Abstract
Vaccination to prevent human papillomavirus (HPV) infections and associated cancers has been recommended for use in the US since 2006; however, vaccine uptake remains suboptimal. Many sociodemographic factors have been evaluated with regard to HPV vaccine uptake but there has been less focus on the role of religion and religiosity.
Our qualitative case study aimed to identify community perceptions of HPV and HPV vaccination via seven focus group discussions (FGDs) with leaders and members of an African Methodist Episcopal (AME) church in metro-Atlanta, Georgia from April 2018 to July 2018. A Social and Behavior Change Communication (SBCC) conceptual framework was used to identify potential avenues to strengthen communication and health promotion strategies in the church community.
Results showed diverse perceptions about HPV vaccine amongst the church community, ranging from viewing the HPV vaccine as essential to unnecessary for adolescents. Two key barriers to the HPV vaccine that may be addressed through the SBCC strategies were identified: 1) general mistrust in the healthcare system and 2) the expectation of abstinence among adolescents. For future HPV prevention opportunities, congregants highlighted they would be more receptive to receiving HPV vaccine promotion messages from pre-established trustworthy sources.
Church leaders hold the trust of their congregation, therefore implementation of a church-based intervention utilizing the SBCC strategies has considerable potential to transform perceptions of the HPV vaccine and increase vaccination uptake. These findings may be implemented in future HPV vaccine promotion strategies within faith-based communities to promote safe and open dialogue for health communication messages to be disseminated in a familiar and trusted setting.
Keywords: Human Papillomavirus, HPV vaccination, religion, church-based intervention, adolescent health, cancer prevention, qualitative research, focus group discussions
Introduction
A vaccine to prevent human papillomavirus (HPV) infections and associated cancers has been recommended for adolescent females in the United States since 2006 (Centers for Disease Control and Prevention [CDC], 2017). In 2011, the vaccine recommendation was extended to include males (CDC, 2017). Despite persistent HPV vaccine promotion, uptake has consistently remained suboptimal (CDC, 2019b). The CDC reports that nearly 1 in 5, or 80 million Americans, are currently affected by HPV (CDC, 2016). Multiple types of HPV exist and persistent infection of high-risk classified types may lead to anogenital cancers over time (American Cancer Society, 2017; Gravitt & Winer, 2017). HPV-associated cancers include cervical, vaginal, vulvar, penile, anal and oropharyngeal (CDC, 2019a). There are 44,000 of these specific cancer cases reported annually and nearly 34,800 (79%) are caused by HPV (CDC, 2019a). Of the reported HPV-associated cancer cases, African Americans are disproportionately affected (American Cancer Society, 2016; CDC, 2019a). African American women are diagnosed with cervical cancer 30% more frequently and are twice as likely to have a death related to their cervical cancer diagnosis compared to Caucasian women (Fu, Zimet, Latkin, & Joseph, 2017). In 2018, only 47% of African-American adolescents living in Georgia were up-to-date on HPV vaccination series (CDC, 2019b). The high HPV-associated cancer statistics among African Americans are concerning, highlighting the need to increase HPV vaccination coverage among this population (American Cancer Society, 2016; CDC, 2019a; Strohl et al., 2015).
Sixty-seven percent of Americans identify as religious and religion is evidently a sociocultural factor in the United States (Newport, 2017; Shelton, Snavely, De Jesus, Othus, & Allen, 2013). The sociocultural role of religion influences health decisions, such as uptake of the HPV vaccine, making religion a social determinant of health (Shelton et al., 2013). A study utilized a survey to examine the influence of religion on the HPV vaccine decision-making process among White, Black, and Hispanic parents (Shelton et al., 2013; Yaqub, 2014). Variables such as religious denomination and frequency of attendance at religious service were included to assess the association between religiosity and vaccine-related beliefs and decisions (Shelton et al., 2013). Results show that parents who frequently attend church were more likely to have decided not to vaccinate their daughter rather than remain undecided (OR = 3.05, 95% CI = 1.41, 6.58) (Shelton et al., 2013). Two additional studies found comparable results of parents with higher rates of church attendance having greater vaccine hesitancy with less intent on having their adolescent child vaccinated against HPV (Barnack, Reddy, & Swain, 2010; Constantine & Jerman, 2007). Another qualitative study has shown that participants of other Christian religious denominations – such as Church of Jesus Christ of Latter-day Saints, Methodists, Seventh-Day Adventists – have credited religion to be the strongest influence on sexual health and inseparable from their culture (DiStefano, 2012). And Catholics have credited religion to having significant impact on attitudes and behaviors and highly influential in health decision making (DiStefano, 2012).
A number of sociodemographic factors have been evaluated in regard to HPV vaccine uptake (Holman et al., 2014; Hull et al., 2014). However, there has not been significant focus on the role of religion (i.e., institution of particular set of beliefs, doctrines and worship with postulated supreme beings) and religiosity (i.e., the extent to which one is religious) in relation to church-based interventions (Anonymous, 2010; Banton, 1966; Mattis, 2000; Taylor, 1998). Religiosity is high for African American populations, with 47% of adults reporting that they attend church at least once a week and 75% of adults reporting religion is ‘very important’ in life, the highest among any racial or ethnic group in the U.S. (Pew Research Center, 2014). Research shows that African American women have strong religious beliefs which often they base health decisions on, more specifically vaccine decisions (Galbraith, Palmer, & Hamilton, 2016). In states with high religiosity, like Georgia, exploring the roots of receptivity and hesitancy towards HPV vaccination among faith communities may allow for the cultivation of tailored church-based HPV prevention strategies. Emory University’s Interfaith Health Program demonstrated how a church-based intervention through capacity building and mobilization of church-based networks linked with public health may be effective, through The Influenza Initiative (Kiser & Lovelace, 2019).
Tailored church-based HPV vaccination promotion strategies could be implemented to increase HPV vaccination coverage and alleviate these racial health disparities (Kiser & Lovelace, 2019). The church is a trusted space that cultivates a safe and supportive environment for congregation members (Hull et al., 2014; Kiser & Lovelace, 2019). Little is known about HPV prevention efforts to educate African American faith communities in a church setting. A shared vision among congregational leaders and public health professionals is central to leveraging capacities and resources to collaboratively build an HPV prevention church-based intervention (Kiser & Lovelace, 2019). Understanding contextual reactions to current HPV prevention strategies may lead to better HPV vaccination promotion among faith communities, ultimately leading to higher HPV vaccination coverage. Collaboration with faith based communities maximizes social capital and ensures the avenue of health promotion in a familiar and trusted setting is utilized (National Academies of Sciences & Medicine, 2019). The influential role faith communities have on community health make them valuable partners for health promotion (National Academies of Sciences & Medicine, 2019). Successfully reaching African American faith communities may increase HPV vaccine coverage and change the landscape of HPV infections. Our study attempts to fill the above mentioned gaps in the literature by conducting a qualitative case study to develop a better of understanding of HPV and HPV vaccination perceptions within an African Methodist Episcopal (AME) church to provide context for future HPV prevention efforts.
Methodology
Our study is part of a larger project to identify the influences on uptake of HPV vaccine through 23 focus group discussions (FGDs) across the state of Georgia. We used a sub-set of data from the parent study to develop a qualitative case study of a large AME church in metro-Atlanta, Georgia (Anonymous, 2011). We chose an AME church to better understand faith-based beliefs and practices about HPV and the vaccine in a predominantly African American church community. This focus is warranted due to the disproportionate rates of HPV-related cancers in the African American community (American Cancer Society, 2016). The AME church we chose for this case study has a large and diverse congregation, with 4,000 members from a large number of counties and 1,200 whom regularly attend Sunday service. The diverse composition of the congregation enables us to capture a range of perceptions on HPV. In addition, we identified a trusted gatekeeper with connections to this church, who could serve as a valuable resource to recruit participants.
Ethical Considerations
The study was approved by the Institutional Review Board (IRB) of Emory University. Participants were provided informed consent or assent forms to review upon arrival to the FGD, which included permission to record the focus group discussions. Written informed consent was required from all adult participants. Participants under 18 years of age were required to sign informed assent forms and have a guardian sign an informed consent form. Assent involved our gatekeeper explaining the study to parents and adolescents and asking if the adolescent would be interested in participating. The gatekeeper explained that the guardian would be required to accompany the adolescent to the FGD, sign an informed consent form for the adolescent to participate and wait for them outside to finish participation in the FGD. Upon arrival to the FGD, the facilitator explained to adolescent participants the purpose of the study and what their involvement would mean. All participants were given a pseudonym to use during the group discussion to provide anonymity in the digital recordings and written notes. To show appreciation, participants received a $30 gift card. This incentive was approved by the IRB as adequate for the participants’ time without being coercive.
Data Collection
Data were collected from April to July 2018. FGDs were the most suitable method of data collection for the goal of this study – to examine the perceptions of HPV vaccination amongst this AME church community (Anonymous, 2020). The group format allowed us to capture a range of views on the study topic, discuss the context of divergent views and identify areas of shared attitudes and practices related to HPV and HPV vaccination. Although HPV may be considered a sensitive topic to discuss in a group setting, our questioning focused on community level perceptions and behaviors so that participants were not compelled to share personal information unless they chose to do so.
We conducted seven FGDs, with six to nine participants in each, with a total of forty-nine study participants. Groups were stratified to capture a diversity of views on the study topics from: a) Church leaders (e.g., pastor, associate pastor, retired pastor), b) the church health ministry, who are medical providers (e.g., physician, nurse, nurse practitioner), c) parents of at least one adolescent child aged between 9–17 years, d) young adults aged between 18–26 years and e) adolescents aged between 9–17 years. Stratification of groups was designed to minimize power dynamics across group participants for open discourse, for example, not having a church leader and church member in the same group. Eligible participants were required to have English literacy (ability to read, write, speak and understand) and the ability to provide informed consent or assent. Our sample of seven FGDs was stratified for diversity and focused on community level perceptions of issues, which enabled us to reach data saturation - whereby no more new issues were identified across the focus groups. Prior experiments on saturation have found that four FGDs are adequate to achieve code saturation (to identify issues) in a homogenous study population, and three to six FGDs to achieve meaning saturation (to understand issues) (Anonymous, 2019). With our diverse sample we planned to conduct FGDs until thematic saturation was reached, estimating that we could need as many as seven focus groups to capture the full range of views on the study topic.
Participants were recruited by a gatekeeper, who was a familiar, trusted member of the AME church. The gatekeeper distributed fliers about the study amongst the congregation and in a monthly church newsletter and described the study through interpersonal communication with eligible members. Participants were recruited during weekly services and assigned to specific group discussions per the eligibility of the groups. Group discussions were conducted in a private room at a church affiliated building and scheduled at times most suitable for the participants and research team.
All FGDs were led by a trained moderator and note taker team. A semi-structured discussion guide was used and reviewed for quality and clarity by the Intervention Development, Dissemination, and Implementation Shared Resource (IDDI) at Emory University. Each FGD began with an introduction of the study and allowed time for participants to ask clarifying questions. The discussion guide contained open-ended questions designed to elucidate information on six topics related to attitudes and practices on HPV and HPV vaccination within this AME church community. These topics included (1) Attitudes on general health, (2) Attitudes on vaccinations/immunizations, (3) Knowledge about HPV and the vaccine, (4) Barriers and motivators for the HPV vaccine, (5) Sources of information on HPV and (6) Development of educational information on HPV. These six topics were chosen for the study to critically examine the complex array of factors that may impact preventive care utilization. Group activities were conducted during the FGDs to elicit a further understanding of participant’s perceptions of HPV and the vaccine. One activity conducted with parents/guardians involved ranking motivators and barriers to the HPV vaccine amongst their church community. Another activity conducted with the church leaders involved identifying the degree of agreement with a series of pre-prepared statements related to perceptions of the HPV vaccine, healthcare providers and health-related religious beliefs within the AME church community. The discussion amongst participants during these activities were recorded and analyzed. In addition, the outcome of the activities themselves (e.g., ranking of barriers) were analyzed to identify any patterns and variability between types of participants. These results are presented throughout the results section.
Data Analysis
Audio recordings of the FGDs were transcribed verbatim and de-identified to remove any identifying information. Transcripts were checked for accuracy and completeness via a three-step review process. First, one team member transcribed the recording verbatim. A second team member reviewed it for accuracy and proposed edits. Finally, a third team member reviewed the transcript and edits and accepted or declined the edits. This process ensured that all transcripts received a double-review to maximize accuracy and ensure data quality. Audio recordings were deleted after transcription was completed to ensure data confidentiality. All transcripts were stored on a password protected, HIPAA compliant server with secured access for only the research team.
All transcripts were uploaded into MAXQDA 2018 (VERBI GmbH, Berlin, Germany) software program for analysis. We used MAXQDA 2018 software as it allows for systematic analysis of textual data and enables data to be easily retrieved for comparison across FGDs. We conducted a thematic analysis involving the following steps. 1. Code development. Two members of the research team (AL & AK) closely read all transcripts to familiarize themselves with the data. They then reviewed three transcripts intensely to identify key issues, ideas and topics, which became initial codes. All codes were listed in a codebook which included the code name, definition and any related sub-codes. Each code included instructions on how to recognize data to be captured with the code, including inclusion and exclusion criteria and examples of text. 2. Coder Consistency. Two researchers (AL & AK) both used the codebook to code three transcripts to assess consistency in interpretation of data and application of codes. Minor inconsistencies were discussed and rectified through adjustments to the codebook and code application. 3. Data Coding. The codebook was then used to code all transcripts. Data were coded to organize the issues, ideas and topics within the data, so that each issue could be retrieved for detailed analysis. The codebook development and coding process was complete once no new ideas or topics arose from the data. If new issues arose during coding, they were added to the codebook or code definitions adjusted to accommodate the new ideas. 4. Description of issues. We searched data by each code and developed comprehensive descriptions of each issue, including any diversity or nuance of the issues. 5. Structured comparisons. We then conducted structured comparisons of issues by the type of participants (e.g., church leader, health ministry member, parents and adolescents) to identify any patterns in issues by participants. Specifically, we focused on whether perceptions of HPV and the HPV vaccination differed between participant types and what strategies or sources of information each type of church member would be most receptive to. 6. Categorizing perceptions. In our descriptive analysis we identified a wide range of perceptions around the acceptance of the HPV vaccine. We defined each perception by distinguishing its characteristics and retrieved coded data to support each perception. We categorized the perceptions and placed them on a continuum to highlight the array of views and identified example quotations to illustrate each perception. 7. Data Validation. Consistency checks were used to validate results by continually referring back to the transcripts and the codebook to ensure that critical concepts developed in the analysis and represented in the conceptual framework accurately reflected participant’s issues. One researcher (AL) conducted consistency checks throughout data analysis. 8. Development of Conceptual Framework. During early analysis we identified a range of influences on HPV vaccine perceptions from the different types of AME church members interviewed - church leadership, health ministry, parents and adolescents. Once we understood these distinct influences, we used a conceptual framework to identify opportunities for social and behavior change communication (SBCC) in this church community. SBCC is the interactive application of communication that is used to promote positive health behaviors and outcomes (Adewuyi & Adefemi, 2016; Briscoe & Aboud, 2012; Kreps & Maibach, 2008). The SBCC framework has proven to have significant effect on targeted individuals and communities to influence positive health behaviors, such as preventative behaviors (Briscoe & Aboud, 2012; Kreps & Maibach, 2008; The Johns Hopkins Center for Communication Programs). After we conducted analyses and understood the relationship between the different elements of the church community and perceptions of HPV vaccine, we used the SBCC framework to inform health communication methods that participants identified they would be receptive to receiving from their church community. SBCC is systematic, targeted, and participatory and may effectively shape future HPV prevention messages in this AME church community (Briscoe & Aboud, 2012; The Johns Hopkins Center for Communication Programs).
Results
Seven FGDs were conducted with a total of forty-nine participants (N=49). Participants ranged in age and sex with thirty-four adult female participants, three adult male participants, three young adult female participants, six adolescent female participants and two adolescent male participants. Twenty-nine codes were identified in the codebook. We determined that thematic saturation was reached by six FGDs, as no new issues, ideas, or topics arose after this point. Results are presented on the following topics (1) Barriers to the HPV vaccine, (2) HPV Vaccination Perceptions, and (3) Opportunities for future HPV prevention strategies.
1. Barriers to the HPV Vaccine
Participants discussed a multitude of barriers to vaccine uptake across all FGDs. However, two barriers stand apart from others because they are based in communal perceptions and may be addressed through SBCC strategies. These two barriers that were repeatedly mentioned in the data are (a) mistrust in the healthcare system and (b) the expectation of abstinence among adolescents.
(a). Mistrust in the healthcare system.
A common theme across many FGDs was the general mistrust in the healthcare system. A church leader shared, “in the African American community in general there is a suspicion of doctors and vaccinations” (FG6). A parent shared personal suspicions of vaccinations in particular by stating, “I have a five-year-old, and I have not given him all the vaccinations…I’m against vaccinations. Because I think it’s just like a test, you’re a guinea pig…So basically what I’ve done with him is I’ve given him just the vaccinations that will get him into schools” (FG4).
Among participants it was common that mistrust in the healthcare system was generally attributed to past unethical medical studies, like the Tuskegee Syphilis Study, conducted on African Americans without their full knowledge and consent. A parent shared, “they used them [African Americans] as test cases, pretend to treat them, and not really treat them and see how bad it can actually get and things of that nature…So yes, that made me very wary, especially when something first comes out” (FG2). Participants also referenced the North Carolina Eugenics Board unethical medical treatment of forced sterilization for selective breeding program. A participant shared, “They [the healthcare system] have given us, like thousands of us [African Americans], um things to sterilize us and say ‘oh, this is a vaccine’…these women, they couldn’t reproduce. And it’s not something they signed up for…we were the guinea pigs…” (FG6). Another participant emphasized how these historical events have contributed to communal mistrust of the healthcare system. She shared, “I know people in my circle, and we don’t want to go to the doctor. We don’t want any kind of medication, no prescription. What are you giving me? No vaccinations, no my child will not be getting no more vaccinations” (FG6).
Participant mistrust in the healthcare system was also commonly spurred by the idea that ‘healthcare just wants a profit’. A participant stated, “And right now there is a suspicion of uh ‘Do I really need this? Or…is this some other type of ploy, maybe this is just a money-making thing?” (FG6). This mistrust of the healthcare system in general also influences participants views about HPV vaccine promotion strategies; specifically, the Merck & CO., Inc. Gardasil® commercial titled “It’s Personal: What Will You Say?”. A participant summarized a communal feeling of the commercial being a potential conflict of interest, by stating, “I don’t want to see it [advertisement] from the company that’s making money off of it” (FG1). One recommendation was for a neutral party to present unbiased research on the HPV vaccine to demonstrate, “the facts, this is the research, we have this much data, and this is what it shows” (FG2).
Participants debated how HPV prevention strategies through the medium of a commercial are ineffective at alleviating preconceived mistrust in the healthcare system. A participant shared, “Because it’s in the media it doesn’t do anything for my suspicions…because I have the same suspicions about the media! That hasn’t made it a more personal way in order to get me this information or to talk to me about it” (FG6). Participants all agreed that the commercial employs scare and guilt tactics but held different opinions on its effectiveness. Some participants did recognize the benefit of the commercial and believed it “is a good way to make people aware and prompt them to take the child in to at least inquire about it [HPV vaccine]” (FG4). Most participants felt the “commercials are scaring people more than anything” (FG5) and agreed that “scare tactics don’t work” (FG6). A participant shared, “It’s scary, the way they [pharmaceutical companies] advertise it. It gets you alarmed, gets your attention. And so you really need more information!” (FG6). A parent added, “It seems to put it back on us like, mom did you know? Well no, I didn’t know!” (FG5). This parent emphasized that more information is needed “so mom could know, dad could know…Because we get blamed for everything” (FG5).
(b). Expectation of abstinence among adolescents.
Participants often discussed the social expectation of abstinence until marriage, which stems from their religious teachings. It was expressed that this communal expectation has prevented discussion of adolescent sexual health topics in the church setting, including HPV or the HPV vaccine. A young adult health ministry member shared, “in the Christian community, it is real taboo to talk about HIV, sex, and everything like that. And it can be a hard topic to talk about with your parents” (FG5).
Misinformation about HPV and the vaccine were present in the FGDs that may not have otherwise been if the avenue of providing adolescent sexual health communication messages in a familiar and trusting setting had been utilized. For example, when asked who is at risk to contract an HPV infection and should receive the vaccine series, a participant believed only “sexually active kids” (FG2). However, the HPV vaccine is recommended for 11–12-year old’s, regardless of sexual activity. With this piece of misinformation and the communal expectation of abstinence in this community, many parents held conflicting attitudes towards the HPV vaccine. Due to this expectation, some parents placed the decision making on their adolescent. A parent shared, “I explained to them [participant’s children], ‘if you choose to live that type of life, if you choose at 18…that you’re going to be promiscuous…then go ahead and get it [the HPV vaccine]! It’s on you now’ But I wouldn’t consent to it” (FG6).
2. HPV Vaccination Perceptions
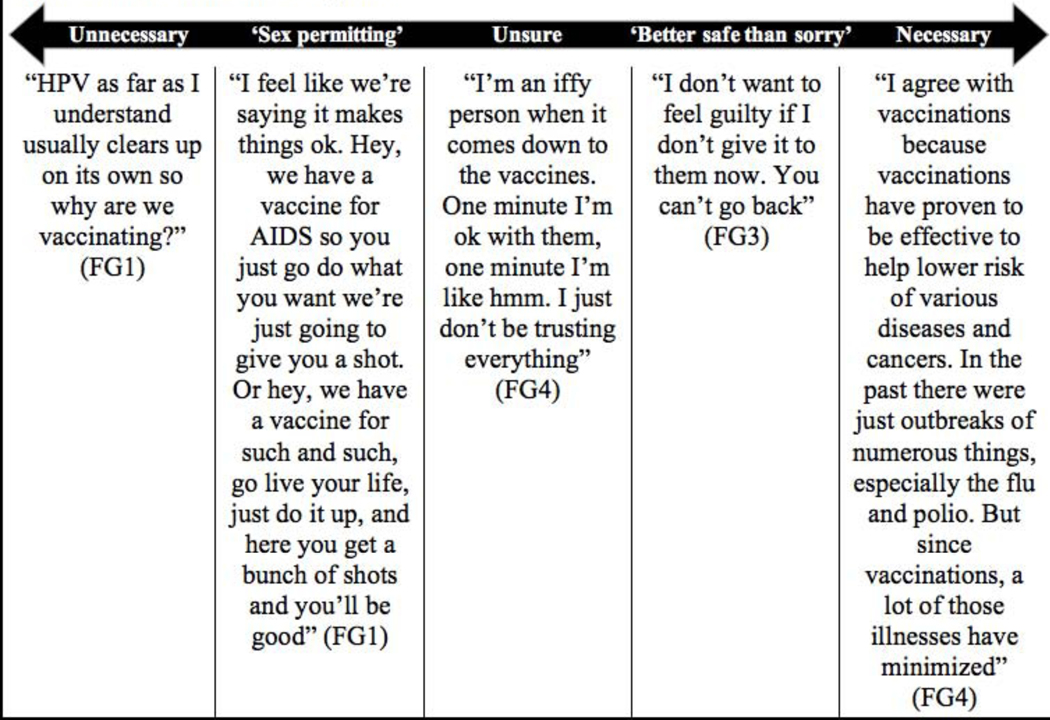
A wide range of perceptions on the HPV vaccine were identified across all FGDs and summarized in figure 1.
Figure 1.
HPV Vaccine Perceptions
At one end of the spectrum, participants viewed the HPV vaccine as completely unnecessary. A participant stated, “Why put your child through anything that unnecessary?” to which another participant added, “Yeah, if you’re not sure it’s gonna work” (FG3). While some participants believed all vaccines are unnecessary, some only believed that unrequired recommended vaccinations (e.g., HPV and influenza) are unnecessary. Participant’s views ranged from, “I’m highly against vaccinations” (FG4) to “my son is up-to-date on all his vaccines, but he doesn’t do the flu vaccine or even the HPV vaccine” (FG1).
Some participants held the perception that the HPV vaccine acts as a ‘sex permitting’ signal to their adolescent child, believing that it “gives them permission” (FG2) to have sex. Participants were often conflicted when it came time to make a decision regarding the HPV vaccine for their child because of the perceived interference with their expectations of abstinence until marriage. For example, a participant shared, “I didn’t tell him what it was for, I just told him it was a regular vaccine that he had to take because he turned 11” (FG2) in fear of the sex permitting signal the vaccine may send to the child. Although this participant ultimately agreed to vaccinate, some parents may choose to not vaccinate their child in fear of communal stigmatization due to the perceived interference with abstinence until marriage.
In the center of the spectrum, participants were still uncertain about the HPV vaccine, even after having their child vaccinated. A participant stated, “so, my daughter was vaccinated but I don’t know how I feel about that…I’m conflicted. Vaccines, I don’t know, I really feel like they’re just testing our bodies” (FG1). Many participants discussed that they have remained unsure because they do not have “enough knowledge to make a decision” (FG3), emphasizing the need for additional HPV information and education.
Other participants were more receptive to the HPV vaccine and shared a ‘better safe than sorry’ attitude due to perceived motivators for vaccination outweighing the perceived barriers. When ranking personal motivators for HPV vaccination, parents indicated that the strongest motivator was to provide their child protection from developing an HPV-associated cancer (FG1/FG2/FG3/FG4). A parent shared, “I was scared giving the vaccinations but I was more scared not to” (FG3). Another parent commented, “I just finally gave in with [daughter’s name] because I was wanting to rather be safe than sorry for her” (FG1).
At the other end of the spectrum participants felt that the HPV vaccine was a necessary preventive health method. A parent adamantly stated, “You just need it, part of turning 12” (FG2). Participants on this end of the spectrum expressed confidence in the HPV vaccine. Another parent stated, “I trusted the vaccine just as much as I trusted the chicken pox vaccine” (FG2). One participant held deep regrets of not having her daughter vaccinated after her daughter faced the scare of an abnormal Pap smear result. She shared, “I should have said yes. Because she faced something that she did not have to face if I had not been so close-minded” (FG6).
3. Opportunities for future HPV prevention strategies
Participants across FGDs shared a desire to break down the taboo of discussing sexual health in the church and the communal mistrust held towards the healthcare system. Health Ministry members recognized the importance of mobilizing efforts to improve adolescent sexual health education in the church, noting these topics are “not [discussed] as much as we should” (FG5). Church leaders also shared their willingness to facilitate the intersection of faith and health, stating “from a…pastoral standpoint…one of the things that we have to be able to do is we have to be open, transparent…and willing to even…talk about these things… especially if we have that platform” (FG6). Another leader added in agreement, “We have to be open to the intersection of medicine and faith” (FG6).
The value of transparency from trusted sources was an emergent theme among participant’s recommendations for future HPV prevention efforts. Adolescent participants discussed their appreciation of transparent sexual health education by stating, “she’s [Health Educator] very real…She didn’t like dance around [the topic]” (FG7). Adolescent participants discussed their receptivity to prevention education rather than abstinence-only education by stating, “That’s like the worst thing when people are like ‘Don’t have sex! What’s the best way to prevent STD’s? DON’T HAVE SEX!’” (FG7). Additionally, parents shared how they value transparency from their child’s pediatrician. A participant shared, “there is a very open, honest, candid dialogue that takes place and for me that makes me respect her more because she is not trying to, you know, sugar coat anything” (FG6). The thread of transparency continued to be discussed among recommended strategies to effectively provide HPV education. Participants shared “I need stats. I want real studies. I even want to see the demographics of the studies” (FG3). Another participant added the need for “true testimonials” (FG2). Across all FGDs participants stated they would be most receptive to hearing testimonies and seeing statistics from populations who share characteristics of their social network (e.g., race/ethnicity, religion).
Church leaders were receptive to moving forward from suspicions of the healthcare system and stigma against the HPV vaccine to advocate for preventive health within the church community. A church leader shared, “I’m trying to move from the suspicion to being open, I’m doing it because I don’t want my children to grow up having that same suspicion of doctors” (FG6). Another leader further iterates, “You know, everybody goes back to the Tuskegee experiment, there are things that have happened but I believe there are suspicions that I hold onto um really blindly and that is one of them as it relates to vaccinations” (FG6). In hope for future generations to transition away from suspicions of the healthcare system, many church leaders believed adolescents (ages 9–17 years) should receive information about vaccine preventable diseases to help make informed decisions (FG6).
Participants highlighted the positive influence of pre-established trust in church-based interventions by stating, “Even though you have a doctor it depends on the relationship you have with that doctor as opposed to someone that you know at church that you can relate to, the trust value” (FG5). Health ministry members discussed how church members will often ask them questions like, “do you have more information about this new shot, it was on the news, CDC said this…what do you think?” (FG5). Further adding, “they feel comfortable that they can come and ask a familiar face. When they know you’re in the health ministry they tend to come to you all the time…” (FG5). There was the common phenomenon present in the FGDs that “it plays a part in how receptive you are to the education if it’s coming from someone that you’re familiar with” (FG5).
Discussion
The results of this study inform how this AME church, and potentially other religious bodies, can be an agent of change to promote preventive health and increase the uptake of HPV vaccination. The SBCC framework aimed to provide guidance to stimulate preventive actions while simultaneously shifting communal perceptions to foster a supportive community for long-term behavior change (Adewuyi & Adefemi, 2016; Briscoe & Aboud, 2012). Actionable recommendations are provided to demonstrate how the AME church can utilize SBCC strategies to improve HPV prevention efforts. Our findings highlight how each type of participant can work to synergistically produce behavior change. For HPV vaccine promotion in this AME church community, the SBCC strategies identified are faith-based mobilization, community mobilization, community engagement, social change communication and behavior change communication. The strategic use of the SBCC framework may stimulate community dialogue to raise HPV awareness, promote HPV knowledge, increase sexual health education, reduce HPV vaccine-related stigma, and promote HPV prevention services (i.e., vaccination) (Briscoe & Aboud, 2012; The Johns Hopkins Center for Communication Programs).
Faith-based Mobilization
A church-based HPV prevention intervention has not yet been attempted at this AME church. However, church leaders of this AME church collectively advocated for a greater integration of faith and health, providing a potential opportunity for the church to be an agent of change to increase HPV coverage within their community. Recognition of the need for faith-based mobilization to promote the HPV vaccine in their community is the first step for a church-based intervention to be well-received. It is important to note that the church leaders advocating for faith-based mobilization and supporting the health ministry is imperative for this intervention process. However, we recognize that church leader’s acceptability and desires for an integration of faith and health does not always translate into implementation (Williams, Fisher, Bayliss, Morris, & O’Leary, 2020). Past research suggests that there may be competing priorities and church leaders have often waited to address vaccines once an outbreak as occurred (Williams et al., 2020). To make HPV vaccination a priority, it is important to inform these church leaders of the low vaccine coverage rates in Georgia and how HPV-related cancers disproportionately affect African Americans (American Cancer Society, 2016). Further, it is important to emphasize the pre-established trust between church leaders and congregation members may allow for church-based interventions to be effective in promoting preventive health behaviors, such as the HPV vaccine (Hull et al., 2014; National Academies of Sciences & Medicine, 2019).
Community Mobilization
Focus group participants from the health ministry not only advocated for faith-based mobilization but were motivated to mobilize in support of HPV prevention efforts in the AME church. Community mobilization is action-oriented and focuses on the health ministry mobilizing to create a positive sexual health environment within the congregation (UNICEF, n.d.). This would entail the health ministry changing the social, cultural, and institutional norm of it being taboo to discuss sexual health in the church to establishing an environment where adolescent sexual health topics are openly discussed, including sensitization on HPV prevention and vaccination.
The health ministry mobilizing the community to foster an environment of community engagement may allow parents to receive transparent information in a familiar setting from trusted individuals. Which more importantly, may allow them to more thoroughly consider the HPV vaccine series. A majority of the participants in the FGDs had seen the Merck & CO., Inc. Gardasil® commercial yet had very low knowledge and understanding of both the HPV virus and HPV vaccine. Several participants shared information related to the HPV virus and vaccination that was not factually correct, yet they believed it to be so. This indicates that the commercial has been ineffective in providing clear HPV education. The pre-established trust between the health ministry and congregation members, provides a way around the mistrust of the healthcare system, and may result in educational reinforcements and an increase in uptake of the HPV vaccine within the church community.
Community Engagement
Community engagement is participatory and is meant to eliminate disadvantageous social norms and behaviors on a large scale by empowering communities, such as this AME congregation, to become agents of change in shifting communal perceptions (UNICEF, n.d.). An important theme that emerged in the data was mistrust in the healthcare system. Other studies have also noted mistrust in the government and pharmaceutical companies as underlying barriers to vaccines (Freimuth, Jamison, An, Hancock, & Quinn, 2017; Jamison, Quinn, & Freimuth, 2019). However, in our study, participants shared they value the pre-established trust developed within their social network at the AME church to the extent that it enhances their receptiveness to information. Therefore, it is likely that congregation members will be receptive to the SBCC community engagement strategy. Not only may community engagement positively affect receptiveness to information, but HPV education will be disseminated to all the AME congregation members potentially allowing for a paradigm shift in communal perceptions.
This strategy requires the church and the health ministry to facilitate and encourage discussions to motivate new communal perceptions and behaviors (UNICEF, n.d.). Community engagement strategies may be carried out in various ways including health fairs, health forums and vaccination campaigns to name a few (UNICEF, n.d.). A potential effective way to achieve social change communication is for pre-established trusted community leaders, such as the health ministry, to create tailored health communication messages that are socially and culturally appropriate. For example, the IHP at Emory University created The Influenza Initiative, which demonstrates how capacity building and mobilization of faith-based organizations (FBOs) has improved community outreach and uptake of 171,747 influenza vaccinations administered over a seven year period (Kiser & Lovelace, 2019). The Influenza Initiative could be used as a guide to engage with religious communities to coordinate HPV vaccination initiatives. The AME health ministry discussing how HPV-associated cancers disproportionally affect African Americans with the church community will demonstrate the AME church network’s health values and therefore reconstruct communal perceptions. An intervention that involves educating the church community through health promotion and community engagement could help reduce HPV associated stigma within this community. The HPV health topic discussion not only creates a space for this conversation to happen but may stimulate reoccurring discussions.
Social Change Communication
Human nature encourages people to seek normative guidance based on what is accepted in their social network and conform to and reinforce these attitudes and behaviors. When church leaders advocate to shift previously defined communal perceptions that act as barriers to the HPV vaccine and the health ministry mobilizes to instill new normative guidance within the church, we may see a shift in communal perceptions (Haines, Perkins, Rice, & Barker, 2005; National Academies of Sciences & Medicine, 2019; Puffer, 2016). A shift in normative guidance utilizing the SBCC strategies requires shifting the paradigm of communal perceptions, or what individuals in the community believe to be acceptable. Since the two main barriers mentioned in the results are communally perceived, social change communication may allow for reconstruction of these perceptions.
For HPV vaccine promotion among parents in this community, it is imperative the health ministry provides consistent evidence that HPV vaccine uptake is not associated with earlier sexual debut or increased promiscuity (Anonymous, 2012; Coles, Patel, Allen, Keeping, & Carroll, 2014; Jena, Goldman, & Seabury, 2015; Mullins, Widdice, Rosenthal, Zimet, & Kahn, 2015; Petrosky, Liu, Hariri, & Markowitz, 2017; Rysavy et al., 2014; Smith, Kaufman, Stumpf, & Levesque, 2015). Previous research conducted with several different communities and demographic populations identifies that receipt of the HPV vaccination has no association with earlier sexual debut or STI prevalence among adolescents (Coles et al., 2014; Jena et al., 2015; Mullins et al., 2015; Petrosky et al., 2017; Rysavy et al., 2014; Smith et al., 2015). It is essential there is emphasis that the HPV vaccine prevents cancer-causing infections and should be administered during the recommended age (11 & 12 years of age) to protect adolescents long before they may be exposed to the virus (CDC, 2018). Church leaders and the health ministry must focus on HPV vaccination as a preventive measure, in the same way that sunscreen protects against harmful UV rays or a seatbelt provides protection in the event of a car accident (Anonymous, 2015). Waiting to vaccinate or waiting to discuss HPV vaccination leaves a number of individuals vulnerable to HPV infection and associated cancers.
Behavior Change Communication
Successful implementation and receptivity of the previous four SBCC strategies in the AME church may result in behavior change (i.e., uptake of the HPV vaccination series for adolescents). HPV vaccination uptake directly affects adolescents; however, their guardians are the decision makers for vaccination uptake and are likely to look to their church community, health ministry and church leaders for behavior guidance. Further, the church-based intervention with sexual health component allows adolescents to receive information to make an informed decision regarding the HPV vaccine when they turn 18 years of age if their guardian did not previously consent to the vaccine. Therefore, we can see that utilization of the SBCC strategies in a church-based setting may provide an opportunity for positive change on congregational health and HPV vaccination rates (Berkman, Glass, Brissette, & Seeman, 2000).
Conclusion
Changing uptake of HPV vaccination requires tailored communication and behavior change strategies to reach communities experiencing suboptimal coverage. Leveraging the pre-established trust within the church with SBCC strategies will likely allow for HPV-focused church-based interventions to be effective for this AME church and possibly other AME communities. Further research is needed to implement an AME church-based HPV prevention intervention utilizing these strategies to first evaluate feasibility, effectiveness and generalizability. Successful implementation of an AME church-based intervention may increase HPV vaccine uptake and reduce HPV infection and associated cancers among AME church members. On a larger scale, if other churches adopted a similar approach with appropriate modifications, there is potential to alter the uptake of HPV vaccine coverage, ultimately reducing the HPV vaccination coverage gap and the disproportionate HPV-associated cancer rates.
Limitations
Although the study findings are from one church in one geographic area, the sample was from a large congregation and included a diverse representation of church members and leaders based on age and sex. This study presented a case study of one religious denomination of one racial group; therefore the results may not be applicable in other religious settings. However, we identified social and behavior change communication strategies within this AME church community, which may be transferable to guide the development and implementation of future health promotion efforts in other religious settings.
Research Highlights.
Tailored behavior change strategies are needed to increase HPV vaccination coverage
Collaboration with faith communities maximizes social capital for vaccine promotion
Church-based interventions may reduce HPV-associated cancer rates
Biography
Author Roles and Responsibilities
Ariana Y Lahijani, MPH is the primary author of this research paper. As such, Ms. Lahijani led the qualitative analysis for this paper. Ms. Lahijani conceptualized the analysis and explanation of results depicted in the research paper. Overall, Ms. Lahijani is assisted with all aspects of the research paper.
Adrian R. King, MPH aided in various aspects of the research paper. Mr. King developed and formalized the focus group discussion guides used for data collection and managed the transcription of all focus group discussion audio recordings. Mr. King defined the methodology to be utilized during data collection, data curation, project administration, and analysis. Mr. King facilitated each of the focus group discussions included in this analysis and collaborated with as she conceptualized the research paper. Mr. King provided edits, revisions, and commentary to Ms. Lahijani through the various versions of the research paper.
Mary M. Gullatte, PhD RN provided advisory support for the research paper and aided in the editing and conceptualizing of the research paper. Dr. Gullatte aided in the development and conceptualization of the results and discussion sections of the research paper and ensured that aspects of the community context and leadership roles were adequately represented within the paper.
Monique Hennink, PhD provided critical review of the qualitative methods and aided in the editing of the research paper. Dr. Hennink aided in the revision of the methods and interpretation of the findings.
Robert A. Bednarczyk, PhD provided supervision for the research project and was responsible for acquiring funding for the research project. Dr. Bednarczyk provided regular edits, revision, and commentary on the research paper and also assisted in the development and conceptualization of the results and discussion sections of the research paper. Dr. Bednarczyk was also involved in the development of methodology to be used during the research project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anonymous. (2010). Details omitted for double-blind review.
- Anonymous. (2011). Details omitted for double-blind review.
- Anonymous. (2012). Details omitted for double-blind review.
- Anonymous. (2015). Details omitted for double-blind review.
- Anonymous. (2019). Details omitted for double-blind review.
- Anonymous. (2020). Details omitted for double-blind review.
- Adewuyi EO, & Adefemi K. (2016). Behavior Change Communication Using Social Media: A Review. The International Journal of Communication and Health, 9. [Google Scholar]
- American Cancer Society. (2016). Cancer Facts and Figures for African-Americans 2016–2018. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2016-2018.pdf
- American Cancer Society. (2017). HPV and Cancer. Retrieved from https://www.cancer.org/cancer/cancer-causes/infectious-agents/hpv/hpv-and-cancer-info.html [Google Scholar]
- Banton M (Ed.) (1966). Anthropological Approaches to the Study of Religion. London, Great Britain: Tavistock Publications. [Google Scholar]
- Barnack JL, Reddy DM, & Swain C. (2010). Predictors of Parents’ Willingness to Vaccinate for Human Papillomavirus and Physicians’ Intentions to Recommend the Vaccine. Women’s Health Issues, 20(1), 28–34. doi: 10.1016/j.whi.2009.08.007 [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, & Seeman TE (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51(6), 843–857. doi: 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Briscoe C, & Aboud F. (2012). Behaviour change communication targeting four health behaviours in developing countries: A review of change techniques. Social Science & Medicine, 75(4), 612–621. doi:doi: 10.1016/j.socscimed.2012.03.016 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). What is HPV? Retrieved from https://www.cdc.gov/hpv/parents/whatishpv.html
- Centers for Disease Control and Prevention. (2018). Six Reasons to Get HPV Vaccine for Your Child. Retrieved from https://www.cdc.gov/hpv/infographics/vacc-six-reasons.html
- Centers for Disease Control and Prevention. (2019a). How Many Cancers Are Linked with HPV Each Year? Retrieved from https://www.cdc.gov/cancer/hpv/statistics/cases.htm
- Centers for Disease Control and Prevention. (2019b). TeenVaxView: 2018 Adolescent Human Papillomavirus Vaccination Coverage Report. Retrieved from https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/datareports/hpv/reports/2018.html
- Centers for Disease Control and Prevention [CDC]. (2017). Clinicians Factsheets and Guidance. Retrieved from https://www.cdc.gov/hpv/hcp/clinician-factsheet.html
- Coles VAH, Patel AS, Allen FL, Keeping ST, & Carroll SM (2014). The association of human papillomavirus vaccination with sexual behaviours and human papillomavirus knowledge: a systematic review. International Journal of STD & AIDS, 26(11), 777–788. doi: 10.1177/0956462414554629 [DOI] [PubMed] [Google Scholar]
- Constantine NA, & Jerman P. (2007). Acceptance of Human Papillomavirus Vaccination among Californian Parents of Daughters: A Representative Statewide Analysis. Journal of Adolescent Health, 40(2), 108–115. doi: 10.1016/j.jadohealth.2006.10.007 [DOI] [PubMed] [Google Scholar]
- DiStefano AS, Hui B, Barrera-Ng A, Quitugua LF, Peters R, Dimaculangan J, Vunileva I, Tui’one V, Takahashi LM, Tanjasiri SP (2012). Contextualization of HIV and HPV risk and prevention among Pacific Islander young adults in Southern California. Social Science & Medicine, 75(4), 699–708. doi: 10.1016/j.socscimed.2012.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freimuth VS, Jamison AM, An J, Hancock GR, & Quinn SC (2017). Determinants of trust in the flu vaccine for African Americans and Whites. Social Science & Medicine, 193, 70–79. doi: 10.1016/j.socscimed.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu LY, Zimet GD, Latkin CA, & Joseph JG (2017). Associations of trust and healthcare provider advice with HPV vaccine acceptance among African American parents. Vaccine, 35(5), 802–807. doi: 10.1016/j.vaccine.2016.12.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galbraith KV, Lechuga J, Jenerette CM, Moore LA,, Palmer MH, & Hamilton JB (2016). Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: A literature review. Social Science & Medicine, 159, 116–126. [DOI] [PubMed] [Google Scholar]
- Gravitt PE, & Winer RL (2017). Natural History of HPV Infection across the Lifespan: Role of Viral Latency. Viruses, 9(10), 267. doi: 10.3390/v9100267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines MP, Perkins HW, Rice RM, & Barker G. (2005). A Guide to Marketing Social Norms for Health Promotion in Schools and Communities. [Google Scholar]
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, & Stokley S. (2014). Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA pediatrics, 168(1), 76–82. doi: 10.1001/jamapediatrics.2013.2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull PC, Williams EA, Khabele D, Dean C, Bond B, & Sanderson M. (2014). HPV vaccine use among African American girls: qualitative formative research using a participatory social marketing approach. Gynecologic oncology, 132 Suppl 1(0 1), S13-S20. doi: 10.1016/j.ygyno.2014.01.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison AM, Quinn SC, & Freimuth VS (2019). “You don’t trust a government vaccine”: Narratives of instituional trust and influenza vaccination among African American and white adults. Social Science & Medicine, 221, 87–94. doi: 10.1016/j.socscimed.2018.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jena AB, Goldman DP, & Seabury SA (2015). Incidence of Sexually Transmitted Infections After Human Papillomavirus Vaccination Among Adolescent Females. JAMA Intern Med, 175(4), 617–623. doi: 10.1001/jamainternmed.2014.7886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiser M, & Lovelace K. (2019). A National Network of Public Health and Faith-Based Organizations to Increase Influenza Prevention Among Hard-to-Reach Populations. American journal of public health, 109(3), 371–377. doi: 10.2105/AJPH.2018.304826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreps G, & Maibach E. (2008). Trandisciplinary Science: The Nexus Between Communication and Public Health. Journal of Communication, 58, 732–748. [Google Scholar]
- Mattis JS (2000). African American Women’s Definitions of Spirituality and Religiosity. Journal of Black Psychology, 26(1), 101–122. doi: 10.1177/0095798400026001006 [DOI] [Google Scholar]
- Mullins TLK, Widdice LE, Rosenthal SL, Zimet GD, & Kahn JA (2015). Risk perceptions, sexual attitudes, and sexual behavior after HPV vaccination in 11–12 year-old girls. Vaccine, 33(32), 3907–3912. doi: 10.1016/j.vaccine.2015.06.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, E., & Medicine. (2019). Faith–Health Collaboration to Improve Community and Population Health: Proceedings of a Workshop. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Newport F. (2017). 2017 Update on Americans and Religion . The Gallup Organization. Retrieved from https://news.gallup.com/poll/224642/2017-update-americans-religion.aspx [Google Scholar]
- Petrosky EY, Liu G, Hariri S, & Markowitz LE (2017). Human Papillomavirus Vaccination and Age at First Sexual Activity, National Health and Nutrition Examination Survey. Clinical pediatrics, 56(4), 363–370. doi: 10.1177/0009922816660541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. (2014). Religious Landscape Study: Racial and ethnic composition. Retrieved from http://www.pewforum.org/religious-landscape-study/racial-and-ethnic-composition/
- Puffer ES, Green EP, Sikkema KJ, Broverman SA, Ogwang-Odhiambo RA, Pian J. (2016). A church-based intervention for families to promote mental health and prevent HIV among adolescents in rural Kenya: Results of a randomized trial. Journal of Consulting and Clinical Psychology, 84(6), 511–525. doi: 10.1037/ccp0000076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rysavy MB, Kresowik JDK, Liu D, Mains L, Lessard M, & Ryan GL (2014). Human Papillomavirus Vaccination and Sexual Behavior in Young Women. Journal of Pediatric and Adolescent Gynecology, 27(2), 67–71. doi: 10.1016/j.jpag.2013.08.009 [DOI] [PubMed] [Google Scholar]
- Shelton RC, Snavely AC, De Jesus M, Othus MD, & Allen JD (2013). HPV vaccine decision-making and acceptance: does religion play a role? J Relig Health, 52(4), 1120–1130. doi: 10.1007/s10943-011-9553-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LM, Kaufman JS, Stumpf EC, & Levesque LE (2015). Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. CMAJ, 187(2), E74–E81. doi: 10.1503/cmaj.140900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohl AE, Mendoza G, Ghant MS, Cameron KA, Simon MA, Schink JC, & Marsh EE (2015). Barriers to prevention: knowledge of HPV, cervical cancer, and HPV vaccinations among African American women. American journal of obstetrics and gynecology, 212(1), 65.e61–65.e655. doi: 10.1016/j.ajog.2014.06.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor MC (1998). Critical terms for religious studies. Chicago: University of Chicago Press. [Google Scholar]
- The Johns Hopkins Center for Communication Programs. Social and Behavior Change Communication Saves Lives. Retrieved from http://ccp.jhu.edu/wp-content/uploads/JHU_Social_and_Behaviour_FULL_OUTLINES_V2.pdf
- UNICEF. (n.d.). Module 1: What are the Social Ecological Model (SEM), Communication for Development (C4D)? Retrieved from https://www.unicef.org/cbsc/files/Module_1_SEM-C4D.docx
- Williams J, Fisher MP, Bayliss EA, Morris MA, & O’Leary ST (2020). Clergy attitudes toward vaccines and vaccine advocacy: a qualitative study. Human Vaccines & Immunotherapeutics, 1–9. doi: 10.1080/21645515.2020.1736451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. (2014). Attitudes to vaccination: A critical review. Social Science & Medicine, 112, 1–11. doi: 10.1016/j.socscimed.2014.04.018 [DOI] [PubMed] [Google Scholar]