Abstract
Background
Implantable cardiac monitors (ICMs) are increasingly used to detect arrhythmias in various clinical situations. However, the data transmission time and accuracy of detecting cardiac arrhythmias are unclear.
Objective
The objective of this study was to compare the efficiency of data transmission and arrhythmia detection accuracy of the Reveal LINQ with TruRhythm Detection with the Confirm Rx with SharpSense Technology.
Methods
In this prospective study, 142 patients were randomized 1:1 to receive Reveal LINQ or Confirm Rx ICM system. Arrhythmic events include atrial fibrillation (AF), pauses, and bradycardia. Data transmission time is defined as the time from event occurrence to physician notification. All the arrhythmic events are adjudicated for accuracy.
Results
A total of 3510 events were transmitted in 61 patients over 7.1 ± 3.5 months. The transmission time both for all events (448 ± 271 vs 610 ± 515 minutes, P = .02) and for patient activated triggers (24 ± 103 vs 475 ± 426 minutes, P < .0001) was significantly shorter in the Confirm Rx group. The total number of events was also higher in the Confirm Rx group (25.5 ± 45.6 vs 0.9 ± 1.1 events per patient‐month, P < .01), which is likely due to event transmission setting differences between the two groups. Kaplan‐Meier analysis showed that the Confirm Rx group detected true arrhythmic episodes sooner with higher percentage of diagnosed patients during 6‐month follow‐up (P = .006). Patient‐averaged true positive detection rates were not statistically significant in the two groups (Reveal LINQ vs Confirm Rx, AF: 52% vs 38%; bradycardia: 67% vs 59%; pause: 24% vs 20%; tachycardia: 81% vs 94%).
Conclusion
Compared to the Reveal LINQ, Confirm Rx has shorter event transmission time, more frequent event detections, shorter duration to diagnose true arrhythmic events, and higher percentage of diagnosed patients. The accuracy of arrhythmia detection in both ICMs remains suboptimal.
Keywords: atrial fibrillation, cryptogenic stroke, implantable cardiac monitor, remote monitoring, syncope
1. INTRODUCTION
The implantable cardiac monitor (ICM) is a subcutaneously implanted device which can continuously monitor patient heart rhythm up to 3 years. 1 ICMs record and transmit automatically detected arrhythmia episodes and manual patient‐activated symptom episodes to a remote monitoring data server and notifies the clinician. Due to device miniaturization, simplified implant procedures, and enhanced automation and wireless data transmission to patient care networks, ICMs have been used to detect occult cardiac arrhythmias in a variety of clinical situations such as subclinical atrial fibrillation (AF) after cryptogenic stroke, unexplained syncope, palpitations, and management of AF. Timely data transmission and accuracy of arrhythmias detection by the ICM can significantly impact clinical workflow and patient management.
In our clinical practice, Reveal LINQ (Medtronic, Dublin, Ireland) and Confirm Rx (Abbott, Sylmar, CA) ICMs are routinely used. With the intent of reducing false positive detections while maintaining sensitivity, both ICMs have introduced algorithm enhancements to the device. The TruRhythm Detection software in Reveal LINQ, released in 2017, applied a dual‐sense algorithm to reduce false bradycardia and pause episode detections 2 and a more adaptive p‐wave evidence algorithm to reduce false AF episode detections. 3 The SharpSense Technology software recently introduced in Confirm Rx contains four additional discriminators to reduce false bradycardia episodes due to undersensing, false pause episodes due to undersensing, and loss of tissue‐electrode contact, and false AF episode with detectable p‐waves. Both ICMs are capable of remote monitoring. While the Reveal LINQ uses a handheld activator and a home‐based bedside transmitter, the Confirm Rx connects directly to the myMerlin smartphone app via Bluetooth wireless technology. The objective of this study was to compare the efficiency of data transmission and arrhythmia detection accuracy between the two ICMs with their latest respective software.
2. METHODS
2.1. Study subjects
In this single‐center, prospective, randomized study, 142 patients with cryptogenic stroke (n = 98), recurrent unexplained syncope (n = 34), or palpitations (n = 10) were randomized 1:1 to receive the Reveal LINQ or Confirm Rx. Patients were scheduled to be followed up for up to 1 year after initial implant. The study protocol was approved by the institutional review board of the Sparrow Health System. All patients provided informed written consent.
2.2. Device implant and arrhythmia detection
ICM devices were inserted near the left parasternal area over the fourth intercostal space at 45° to the sternum. At the end of the implant procedure, subcutaneous electrocardiogram (ECG) was recorded with an external programmer to confirm reliable signal quality and R‐wave sensing.
ICMs were programmed with the exact same parameters in all patients. Arrhythmic events were defined as pause ≥3 seconds, bradycardia with heart rate ≤40 beats per minute (bpm), tachycardia with heart rate ≥150 bpm, and AF episodes lasting at least 6 minutes.
2.3. Data transmission
In the Reveal LINQ, data were sent wirelessly to a bedside transmitter automatically the next day around midnight and then transmitted through a cellular network to the CareLink network. Symptom episodes were recorded when patients held a patient activator device over the implanted Reveal LINQ and pressed the record symptoms button, however, the symptom episodes would not be transmitted until the device was synced with the bedside transmitter. The Confirm Rx used Bluetooth wireless technology, allowing patients to connect and transmit data using their own mobile devices. The myMerlin mobile app automatically connected to the ICM device the next day around midnight and transmitted the data to the Merlin Patient Care Network. Patients could also use the app to initiate symptom recordings that were immediately transmitted. Event transmission time was calculated as the time from the device‐detected cardiac event to the time in which the data were available on the remote monitoring website (i.e., Merlin.net for Confirm Rx or CareLink for Reveal LINQ). For patient‐activated transmissions, event transmission time was calculated as the time from the patient‐activated event to the time the event was available on Merlin.net or the Carelink system.
2.4. Accuracy of transmitted events
The time from detected arrhythmic events and patient‐activated events to the time of data availability on the respective website for analysis were compared between the two ICMs. All arrhythmic events with subcutaneous ECG were independently adjudicated by two cardiologists who remained blinded to patient demographic and clinical information. If reviewers agreed, the adjudication was considered final. If not, the discrepancies were discussed to reach consensus. In the Confirm Rx group, arrhythmic events prior to the device upgrade to SharpSense technology were excluded from the analysis. For each arrhythmic event category, a true positive detection rate defined as the number of true positive detections over the total number of detections was calculated for each individual patient, and a patient‐averaged true positive detection rate was used to compare the detection accuracy between the two ICM groups.
2.5. Follow‐up
After the ICM implantation, patients were discharged at the same day. Patients were seen in an outpatient clinic 1 week after the procedure and every 3 months thereafter for up to 1 year. They were instructed to transmit events whenever they experienced symptoms.
2.6. Statistical analysis
In this prospective analysis, continuous variables were expressed as mean ± SD and were compared using the Student's t‐test. Categorical variables were compared using the Fisher's exact test. Two‐group Wilcoxon rank sum test was used to compare the true positive rates. Kaplan‐Meier analysis with the log rank test was used to compare freedom from arrhythmias between Confirm Rx and Reveal LINQ. A P‐value of <.05 indicates statistical significance.
3. RESULTS
3.1. Study population
The study has enrolled a total of 142 patients since May 2018. The baseline characteristics of the enrolled patients are listed in Table 1. The mean age of patients was 61 ± 16 years, 45% were male, and the mean body mass index was 30 ± 1.7 kg/m2, and there were no significant differences in the baseline characteristics between the Reveal LINQ group and the Confirm Rx group. Five patients who received the Confirm Rx had not been upgraded to SharpSense technology and were excluded from the analysis. In addition, eight patients in the Confirm Rx group and two patients in the Reveal LINQ group were excluded from the analysis due to inadequate R‐wave amplitudes post‐implant.
TABLE 1.
Baseline demographics of study population
| Variables | Confirm Rx (n = 70) | Reveal LINQ(n = 72) | P value |
|---|---|---|---|
| Age (mean ± SD, years) | 58 ± 17 | 63 ± 13 | .09 |
| Male, % (n/N) | 48.6% (34/70) | 41.6% (30/72) | .97 |
| Body mass index (mean ± SD, kg/m2) | 29 ± 6 | 30 ± 5 | .83 |
| Indications for implant | .24 | ||
|
Stroke Palpitations Syncope |
48 6 16 |
50 4 18 |
Data are shown as mean ± 1 SD and percent values are shown in parentheses.
3.2. Events transmission
A total of 3510 arrhythmic events including 1689 AFs, 817 tachycardias, 166 bradycardias, and 838 pauses were transmitted over 7.1 ± 3.5 months. The number of transmitted arrhythmic events was significantly higher in the Confirm Rx group than the Reveal LINQ group (25.5 ± 45.6 vs 0.9 ± 1.1 events per patient‐month, P < .01). The event transmission time for all events was faster in the Confirm Rx group (448 ± 271 vs 610 ± 515 minutes, P = .02).
A total of 106 manual patient‐activated symptom events were transmitted during the same follow‐up period. The number of transmitted patient‐activated events per patient was also significantly higher in the Confirm Rx group than in the Reveal LINQ group (6.3 ± 3.8 events per patient‐month vs 1.8 ± 1.6 events per patient‐month, P < .0001). The mean time from patient‐activated events to data transmission was significantly faster in the Confirm Rx group than in the Reveal LINQ group (24 ± 103 minutes vs 475 ± 426 minutes, P < .0001).
3.3. Accuracy of AF events
There were 92 AF events transmitted from 11 patients in the Reveal LINQ group and 1597 AF events transmitted from 20 patients in the Confirm Rx group. True AF events were detected in seven patients in the Reveal LINQ group and 12 patients in the Confirm Rx group. Patient‐averaged true positive detection rate was 52% versus 38% for AF (P = .5039). For both groups, the reason for inaccurate AF detection was frequent ectopic beats (Figure 1), p‐wave and/or T‐wave oversensing (Figure 2), and sinus tachycardia with R‐wave undersensing.
FIGURE 1.
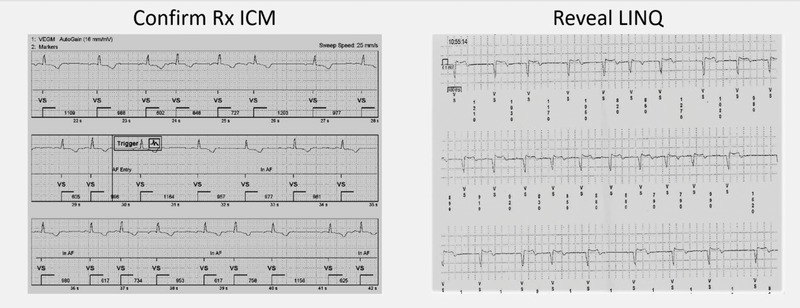
Representative example of false positive AF detection due to frequent ectopic beats
FIGURE 2.
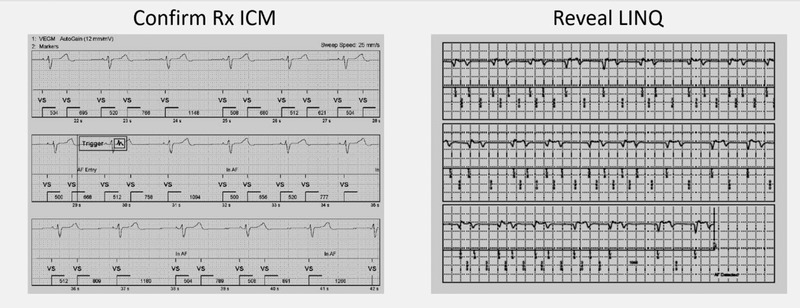
Representative example of false AF detection due to T‐wave and/or p‐wave oversensing
3.4. Accuracy of bradycardia, pause, and tachycardia events
The Reveal LINQ group transmitted eight bradycardias from three patients, 22 pauses from eight patients, and 129 tachycardias from 16 patients. The Confirm Rx group transmitted 158 bradycardias from five patients, 816 pauses from 10 patients, and 688 tachycardias from 21 patients. The number of patients with true bradycardia, pause, and tachycardia events was 2, 3, and 13, respectively, in the Reveal LINQ group and 3, 2, and 17, respectively, in the Confirm Rx group. Patient‐averaged true positive detection rate (Reveal LINQ vs Confirm Rx) was 67% versus 59% (P = .7857) for bradycardia, 24% versus 20% (P = .6471) for pause, and 81% versus 94% (P = .4633) for tachycardia. For both groups, false bradycardia detection was often caused by intermittent undersensing during R‐wave amplitude variations. False pause detection was primarily caused by severe undersensing of R‐waves when the subcutaneous ECG signal had suddenly diminished amplitude (Figure 3). False tachycardia detections were often caused by oversensing of noise artifacts or T‐waves.
FIGURE 3.
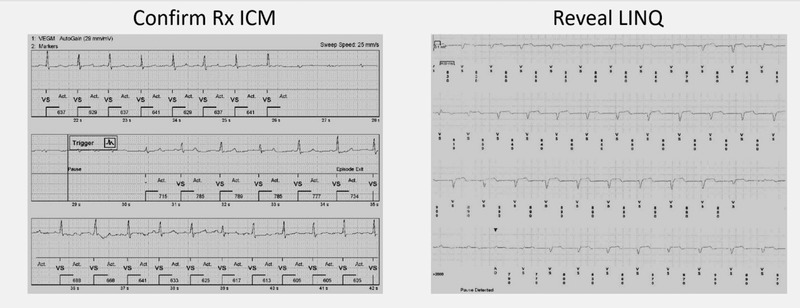
Representative example of false pause detection due to R‐wave undersensing
3.5. Symptom correlation with arrhythmic events
Sixteen patients in the Confirm Rx group and 14 patients in the Reveal LINQ group reported symptoms. A total of 106 symptomatic events were transmitted. Among the transmitted patient‐activated events, 88 arrhythmic events were reported as AF and 18 events were tachycardia. While 55 (62%) of the AF events were accurate, all of the tachycardia events were accurate for either sinus tachycardia or supraventricular tachycardia.
3.6. Freedom from arrhythmias and time to diagnosis
Kaplan‐Meier estimates of freedom from any true arrhythmia episode in the two ICM groups are shown in Figure 4. The curves diverge quickly and continue to have separate paths thereafter, with significantly more patients detected with arrhythmia in the Confirm Rx group than the Reveal LINQ group. By 6 months of follow‐up, freedom from any arrhythmia episode was 43% in the Confirm Rx group, as compared with 79% in the Reveal LINQ group (P = .006).
FIGURE 4.
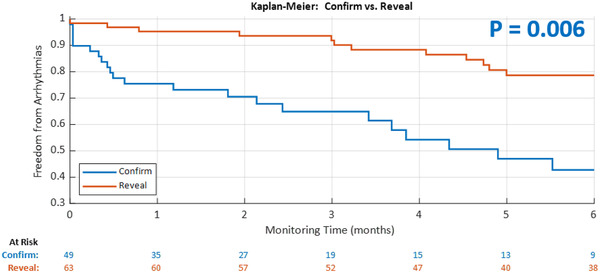
Freedom from any arrhythmia (AF/bradycardia/pause/tachycardia) [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
Usefulness of ICM relies on timely transmission of accurate arrhythmia data to clinician, so prompt medical care can be prescribed to the patients. This study is believed to be the first randomized clinical study comparing arrhythmic data transmission efficiency and accuracy of the two most commonly used ICMs. Arrhythmia data transmission appears to be significantly faster in patients with Confirm Rx particularly for symptomatic patient‐activated episodes. The differences may be attributed to the BlueTooth technology of the Confirm Rx platform. Our study is not designed to assess whether faster data transmission offers favorable clinical outcomes in this group of patients.
Arrhythmia detection accuracy is the most important feature of ICMs. The Reveal LINQ AF detection algorithm employs a three‐step process. First, it looks at the patterns of incoherence of R‐R intervals in a Lorenz plot and assigns an AF score to specific arrhythmia events. Second, it looks for the presence of p‐waves and computes a p‐wave evidence score, and then finally, an AF evidence score is computed. Clinical studies demonstrated that the true positive rate for AF detection is dependent on the AF prevalence in the study cohorts, the programmed sensitivity of AF algorithm, as well as the duration of detected AF episodes. 2 , 4 The TruRhythm Detection for Reveal LINQ applies an adaptive p‐wave evidence algorithm to further reduce false AF detection with minimal reduction in sensitivity. 3 The base algorithm in Confirm Rx is similar to the prior Confirm ICM. The details of this algorithm have been described in a previous study. 5 Briefly, the algorithm uses a Markov Chain model to detect R‐R interval irregularities, a variance model to reject regularly irregular rhythms such as bigeminy and trigeminy, and sudden onset criteria to reject rhythms that are not sudden. In SharpSense Technology, a p‐wave detection algorithm is activated when the base algorithm triggers AF detection. The p‐wave detection algorithm analyzes the EGM signal prior to the trigger and rejects the initial detection if consistent p‐waves are found.
Earlier studies have suggested that ICMs have highly acceptable AF accuracy detection. Hindricks et al 6 reported Medtronic Reveal ICMs have an overall 98% AF detection accuracy in patients with paroxysmal AF. Accuracy of arrhythmia detection in both ICMs in our study was suboptimal.
Our data reported that AF false positive rate was high in both ICMs (48% in Reveal LINQ and 62% in Confirm Rx). Adjudication of the false positive AF events concluded that premature beats are the most common reason for a false positive result followed by double counting of p‐wave, T‐wave, and noise. Our findings are in line with recently published studies. Afzal et al 7 recently reported that the incidence of false positive transmissions in patients with Reveal LINQ was substantial, ranging from 46% to 86% depending on the indication for implantation. Chorin et al 8 studied 145 patients with cryptogenic strokes implanted with Reveal LINQ. The authors reported that the incidence of AF false positives during remote monitoring with nominal settings remained significantly high, ranging from 84% (with the TruRhythm software) to 96% (without TruRhythm). The authors concluded that oversensing of T‐wave and atrial premature beats were the most common reasons for the inaccuracy.
Even though the accuracy of non‐AF events including bradycardia and tachycardia appears to be better than AF events, the false positive rate for pauses detection in both ICMs was close to 80%. R‐wave undersensing was the culprit in dismal true detection of pause episodes.
One interesting finding of the study showed that the number of arrhythmic events transmitted by Confirm Rx was far more than Reveal LINQ in this randomized study. Arrhythmic events transmitted in patients with Confirm Rx were 25.5 per patient‐month versus only 1.1 events per patient‐month. The difference in number of transmitted events could be partially due to the arrhythmia detection algorithms in these ICMs. However, another importance aspect is that the two ICM systems have different transmission logics. In its daily audit, Confirm Rx ICM transmits all arrhythmic events stored in the device memory. In contrast, Reveal LINQ ICM limits the number of events in the daily audit based on prespecified data priority for ventricular episodes, and the longest AF episode occurred. Clinics need to contact the patient to pick up the home equipment and perform a manual transmission in order to see the remaining events stored in the device. The large number of transmitted events by Confirm Rx ICM may overburden the remote clinic technicians as well as the physician who adjudicates these events. On the other hand, the arrhythmia transmission algorithm in the Reveal LINQ only transmitting one arrhythmic event per day could potentially underestimate arrhythmic burden of the patient or delay the diagnosis. The fewer AF events from Reveal LINQ could potentially influence positive predictive value. Further studies are warranted to determine if these differences in events transmission logics result in differences in clinical outcomes.
Results from the Kaplan‐Meier analysis showed that freedom from any arrhythmia (AF/bradycardia/pause/tachycardia) was significantly different between the two ICM groups. The Confirm Rx detected arrhythmias more quickly than the Reveal LINQ. In addition, the Confirm Rx identified more patients with arrythmias by 6 months of follow‐up. Further studies with larger samples sizes and longer follow‐up duration are needed to confirm these results.
4.1. Clinical utility of the devices
During follow‐up, device‐detected episodes were utilized to change clinical management in 36 patients. Permanent pacemaker implantation was performed in six patients due to either prolonged pauses or symptomatic bradycardia (three patients with Confirm Rx and three patients with Reveal LINQ). Oral anticoagulation was prescribed in another five patients with episodes of AF (three patients with Confirm Rx and two patients with Reveal LINQ). In the cryptogenic stroke cohort, 22 patients (12 patients with Confirm Rx and 10 patients with Reveal LINQ) received oral anticoagulant after AF detection.
It is recognized that this study was not powered to assess the impact of ICM use on the clinical management of patients. Larger studies are needed to confirm these findings. However, it is important to assess whether actionable interventions and clinical outcomes would be different in patients implanted with these two ICMs. Larger, multicenter studies are needed to further investigate and answer these important questions.
4.1.1. Limitations
First, this study is only a single‐center study. Second, the patient population for ICM indication in this study may be different from other institutions. Third, the impact of R‐wave amplitude to arrhythmia detection accuracy was not studied. Despite the limitations, this is the first randomized clinical study looking at device performance and arrhythmia detection accuracy of the two most commonly ICMs. Larger studies are warranted to confirm these findings.
5. CONCLUSIONS
Data transmission of arrhythmic events using the Confirm Rx ICM is significantly faster than the Reveal LINQ, particularly the patient‐activated symptom events. The Confirm Rx ICM resulted in faster diagnosis of arrhythmias and identified higher percentage of patients with arrhythmias. However, the burden of transmitted events in the Confirm Rx ICM is significantly higher than the Reveal LINQ ICM. The accuracy of arrhythmia detection with current algorithms in both ICMs remains suboptimal. Differences in arrhythmia detection algorithms and transmission logics in these two ICM systems contribute to the significant disparity in the amount of data generated. New detection algorithms are needed in the future ICM platform to ensure that all clinically relevant and accurate arrhythmic events can be captured.
CONFLICT OF INTEREST
Dr John Ip is a member of the Speakers Bureau for Abbott and has received research grants from Medtronic and Abbott.
AUTHOR CONTRIBUTIONS
Study concept and design: John Ip. Analysis and interpretation of data: John Ip, Ali Sheikh, Carson Castellani, and Randy Ip. Drafting of the manuscript: Randy Ip. Critical revision of the manuscript for important intellectual content: John Ip, Brian Jaffe, Mark Castellani, Ali Sheikh, and Carson Castellani. Approval of submitted and final manuscript: John Ip, Brian Jaffe, Mark Castellani, Ali Sheikh, Carson Castellani, and Randy Ip. Acquisition of data: Brian Jaffe and Mark Castellani.
Funding information
Abbott, Inc.
Ip J, Jaffe B, Castellani M, Sheikh A, Castellani C, Ip R. Accuracy of arrhythmia detection in implantable cardiac monitors: A prospective randomized clinical trial comparing Reveal LINQ and Confirm Rx. Pacing Clin Electrophysiol. 2020;43:1344–1350. 10.1111/pace.14076
REFERENCES
- 1. Giancaterino S, Lupercio F, Nishimura M, Hsu JC. Current and future use of insertable cardiac monitors. JACC Clin Electrophysiol. 2018;4:1383‐1396. [DOI] [PubMed] [Google Scholar]
- 2. Mittal S, Rogers J, Sarkar S, et al. Real‐world performance of an enhanced atrial fibrillation detection algorithm in an insertable cardiac monitor. Heart Rhythm. 2016;13:1624‐1630. [DOI] [PubMed] [Google Scholar]
- 3. Purerfellner H, Sanders P, Sarkar S, et al. Adapting detection sensitivity based on evidence of irregular sinus arrhythmia to improve atrial fibrillation detection in insertable cardiac monitors. Europace. 2018;20:f321‐f328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sanders P, Purerfellner H, Pokushalov E, et al. Performance of a new atrial fibrillation detection algorithm in a miniaturized insertable cardiac monitor: results from the Reveal LINQ Usability Study. Heart Rhythm. 2016;13:1425‐1430. [DOI] [PubMed] [Google Scholar]
- 5. Nolker G, Mayer J, Boldt LH, et al. Performance of an implantable cardiac monitor to detect atrial fibrillation: results of the DETECT AF Study. J Cardiovasc Electrophysiol. 2016;27:1403‐1410. [DOI] [PubMed] [Google Scholar]
- 6. Hindricks G, Pokushalov E, Urban L, et al. Performance of a new leadless implantable cardiac monitor in detecting and quantifying atrial fibrillation: results of the XPECT trial. Circ Arrhythm Electrophysiol. 2010;3:141‐147. [DOI] [PubMed] [Google Scholar]
- 7. Afzal MR, Mease J, Koppert T, et al. Incidence of false‐positive transmissions during remote rhythm monitoring with implantable loop recorders. Heart Rhythm. 2020;17:75‐80. [DOI] [PubMed] [Google Scholar]
- 8. Chorin E, Peterson C, Kogan E, et al. Comparison of the effect of atrial fibrillation detection algorithms in patients with cryptogenic stroke using implantable loop recorders. Am J Cardiol. 2020;129:25‐29. [DOI] [PubMed] [Google Scholar]


