Abstract
Importance
This is the first comprehensive comparison between ab interno approach and ab externo approach for microcatheter‐assisted trabeculotomy in primary congenital glaucoma with clear cornea.
Background
Ab externo microcatheter‐assisted trabeculotomy is considered to be the gold standard for primary congenital glaucoma. The novel ab interno approach would intuitively be similar to ab externo approach for microcatheter‐assisted trabeculotomy in eyes with clear cornea; however, there is no evidence yet.
Design
Non‐contemporary comparison of retrospective case series.
Participants
Fifty‐eight and fifty‐seven consecutive primary congenital glaucoma eyes with clear corneas underwent ab interno and ab externo microcatheter‐assisted trabeculotomy, respectively.
Methods
Retrospective comparison of clinical outcomes.
Main Outcome Measures
Surgical success was defined as a postoperative intraocular pressure of ≤21 mmHg with at least a 30% reduction from preoperative IOP with or without the use of anti‐glaucoma medication (qualified and complete success, respectively).
Results
The qualified success rate (87.9% vs 82.2%, P = .40) and complete success rates (81.0% vs 73.3%, P = .32) were comparable between groups. Complications were minimal and comparable. Less than 360° trabeculotomy (P = .009) and a higher number of previous surgeries (P = .03) were both associated with worse surgical outcomes.
Conclusions and Relevance
Ab interno approach provide good and comparable outcomes as ab externo approach for microcatheter‐assisted trabeculotomy in primary congenital glaucoma eyes with clear cornea. It should be considered as the initial choice in these patients with the benefit of sparing conjunctiva. Successful trabeculotomy with either technique during the first attempt is critical to overall success and underscores the need for proficiency before independent practice.
Keywords: ab externo microcatheter‐assisted trabeculotomy, ab interno microcatheter‐assisted trabeculotomy, clear cornea, primary congenital glaucoma
1. INTRODUCTION
The definitive treatment for primary congenital glaucoma (PCG) is ocular surgery. First pioneered by Barkan in 1938, angle surgery—initially goniotomy, closely followed by Smith and Burian's trabeculotomy ab externo—revolutionized the treatment of PCG, and led to drastic improvement in prognosis for these patients. 1 , 2 , 3 , 4 Both goniotomy and traditional trabeculotomy have been found to have comparable results when controlling for disease severity. 2 , 4 , 5 , 6 The choice between the two surgeries is typically dictated by corneal clarity and surgeon preference. 7 Over the past two decades, improvements in trabeculotomy have included circumferential suture techniques, 8 , 9 , 10 and a flexible illuminated microcatheter technique (iTrack, Ellex, Menlo Park, California). 11 , 12 , 13 , 14 , 15 Since the ab externo microcatheter‐assisted trabeculotomy (MAT) using the illuminated microcatheter can avoid the most serious consequences encountered using the suture technique, 8 , 16 , 17 and had been proved to have better outcomes than both goniotomy and traditional trabeculotomy, it is now considered by some specialists to be the gold standard for PCG. 11 , 12 , 13 , 18 , 19
For the PCG patients with clear corneas, ab interno approach would have advantage because it spares conjunctiva. Therefore, we introduced ab interno MAT into our PCG patients with clear corneas since 2018, 20 which initially described by Grover. 21 However, there is no direct comparison between the two procedures in terms of their surgical outcome. The aim of this study is to compare the outcomes of these two techniques in PCG eyes with clear corneas.
2. METHODS
2.1. Participants
This study was a retrospective, consecutive case series of PCG eyes undergoing either an ab externo MAT from January 2018 to September 2018 or an ab interno MAT from September 2018 to August 2019 at Beijing Tongren Eye Center. Surgeries were performed by two surgeons (HZ Wang and NL Wang) using an ophthalmic microcatheter (iTRACK 250A; iScience Interventional, Menlo Park, California). Patients with PCG included in the analysis had examinations consistent with the diagnosis of PCG, including isolated trabeculodysgenesis without any other ocular or systemic abnormalities, elevated IOP, increased corneal diameter, corneal edema, increased axial length, and glaucomatous cupping of the optic nerve. And only eyes with visible iris details and angle details were included. Exclusion criteria included eyes with previous non‐glaucoma ophthalmic surgery, and less than 3 months follow‐ups. In patients with bilateral PCG, both eyes were included if they both met inclusion criteria. This study was approved by the Ethics Committee of Beijing Tongren Hospital, adhered to the tenets of the Declaration of Helsinki, and was registered under the Chinese Clinical Trials Registry (ChiCTR1900023571). Each patient's legal guardian or representative signed an informed consent to provide the clinical data for this study.
2.2. Surgical procedure and postoperative care
2.2.1. Ab interno MAT
The detailed surgical procedure has previously been described including illustrations. 22 Briefly, a temporal paracentesis is created and viscoelastic (2.0% sodium hyaluronate) is injected into the anterior chamber. A microcatheter is inserted into the anterior chamber through a paracentesis track placed in either the superonasal or inferonasal quadrant. Using direct visualization with a gonioprism, a 1‐2 mm goniotomy is created in the nasal angle with a microsurgical blade (25‐gauge microvitreoretinal blade). Microsurgical forceps are then used to grasp the microcatheter within the anterior chamber and insert it into Schlemm's canal (SC) at the goniotomy incision and advance the catheter through the canal circumferentially within the anterior chamber. Upon retrieval of the distal tip after the catheter has passed 360°, the tip is externalized from the temporal corneal incision and creating a 360° ab interno trabeculotomy. In some cases, the microcatheter becomes obstructed or misdirected. In these cases, the distal tip of the microcatheter is retrieved under direct visualization using the gonioprism. Viscoelastic is then removed from the anterior chamber. The wounds are hydrated and checked to ensure watertight closure. Sutures are applied for the corneal wound(s) with persistently leaking after hydration.
2.2.2. Ab externo MAT
The details have been described previously. 12 , 13 Briefly, following a conjunctival peritomy, SC is exposed by either scleral cut down under a superficial scleral flap or direct unroofing via a deep scleral flap. Surgery was performed superiorly in eyes without previous angle surgery, and in those with previous surgery, the scleral flap was created at least 60° lateral to the site of previous surgery to avoid possible prior scarring of Schlemm's canal. Once SC is identified, the microcatheter is inserted into the canal and threaded circumferentially. In the case of microcatheter obstruction or misdirection in one direction, the microcatheter is directed the opposite way. In the case of microcatheter obstruction in both directions, the conjunctiva is incised and a scleral cut down is performed over the illuminated catheter tip and the trabeculotomy is performed in the direction providing the greatest degree of microcatheter advancement. Both exposed ends of the catheter are then grasped and pulled in opposite directions like a purse string creating a partial trabeculotomy. In all cases, the scleral flap is closed with interrupted 10‐0 nylon sutures and the conjunctiva is approximated with 8‐0 vicryl sutures. Gentle anterior chamber irrigation is performed via a paracentesis in cases with significant hyphema.
2.2.3. Postoperative care
Postoperatively, tobramycin/dexamethasone (TobraDex, Alcon, Rijksweg, Belgium) was prescribed 4 times daily and tapered over 2 weeks, Panoprofen (PRA, Pranopulin, Sunju Pharmaceutical Co, Ltd, Japan) 4 times daily for 2 weeks, and pilocarpine 2% (Bausch & Lomb, Rochester, New York) 4 times daily for 3 months. We routinely use pilocarpine for up to 3 months to prevent the development of peripheral anterior synechiae after trabeculotomy regardless of IOP and it was not considered as an IOP lowering medication in our analysis.
2.3. Data collection
All patients' follow‐up results at preoperation and postoperative months 1, 3, 6, 9 and 12 were collected. The following information was collected: gender, disease laterality, age of onset, age at time of surgery, prior surgeries, corneal diameter, cup‐to‐disc ratio, the extent of successful trabeculotomy (degree), intraoperative and postoperative complications, duration of follow‐up, IOP and number of medications at each follow‐up visit. The age of onset was divided into three stages according to the classification of PCG 23 : (a) neonatal or newborn onset (0‐1 month); (b) infantile onset (>1‐24 months); (c) late onset or late‐recognized (>2 years). IOP results used in this study were all measured by the Icare tonometer (Icare TA01i, Icare, Finland) under chloral hydrate sedation. The median dosage of chloral hydrate given was 75 mg/kg (range: 50‐100 mg) with either oral or rectal administration.
2.4. Main outcome measurements
Surgical success was defined as: (a) a postoperative intraocular pressure of ≤21 mmHg with at least a 30% reduction from preoperative IOP with or without the use of anti‐glaucoma medications (qualified and complete success, respectively); (b) no further surgical therapy; (c) stabilized corneal diameter and (d) no enlargement of cup to disc ratio.
2.5. Statistical analysis
2.5.1. Sample size calculation
We calculated sample size based on primary outcome. Our previously published data demonstrated an overall success rate of approximately 95% for ab externo MAT 24 and 90% for ab interno MAT 20 in PCG patients with clear corneas. We estimated the sample size based on a difference of 15% in terms of the qualified success between these two procedures as a non‐inferiority study. With a 2‐sided test using a level of 0.05 and a power of 80%, and an attrition rate up to 15%, the sample size was 55 subjects per arm. According to the sample size, we determined the time period of collecting case series.
The Pearson χ 2 test was used to compare parameters between groups and the linear mixed model was employed when adjusting for the correlation between two eyes of patients with both eyes involved among groups were needed. The linear mixed model with time as the repeated measurement was used to compare IOP and number of medications from preoperative baseline to 12 months postoperatively in each group and between groups after adjusting for the correlation between two eyes in patients with bilateral disease. Bonferroni correction was used to counteract multiple comparisons. Kaplan‐Meier survival functions were constructed for complete and qualified success and compared between groups using a robust variance estimator to account for the clustering of eyes within patients. Eyes undergoing a secondary surgical procedure were defined as failure and censored from analysis subsequent to the intervention. Additionally, Cox regression (stepwise regression) was used to analyse the risk factors affecting the surgical success rate in all cases, using the following factors as independent variables: age of disease onset, disease laterality, age at the time of surgery, gender, number of previous operations, preoperative IOP, preoperative number of medications, corneal diameter, cup‐to‐disc ratio, extent of trabeculotomy, different surgeons and groups (ab interno MAT and ab externo MAT). All statistical analyses were performed using SPSS (V.24.0; SPSS, Chicago, Illinois). Alpha values of 0.05 were used for statistical calculations.
3. RESULTS
3.1. Demographics and preoperative parameters
Of the 89 patients enrolled, 66 were male (74%) and 23 were female (26%). A total of 115 PCG eyes were included, with 58 eyes of 49 patients who underwent ab interno MAT (Group 1) and 57 eyes of 40 patients who underwent ab externo MAT (Group 2). Eighteen (20%) patients were unilateral and 71 (80%) were bilateral disease. There was a higher prevalence of bilateral disease in females (96% vs 74%, P = .03). Sixty‐four (56%) eyes were operated by NL Wang, and 51 (44%) eyes were operated by HZ Wang (P = .23). Table 1 reports the demographic variables of the cohort. Median follow‐up duration was 12 months (range: 3‐12) in Group 1 and 12 months (range: 3‐12) in Group 2 (P = .50). No differences were found with respect to age, stage of onset age, horizontal corneal diameter, cup‐to‐disc ratio, previous surgeries, number of preoperative medications, or preoperative IOP (all P > .05) between the two study groups (Table 1). There were more females (P = .03) and more bilateral cases (P = .003) in Group 2. In Group 1, 40 eyes (69%) had complete 360° trabeculotomy, 18 eyes (31%) had incomplete catheterization due to obstructions. In Group 2, 37 eyes (65%) had complete 360° trabeculotomy, 20 eyes (35%) had incomplete catheterization due to obstructions.
TABLE 1.
Comparison of subject clinical characteristics and extent of trabeculotomy between ab interno and ab externo MAT
| Parameter | Total | Ab interno MAT | Ab externo MAT | P |
|---|---|---|---|---|
| Number of patients (N, %) | 89 | 56 (54) | 47 (46) | .38 |
| Number of eyes (N, %) | 115 | 58 (50) | 57 (50) | .93 |
| Unilateral/bilateral onset | 14/75 | 11/45 | 3/44 | .003 a |
| Gender (male/female) | 83/32 | 47/11 | 36/21 | .03 a |
| OD/OS | 63/52 | 33/25 | 30/27 | .65 |
| Age (months, median, range) | 31 (3‐168) | 31 (4‐168) | 30 (3‐130) | .90 |
| Stage of onset age (stage 1/2/3) | 52/44/19 | 27/22/9 | 25/22/10 | .68 |
| Corneal diameter (mm, median, range) | 13.0 (10.0‐16.0) | 13 (10.5‐15.0) | 13.0 (10.0‐16.0) | .17 |
| Cup‐to‐disc ratio (median, range) | 0.8 (0.4‐1.0) | 0.85 (0.6‐1.0) | 0.8 (0.4‐1.0) | .20 |
| Number of eyes with previous surgeries (0/1/2 surgeries) | 61/36/18 | 33/14/11 | 28/22/7 | .93 |
| Trabeculotomy (1/2 surgeries) | 16/0 | 9/0 | 7/0 | |
| Goniotomy (1/2 surgeries) | 7/0 | 2/0 | 5/0 | |
| Trabeculotomy + trabeculectomy (1/2 surgeries) | 16/4 | 7/2 | 9/2 | |
| Glaucoma drainage implant (1/2 surgeries) | 5/0 | 2/0 | 3/0 | |
| Trabeculectomy (1/2 surgeries) | 14/3 | 8/2 | 6/1 | |
| Number of preoperative medications (median, range) | 3 (0‐4) | 3 (1‐4) | 3 (0‐4) | .14 |
| Preoperative IOP (mmHg, mean [95% confidence intervals]) | 33.7 (32.4‐35.0) | 33.5 (31.7‐35.3) | 33.8 (32.0‐35.7) | .81 |
| Number of eyes with different extent of trabeculotomy (360°/≥180° and <360°/<180°) | 77/30/8 | 40/18/0 | 37/12/8 | .13 |
Abbreviations: IOP, intraocular pressure; MAT, microcatheter‐assisted trabeculotomy; OD, oculus dexter; OS, oculus sinister.
Statistical significance.
3.2. Success rate
Table 2 shows the cumulative success rates at various postoperative time points and Figure 1 shows the Kaplan‐Meier survival plots. At 12‐month follow‐up, Group 1 achieved an 81.0% complete and 87.9% qualified success rate, while this was achieved in Group 2 at rates of 73.3% and 82.2%, respectively. There were no significant differences between groups for either complete or qualified success (P = .32 and P = .40, respectively). In Group 1, 5 eyes (9%) underwent other glaucoma surgeries at 3‐ or 6‐month follow‐up (3 eyes underwent goniotomy and goniosynechialysis, 2 eye underwent transscleral diode laser cyclophotocoagulation [TDLCP]). In Group 2, 3 eyes (5%) underwent other glaucoma surgeries at 3‐ or 6‐month follow‐up (1 eye underwent ab interno MAT, 2 eyes underwent TDLCP). These 8 eyes were then considered failures and censored from analysis subsequent to the intervention. At 12‐month follow‐up, the success rate was not different between boys and girls (qualified success rate: 86.8% vs 80.5%, P = .39; complete success rate: 80.8% vs 67.6%, P = .11). Four eyes in Group 1 and 6 eyes in Group 2 did not complete 12 month follow‐up. Among these 10 eyes, only 1 eye in Group 1 and 2 eyes in Group 2 had an IOP higher than 21 mmHg and were defined as failure before their last follow‐up. The remaining eyes demonstrated treatment success at last follow‐up.
TABLE 2.
Cumulative success rate for groups
| Follow‐up | Complete success (%) | Qualified success (%) | N (eyes) | ||||
|---|---|---|---|---|---|---|---|
| Ab interno MAT | Ab externo MAT | Ab interno MAT | Ab externo MAT | Ab interno MAT | Ab externo MAT | ||
| 1 month | 91.4 | 82.5 | 94.8 | 89.5 | 58 | 57 | |
| 3 months | 84.5 | 78.9 | 89.7 | 87.7 | 58 | 57 | |
| 6 months | 82.8 | 77.1 | 87.9 | 85.9 | 57 | 55 | |
| 9 months | 81.0 | 73.3 | 87.9 | 82.2 | 51 | 53 | |
| 12 months | 81.0 | 73.3 | 87.9 | 82.2 | 49 | 47 | |
Abbreviation: MAT, microcatheter‐assisted trabeculotomy.
FIGURE 1.
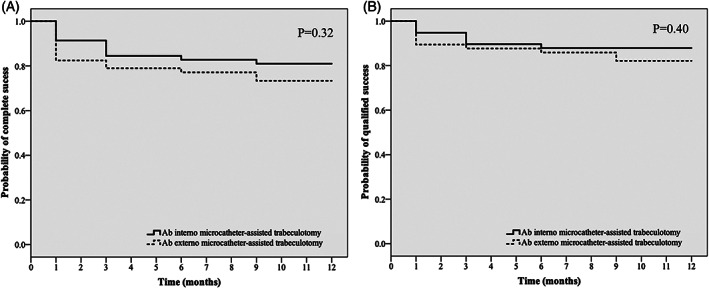
Kaplan‐Meier survival plots of the cumulative probability of success rate for ab interno and ab externo microcatheter‐assisted trabeculotomy
Since the success rate of the two groups were comparable, all data were combined to analyse the risk factors affecting the success rate. Among all study variables, Cox stepwise regression survival analysis demonstrated that extent of trabeculotomy (P = .009, ORextent of trabeculotomy = 0.994 (95% confidence intervals [CI]: [0.990, 0.999])), and number of previous surgeries (P = .03, ORno. of previous surgeries = 1.730 (95% CI: [1.065, 2.811])) contributed most to complete surgical success. The risk function was defined as:
In this equation, h t is the risk of failure, h0(t) represents the amount of background risk.
3.3. Change in IOP and anti‐glaucoma medication usage
Mean IOP decreased from 33.5 (95% CI: 31.7‐35.3) mmHg in Group 1 and 33.8 (95% CI: 32.0‐35.7) mmHg in Group 2 preoperatively to 15.5 (95% CI: 14.5‐16.5) mmHg and 15.9 (95% CI: 14.7‐16.7) mmHg at 12 months postoperatively, respectively. Median number of medications decreased from 3 in each group (range: 1‐4) preoperatively to 0 (0‐3) in each group at 12 months postoperatively. IOP and number of medications were significantly reduced from baseline at all postoperative visits in both groups (all P < .001), and there were significant differences in number of medications (P = .02) but no significant differences in IOP between groups (P = .44) (Table 3).
TABLE 3.
IOP and number of medications between groups at each follow‐up
| IOP (mmHg, Mean [95% confidence intervals]) | Medications (Mean [95% confidence intervals]) | ||||||
|---|---|---|---|---|---|---|---|
| Follow‐up | Ab interno MAT | Ab externo MAT | P | Ab interno MAT | Ab externo MAT | P | |
| Preoperative | 33.5 (31.7‐35.3) | 33.8 (32.0‐35.7) | .81 | 2.7 (2.5‐2.9) | 2.9 (2.7‐3.0) | .14 | |
| 1 month | 15.0 (13.3‐16.7) | 16.1 (14.3‐17.8) | .38 | 0.4 (0.1‐0.7) | 0.6 (0.3‐0.9) | .36 | |
| 3 months | 16.0 (14.0‐18.0) | 16.3 (14.2‐18.3) | .87 | 0.4 (0.2‐0.7) | 0.6 (0.3‐0.9) | .52 | |
| 6 months | 16.1 (14.4‐17.9) | 16.2 (14.4‐18.0) | .95 | 0.5 (0.2‐0.7) | 0.4 (0.2‐0.7) | .98 | |
| 9 months | 15.7 (14.4‐16.9) | 16.0 (14.7‐17.3) | .71 | 0.2 (0‐0.4) | 0.4 (0.2‐0.6) | .15 | |
| 12 months | 15.5 (14.5‐16.5) | 15.7 (14.7‐16.7) | .78 | 0.2 (0‐0.4) | 0.5 (0.3‐0.8) | .04 a | |
Abbreviations: IOP, intraocular pressure; MAT, microcatheter‐assisted trabeculotomy.
Statistical significance.
The median percentage change in IOP from preoperative to the last postoperative follow‐up was greater in eyes with 360° trabeculotomy (56.3%, interquartile range: 45.5%‐63.0%) than in eyes with partial trabeculotomy (44.3%, interquartile range: 27.9%‐52.4%) (P = .001, Figure 2A). For those with previous surgery, 360° trabeculotomy was achieved in only 26 eyes (48%), significantly lower than in eyes without previous surgery, 51 eyes (84%, P < .001). The median percentage of IOP reduction from preoperative to the last postoperative follow‐up was greater in eyes without previous surgery (57.1%, interquartile range: 50.0%‐64.4%) than in eyes with previous surgery (44.1%, interquartile range: 25.2%‐55.7%) (P < .001, Figure 2B).
FIGURE 2.
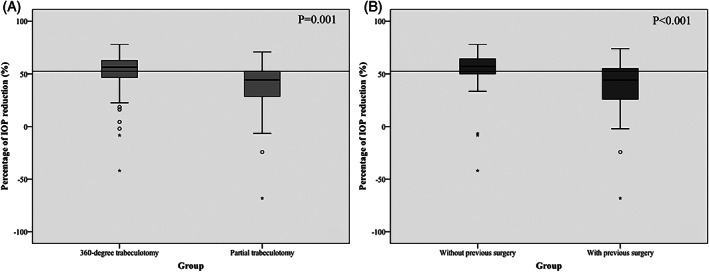
A, Box‐and‐whiskers plots showing the percentage of IOP reduction across eyes with 360° trabeculotomy and eyes with partial trabeculotomy. B, Box‐and‐whiskers plots showing the percentage of IOP reduction across eyes without previous surgeries and eyes with previous surgery. Box plots illustrate the median (50th percentile) as a black centre line and the 25th and 75th percentile as the lower and upper hinges of the box. Circles represent minor outliers and star represent extreme outliers. The black line across each chart is the median percentage of IOP reduction of all eyes. IOP, intraocular pressure
3.4. Complications and secondary procedures
Hyphema was noted intraoperatively and on the first postoperative day in all subjects, resolving within a median of 3 days (range: 1‐7 days) in each group (P = .871). Anterior chamber irrigation was required in 2 eyes in Group 1 and 1 eye in group 2 due to significant hyphema on postoperative day 5‐7. At the 1‐month follow‐up examination, no patients in either group had any evidence of hyphema. Eleven eyes in Group 1 and 5 eyes in Group 2 (percentages; P = .086) suffered from IOP spikes to 30 mmHg that lasted 3‐8 days. No cases of iris tear, Descemet's tears or persistent hypotony were noted.
4. DISCUSSION
Recently, there have been advances in the approach for goniotomy and trabeculotomy that have increased the ease of these surgeries. First, a flexible illuminated microcatheter (iTrack), which aids in the identification and cannulation of SC, has been developed and extensively used for circumferential trabeculotomy. 11 , 12 , 13 , 14 , 15 Second, an ab interno approach to trabeculotomy, initially described by Grover as a promising minimally invasive approach, 22 is a continuation of the evolution, though its surgical outcomes in PCG eyes were rarely reported. 20 , 21 Our group's clinical experience over the past 8 years with ab externo MAT has mirrored the high success rates of published studies, 11 , 12 , 13 , 14 , 15 , 24 and several paediatric glaucoma specialists consider it as their initial surgical treatment for PCG. 12 , 13 , 18 , 19 We hypothesized similar surgical outcomes between ab interno and ab externo approach for MAT and led to the first comprehensive comparison between the two approaches.
Our study found significant reductions in IOP and number of medications in PCG eyes with clear corneas treated using either the ab interno or ab externo approach, demonstrating similar success rates between groups. These results are consistent with previously reported outcomes for ab externo MAT in childhood glaucomas, 12 , 13 , 14 , 15 and comparable to the success rate of 360° suture trabeculotomy reported in the literature. 8 , 17 We observed a greater IOP lowering effect in eyes treated with 360° trabeculotomy compared to partial trabeculotomy. The higher success rate associated with a greater degree of angle surgery suggests that 360° trabeculotomy provides the best chance of successful IOP control, consistent with a previous study showing the superiority of 360° trabeculotomy compared to a limited trabeculotomy with a trabeculotome 13 , 19 or traditional goniotomy. 14 , 17 The similar rates of success in our groups likely reflects the finding that both groups treated similar amounts of anterior chamber angle.
Trabeculotomy or goniotomy as bleb‐less techniques are especially desirable in children who would otherwise be subject to a lifelong risk of blebitis and endophthalmitis. 25 Currently, the most common approach to circumferential trabeculotomy is ab externo, which requires an extensive conjunctival and scleral flap dissection and may diminish the success rate of future incisional surgeries if needed. Given this and the findings of our study, sparing the conjunctiva using an ab interno approach for MAT should be the first choice for PCG patients with clear corneas.
Both surgical destruction of Schlemm's canal and potential severe angle maldevelopment involving Schlemm's canal 26 , 27 , 28 , 29 account for the instances where the microcatheter could not be passed 360°, most frequently in eyes with prior surgery (52% compared to 16% in eyes without previous surgery). This may also explain why the IOP reduction in eyes without previous surgeries was higher, and the Cox regression survival analysis demonstrated that the number of previous surgeries contributed to surgical success. This suggests that the previous failed surgeries compromise the outcome of MAT, and the first surgery performed for PCG is extremely important. Additionally, eyes with multiple previous surgeries may generally represent more advanced disease.
Seventy‐four percent of our patients were male, supporting previous studies describing a male predominance in PCG, and 80% of patients had bilateral disease with a female predominance, similar to previous studies. 24 , 30 , 31 The higher prevalence of bilateral disease in girls may represent a tendency for girls to exhibit a more severe phenotype, which correlates with disease severity and difficult IOP control. 24 This gender difference may explain the moderately lower success rate and higher ratio of bilateral cases and number of postoperative medications in the ab externo MAT group. Further studies are warranted to further address the gender issue.
Hyphema was noted intraoperatively and on the first postoperative day in all subjects. This is a common postoperative complication following MAT possibly related to greater extent of tissue disturbance with circumferential treatment. 11 , 14 , 15 The hyphema was transient in most cases with only three patients requiring anterior chamber irrigation performed without sequelae. More eyes suffered from postoperative IOP spike in the ab interno MAT group. Although exact explanation for the IOP spike is under exploration, it is possible that retention of viscoelastic may account for the IOP spike in the ab interno MAT group, and small leakage through the scleral incision in the ab externo group may masked an IOP spike in the early postoperative stage in that group.
We know our study is limited by the retrospective nature of this study. However, given the low incidence of PCG, we believed that the non‐contemporary comparison with a moderately large sample could also have certain strength to reflect the non‐inferiority of ab interno MAT to ab externo MAT in PCG eyes with clear corneas, especially when the benefit of sparing the conjunctiva was considered. Of course, further prospective randomized controlled trials are also warranted to investigate these issues further. Also, follow‐up of our case series is limited by 12 months or less in this study. Ongoing follow up will provide more information in the future study.
In conclusion, both ab interno and ab externo approaches to MAT in patients with PCG and clear corneas provide good and similar outcomes. Given these findings, we recommend performing ab interno MAT as the initial procedure for PCG eyes with clear corneas. In addition, this study supported the superiority of 360° trabeculotomy compared to a limited trabeculotomy in a large cohort of PCG eyes, and suggests that successful trabeculotomy during the first attempt is critical to overall success and underscores the need for proficiency before independent practice.
CONFLICT OF INTEREST
None declared.
ACKNOWLEDGEMENTS
The authors would sincerely like to thank all patients and their parents for their participation and support in this study. The authors would like to thank Beijing Municipal Administration of Hospitals' Youth Programme and Beijing Municipal Science & Technology Commission for providing the grants for this study.
Shi Y, Wang H, Oatts J, et al. Ab interno vs ab externo microcatheter‐assisted trabeculotomy for primary congenital glaucoma with clear cornea. Clin Experiment Ophthalmol. 2020;48:1201–1209. 10.1111/ceo.13868
Yan Shi and Huaizhou Wang contributed equally as co‐first authors.
This study was registered at Chinese Clinical Trials Registry (ChiCTR1900023571) on June 2, 2019.
Funding information Beijing Municipal Administration of Hospitals’ Youth Programme, Grant/Award Number: QML20190203; Beijing Municipal Science & Technology Commission, Grant/Award Number: Z181100001718044
Contributor Information
Ying Han, Email: wningli@vip.163.com.
Ningli Wang, Email: wningli@vip.163.com.
REFERENCES
- 1. Broughton WL, Parks MM. An analysis of treatment of congenital glaucoma by goniotomy. Am J Ophthalmol. 1981;91(5):566‐572. [DOI] [PubMed] [Google Scholar]
- 2. Barkan O. Surgery of congenital glaucoma. Review of 196 eyes operated by goniotomy. Am J Ophthalmol. 1953;36(11):1523‐1534. [DOI] [PubMed] [Google Scholar]
- 3. Harms H, Dannheim R. Epicritical consideration of 300 cases of trabeculotomy ‘ab externo’. Trans Ophthalmol Soc U K. 1970;89:491‐499. [PubMed] [Google Scholar]
- 4. Akimoto M, Tanihara H, Negi A, Nagata M. Surgical results of trabeculotomy ab externo for developmental glaucoma. Arch Ophthalmol. 1994;112(12):1540‐1544. [DOI] [PubMed] [Google Scholar]
- 5. Anderson DR. Trabeculotomy compared to goniotomy for glaucoma in children. Ophthalmology. 1983;90(7):805‐806. [DOI] [PubMed] [Google Scholar]
- 6. Dietlein TS, Jacobi PC, Krieglstein GK. Prognosis of primary ab externo surgery for primary congenital glaucoma. Br J Ophthalmol. 1999;83(3):317‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ko F, Papadopoulos M, Khaw PT. Primary congenital glaucoma. Prog Brain Res. 2015;221:177‐189. [DOI] [PubMed] [Google Scholar]
- 8. Beck AD, Lynch MG. 360 degrees trabeculotomy for primary congenital glaucoma. Arch Ophthalmol. 1995;113(9):1200‐1202. [DOI] [PubMed] [Google Scholar]
- 9. Mcpherson SD, McFarland D. External trabeculotomy for developmental glaucoma. Ophthalmology. 1980;87(4):302‐305. [DOI] [PubMed] [Google Scholar]
- 10. John RL, Priscilla BB. A new trabeculotome. Am J Ophthalmol. 1969;68(3):430‐435. [DOI] [PubMed] [Google Scholar]
- 11. Sarkisian SR. An illuminated microcatheter for 360‐degree trabeculotomy [corrected] in congenital glaucoma: a retrospective case series. J AAPOS. 2010;14(5):412‐416. [DOI] [PubMed] [Google Scholar]
- 12. Shi Y, Wang H, Yin J, et al. Outcomes of microcatheter‐assisted trabeculotomy following failed angle surgeries in primary congenital glaucoma. Eye (Lond). 2016;31(1):132‐139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shi Y, Wang H, Yin J, et al. Microcatheter‐assisted trabeculotomy versus rigid probe trabeculotomy in childhood glaucoma. Br J Ophthalmol. 2015;100(9):1257‐1262. [DOI] [PubMed] [Google Scholar]
- 14. Girkin CA, Rhodes L, McGwin G, Marchase N, Cogen MS. Goniotomy versus circumferential trabeculotomy with an illuminated microcatheter in congenital glaucoma. J AAPOS. 2012;16(5):424‐427. [DOI] [PubMed] [Google Scholar]
- 15. Girkin CA, Marchase N, Cogen MS. Circumferential trabeculotomy with an illuminated microcatheter in congenital glaucomas. J Glaucoma. 2012;21(3):160‐163. [DOI] [PubMed] [Google Scholar]
- 16. Neely DE. False passage: a complication of 360° suture trabeculotomy. J AAPOS. 2005;9(4):396‐397. [DOI] [PubMed] [Google Scholar]
- 17. Mendicino ME, Lynch MG, Drack A, et al. Long‐term surgical and visual outcomes in primary congenital glaucoma: 360° trabeculotomy versus goniotomy. J AAPOS. 2000;4(4):205‐210. [DOI] [PubMed] [Google Scholar]
- 18. Temkar S, Gupta S, Sihota R, et al. Illuminated microcatheter circumferential trabeculotomy versus combined trabeculotomy‐trabeculectomy for primary congenital glaucoma: a randomized controlled trial. Am J Ophthalmol. 2015;159(3):490‐497. [DOI] [PubMed] [Google Scholar]
- 19. Neustein RF, Beck AD. Circumferential trabeculotomy versus conventional angle surgery: comparing long‐term surgical success and clinical outcomes in children with primary congenital glaucoma. Am J Ophthalmol. 2017;183:17‐24. [DOI] [PubMed] [Google Scholar]
- 20. Shi Y, Wang H, Yin P, et al. Six‐month outcomes of ab‐interno microcatheter‐assisted trabeculotomy in primary congenital glaucoma. Ophthalmol China. 2019;3:165‐168. [Google Scholar]
- 21. Grover DS, Smith O, Fellman RL, et al. Gonioscopy assisted transluminal trabeculotomy: an ab interno circumferential trabeculotomy for the treatment of primary congenital glaucoma and juvenile open angle glaucoma. Br J Ophthalmol. 2015;99(8):1092‐1096. [DOI] [PubMed] [Google Scholar]
- 22. Grover DS, Godfrey DG, Smith O, Feuer WJ, Montes de Oca I, Fellman RL. Gonioscopy‐assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology. 2014;121:855‐861. [DOI] [PubMed] [Google Scholar]
- 23. Beck ACT, Freedman S. Definition, classification and differential diagnosis in childhood glaucoma In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, eds. WGA Consensus Series‐9. Amsterdam: Kugler Publications; 2013:3‐10. [Google Scholar]
- 24. Shi Y, Wang H, Han Y, et al. Correlation between trabeculodysgenesis assessed by ultrasound biomicroscopy and surgical outcomes in primary congenital glaucoma. Am J Ophthalmol. 2018;196:57‐64. [DOI] [PubMed] [Google Scholar]
- 25. Haas J. Principles and problems of therapy in congenital glaucoma. Invest Ophthalmol. 1968;7(2):140‐146. [PubMed] [Google Scholar]
- 26. Walton DS, Katsavounidou G. Newborn primary congenital glaucoma: 2003 update. J Pediatr Ophthalmol Strabismus. 2005;42(6):333‐341. [DOI] [PubMed] [Google Scholar]
- 27. Perry LP, Jakobiec FA, Zakka FR, Walton DS. Newborn primary congenital glaucoma: histopathologic features of the anterior chamber filtration angle. J AAPOS. 2012;16(6):565‐568. [DOI] [PubMed] [Google Scholar]
- 28. Tawara A, Inomata H. Developmental immaturity of the trabecular meshwork in congenital glaucoma. Am J Ophthalmol. 1981;92(4):508‐525. [DOI] [PubMed] [Google Scholar]
- 29. Hollander DA, Sarfarazi M, Stoilov I, Wood IS, Fredrick DR, Alvarado JA. Genotype and phenotype correlations in congenital glaucoma: CYP1B1 mutations, goniodysgenesis, and clinical characteristics. Am J Ophthalmol. 2006;142(6):993‐1004. [DOI] [PubMed] [Google Scholar]
- 30. Mandal AK, Chakrabarti D. Update on congenital glaucoma. Indian J Ophthalmol. 2011;59(l1):148‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mandal AK, Naduvilath TJ, Jayagandan A. Surgical results of combined trabeculotomy‐trabeculectomy for developmental glaucoma. Ophthalmology. 1998;105(6):974‐982. [DOI] [PubMed] [Google Scholar]


