1. Visual case discussion
A 51-year-old man attended the emergency department for left eye immediate pain after face mask removal for office lunch. He complained of left eye tearing and foreign body sensation. Without any ocular disease or ophthalmic surgery history, he did not wear glasses or contact lens. Patient postulated his left eye was scratched by the sharp edge of the face mask upon removal.
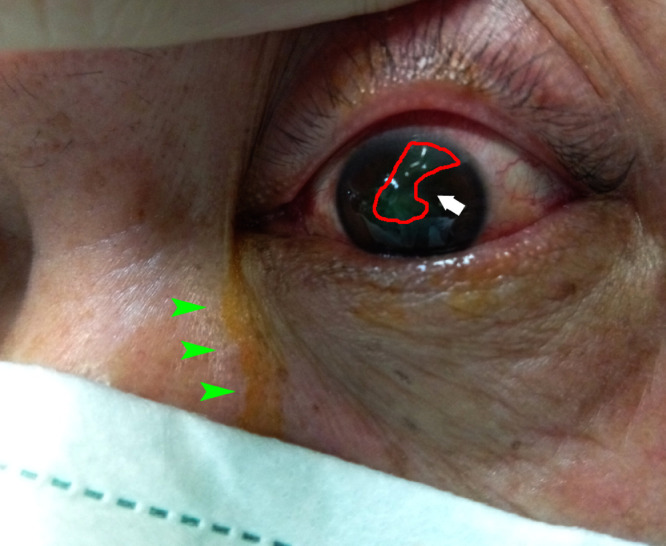
Emergency screening examinations found injected left eye (Fig. 1 ) with an oblique area of simple corneal abrasion, stained up by fluorescein, without corneal infiltration. The corneal laceration was superficial without deep stromal involvement upon slit lamp examination, and Seidel test was negative. Analgesic eye drops were given to complete a thorough eye examination. Visual acuity was Snellen 1.0 and 0.3 over right and left eye respectively, and intraocular pressures were normal of 15 mmHg over both eyes. Anterior chambers were deep bilaterally and symmetrical; pupils were round and reactive, of equal 3 mm size, without any signs of subtle eyeball rupture. Fundus examinations were unremarkable.
Fig. 1.
Clinical photo of patient's left eye after the injury. The oblique corneal abrasion area (white arrow) was stained green (outlined by red line) with fluorescein; note the fluorescein stained tears (green arrowheads).
Patient was given hypromellose eye drops, symptoms gradually improved, and the corneal abrasion was healed in 4 days. Follow-up visits did not reveal any infection, nor corneal scarring. Visual acuity of the left eye was back to Snellen 1.0 after full recovery. Patient voiced out an adaptive change on his face mask removal technique after the incident, aiming to avoid edges of the face mask passing around the cornea.
Despite the vigorous debate across parties worldwide, face mask wear is promising in minimizing the spread of COVID-19. Most healthcare workers are now wearing face masks within clinical areas. On the other hand, simple surgical face mask is gaining popularity among the public.1 With an increased usage, face mask related ocular complaints such as dry eyes, ocular allergies, periocular skin deconditioning etc. all become hot research topics. However, face mask related direct ocular trauma was rarely reported in literature, in contrast to previous report on alcohol-based hand sanitizer related ocular injury.2
Our reported case of ocular surface injury by the sharp edge of face mask serves as an important reminder to both daily face mask users of the general public, and the manufacturers for improving their products' design. The injury mechanism in our case was thought to be a rotational move of the mask in front of the face (Fig. 2 , green arrow) when the eye was hit by the squared edge (Fig. 2, red arrow). Reviewing the commonly available face masks, we found their corners and the corrugated side edges (Fig. 3 , red arrows) are all potential sharp points that could lacerate the corneal surface.
Fig. 2.
Proposed mechanism of injury was demonstrated by the attending physician. The face mask was taken off with right hand with a rotational move (green arrow), the sharp edge of the mask then scratched the left cornea (red arrow).
Fig. 3.
Simple corneal abrasion alone can cause intense pain and distress, as denuding the corneal epithelium exposes the nociceptors in the corneal stroma. Cornea is one of the most richly innervated human tissues, with a few hundred times more densely packed pain receptors than our surface skin.3 This pain is often accompanied by photophobia and lacrimation, mimicking the picture of more severe ocular inflammations like uveitis or scleritis flare. Simple corneal abrasion could be treated barely by supportive lubrications, whereas topical antibiotic eye drop is indicated in corneal infiltrate cases. Short term topical cycloplegic eye drop might be given for comfort purpose, or dampening the anterior chamber activities. Patching of the injury eye is often not advisable as it delays healing.
Complications of corneal abrasion include, but not limited to, recurrent corneal erosion syndrome (RCES) and microbial keratitis. RCES defined as recurrent episodes of spontaneous breakdown of corneal epithelium, is particularly vulnerable in large and ragged abrasion. With defects in hemi-desmosomes, RCES's pathology lies on the failure of epithelium to basement membrane re-adhesion. Diabetes, dry eye, ocular rosacea, previous sharp trauma, and corneal dystrophies (e.g. epithelial basement membrane dystrophy) are all risk factors of RCES. Therefore, patients with traumatic corneal abrasion should be warned of RCES, when the recurrent episodes usually start at eye opening after sleep.
In short, face mask usage is more prevalent worldwide in the COVID-19 era. Other than proper handling of face mask to prevent infection, users are reminded of its potential harm from the subtle sharp edges.
Declaration of Competing Interest
None
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.visj.2020.100958.
Appendix
Multiple Choice Questions
Question 1:
Which of the following clinical examinations is useful to differentiate full-thickness corneal laceration from partial/ superficial corneal laceration?
-
A)
Hirschberg test
-
B)
Jones test
-
C)
Krimsky test
-
D)
Schirmer's test
-
E)
Seidel test
Correct answer: (E) Seidel test
Discussion & rationale:
Seidel test is the use of fluorescein stain/ strip to assess corneal wound leakage. A full-thickness corneal laceration would allow aqueous humor to leak outside the eye, thus a positive Seidel test. There should not be leakage in partial/ superficial corneal laceration.
Hirschberg test and Krimsky test are both corneal reflection tests used to assess ocular motility, strabismus and manifest deviations. Jones test involves the use of fluorescein dye to examine the patency of nasolacrimal drainage system. Schirmer's test is used to evaluate tear secretion in dry eyes patient.
Question 2:
Which of the following diseases could present with pain simulating corneal abrasion?
-
a)
Acute angle closure attack with intraocular pressure (IOP) of 60 mmHg
-
b)
Contact lens related microbial keratitis
-
c)
Rheumatoid arthritis associated necrotizing anterior scleritis
-
d)
Uveitis with elevated IOP
-
e)
All of the above
Correct answer: (e) All of the above
Discussion & rationale:
All of the above are acute ocular conditions presenting with eye pain. High IOP, no matter of what causes, is associated with headache and nausea. Similar to corneal abrasion, inflammatory ocular diseases release mediators that stimulate the densely packed nociceptors over the cornea, ocular surface and uveal tract, resulting in ocular pain.
Question 3:
Which of the following are risk factors for recurrent corneal erosion syndrome?
-
A
Corneal dystrophies
-
B
Dry eye
-
C
Ocular rosacea
-
D
Previous sharp trauma
-
E
All of the above
Correct answer: (E) All of the above
Discussion & rationale:
Recurrent corneal erosion syndrome (RCES) defined as recurrent episodes of spontaneous breakdown of corneal epithelium, is particularly vulnerable in large and ragged abrasion. With defects in hemi-desmosomes, RCES's pathology lies on the failure of epithelium to basement membrane re-adhesion. Diabetes, dry eye, ocular rosacea, previous sharp trauma, and corneal dystrophies (e.g. epithelial basement membrane dystrophy) are all risk factors of RCES.
Appendix B. Supplementary materials
References
- 1.Au SC. A surge in eye clinic nonattendance under 2019 novel coronavirus outbreak. Indian J. Ophthalmol. 2020;68:948. doi: 10.4103/ijo.IJO_673_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Au SCL. Hand sanitizer associated ocular chemical injury: A mini-review on its rise under COVID-19. Vis J Emerg Med. 2020;21 doi: 10.1016/j.visj.2020.100881. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zander E, Weddell G. Observations on the innervation of the cornea. J. Anat. 1951;85:68–99. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.