Abstract
We study the spread of COVID-19 infections and deaths by county poverty level in the US. In the beginning of the pandemic, counties with either very low poverty levels or very high poverty levels reported the highest numbers of cases. A U-shaped relationship prevails for counties with high population density while among counties with low population density, only poorer counties report high incidence rates of COVID-19. Second, we discuss the pattern of infections spreading from higher to lower income counties. Third, we show that stay-at-home mandates caused significantly higher reductions in mobility in high income counties that experienced adverse weather shocks than counties that did not. These effects are not present in counties with high poverty rates. Using weather shocks in combination with stay-at-home mandates as an instrument for social distancing, we find that measures taken to promote social distancing helped curb infections in high income counties but not in low income counties. These results have important policy implications for containing the spread of infectious diseases in the future.
Keywords: Coronavirus, Pandemic, SARS-CoV-2, COVID-19, Heterogeneous health effects, Infections by poverty status, Death rates by poverty status
1. Introduction
Since the first US case of a SARS-CoV-2 infection was identified in Washington on January 21, 2020, both cases of SARS-CoV-2 infections and deaths due to COVID-19 have surged exponentially. On March 13, a little over 2000 identified infection cases were reported. Subsequently this number increased to over 161,000 by March and over 600,000 by April .1 By early April the US had the highest numbers of infections and COVID-19 related deaths in the world. Due to growing public health concerns almost all US states declared a state of emergency and numerous states issued stay-at-home orders. In this early period, the increase in the number of cases (infections as well as deaths) was concentrated in the East and West coastal regions. Although the geographic spread of the disease has been closely tracked, less is known about the relationship between the growth of SARS-CoV-2 infections and socioeconomic indicators.
The socioeconomic disparity in health outcomes is well-established in the field of Health Economics. According to Santerre and Neun (2010) there are three major channels that affect these differences: the education health gradient, the income health gradient, and differences in environmental exposure. Recently, the social psychology literature has highlighted that social interactions with close friends and family and even with peripheral members of our social networks contribute strongly to our overall well-being (Sandstrom and Dunn, 2014). However, a priori it is not clear how socioeconomic status correlates with social interactions. In light of the COVID-19 pandemic these contributing factors to socioeconomic disparity need to be reassessed as the pandemic has the potential to amplify them.
For example, although richer individuals have more resources to self-isolate, they are initially more likely to participate in economic and social activities compared to poorer individuals as many forms of social interaction are normal goods.2 This could make richer individuals more susceptible to being infected in the beginning of the pandemic. On the other hand, once infected, richer individuals have more resources to self-isolate and therefore prevent the spread within their social networks, while poorer individuals, once infected, may not be able to efficiently self-isolate due to resource constraints. Additionally, relatively poor individuals tend to be more involved in “frontline” essential work which may prevent them from self-isolating, even if non-pharmaceutical interventions (NPIs) such as stay-at-home mandates are in place (Blau et al., 2020b). Hence, differences in initial transmission pathways between rich and poor individuals as well as resource inequities warrant an investigation of the trends in the spread of SARS-CoV-2 infections and COVID-19 related deaths along the poverty spectrum.
Focusing on county-level effects, this paper describes trends of both SARS-CoV-2 infections cases and COVID-19 related deaths as of April 28, 2020 by socioeconomic status. We pursue three avenues of inquiry: first, we descriptively summarize the relationship between infection cases and poverty; second, we track the propagation of cases from richer to poorer counties; and third, we break down the effects of the chief countermeasure deployed against the disease, the stay-at-home order, by its effectiveness among high and low income county groups.
In the first part of this paper we rank counties by their poverty rates measured in 2016 and form 20 county groups with each group representing about the same number of people. We show that the relation between poverty and the cumulative number of identified infections is U-shaped, with infections concentrated among the richest and the poorest counties. The U-shaped curve is also present if we only examine highly populated areas. On the other hand, in a sub-sample of low density counties the COVID-19 case rates increase monotonically with the poverty level and the U-shape disappears. This may be indicative of an increased ability to self-isolate in rich low density areas compared to densely populated areas that are equally rich where self-isolation might be more difficult to achieve.
Furthermore, we observe that COVID-19 spread from higher to lower income communities during the early stages of the pandemic. Until the second week of March 2020, the number of cumulative cases of infections was significantly higher in high income counties. This is consistent with reports that the virus entered the US through international travel, which is disproportionately more prevalent among richer individuals.3 However, by the end of March a U-shaped pattern emerges, depicting high infection numbers in both tails of the county based poverty distribution. The increases in the number of cases in low income areas may be explained by a lack of resources in combination with specific job attributes that simply make it more difficult to practice adequate social distancing. This also makes NPIs such as the stay-at-home mandate less effective in poorer communities.
The third task of this paper is to investigate the interaction between socioeconomic status and the most widely implemented countermeasure: the stay-at-home order. By the 15th of March, 2020, almost all states in the US had declared a state of emergency and 15 states had implemented a stay-at-home order.4 It is difficult to directly assess the adequacy of these stay-at-home orders for various reasons. First, we are unsure of how effectively these laws were implemented. For instance, most of the mandates allow for essential tasks such as grocery shopping, dog-walking, visiting the pharmacy, etc. Numerous sources also document that NPIs were relatively lax in the US compared to other countries. For instance, out of 16 countries Chen et al. (2020) rank the US and UK as the two countries with the least effective NPIs. Pan et al. (2020) conclude that in the US, only the most aggressive NPIs were effective, with some less restrictive policies actually increasing death rates. Second, enforcement of these laws in the US is determined at the local level and varies by state and even county. Finally, the timing of the mandates might have been determined by expectations about the future spread of infections which creates a methodological challenge (Gupta et al., 2020b).
Table 1.
Non-Pharmaceutical Intervention (NPI) Roll-Out by State.
| State | SaH-Announce | SaH-Implem. | Emergency | School | Restaurant | NE-Business | Gathering | |
|---|---|---|---|---|---|---|---|---|
| 1 | Alaska | 3/27/20 | 3/28/20 | 03/11/20 | 03/16/20 | 03/17/20 | 03/24/20 | 03/28/20 |
| 2 | Alabama | 4/3/20 | 4/4/20 | 03/13/20 | 03/19/20 | 03/20/20 | 03/20/20 | |
| 3 | Arkansas | 03/11/20 | 03/17/20 | 03/19/20 | ||||
| 4 | Arizona | 3/30/20 | 3/31/20 | 03/11/20 | 03/16/20 | 03/20/20 | ||
| 5 | California | 3/19/20 | 3/19/20 | 03/04/20 | 03/19/20 | 03/15/20 | 03/11/20 | 03/19/20 |
| 6 | Colorado | 3/25/20 | 3/26/20 | 03/10/20 | 03/23/20 | 03/17/20 | 03/19/20 | 03/26/20 |
| 7 | Connecticut | 3/22/20 | 3/23/20 | 03/10/20 | 03/17/20 | 03/16/20 | 03/12/20 | 03/23/20 |
| 8 | Delaware | 3/24/20 | 3/24/20 | 03/13/20 | 03/16/20 | 03/16/20 | 03/16/20 | 03/24/20 |
| 9 | Florida | 4/1/20 | 4/3/20 | 03/09/20 | 03/16/20 | 03/17/20 | 04/03/20 | 03/30/20 |
| 10 | Georgia | 4/1/20 | 4/3/20 | 03/14/20 | 03/18/20 | 03/24/20 | 03/24/20 | |
| 11 | Hawaii | 3/23/20 | 3/25/20 | 03/04/20 | 03/23/20 | 03/17/20 | 03/16/20 | 03/25/20 |
| 12 | Iowa | 03/09/20 | 04/03/20 | 03/17/20 | 03/17/20 | |||
| 13 | Idaho | 3/25/20 | 3/25/20 | 03/13/20 | 03/23/20 | 03/25/20 | 03/25/20 | 03/25/20 |
| 14 | Illinois | 3/20/20 | 3/21/20 | 03/09/20 | 03/17/20 | 03/16/20 | 03/13/20 | 03/21/20 |
| 15 | Indiana | 3/23/20 | 3/25/20 | 03/06/20 | 03/19/20 | 03/16/20 | 03/12/20 | 03/24/20 |
| 16 | Kansas | 3/28/20 | 3/30/20 | 03/12/20 | 03/18/20 | 03/17/20 | ||
| 17 | Kentucky | 3/25/20 | 3/26/20 | 03/06/20 | 03/16/20 | 03/16/20 | 03/19/20 | 03/26/20 |
| 18 | Louisiana | 3/22/20 | 3/23/20 | 03/11/20 | 03/16/20 | 03/17/20 | 03/13/20 | 03/23/20 |
| 19 | Massachusetts | 3/23/20 | 3/24/20 | 03/10/20 | 03/17/20 | 03/17/20 | 03/13/20 | 03/24/20 |
| 20 | Maryland | 3/30/20 | 3/30/20 | 03/05/20 | 03/16/20 | 03/16/20 | 03/16/20 | 03/23/20 |
| 21 | Maine | 3/31/20 | 4/2/20 | 03/15/20 | 03/16/20 | 03/18/20 | 03/18/20 | 03/25/20 |
| 22 | Michigan | 3/23/20 | 3/24/20 | 03/10/20 | 03/16/20 | 03/16/20 | 03/13/20 | 03/23/20 |
| 23 | Minnesota | 3/25/20 | 3/28/20 | 03/13/20 | 03/18/20 | 03/17/20 | ||
| 24 | Missouri | 4/6/20 | 4/6/20 | 03/13/20 | 03/23/20 | 03/17/20 | 03/23/20 | |
| 25 | Mississippi | 4/1/20 | 4/3/20 | 03/14/20 | 03/20/20 | 03/24/20 | 03/24/20 | 03/31/20 |
| 26 | Montana | 3/23/20 | 3/28/20 | 03/12/20 | 03/16/20 | 03/20/20 | 03/24/20 | 03/28/20 |
| 27 | North Carolina | 3/27/20 | 3/30/20 | 03/10/20 | 03/16/20 | 03/17/20 | 03/14/20 | 03/30/20 |
| 28 | North Dakota | 03/13/20 | 03/16/20 | 03/20/20 | ||||
| 29 | Nebraska | 03/13/20 | 04/03/20 | 03/19/20 | 03/16/20 | |||
| 30 | New Hampshire | 3/27/20 | 3/28/20 | 03/13/20 | 03/16/20 | 03/16/20 | 03/16/20 | 03/28/20 |
| 31 | New Jersey | 3/21/20 | 3/21/20 | 03/09/20 | 03/18/20 | 03/16/20 | 03/16/20 | 03/21/20 |
| 32 | New Mexico | 3/23/20 | 3/24/20 | 03/11/20 | 03/16/20 | 03/16/20 | 03/16/20 | 03/24/20 |
| 33 | Nevada | 4/1/20 | 4/1/20 | 03/12/20 | 03/16/20 | 03/17/20 | 03/19/20 | 03/21/20 |
| 34 | New York | 3/20/20 | 3/22/20 | 03/07/20 | 03/18/20 | 03/16/20 | 03/13/20 | 03/20/20 |
| 35 | Ohio | 3/23/20 | 3/24/20 | 03/09/20 | 03/17/20 | 03/15/20 | 03/12/20 | 03/24/20 |
| 36 | Oklahoma | 03/15/20 | 03/17/20 | 03/25/20 | 03/24/20 | 03/26/20 | ||
| 37 | Oregon | 3/20/20 | 3/23/20 | 03/08/20 | 03/16/20 | 03/17/20 | 03/16/20 | |
| 38 | Pennsylvania | 3/23/20 | 3/23/20 | 03/06/20 | 03/16/20 | 03/17/20 | 03/16/20 | 03/23/20 |
| 39 | Rhode Island | 3/28/20 | 3/28/20 | 03/09/20 | 03/16/20 | 03/16/20 | 03/17/20 | |
| 40 | South Carolina | 4/6/20 | 4/7/20 | 03/13/20 | 03/16/20 | 03/18/20 | 03/18/20 | |
| 41 | South Dakota | 03/13/20 | 03/16/20 | 04/06/20 | ||||
| 42 | Tennessee | 3/30/20 | 4/1/20 | 03/12/20 | 03/20/20 | 03/23/20 | 03/23/20 | 04/01/20 |
| 43 | Texas | 3/31/20 | 4/2/20 | 03/13/20 | 03/23/20 | 03/20/20 | 03/20/20 | |
| 44 | Utah | 3/29/20 | 4/1/20 | 03/06/20 | 03/16/20 | 03/18/20 | 03/16/20 | |
| 45 | Virginia | 3/30/20 | 3/30/20 | 03/12/20 | 03/16/20 | 03/17/20 | 03/15/20 | |
| 46 | Vermont | 3/25/20 | 3/25/20 | 03/13/20 | 03/18/20 | 03/17/20 | 03/13/20 | 03/25/20 |
| 47 | Washington | 3/23/20 | 3/23/20 | 02/29/20 | 03/17/20 | 03/16/20 | 03/11/20 | 03/25/20 |
| 48 | Wisconsin | 3/24/20 | 3/25/20 | 03/12/20 | 03/18/20 | 03/17/20 | 03/17/20 | 03/25/20 |
| 49 | West Virginia | 3/23/20 | 3/24/20 | 03/16/20 | 03/16/20 | 03/17/20 | 03/24/20 | |
| 50 | Wyoming | 03/13/20 | 03/16/20 | 03/19/20 | 03/20/20 |
Notes: Author’s search and Ortiz and Hauck (2020) for stay-at-home announcement date, Mervosh et al. (2020) for stay-at-home implementation and Gupta et al. (2020b) for the other categories. SaH refers to stay-at-home mandate and NE-Business refers to non-essential business closures.
In order to investigate the relationship between social distancing and infections at the onset of the pandemic, we use arguably exogenous county level weather shocks (i.e., unusually low temperatures) coupled with the local stay-at-home mandate as instruments for mobility, and then estimate the effects on COVID-19 cases in rich (below the 50th percentile of the 2016 county poverty ranking) and poor (above the 50th percentile of the 2016 county poverty ranking) county groups, respectively. The working assumption for identification is that while the marginal cost of mobility itself is high during a lockdown period, extreme weather during the lockdown will further constrain mobility.
In order to implement the two-step procedure we use cell phone mobility data and track the interaction effect of the legal mandate and weather shocks on mobility in an event study framework. We first show that prior to the mandate there are no statistically significant differential trends in mobility between counties that experience a bad weather shock and counties that do not. Second, we show that after a mandate is in effect, average mobility in richer counties that experience weather shocks decreases compared to similarly rich counties without a weather shock. We are not able to detect such differences in mobility in lower income counties. One possible explanation for this finding is that essential (frontline) workers, who are to some extent excluded from the constraints imposed by stay-at-home mandates, tend to live in poorer neighborhoods (Blau et al., 2020b). Next, we use the predicted mobility measures from the first step and show that a 1% decrease in mobility in either week two, three, or four following the mandate announcement decreases COVID-19 caseloads by 1.6, 2.16, and 2.2%, respectively. However, these results are only observable in richer counties as poorer counties did not experience decreases in mobility of the same magnitude. Our back-of-the-envelope calculation suggests that an increase in social distancing following a stay-at-home mandate leads to a 38% reduction in COVID-19 infections among high income counties.
Our findings come with two caveats. First, the exclusion restriction for a valid instrument in this context is governed by the assumption that weather shocks affect coronavirus infections only through a reduction in human-to-human interactions and not directly through a biological channel.5 Second, this calculation is based on an IV estimator which only measures the Local Average Treatment Effect (LATE).
Literature Review. COVID-19 studies in economics are emerging rapidly, with researchers investigating various forms of economic disruptions created by the disease. Our paper makes contributions to the following strands of this literature.
First, there is a literature tracking the early economic effects of the pandemic on mobility patterns and population health. Some of these studies such as Brown and Ravallion (2020) and Chang et al. (2020) show correlations between socioeconomic characteristics and COVID-19 caseloads in connection with observed changes in mobility which is mostly based on newly available cell phone data.6 We contribute to this literature and show a distinct U-shape pattern between COVID-19 cases and county poverty measures that appears early on in the pandemic. This pattern subsequently dissipates as the virus spreads more broadly. As far as we are aware, we are the first to show this systematically in a non-parametric framework. We then relate this pattern to a plausible pathway of the virus spreading from high to low income areas with high population density.
Second, the program evaluation literature investigates the effects of the stay-at-home orders on coronavirus cases and associated labor market effects. Friedson et al. (2020) find that in California the adoption of a statewide Shelter-In-Place Order on March 19, 2020 reduced COVID-19 cases by 125.5–219.7 per 100,000 individuals by April 20, 2020. In a follow up study, Dave et al. (2020) expand their identification strategy by utilizing across state variation in the timing of stay-at-home mandates. They find that mandates decrease the number of cumulative COVID-19 cases by 44%.7 However, Gupta et al. (2020b) express methodological concerns in conducting a program evaluation of stay-at-home mandates by highlighting that a state government’s decision to adopt the law is based on the projection of future growth in the number of caseloads and often predates increases in cases and deaths. This creates non-trivial methodological challenges in using these laws as valid natural experiments.
Our novel approach to evaluate the effectiveness of social distancing on slowing the spread of infections in high vs. low income communities uses arguably exogenous weather shocks along with stay-at-home mandates as instruments for mobility. The only other studies we are aware of that also use weather data to construct instrumental variables in connection with the coronavirus pandemic are Qiu et al. (2020), Brzezinski et al. (2020) and Kapoor et al. (2020). Our approach differs from theirs in two ways. First, previous studies have used weather patterns as arguably exogenous instruments for social distancing which results in consistent estimates of the effect of social distancing on the transmission rate of COVID-19. We, on the other hand, use stay-at-home mandates as a second instrument which is a subtle but important methodological change of the estimation method. Our analysis uses variation from arguably exogenous natural forces (weather patterns) that bolster the effectiveness of government regulation in order to identify the effect of stay-at-home mandates on COVID-19 infections through the channel of reduced mobility (i.e., social distancing). Second, we investigate the differential effects of government mandates on mobility and COVID-19 infections between high and low income communities which will provide policymakers with new evidence concerning the efficacy of pandemic response regulations.
A closely related strand of literature focuses on documenting the labor market disruptions associated with COVID-19 (e.g., Atkinson, Dolmas, Koch, Koenig, Mertens, Murphy, Yi, 2020, Andersen, Maclean, Pesko, Simon, 2020, Coibion, Gorodnichenko, Weber, 2020, Kong, Prinz, 2020). These studies document significant increases in unemployment and estimate job loss numbers of up to 20 million. Mongey et al. (2020) indicate that workers in “low-ability-to-work-from-home” sectors experience greater losses in short-term employment and are also more likely to be economically vulnerable. Similarly, some studies argue that the effects of NPIs such as the “Great Lockdown” can vary across populace and are less-binding among frontline essential workers, who find it difficult to substitute their work with work done from their homes. (Blau, Koebe, Meyerhofer, 2020, Kahn, Lange, Wiczer, 2020). Our research is complementary in that we document that mandates are less effective in reducing mobility in low income counties. And while we do not make a direct connection from mobility to employment, the literature mentioned here certainly has established this link, especially for lower paying jobs in some of the essential sectors.
The study is organized as follows. Section 2 documents the data used in the study, Section 3 describes the estimation, while Section 4 discusses the results. Section 5 concludes the study.8
2. Data
2.1. County level SARS-CoV-2/COVID-19 data
The county level data for cases of SARS-CoV-2 infections and COVID-19 related deaths are extracted from the USAFacts website. This database provides cumulative numbers of infection cases and deaths for each county since January 22nd, 2020 and the numbers at the county-levels are updated by referencing the state and local agencies directly.9
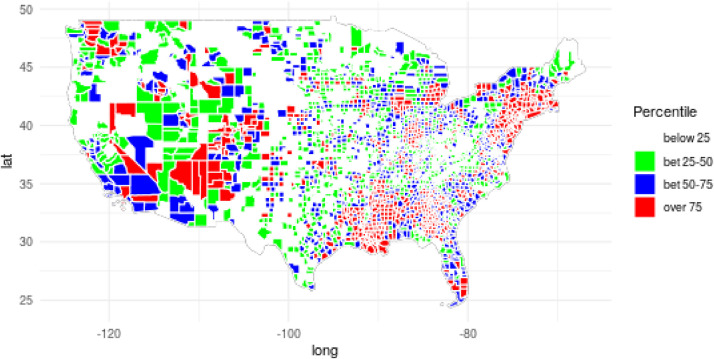
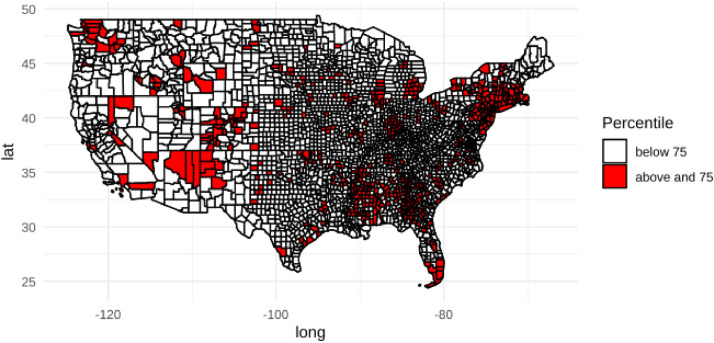
Using the cumulative number of events (infection cases and deaths), we focus on five cross sections at the county level: March 11th, March 23rd, April 7th April 20th, and April 28th to conduct descriptive analysis of the spread in infections across poverty spectrum. The spatial dispersion of cases and deaths are presented in Figs. 1 and 2 for April 28th respectively. We also construct the weekly number of new cases aggregated at the county level starting from the week following January 22nd–April 28th, 2020 which results in 14 weeks of panel data. The county level panel sample is used to evaluate the impacts of effective social distancing on the spread of infection across higher income and lower income communities. Table 2 shows the summary statistics of the county level panel sample from weeks of January 22nd to April 28th, 2020.
Fig. 1.
SARS-CoV-2 Confirmed Infections by County.
Notes: The data is from USAFacts as of April 28, 2020.
Fig. 2.
COVID-19 Related Deaths by County.
Notes: The data is from USAFacts and shows counties with deaths above the 75th percentile as of April 28, 2020.
Table 2.
Summary Statistics.
| Variable |
Sample |
|
|---|---|---|
| Mean | S.D. | |
| Total Cases on March 11, 2020 (per county) | 0.42 | 5.55 |
| Total Cases March 23, 2020 (per county) | 13.83 | 137.27 |
| Total Cases April 7, 2020 (per county) | 126.07 | 948.82 |
| Total Cases April 20, 2020 (per county) | 249.30 | 1734.36 |
| Total Cases April 28, 2020 (per county) | 323.16 | 2128.89 |
| Total Deaths on March 11, 2020 (per county) | 0.01 | 0.48 |
| Total Deaths March 23, 2020 (per county) | 0.17 | 2.03 |
| Total Deaths April 7, 2020 (per county) | 4.02 | 39.31 |
| Total Deaths April 20, 2020 (per county) | 11.98 | 109.37 |
| Total Deaths April 28, 2020 (per county) | 17.92 | 168.51 |
| Log of Population Density | 3.74 | 1.75 |
| Unemployment Rate | 4.44 | 1.81 |
| Percent Less than High School | 13.77 | 6.42 |
| Percent over 55 | 33 | 6 |
| Percent Black over 55 | 2 | 4 |
| Percent on Poverty | 16.23 | 6.44 |
| Total Number of Coronavirus Tests | 161,343 | 432,220 |
| Stay-at-Home Mandate (Announcement) | 0.31 | 0.46 |
| Emergency Declaration | 0.50 | 0.50 |
| Restaurant and Bar Restriction | 0.39 | 0.49 |
| Non-Essential Business Restriction | 0.38 | 0.49 |
| Restriction on Large Gathering | 0.18 | 0.39 |
| Average Temperature (in Fahrenheit) | 46.42 | 12.88 |
| Precipitation (in inches) | 0.10 | 0.13 |
| Weather Shock (Proportion) | 0.13 | 0.34 |
Notes: The sample is a balanced panel of weekly observations from 3092 US counties starting from January 22–April 28, (14 weeks), 2020 with a total of N=43,288 county/week observations.
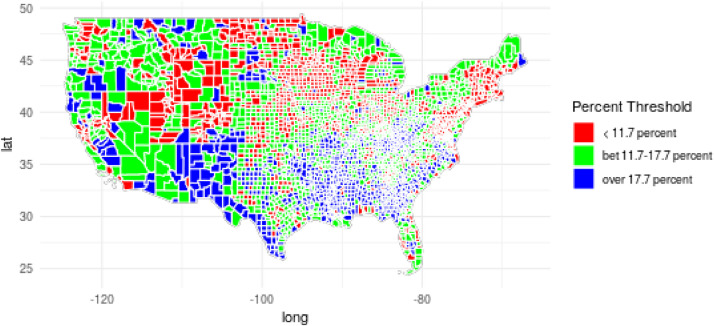
2.2. Other data sources
Poverty Data. We use the Small Area Income and Poverty Estimates (SAIPE) county estimates for 2016. The data show the percentage of the population in a county living below the poverty level.10 The spatial distribution of poverty across counties is shown in Fig. 3. The county level population data by age and race is extracted from the Survey of Epidemiology and End Results (SEER) through the NBER website.11 The land area and unemployment rate data are obtained from the US Census Bureau and Bureau of Labor Statistics, respectively.
Fig. 3.
Poverty Rates in 2016.
Notes: The data is based on Small Area Income and Poverty Estimates (SAIPE) county estimates.
Social Distancing Data. We use social distancing data from SafeGraph.12 SafeGraph is offering a temporary social distancing metric that provides daily views of median movements from one’s home (in meters) based on cell phone data aggregated at the census block level. Daily data is available going back to January 1, 2020. The data is generated using a panel of GPS pings from anonymous mobile devices. A common nighttime location of each mobile device over a 6 week period is generated at the Geohash-7 granularity which is approximately a meters area. This location is referred to as the device’s “home”. Devices are then aggregated by home census block group. Variables are provided for each census block group. We use two variables: device-count and distance-traveled-from-home. The first is simply the total number of active devices in the census block group. Census block groups with device counts less than five are excluded and the distance traveled variable is the median distance (in meters) traveled from the home location by the devices included in the device count during the time period (excluding any distances of 0). First the median for each device is calculated and then the median (distance traveled from home) over all devices is reported in the SafeGraph data. We then aggregate these census block group medians to the county level using the number of devices in each census block as weights.
Weather Data. We gather daily weather data from Weather Underground13 for each county and aggregate the data at weekly level. We searched Wikipedia to determine the largest (most populous) community in each county and put the result into Weather Underground to obtain historical weather data for each county using the weather station assigned to that jurisdiction by Weather Underground. More specifically, we first searched a county in Google. We then looked through the results to see if the first page mentioned the largest community in the county. If it was not mentioned on the first page, we used Wikipedia which was linked on the first page of every set of Google results. Once we had the name of the largest community, we searched for this community on the Weather Underground website. We then navigated to History which automatically updates to the nearest weather station that retains historical weather data. We then saved the name of the weather station and extracted the weather data from January–April 2020 for this county.
Following the procedure mentioned in the previous paragraph, we collect daily weather data at the county level for 3092 counties, which are used to calculate weekly averages. This gives us a balanced panel for 3092 counties over the span of 14 weeks, starting from January 22 until April 28.14 The weather data is used to construct arguably exogenous weather shocks, which along with the mandate are used as instruments as described in Section 3.
Testing data. We gather daily cumulative number of tests administered at the state level from The COVID Tracking Project.15 The number of coronavirus tests conducted is extracted from the local or state public health authorities. The cumulative number of tests is aggregated at the weekly level.
2.3. Descriptive analysis: emerging patterns of coronavirus cases by poverty level
Our first goal is to analyze the relationship between poverty levels at the county level and coronavirus infections/deaths. We first proceed with a non-parametric approach and rank each county according to its poverty level – defined as the percentage of the county’s population with income below the national poverty level in 2016. We next form 20 county-groups so that the overall population size of each county-group is approximately the same. The first so constructed county-group contains the counties with the lowest poverty levels and the last county-group contains counties with the highest poverty levels.16 We then produce scatter plots with the county-grouping poverty levels on the horizontal axis and the county-group coronavirus infections/deaths on the vertical axis.
Although the approach defined in the preceding paragraph adjusts for population size, it does not account for population density of an area, which is arguably an important determinant of coronavirus infections. We next account for population density within a county-group and divide counties into low and high density counties according to the median density value of all counties. We then rank all low density counties and all high density counties separately and repeat the county-group procedure from the previous paragraph for low and high density counties separately to produce scatter plots of the two different county-group categories.
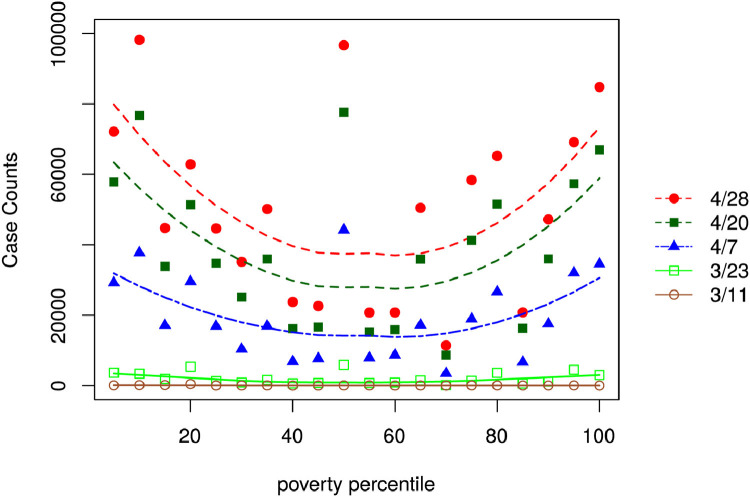
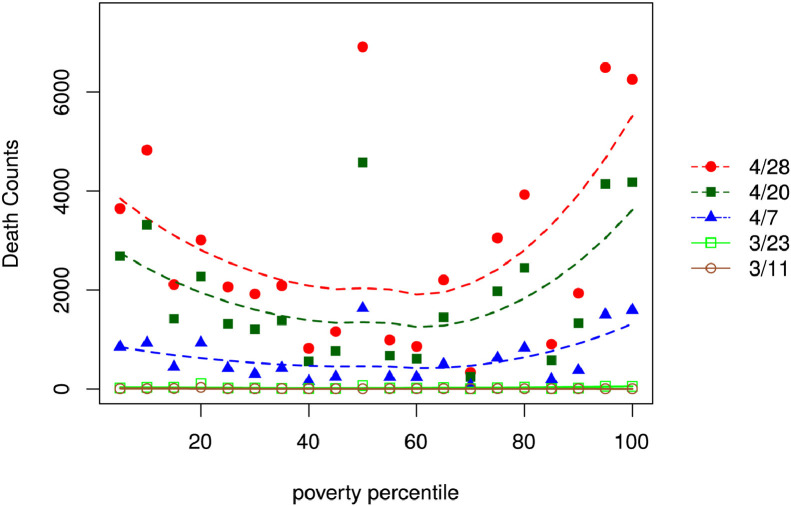
County Poverty Rates and Coronavirus Cases.Figs. 4 and 5 plot the number of coronavirus infections and COVID-19 related deaths for each percentile of the county-group poverty distribution. We split the sample into five time periods that are indicated by markers that correspond to the total number of cases by March 11th, March 23rd, April 7th, April 20th, and April 28th, respectively. We use local linear regressions and smoothing parameters based on the leave-one-out cross-validation method to fit a curve for each period sample.17
Fig. 4.
SARS-CoV-2 Confirmed Infections by Poverty Percentile.
Notes: The source of data is USAFacts, as of April 28, 2020. We report the number of cumulative (infection) cases for March 11, March 23, April 7, April 20, and April 28 in 2020 for 20 county-groups ranked by poverty rate percentile. The curves are fitted using a smoothing method based on local linear regressions as described in Appendix A.
Fig. 5.
COVID-19 Related Deaths by Poverty Percentile.
Notes: The source of data is USAFacts, as of April 28, 2020. We report the number of cumulative deaths due to COVID-19 for March 11, March 23, April 7, April 20, and April 28, in 2020 for 20 county-groups ranked by poverty rate percentile. The curves are fitted using a smoothing method based on local linear regressions as described in Appendix A.
Both Figs. 4 and 5 show emerging trends in the number of infections and deaths according to county-groupings, sorted by the county poverty level. The fitted curve pertaining to March 11 is flat, indicating that the number of identified cases was very low at this time so that no discernible difference between rich and poor counties is detectable. By March 23 a pattern begins to emerge with relatively higher case counts at the very low and very high poverty percentiles. This pattern becomes more pronounced by April 7 where a U-shaped curve begins to show. This indicates that the number of infections are higher at the lowest and the highest poverty groupings with a relatively low number of cases at the mid-level poverty levels. By April 20 the U-shaped curve is well pronounced and appears consistently thereafter.18
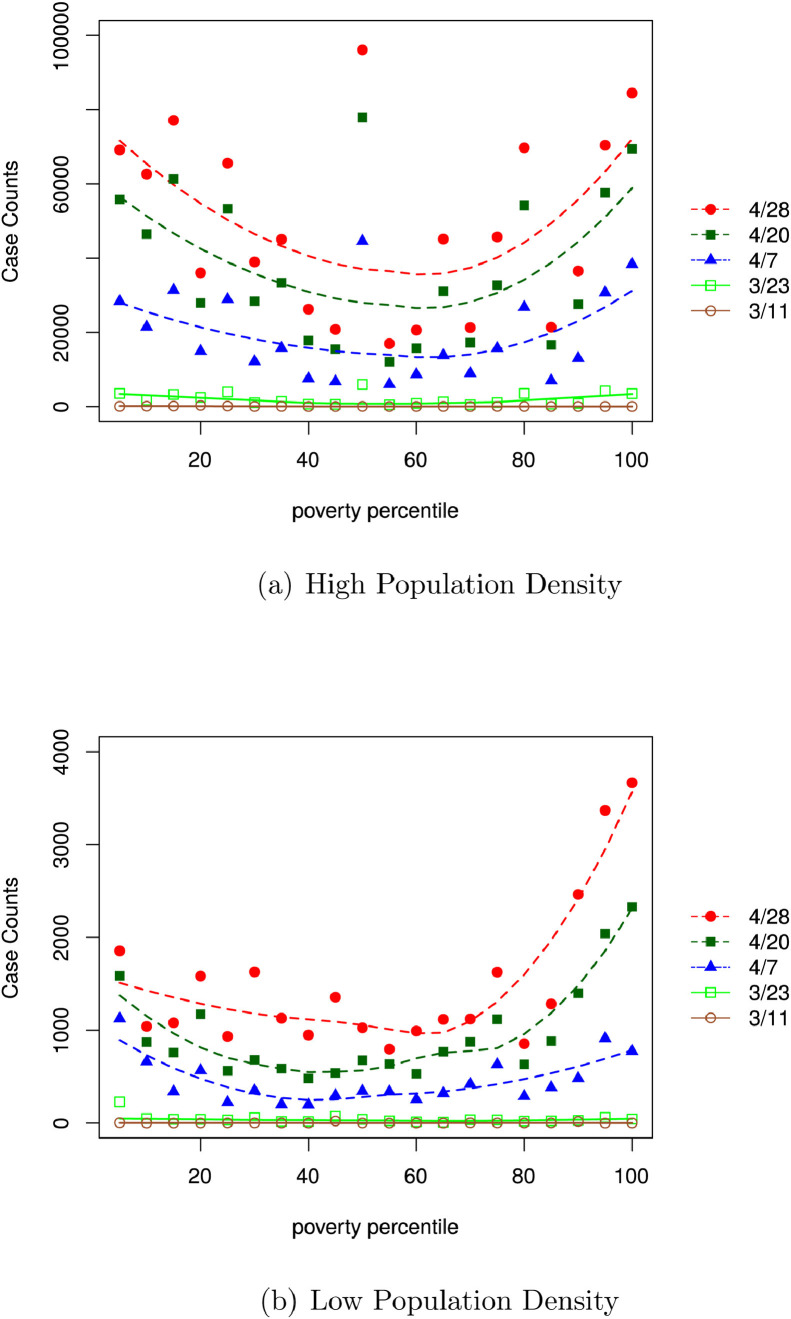
The pattern of COVID-19 related deaths, shown in Fig. 5, is similar except that deaths are disproportionately concentrated in county-groupings with higher poverty levels. In order to discern patterns by population density, we use the median population density of all counties and split the sample into a low density counties sample and a high density counties sample. We then repeat the grouping procedure above for each sample separately. Fig. 6 (a) and (b) show the patterns of the number of infections by poverty percentile in the high and low population density sample, respectively. As expected, the number of cases in low density counties is substantially lower than in high density counties. For instance, at the 5th percentile of the county poverty grouping, the total number of cases on April 20, 2020 is over 50,000 in the high density group but only 1500 in the low density group.
Fig. 6.
SARS-CoV-2 Confirmed Infections in Counties with Low vs. High Population Density.
Notes: The sources of data are USAFacts and the Census. Low density regions are those counties below the median value of county level population density. We report the number of cumulative (infection) cases for March 11, March 23, April 7, April 20, and April 28, in 2020 for 20 county-groups ranked by poverty rate percentile for high and low density areas separately. The curves are fitted using a smoothing method based on local linear regressions as described in Appendix A.
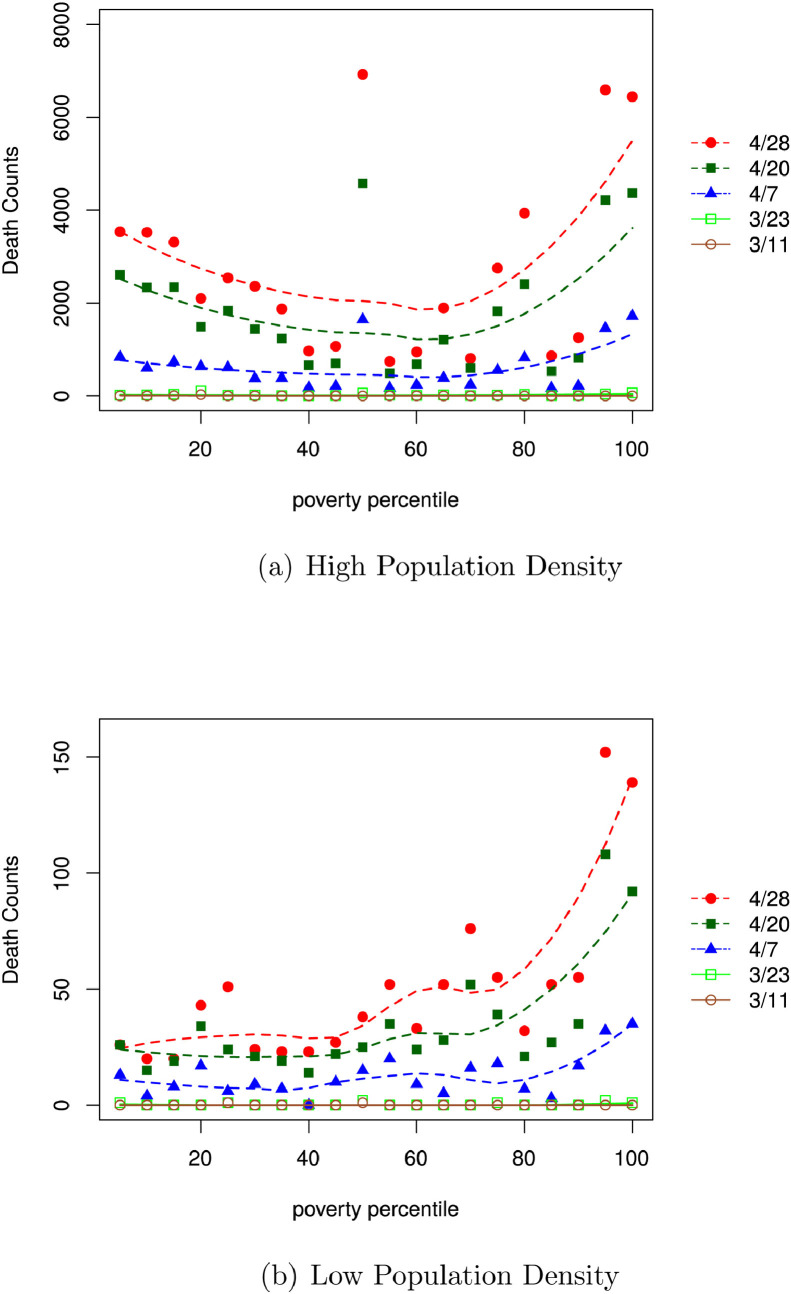
The U-shaped relationship between the county-groupings and cases prevails in high density counties as shown in Fig. 6(a). In contrast, the relationship between the county-groupings and coronavirus infections in low density counties does not follow a U-shape. It is relatively flat for counties with low poverty rates and strongly increases in counties with high poverty rates as depicted in Fig. 6(b). The patterns of COVID-19 related deaths in high and low density counties, shown in Fig. 7 (a) and (b) respectively, mirror the trends for infections as shown in the earlier figures except that COVID-19 related deaths seem to be even more associated with high poverty levels, especially in areas with low population density.
Fig. 7.
COVID-19 Related Deaths in Counties with Low vs. High Population Density.
Notes: The sources of data are USAFacts and the Census. Low density regions are those counties below the median value of county level population density. We then report the number of cumulative deaths due to COVID-19 for March 11, March 23, April 7, April 20, and April 28 in 2020 for 20 county-groups ranked by poverty rate percentile for high and low density areas separately. The curves are fitted using a smoothing method based on local linear regressions as described in Appendix A.
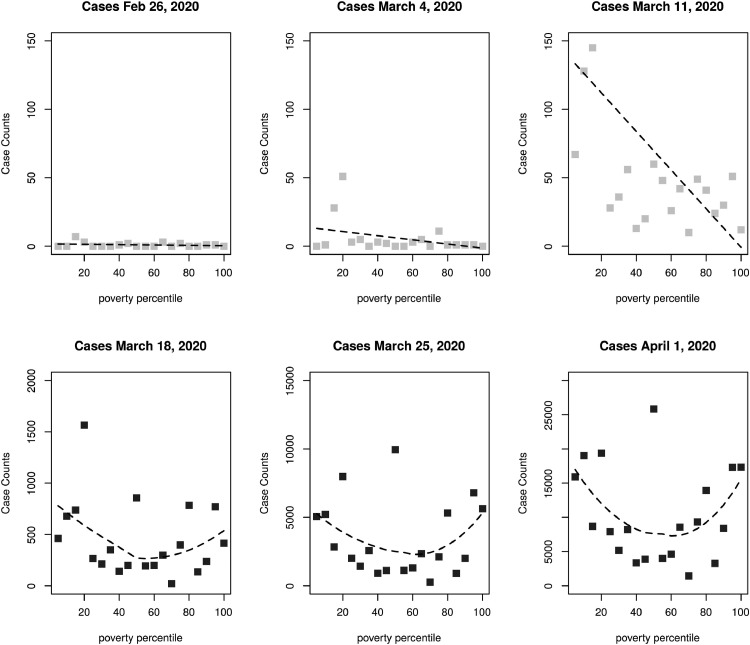
Rich to Poor Propagation Pattern. Coronavirus cases entered the US through international travel (airways and ships)—activities that are likely to be undertaken by richer individuals. To investigate this hypothesis, we first track the initial patterns in COVID-19 cases starting from the last week of February until March 11, 2020. The early relationship between poverty levels and coronavirus cases is shown in Fig. 8 . In these figures we track the number of cumulative (infection) cases from late February through early April. The downward sloping best-fit line on the rightmost figure suggests that in the initial phase of the pandemic infections in the US were more concentrated in richer counties, and the second row shows the emergence of the U-shaped pattern.
Fig. 8.
Coronavirus Infections and Poverty in the Early Months.
Notes: Data are from USAFacts. We report the number of cumulative (infection) cases for February 26, March 4, and March 11, 2020 in the top panel. The downward sloping best-fit line on the rightmost figure suggests that in the initial phase of the pandemic, infections in the US were more prevalent in richer counties. The bottom panel reports the number of cumulative (infection) cases for April 7, April 20, and April 28, 2020.
Two channels can potentially explain the dramatic propagation of infections in richer areas over a short period of time. First, at the very early stages, people may not have fully realized the seriousness of the virus.19 Since infections were initially concentrated in higher income groups, who are also more likely to be involved in social activities (through both employment and social activities), it may have been easier for the virus to spread in richer neighborhoods first. A comparison between Fig. 6(a) and (b) shows that the ratio between the number of cases in rich to poor counties is higher in densely populated counties compared to low density areas. The ratio of infections between rich and poor counties in areas with high population density is close to 1 but only around 0.4 in areas with low population density. In other words, having high income and residing in low-density communities could be indicative of a better ability to effectively self-isolate, compared to an equally wealthy person living in a densely populated area. Second, once the disease enters poor neighborhoods, it becomes very difficult to control the further spread of infections as poor households may neither have the resources to effectively self-isolate nor jobs that can easily be switched to working-from-home. It is therefore not surprising that the number of cases started to increase dramatically in poor neighborhoods in early April—eventually catching up with high income areas by April 28—as can be seen in the bottom row panels in Fig. 8.
3. Methods
Following California’s implementation of a stay-at-home mandate on March 19, 2020, almost all of the states implemented similar mandates within the next two weeks. However, as mentioned in Gupta et al. (2020b), the mandates are endogenously set, as mandates depend on current and the projection of future COVID-19 cases. In order to evaluate the impacts of social distancing on COVID-19 caseloads across rich and poor county groups, we propose a novel methodology that combines announcement dates of the stay-at-home mandate with arguably exogenous weather shocks. The poor county group comprises counties below the median of our county ranking according to the fraction of the population below the 2016 poverty level.
Our identification argument goes as follows. Severe weather patterns can reduce mobility. However, weather shocks can have a compounding effect during a period of stay-at-home mandate as the marginal cost of mobility is already high during the shutdown and extreme weather can increase it even more. Hence, detrimental weather patterns can increase the effectiveness of a mandate. We then measure the differential effect between counties with severe and counties with normal weather patterns under the mandate. In order to accomplish this, we propose to estimate three empirical specifications.
3.1. The impact of weather shocks and stay-at-home mandates on mobility
First, we estimate the effects of detrimental weather shocks coupled with the mandate on mobility across rich and poor county groups by using the following event-study specification:
| (1) |
where, mobility is the average distance traveled away from home in county and week as obtained from Safegraph. We use this distance measure as a proxy measure for social distancing. Variables and are indicators for the rich and poor county groups, respectively. We interact these indicators with indicator variable where is defined as weeks prior (negative signs) or past (positive signs) the initial announcement date of the mandate. The week before the mandate announcement is used as the omitted category. Next, poverty group and weeks away from the mandate are further interacted with an indicator variable for temperature shocks, . This variable equals one if the minimum temperature in county in week is below the 25th percentile of recorded temperatures in a specific month and state denoted as .20 In other words, captures weather shocks in county at time that are defined as unusually cold weather relative to weather pattern of the respective county’s state in a given month. Furthermore, a vector of NPIs including restaurant restrictions, closure of businesses, and declarations of emergency are accounted for in the specification by interacting the NPI vector with rich vs. poor county groups.21 The county level time invariant population density measure in 2019 is interacted with weekly indicators. The county groups (rich vs. poor counties) are also interacted with weekly dummies to absorb common time trends across rich and poor county groups, respectively. Variable represents the county fixed effects and captures unobserved time invariant heterogeneous relationships between area specific weather patterns and mobility outcomes. In order to capture the possible correlation within counties, the standard errors are clustered at the county level.
In specification 1, the coefficients of interest are and . They show the effect of the stay-at-home mandate coupled with arguably exogenous extreme weather shocks on mobility patterns during the onset of the pandemic for rich and poor county groups, respectively. The identification of and is obtained from the weather shock. After controlling for the interaction between weeks away from the mandate and poverty groupings (rich vs. poor county groups), county fixed effects and week fixed effects (also interacted with poverty groups), a county “” with a mandate can serve both as affected or unaffected unit, depending on the weather pattern of the county. Moreover, the event-study nature of the specification allows for the evaluation of the effects in the weeks before and after the mandate is announced. This provides a test for our claim that weather shocks constitute an additional cost during the lockdown period and decrease mobility more in counties with unusually cold weather. The event study setting is particularly important as it reveals plausibility regarding the validity of the identification (to an extent), which rests on the assumption that there are no preexisting differences in trends of the outcome across the treated and untreated units. As suggestive evidence regarding the validity of our assumption, the estimates of and should be close to zero for and decrease in magnitude for . However, these effects are likely to vary across rich and poor county groups.
3.2. The impact of weather shocks and stay-at-home mandates on COVID-19 cases
We next estimate the reduced form effects of effective social distancing on COVID-19 cases using the following specification:
| (2) |
which is similar to specification 1, except that the dependent variable is the logarithm of the number of new COVID-19 infection cases in county in week .22 Here, and track the reduced form effects of social distancing, through both legal (mandate) and natural (weather shock) forces, on the number of COVID-19 cases during the onset of pandemic for both rich and poor county groups, respectively.
3.3. Two-stage IV estimation of the impact of mobility on COVID-19 cases
The specification in Eq. (1) can also be used as the first stage of an IV estimation procedure, with the triple interaction between the county grouping based on income level, mandate week, and weather shocks as potential instrument for social distancing. The validity of using arguably exogenous weather shocks in the construction of this instrument is based on the assumption that extreme weather shocks affect the COVID-19 cases only through a reduction in human-to-human interaction but weather patterns do not biologically facilitate the transmission of the virus.
Although the timing of the mandate is endogenous as it is driven by the initial number and future projections of COVID-19 cases, the weather shocks are arguably exogenous in the model specifications. The interaction between the legal mandate and weather shocks can therefore be used as an instrument for mobility patterns—our proxy for social distancing—under the assumption (or exclusion restriction) that weather patterns influence COVID-19 cases through social distancing only but do not otherwise directly affect transmissions through, say a biological pathway of pathogens that is temperature dependent. This exclusion restriction would be violated if the transmission of the SARS-CoV-2 coronavirus is influenced by weather similar to other viruses (e.g., influenza, MERS, and SARS). Contrary to earlier beliefs that the spread of virus would subside over the summer months due to a rise in temperature, a growing body of literature has produced evidence suggesting very modest effects of weather on transmission of SARS-CoV-2 coronavirus (Baker, Yang, Vecchi, Metcalf, Grenfell, 2020, Carlson, Gomez, Bansal, Ryan, 2020, Schuit, Ratnesar-Shumate, Yolitz, Williams, Weaver, Green, Miller, Krause, Beck, Wood, et al., 2020, Weed, Foad, Xu, Rahmandad, Gupta, DiGennaro, Ghaffarzadegan, Amini, Jalali). The findings from these studies are consistent with the actual rise in COVID-19 cases throughout 2020, including the summer period. This further provides empirical evidence that weather has a very modest (if any) direct influence on the spread of COVID-19.23
There is no direct evidence to suggest that weather patterns significantly dictate COVID-19 spread (Carlson et al., 2020). Schuit et al. (2020) find that only 1 percent of the reduction in COVID-19 transmissions can be explained by environmental UV radiation and Baker et al. (2020) show that climate drives only modest changes in the size of the COVID-19 pandemic. Furthermore, Weed and Foad (2020) review recent studies that all find only an indirect impact of temperature on COVID-19, i.e. by keeping people indoors and/ or closer to each other. In light of this body of work, the IV estimates obtained can be gauged in basis of their magnitude as to whether it can be cohesively explained by weather directly influencing transmission of the virus.
Using specification 1 as the first stage, we use the predicted values of log of mobility in our second stage to investigate the direct relationship between social distancing on COVID-19 caseloads during the onset of the pandemic. Specifically, we estimate the following specification:
| (3) |
where all of the variables are similar to those in Eq. (2), except that are the predicted values of log of mobility from the first stage, as defined in Eq. (1). Parameters and again track the effect of social distancing on COVID-19 caseloads under the assumption that the exclusion restriction holds.
4. Results
4.1. The effects of social distancing on COVID-19 infections by income levels
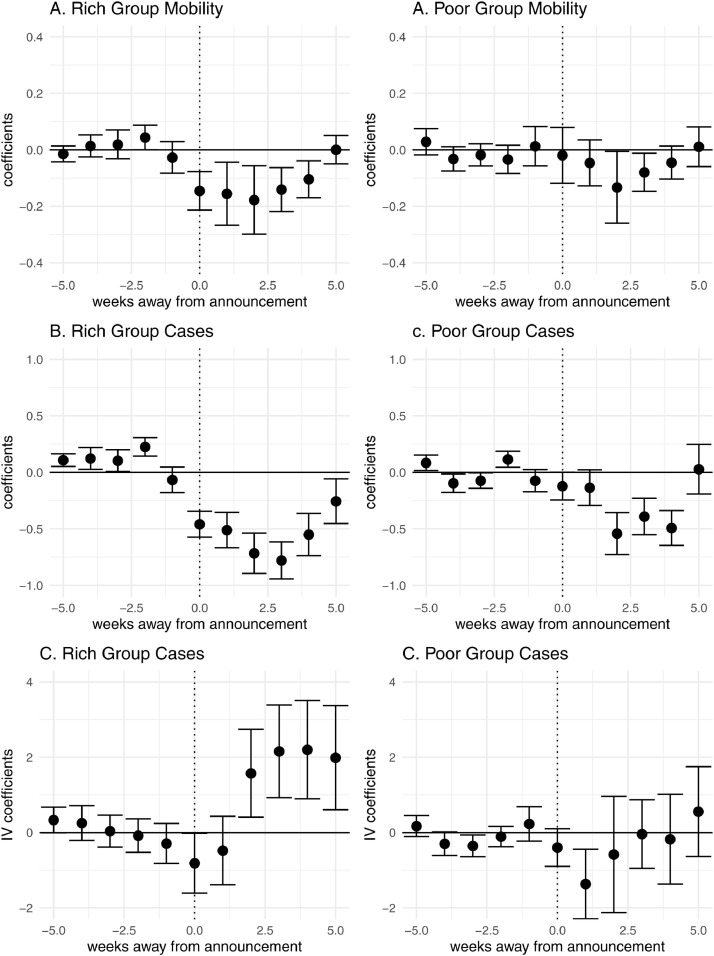
We next investigate the role of stay-at-home mandates on the number of COVID-19 cases across poverty groups. We first begin by highlighting the compounding effects of stay-at-home mandates and extreme weather patterns on reductions in mobility across rich and poor county groups by estimating specification 1 from Section 3. The interaction coefficients between the indicator variables representing the weeks before or after the announcement of the mandate, the rich vs. poor county groups, and the presence of extreme weather shocks are plotted in Panel A of Fig. 9 for high (left) and low (right) income county groups. The figure pertaining to the rich county group shows that the interaction coefficients are small and statistically indistinguishable from zero in the weeks prior to the announcement of the mandate. This is followed by a significant drop in the magnitude of the coefficient estimate in the announcement week itself. Thereafter the magnitude of the interaction coefficients pertaining to weeks following the announcement week remain negative for four subsequent weeks, before slowly rising back to zero in the fifth week from the announcement date. These results provide evidence of a compounding effect of the mandate and weather shocks in reducing mobility among high income counties in the immediate weeks following the announcement of a mandate. More specifically, weather shocks present more binding mobility constraints while a stay-at-home mandate is in effect as the marginal cost of mobility is already high during the shutdown and extreme weather increases it further. However, the results do suggest that mobility eventually reverts back to its initial level. The detailed results are presented in Table 3 . Column (6) shows coefficient estimates of our preferred specification which we plot in Panel A of Fig. 9. From Column (6) in Table 3 we can see that the interaction coefficient between the indicator representing the week of the mandate announcement (week 0), the rich county group, and a weather shock suggests that the mandate reduced mobility in the rich county group which also experienced a weather shock by = 13.5% on average in the week of announcement compared to counties that announced the mandate but did not experience a weather shock in that week.
Fig. 9.
The Effects of Weather Shocks and Mandates on Mobility and COVID-19.
Notes: Panel A uses log of mobility as the dependent variable, whereas Panels B and C use the log of weekly new cases. Panel A plots the coefficients on the interaction term between the county poverty group, weeks away from the mandate, and weather shock indicators as depicted in specification 1, where the figures on the left and right plot the estimates on and respectively. Panel B plots the reduced form effect of stay-at-home mandate coupled with the extreme weather shock by plotting the estimates of and after estimating Eq. (2) on the left and right side of Panel B, respectively. Panel C shows the IV results for rich (left) and poor (right) county groups by plotting the estimates of and in specification 3.
Table 3.
Mobility, Mandates and Weather Shocks (First Stage).
| Dependent variable: |
||||||
|---|---|---|---|---|---|---|
| log of Mobility |
log of Mobility |
|||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| -5 weeks Rich I(min ) | 0.017 | 0.017 | 0.014 | 0.013 | 0.014 | 0.014 |
| (0.014) | (0.014) | (0.014) | (0.014) | (0.014) | (0.014) | |
| -4 weeks Rich I(min ) | 0.006 | 0.006 | 0.009 | 0.010 | 0.013 | 0.014 |
| (0.020) | (0.020) | (0.020) | (0.020) | (0.020) | (0.020) | |
| -3 weeks Rich I(min ) | 0.026 | 0.026 | 0.023 | 0.023 | 0.019 | 0.019 |
| (0.026) | (0.026) | (0.026) | (0.026) | (0.026) | (0.026) | |
| -2 weeks Rich I(min ) | 0.040 | 0.040 | 0.043 | 0.043 | 0.044 | 0.044 |
| (0.022) | (0.022) | (0.022) | (0.022) | (0.022) | (0.022) | |
| -1 week Rich I(min ) | 0.023 | 0.023 | 0.025 | 0.025 | 0.028 | 0.027 |
| (0.028) | (0.028) | (0.028) | (0.029) | (0.029) | (0.029) | |
| 0 week Rich I(min ) | ||||||
| (0.034) | (0.034) | (0.034) | (0.035) | (0.035) | (0.035) | |
| 1 week Rich I(min ) | ||||||
| (0.057) | (0.057) | (0.057) | (0.057) | (0.057) | (0.057) | |
| 2 weeks Rich I(min ) | ||||||
| (0.061) | (0.061) | (0.061) | (0.061) | (0.062) | (0.062) | |
| 3 weeks Rich I(min ) | ||||||
| (0.040) | (0.040) | (0.040) | (0.040) | (0.040) | (0.040) | |
| 4 weeks Rich I(min ) | ||||||
| (0.034) | (0.034) | (0.034) | (0.034) | (0.033) | (0.033) | |
| 5 weeks Rich I(min ) | 0.005 | 0.005 | 0.0001 | 0.00000 | 0.005 | 0.001 |
| (0.026) | (0.026) | (0.026) | (0.026) | (0.026) | (0.026) | |
| -5 weeks Poor I(min ) | 0.029 | 0.029 | 0.030 | 0.030 | 0.031 | 0.029 |
| (0.024) | (0.024) | (0.024) | (0.024) | (0.024) | (0.024) | |
| -4 weeks Poor I(min ) | 0.033 | 0.032 | 0.032 | 0.032 | 0.031 | 0.032 |
| (0.022) | (0.022) | (0.022) | (0.022) | (0.022) | (0.022) | |
| -3 weeks Poor I(min ) | 0.019 | 0.019 | 0.019 | 0.016 | 0.015 | 0.018 |
| (0.020) | (0.020) | (0.020) | (0.020) | (0.020) | (0.020) | |
| -2 weeks Poor I(min ) | 0.037 | 0.034 | 0.033 | 0.030 | 0.030 | 0.034 |
| (0.025) | (0.025) | (0.025) | (0.025) | (0.026) | (0.026) | |
| -1 week Poor I(min ) | 0.018 | 0.014 | 0.014 | 0.016 | 0.017 | 0.013 |
| (0.036) | (0.036) | (0.036) | (0.036) | (0.036) | (0.036) | |
| 0 week Poor I(min ) | 0.029 | 0.027 | 0.024 | 0.028 | 0.027 | 0.019 |
| (0.050) | (0.050) | (0.050) | (0.050) | (0.051) | (0.050) | |
| 1 week Poor I(min ) | 0.059 | 0.061 | 0.060 | 0.059 | 0.058 | 0.046 |
| (0.042) | (0.042) | (0.042) | (0.042) | (0.042) | (0.042) | |
| 2 weeks Poor I(min ) | ||||||
| (0.065) | (0.065) | (0.065) | (0.065) | (0.065) | (0.065) | |
| 3 weeks Poor I(min ) | ||||||
| (0.034) | (0.034) | (0.034) | (0.034) | (0.035) | (0.034) | |
| 4 weeks Poor I(min ) | 0.045 | |||||
| (0.030) | (0.030) | (0.030) | (0.030) | (0.030) | (0.030) | |
| 5 weeks Poor I(min ) | 0.0004 | 0.001 | 0.001 | 0.002 | 0.002 | 0.011 |
| (0.036) | (0.036) | (0.036) | (0.036) | (0.036) | (0.036) | |
| emergency + emergency rich group | X | X | X | X | X | |
| restaurant + restaurant rich group | X | X | X | X | ||
| business + business Rich group | X | X | X | |||
| gathering + gathering Rich group | X | X | ||||
| density Week indicator | X | |||||
| F-Stat | 10.59 | 10.62 | 11.05 | 10.78 | 11.19 | 10.02 |
| Observations | 43,288 | 43,288 | 43,288 | 43,288 | 43,288 | 43,288 |
Notes:p0.1; p0.05; p0.01 All model specifications control for the county fixed effects, week fixed effects, logarithm of state specific COVID-19 testing, and the interaction terms between the rich county group and a) week fixed effects and b) the logarithm of state specific COVID-19 testing. Additionally, Column (2) controls for an indicator of whether a state of emergency was declared in county at time and the interaction of this indicator with rich county group. Similarly, Column (3) controls for an indicator representing restaurant ban and its interaction with rich county group. Columns (4) and (5) include indicators representing business closure and bans on large gathering along with their interactions with the rich county group. Next, Column (6) adds the interaction between week indicators and county level density. To account for within county correlation, standard errors are clustered at the county level.
In contrast to the rich county group, results pertaining to the poor county group suggest that mandates do not affect mobility to a similar extent. The interaction coefficients before the announcement week are indistinguishable from zero as is the interaction term indicating the announcement week itself. In the week following the announcement, we observe a drop in the magnitude of the coefficient estimate. However, the drop in mobility is transitory as it rises back up in the subsequent week. These differential patterns between high and low income groups are consistent with Blau et al. (2020a)’s discussion that the effects of NPIs during the “Great Lockdown” can vary across populace and is likely to be less-binding for essential workers who are less able to substitute onsite work with work performed at home. We also show precisely estimated zero effects for weeks prior to the mandate as a validation of the common trend assumption between treated and control units. Crucially, this differential impact cannot be detected in poorer counties, perhaps because essential workers—who on average tend to be less educated, have lower wages, and have a higher representation of men, disadvantaged minorities such as Hispanics, and immigrants—are more likely to reside in poorer counties (Blau et al., 2020b).
Panel B in Fig. 9 shows the reduced form results obtained from estimating specification 2, where the dependent variable is the log of the weekly number of new COVID-19 cases. It is reassuring to note that the pattern of the interaction coefficient estimates mimics the pattern of the interaction coefficients describing mobility patterns in Panel A. This is indicative of a strong positive relationship between mobility and new COVID-19 cases during the onset of the pandemic. While we do observe a reduction of COVID-19 cases in poor county groups in week 2, 3 and 4 following the announcement of the mandate, it is obvious that the reductions in cases are more pronounced in the rich county group. The fact that we did not observe significant reductions in mobility in low income areas while we do observe reductions in COVID-19 cases could be the result of spillover effects from reduced mobility in richer counties.
As previously described in Section 3, the results shown in Panel A of Fig. 9 are also the first stage estimates of the IV setup in expression 3. In all first stage specifications presented in Table 3 the F-statistics—based on a Wald test that compares the restricted to the unrestricted specification by using White’s standard errors to account for heteroskedasticity—are greater than 10 which is a widely used cut-off value to determine the strength of the instrument (Staiger and Stock, 1994). Next, using the predicted values of log-mobility from the first stage, we estimate the second IV stage described in specification 3 and plot the results in Panel C of Figure 9 for both rich (left) and poor (right) groups. The interaction coefficients are statistically indistinguishable from zero in the weeks before the mandate is announced for both rich and poor county groups. This is suggestive of no systematic relationship between predicted mobility and COVID-19 cases prior to the announcement of the mandate which is reassuring as the instrument itself is not binding during the period before the announcement week (as shown in Panel A). The interaction coefficient related to the announcement week itself drops in magnitude. However, there is a discontinuous spike in the coefficient estimate following the second week of the mandate announcement as the coefficients increase in magnitude, are positive, and statistically significant at the 5% levels. This depicts a direct positive relationship between mobility and COVID-19 caseloads. We provide detailed coefficient estimates in Table 4 . The coefficients for the rich county group during the second and third week following the announcement week in Column (6) of Table 4 suggest that a 1 percent increase in mobility leads to 1.6 and 2.1% reduction in the weekly number of cases, respectively.
Table 4.
Mobility, Mandates and Weather Shocks (IV Estimates).
| Dependent variable: |
||||||
|---|---|---|---|---|---|---|
| log of Cases |
log of Cases |
|||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| -5 weeks Rich I(min ) | 0.278 | 0.279 | 0.358 | 0.337 | 0.336 | 0.334 |
| (0.177) | (0.177) | (0.179) | (0.181) | (0.179) | (0.173) | |
| -4 weeks Rich I(min ) | 0.529 | 0.529 | 0.365 | 0.328 | 0.304 | 0.254 |
| (0.266) | (0.266) | (0.259) | (0.258) | (0.256) | (0.236) | |
| -3 weeks Rich I(min ) | 0.240 | 0.239 | 0.158 | 0.137 | 0.072 | 0.039 |
| (0.247) | (0.247) | (0.242) | (0.240) | (0.232) | (0.215) | |
| -2 weeks Rich I(min ) | 0.083 | 0.093 | 0.026 | 0.002 | 0.047 | 0.079 |
| (0.257) | (0.260) | (0.251) | (0.250) | (0.243) | (0.227) | |
| -1 week Rich I(min ) | 0.216 | 0.220 | 0.188 | 0.234 | 0.311 | 0.289 |
| (0.280) | (0.279) | (0.280) | (0.282) | (0.280) | (0.271) | |
| 0 week Rich I(min ) | ||||||
| (0.405) | (0.405) | (0.414) | (0.426) | (0.418) | (0.406) | |
| 1 week Rich I(min ) | 0.486 | 0.477 | ||||
| (0.485) | (0.485) | (0.480) | (0.479) | (0.483) | (0.464) | |
| 2 weeks Rich I(min ) | 1.436 | 1.436 | 1.656 | 1.627 | 1.787 | 1.574 |
| (0.637) | (0.637) | (0.643) | (0.638) | (0.626) | (0.595) | |
| 3 weeks Rich I(min ) | 2.040 | 2.039 | 2.316 | 2.288 | 2.374 | 2.159 |
| (0.671) | (0.671) | (0.678) | (0.673) | (0.663) | (0.628) | |
| 4 weeks Rich I(min ) | 1.844 | 1.844 | 2.234 | 2.221 | 2.417 | 2.202 |
| (0.697) | (0.697) | (0.694) | (0.694) | (0.700) | (0.666) | |
| 5 weeks Rich I(min ) | 1.675 | 1.675 | 1.970 | 1.978 | 2.245 | 1.990 |
| (0.729) | (0.729) | (0.738) | (0.738) | (0.748) | (0.705) | |
| -5 weeks Poor I(min ) | 0.190 | 0.190 | 0.214 | 0.210 | 0.249 | 0.171 |
| (0.152) | (0.152) | (0.151) | (0.151) | (0.152) | (0.143) | |
| -4 weeks Poor I(min ) | ||||||
| (0.212) | (0.212) | (0.215) | (0.215) | (0.211) | (0.160) | |
| -3 weeks Poor I(min ) | ||||||
| (0.185) | (0.185) | (0.190) | (0.189) | (0.185) | (0.147) | |
| -2 weeks Poor I(min ) | 0.178 | 0.186 | 0.199 | 0.198 | 0.210 | 0.104 |
| (0.139) | (0.144) | (0.143) | (0.143) | (0.143) | (0.137) | |
| -1 week Poor I(min ) | 0.173 | 0.174 | 0.189 | 0.200 | 0.185 | 0.230 |
| (0.224) | (0.225) | (0.227) | (0.233) | (0.235) | (0.232) | |
| 0 week Poor I(min ) | 0.405 | 0.405 | 0.397 | |||
| (0.263) | (0.263) | (0.261) | (0.262) | (0.264) | (0.255) | |
| 1 week Poor I(min ) | ||||||
| (0.460) | (0.461) | (0.453) | (0.453) | (0.465) | (0.471) | |
| 2 weeks Poor I(min ) | 0.738 | 0.738 | 0.734 | 0.740 | 0.727 | 0.582 |
| (0.859) | (0.859) | (0.857) | (0.859) | (0.872) | (0.787) | |
| 3 weeks Poor I(min ) | 0.210 | 0.210 | 0.201 | 0.204 | 0.196 | 0.039 |
| (0.517) | (0.517) | (0.515) | (0.516) | (0.520) | (0.464) | |
| 4 weeks Poor I(min ) | 0.410 | 0.411 | 0.405 | 0.412 | 0.421 | 0.177 |
| (0.664) | (0.664) | (0.663) | (0.664) | (0.672) | (0.608) | |
| 5 weeks Poor I(min ) | 0.302 | 0.302 | 0.311 | 0.305 | 0.353 | 0.558 |
| (0.766) | (0.766) | (0.761) | (0.762) | (0.752) | (0.609) | |
| emergency + emergency rich group | X | X | X | X | X | |
| restaurant + restaurant rich group | X | X | X | X | ||
| business + business Rich group | X | X | X | |||
| gathering + gathering Rich group | X | X | ||||
| density Week indicator | X | |||||
| Observations | 43,288 | 43,288 | 43,288 | 43,288 | 43,288 | 43,288 |
Notes:p0.1; p0.05; p0.01 All model specifications control for the county fixed effects, week fixed effects, logarithm of state specific COVID-19 testing, and the interaction terms between the rich county group and a) week fixed effects and b) the logarithm of state specific COVID-19 testing. Additionally, Column (2) controls for an indicator of whether a state of emergency was declared in county at time and the interaction of this indicator with rich county group. Similarly, Column (3) controls for an indicator representing restaurant ban and its interaction with rich county group. Columns (4) and (5) include indicators representing business closure and bans on large gathering along with their interactions with the rich county group. Next, Column (6) adds the interaction between week indicators and county level density. To account for within county correlation, standard errors are clustered at the county level.
For the validity of the IV estimate, weather shocks— defined as extreme cold temperatures—should not directly affect the transmission of COVID-19. Genetically, the structure of SARS-COV2 is similar to other coronaviruses, with four genes encoding proteins S (spike), E (envelope), M (membrane), and N (nucleocapsid). Theoretically, the lipid bilayer enveloping the virus is more likely to be destroyed when exposed to dry heat (Neuman et al., 2011). Hence, it was initially hypothesized that cold temperatures favor the survival of the virus and the infections would decrease over the summer months (at least as circulated in media, although experts disagreed).24
It should be noted that if cold weather shocks increase the likelihood of the survival of SARS-COV2 viruses and therefore infections, the IV estimates in our setting will be biased downwards. However, contrary to initial beliefs, a growing body of literature suggests that weather patterns are not a critical direct driver for COVID-19 infections compared to other pathogens such as influenza, MERS, or SARS. (e.g., Baker, Yang, Vecchi, Metcalf, Grenfell, 2020, Carlson, Gomez, Bansal, Ryan, 2020, Schuit, Ratnesar-Shumate, Yolitz, Williams, Weaver, Green, Miller, Krause, Beck, Wood, et al., 2020, Weed, Foad, Xu, Rahmandad, Gupta, DiGennaro, Ghaffarzadegan, Amini, Jalali). This is also evident from increases in the number of COVID-19 cases throughout 2020, including the summer months. Moreover, people’s perception regarding the impacts of weather on the transmission of COVID-19 can further lead to changes in behavior, which will invalidate the single-channel mechanism proposed in the first stage. Using twitter posts collected between January 23 and June 22, 2020, Gupta et al. (2020a) show that people are in general uncertain about the potential impact of weather on COVID-19. In light of these findings, the magnitudes of our IV estimates are too large in order to be cohesively explainable by weather directly influencing the transmission of the virus.
In order to give the reader a sense of the magnitude of the IV estimates, we conduct a back-of-the-envelope calculation of the effects of the stay-at-home mandate on COVID-19 cases through decreases in social interactions. Using the percent drop in mobility following the announcement of a mandate as proxy measure for social distancing, we estimate that stay-at-home mandates helped reduce the number of COVID-19 infections in high income counties by 341,737 cases in the first five weeks following the mandate announcement. In order to estimate this effect, we proceed as follows. First, the average decreases in mobility in the first five weeks following the announcement of a mandate are percent, respectively. Using the average number of cases in high income counties in the first five weeks after the mandate was announced combined with the IV coefficients in Table 4, we calculate what the number of cases would have been without any stay-at-home mandates in place. We then multiply this vector with the weekly percent reduction in mobility and the total number of rich counties (1529). Adding up the effects over all five weeks results in 341,737 fewer cases. According to the cumulative number of cases reported in high income counties by April 27 (557,349), our estimates suggest that 38% of reductions in COVID-19 infections in high income communities can be attributed to social distancing (or reduced mobility) due to the stay-at-home mandate. In comparison, Dave et al. (2020) find that the stay-at-home mandate reduced the cumulative COVID-19 cases by 44% in the first three weeks following the implementation of the mandate.25
4.2. Robustness exercises
We conduct several robustness checks to validate our findings. First, we replicate our descriptive findings from Figs. 4 and 5 which were based on 20 county-groups and use 25 county-groups instead. The results are very similar and the U-shaped relationship between COVID-19 cases and poverty percentile by county-group is maintained. Overall, our result are robust to alternative county groupings.26
Second, given the very obvious outlier observations from the median county-group which contains counties from the state of New York that we described earlier in Section 2.3, we next repeat our descriptive analysis without county observations from New York. In addition, we re-estimate specification (1), (2), and 3 using the reduced sample in order to check whether our results are driven by the dramatic surge in COVID-19 cases in New York during the onset of the pandemic. Overall, the descriptive analysis as well as the estimation results of the parametric models are robust to excluding observations from the state of New York. The U-shaped relationship between COVID-19 cases and related deaths are both maintained in the reduced sample. In addition, the quantitative results from the regression analysis can be replicated without observations from New York and the quantitative results are very similar to the estimation results based on the full sample.27
Third, we allow for differential growth in the number of cases over time within a given state and control for the interaction between state and week fixed effects. We again find that our main results are robust with respect to these specification changes.28
Finally, the true number of COVID-19 infections could be much higher than the reported infections due to measurement error as recently discussed in Manski and Molinari (2020). For the purpose of our analysis we maintain that any possible measurement error in reported COVID-19 cases is unlikely to be systematically correlated with weather patterns. While the estimated specifications do account for time variant testing at the state level, due to data limitation we are unable to control for across county variation in testing within a state over time. As with any study of COVID-19, we acknowledge the caveats presented by inaccurate reporting of infections.
5. Conclusion
Reviewing evidence of the 2020 outbreak of COVID-19 in the United States, we observe a strong poverty gradient in both infections and deaths in addition to important interactions between poverty and population density. Overall infections increase at both tails of the distribution of counties according to their poverty rates, creating a U-shaped curve. A similar pattern is observed for confirmed deaths due to COVID-19 with an overall higher death rate among counties with higher poverty levels. These rates decrease for counties with more moderate poverty levels and increase again for counties with very low poverty levels. Furthermore, distinguishing between areas with low and high population density, we demonstrate that the U-shaped pattern prevails in high density counties but disappears in low density areas. In low population density areas, the infection rates in counties with high poverty rates dwarf the rates in counties with lower poverty rates, essentially creating an exponential curve of COVID-19 cases when counties are lined up according to their poverty rate. Along the same lines we see that while death rates are higher across the board in high density counties, the impact of poverty is observed more more clearly in low density areas.
Figs. 4 –7 raise an interesting question. Why does the overall relationship between coronavirus events and local area socioeconomic status—as defined by the poverty levels—follow a U-shaped pattern in high density areas but not in low density areas? The U-shaped pattern contradicts the well-established positive relationship between income and health outcomes.29 One possible explanation for the observed difference in the high and low density samples could be due to disproportionately more testing for infections in rich counties which could result in more identified cases in richer county-groupings. This could explain why we observe seemingly higher infection rates as well as COVID-19 death rates in richer counties contrary to what the income gradient literature would predict for other health outcomes. This possibility has been highlighted by the media, suggesting that testing for coronavirus infections is a function of income inequality and as such mirrors the overall trend in health disparity by income.30 However, in a recent study focused on New York City, Schmitt-Grohé et al. (2020) find that the spread in the number of tests administered as of April 2, 2020 is evenly distributed across income levels. More importantly, another explanation for the difference in the pattern between high and low density counties could be that high income individuals can only self-isolate more effectively than low income individuals when they live in thinly populated areas, whereas in high density counties, richer individuals may not be able to benefit as strongly from this logistical advantage due to necessary day-to-day interactions.
Along these lines, we find indications of the spread in COVID-19 infections from high income to low income communities. Evidence suggests that richer counties in densely populated areas are the first to be infected; residents of the nearby lower income areas provide services to the more economically active, resulting in their infection. Once the disease enters poor neighborhoods, the number of cases starts to increase dramatically as economic disadvantage exacerbates extant health, economic, and information disparities. At this point it becomes very difficult to control the further spread of the disease as poor households do not have the resources to effectively self-isolate.
This is our third main finding: the relative effectiveness of social distancing differs by income group. By using arguably exogenous weather shocks along with stay-at-home mandates, we find compounding effects of legal (mandate) and natural forces in curbing mobility among high income counties following the announcement of a mandate. However, such effects are not present among low income counties. Furthermore, our IV estimates indicate that homogeneously implemented NPIs are not very effective in curbing COVID-19 cases in low income counties. Overall, our findings support the claim that although NPIs such as the stay-at-home mandate are useful in curbing cases in richer areas, the same NPIs are not as successful in promoting social distancing in relatively poorer areas.
The IV finding—policy measures taken to promote social distancing affect high income communities more than low income areas—is consistent with the pattern of spread in infections documented in our descriptive analysis. Initially, infections were higher in high income communities but lockdowns successfully slowed down the infection growth rate. However, as infections also started spreading in low income communities, the lockdown was less successful in effectively promoting social distancing in these areas, which subsequently led to further increases in infections in poorer communities. Overall, our results provide insights for the design of future prevention strategies against COVID-19 (or similar infectious diseases) by suggesting that, especially for low income areas, new policies need to be developed to prevent the spread of infectious diseases.
Although we account for testing at the state level by using data from The Covid Tracking Project in many specifications, we caution that lack of quality data on testing at the county level may underestimate the number of infections (Manski and Molinari, 2020). This imposes a limitation on the findings of this study, particularly if testing is correlated with socioeconomic characteristics. Presuming that the cause of death is accurately classified, a U-shaped curve portraying COVID-19 deaths is consistent with a U-shaped curve for infections. This, to some extent, helps reduce our concern about possible differences in testing across localities. Nevertheless, we emphasize the need for adequate testing data at the local level, which can further benefit studies in this sector.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Funding
The study was not supported by any funding source.
Footnotes
We would like to thank Victoria from Weather Underground for helping us with data. All remaining errors are ours. This paper was previously circulated with the title: “Coronavirus Infections and Deaths by Poverty Status: Time Trends and Patterns”
Saffer (2008) shows that social interaction is not only a function of its price, but also the prices of complements and substitutes as well as income. He further shows that many forms of social interactions increase with income.
Becken and Pant (2019), for instance, shows that the richest half of the world is responsible for 90 percent of emissions from air travel.
See a report in USA Today from March 3, 2020: https://www.usatoday.com/story/news/nation/2020/03/30 and Table 1 for a summary of announcement dates of stay-at-home mandates in all 50 states.
A detailed discussion of this issue is provided Section 4.1.
Gupta et al. (2020c) provide a short review of the literature addressing the early phase of the pandemic.
In related studies both Fowler et al. (2020) and Courtemanche et al. (2020) use difference-in-differences designs to show that the stay-at-home mandate helped flatten the growth curve of new COVID-19 infections.
Appendices A contain more detailed results about the curve fitting method used to track the COVID-19 patterns.
Data from USAFacts is essentially identical to data released from the Johns Hopkins University Center for Systems Science and Engineering of the Whiting School of Engineering which is freely accessible at: https://github.com/CSSEGISandData/ .
The link to the SAIPE website where poverty estimates can be found is https://www.census.gov/data/datasets/2016/demo/saipe/2016-state-and-county.html .
The link to the website is https://data.nber.org/data/seer_u.s._county_population_data.html.
There are 3143 counties or county-equivalents including DC in the US. We dropped 51 counties due to missing weather or mobility data.
The data is available on this website. https://covidtracking.com/api.
This approach is similar to the method in Currie and Schwandt (2016) who analyze county level trends in mortality by poverty levels.
We provide a detailed description of the curve fitting procedure in Appendix A.
One observation point that does not align well with the U-shaped curve is the observation pertaining to the 50th percentile on the distribution of county-group poverty rates. This particular county-group includes Queens county of New York City which was especially hard hit by COVID-19 at the onset of the pandemic.
Several media outlets as well as the Trump administration have downplayed the danger of the virus, especially in the early days of the outbreak. Compare https://www.mediamatters.org/coronavirus-covid-19/fox-news-downplaying-risk-coronavirus-could-get-people-killed and https://www.vox.com/2020/6/8/21242003/trump-failed-coronavirus-response .
Using other state temperature percentiles as cutoffs, such as the median, does not change the estimates but weakens the F-statistic. Also, in order to account for the seasonal rise in temperature over the months in the sample, we use also estimate a specification with an absolute cut-off point, given by the 25th percentile of recorded temperatures in all months. The findings from these alternative estimates yield similar results. These results are not presented but are available upon request.
Restaurant restrictions were imposed to reduce mobility and contain the spread of COVID-19. Restaurant restrictions were implemented widely. A total of 49 states have imposed such restrictions by April 7, 2020. Moreover, closure of businesses imply a state’s decision to close all non-essential businesses when a partial closing was already in place. In this sense, closure of businesses are more restrictive than restaurant restrictions.
Before taking the log, we add 1 to the actual number of cases. We test the robustness of this method by adding smaller values than one. The results do not change. These alternative results are available upon request.
Nevertheless, it can be argued that if low temperature and dry air did expedite the spread of COVID-19, our results obtained from using unusually cold temperatures would likely be downward biased.
For a March 2020 newspaper article discussing the effects of Summer temperature on the spread of COVID-19 infections see: https://www.theguardian.com/us-news/2020/mar/30/is-coronavirus-seasonal-summer .
We caution that our back-of-the envelope calculation is based on the local average treatment effect (LATE) of the mandate and is therefore driven by individuals affected by weather shocks during the period following the announcement of the mandate.
Detailed results are available in Appendix B.
Detailed results are available in Appendix C.
These results are not presented but are available upon request.
For a review of this literature see Wolfe et al. (2012). In a more recent study, Currie and Schwandt (2016) show that the income gradient is well defined at local levels using life expectancy across counties. Shrestha (2019) shows a similar pattern when analyzing the relationship between infant birth weight and the prevalence of low birth weight across counties grouped by poverty levels.
See New York Times article from March 18, 2020: https://www.nytimes.com/2020/03/18/us/coronavirus-testing-elite.html.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jebo.2020.12.019.
Appendix A. Supplementary materials
Supplementary Raw Research Data. This is open data under the CC BY license http://creativecommons.org/licenses/by/4.0/
References
- Andersen M., Maclean J.C., Pesko M.F., Simon K.I. NBER Working Paper No. 27138. 2020. Effect of a Federal Paid Sick Leave Mandate on Working and Staying at Home: Evidence from Cellular Device Data. [DOI] [Google Scholar]
- Atkinson T., Dolmas J., Koch C., Koenig E., Mertens K., Murphy A., Yi K.-M. FED Dallas Working Paper 2014. 2020. Social Distancing Following the SARS-Cov-2 Outbreak. [DOI] [Google Scholar]
- Baker R.E., Yang W., Vecchi G.A., Metcalf C.J.E., Grenfell B.T. Susceptible supply limits the role of climate in the early SARS-cov-2 pandemic. Science. 2020 doi: 10.1126/science.abc2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becken S., Pant P. Technical Report. Amadeus; 2019. Airline Initiatives to Reduce Climate Impact. [Google Scholar]
- Blau F.D., Koebe J., Meyerhofer P.A. Econofact. 2020. Essential and frontline workers in the covid-19 crisis. [Google Scholar]
- Blau F.D., Koebe J., Meyerhofer P.A. NBER Working Paper No 27791. 2020. Who are the Essential and Frontline Workers? [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown C.S., Ravallion M. NBER Working Paper No. 27549. 2020. Inequality and the Coronavirus: Socioeconomic Covariates of Behavioral Responses and Viral Outcomes Across US Counties. [DOI] [Google Scholar]
- Brzezinski A., Deiana G., Kecht V., Dijcke D.V. The COVID-19 pandemic: government versus community action across the united states. COVID Econ. 2020;7:115–156. [Google Scholar]
- Carlson C.J., Gomez A.C., Bansal S., Ryan S.J. Misconceptions about weather and seasonality must not misguide COVID-19 response. Nat. Commun. 2020;11(1):1–4. doi: 10.1038/s41467-020-18150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S., Pierson E., Koh P.W., Gerardin J., Redbird B., Grusky D., Leskovec J. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2020 doi: 10.1038/s41586-020-2923-3. [DOI] [PubMed] [Google Scholar]
- Chen, Y., Feng, Y., Yan, C., Zhang, X., Gao, C., 2020. Modeling COVID-19 growing trends to reveal the differences in the effectiveness of non-pharmaceutical interventions among countries in the world. medRxiv.
- Coibion O., Gorodnichenko Y., Weber M. Technical Report. National Bureau of Economic Research; 2020. Labor Markets During the COVID-19 Crisis: aPreliminary View. [Google Scholar]
- Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff. 2020 doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- Currie J., Schwandt H. Mortality inequality: the good news from a county-level approach. J. Econ. Perspect. 2016;30(2):29–52. doi: 10.1257/jep.30.2.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dave D.M., Friedson A.I., Matsuzawa K., Sabia J.J. Technical Report. IZA Discussion Papers; 2020. When Do Shelter-In-Place Orders Fight COVID-19 Best? Policy Heterogeneity across States and Adoption Time. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler, J. H., Hill, S. J., Obradovich, N., Levin, R., 2020. The effect of stay-at-home orders on COVID-19 cases and fatalities in the united states. medRxiv10.1101/2020.04.13.20063628.
- Friedson A.I., McNichols D., Sabia J.J., Dave D. Technical Report. National Bureau of Economic Research; 2020. Did Californias Shelter-in-Place Order Work? Early Coronavirus-Related Public Health Effects. [Google Scholar]
- Gupta M., Bansal A., Jain B., Rochelle J., Oak A., Jalali M.S. Whether the weather will help us weather the COVID-19 pandemic: using machine learning to measure twitter users perceptions. Int. J. Med. Inform. 2020:104340. doi: 10.1016/j.ijmedinf.2020.104340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Nguyen T.D., Rojas F.L., Raman S., Lee B., Bento A., Simon K.I., Wing C. NBER Working Paper No. 27027. 2020. Tracking Public and Private Response to the COVID-19 Epidemic: Evidence from State and Local Government Actions. [DOI] [Google Scholar]
- Gupta S., Simon K.I., Wing C. NBER Working Paper No. 28139. 2020. Mandated and Voluntary Social Distancing During the COVID-19 Epidemic: a Review. [DOI] [Google Scholar]
- Kahn L.B., Lange F., Wiczer D.G. NBER Working Paper No. 27061. 2020. Labor Demand in the Time of COVID-19: Evidence from Vacancy Postings and UI Claims. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapoor R., Rho H.A., Sangha K., Sharma B., Shenoy A., Xu G. God is in the rain: the impact of rainfall-induced early social distancing on COVID-19 outbreaks. COVID Econ. 2020;24:76–110. doi: 10.1016/j.jhealeco.2021.102575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong E., Prinz D. The impact of shutdown policies on unemployment during a pandemic. COVID Econ. 2020;17:24–72. [Google Scholar]
- Manski C.F., Molinari F. Estimating the COVID-19 infection rate: anatomy of an inference problem. J. Econ. 2020 doi: 10.1016/j.jeconom.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervosh, S., Lu, D., Swales, V., 2020. See which states and cities have told residents to stay at home.
- Mongey S., Pilossoph L., Weinberg A. University of Chicago, Becker Friedman Institute for Economics Working Paper. 2020. Which Workers Bear the Burden of Social Distancing Policies? [Google Scholar]
- Neuman B.W., Kiss G., Kunding A.H., Bhella D., Baksh M.F., Connelly S., Droese B., Klaus J.P., Makino S., Sawicki S.G., et al. A structural analysis of m protein in coronavirus assembly and morphology. J. Struct. Biol. 2011;174(1):11–22. doi: 10.1016/j.jsb.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz, J. L., Hauck, G., 2020. Coronavirus in the us: How all 50 states are responding and why eight still refuse to issue stay-at-home orders.
- Pan, W., Tyrovolas, S., Vazquez, I. G., Raj, R., Fernandez, D., Zaitchik, B., Lantos, P., Woods, C. W., 2020. Covid-19: effectiveness of non-pharmaceutical interventions in the United States before phased removal of social distancing protections varies by region. medRxiv.
- Qiu Y., Chen X., Shi W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in china. J. Popul. Econ. 2020:1. doi: 10.1007/s00148-020-00778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffer H. The demand for social interaction. J. Socio-Econ. 2008;37(3):1047–1060. [Google Scholar]
- Sandstrom G.M., Dunn E.W. Social interactions and well-being: the surprising power of weak ties. Personal. Soc. Psychol. Bull. 2014;40(7):910–922. doi: 10.1177/0146167214529799. [DOI] [PubMed] [Google Scholar]
- Santerre R., Neun S. South-Western Cengage Learning; Mason (Ohio): 2010. Health Economics : Theories, Insights, and Industry Studies. [Google Scholar]
- Schmitt-Grohé S., Teoh K., Uribe M. Technical Report. National Bureau of Economic Research; 2020. Covid-19: Testing Inequality in New York City. [Google Scholar]
- Schuit M., Ratnesar-Shumate S., Yolitz J., Williams G., Weaver W., Green B., Miller D., Krause M., Beck K., Wood S., et al. Airborne SARS-COV-2 is rapidly inactivated by simulated sunlight. J. Infect. Dis. 2020 doi: 10.1093/infdis/jiaa334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha V. Towson University, Economics Working Paper Series. 2019. Maternal Education and Infant Health Gradient: New Answers to Old Questions. [DOI] [PubMed] [Google Scholar]
- Staiger D., Stock J.H. Technical Report. National Bureau of Economic Research; 1994. Instrumental Variables Regression With Weak Instruments. [Google Scholar]
- Weed, M., Foad, A., 2020. Rapid scoping review of evidence of outdoor transmission of COVID-19. medRxiv.
- Wolfe B., Evans W., Seaman T. Russell Sage Foundation; New York: 2012. The Biological Consequences of Economic Inequalities. [Google Scholar]
- Xu, R., Rahmandad, H., Gupta, M., DiGennaro, C., Ghaffarzadegan, N., Amini, H., Jalali, M. S., 2020. The modest impact of weather and air pollution on covid-19 transmission. medRxiv. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Raw Research Data. This is open data under the CC BY license http://creativecommons.org/licenses/by/4.0/