Abstract
Aim
Polypharmacy in elderly people is a social issue and has been reported to cause not only drug adverse events, but also falls, dysfunction and cognitive decline. Those events may trigger prolonged length of hospitalization. Therefore, the aim of this study was to investigate whether polypharmacy has a prolonging effect on hospitalization.
Methods
The study subjects were 584 patients in a university hospital in Japan who had been admitted for hepatectomy, pancreaticoduodenectomy, gastrectomy or colectomy, and to whom clinical pathways had been applied. In this study, polypharmacy was defined as taking five or more regular oral medications, and prolonged hospitalization was defined as hospitalization longer than that determined by the clinical pathway. Multiple logistic regression analysis was performed to investigate whether polypharmacy affects the length of hospitalization.
Results
The subjects were 348 males and 236 females, mean ± SD age of 65.8 ± 12.9 years. Among all subjects, 228 (39.0%) were receiving polypharmacy at admission, and the number of patients with prolonged hospitalization was 262 (44.9%). Multiple logistic regression analysis revealed that the following variables were significantly associated with prolonged hospitalization; polypharmacy (odds ratio = 1.532; 95% confidence interval = 1.010–2.327), age 50–59; 2.971 (1.216–7.7758), age 60–69; 2.405 (1.059–5.909), organ pancreas; 0.298 (0.122–0.708), operation time ≥386 min; 2.050 (1.233–3.432), intraoperative bleeding volume ≥401 mL; 2.440 (1.489–4.038), postoperative delirium; 2.395 (1.240–4.734), postoperative infection; 10.715 (4.270–33.059).
Conclusion
The current study revealed that polypharmacy at admission was an independent factor for prolonged hospitalization. In future, measures against polypharmacy are required, collaborating with outpatient clinics, family doctors and dispensing pharmacies. Geriatr Gerontol Int 2020; 20: 1085–1090..
Keywords: clinical pathway, elderly people, gastrointestinal surgery, polypharmacy, prolonged hospitalization
Introduction
Recently, polypharmacy in elderly people has become a serious issue. The Japan Geriatrics Society formulated Guidelines for Medical Treatment and Its Safety in the Elderly in 2005 for the purpose of improving pharmacotherapy safety in the elderly, because elderly people in general tend to have multiple diseases, thus requiring polypharmacy. 1 The latest version of these guidelines includes prescription optimization screening to avoid adverse drug events by polypharmacy, such as drug allergy and organ failure by metabolic and/or excretion abnormalities associated with age‐related changes. According to the Ministry of Health, Labor and Welfare in Japan, the number of prescribed medicines increases with age. 2 In addition, it has been reported that an average of six drugs is prescribed in elderly people when they have a complication of a chronic disease and dementia, or have two or more chronic diseases. 3 Furthermore, past research on hospitalized elderly patients revealed that the risk of adverse drug events increases when individuals take six or more drugs concurrently. 4 However, the problems caused by polypharmacy include not only drug adverse events,5 but also incidents such as falls, 6 , 7 dysfunction and cognitive decline. 8 Therefore, it may be reasonable to assume that polypharmacy at admission may be associated with prolonged hospitalization.
In regard to the effect of polypharmacy/medication on hospitalization, a previous study conducted in Europe revealed that use of non‐steroidal anti‐inflammatory drugs for more than 6 days before admission is associated with the length of hospitalization. 9 Moreover, a previous study on patients undergoing total hip arthroplasty 10 reported that the prehospital dose is related to the length of hospitalization, and suggested that the number of drugs may affect the duration of hospitalization.
However, there are few such studies in Japan, and therefore, in the present study, we aimed to clarify whether polypharmacy at admission has a prolonging effect on hospitalization in Japan.
Methods
Research design
This research was designed as a retrospective study.
Study subjects
The subjects of this study were selected from 4132 patients who were admitted to the gastrointestinal surgery ward of a university hospital in Japan between November 1, 2013 and March 31, 2017. Of these patients, 652 patients to whom clinical pathways were applied and whose number of days in hospital could be identified were extracted. Clinical pathways used in this study were those for gastrectomy, colectomy, colostomy, proctectomy, hepatectomy and pancreaticoduodenectomy (Table 1). 68 patients were excluded due to drop out from the clinical pathways. Finally, 584 subjects were enrolled in the current study (Fig. 1).
Table 1.
Study subjects with clinical pathways
| Name of clinical pathway | Hospitalization days | Disease |
|---|---|---|
| Stomach | ||
| Gastrectomy | 10 | Gastric cancer, Barrett's esophagusGIST † |
| Colon | ||
| Laparoscopic colectomy | 10 | Colon cancer Gastrointestinal perforation Ileus Ulcerative colitisGIST † Crohn's disease adenomatous polyposis |
| Laparotomy colectomy | 15 | |
| Colostomy | 18 | |
| Rectum | ||
| Proctectomy | 17 | GIST † Rectal prolapse, anal canal cancer |
| Liver | ||
| Hepatectomy (segmentectomy, not hepatic cirrhosis) | 10 | Liver cancer, hepatic hemangiomaBile duct cancerLiver donor |
| Hepatectomy (two or larger segmentectomy, hepatic cirrhosis) | 15 | Liver cancer Metastatic liver cancer |
| Pancreas | ||
| Pancreaticoduodenectomy | 23 | Pancreatic cancer Duodenal cancerIntraductal papillary mucinous neoplasmPancreatic neuroendocrine tumor |
Gastrointestinal stromal tumor.
Figure 1.
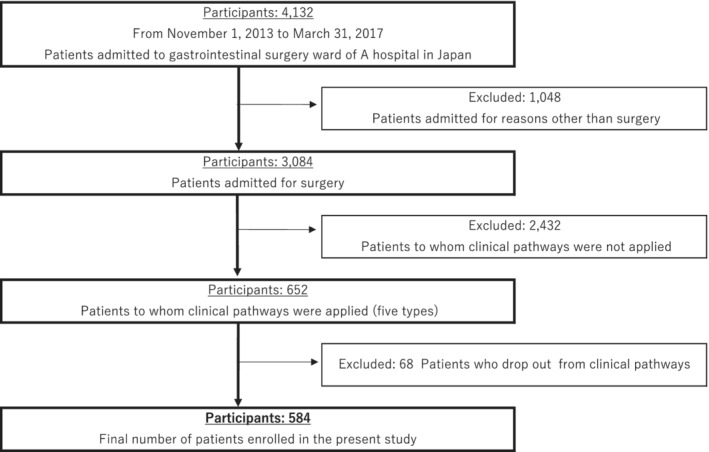
Flow chart of criteria regarding enrollment and exclusion of study participants.
Research items
From medical records, we collected data on age, gender, residence (residence in a municipality where a hospital is located or not), presence or absence of cancer, multimorbidity, operative procedure, operation time (min), intraoperative bleeding volume (mL), presence or absence of physical paralysis, hospitalization longer than or the same length as that determined by the clinical pathway, medication at admission, family structure, course during hospitalization such as malnutrition at admission, postoperative course, activities of daily living, medication management status and family support status.
The length of hospital stay in the clinical pathway is determined based on the Diagnosis Procedure Combination/Per‐Diem Payment System by the in‐hospital review committee.
Evaluation of length of hospitalization
Patients were classified into two groups according to the length of hospitalization; regular and prolonged. The regular group was comprised of patients whose length of hospitalization was shorter or the same as that determined by the clinical pathway. The prolonged group included patients whose length of hospitalization was longer than that determined by the clinical pathway.
Definition of polypharmacy
Currently, there is no clear definition of polypharmacy. In Japan, studies on polypharmacy have reported that the risk of adverse drug events increases when the patient is taking six or more drugs concurrently, 4 and the occurrence of falls is increased with taking five or more drugs concurrently. 6 Based on those results, the medical service fee system in Japan defines polypharmacy as taking six or more drugs concurrently, whereas academic studies in Japan have commonly defined it as more than five or six drugs. On the other hand, in European countries and the United States, many studies define polypharmacy as the concurrent use of five or more drugs, in light of a report by Gnjidic et al. that vulnerability, dysfunction, cognitive decline and death of the elderly increase when they are taking five or more drugs. 8 In the present study, we defined the polypharmacy group as subjects who were taking five or more regular oral drugs at admission and the non‐polypharmacy group for all others.
Analysis
Continuous variables (age, operation time, intraoperative bleeding volume and multimorbidity), are described as median (25–75th percentile) and number (%) for categorical variables. To compare each categorical variable between two groups, we used the Mann–Whitney U‐test and chi‐squared test.
Age (years) was classified into seven groups (20–29, 30–39, 40–49, 50–59, 60–69, 70–79 and ≥80 years). The operation time, intraoperative bleeding volume and multimorbidity were each classified into two groups at the 75th percentile: for operation time, the ≤385‐min and ≥386‐min groups; for intraoperative bleeding volume, the ≤400‐mL and ≥401‐mL groups; and for multimorbidity, the ≤2 and ≥3.
Confounding factors were age, gender, target organs, cancer, operation time, intraoperative bleeding volume, multimorbidity, postoperative infection, postoperative delirium and malnutrition at admission.
To investigate whether polypharmacy affects the length of hospitalization, multiple logistic regression analysis was performed. In this analysis, the age group 40–49 and the stomach were set as references, because the numbers of subjects who were in the regular group were highest in such categories. The objective variable was length of hospitalization, and the explanatory variables were polypharmacy and 10 other factors that may affect the length of hospitalization: age, gender, target organs, operation time, intraoperative bleeding volume, cancer, multimorbidity, postoperative infection, postoperative delirium and malnutrition at admission. Odds ratio (OR) and 95% confidence interval (95% CI) were calculated. It is notable that the explanatory variables consisted of factors that were considered related to outcome, based on the findings of previous studies and clinical judgment.
For statistical analysis, we used R 3.5.2.
Ethics committee approval
This research was approved by the Fukushima Medical University Ethics Committee (approval number: 2456). Informed consent was obtained in the following two ways, according to the date of admission to hospital, i.e., (i) for subjects who were admitted to hospital by June 30, 2016, the scheme of our research was disclosed on our website, instead of obtaining written informed consent, and (ii) for those who were admitted from July 1, 2016 onwards, the updated criteria and procedure of the committee were used for explanation, and only those who agreed to the participation were included.
Results
The study population comprised 584 patients, 348 males and 236 females, with a mean ± SD age of 65.8 ± 12.9 years. Of all patients, 228 (39.0%) were categorized into the polypharmacy group. Regarding the length of hospitalization, 322 (55.1%) were categorized into the regular group and 262 (44.9%) into the prolonged group.
As shown in Table 2, the results of a comparison of patient characteristics between the polypharmacy and non‐polypharmacy groups showed age, prevalence of cancer, malnutrition at admission, prolonged hospitalization, multimorbidity, hypertension, diabetes, respiratory disease, heart disease, cerebrovascular disease, motor disorder, neuropsychiatric disorders, postoperative delirium and physical paralysis were significantly higher in the polypharmacy group (P < 0.001, P = 0.022, P < 0.001, P = 0.003, P < 0.001, P < 0.001, P < 0.001, P = 0.009, P < 0.001, P < 0.001, P = 0.023, P < 0.001, P < 0.001, P = 0.005, respectively).
Table 2.
Comparison between polypharmacy and non‐polypharmacy groups
| n = 584 | |||
|---|---|---|---|
| Polypharmacy | P‐value | ||
| Polypharmacy(n = 228) | Non‐polypharmacy (n = 356) | ||
| Age | 72.0 (66.0–79.0) | 63.0 (55.8–72.0) | P < 0.001 * † |
| Gender (male) | 136 (59.6) | 212 (59.6) | 0.98 ‡ |
| Organ | |||
| Stomach | 42 (18.4) | 103 (28.9) | |
| Colon | 62 (27.2) | 78 (21.9) | |
| Rectum | 27 (11.8) | 33 (9.3) | |
| Liver | 42 (18.4) | 77 (21.6) | |
| Pancreas | 22 (9.6) | 22 (6.2) | |
| Bile duct | 19 (8.3) | 27 (7.6) | |
| Duodenum | 12 (5.3) | 11 (3.1) | |
| Other | 2 (0.9) | 5 (1.4) | 0.057 ‡ |
| Cancer | 196 (86.0) | 279 (78.4) | 0.022 * ‡ |
| Malnutrition at admission | 72 (31.6) | 56 (15.7) | P < 0.001 * ‡ |
| Prolonged hospitalization | 120 (52.6) | 142 (39.9) | 0.003 * ‡ |
| Operation time (min) | 286.5 (203.8–410.8) | 298.0 (202.0–380.2) | 0.93 † |
| Intraoperative bleeding volume (mL) | 110.0 (20.0–382.5) | 100.0 (20.0–402.5) | 0.93 † |
| Multimorbidity | 2.00 (1.00–3.00) | 1.00 (0.00–2.00) | P < 0.001 * ‡ |
| Past medical history | |||
| Hypertension | 115 (50.4) | 85 (23.9) | P < 0.001 * ‡ |
| Diabetes | 85 (37.3) | 31 (8.7) | P < 0.001 * ‡ |
| Respiratory disease | 21 (9.2) | 14 (3.9) | 0.009 * ‡ |
| Heart disease | 61 (26.8) | 30 (8.4) | P < 0.001 * ‡ |
| Cerebrovascular disease | 24 (10.5) | 7 (2.0) | P < 0.001 * ‡ |
| Motor disorder | 27 (11.8) | 23 (6.5) | 0.023 * ‡ |
| Neuropsychiatric disorder | 17 (7.5) | 2 (0.6) | P < 0.001 * ‡ |
| Postoperative complication | |||
| Postoperative infection | 16 (7.0) | 29 (8.1) | 0.62 ‡ |
| Obstruction | 14 (6.1) | 15 (4.2) | 0.3 ‡ |
| Postoperative delirium | 38 (16.7) | 19 (5.3) | P < 0.001 * ‡ |
| Postoperative IVH § | 34 (14.9) | 41 (11.5) | 0.23 ‡ |
| Early ambulation | 200 (87.7) | 319 (89.6) | 0.48 ‡ |
| Alone | 33 (14.5) | 46 (12.9) | 0.6 ‡ |
| Residence | 192 (84.2) | 285 (80.1) | 0.21 ‡ |
| Physical paralysis | 26 (11.4) | 18 (5.1) | 0.005 * ‡ |
Median (range), n (%).
P < 0.05.
Mann–Whitney U‐test.
Chi‐squared test.
Intravenous Hyperalimentation.
As shown in Table 3, the results of logistic regression analysis analyzing factors that affected the length of hospitalization indicated that polypharmacy significantly prolonged hospitalization (OR = 1.532; 95% CI = 1.010–2.327). As for the rest, the following factors significantly increased the length of hospitalization (OR [95% CI]): operation time ≥386 min, 2.050 (1.233–3.432), and intraoperative bleeding volume ≥401 mL, 2.440 (1.489–4.038). In addition, the length of hospitalization was significantly longer in the following categories compared with the references (OR [95% CI]): 50–59 age group, 2.971 (1.216–7.758); 60–69 age group, 2.405 (1.059–5.909); with postoperative delirium, 2.395 (1.240–4.734); with postoperative infection, 10.715 (4.270–33.059).
Table 3.
Results of logistic regression analysis
| (AIC = 742.83) n = 584 | |||
|---|---|---|---|
| Number | Crude OR† (95% CI) | Multivariate‐adjusted OR (95% CI) | |
| Polypharmacy | |||
| Without | 356 | 1.000 (reference) | 1.000 (reference) |
| With | 228 | 1.674 (1.198–2.345) | 1.532 (1.010–2.327) |
| Age (years) | |||
| 20–29 | 9 | 2.133 (0.462–9.446) | 2.769 (0.522–14.337) |
| 30–39 | 17 | 2.370 (0.737–7.691) | 2.963 (0.788–11.164) |
| 40–49 | 44 | 1.000 (reference) | 1.000 (reference) |
| 50–59 | 78 | 2.286 (1.047–5.223) | 2.971 (1.216–7.758) |
| 60–69 | 191 | 2.138 (1.063–4.555) | 2.405 (1.059–5.909) |
| 70–79 | 170 | 2.261 (1.116–4.845) | 2.249 (0.972–5.609) |
| ≤80 | 75 | 2.889 (1.318–6.635) | 2.583 (0.985–7.179) |
| Gender | |||
| Male | 348 | 1.000 (reference) | 1.000 (reference) |
| Female | 236 | 0.752 (0.537–1.049) | 0.929 (0.636–1.357) |
| Organ | |||
| Stomach | 145 | 1.000 (reference) | 1.000 (reference) |
| Colon | 140 | 1.503 (0.938–2.417) | 1.436 (0.852–2.428) |
| Rectum | 60 | 1.475 (0.800–2.714) | 1.039 (0.515–2.077) |
| Liver | 119 | 1.139 (0.692–1.875) | 0.805 (0.452–1.424) |
| Pancreas | 44 | 1.167 (0.580–2.314) | 0.298 (0.122–0.708) |
| Bile duct | 46 | 3.483 (1.751–7.187) | 1.675 (0.757–3.762) |
| Duodenum | 23 | 2.621 (1.077–6.683) | 0.928 (0.321–2.705) |
| Others | 7 | 1.264 (0.241–5.940) | 1.265 (0.219–6.624) |
| Operation time (min) | |||
| ≤385 | 439 | 1.000 (reference) | 1.000 (reference) |
| ≥386 | 145 | 2.263 (1.546–3.332) | 2.050 (1.233–3.432) |
| Intraoperative bleeding volume (mL) | |||
| ≤400 | 443 | 1.000 (reference) | 1.000 (reference) |
| ≥401 | 141 | 2.281(1.553–3.373) | 2.440 (1.489–4.038) |
| Cancer | |||
| Without | 109 | 1.000 (reference) | 1.000 (reference) |
| With | 475 | 1.091 (0.718–1.666) | 0.885 (0.534–1.475) |
| Postoperative delirium | |||
| Without | 527 | 1.000 (reference) | 1.000 (reference) |
| With | 57 | 2.705 (1.538–4.910) | 2.395 (1.240–4.734) |
| Postoperative infection | |||
| Without | 539 | 1.000 (reference) | 1.000 (reference) |
| With | 45 | 11.423 (4.860–33.513) | 10.715 (4.270–33.059) |
| Multimorbidity | |||
| ≤2 | 472 | 1.000 (reference) | 1.000 (reference) |
| ≥3 | 112 | 1.350 (0.893–2.042) | 1.050 (0.629–1.746) |
| Malnutrition on admission | |||
| Without | 456 | 1.000 (reference) | 1.000 (reference) |
| With | 128 | 1.728 (1.166–2.572) | 1.440 (0.924–2.247) |
Multivariate‐adjusted odds ratio (OR) adjusted all variables in table.
CI, confidence interval.
Discussion
In the present study, we revealed that polypharmacy was an independent factor that prolonged hospitalization. In recent years, polypharmacy has attracted attention in terms of adverse drug events and medical costs, leading to many studies being conducted on polypharmacy. These studies have revealed various complications due to polypharmacy, such as adverse drug events, 4 , 5 falls 7 , 11 and increased mortality. 12 , 13 However, to our knowledge, few studies have predicted the length of hospitalization using patient characteristics and medical history. In the current study, polypharmacy at admission was identified as a predictor of prolonged hospitalization. Importantly, polypharmacy is not only influenced by various factors during hospital stay, but also depends on the prehospital treatment situation. Our results suggested that for patients undergoing surgery or during hospitalization for a reason other than their chronic diseases, the medical care being administered should be considered as part of, not independent from their daily life.
Generally, Japanese people tend to perceive security and satisfaction when their drugs are prescribed. In addition, elderly people tend to receive polypharmacy unconsciously, because they often have a high prevalence of complications of multiple diseases. 1 Physicians, nurses and pharmacists provide patient compliance instructions to patients who receive medical treatment. These instructions are implemented for both inpatients and outpatients to explain the safety and efficacy of each drug, and to make sure the patient understands the need to take them correctly. However, polypharmacy can lead to a decrease in medication adherence. 14 , 15 In particular, elderly people may require increased time to acquire medication management skills due to age‐related decline in cognitive function and adaptive ability. 16 If patients with polypharmacy are admitted to hospital, their medications are scheduled and administered by their attending nurses. At discharge, the patients are required to attain self‐management of medication. Otherwise, hospitalization may be prolonged. It may be difficult for elderly people to acquire medication management skills within a limited hospitalization period with the reasons mentioned above. Furthermore, medication management becomes more difficult in cases of elderly individuals who are taking polypharmacy, who use complicated dosing methods, and who have a lack of support. It is assumed that the length of hospitalization may be extended in such cases due to the inability to manage the medication, even if the treatment is completed.
In Japan, shortening the length of hospitalization is promoted by the standardization of medical care and reform of the medical service system. In 2003, a comprehensive evaluation system for diagnosis and treatment fees, the Diagnosis Procedure Combination/Per‐Diem Payment System, was introduced, after which the use of clinical pathways increased dramatically. The clinical pathway is a standardized care plan, including goals, evaluation, and recording of both patient conditions and treatment. 17 Because of the broad use of the clinical pathway, the average length of hospitalization in acute care hospitals in Japan decreased from 20.3 days in 2004, to 16.3 days in 2016. However, this length of stay is still the longest among major developed countries, where the average hospital stay was 9.4 days in Russia, 7.5 days in Germany, 7.3 days in Korea, 6.9 days in Italy and 6.0 days in Britain. 18
Prolonged hospitalization is associated with many problems, such as increases in healthcare costs, 19 onset of disuse syndrome 20 and risk of dementia in the elderly. 21 , 22 Although improvement to decrease these incidences may contribute to the shortening of hospitalization length, it is difficult to predict such incidences. Therefore, factors that predict such incidences are required for the shortening of hospitalization.
An increase in the length of hospitalization increases medical expenses. 19 Since the FY2016 Revision of Reimbursement of Medical Fees in Japan, 23 most medical institutions have been allowed to charge additional medical fees when the number of drugs prescribed for the patient is six or more before admission and is reduced by two or more at discharge. However, while promoting the shortening of hospitalization, reduction of the number of prescribed drugs is assumed to be difficult. Therefore, a method for polypharmacy prevention, collaborating with outpatient clinics, family doctors and regional dispensing pharmacies is required. In addition, the finding that polypharmacy prolongs hospitalization in the current study suggests that further intervention is required by outpatient clinics for polypharmacy prevention.
In the present study, the length of hospitalization was extended whose operation time was ≥386 min, whose intraoperative bleeding volume was ≥401 mL, and who developed postoperative delirium or postoperative infection. These results are consistent with those of previous studies. 24 , 25 , 26
This study has some limitations. First, we did not acquire information of administered medical drugs although they may have affected the hospitalization duration. In a future study, such information should be included in the analysis of the relationship between polypharmacy and hospitalization duration. Second, this study was conducted in an abdominal surgery ward in one hospital. Whether these findings are adopted by other hospitals or other disease conditions such as thoracic surgery or orthopedic surgery, warrants more study in the future.
In the current study, we found that polypharmacy prolonged hospitalization. Our study results suggest that collaboration among outpatient clinics, family doctors, and dispensing pharmacies may be required to ensure that patients follow medication instructions and to adjust polypharmacy before admission. This may enable scheduled discharge and optimal outcome.
Disclosure statement
The authors declare no conflict of interest.
Acknowledgements
The authors are deeply grateful to the patients and medical staff at Fukushima Medical University Hospital for their help in this research.
Abe N, Kakamu T, Kumagai T, et al. Polypharmacy at admission prolongs length of hospitalization in gastrointestinal surgery patients. Geriatr. Gerontol. Int. 2020;20:1085–1090. 10.1111/ggi.14044
Contributor Information
Natsuki Abe, Email: b1950737@fmu.ac.jp.
Takeyasu Kakamu, Email: bamboo@fmu.ac.jp.
References
- 1. Society TJG . Guidelines for Medical Treatment and its Safety in the Elderly 2015 (in Japanese). Tokyo: Medical View Co, Ltd, 2015; 2015. [Google Scholar]
- 2. Ministry of Health LaW . Ministry of Health, Labour and Welfare Statistics of Medical Care Activities in Public Health Insurance. 2016.
- 3. Ministry of Health LaW . Ministry of Health, Labour and Welfare 2017.
- 4. Kojima T, Akishita M, Kameyama Y et al High risk of adverse drug reactions in elderly patients taking six or more drugs: analysis of inpatient database. Geriatr Gerontol Int 2012; 12: 761–762. [DOI] [PubMed] [Google Scholar]
- 5. Field TS, Gurwitz JH, Avorn J et al Risk factors for adverse drug events among nursing home residents. Arch Intern Med 2001; 161: 1629–1634. [DOI] [PubMed] [Google Scholar]
- 6. Kojima T, Akishita M, Nakamura T et al Polypharmacy as a risk for fall occurrence in geriatric outpatients. Geriatr Gerontol Int 2012; 12: 425–430. [DOI] [PubMed] [Google Scholar]
- 7. Dhalwani NN, Fahami R, Sathanapally H, Seidu S, Davies MJ, Khunti K. Association between polypharmacy and falls in older adults: a longitudinal study from England. BMJ Open 2017; 7: e016358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gnjidic D, Hilmer SN, Blyth FM et al Polypharmacy cutoff and outcomes: five or more medicines were used to identify community‐dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 2012; 65: 989–995. [DOI] [PubMed] [Google Scholar]
- 9. Kotsiou OS, Zarogiannis SG, Gourgoulianis KI. Prehospital NSAIDs use prolong hospitalization in patients with pleuro‐pulmonary infection. Respir Med 2017; 123: 28–33. [DOI] [PubMed] [Google Scholar]
- 10. Dietrich M, Zingg PO, Egbring M, Kamath AF, Dora C. Pre‐hospital medications in total hip arthroplasty: risk factors for poor outcomes. Hip Int 2015; 25: 215–220. [DOI] [PubMed] [Google Scholar]
- 11. Borenstein J, Aronow HU, Bolton LB, Choi J, Bresee C, Braunstein GD. Early recognition of risk factors for adverse outcomes during hospitalization among Medicare patients: a prospective cohort study. BMC Geriatr 2013; 13: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Choi KS, Jeong YM, Lee E et al Association of pre‐operative medication use with post‐surgery mortality and morbidity in oncology patients receiving comprehensive geriatric assessment. Aging Clin Exp Res 2018; 30: 1177–1185. [DOI] [PubMed] [Google Scholar]
- 13. Leelakanok N, Holcombe AL, Lund BC, Gu X, Schweizer ML. Association between polypharmacy and death: a systematic review and meta‐analysis. J Am Pharm Assoc 2017; 57: 729‐38.e10. [DOI] [PubMed] [Google Scholar]
- 14. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005; 353: 487–497. [DOI] [PubMed] [Google Scholar]
- 15. Pasina L, Brucato AL, Falcone C et al Medication non‐adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging 2014; 31: 283–289. [DOI] [PubMed] [Google Scholar]
- 16. Hishikawa N, Fukui Y, Sato K et al Characteristic features of cognitive, affective and daily living functions of late‐elderly dementia. Geriatr Gerontol Int 2016; 16: 458–465. [DOI] [PubMed] [Google Scholar]
- 17.Pathway JSfC. Definition of Clinical Pathway.
- 18. OECD: Length of hospital stay.
- 19. Ministry of Health LaW . Ministry of Health, Labour and Welfare. 2006.
- 20. Sonoda S. Immobilization and disuse syndrome. Jpn J Rehabil Med 2015; 52: 265–271. [Google Scholar]
- 21. Ehlenbach WJ, Hough CL, Crane PK et al Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA 2010; 303: 763–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wilson RS, Hebert LE, Scherr PA, Dong X, Leurgens SE, Evans DA. Cognitive decline after hospitalization in a community population of older persons. Neurology 2012; 78: 950–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ministry of Health LaW . Health and Medical Services 2017.
- 24. Andersen K, Thastum M, Norholt SE, Blomlof J. Relative blood loss and operative time can predict length of stay following orthognathic surgery. Int J Oral Maxillofac Surg 2016; 45: 1209–1212. [DOI] [PubMed] [Google Scholar]
- 25. Emond M, Boucher V, Carmichael PH et al Incidence of delirium in the Canadian emergency department and its consequences on hospital length of stay: a prospective observational multicentre cohort study. BMJ Open 2018; 8: e018190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kusachi S, Kashimura N, Konishi T et al Length of stay and cost for surgical site infection after abdominal and cardiac surgery in Japanese hospitals: multi‐center surveillance. Surg Infect (Larchmt) 2012; 13: 257–265. [DOI] [PubMed] [Google Scholar]


