, & Wolf, 2017; Haines, 2001). Our research of the United States Vital Statistics from 1890–1964 suggests there was an urban mortality penalty throughout this period, especially between 1890 and 1920, with urban-rural mortality rates converging over time over time (See Table 1 and the Appendix).
Table 1:
Death rate from all causes per 100,000 estimated population, 1890–1960
| Urban and Rural | Urban | Rural | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1890 | - | - | - | 2,210 | - | - | 1,530 | - | - |
| 1900 | - | - | - | 1,860 | - | - | 1,540 | - | - |
| 1910 | 1,500 | 1,460 | 2,410 | 1,610 | 1,550 | 2,640 | 1,340 | 1,330 | 1,740 |
| 1920 | 1,310 | 1,260 | 1,800 | 1,420 | 1,360 | 2,270 | 1,190 | 1,150 | 1,530 |
| 1929+ | 1,190 | 1,140 | 1,690 | 1,310 | 1,240 | 2,050 | 1,090 | 1,040 | 1,490 |
| 1940 | 1,080 | 1,040 | 1,380 | 1,135 | 1,095 | 1,550 | 1,119 | 1,075 | 1,505 |
| 1960 | 950 | 950 | 1,010 | 1,029 | 1,039 | 1,040 | 990 | 925 | 1,120 |
1929 data was selected as there is no vital statistics report with data specific to race and residency (U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division)
Differences by Race
The rural mortality penalty affects all races in the US, yet it began at different times for various races (Cossman et al., 2016). One study examining mortality rates from 1968–2007 reported that for non-Hispanic white populations, the rural mortality penalty began in the mid-1980s, whereas it started in the late 1990s for black populations (Cossman et al., 2016). Despite the difference in onset, the gap between urban and rural deaths is as large in black populations as it is in non-Hispanic white populations (Cossman et al., 2016). Yet, black individuals have substantially higher absolute mortality rates than non-Hispanic white regardless of urban-rural differences (Cossman et al., 2016). In 2008, the age-adjusted excess mortality rate was approximately 720 per 100,000 for urban white individuals and 820 per 100,000 for rural white individuals (Cossman et al., 2016). In contrast, for black populations, the age-adjusted mortality rate was approximately 950 per 100,000 for urban black individuals and 1,050 per 100,000 for rural black individuals in 2008 (Cossman et al., 2016).
There have been recent trends of increasing death rates among middle-aged non-Hispanic white populations, especially those with lower socio-economic status, while death rates have declined among non-Hispanic black populations (Case & Deaton, 2015). Many of these deaths were attributed to suicide, accidental poisonings, and liver disease, which Case and Deaton coined “deaths of despair” (Case & Deaton, 2015). The recent increase in mortality of white people notwithstanding, overall black populations still experience a higher rate of absolute mortality compared to non-Hispanic white people in both urban and rural areas (Stein, Gennuso, Ugboaja, & Remington, 2017).
3. Southern Rural Mortality Penalty: Not All Rural Areas Are Created Equal
Rural places are not homogenous and some rural areas of America experience better health outcomes compared to people residing in urban places (W James, 2014). Individuals living in rural areas in the Northeast, and some parts of the Midwest and West of the US tend to have lower rates of death and disease compared to both the US in general and to their urban counterparts (W. James, Cossman, & Wolf, 2018; Meit et al., 2014; Murray et al., 2006).
Those living in the rural South, especially in the Appalachia and Mississippi Delta region, have the lowest life expectancy in the country, (Singh & Siahpush, 2014b) and the highest mortality rates due to heart, lung, blood, and sleep (HLBS) disorders; stroke; and cancer (W. James et al., 2018; Meit et al., 2014; Murray et al., 2006; U.S. Census Bureau 2011–2015 American Community Survey 5-Year Estimates, 2015). Individuals residing in the rural South experience higher mortality rates compared to both their urban counterparts and other populations living in other rural regions across the US (W. James et al., 2018; Meit et al., 2014; Murray et al., 2006; U.S. Census Bureau 2011–2015 American Community Survey 5-Year Estimates, 2015).
The southern mortality penalty is persistent and has exceeded mortality rates in other geographic areas over the past five decades (W. James et al., 2018). The disparity in mortality rates between rural regions is stark, with people living in rural communities in the East South Central Region (Kentucky, Tennessee, Mississippi, and Alabama) experiencing more than 1,000 deaths per 100,000 from 2013 to 2015, compared to 850 deaths per 100,000 in all rural areas in the US (W. James et al., 2018). Furthermore, while all rural regions in the South experience high rates of mortality, populations living in the rural East South Central Region have the highest mortality rate (W. James et al., 2018).
The southern rural mortality penalty impacts all races and ethnicities, with black populations experiencing the highest mortality rates, and also persists after adjusting for poverty (See Table 2) (C. V. James et al., 2017; Murray, Kulkarni, & Ezzati, 2005; Murray et al., 2006; Singh, Williams, Siahpush, & Mulhollen, 2011; U.S. Census Bureau 2011–2015 American Community Survey 5-Year Estimates, 2015).
Table 2:
Rural Health Penalty in Southern United States
| Characteristic | Entire US | Healthiest Region† | Southern US | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mortality (deaths/100,000) | |||||||||
| 25–64 yrs | 330 | 414 | 276 (W) | 315 (NE) | 370 | 490 | 56% ↑ | 32%↑ | 78%↑ |
| ≥65 yrs | 4222 | 4830 | 3914 (W) | 4315 (W) | 4487 | 5184 | 20%↑ | 16%↑ | 32%↑ |
| Due to CAD, ≥20 yr | 193 | 207 | 173 (W) | 155 (W) | 180 | 228 | 47%↑ | 27%↑ | 32%↑ |
| Due to COPD, ≥20 yr | 56 | 82 | 43 (NE) | 76 (NE) | 61 | 89 | 17%↑ | 46%↑ | 107%↑ |
| Due to Stroke | 43 | 51 | 34 (NE) | 43 (NE) | 48 | 57 | 33%↑ | 19%↑ | 68%↑ |
| Due to Diabetes | 23 | 26 | 21 (W) | 23 (W) | 25 | 29 | 26%↑ | 16%↑ | 38%↑ |
| Morbidity, % | |||||||||
| Major Psych Distress, 30days | 5 | 6 | 4 (S) | 4 (MW) | 4 | 7 | 75%↑ | 75% ↑ | 75%↑ |
| Chronic Physical Limitation | 13 | 19 | 12 (NE) | 15 (MW) | 13 | 21 | 40%↑ | 62%↑ | 75%↑ |
| Risk Factors, % | |||||||||
| Poverty | 18 | 19 | 16 (W) | 15 (NE) | 12 | 22 | 47%↑ | 83%↑ | 38%↑ |
| Adiposity | 27 | 37 | 25 (W) | 34 (MW) | 30 | 37 | 9%↑ | 23%↑ | 48%↑ |
| Smokers, ≥18 yrs | 16 | 27 | 13 (W) | 23 (W) | 17 | 30 | 30%↑ | 76%↑ | 131%↑ |
| Smokers, adolescent | 5 | 11 | 5 (NE) | 9 (W) | 5 | 11 | 22%↑ | 120%↑ | 120%↑ |
| Physically inactive | 32 | 41 | 28 (W) | 27 (W) | 33 | 45 | 67%↑ | 36%↑ | 61%↑ |
| Health Care Access | |||||||||
| Uninsured, % <65 yrs | 20 | 23 | 11 (NE) | 14 (NE) | 22 | 25 | 79%↑ | 14%↑ | 127%↑ |
| Physicians/100,000 | 381 | 77 | 496 (NE) | 124 (NE) | 370 | 68 | 45%↓ | 82%↓ | 86%↓ |
Health Penalty = mortality penalty + health span penalty;
Northeast (NE), West (W), Midwest (MW), South (S). Urban = Large Central (inner cities). Rural = Non-Core (small rural) Psych=psychological, CAD= Coronary Artery Disease, COPD= Chronic Obstructive Pulmonary Disease. Rates are age-adjusted.
Note. Evidence of the Rural Health Penalty in Southern United States (Centers for Disease Control and Prevention; Meit et al., 2014).
3.1. Southern Rural Health Penalty
In addition to urban-rural geographic differences in mortality rates, people living in rural areas in the South of the US are also less healthy compared to both their urban counterparts and other rural areas, including experiencing a greater burden of risk factors and higher rates of morbidity due to chronic diseases (Matthews et al., 2017; Meit et al., 2014; Murray et al., 2005; Singh et al., 2011; U.S. Census Bureau 2011–2015 American Community Survey 5-Year Estimates, 2015). Research investigating persistent deaths in the US reported there were 417 persistently ‘high’ mortality counties, which was defined as greater than 1 standard deviation above the national mean. Of the ‘high’ mortality counties, 88 percent were concentrated in the South (W. James et al., 2018). The high rate of mortality in the South is exacerbated in rural areas, whereby rural counties in East South Central experience an excess rate of 1,000 deaths per 100,000, compared to 740 per 100,000 in the urban West North Central, and 840 per 100,000 in all rural areas (W. James et al., 2018). The trend of high mortality in rural southern areas has persisted since the late 1960s and is worsening over time (W. James et al., 2018).
4. Factors that Influence Rural Health Disparities
Rural-urban health disparities, especially in southern parts of the US, can be explained by multiple interacting factors, including individual, interpersonal, social, and structural reasons.
4.1. Geospatial Clustering of Individual Risk Factors
Geographic variation between rural regions may be caused by geospatial clustering of individual level risk factors in certain rural areas (Howard, 2013). Some geospatial mortality differences occur due to individuals in particular areas experiencing different levels of individual level risk factors and dissimilar effects of these risk factors on health outcomes (Gebreab et al., 2015; Howard, 2013; Roth et al., 2017). Further investigation of research gaps in geospatial clustering of individual level risk factors may increase our understanding of geographic variation in morbidity and mortality between rural areas.
4.2. Macrosocial and Structural Determinants of Health
Macrosocial determinants of health are the upstream, systemic, and structural conditions which influence population health and drive health inequities (Lantz, 2019). These include race, structural racism, and intersectionality; education; socioeconomic status and poverty; access to healthcare, and its quality; and the built environment.
Upstream determinants of health are social conditions that influence mortality and morbidity, such as socioeconomic status, neighborhood characteristics, and social inequities (Hummer & Hernandez, 2013; Link & Phelan, 1995). Proximal or downstream determinants of health are often individual level risk factors that influence disease, such as physical activity, alcohol consumption, and diet (Hummer & Hernandez, 2013; Link & Phelan, 1995). Researchers often focus on proximal individual level risk factors to understand health disparities, whereas fewer studies investigate how the context of people’s lives impacts their health (Diez-Roux, 1998; Roux, Mujahid, Hirsch, Moore, & Moore, 2016). Contextual factors include upstream macrosocial and economic determinants of health, such as environmental, societal, neighborhood, and structural influences on health outcomes (Hale, Probst, & Robertson, 2015; Patel, Ali, Narayan, & Mehta, 2016; Roux et al., 2016). Macrosocial determinants of health may explain both urban-rural health inequities and differences between rural regions.
4.2.1. Differences According to Race
All races experience higher mortality rates in rural areas compared to urban areas throughout the US (Cosby et al., 2019; Cossman et al., 2016; W. James & Cossman, 2017; W. James et al., 2018). However, people of color in the rural South, and particularly the Appalachia and the Mississippi Delta region, fare worst (C. V. James et al., 2017; W. James et al., 2018; Murray et al., 2005). People of color have the highest cardiovascular disease, stroke, and cancer mortality rates (C. V. James et al., 2017; Singh et al., 2011; U.S. Census Bureau 2011–2015 American Community Survey 5-Year Estimates, 2015). Non-white populations also tend to have less education, are more economically stressed, report higher rates of illness, and lack health insurance (C. V. James et al., 2017; Meit et al., 2014).
Moreover, evidence indicates that rural health disparities are different between groups of people of color, yet this is rarely investigated (C. V. James et al., 2017). When research does consider racial health disparities, it often focuses exclusively on Black and White communities and ignores other people of color or compares Non-Hispanic White populations to all people of color as one group, thereby masking important variations in health between different nonwhite groups. A recent publication on rural racial health disparities from the 2012–2015 Behavioral Risk Factor Surveillance System (BRFSS) questionnaire reported differences between different groups of people of color for health behaviors and rates of disease (C. V. James et al., 2017). Among all races in rural areas, American Indians/ Alaska Natives had the highest rates of physical inactivity due to physical, mental, or emotional problems (28.5%); Hispanic individuals had the lowest rate of healthcare coverage (61.1%); Non-Hispanic Whites had the highest rates of binge drinking (16.3%); and Black individuals had the highest rates of adiposity (45.9%) (C. V. James et al., 2017).
4.3. Race and Intersectionality
Furthermore, there are also differences in health outcomes within groups of people from the same race (Murray et al., 2006). For example, rural blacks in the south experience higher mortality rates than urban blacks in Middle America (Murray et al., 2006), and low-income whites in the Appalachia and Mississippi Valley have a lower life expectancy than low-income rural whites in the Midwest (Murray et al., 2006).
Individuals have multiple identities based on their race, age, geography, socioeconomic status, education, gender, sexuality, and other identity traits, and these identities intersect to create differences in health outcomes within the same racial groups (López & Gadsden, 2016). Intersectionality is a sociological term that can be useful for understanding differences within the same racial groups. Intersectionality was coined by Black American feminist scholars who sought to understand how different social identities interacted together with structures of power and oppression to create inequities, instead of focusing on discrete categories, such as sex, gender, race, or class alone (Crenshaw, 2018; Hill Collins, 1990). Some identity traits are protective factors for diseases, life expectancy, and mortality, such as having a high socioeconomic status, education, and being white, while others may act as risk factors, such as having a low socioeconomic status, or living in a rural area (Singh & Siahpush, 2014a, 2014b).
To illustrate how different identities interact to create health risks, one study in the US observed that life expectancy differed according to race, income, and geography (See Table 3) (Singh & Siahpush, 2014b). Yet, if we only assess life expectancy according to race and ignore income and rurality, we could miss potentially important differences within racial groups.
Table 3:
Life expectancy (in years) by metropolitan status, poverty level, and race, U.S., 2005–2009
| Urban (Both Genders) | Rural (Both Genders) | |
|---|---|---|
| Race/ Ethnicity | ||
| All whites | 79.2 | 77.2 |
| All blacks | 74.2 | 72.8 |
| All American Indians/Alaska Natives | 85.8 | 74.8 |
| All Asians and Pacific Islanders | 86.9 | 84.9 |
| All Hispanics | 83.1 | 82.2 |
| Race/Ethnicity and Poverty | ||
| High income whites | 79.9 | 78.8 |
| High income blacks | 76.1 | 76.7 |
| High income American Indians/ Alaska Natives | 85.7 | 77.3 |
| High income Asians and Pacific Islanders | 87.2 | – |
| High income Hispanics | 86.2 | – |
| Low income whites | 78.8 | 75.4 |
| Low income blacks | 74.0 | 71.6 |
| Low income American Indians/ Alaska Natives | – | 72.6 |
| Low income Asians and Pacific Islanders | 86.7 | – |
| Low income Hispanics | 81.0 | 79.8 |
Note. Life expectancy by metropolitan status, poverty level, and race in the U.S. (Singh & Siahpush, 2014b)
4.4. Structural Racism
Race-related health disparities can be partially explained by structural racism (Bailey et al., 2017; Gee & Ford, 2011; Nazroo, 2003). People of color are more likely to face unequal social conditions than white people that lead to differences in experiencing poor health outcomes (Bailey et al., 2017; Gee & Ford, 2011; Krieger, 2014; Nazroo, 2003). This may stem from structural racism, which represents “…the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice. These patterns and practices in turn reinforce discriminatory beliefs, values, and distribution of resources” (Bailey et al., 2017). Structural racism has formed over centuries and, therefore, is deeply ingrained in the beliefs, values, and behaviors of people, institutions, organizations, and governments (Bailey et al., 2017; Gee & Ford, 2011).
An example of structural racism is the current residential segregation of Black Americans in many areas of the US, which is associated with adverse health outcomes, such as poor birth outcomes, increased risk of chronic disease, and greater exposure to environmental pollutants (Bailey et al., 2017; Gee & Ford, 2011; Krieger, 2014). Residential segregation also impacts access to healthcare services and quality of healthcare as there tends to be fewer primary-care providers and specialists in predominantly Black neighborhoods (Bailey et al., 2017; Gee & Ford, 2011; Krieger, 2014).
In rural areas, especially in the South, it is important to understand how institutional policies, such as the Jim Crow laws that segregated hospitals and neighborhoods, led to differences in resource allocation between white populations and nonwhite populations, which may impact healthcare access today (Bailey et al., 2017; Jones, 2002; Kozhimannil & Henning-Smith, 2018). Structural racism may serve as an important contributor to the high rate of mortality and morbidity among people of color living in the rural South.
4.5. Socioeconomic Status and Poverty
There is substantial evidence of associations between individual level poverty, income inequality, census tract-level poverty, and poor health (Auchincloss & Hadden, 2002; Shi et al., 2005; Singh & Siahpush, 2014a, 2014b). Although overall poverty rates are higher in rural compared to urban areas, there are higher concentrations of economic deprivation in certain areas, particularly in the South. Among rural counties, the South has the highest rate of poverty (20.8%), while the Northeast has the lowest prevalence of poverty (13.4%). The South also has the biggest gap between rural and urban rates of poverty, with rural southern areas averaging 6 percentage points higher than urban southern areas (United States Department of Agriculture, 2019).
Socioeconomic status can be measured in absolute or relative terms, with research indicating that relative poverty — comparing an individual/households’ socioeconomic status in relation to other people — is an important indicator of health outcomes (Shi et al., 2005). Income inequality is often measured by the Gini coefficient (Yitzhaki, 1979), or the Index of Concentration at the Extremes (ICE) (Krieger et al., 2016; Massey, 2001). The Gini coefficient measures income distribution where high values specify greater difference in income distribution (Yitzhaki, 1979). The Index of Concentration at the Extremes (ICE) measures the degree of economic privilege and deprivation at both small and large geographic areas, where low values indicate high deprivation (Krieger et al., 2016; Massey, 2001). One study found that rural counties had a higher Gini coefficient compared to urban counties, indicating higher income inequality (Shi et al., 2005). The study also reported that counties with a high Gini coefficient also had high rates of mortality (Shi et al., 2005). Specifically, those who lived in rural areas with the highest income inequality had 11% higher all-cause mortality, 9% higher heart disease mortality, and 9% higher cancer mortality in comparison to those who lived in rural areas with the lowest income inequality (Shi et al., 2005).
Comparing groups from the “eight Americas” (Murray et al., 2006), Low Income Whites in the Appalachia and Mississippi Valley experience a 12% higher mortality rate than white individuals with above-average income from Middle America, after adjusting for age and sex (Limdi et al., 2016). Moreover, Middle American Blacks and High Risk Urban Blacks experienced lower mortality compared to Southern Low Income Rural Blacks (13% lower and 9% lower, respectively) (Limdi et al., 2016). Higher mortality rates were reported for both Black and White low-income populations, with highest rates being reported among Southern Low Income Rural Blacks, highlighting the interacting factors of race, income, and geography (Limdi et al., 2016).
4.6. Access to Healthcare
In rural areas, there are often barriers to accessing healthcare, including limited healthcare supply, long distances from people’s homes to healthcare facilities, lack of insurance, and high costs of healthcare (Laditka, Laditka, & Probst, 2005; Probst, Laditka, & Laditka, 2009). Areas in the rural South have the lowest supply of physicians compared to both urban areas in the South and other rural places in the US. Specifically, in the rural South there were 68 physicians per 100,000 compared to 370 per 100,000 in urban areas in the South, and 124 physicians per 100,000 in rural areas in the Northeast (Meit et al., 2014).
Rural areas also tend to have a lower supply of all healthcare professionals, including mental health professionals and services compared to urban areas (Cherry, Albert, & McCaig, 2018; Olfson, 2016). As of 2020, the Bureau of Health Workforce reported in their Designated HSPA Quarterly Summary that rural areas have a higher percentage of health professional shortage areas compared to urban areas for primary care providers (61% vs 32%), mental health professionals (58% vs 34%), and dental care providers (62% vs 32%) (Bureau of Health Workforce: HRSA and US Department of Health & Human Services., 2020).
Health insurance coverage also varies by urbanization level, with the most rural counties having higher levels of uninsured people, and lower proportions of people with private insurance coverage compared to urban areas (Meit et al., 2014). In the South, 24.5% of people under the age of 65 years did not have health insurance in rural counties, compared to 17.6% of people in large fringe metropolitan counties (suburbs) and 22.1% of people in large central metropolitan counties (inner cities) (Meit et al., 2014).
4.7. Built Environment
The built environment, including access to healthy food retailers and recreational facilities, can influence people’s physical activity levels, diet, and other behaviors related to adiposity (Gordon-Larsen, Nelson, Page, & Popkin, 2006). Consumption of fruits and vegetables may reduce peoples’ risk of developing chronic diseases, including heart disease, stroke, and diabetes (He, Nowson, Lucas, & MacGregor, 2007; Montonen, Knekt, Jarvinen, & Reunanen, 2004). People who live in areas close to healthy food retailers, such as large grocery stores, may have a healthier diet (Larson, Story, & Nelson, 2009). However, access to healthy retailers is not equally distributed, with rural people in the South being approximately four times less likely to have access to a healthy food retailer compared to those living in urban areas in the South (Edwards, Jilcott, Floyd, & Moore, 2011; Grimm, Moore, & Scanlon, 2013).
Physical activity is also influenced by the built environment, for example access to recreational facilities, including parks, sports fields, and greenways is associated with lower BMI (Pitts et al., 2013). Individuals living in the rural South have the lowest prevalence of meeting physical activity guidelines compared to urban areas in the South (14.7%, and 22.5% respectively) (Whitfield, 2019). Furthermore, rural populations in other regions have a higher rate of meeting national physical activity guidelines compared to populations in the rural South (Northeast:24.2%, Midwest: 19.9%, West:25.4%) (Whitfield, 2019).
5. Syndemics
The contexts and places where people are born, live, work and age are powerful predictors of their health, and can render entire communities vulnerable to syndemic clusters of chronic health problems, including heart, lung, blood and sleep disease (Gebreab et al., 2015; Murray et al., 2006; Roth et al., 2017; Singer, 2009).
Syndemics are clusters of synergistic health problems precipitated by structural inequalities associated with poverty, racism, and other forms of social exclusion, displacement, exploitation, and oppression (Hart & Horton, 2017; Lewis, Williams, Tamene, & Clark, 2014; Lichtman et al., 2014; Mendenhall, 2017; Roux et al., 2016; Singer, 2009; Starfield, 2007; Tsai, Mendenhall, Trostle, & Kawachi, 2017; Vaccarino & Bremner, 2013; Willen, Knipper, Abadía-Barrero, & Davidovitch, 2017). The syndemics concept challenges mainstream approaches to treating diseases as distinct entities or decontextualized states of comorbidity (Hart & Horton, 2017; Mendenhall, 2017; Singer, 2009; Tsai et al., 2017; Willen et al., 2017). It also questions the model of solely treating individuals rather than communities. Syndemics highlights why morbid states cluster in ‘environments of risk’ and illustrates how the contextual, social, economic, political, psychological, and biological pathways through which morbid states interact can reinforce and exacerbate each other (Barnidge et al., 2013; Boehmer, Lovegreen, Haire-Joshu, & Brownson, 2006; Hart & Horton, 2017; Mendenhall, 2017; Singer, 2009; Starfield, 2007; Trujillo & Plough, 2016; Tsai et al., 2017; Willen et al., 2017).
In rural areas, there are often higher levels of unemployment, low education, and poverty compared to urban areas, factors that cluster together in certain communities (C. V. James et al., 2017; Meit et al., 2014; Shi et al., 2005). There are also regional differences, whereby individuals in the rural South tend to experience higher rates of structural inequalities, such as poverty and low educational attainment, compared to other rural regions (Meit et al., 2014; United States Department of Agriculture, 2019). These structural inequalities that cluster together may explain why rural populations in the South have a high prevalence of risk factors for chronic disease, and also morbidity and mortality compared to their urban peers and individuals in other rural regions (Cossman et al., 2016; W. James et al., 2018; Murray et al., 2006). Syndemics is a useful concept for understanding health disparities at multiple levels, including variation by urban-rural areas, regional rural areas, and even within rural areas, such as the rural South.
6. Future Research Directions
Despite the wealth of research investigating rural health disparities, additional research should focus on regional differences between rural places. Moreover, there are potential explanatory variables that may explain rural health disparities that need to be explored in the context of southern rural populations, including measuring individual and community level resilience, improving measurements of macrosocial determinants of health, and using and assessing the validity of indexes to measure health disparities between different populations.
6.1. In-Depth Research: Regional Health Disparities
Future research should investigate health disparities by region, rural-urban status, and individual characteristics to create a more in-depth understanding of rural health in the US. It is also important for future research to examine why health disparities exist in the rural South by studying macrosocial and structural determinants of health. Rural geospatial differences in health inequities is a vital field of research, which requires further research for public health interventions to better serve underserved vulnerable communities in the rural South of the US.
6.2. Understanding and Measuring Resilience
The allostasis-resilience framework measures resilience, specifically how individuals respond to stress, which in turn may impact health outcomes. Allostasis is the physiological response to external stressors, where the brain and body achieves stability by adapting to changes caused by stress (Gustafsson et al., 2014; Schulz et al., 2012). However, over time adaptation has a cumulative cost on the body, which leads to pathophysiological changes called allostatic load or ‘wear and tear’. Although most people have some degree of allostatic load, those who experience chronic stress experience greater ‘wear and tear’ on their body (Gustafsson et al., 2014; Schulz et al., 2012). Allostatic load can reduce the effectiveness of the body to respond to stressors, which can increase an individual’s susceptibility to disease and illness (Gustafsson et al., 2014; Schulz et al., 2012).
People’s ability to cope with stressors may be mediated by differing levels of resilience and vulnerability (Karatsoreos & McEwen, 2011). Individuals can be resilient to changes that may cause stress, whereby they resist, adapt, or transform in response to stressors (Daskalakis, Bagot, Parker, Vinkers, & de Kloet, 2013; Karatsoreos & McEwen, 2011). In contrast, individuals may be vulnerable to stressors, which can result in ineffective adaptive responses (Daskalakis et al., 2013). An individual’s ability to effectively respond to stressors is dependent on multiple factors, including their genetic make-up and their life experiences (Daskalakis et al., 2013; Karatsoreos & McEwen, 2011). Those who experience neighborhood poverty, household poverty, low socioeconomic status, racism, educational disadvantage, or perceived stress, tend to have a higher allostatic load compared to those who do not experience these inequities (Gustafsson et al., 2014; Schulz et al., 2012).
There is limited research on how place of residence (urban, rural) impacts allostatic load (Brody et al., 2013). One study examined allostatic load in African American youths living in the rural South to determine factors related to rural residence that may increase allostatic load, including chronic poverty, limited occupational and educational opportunities, interpersonal and structural racism, and challenges in accessing health care (Brody et al., 2013). Participants with protective factors, such as protective parenting experienced a lower allostatic load and high behavioral and emotional functioning (Brody et al., 2013). In contrast, youth who had fewer protective factors experienced a higher allostatic load and lower levels of behavioral and emotional functioning (Brody et al., 2013). A high allostatic load may be a plausible explanation for the southern rural health penalty, which needs to be further tested and validated among populations in the rural South.
6.3. Improving Measurements of Macrosocial and Structural Determinants of Health
Public health research that focuses on health behaviors tends to ignore the contexts in which people live, and this also risks shaming people for their health behaviors and poor health outcomes without understanding what shaped their decisions (including risk perception) to adopt certain health behaviors (Braveman & Gottlieb, 2014; Martin, 2001). It is important to consider the underlying macrosocial determinants that influence health behaviors and health outcomes (Solar & Irwin, 2010). Structural determinants, including racism, poverty, and sexism influence health through intermediate determinants, such as material circumstances and psychosocial circumstances (Solar & Irwin, 2010). These intermediate determinants can be further divided into specific examples, such as housing and neighborhood quality, consuming power (financial ability to buy healthy food), social support, stressful living circumstances, coping skills, health services use, and health behaviors (Solar & Irwin, 2010).
Measuring both structural and intermediate determinants of health among rural southern populations may provide some explanations for the high morbidity and mortality in these areas compared to other rural regions and individuals living in urban southern places.
6.4. Using and Measuring Validity of Indexes in Southern Rural Populations
Creating indexes to measure macrosocial determinants of health is important for investigating health disparities both between different groups and within groups. Hale and colleagues recently developed an area deprivation index, which includes multiple social determinants of health, to measure county-level deprivation (Hale et al., 2015). The index includes 5 measures of deprivation (income, poverty, unemployment, high school graduation rate, single parent home) (Hale et al., 2015). The area deprivation index accounts for numerous social determinants of health collectively. From this index, the authors inferred that rural counties are disproportionally affected by high levels of deprivation with 80% of the most deprived counties being in rural areas compared to 20% in urban areas (Hale et al., 2015). However, not all rural counties have high levels of deprivation, with the most deprived areas clustering in the South, Southeast, and West of the United States (Hale et al., 2015).
Another useful index defined earlier is the Index of Concentration at the Extremes (ICE) (Krieger et al., 2016; Massey, 2001). Although ICE has largely been used in social science research, it can also be useful for public health research. The ICE is particularly favorable because it examines both socioeconomic and racial data concomitantly (Krieger et al., 2016; Massey, 2001). As ICE can measure inequality at the neighborhood level (Krieger et al., 2016; Massey, 2001), it is a suitable tool to be used in southern rural communities to measure two predictors—income and race—of health inequities.
Another tool for measuring factors that impact health outcomes is the Rural Active Living Assessment (RALA) tools created by researchers at the Maine Rural Health Research Center (Yousefian et al., 2010). RALA tools assess how physical environmental features, town characteristics, community programs, and policies impact rural residents’ physical activity levels (Yousefian et al., 2010). The RALA tools may be useful in examining physical activity-friendliness between different rural regions in the US. RALA tools could also guide new public health interventions to improve the health of southern rural communities.
Future research could use indexes and tools to assess their face, construct, and content validity when applied to communities in the rural South.
7. Conclusion
The southern rural health penalty is a public health issue that merits further research. The aim of the review is threefold. Firstly, we have illustrated some key health disparities between southern rural communities and their urban counterparts and between southern rural regions and their non-southern rural equivalents. Secondly, we have highlighted the role of macrosocial determinants as potential reasons why health inequities exist between southern rural and southern urban populations, and southern rural individuals and those in other rural regions. Finally, we have attempted to track the history of the urban mortality penalty, which transitioned to the rural mortality penalty from the late 19th century to present day.
Research Highlights.
Rural health and mortality disparities are worse in the southern US compared to other rural regions
Southern rural health inequities may be explained by macrosocial determinants of health
Non-white populations tend to have poorer health than white populations in the rural Southern US
A review and potential explanations of rural health disparities between southern US populations and their non-southern counterparts
Highlights.
Rural health disparities are worse in the rural south compared to other rural areas
Southern rural health inequities may be explained by macrosocial determinants of health
In the rural south, non-white populations often have worse health than whites
History of the transition of the urban-rural mortality penalty in the US
Rural mortality rates are worse in the rural south compared to other rural areas
Acknowledgements
Charlotte E. Miller and Dr. Ramachandran S. Vasan acknowledge their partial support for this work from National Heart, Lung and Blood Institute (NHLBI) grant U01HL146382, The RURAL Cohort Study. Dr. Ramachandran S. Vasan also acknowledges his partial support from Evans Medical Foundation and the Jay and Louis Coffman Endowment from the Department of Medicine, Boston University School of Medicine.
Appendix
Methods
To create Table 1, we examined the Vital Statistics Annual Reports from 1890–1964 to source data on urban and rural mortality rates for the total population and also by race. (U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division) The Vital Statistics annual reports used varying classifications of “urban” and “rural” areas in the late 19th and early 20th century, which creates challenges in comparing mortality trends over this time period.
To determine how we defined “urban” and “rural” for Table 1, we examined how “urban” and “rural” was classified in different annual reports (See Table 1B). Over time, the annual reports began to stratify “urban” into different subcategories based on population size. In an attempt to make comparisons, we only reported data in Table 1 where the annual reports specified the mortality rate by population size. We also used the definition of “rural” and “urban” from 1900 onwards where “urban’ was defined as cities of 10,000 or more inhabitants and all other areas were classified as “rural”. For Vital Statistics reports that included populations of 2,500 to 10,000 in their definition of “urban” we recalculated the mortality rate to include this population as “rural” rather than “urban”.
Table 1B:
Definitions of “Urban” and “Rural” in Vital Statistics Annual Reports
| Urban | Rural | |
|---|---|---|
| 1900–1929 | Cities of 10,000 or more inhabitants | All other areas |
| 1930–1934 | Cities of 2,500–10,000 inhabitants Cities of 10,000 or more inhabitants |
All other areas |
| 1935–1940 | Cities of 2,500–10,000 inhabitants Cities of 10,000–25,000 inhabitants Cities of 25,000–100,000 inhabitants Cities of 100,000 or more inhabitants |
All other areas |
| 1941–1959 | Cities of 2,500 or more inhabitants | All other areas |
| 1960 | Cities of 2,500–10,000 inhabitants Cities of 10,000–25,000 inhabitants Cities of 25,000–50,000 inhabitants Cities of 50,000–100,000 inhabitants Cities of 100,000–250,000 inhabitants Cities of 250,000–500,000 inhabitants Cities of 500,000–1,000,000 inhabitants Cities of 1,000,000 or more inhabitants |
All other areas |
(U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division., 1947, 1954, 1963)
Note: In general, each annual census report followed the classifications detailed above when reporting rural and urban mortality rates by total population and race, however there are some variations between annual reports.
From 1950 onwards, the Vital Statistics began classifying counties as metropolitan or non-metropolitan, and within these broader categories defining areas as urban or rural (U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division., 1954). As this was a new classification, we did not report data stratified by metropolitan and non-metropolitan areas. In addition, the Vital Statistics from 1941–1959 rarely stratified mortality rates by population size. Instead they provided mortality rates for “urban” and “rural” areas, whereby they defined “urban” as areas of 2,500 or more inhabitants and all other areas as “rural”, therefore we have not included 1950 data in Table 1. However, in 1960 the Vital Statistics reported mortality rates by degrees of “urbanization” according to population size (See Table 1B). This stratified data is similar to how data was reported in other years in Table 1, and therefore we included this data in our table.
It is also important to note that the Vital Statistics in 1960 stated that urban mortality was higher than rural mortality (U. S. National Center for Health Statistics (US). National Vital Statistics Division, & United States Bureau of the Census, Vital Statistics Division., 1963). This difference is more marked if we classify “urban” as cities of 2,500 or more inhabitants, however if “urban” is defined as cities of 10,000 or more inhabitants the difference between urban and rural mortality declines.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Bibliography
- Auchincloss AH, & Hadden W (2002). The Health Effects of Rural-Urban Residence and Concentrated Poverty. Journal of Rural Health, 18(2), 319–336. doi: 10.1111/j.1748-0361.2002.tb00894.x [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequities in the USA: evidence and interventions. The Lancet, 389(10077), 1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Barnidge EK, Radvanyi C, Duggan K, Motton F, Wiggs I, Baker EA, & Brownson RC (2013). Understanding and addressing barriers to implementation of environmental and policy interventions to support physical activity and healthy eating in rural communities. J Rural Health, 29(1), 97–105. doi: 10.1111/j.1748-0361.2012.00431.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer E (2010). Vision 2020-Rural Health: The Startling Statistics September-October 2010. [PubMed]
- Boehmer TK, Lovegreen SL, Haire-Joshu D, & Brownson RC (2006). What constitutes an obesogenic environment in rural communities? Am J Health Promot, 20(6), 411–421. doi: 10.4278/0890-1171-20.6.411 [DOI] [PubMed] [Google Scholar]
- Braveman P, & Gottlieb L (2014). The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep, 129 Suppl 2, 19–31. doi: 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen YF, Kogan SM, Evans GW, Beach SR, …. Philibert RA (2013). Cumulative socioeconomic status risk, allostatic load, and adjustment: a prospective latent profile analysis with contextual and genetic protective factors. Dev Psychol, 49(5), 913–927. doi: 10.1037/a0028847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Health Workforce: HRSA and US Department of Health & Human Services. (2020). Designated Health Professional Shortage Areas Statistics: Second Quarter of Fiscal Year 2020 Designated HPSA Quarterly Summary. Retrieved from https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport
- Case A, & Deaton A (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences, 112(49), 15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, N. C. f. H. S. Compressed Mortality File 1999–2016 on CDC WONDER Online Database, released June 2017. Data are from the Compressed Mortality File 1999–2016 Series 20 No. 2U, 2016, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program Retrieved from http://wonder.cdc.gov/cmf-icd10.html
- Cherry D, Albert M, & McCaig L (2018). Mental Health-related Physician Office Visits by Adults Aged 18 and Over: United States, 2012–2014. NCHS data brief(311), 1–8. [PubMed] [Google Scholar]
- Cosby AG, McDoom-Echebiri MM, James W, Khandekar H, Brown W, & Hanna HL (2019). Growth and Persistence of Place-Based Mortality in the United States: The Rural Mortality Penalty. American journal of public health, 109(1), 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cossman J, James W, & Wolf JK (2016). Race and Rural: An Investigation of the Rural Mortality Penalty and the Role of Public Health Infrastructure Paper presented at the Population Association of America, Washington DC: https://paa.confex.com/paa/2016/mediafile/ExtendedAbstract/Paper4420/PAA%202016%20--%20Rural%20Race%20and%20Public%20Health%20Infrastructure.pdf [Google Scholar]
- Cossman J, James W, & Wolf JK (2017). The differential effects of rural health care access on race-specific mortality. SSM - Population Health, 3, 618–623. doi: 10.1016/j.ssmph.2017.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (2018). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory, and antiracist politics [1989] In Feminist legal theory (pp. 57–80): Routledge. [Google Scholar]
- Cromartie J (2018). Rural America At A Glance 2018 Edition. Retrieved from https://www.ers.usda.gov/webdocs/publications/90556/eib-200.pdf
- Daskalakis NP, Bagot RC, Parker KJ, Vinkers CH, & de Kloet ER (2013). The three-hit concept of vulnerability and resilience: toward understanding adaptation to early-life adversity outcome. Psychoneuroendocrinology, 38(9), 1858–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV (1998). Bringing context back into epidemiology: variables and fallacies in multilevel analysis. American journal of public health, 88(2), 216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Mackenbach JP, van Lenthe FJ, … Murray CJ (2017). Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA internal medicine, 177(7), 1003–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards MB, Jilcott SB, Floyd MF, & Moore JB (2011). County-level disparities in access to recreational resources and associations with adult obesity. Journal of Park and Recreation Administration, 29(2). [Google Scholar]
- Gebreab SY, Davis SK, Symanzik J, Mensah GA, Gibbons GH, & Diez-Roux AV (2015). Geographic variations in cardiovascular health in the United States: Contributions of state-and individual-level factors. Journal of the American Heart Association, 4(6), e001673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, & Ford CL (2011). Structural racism and health inequities: old issues, new directions. Du Bois review: social science research on race, 8(1), 115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, & Popkin BM (2006). Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics, 117(2), 417–424. doi: 10.1542/peds.2005-0058 [DOI] [PubMed] [Google Scholar]
- Grimm KA, Moore LV, & Scanlon KS (2013). Access to healthier food retailers - United States, 2011. MMWR Suppl, 62(3), 20–26. [PubMed] [Google Scholar]
- Gustafsson PE., San Sebastian M., Janlert U., Theorell T., Westerlund H., & Hammarström A. (2014). Life-course accumulation of neighborhood disadvantage and allostatic load: empirical integration of three social determinants of health frameworks. American journal of public health, 104(5), 904–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines MR (2001). The Urban Mortality Transition in the United States, 1800–1940. Annales de démographie historique(1), 33–64. [Google Scholar]
- Hale N, Probst J, & Robertson A (2015). Area deprivation is higher among rural counties-but not all rural counties are deprived. Area deprivation is higher among rural counties-but not all rural counties are deprived.
- Hart L, & Horton R (2017). Syndemics: committing to a healthier future. The Lancet, 389(10072), 888–889. [DOI] [PubMed] [Google Scholar]
- He FJ, Nowson CA, Lucas M, & MacGregor GA (2007). Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens, 21(9), 717–728. doi: 10.1038/sj.jhh.1002212 [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration. (2017, January). Defining Rural Population. Retrieved from https://www.hrsa.gov/rural-health/about-us/definition/index.html
- Hill Collins P (1990). Black feminist thought : knowledge, consciousness, and the politics of empowerment. Boston: Boston: : Unwin Hyman. [Google Scholar]
- Housing Assistance Council. (2011). Population Change in Rural America. Retrieved from http://www.ruralhome.org/storage/research_notes/rural_research_note_population_change.pdf
- Housing Assistance Council. (2012). Race & ethnicity in rural America. Retrieved from http://www.ruralhome.org/storage/research_notes/rrn-race-and-ethnicity-web.pdf
- Howard G (2013). Ancel keys lecture: adventures (and misadventures) in understanding (and reducing) disparities in stroke mortality. Stroke, 44(11), 3254–3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer RA, & Hernandez EM (2013). The effect of educational attainment on adult mortality in the United States. Population bulletin, 68(1), 1. [PMC free article] [PubMed] [Google Scholar]
- James CV, Moonesinghe R, Wilson-Frederick SM, Hall JE, Penman-Aguilar A, & Bouye K (2017). Racial/Ethnic Health Disparities Among Rural Adults—United States, 2012–2015. MMWR Surveillance Summaries, 66(23), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James W (2014). All rural places are not created equal: revisiting the rural mortality penalty in the United States. American journal of public health, 104(11), 2122–2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James W, & Cossman J (2017). Long-Term Trends in Black and White Mortality in the Rural United States: Evidence of a Race-Specific Rural Mortality Penalty. The Journal of Rural Health, 33(1), 21–31. [DOI] [PubMed] [Google Scholar]
- James W, Cossman J, & Wolf JK (2018). Persistence of death in the United States: The remarkably different mortality patterns between America’s Heartland and Dixieland. Demographic Research, 39, 897–910. [Google Scholar]
- Jones CP (2002). Confronting institutionalized racism. Phylon (1960-), 7–22. [Google Scholar]
- Karatsoreos IN, & McEwen BS (2011). Psychobiological allostasis: resistance, resilience and vulnerability. Trends in cognitive sciences, 15(12), 576–584. [DOI] [PubMed] [Google Scholar]
- Kozhimannil KB, & Henning-Smith C (2018). Racism and Health in Rural America. Journal of health care for the poor and underserved, 29(1), 35–43. [DOI] [PubMed] [Google Scholar]
- Krieger N (2014). Discrimination and health inequities. International Journal of Health Services, 44(4), 643–710. [DOI] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, & Van Wye G (2016). Public health monitoring of privilege and deprivation with the index of concentration at the extremes. American journal of public health, 106(2), 256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB, & Probst JC (2005). More may be better: evidence of a negative relationship between physician supply and hospitalization for ambulatory care sensitive conditions. Health Serv Res, 40(4), 1148–1166. doi: 10.1111/j.1475-6773.2005.00403.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz PM (2019). The Medicalization of Population Health: Who Will Stay Upstream? Milbank Q, 97(1), 36–39. doi: 10.1111/1468-0009.12363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson NI, Story MT, & Nelson MC (2009). Neighborhood environments: disparities in access to healthy foods in the US. American journal of preventive medicine, 36(1), 74–81. e10. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Williams DR, Tamene M, & Clark CR (2014). Self-Reported Experiences of Discrimination and Cardiovascular Disease. Curr Cardiovasc Risk Rep, 8(1), 365. doi: 10.1007/s12170-013-0365-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, … Stroke N (2014). Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation, 129(12), 1350–1369. doi: 10.1161/CIR.0000000000000019 [DOI] [PubMed] [Google Scholar]
- Limdi NA, Howard VJ, Higginbotham J, Parton J, Safford MM, & Howard G (2016). US mortality: influence of race, geography and cardiovascular risk among participants in the population-based REGARDS cohort. Journal of racial and ethnic health disparities, 3(4), 599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, & Phelan J (1995). Social conditions as fundamental causes of disease. Journal of health and social behavior, 80–94. [PubMed] [Google Scholar]
- López N, & Gadsden VL (2016). Health inequities, social determinants, and intersectionality. In.
- Martin MW (2001). Responsibility for health and blaming victims. Journal of Medical Humanities, 22(2), 95–114. [Google Scholar]
- Massey DS (2001). The prodigal paradigm returns: Ecology comes back to sociology. Does it take a village, 41–48. [Google Scholar]
- Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, … Giles WH (2017). Health-Related Behaviors by Urban-Rural County Classification - United States, 2013. MMWR Surveill Summ, 66(5), 1–8. Retrieved from doi: 10.15585/mmwr.ss6605a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meit M, Knudson A, Gilbert T, Yu AT-C, Tanenbaum E, Ormson E, & Popat M (2014). The 2014 update of the rural-urban chartbook. Bethesda, MD: Rural Health Reform Policy Research Center. [Google Scholar]
- Mendenhall E (2017). Syndemics: a new path for global health research. The Lancet, 389(10072), 889–891. [DOI] [PubMed] [Google Scholar]
- Montonen J, Knekt P, Jarvinen R, & Reunanen A (2004). Dietary antioxidant intake and risk of type 2 diabetes. Diabetes Care, 27(2), 362–366. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Kulkarni S, & Ezzati M (2005). Eight Americas: new perspectives on U.S. health disparities. Am J Prev Med, 29(5 Suppl 1), 4–10. doi: 10.1016/j.amepre.2005.07.031 [DOI] [PubMed] [Google Scholar]
- Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, & Ezzati M (2006). Eight Americas: Investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med, 3(9), e260. doi: 10.1371/journal.pmed.0030260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1890–1938). Vital Statistics of the United States: 1890–1938. Retrieved from https://www.cdc.gov/nchs/products/vsus/vsus_1890_1938.htm
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1939–1964). Vital Statistics of the United States: 1939–1964. Retrieved from https://www.cdc.gov/nchs/products/vsus/vsus_1939_1964.htm
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1902). Twelfth Census of the United States, Taken in the Year 1900. Volume III. Part I. Analysis and Ratio Tables Retrieved from https://www.cdc.gov/nchs/data/vsushistorical/vsush_1900_3.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1923). Mortality Rates 1910–1920. With Population of the Federal Censuses of 1910 and 1920 and Intercensal Estimates of the Population Retrieved from https://www.cdc.gov/nchs/data/vsushistorical/mortrates_1910-1920.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1927). Mortality Statistics 1925. Twenty-Sixth Annual Report. Part I. Summary and Rate Tables and General Tables for the Death Registration Area in Continental United States, with Supplemental Statistics for Hawaii and the Virgin Islands Retrieved from https://www.cdc.gov/nchs/data/vsushistorical/mortstatsh_1925.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1932). Mortality Statistics 1929. Thirtieth Annual Report, p.62.
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1947). Vital Statistics Rates in the United States, 1900–1940. Retrieved from https://www.cdc.gov/nchs/data/vsus/vsrates1900_40.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1954). Vital Statistics Rates in the United States 1950, Volume I, Analysis and Summary Tables with Supplemental Tables for Alaska, Hawaii, Puerto Rico, and Virgin Islands. Retrieved from https://www.cdc.gov/nchs/data/vsus/vsus_1950_1.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1963). Vital Statistics of the United States, 1960. Volume II, Mortality, Part A Retrieved from https://www.cdc.gov/nchs/data/vsus/VSUS_1960_2A.pdf
- Nazroo JY (2003). The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. American journal of public health, 93(2), 277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NPR, T. R. W. J. F., and the Harvard T.H. Chan School of Public Health,. (2018). Life in Rural America. Retrieved from https://www.npr.org/buckets/HARVARD-POLL/rural-health-poll-10-15-18-updated.pdf
- Olfson M (2016). The Rise of Primary Care Physicians in the Provision of US Mental Health Care. J Health Polit Policy Law, 41(4), 559–583. doi: 10.1215/03616878-3620821 [DOI] [PubMed] [Google Scholar]
- Patel SA, Ali MK, Narayan KV, & Mehta NK (2016). County-level variation in cardiovascular disease mortality in the United States in 2009–2013: comparative assessment of contributing factors. American journal of epidemiology, 184(12), 933–942. [DOI] [PubMed] [Google Scholar]
- Pitts SBJ, Edwards MB, Moore JB, Shores KA, DuBose KD, & McGranahan D (2013). Obesity is inversely associated with natural amenities and recreation facilities per capita. Journal of physical activity and health, 10(7), 1032–1038. [DOI] [PubMed] [Google Scholar]
- Probst JC, Laditka JN, & Laditka SB (2009). Association between community health center and rural health clinic presence and county-level hospitalization rates for ambulatory care sensitive conditions: an analysis across eight US states. BMC Health Services Research, 9(1), 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth GA, Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Naghavi M, … Murray CJL (2017). Trends and Patterns of Geographic Variation in Cardiovascular Mortality Among US Counties, 1980–2014. JAMA, 317(19), 1976–1992. doi: 10.1001/jama.2017.4150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux AVD, Mujahid MS, Hirsch JA, Moore K, & Moore LV (2016). The impact of neighborhoods on CV risk. Global heart, 11(3), 353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Mentz G, Lachance L, Johnson J, Gaines C, & Israel BA (2012). Associations between socioeconomic status and allostatic load: effects of neighborhood poverty and tests of mediating pathways. Am J Public Health, 102(9), 1706–1714. doi: 10.2105/AJPH.2011.300412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Macinko J, Starfield B, Politzer R, Wulu J, & Xu J (2005). Primary care, social inequalities and all-cause, heart disease and cancer mortality in US counties: a comparison between urban and non-urban areas. Public Health, 119(8), 699–710. doi: 10.1016/j.puhe.2004.12.007 [DOI] [PubMed] [Google Scholar]
- Singer M (2009). Introduction to syndemics: A critical systems approach to public and community health: John Wiley & Sons. [Google Scholar]
- Singh GK, & Siahpush M (2014a). Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. J Urban Health, 91(2), 272–292. doi: 10.1007/s11524-013-9847-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, & Siahpush M (2014b). Widening rural-urban disparities in life expectancy, US, 19692009. American journal of preventive medicine, 46(2), e19–29. [DOI] [PubMed] [Google Scholar]
- Singh GK, Williams SD, Siahpush M, & Mulhollen A (2011). Socioeconomic, rural-urban, and racial inequalities in US cancer mortality: Part I—All cancers and lung cancer and Part II—Colorectal, prostate, breast, and cervical cancers. Journal of cancer epidemiology, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Dickerson JB, Wendel ML, Ahn S, Pulczinski JC, Drake KN, & Ory MG (2013). The utility of rural and underserved designations in geospatial assessments of distance traveled to healthcare services: implications for public health research and practice. Journal of environmental and public health, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solar O, & Irwin A (2010). A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice) Retrieved from
- Starfield B (2007). Pathways of influence on equity in health. Social Science & Medicine, 64(7), 1355–1362. [DOI] [PubMed] [Google Scholar]
- Stein EM, Gennuso KP, Ugboaja DC, & Remington PL (2017). The Epidemic of Despair Among White Americans: Trends in the Leading Causes of Premature Death, 1999–2015. American journal of public health, 107(10), 1541–1547. doi: 10.2105/AJPH.2017.303941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trujillo MD, & Plough A (2016). Building a culture of health: A new framework and measures for health and health care in America. Social Science & Medicine, 165, 206–213. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Mendenhall E, Trostle JA, & Kawachi I (2017). Co-occurring epidemics, syndemics, and population health. The Lancet, 389(10072), 978–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau 2011–2015 American Community Survey 5-Year Estimates. (2015).
- United States Department of Agriculture, E. R. S. (2019). Rural Poverty and Well-Being. Retrieved from https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/#geography
- Vaccarino V, & Bremner JD (2013). Traumatic stress is heartbreaking. Biol Psychiatry, 74(11), 790–792. doi: 10.1016/j.biopsych.2013.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield M, Beale C, Coburn A, Detmer D, Grigsby J, Hartley D, … Rosenblatt R (2004). Quality Through Collaboration: The Future of Rural Health. In: The National Academies Press; Washington, DC. [Google Scholar]
- Whitfield GP (2019). Trends in Meeting Physical Activity Guidelines Among Urban and Rural Dwelling Adults—United States, 2008–2017. MMWR. Morbidity and mortality weekly report, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willen SS, Knipper M, Abadía-Barrero CE, & Davidovitch N (2017). Syndemic vulnerability and the right to health. The Lancet, 389(10072), 964–977. [DOI] [PubMed] [Google Scholar]
- Yitzhaki S (1979). Relative deprivation and the Gini coefficient. The quarterly journal of economics, 321–324. [Google Scholar]
- Yousefian A, Hennessy E, Umstattd MR, Economos CD, Hallam JS, Hyatt RR, & Hartley D (2010). Development of the Rural Active Living Assessment Tools: measuring rural environments. Prev Med, 50 Suppl 1, S86–92. doi: 10.1016/j.ypmed.2009.08.018 [DOI] [PubMed] [Google Scholar]
Appendix Bibliography
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1890–1938). Vital Statistics of the United States: 1890–1938. Retrieved from https://www.cdc.gov/nchs/products/vsus/vsus_1890_1938.htm
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1939–1964). Vital Statistics of the United States: 1939–1964. Retrieved from https://www.cdc.gov/nchs/products/vsus/vsus_1939_1964.htm
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1902). Twelfth Census of the United States, Taken in the Year 1900. Volume III. Part I. Analysis and Ratio Tables Retrieved from https://www.cdc.gov/nchs/data/vsushistorical/vsush_1900_3.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1923). Mortality Rates 1910–1920. With Population of the Federal Censuses of 1910 and 1920 and Intercensal Estimates of the Population Retrieved from https://www.cdc.gov/nchs/data/vsushistorical/mortrates_1910-1920.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1927). Mortality Statistics 1925. Twenty-Sixth Annual Report. Part I. Summary and Rate Tables and General Tables for the Death Registration Area in Continental United States, with Supplemental Statistics for Hawaii and the Virgin Islands Retrieved from https://www.cdc.gov/nchs/data/vsushistorical/mortstatsh_1925.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1932). Mortality Statistics 1929. Thirtieth Annual Report, p.62.
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1947). Vital Statistics Rates in the United States, 1900–1940. Retrieved from https://www.cdc.gov/nchs/data/vsus/vsrates1900_40.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1954). Vital Statistics Rates in the United States 1950, Volume I, Analysis and Summary Tables with Supplemental Tables for Alaska, Hawaii, Puerto Rico, and Virgin Islands. Retrieved from https://www.cdc.gov/nchs/data/vsus/vsus_1950_1.pdf
- National Center for Health Statistics (US). National Vital Statistics Division, U. S., & United States Bureau of the Census, Vital Statistics Division. (1963). Vital Statistics of the United States, 1960. Volume II, Mortality, Part A Retrieved from https://www.cdc.gov/nchs/data/vsus/VSUS_1960_2A.pdf


