Dear Editor,
In December 2019, the first cases of COVID-19 were reported in Wuhan, China and it rapidly spread around the world to more than 188 countries. Among these, Latin American countries such as Brazil, Peru, Colombia, Mexico and Argentina are part of the ten countries with more COVID-19 confirmed cases, placing Peru in the first place with the highest number of deaths registered per 100 000 inhabitants due to this disease (1).
The Ministry of Health of Peru(MINSA, by its initials in Spanish) confirmed the first COVID-19 case on March 6, 2020 and registered 657 129 cases and 29 068 deaths until August 31, 2020 (2). Comorbidities such as high blood pressure, diabetes mellitus, cardiovascular diseases, and cancer have been described as severity and mortality predictors for COVID-19, predominantly affecting older adults (3). In addition, with the increase of older adults’ population in low-and middle-income countries and the higher prevalence of chronic diseases in this age group (4), they require better monitoring in health systems. However, health systems have collapsed during the context of the COVID-19 pandemic, generating negative consequences. For this reason, it is relevant to assess mortality in older adults during the COVID-19 pandemic in Peru.
We carried out a secondary analysis of the National Computer System of Deaths registry(SINADEF, by its initials in Spanish), obtained from the National Repository of Health Information(REUNIS, by its initials in Spanish), an open-access Peruvian system (5). We performed data analysis and graphs using the Microsoft Excel program. Excess deaths were defined by the difference between observed deaths and expected deaths according to previous years before the COVID-19 pandemic. We calculated the expected mortality(EM) as the average of the registered deaths in the SINADEF from January to August 2018 and 2019 (6). We included these years because, during this period, there was greater coverage of the virtual death registry. We only analyzed the non-violent deaths reported.
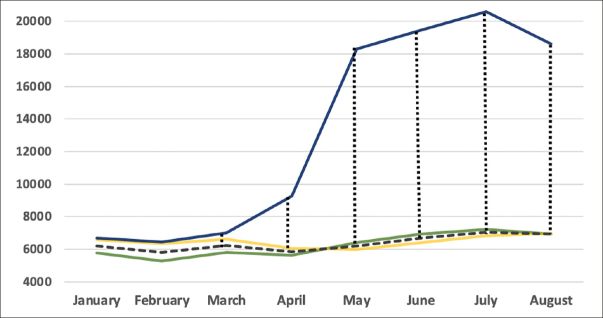
The older adult’s death excess from March to August in 2020 was 54337 and 54411 deaths compared to 2018 and 2019, respectively. The older adults’ death represented 70.2%, 71.8% and 73.1% of the total deaths from March to August in 2018, 2019 and 2020, respectively. Furthermore, the excess of deaths in this group during 2020 was 802(13%) in March, 3426(59%) in April, 12121(196%) in May, 12795(191%) in June, 13559(193%) in July and 11672(168%) in August (Figure 1).
Figure 1.
Death excess in older adults (60 years or above) during COVID-19 pandemic in Peru
The results showed that there was an increase in older adults’ mortality during the COVID-19 pandemic period compared to previous years. We have estimated a death excess of 139.7% regardless of the cause of death reported. However, deaths attributed to COVID-19 in this age group represented only one-fifth of deaths registered in older adults’ during this period (2). This circumstance would explain the approach to other possible causes that justify this excess of death.
Physiological changes associated with aging, a decrease in immune system response, the presence of disability, chronic diseases and polypharmacy are characteristic conditions of frail older adults. Thus, they require periodic control of their chronic diseases, to receive their medication and prevent complications (7). However, in Peru, due to the state of emergency, the health services restricted their attention only to emergencies, suspending the outpatient consulting service. Consequently, complications of uncontrolled chronic diseases could be one of the leading causes of this mortality increase in older adults.
Similarly, health services narrowed the COVID-19 attention in this age group and given the lack of intermediate and intensive care beds, the younger population without comorbidities and a greater probability of recovery was prioritized (7). In addition, the absence of outpatient services and the health services collapse could have led to an increase in self-medication and over-medication in older adults (7). These practices could have been harmful considering their comorbidities and the necessity for more specialized attention, leading to more complications and deaths in their homes or nursing homes.
It is necessary to improve health care services for older adults in Peru. The Peruvian health system is currently collapsed, fragmented, and under-resourced (8). Despite the increase in universal health coverage, there are only approximately 0.2 intensive care units(ICU) beds per 100 000 inhabitants (9). However, the health budget for 2019 was 2.3% of the Gross National Product and only less than half was executed (10). The national budget designated to provide home health care services for this population should be strengthened. In addition, follow-up programs for patients with chronic diseases should be prioritized to supply them with their medication and prevent complications. The COVID-19 pandemic has evidenced a lack of resources and health care services for older adults, a vulnerable population that requires more attention and effort to maintain healthy aging.
Footnotes
Funding
The study was self-funded.
Conflict of interests
The authors disclose no conflict of interest.
References
- 1.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–4. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministerio de Salud. Sala Situacional COVID-19 Perú. MINSA: Lima, Perú. 2020 https://covid19.minsa.gob.pe/sala_situacional.asp. Accessed 3 October 2020.
- 3.Potere N, Valeriani E, Candeloro M, Tana M, Porreca E, Abbate A, et al. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Critical care. 2020;24(1):1–12. doi: 10.1186/s13054-020-03022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melorose J, Perroy R, Careas S. World population prospects. United Nations. 2015;1(6042):587–92. [Google Scholar]
- 5.Ministerio de Salud. Sistema Informático Nacional de Defunciones — SINADEF. 2020. https://www.minsa.gob.pe/defunciones. Accessed 3 October 2020.
- 6.Wu J, McCann A, Katz J, Peltier E. 60,000 Missing Deaths: Tracking the True Toll of the Coronavirus Outbreak. New York Times. 2020.
- 7.Lloyd-Sherlock P, Ebrahim S, Geffen L, McKee M. Bearing the brunt of covid-19: older people in low and middle income countries. BMJ. 2020;368:m1052. doi: 10.1136/bmj.m1052. [DOI] [PubMed] [Google Scholar]
- 8.Alcalde-Rabanal JE, Lazo-González O, Nigenda G. Sistema de salud de Perú. Salud Públ Méx. 2011;53:s243–s54. [PubMed] [Google Scholar]
- 9.Almeida F. Exploring the impact of COVID-19 on the sustainability of health critical care systems in South America. Int J Health Policy Manag. 2020. [DOI] [PMC free article] [PubMed]
- 10.García E. Comex: Perú gasta en salud por debajo del promedio en América Latina. Diario Gestión. 2019. https://gestion.pe/economia/comex-peru-gasta-salud-debajo-promedioamerica-latina-268172. 2019. Accessed 3 October 2020.