Abstract
Objective
The PULSE survey investigated contraceptive decision making, focusing on the use of long‐acting reversible contraceptives (LARCs) to determine reasons for their low adoption rates.
Methods
An online questionnaire was sent to women aged 18–49 years in 14 European countries who were considering starting or changing contraceptive method and asked questions based on four stages of contraceptive decision making: awareness, consideration, consultation, and adoption.
Results
Overall, 7221 women responded. LARC awareness was high (~73%) but current usage was low (11.3%). Only 24% of LARC‐aware women would consider switching to them. Factors associated with decision making differed depending on the stage: e.g. at the awareness phase, women were concerned with suitability, reversibility, and whether the method is hormonal; and at the consideration phase, the efficacy, convenience, and adverse‐effect profile were important. Healthcare professionals (HCPs) were the most trusted information source for women’s contraceptive decision making. LARCs were discussed less frequently during consultations than other contraceptives and HCPs may be perceived to hold negative opinions on LARCs.
Conclusion
A lack of knowledge about the features and benefits of LARCs can contribute to misconceptions and low adoption rates. HCPs play an important role in addressing this, as information conveyed during consultations influences women’s contraceptive choices.
Keywords: Contraception, Counseling, Informed decision making, Intrauterine contraception, Long‐acting reversible contraceptive, Misconception
Short abstract
European women are usually aware of long‐acting reversible contraceptives but often do not choose these methods, perhaps through misinformation about their effectiveness, suitability, and safety profile.
1. INTRODUCTION
Long‐acting reversible contraceptives (LARCs) include the hormonal and copper intrauterine devices and the contraceptive implant. These methods are highly effective, with annual pregnancy rates of less than 1% for women using LARCs, compared with 9% for oral contraceptives and 18% for condoms. 1 This is mainly due to the fact that these methods are independent of user compliance. LARCs are recommended by multiple guidelines 2 , 3 , 4 , 5 ; however, oral contraceptives and condoms remain the most popular methods of contraception in many countries. 6 , 7 Worldwide, the percentage of women of reproductive age using LARCs is estimated to be less than 14%. 8 The prevalence of LARC usage in Europe, as for the rest of the world, varies by country, with estimates in 2019 ranging between 2.9% for Poland and 16.0% for France. 8 The relatively low prevalence of LARC use may contribute to the high global rate of unplanned pregnancies, which has been estimated at 85 million per year, or approximately 40% of all pregnancies. 9 A US study showed that half of unplanned pregnancies were attributed to imperfect contraceptive adherence. 10 Unplanned pregnancy rates are generally highest among women younger than 25 years, who are more likely to be nulliparous and use user‐dependent contraception. 11 As well as the potential negative psychological impact on mother and child, 12 , 13 , 14 , 15 the economic consequences of unplanned pregnancy are considerable. In the USA in 2012, approximately 3.6 million pregnancies were unplanned, 9 and economic models estimated the associated annual medical costs at $4.5 billion. 10
Choosing a contraceptive method is a multi‐stage process. To consider using a contraceptive method, women first need to be aware of its existence, and indeed familiarity with a method has been linked to its subsequent use. 16 After gathering information regarding different methods of contraception, women consider which option could be most suitable for them based on factors such as contraceptive efficacy, hormone dose, and ease and duration of use, as well as suitability for individual lifestyle. 17 Following this, consultation with healthcare professionals (HCPs), friends, and family, ultimately leads to a contraceptive decision, with these external information and opinion sources often playing a key role in decision making. 11 , 18 The large international online PULSE survey was therefore designed to investigate the four main stages of contraceptive decision making (awareness, consideration, consultation, and adoption) with a focus on the use of LARCs to determine potential reasons for their low adoption rates.
2. METHODS
2.1. Questionnaire scope and development
The PULSE online birth‐control survey was conducted in Europe and South America by Epiphany RBC BV (Amsterdam, Netherlands). Here we present results from women from 14 European nations surveyed between May 19 and July 19, 2017.
The questionnaire was developed in English by Bayer AG (Berlin, Germany) in collaboration with Epiphany, who conducted the programming and logic testing. It was designed specifically to address the factors that influence the final decision on contraceptive choice: awareness, consideration, consultation, and adoption. After approval of the English version, the questionnaire was translated, and the translations were tested and corrected iteratively by native‐language speakers and Epiphany. Where multiple languages are spoken in the same nation, a translation language was chosen to ensure that the survey would be understood in all participating regions. All translations were based on the English questionnaire, and were conducted by GlobaLexicon (London, UK) to standardize procedures and quality‐control measures across the survey. For legal reasons, certain questions in the questionnaire were not posed to respondents in the Netherlands and in Switzerland. Programming logic was applied to ensure that participants were not asked questions that were irrelevant to them based on their responses to previous questions. An abridged version of the survey is presented in Table S1.
2.2. Participants
Eligible participants were women aged 18–49 years who were considering starting or changing birth‐control methods. To ensure that younger women were well represented in the survey, the enrollment target in Europe was to have 60% of participating women aged 18–29 years (younger group) and 40% aged 30–49 years (older group).
2.3. Recruitment and participation
Individuals were asked to join regional market‐research panels by Research Now (London, UK), either by open enrollment or targeted invitation. Signed consent was provided at the enrollment stage. Enrollment into a market‐research panel required a double opt‐in process, entailing completion of a registration form that included provision of agreement to all terms and conditions, followed by email verification of registration. Panel management (including all aspects of panel‐member engagement and data quality control) complied with industry standards endorsed by the European Society for Opinion and Market Research.
Research Now emailed survey‐questionnaire links to panel members inviting them to participate. The questionnaire could be accessed by tablet, smartphone, or desktop computer.
Depending on local laws, incentives such as vouchers, cash, gifts, or charitable contributions could be redeemed by panel members, based on points accrued for survey completion.
2.4. Data handling and analysis
Research Now had no access to survey data, which were stored by Epiphany. Epiphany employed proprietary software to exclude multiple responses returned by the same participant, and to exclude questionnaires completed too quickly to provide reliable data. Further data‐quality check procedures, such as screening for respondents who answered the same way for each question (straight‐lining) or poor‐quality answers to open‐ended questions, were applied when all data were collected.
Participant data were dichotomized by age group (younger or older group) and summarized descriptively at the European level. The subgroup of LARC combined data relating to intrauterine devices (referred to as copper and hormonal coils in the survey as these terms are more familiar to women) and contraceptive implants. Satisfaction was rated on a scale from 0 (not at all satisfied) to 10 (very satisfied). All responses were checked for descriptions of possible drug‐related adverse events and, where identified, the relevant pharmacovigilance bodies were informed.
A retrospective sensitivity power analysis (G*Power 3 19 ) was conducted following the close of the survey and demonstrated that with an α of 0.05, power of 0.80, and a sample of 7221 the survey was powered to detect very small effect sizes (Cohen’s w=0.03).
3. RESULTS
3.1. Survey population
The survey response rate was high overall, with some variation between countries (response rates 79%–96%). Responses from 7221 women were included in the analysis (Table 1). There were 4243 respondents (58.8%) in the younger group and 2978 respondents (41.2%) in the older group. Compared with older women, younger women were more likely to rely on others to help them make important decisions (47.1% versus 32.5%), felt they knew too little about contraception (31.0% versus 21.6%), and tended to worry more about unintended pregnancy (48.0% versus 32.9%) (Fig. 1A). In other respects, the profiles of the two age groups were similar.
Table 1.
Respondent characteristics.
| Characteristic, n (%) |
Respondents aged 18–29 years, n (%) (n=4243) |
Respondents aged 30–49 years, n (%) (n=2978) |
Total respondent population, n (%) (N=7221) |
|---|---|---|---|
| Age‐group, years | |||
| ≤19 | 61 (1.4) | 0 | 61 (0.8) |
| 20–29 | 4182 (98.6) | 0 | 4182 (57.9) |
| 30–39 | 0 | 1656 (55.6) | 1656 (22.9) |
| 40–49 | 0 | 1322 (44.4) | 1322 (18.3) |
| Country (N=7220) a | |||
| Austria | 302 (7.1) | 195 (6.5) | 497 (6.9) |
| Belgium b | 282 (6.6) | 217 (7.3) | 499 (6.9) |
| Denmark | 293 (6.9) | 214 (7.2) | 507 (7.0) |
| Finland | 293 (6.9) | 215 (7.2) | 508 (7.0) |
| France | 299 (7.0) | 198 (6.6) | 497 (6.9) |
| Germany | 337 (7.9) | 163 (5.5) | 500 (6.9) |
| Italy | 298 (7.0) | 202 (6.8) | 500 (6.9) |
| Netherlands | 300 (7.1) | 200 (6.7) | 500 (6.9) |
| Poland | 347 (8.2) | 247 (8.3) | 594 (8.2) |
| Portugal | 298 (7.0) | 318 (10.7) | 616 (8.5) |
| Spain | 302 (7.1) | 198 (6.6) | 500 (6.9) |
| Sweden | 298 (7.0) | 202 (6.8) | 500 (6.9) |
| Switzerland | 302 (7.1) | 200 (6.7) | 502 (7.0) |
| UK | 292 (6.9) | 208 (7.0) | 500 (6.9) |
| Highest level of education | |||
| Primary/secondary | 1985 (46.8) | 1240 (41.6) | 3225 (44.7) |
| Tertiary | 2258 (53.2) | 1738 (58.4) | 3996 (55.3) |
| Relationship status | |||
| In a steady relationship | 3149 (74.2) | 2317 (77.8) | 5466 (75.7) |
| Not in a steady relationship | 984 (23.2) | 584 (19.6) | 1568 (21.7) |
| Not disclosed | 110 (2.6) | 77 (2.6) | 187 (2.6) |
| Sexual‐activity status | |||
| Yes | 3188 (75.1) | 2229 (74.8) | 5417 (75.0) |
| No | 778 (18.3) | 559 (18.8) | 1337 (18.5) |
| Not disclosed | 277 (6.5) | 190 (6.4) | 467 (6.5) |
| Pregnancy intention | |||
| Currently pregnant | 186 (4.4) | 71 (2.4) | 257 (3.6) |
| Would like to have children in future | 2667 (62.9) | 714 (24.0) | 3381 (46.8) |
| Would not like to have children in future | 500 (11.8) | 1630 (54.7) | 2130 (29.5) |
| Unsure | 890 (21.0) | 563 (18.9) | 1453 (20.1) |
| Number of children | |||
| 0 | 3347 (78.9) | 1018 (34.2) | 4365 (60.4) |
| 1 | 555 (13.1) | 750 (25.2) | 1305 (18.1) |
| 2 | 280 (6.6) | 873 (29.3) | 1153 (16.0) |
| 3 | 49 (1.2) | 252 (8.5) | 301 (4.2) |
| 4 | 10 (0.2) | 56 (1.9) | 66 (0.9) |
| >4 | 2 (0.05) | 29 (1.0) | 31 (0.4) |
Country data missing for one respondent in the 30–49‐year age group.
Including Luxembourg.
Figure 1.

Respondent profiles. (A) Statements identified by respondents as representing them and their views (younger [n=4243] versus older [n=2978] group). (B) Current birth‐control methods. Note: Eight participants in the younger group and two participants in the older age group did not respond to this question.
The pill and condoms were used by 2577 younger respondents (60.9%) and 1323 older respondents (44.5%; Fig. 1B). There were 818 current LARC users (11.3%), and usage was proportionally greater in the older (14.8%) than in the younger group (8.9%). Approximately 20% of respondents (younger, 18.2%; older, 22.1%) used no birth control.
Both age groups were generally satisfied with their chosen method of contraception (mean score: older, 7.8; younger, 7.5), and overall satisfaction was numerically greater with LARCs than with the pill or condoms. Mean scores (older versus younger) were 8.5 versus 7.9 for LARCs, 7.9 versus 7.8 for the combined pill, and 6.9 versus 6.9 for condoms.
An overview of respondents’ awareness, consideration, consultation, and usage of LARCs is presented in Figure 2. Each stage will be discussed further below.
Figure 2.
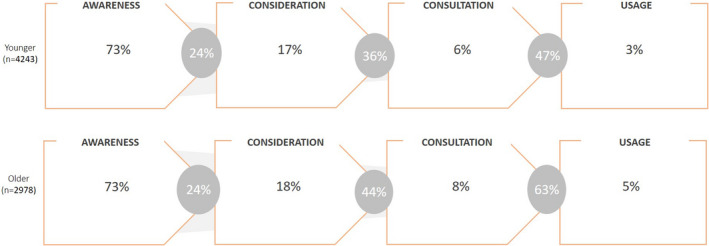
Rates of adoption of long‐acting reversible contraceptives (LARCs) among younger and older women. Boxes represent the overall proportion of either younger or older women surveyed who were aware of, considered, consulted with their healthcare professional (HCP) or used LARCs. Circles represent the proportion of women who progressed from one decision stage to the next, e.g. the proportion of women who were aware of LARCs who went on to consider them.
3.2. Awareness
With the exception of contraceptive injections and spermicide, the majority of respondents were aware of each of the birth‐control methods surveyed (Table 2). Awareness of LARCs was generally high (hormonal coil, 77.6%; copper coil, 76.1%; implant, 63.9%) and was similar in both younger and older groups. Highest overall levels of awareness of other birth‐control methods were for condoms (96.6%) and the morning‐after pill (91.1%) (Table 2).
Table 2.
Respondent aided awareness a of different birth‐control methods.
| Awareness of birth‐control method, n (%) |
Respondents aged 18–29 years, n (%) (n=4243) |
Respondents aged 30–49 years, n (%) (n=2978) |
Total respondent population, n (%) (N=7221) |
|---|---|---|---|
| Condom | 4101 (96.7) | 2877 (96.6) | 6978 (96.6) |
| Morning‐after pill | 3890 (91.7) | 2688 (90.3) | 6578 (91.1) |
| Sterilization/vasectomy | 3316 (78.2) | 2455 (82.4) | 5771 (79.9) |
| Hormonal coil | 3329 (78.5) | 2274 (76.4) | 5603 (77.6) |
| Copper coil | 3199 (75.4) | 2299 (77.2) | 5498 (76.1) |
| Natural methods | 3134 (73.9) | 2257 (75.8) | 5391 (74.7) |
| Mini‐pill | 3053 (72.0) | 2172 (72.9) | 5225 (72.4) |
| Combined pill | 3114 (73.4) | 2084 (70.0) | 5198 (72.0) |
| Ring | 3012 (71.0) | 1870 (62.8) | 4882 (67.6) |
| Cap/diaphragm | 2618 (61.7) | 2228 (74.8) | 4846 (67.1) |
| Patch | 2953 (69.6) | 1809 (60.7) | 4762 (65.9) |
| Implant | 2715 (64.0) | 1898 (63.7) | 4613 (63.9) |
| Injection | 2229 (52.5) | 1524 (51.2) | 3753 (52.0) |
| Spermicide | 1541 (36.3) | 1432 (48.1) | 2973 (41.2) |
| None of these | 8 (0.2) | 2 (0.1) | 10 (0.1) |
Participants were asked to select all the methods that they had heard of from a comprehensive list.
Knowledge of the characteristics of different birth‐control methods was also investigated (Fig. 3A). Most respondents (71.4%–74.7%, depending on the type of LARC) indicated that there was no need to think about LARCs every day. Nearly 70% of respondents (66.5%–69.6%) noted that LARCs offer long‐term protection against pregnancy, although many believed that placement of copper coils (55.4%) and hormonal coils (61.0%) would be a painful process. LARCs were regarded as suitable for women of different ages by 30.6%–35.3% of respondents, compared with 40.1% for the pill. Few respondents believed that LARCs could make periods less painful (≤22.2%) or improve skin conditions (≤10.9%), compared with 48.4% who associated these effects with the pill. A smaller proportion of respondents considered LARCs to be reversible at any time (25.9%–33.6%) compared with the pill (45.1%).
Figure 3.
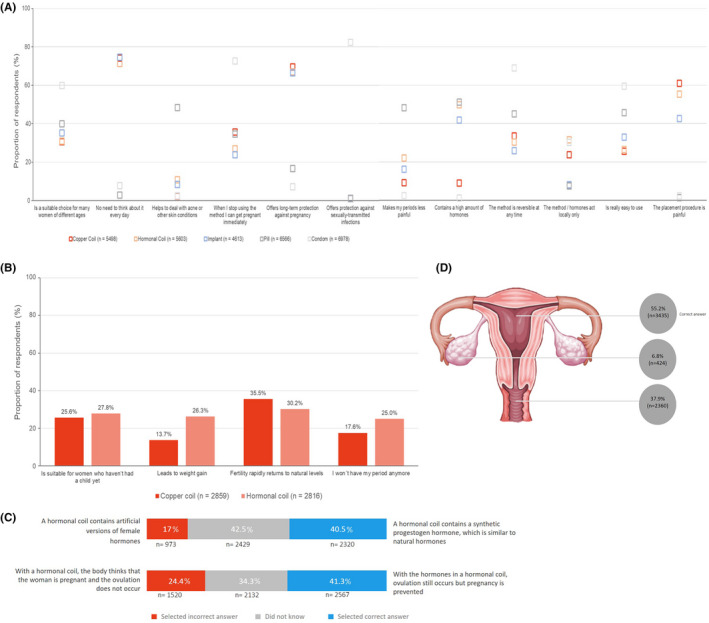
Respondent understanding of birth‐control methods. (A) Descriptors associated with different birth‐control methods. (B) Perceptions of copper and hormonal coils. (C) Perceptions of hormonal coils and their effects. (D) Perception of uterine placement of hormonal and copper coils (n=6219).
Among respondents who were aware of copper coils (n=2859) or of hormonal coils (n=2816), a greater proportion associated weight gain and amenorrhea with hormonal coils (26.3% and 25.0%, respectively) than with copper coils (13.7% and 17.6%, respectively; Fig. 3B). Fewer than half of respondents knew that synthetic hormones used in hormonal coils are similar to natural hormones (2320; 40.5%), and that hormonal coils act to prevent pregnancy without inhibiting ovulation (2567; 41.3%; Fig. 3C). Nearly half of respondents incorrectly identified where a coil is placed in the uterus (2784; 44.7%; Fig. 3D). Based on these responses, it was estimated that approximately 58% of respondents could be considered knowledgeable of birth control in general, with 18% of women being considered knowledgeable about hormonal and copper coils.
3.3. Consideration
Overall, despite relatively high levels of LARC awareness among the respondents, only 24% of individuals who knew about them would go on to consider them (Fig. 2). Consideration of LARCs was highest among women who were knowledgeable about these methods; for example, those who were aware that hormones contained in LARCs were similar to natural hormones, knew that ovulation still occurs with LARC methods, or believed that LARCs were a suitable choice for women of different ages (data not shown).
When asked which birth‐control method they might switch to in the future, respondents in the younger group mostly considered condoms (49.6%) or the combined pill (36.7%; Fig. 4). LARC usage was considered by similar proportions of older and younger respondents. Hormonal coils were considered slightly more often among older than younger respondents (21.3% versus 19.9%), copper coils slightly less often (15.8% versus 18.3%), and 14.7% of respondents in both groups had considered implants. Among those who had considered using a hormonal coil, the main reasons were convenience, longevity of action, local rather than systemic hormone exposure, and reduction in menstrual bleeding.
Figure 4.
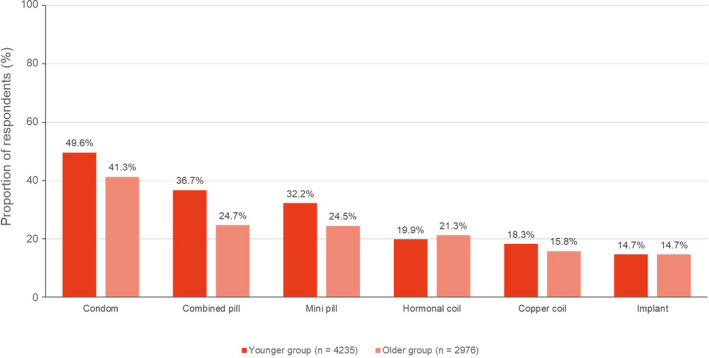
Birth‐control methods considered by respondents thinking of changing their contraception.
After effectiveness, convenience and a favorable side‐effect profile were regarded as the most important factors when selecting a birth‐control method, both overall and by LARC users (Fig. 5A). Lack of influence on the menstrual cycle was ranked fourth both overall and by LARC users, whereas low or no hormone exposure was ranked sixth overall and fifth among LARC users.
Figure 5.
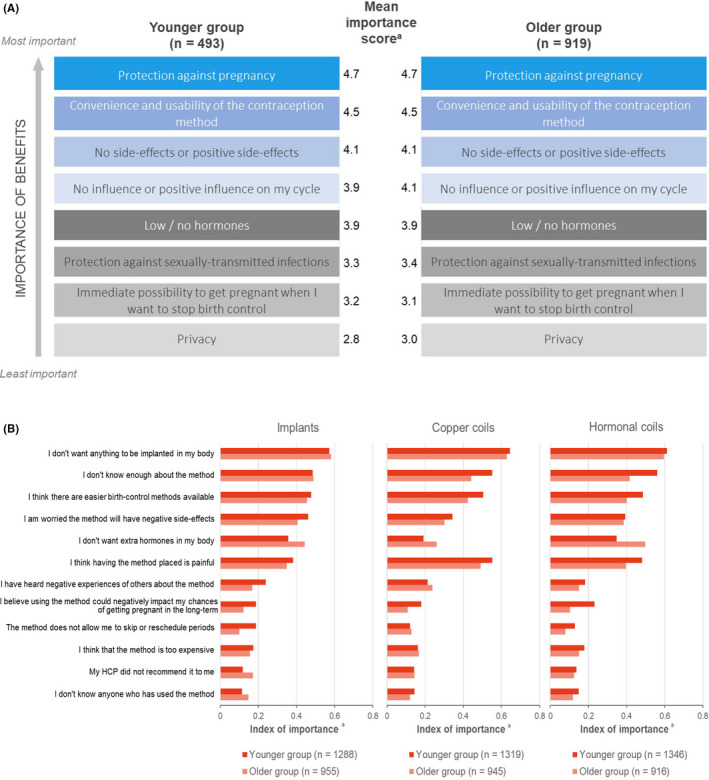
Factors influencing selection of birth‐control methods among long‐acting reversible contraceptive (LARC) users. (A) Relative importance of benefits associated with methods of birth control—importance was rated from 0 (not at all important) to 5 (very important). (B) Barriers to using implants, copper and hormonal coils—respondents ranked the criteria for importance, and the rankings were converted into an average index score of importance in the range 0–1 (0=least important; 1=most important).
When respondents ranked pre‐defined barriers to adoption of different birth‐control methods for importance, aversion to insertion and lack of knowledge were among the main reasons that discouraged respondents from using intrauterine contraception (Fig. 5B). For implants and hormonal coils, the older group perceived having extra hormones in their bodies as a more important barrier, and the younger group viewed pain during placement as more important.
Among 2091 respondents who would not consider using a hormonal coil, the main reason was to switch to hormone‐free methods, with 41% indicating that they did not want more hormones in their bodies. Concerns related to this were that hormones released by coils could adversely affect mood, libido, or fertility. Fear of pain during coil insertion was another factor. Of women who would not consider hormonal coils, copper coils and implants were considered by 11.9% and 10.7%, respectively.
3.4. Consultation
Approximately 36% of younger and 44% of older participants who were considering switching to LARCs actually went on to discuss them with their HCP (Fig. 2).
Overall, 4590 respondents (63.6%) had visited an HCP to discuss birth control, 1729 (23.9%) did not plan to visit an HCP for this reason, and the remainder (902; 12.5%) had not yet visited an HCP to discuss birth control but expressed an intention to do so. Respondents had most commonly discussed condoms, the combined pill, and the mini‐pill with an HCP, all more frequently in the younger than the older group (Fig. 6A). Hormonal coils were discussed with a greater proportion of older than younger respondents (11.9% versus 8.2%). Similar proportions in the older and younger groups discussed copper coils (7.1% versus 6.7%) and implants (4.3% versus 4.6%).
Figure 6.
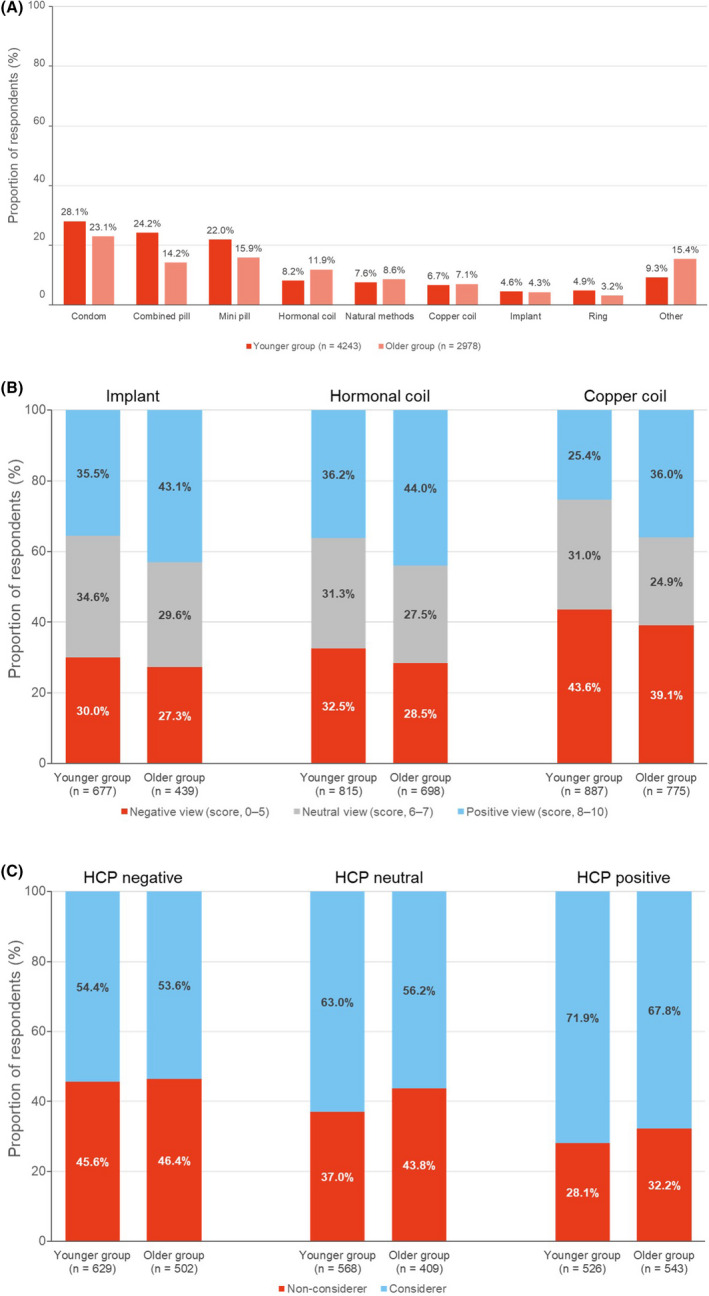
Educational role and influence of healthcare professionals (HCPs) in respondent choice of birth‐control methods. (A) Birth‐control methods discussed most commonly with HCPs. (B) Perception of HCP’s view when discussing types of long‐acting reversible contraceptive (LARC) for birth control. (C) Influence of HCP’s view on giving further consideration to LARCs for birth control.
When considering changing birth control methods, the information sources that both groups of respondents used most frequently were their gynecologist (592; 51.7%) or another HCP (524; 45.8%). Greater proportions of younger than older respondents sought information from friends and family (50.9% versus 33.0%), from online sources (non‐pharma websites, 27.0% versus 15.9%; pharma websites, 26.7% versus 10.6%; blogs, 27.6% versus 12.2%), or from flyers at their HCP’s office (26.3% versus 18.5%). Proportionally more of the older group felt that their HCP conveyed positive views about all three types of LARC than did the younger group (Fig. 6B).
Overall, similar proportions of respondents in each age group considered using LARCs, irrespective of their HCP’s opinion (Fig. 6C). However, among women already aware of LARCs in both age groups, having an HCP with negative or neutral rather than positive opinions about LARCs seemed to discourage approximately 13% of respondents from considering them further. Negative opinions about LARCs among HCPs who had been consulted by respondents in the younger group, related to pain during insertion, the unsuitability of the method for nulliparous women, and adverse effects, including a delayed ability to conceive after discontinuation.
3.5. Adoption
After consultation with their HCP, approximately 47% of younger participants and 63% of older participants went on to use a LARC method. Adoption of LARC methods was generally higher among women who were considered to be knowledgeable about LARCs (data not shown).
Among women who switched to LARCs, most previous users of the condom, combined pill, and mini‐pill chose the hormonal coil, whereas women who previously used the contraceptive ring mostly switched to the copper coil (data not shown).
On average, respondents switched to LARCs at approximately 29 years of age. The most common reason for doing so was to avoid pregnancy in the near‐term (Fig. S1). Nearly half of women who chose to use LARCs had not considered any other birth‐control methods.
4. DISCUSSION
Our findings show that a high percentage (73%) of women are aware of LARC methods, yet only 17%–18% of women would actually consider using them. Aided awareness of hormonal coils was slightly greater than that of either the combined or mini‐pill. Despite the high awareness, only one‐quarter of women would give LARCs further consideration as a form of birth control. Most women in the survey relied on condoms or oral contraceptives and it was notable how few women considered LARCs when switching to a different birth‐control method. It seems likely that this is a result of misconceptions, myths, and knowledge gaps regarding LARC methods. Our finding that only 18% of women could be considered knowledgeable about coils would seem to support this. Indeed, in the contraceptive CHOICE study, where all options were available at no cost and women were provided with comprehensive information regarding different long‐acting and short‐acting contraceptive methods and given the opportunity to address any knowledge gaps or misperceptions, the majority of women opted for a LARC. This shows the importance of ensuring women are able to access accurate and balanced information about a variety of contraceptive methods. 20
A common reason why respondents discounted hormonal coils and implants was the desire to use hormone‐free birth control, and indeed nearly half of women who discounted using a hormonal coil gave this reason, despite the very low systemic hormone levels associated with this method. Additionally, approximately 30% of these women (data not shown) were current users of the combined or mini‐pill, potentially indicating a lack of knowledge regarding the hormone content of different contraceptive methods. Other reasons women indicated for discounting LARC methods included concern about insertion pain, as well as possible adverse effects on return to fertility, which is a myth many respondents associated with hormonal and copper coils. Previous studies have reported, however, that intrauterine contraception has no effect on fertility once the method is stopped. 21 , 22
Women’s perceptions of LARCs in the PULSE study also suggested a lack of knowledge regarding these methods. Respondents generally considered that LARCs had no non‐contraceptive benefits such as reducing dysmenorrhea and menstrual bleeding. Many respondents also believed LARCs, particularly hormonal and copper coils, were only suitable for certain age groups, which is a common myth among women and some HCPs. 23 Importantly, age should not be a limiting factor in determining contraceptive choice, and guidance from WHO states that age alone does not constitute a medical reason for denying any contraceptive method to young women. 2
When women who were considering LARCs had the opportunity to discuss them with their HCP, approximately half subsequently went on to use these methods. However, despite women in both age groups being interested in LARCs, it was notable that they were often not among the top three methods discussed at such consultations (condom, combined pill, mini‐pill). Reasons for not discussing various contraceptive methods were not assessed in the PULSE survey, but a possible explanation may be that HCPs underestimate women’s interest in receiving information about LARCs and so do not include these methods in their counseling. 17 Additionally, the comfort and confidence a woman feels when speaking to her healthcare provider may play a role in their openness to have conversations about their requirements and opinions of a variety of birth control methods. 18 , 24
An important factor in the discounting of LARCs by women after consultation appears to be the perception that HCPs have of such methods. In this study and others, HCPs were found to be women’s most important source of information. 25 LARCs were discussed less often with women in the younger group than with women in the older group, and only 25%–36% of respondents in the younger group considered that their HCP viewed LARCs favorably. Those HCPs with negative views had raised concerns, including their suitability for nulliparous women, insertion pain, and delayed return to fertility after discontinuation. Such misconceptions might have an impact on counseling, and could prevent some women gaining access to LARCs. Balanced, patient‐centred counseling that educates about the effectiveness, adverse effects, and non‐contraceptive benefits of different options is central to addressing shortfalls in understanding and helping women find the contraceptive method that is right for them. 20 , 24 , 26
PULSE was the first survey of its kind to investigate the decision processes from initial awareness to final adoption of LARCs, looking into multiple factors that influence the final decision, rather than a single criterion, such as awareness. In addition, this was a large, multinational survey that recruited respondents using methods widely applied in market research to obtain a survey population broadly representative of the general public. It is, however, difficult to correlate self‐reported knowledge with actual knowledge of contraceptive methods using an online survey. Furthermore, identifying specific features of contraceptives with which respondents were satisfied or dissatisfied was not undertaken as part of this survey, and no in‐depth follow‐up interviews were conducted to explore issues in more detail. The potential for “online bias” should be noted, as only women who had access to a digital device were able to participate in the survey. As the survey was sponsored by Bayer, women who are unwilling to participate in industry‐sponsored research were naturally excluded—these women’s experiences may potentially differ from those of the women included in the PULSE survey.
In conclusion, unintended pregnancy rates are still high in Europe, despite the availability of a large variety of contraceptive methods. 8 , 27 Although they are among the most effective birth‐control methods, LARCs are not widely used. European women are usually aware of LARCs but are often poorly informed about their effectiveness, suitability, and safety profiles, leading them to consider other contraceptive methods in preference to LARCs. Comprehensive, unbiased contraceptive counseling by HCPs is essential to address this issue and to allow women to make informed choices regarding the contraception that best suits their needs as well as to increase access to these highly effective methods, which can have an impact on the rates of unintended pregnancy. 28
AUTHOR CONTRIBUTIONS
CC, SB, YE, and ML have all contributed to the development of the manuscript including data interpretation and critical review of content. SB generated figures and tables and has performed data quality checks against raw survey data.
CONFLICTS OF INTEREST
CC and YE are employees of Bayer AG. SB is an employee of Epiphany RBC BV, who conducted the survey with funding by Bayer AG. ML has participated in advisory boards for Bayer and Jenapharm, as well as given lectures and talks sponsored by Bayer and Jenapharm.
Supporting information
Fig. S1. Main reasons for switching to LARCs from another birth‐control method.
Table S1. Abridged PULSE Survey questionnaire
Acknowledgments
We would like to acknowledge Katja Wiggers (Bayer AG) for providing valuable insight into data interpretation. The authors would also like to acknowledge Highfield, Oxford, UK for providing medical writing assistance with funding from Bayer AG.
REFERENCES
- 1. Centers for Disease Control . Effectiveness of Family Planning Methods. https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/pdf/Contraceptive_methods_508.pdf. Accessed October 13, 2019.
- 2. World Health Organization . Selected Practice Recommendations for Contraceptive Use. Third Edition [WHO website]. 2016. http://www.who.int/reproductivehealth/publications/family_planning/SPR‐3/en/. Accessed October 13, 2019.
- 3. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice; Long‐Acting Reversible Contraception Working Group . ACOG Committee Opinion No. 450: Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2009;114:1434–1438. [DOI] [PubMed] [Google Scholar]
- 4. Black A, Guilbert E, Costescu D, et al. Canadian contraception consensus (Part 3 of 4): Chapter 7 – intrauterine contraception. J Obstet Gynaecol Can. 2016;38:182–222. [DOI] [PubMed] [Google Scholar]
- 5. Faculty of Sexual & Reproductive Healthcare . Clinical Effectiveness Unit. FSRH Clinical Guideline: Intrauterine Contraception. [2015, amended September 2019]. www.fsrh.org/pdfs/CEUGuidanceIntrauterineContraception.pdf. Accessed October 13, 2019.
- 6. Cibula D. Women’s contraceptive practices and sexual behaviour in Europe. Eur J Contracept Reprod Health Care. 2008;13:362–375. [DOI] [PubMed] [Google Scholar]
- 7. Kavanaugh ML, Jerman J. Contraceptive method use in the United States: Trends and characteristics between 2008, 2012 and 2014. Contraception. 2018;97:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. United Nations, Department of Economic and Social Affairs, Population Division . Contraceptive Use by Method 2019. https://www.un.org/en/development/desa/population/publications/pdf/family/ContraceptiveUseByMethodDataBooklet2019.pdf. Accessed May 29, 2020. [Google Scholar]
- 9. Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45:301–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: Potential savings with increased use of long‐acting reversible contraception. Contraception. 2013;87:154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Faustmann T, Crocker J, Moeller C, Engler Y, Caetano C, Buhling KJ. How do women and health care professionals view hormonal long‐acting reversible contraception? Results from an international survey. Eur J Contracept Reprod Health Care. 2019;24:422–429. [DOI] [PubMed] [Google Scholar]
- 12. McCrory C, McNally S. The effect of pregnancy intention on maternal prenatal behaviours and parent and child health: Results of an Irish cohort study. Paediatr Perinat Epidemiol. 2013;27:208–215. [DOI] [PubMed] [Google Scholar]
- 13. Hayatbakhsh MR, Najman JM, Khatun M, et al. A longitudinal study of child mental health and problem behaviours at 14 years of age following unplanned pregnancy. Psychiatry Res. 2011;185:200–204. [DOI] [PubMed] [Google Scholar]
- 14. Barton K, Redshaw M, Quigley MA, et al. Unplanned pregnancy and subsequent psychological distress in partnered women: A cross‐sectional study of the role of relationship quality and wider social support. BMC Pregnancy Childbirth. 2017;17:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bener A, Gerber LM, Sheikh J. Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: a major public health problem and global comparison. Int J Women Health. 2012;4:191–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Glaseir A, Scorer J, Bigrigg A. Attitudes of women in Scotland to contraception: A qualitative study to explore the acceptability of long‐acting methods. J Fam Plann Reprod Health Care. 2008;34:213–215. [DOI] [PubMed] [Google Scholar]
- 17. Merki‐Feld GS, Caetano C, Porz TC, Bitzer J. Are there unmet needs in contraceptive counselling and choice? Findings of the European TANCO Study. Eur J Contracept Reprod Health Care. 2018;23:183–193. [DOI] [PubMed] [Google Scholar]
- 18. Dehlendorf C, Levy K, Kelley A, et al. Women’s preferences for contraceptive counseling and decision making. Contraception. 2013;88:250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Faul F, Erdfelder E, Lang A‐G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. [DOI] [PubMed] [Google Scholar]
- 20. Secura GM, Allsworth J, Madden T, et al. The contraceptive CHOICE project: Reducing barriers to long‐acting reversible contraception. Am J Obstet Gynecol. 2010;203:115.e1–115.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Foran T, Butcher BE, Kovacs G, Bateson D, O’Connor V. Safety of insertion of the copper IUD and LNG‐IUS in nulliparous women: A systematic review. Eur J Contracept Reprod Health Care. 2018;23:379–386. [DOI] [PubMed] [Google Scholar]
- 22. Higgins JA, Ryder K, Skarda G, Koepsel E, Bennett EA. The sexual acceptability of intrauterine contraception: A qualitative study of young adult women. Perspect Sex Reprod Health. 2015;47:115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bitzer J, Abalos V, Apter D, et al. Targeting factors for change: Contraceptive counselling and care of female adolescents. Eur J Contracept Reprod Health Care. 2016;21:417–430. [DOI] [PubMed] [Google Scholar]
- 24. Bitzer J, Marin V, Lira M. Contraceptive counselling and care: A personalized interactive approach. Eur J Contracept Reprod Health Care. 2017;22:418–423. [DOI] [PubMed] [Google Scholar]
- 25. Spiedel JJ, Harper CC, Sheilds WC. The potential of long‐acting reversible contraception to decrease unintended pregnancy. Contraception. 2008;78:197–200. [DOI] [PubMed] [Google Scholar]
- 26. Dehlendorf C. Contraceptive counseling: Best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57:659–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. European Society of Human Reproduction and Embryology Capri Workshop Group . Why after 50 years of effective contraception do we still have unintended pregnancy? A European perspective. Hum Reprod. 2018;33:777–783. [DOI] [PubMed] [Google Scholar]
- 28. Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long‐acting reversible contraception. N Engl J Med. 2012;366:1998–2007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1. Main reasons for switching to LARCs from another birth‐control method.
Table S1. Abridged PULSE Survey questionnaire


