Abstract
Objectives
Theory suggests that individuals with higher neuroticism have more severe negative reactions to stress, though empirical work examining the interaction between neuroticism and stressors has yielded mixed results. The present study investigated whether neuroticism and other Big Five traits moderated the effects of recent stressful life events on older adults’ health outcomes.
Method
Data were drawn from the subset of Health and Retirement Study participants who completed a Big Five personality measure (N = 14,418). We used latent growth curve models to estimate trajectories of change in depressive symptoms, self-rated physical health, and C-reactive protein levels over the course of 10 years (up to six waves). We included Big Five traits and stressful life events as covariates to test their effects on each of these three health outcomes. We examined stressful life events within domains of family, work/finances, home, and health, as well as a total count across all event types.
Results
Big Five traits and stressful life events were independently related to depressive symptoms and self-rated health. There were no significant interactions between Big Five traits and stressful life events. C-reactive protein levels were unrelated to Big Five traits and stressful life events.
Discussion
Findings suggest that personality and stressful life events are important predictors of health outcomes. However, we found little evidence that personality moderates the effect of major stressful events across a 2-year time frame. Any heightened reactivity related to high neuroticism may be time-limited to the months immediately after a major stressful event.
Keywords: Mental health, Personality, Physical health, Stress reactivity, Stressful life events
Personality traits are consistent predictors of health outcomes across the life span (Hill & Roberts, 2016; Roberts, Kuncel, Shiner, Caspi, & Goldberg, 2007; Smith, 2006). The Big Five model includes five traits that capture meaningful variation in personality across individuals: neuroticism, extraversion, conscientiousness, agreeableness, and openness to experience (McCrae & Costa, 2008). Though not the only Big Five trait that is linked with health outcomes (see, e.g., Bogg & Roberts, 2004, on conscientiousness), neuroticism has been identified as one of the stronger personality predictors of health (Lahey, 2009). Neuroticism reflects the tendency to experience negative emotions including irritability, anxiety, and sadness. High neuroticism is associated with a range of detrimental health outcomes, including depressive symptoms (Hakulinen et al., 2015), chronic disease onset (Weston, Hill, & Jackson, 2015), and mortality (Roberts et al., 2007).
Despite robust evidence linking personality traits and health, the specific mechanisms driving such connections are not yet clear (Hampson, 2012; Iacovino, Bogdan, & Oltmanns, 2016; Smith, 2006). Lahey (2009) outlines a theoretical model with three working hypotheses to explain how neuroticism is associated with adverse outcomes. The first hypothesis, focused on overlapping genetic influences, suggests that correlations between neuroticism and mental health concerns can be explained by genetic variations that cause both trait neuroticism and mental disorders. The second hypothesis centers around stress generation: the idea that individuals high in neuroticism act in ways that increase their exposure to stress and decrease buffering resources like social support, resulting in worse life outcomes (see, e.g., Kendler, Gardner, & Prescott, 2003, and Iacovino et al., 2016, for evidence of stress generation via life experiences that are attributable to individuals’ behavior). The third hypothesis focuses on emotional reactivity. Consistent with a diathesis–stress model, this hypothesis suggests that individuals with high neuroticism have more severe reactions to stressful events, predisposing them to adverse outcomes in the context of stressful experiences. The present study focuses on this third hypothesis to better understand the degree to which older adults’ level of neuroticism affects their responses to major stressful life events (SLEs).
We focused specifically on the stress reactivity hypothesis for several reasons. First, the literature on neuroticism and stress reactivity includes important yet seemingly contradictory findings, as we discuss in more detail below. Second, neuroticism may interact differently with many possible manifestations of stress (e.g., severity, timing, type), and existing research has not fully explored this wide range of possibilities. Third, of Lahey’s (2009) three working hypotheses about the connections between neuroticism and health, stress reactivity is one that is relatively amenable to intervention. Many psychosocial interventions to promote older adults’ health are oriented toward improving responses to stress (e.g., Martire, Schulz, Helgeson, Small, & Saghafi, 2010), and a better understanding of the circumstances under which stress reactivity explains health outcomes may help to better target such therapies.
Prior studies exploring the interaction between neuroticism and stressors have yielded mixed results. Laboratory and daily diary studies, which examine short-term reactions to daily stressors, tend to support the hypothesis that neuroticism equates to greater reactivity (Bolger & Schilling, 1991; Gross, Sutton, & Ketelaar, 1998; Mroczek & Almeida, 2004; Suls & Martin, 2005). In contrast, longer-term studies examining major stressful events have found small and inconsistent effects of Big Five traits on responses to such events (e.g., Anusic, Yap, & Lucas, 2014; Hahn, Specht, Gottschling, & Spinath, 2015; Pai & Carr, 2010; Yap, Anusic, & Lucas, 2012). Despite theoretical and empirical links between neuroticism and stress reactivity, these longer-term studies of major stressful events provide little evidence for the hypothesized interaction. The present study contributes to this literature by testing whether Big Five traits, especially neuroticism, moderate the effect of a broad range of major SLEs on health outcomes in the context of a longitudinal, population-based study of older adults.
Major SLEs include potentially traumatic events (such as exposure to violence and natural disasters), as well as events that reflect significant and stressful changes in one’s life (such as bereavement or job loss; Hatch & Dohrenwend, 2007; Holmes & Rahe, 1967). SLEs increase the risk of developing major depression (Kendler, Karkowski, & Prescott, 1999), and some evidence also suggests that SLEs are prospectively related to the onset of chronic physical health conditions (e.g., Renzaho et al., 2014). Major SLEs are common in later life (Ogle, Rubin, Berntsen, & Siegler, 2013), as events such as spousal bereavement, retirement, and the onset of chronic health conditions are associated with advancing age.
The present study extends prior research on personality–SLE interactions by applying a highly inclusive approach to measuring SLEs. We use longitudinal data on a wide variety of SLEs such as bereavement, retirement, job loss, and health transitions among others. Whereas past research has tended to examine different types of SLEs in isolation (e.g., examining the independent effects of retirement or divorce; Anusic et al., 2014; Hahn et al., 2015; Pai & Carr, 2010; Yap et al., 2012), the present study aggregates SLEs across event types. This allows us to examine the accumulation of SLEs over a given time frame (in this case, 2-year intervals). The effects of traumatic events accumulate over time following a dose–response pattern, with multiple traumatic events predicting negative outcomes more strongly than a single, discrete event (e.g., Ogle, Rubin, & Siegler, 2014). Similarly, neuroticism and other Big Five traits may have stronger interactions with SLEs as they accumulate within a relatively short period. Recognizing that the type of event may also matter, we further examine interactions with specific domains of SLEs (i.e., work/financial, family, health, and home-related events).
Expanding on prior research in this area, we investigate multiple health outcomes concurrently. Specifically, we test whether Big Five traits moderate the effects of SLEs on depressive symptoms, self-rated physical health (SRH), and C-reactive protein levels (CRP; a biomarker capturing systemwide inflammation). Depressive symptoms are associated with both neuroticism and stress (e.g., Hutchinson & Williams, 2007; Kendler, Kuh, & Prescott, 2004), and are a relevant mental health concern in later life (Sutin et al., 2013). A range of physical health issues may arise during the course of aging, so we also included measures that reflect overall health status. Self-rated physical health represents a broad, subjective evaluation of health status, and correlates strongly with objective physical health markers (e.g., Idler & Benyamini, 1997). CRP is a marker of allostatic load, or “wear and tear” on the body at a systemwide level, which is exacerbated by exposure to stress (Juster, McEwen, & Lupien, 2010). Collectively, these outcomes reflect both mental and physical health, and make use of both subjective and objective measures.
We had two primary research questions. First, is exposure to later-life stressful events associated with decreasing health trajectories? Based on prior research linking SLEs to our focal health outcomes, we expected that recent SLEs would be associated with subsequent increases in depressive symptoms (e.g., Hammen, 2005), decreases in SRH (e.g., Ullman & Siegel, 1996), and increases in CRP (Lin, Neylan, Epel, & O’Donovan, 2016). Second, do baseline personality traits moderate the association between SLEs and health trajectories? We expected neuroticism to moderate the effects of SLEs on health, with higher neuroticism predicting steeper increases in depressive symptoms and CRP, and steeper decreases in SRH, in the context of SLEs.
Method
Participants and Procedure
The present study used data from the Health and Retirement Study (HRS), a national longitudinal study of older adults in the United States (Sonnega et al., 2014). The original cohort was recruited in 1992 and included individuals ages 51–61 and their spouses. Participants completed the HRS core interview (an in-person or telephone survey) every 2 years. This core interview included measures of depressive symptoms and SRH. In addition, participants completed a leave-behind questionnaire (LBQ) starting in 2006. Half of the sample (Cohort 1) were randomly selected to complete the survey in 2006, 2010, and 2014, while the other half (Cohort 2) completed the survey in 2008, 2012, and 2016. We drew scores for Big Five traits from the first wave when participants completed the LBQ. Biomarkers, including CRP, were collected on the same schedule as the LBQ via saliva and blood samples. Major SLEs were assessed through the core interview and the LBQ, as described in detail in the Measures section.
Participants who completed the LBQ (N = 14,418) in 2006 or 2008 were included in the present study. In terms of demographics, 59% of the sample were women, 83% were White/Caucasian, 13% were Black/African American, and 4% Other. The average age was 67.8 (SD = 10.4) years in 2006. Wealth was assessed as total assets minus all debts, with a mean of $513,424, SD of $1,319,986, and median of $210,350. About half of participants (54%) had a high school diploma or equivalent, 19% had less than a high school degree, and 22% had a Bachelor’s degree or higher. The intraclass correlation for depressive symptoms and SRH between Cohort 1 and Cohort 2 was <0.001, and the confidence interval for each wave included 0. Thus, we combined both cohorts into one sample. Because CRP data were only available through 2014, we restricted CRP analyses to Cohort 1, who were assessed three times (allowing estimation of linear trajectories). Correlations among the variables are reported in Table 1.
Table 1.
Correlations Among Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | ||||||||||||||||||
| 2. Education | −0.08 | |||||||||||||||||
| 3. Race | 0.04 | −0.14 | ||||||||||||||||
| 4. Age | −0.04 | −0.14 | −0.10 | |||||||||||||||
| 5. Wealth | −0.04 | 0.21 | −0.11 | 0.01 | ||||||||||||||
| 6. MIDI—E | 0.09 | 0.06 | 0.04 | −0.05 | 0.04 | |||||||||||||
| 7. MIDI—A | 0.26 | 0.02 | <0.01 | −0.03 | −0.01 | 0.57 | ||||||||||||
| 8. MIDI—C | 0.09 | 0.18 | −0.05 | −0.10 | 0.08 | 0.41 | 0.44 | |||||||||||
| 9. MIDI—N | 0.09 | −0.11 | −0.04 | −0.11 | −0.04 | −0.23 | −0.13 | −0.25 | ||||||||||
| 10. MIDI—O | <0.01 | 0.28 | 0.01 | −0.13 | 0.09 | 0.55 | 0.42 | 0.47 | −0.20 | |||||||||
| 11. Previous SLE | −0.05 | −0.09 | −0.02 | 0.18 | −0.02 | −0.02 | <0.01 | −0.08 | 0.03 | −0.02 | ||||||||
| 12. W2 SLE | 0.01 | −0.09 | 0.04 | 0.06 | −0.05 | −0.03 | <0.01 | −0.08 | 0.07 | −0.03 | 0.10 | |||||||
| 13. W3 SLE | 0.02 | −0.04 | 0.03 | <0.01 | −0.04 | <0.01 | 0.01 | −0.03 | 0.05 | −0.01 | 0.10 | 0.05 | ||||||
| 14. W4 SLE | 0.02 | −0.04 | 0.02 | −0.04 | −0.03 | 0.01 | 0.03 | <0.01 | 0.03 | 0.01 | 0.06 | 0.10 | 0.12 | |||||
| 15. W5 SLE | 0.03 | −0.04 | 0.05 | −0.04 | −0.03 | 0.03 | 0.03 | 0.01 | 0.03 | 0.02 | 0.04 | 0.03 | 0.11 | 0.16 | ||||
| 16. W6 SLE | 0.03 | <0.01 | 0.04 | −0.12 | 0.01 | 0.04 | 0.03 | 0.03 | 0.02 | 0.04 | 0.01 | 0.01 | 0.07 | 0.12 | 0.18 | |||
| 17. 2006 DEP | 0.11 | −0.21 | 0.09 | −0.02 | −0.10 | −0.19 | −0.05 | −0.20 | 0.38 | −0.14 | 0.13 | 0.14 | 0.08 | 0.07 | 0.04 | 0.03 | ||
| 18. 2006 SRH | −0.01 | 0.30 | −0.13 | −0.13 | 0.14 | 0.22 | 0.10 | 0.26 | −0.23 | 0.22 | −0.24 | −0.18 | −0.09 | −0.08 | −0.04 | 0.02 | −0.41 | |
| 19. 2006 CRP | <0.01 | 0.06 | −0.08 | −0.02 | 0.09 | 0.05 | −0.01 | 0.02 | −0.04 | 0.01 | −0.06 | −0.15 | −0.11 | −0.15 | −0.18 | −0.23 | −0.02 | 0.05 |
Note. MIDI = Midlife Development Inventory; E = extraversion; A = agreeableness; C = conscientiousness; N = neuroticism; O = openness; SLE = stressful life events; DEP = depressive symptoms; SRH = self-rated health; CRP = C-reactive protein. Nonsignificant correlations are italicized. Only 2006 measurements for depressive symptoms, self-rated health, and CRP are presented, for space considerations.
Project materials, including preregistration and analysis scripts are available at https://osf.io/3sqc7. A table detailing the authors’ previous exposure to the data is provided in Supplementary Table S1. The study was determined exempt from review by the Minneapolis VA IRB, project number VAM-19-00453.
Missing data
We included assessments of health outcomes and life events from the six waves of the study between 2006 and 2016. Of the 14,418 participants, 93% were retained in 2008, 82% in 2010, 76% in 2012, 68% in 2014, and 58% in 2016. Compared to those who dropped out, participants who remained in the study through 2016 had higher levels of education, were relatively younger, had more wealth, and were higher on extraversion, agreeableness, openness, and slightly lower on neuroticism. Women and White/Caucasian individuals were overrepresented among those who remained in the study (see Supplementary Table S2). To handle missing data on the outcomes, we used Full Information Maximum Likelihood (FIML) estimation.
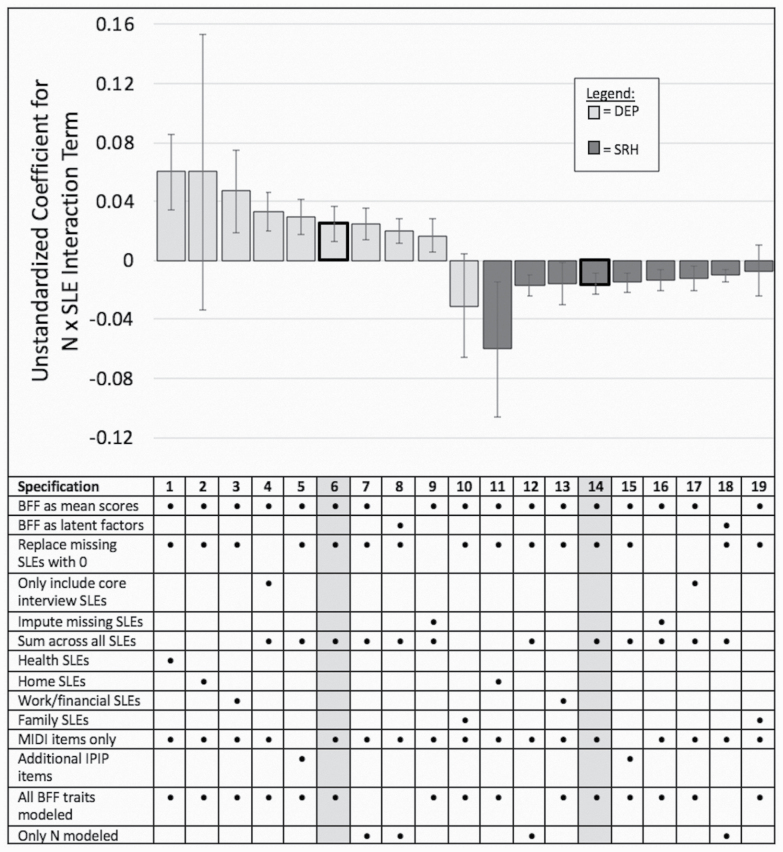
For handling missing data within SLE variables, we compared three different approaches. For the first approach, we assigned a score of “0” for any missing SLE variables (i.e., assuming that a missing response indicated the event did not occur). Noting that much of the missingness in SLEs appears to be a result of participants not completing the LBQ, our second approach focused our analysis only on the events assessed in the core interview. For our third approach, we used multiple imputation to estimate the number of SLEs for participants who were missing data on SLEs assessed via the LBQ. The implications of these three missing data approaches are summarized in Figure 1 and Supplementary Figure S1.
Figure 1.
Alternative specifications for depressive symptom and self-rated health models. Note. Preferred specifications (6 and 14) are shaded in gray in the table. Error bars represent standard errors. BFF = Big Five Factors; SLE = stressful life event; LBQ = leave-behind questionnaire; IPIP = International Personality Item Pool; N = neuroticism; DEP = depressive symptoms; SRH = self-rated health. C-reactive protein (CRP) is not depicted because standard errors are large relative to other outcomes and interfere with the interpretability of the figure. A separate, analogous figure for CRP is available in Supplementary Figure S1. In the preferred specifications, the p-value for the N × SLE interaction is p = .03 for depressive symptoms and p = .03 for self-rated health.
Measures
Personality
Big Five traits were assessed using the Midlife Development Inventory (MIDI; Lachman & Weaver, 1997), a personality assessment designed for use in large panel surveys of adults. The scale lists 26 adjectives, and participants are asked to rate how well each describes them on a scale from 1 (not at all) to 4 (a lot). There are four items for extraversion, five for agreeableness, five for conscientiousness, four for neuroticism, and seven for openness. For our main analyses, we took the mean of each subscale as the score for each trait. Reliabilities ranged from alpha = 0.66 to alpha = 0.79 across the five subscales.
Stressful life events
The HRS contains several survey questions that correspond to events listed on frequently used SLE checklists (e.g., Holmes & Rahe, 1967). Informed by such checklist approaches, we sought to include the broadest range of SLEs as possible. This would maximize detection of multiple stressors accumulating between study waves. The following events were assessed via the core interview: spouse died, began receiving Medicaid, entered poverty, parent died, parent-in-law died, cancer diagnosis, spouse’s cancer diagnosis, entered nursing home, retired, married, divorced, hospitalized, and heart attack. Participants whose indicated that they experienced one of these events within the 2 years prior to the interview were coded as “1.” The following events were assessed via the LBQ, which asked whether any of the following events had occurred within the last 5 years, and if so, what year: involuntary job loss; unemployed longer than 3 months; anyone in the household was unemployed longer than 3 months; moved to worse residence or neighborhood; robbed or burglarized; fraud victimization; death of a child; natural disaster; combat exposure; a family member was addicted to drugs or alcohol; physically attacked; life-threatening illness or accident; spouse or child had a life-threatening illness or accident. Participants who indicated that an event occurred within 2 years prior to any wave were coded with a “1” for that event in the appropriate wave. See Supplementary Table S3 for SLE frequencies.
We used two different strategies for aggregating SLEs, including an examination of the overall effects of SLEs (regardless of event type), as well as SLEs by domain. For the first strategy, we followed Musliner et al.’s (2015) approach and first determined which events were significantly associated with each outcome. Among the significantly associated events, we tallied the number that occurred in the 2-year period before each wave. Because health-related SLEs are likely highly endogenous with physical health outcomes, we excluded health-related SLEs when analyzing SRH and CRP.
For the second strategy, following prior research that sorts stressors by domain (e.g., Neupert, Almeida, & Charles, 2007), we sorted events into four domains determined a priori: health stressors (heart attack, cancer, nursing home, hospitalization), work/financial stressors (job loss, unemployment, anyone in household unemployed, fraud, Medicaid, poverty, and retirement), family stressors (death of spouse, parent, or parent-in-law, marriage, divorce, spouse’s cancer, spouse or child addicted, spouse or child life-threatening illness or accident), and home stressors (moved, burglarized). Separate sum scores were calculated for each domain.
All events reported between 1992 and 2006 were tallied to obtain a count of SLEs prior to the current study period. This sum score was included as a covariate to control for the effects of previous SLEs.
Depressive symptoms
Depressive symptoms were measured every 2 years using an 8-item version of the Center for Epidemiological Studies-Depression scale (CES-D; Radloff, 1977). Participants were asked to focus on the past week, and respond to binary (0 = no, 1 = yes) items. A sample item is, “Much of the time during the past week, you felt that everything you did was an effort.” We calculated a mean score across all items; alpha ranged from 0.80 to 0.81 across the six waves.
Self-rated health
Self-rated health was assessed in all six waves between 2006 and 2016 with the item: “Would you say your health is excellent, very good, good, fair, or poor?” Responses were coded so that 5 = excellent, 1 = poor.
C-reactive protein
Blood spots were collected from Cohort 1 in 2006, 2010, and 2014. The overall completion rates in 2006 and 2010 were 81% and 84%, respectively. In 2006 CRP was assayed by the University of Vermont and high-sensitivity CRP (hsCRP) was assayed by the University of Washington using standard enzyme-linked immunosorbent assays (ELISA). In 2010 hsCRP was assayed by the University of Washington using ELISA. Completion rates and assay sites have not been released for the 2014 data.
Analysis Plan
We tested our hypotheses using latent growth curve modeling (LGM; Singer & Willett, 2003). LGM is a longitudinal structural equation modeling technique used to estimate latent parameters that describe a trajectory of change over time. We developed a separate model for each outcome. First, we fit unconditional models to test functional forms, including intercept-only, linear, and quadratic forms. We compared model fit using fit statistics and visual inspection of the plots of estimated and sample means, selecting the functional form with the best overall fit. Lower Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) values, root mean square error of approximation (RMSEA) values less than 0.06, standardized root mean square residual (SRMR) values less than 0.08, and comparative fit index (CFI) values greater than 0.95 were considered indicators of good fit (Hu & Bentler, 1999).
We then added covariates to the best-fitting unconditional model. Demographics, previous SLEs, and Big Five trait scores were added as time-invariant predictors. The count of recent (i.e., within the past 2 years) SLEs and interaction terms for each Big Five trait crossed with recent SLEs were added as time-varying covariates. Age, wealth, education level, and Big Five traits were mean-centered; values for wealth were also divided by 1,000,000 to facilitate computation. Because race was not a focus of the present study, it was transformed to a binary variable (0 = White/Caucasian, 1 = Black/African American or Other). Because the distribution of CRP scores was highly skewed, we used log-transformed CRP scores. A sample diagram for the preferred specification (i.e., the model specification that was the primary focus of our preregistered analysis plan) is included in Supplementary Figure S2. For our final models, we applied the Holm correction (Holm, 1979) to control for family-wise error.
We conducted sensitivity analyses to examine the robustness of our results to various analytic decisions. As detailed above, we tested three different approaches to handling missing SLE data, and two approaches to aggregating SLEs. Furthermore, we tested whether a measurement model using trait items as indicators for latent trait scores yielded different findings. We also incorporated additional neuroticism items and conscientiousness items into our Big Five measures. These items were drawn from the International Personality Item Pool (IPIP; Goldberg et al., 2006), and were included in some versions of the LBQ to supplement the MIDI. Finally, we tested whether modeling neuroticism alone, rather than all of the Big Five, affected the findings. Each of the alternative model specifications, and the effect sizes they produced for the N × SLE interaction, are catalogued in Figure 1, and in Supplementary Tables S4–S8.
Finally, we investigated the importance of SLE recency through exploratory analyses focused on spouse death. Because this SLE was measured with a precise date, we could calculate the exact number of days between the HRS interview and the spouse’s death. We compared the effects of a death within the past 90 days versus the past 2 years.
Results
Unconditional Growth Models
Fit statistics for unconditional models are reported in Table 2. All coefficients are unstandardized. The unconditional model for depressive symptoms indicated a shallowly curved, upward trajectory that began at a level between one and two symptoms and increased slightly over time (I = 1.43, p < .001; S = −0.02, p = .03; Q = 0.007, p = .001). For SRH, a linear model fit best, suggesting that participants on average started with a score corresponding to “good” with slight linear decreases over time (I = 3.20, p < .001; S = −0.06, p = .03). For CRP, the linear growth model produced a negative variance estimate. The constant (i.e., intercept-only) model provided good fit based on fit statistics and visual inspection of the means, so this functional form was retained. On average, participants had a stable level of CRP (I = 4.13, p < .001).
Table 2.
Fit Indices for Latent Growth Curve Models
| Model | AIC | BIC | Chi square | RMSEA [CI] | CFI | SRMR |
|---|---|---|---|---|---|---|
| DEP: Unconditional constant | 254,265 | 254,326 | χ 2 = 631.63, df = 19, p < .001 | 0.048 [0.044, 0.051] | 0.98 | 0.032 |
| DEP: Unconditional linear | 253,814 | 253,897 | χ 2 = 174.50, df = 16, p < .001 | 0.026 [0.023, 0.030] | 0.99 | 0.020 |
| DEP: Unconditional quadratic | 253,722 | 253,835 | χ 2 = 74.97, df = 12, p < .001 | 0.019 [0.015, 0.023] | 0.99 | 0.013 |
| DEP: Preferred specification | 245,125 | 245,532 | χ 2 = 739.99, df = 219, p < .001 | 0.013 [0.012, 0.014] | 0.98 | 0.009 |
| SRH: Unconditional constant | 174,644 | 174,704 | χ 2 = 2700.40, df = 19, p < . 001 | 0.099 [0.096, 0.102] | 0.94 | 0.057 |
| SRH: Unconditional linear | 172,305 | 172,388 | χ 2 = 355.32, df = 16, p < .001 | 0.038 [0.035, 0.042] | 0.99 | 0.025 |
| SRH: Unconditional quadratic | 172,089 | 172,202 | χ 2 = 131.21, df = 12, p < .001 | 0.026 [0.022, 0.030] | 0.99 | 0.010 |
| SRH: Preferred specification | 164,910 | 165,190 | χ 2 = 679.46, df = 230, p < .001 | 0.012 [0.011, 0.013] | 0.99 | 0.006 |
| CRP: Unconditional constant | 103,128 | 103,162 | χ 2 = 24.34, df = 4, p < .001 | 0.028 [0.018, 0.039] | 0.95 | 0.022 |
| CRP: Preferred specification | 103,008 | 103,151 | χ 2 = 109.86, df = 54, p < .001 | 0.013 [0.009, 0.016] | 0.91 | 0.007 |
Note. CRP = C-reactive protein; DEP = depressive symptoms; SRH = self-rated health.
Conditional Growth Models
Our preferred specification indicated that all Big Five traits were significantly associated with depressive symptoms (see Table 3). Higher neuroticism, agreeableness, and openness as well as lower extraversion and conscientiousness were each associated with a higher intercept. Among these, neuroticism had the strongest effect. Each additional SLE was associated with a 0.12 increase in the number of depressive symptoms in the subsequent wave. The interaction term for neuroticism and SLEs was small (B = 0.03, p = .03) and nonsignificant after the Holm correction. When examining events by domain, family, work/financial, and health-related events each predicted increased depressive symptoms in the subsequent wave (see Table 4).
Table 3.
Models Predicting Health Outcomes on Big Five Traits and SLEs
| Depressive symptoms | Self-rated health | CRP | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | Coefficient | SE | Coefficient | SE | |
| Fixed effects for time-invariant covariates | ||||||
| For intercept | ||||||
| Intercept | 0.91*** | 0.03 | 3.52*** | 0.01 | 3.23*** | 0.18 |
| Extraversion | −0.54*** | 0.04 | 0.34*** | 0.02 | −0.41 | 0.22 |
| Agreeableness | 0.24*** | 0.04 | −0.16*** | 0.02 | 0.25 | 0.25 |
| Conscientiousness | −0.32*** | 0.04 | 0.28*** | 0.02 | −0.45 | 0.23 |
| Neuroticism | 1.02*** | 0.03 | −0.30*** | 0.01 | −0.12 | 0.16 |
| Openness | 0.18*** | 0.03 | −0.03 | 0.02 | 0.02 | 0.21 |
| For linear slope | ||||||
| Intercept | 0.001 | 0.02 | −0.08*** | 0.003 | — | — |
| Extraversion | 0.06 | 0.03 | −0.02*** | 0.004 | — | — |
| Agreeableness | 0.01 | 0.03 | 0.01 | 0.005 | — | — |
| Conscientiousness | −0.07 | 0.03 | −0.006 | 0.005 | — | — |
| Neuroticism | −0.05 | 0.02 | 0.01** | 0.003 | — | — |
| Openness | −0.01 | 0.03 | −0.001 | 0.004 | — | — |
| For quadratic slope | ||||||
| Intercept | 0.004 | 0.004 | — | — | — | — |
| Extraversion | −0.01 | 0.005 | — | — | — | — |
| Agreeableness | −0.004 | 0.006 | — | — | — | — |
| Conscientiousness | 0.01 | 0.005 | — | — | — | — |
| Neuroticism | 0.004 | 0.004 | — | — | — | — |
| Openness | 0.001 | 0.005 | — | — | — | — |
| Fixed effects for time-varying covariates | ||||||
| Recent SLEs | 0.12*** | 0.007 | −0.02*** | 0.004 | 0.09 | 0.13 |
| Extraversion × SLEs | <0.001 | 0.02 | 0.01 | 0.01 | 0.18 | 0.32 |
| Agreeableness × SLEs | 0.007 | 0.02 | −0.02 | 0.01 | 0.42 | 0.36 |
| Conscientiousness × SLEs | −0.001 | 0.02 | −0.003 | 0.01 | −0.12 | 0.33 |
| Neuroticism × SLEs | 0.03 | 0.01 | −0.02 | 0.007 | 0.22 | 0.21 |
| Openness × SLEs | −0.02 | 0.02 | 0.005 | 0.01 | 0.24 | 0.29 |
| Random effects | ||||||
| Intercept | 1.47*** | 0.05 | 0.57*** | 0.01 | 17.52*** | 1.02 |
| Slope | 0.18*** | 0.03 | 0.01*** | 0.001 | — | — |
| Quadratic slope | 0.004*** | 0.001 | — | — | — | — |
Note. CRP = C-reactive protein; SLEs = stressful life events.
***p < .001. **p < .01. *p < .05. Indicators of statistical significance account for the Holm correction for family-wise error.
Table 4.
Fixed Effects of SLEs on Health Outcomes, by Event Domain
| Depressive symptoms | Self-rated health | CRP | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | Coefficient | SE | Coefficient | SE | |
| Family events | ||||||
| Recent SLEs | 0.18*** | 0.02 | −0.004 | 0.01 | 0.04 | 0.20 |
| Extraversion × SLEs | −0.007 | 0.05 | 0.02 | 0.02 | −0.26 | 0.49 |
| Agreeableness × SLEs | 0.10 | 0.06 | −0.02 | 0.03 | 1.13 | 0.53 |
| Conscientiousness × SLEs | −0.04 | 0.05 | −0.03 | 0.03 | −1.23 | 0.51 |
| Neuroticism × SLEs | −0.03 | 0.04 | −0.007 | 0.02 | 0.31 | 0.33 |
| Openness × SLEs | −0.02 | 0.05 | −0.003 | 0.02 | 0.56 | 0.44 |
| Work/financial events | ||||||
| Recent SLEs | 0.07*** | 0.02 | −0.03** | 0.008 | 0.14 | 0.15 |
| Extraversion × SLEs | 0.02 | 0.04 | 0.002 | 0.02 | −0.10 | 0.38 |
| Agreeableness × SLEs | −0.005 | 0.05 | −0.01 | 0.02 | 0.07 | 0.41 |
| Conscientiousness × SLEs | −0.06 | 0.04 | −0.005 | 0.02 | 0.33 | 0.39 |
| Neuroticism × SLEs | 0.05 | 0.03 | −0.016 | 0.01 | −0.05 | 0.25 |
| Openness × SLEs | 0.026 | 0.04 | −0.01 | 0.02 | −0.13 | 0.33 |
| Home events | ||||||
| Recent SLEs | −0.01 | 0.06 | −0.03 | 0.03 | −0.12 | 0.78 |
| Extraversion × SLEs | 0.17 | 0.14 | 0.008 | 0.07 | −0.24 | 1.9 |
| Agreeableness × SLEs | 0.009 | 0.16 | −0.02 | 0.08 | 1.34 | 2.01 |
| Conscientiousness × SLEs | 0.30 | 0.15 | −0.14 | 0.07 | −3.22 | 2.34 |
| Neuroticism × SLEs | 0.06 | 0.09 | −0.06 | 0.05 | 0.71 | 1.08 |
| Openness × SLEs | −0.18 | 0.14 | 0.10 | 0.07 | 0.72 | 1.49 |
| Health events | ||||||
| Recent SLEs | 0.17*** | 0.02 | — | — | — | — |
| Extraversion × SLEs | 0.04 | 0.04 | — | — | — | — |
| Agreeableness × SLEs | −0.06 | 0.04 | — | — | — | — |
| Conscientiousness × SLEs | 0.03 | 0.04 | — | — | — | — |
| Neuroticism × SLEs | 0.06 | 0.03 | — | — | — | — |
| Openness × SLEs | −0.02 | 0.04 | — | — | — | — |
Note. CRP = C-reactive protein; SLEs = stressful life events.
***p < .001. **p < .01. *p < .05. Indicators of statistical significance account for the Holm correction for family-wise error.
The preferred model for SRH revealed that extraversion and conscientiousness were positively related to baseline SRH, whereas neuroticism and agreeableness were negatively related to SRH (see Table 3). Higher extraversion and lower neuroticism were associated with slightly steeper decreases in SRH. Each recent SLE was associated with a small but statistically significant decrease in SRH. The interaction term between neuroticism and SLEs was small (B = −0.02, p = .03) and nonsignificant after applying the Holm correction. Among the specific event domains, only work/financial-related events were significantly related to reductions in SRH.
Unlike depressive symptoms and SRH, CRP was not significantly associated with any Big Five traits or SLEs (see Table 3). The N × SLE interaction was also not significantly different from zero. No specific SLE domains were associated with change in CRP.
Exploratory Analyses
We compared the effects of a spouse’s death within 90 days versus 2 years prior to a given wave for both depressive symptoms and SRH. We did not investigate CRP because there were no significant effects for CRP from our planned models.
The effect of a spouse’s death on depressive symptoms was larger when the death occurred within 90 days (B = 1.68, p < .001) than when the death occurred within 2 years (B = 0.87, p < .001). Furthermore, the interaction between neuroticism and spouse death was stronger within 90 days (B = 0.41, p = .006) than 2 years (B = 0.12, p = .04). However, neither interaction effect remained significant after applying the Holm correction.
For SRH, there were no significant main effects for the 90-day window (B = 0.01, p = .78) nor for the 2-year window (B = 0.03, p = .05). There were also no significant interactions between neuroticism and spouse death (for 90 days, B = 0.004, p = .96; for 2 years, B = 0.04, p = .14).
Discussion
Older adults are at high risk of experiencing bereavement, chronic illness onset, and other major SLEs (Ogle et al., 2013). It is crucial to understand the health consequences of such events, and how personality may exacerbate or buffer against the potentially negative effects of SLEs. The present study revealed that older adults experienced increased depressive symptoms and declines in self-rated physical health following recent SLEs. These effects varied by event type, with depressive symptoms affected most strongly by family and health-related events, whereas SRH was affected mostly by work/financial-related events. Furthermore, trait neuroticism was directly associated with elevated depressive symptom levels and worse SRH. However, in most instances, there was no evidence that neuroticism and SLEs interacted significantly to affect these health outcomes.
Researchers have hypothesized that neuroticism exerts a detrimental effect on health by intensifying reactions to stressors (Hampson, 2012; Lahey, 2009). The present study contributes to a growing body of literature that does not find notable long-term moderating effects of neuroticism on reactions to major SLEs (e.g., Anusic et al., 2014; Hahn et al., 2015; Pai & Carr, 2010; Yap et al., 2012). Such findings may inform future work on process models of personality and health. For example, the specific processes by which personality dispositions and stressful events affect health outcomes may be mostly similar across individuals, regardless of particular combinations of traits and experiences. A strength of the present study is the use of prospective data from a large, national sample of older adults. Furthermore, whereas prior studies most often examined specific types of events in isolation, we aggregated across event types, allowing for the accumulation of several events within a 2-year time frame. We also extended prior findings by exploring several different health outcomes, including depressive symptoms, self-reported physical health, and an objectively measured indicator of systemwide inflammation. None of these outcomes seemed to be affected by an interaction between neuroticism and SLEs.
Though neuroticism appears to heighten short-term emotional response to daily stressors (e.g., Bolger & Schilling, 1991; Gross et al., 1998; Mroczek & Almeida, 2004; Suls & Martin, 2005), the present findings raise questions about the persistence of heightened responsivity. We found that individuals high in neuroticism did not experience detectably worse long-term outcomes following major life stressors. Instead, SLEs had a significant direct effect on depressive symptoms and self-rated health, suggesting that SLEs are harmful regardless of personality. Given the strong evidence base connecting neuroticism with stress reactivity, there are important questions to investigate about how older adults with high neuroticism cope with major SLEs. For example, they may engage resources that counteract the effects of any heightened reactivity, or they may prepare for anticipated SLEs in ways that dampen their heightened response. Though neuroticism has been linked with less adaptive coping (Lahey, 2009), coping also tends to become more efficient and nuanced with age (Aldwin, 2011), so older adults who are higher in neuroticism may have developed effective means of compensating for their dispositional traits. In that case, any differential effects of neuroticism in the face of SLEs may manifest at the level of coping processes, but not affect health outcomes directly—an important hypothesis to pursue in future research.
It is also possible that individuals with high neuroticism may react more negatively in the immediate aftermath of an SLE, but that any discrepancy resolves within a few months. Our comparison of the effects of spouse death within the most recent 90 days versus 2 years seems to support this idea. Given the exploratory nature of our findings, future research is needed to confirm whether neuroticism exerts a decaying effect on the relationships between SLEs and health outcomes. However, if confirmed, this could have meaningful implications for clinical practice with older adults. For example, there may be a sensitive period in which individuals high in neuroticism are at higher risk of adverse outcomes following an SLE. Through that period, clinicians may use information about clients’ personalities to select appropriate interventions (Bagby, Gralnick, Al-Dajani, & Uliaszek, 2016; Harkness & Lilienfeld, 1997). Given recent meta-analytic evidence that high neuroticism is associated with worse therapeutic outcomes (Bucher, Suzuki, & Samuel, 2019), personality-tailored treatments are important to pursue. However, the added value of personality-tailoring for SLE-focused interventions may be highest within the first few months after the focal event.
Notably, we found that the effects of personality and SLEs differed across the three health measures we evaluated. Individuals who experienced more SLEs reported more depressive symptoms and worse SRH, but did not have elevated CRP levels. Similarly, personality traits such as neuroticism, extraversion, and conscientiousness were related to depressive symptoms and SRH in directions consistent with prior research (Hill & Roberts, 2016), whereas CRP was not significantly related to any of the Big Five traits after correcting for multiple comparisons. These findings suggest that the interaction between stressors and neuroticism may be more important for some health outcomes than others. Other health outcomes that are worth exploring in the future, given their relevance to older adults’ well-being and evidence linking them to personality and/or stressors, include anxiety (Bryant, Jackson, & Ames, 2008), cognitive function (Chapman et al., 2012), and mortality (Roberts et al., 2007).
The present study only tested initial level of personality traits as a predictor, and did not investigate change in personality traits. Though relatively stable, personality traits can and do change over time; this malleability is often overlooked based on misconceptions that personality is fixed in adulthood (Bleidorn et al., 2019). Given evidence suggesting that both personality trait level and change in personality predict health outcomes (Turiano et al., 2012), future research that tests whether changes in neuroticism predict heightened stress reactivity is warranted.
Several limitations of the present study involved measurement issues. Most research involving SLEs is limited by inherent challenges of measuring event occurrence (Harkness & Monroe, 2016). Though we attempted to include as many SLE types as possible, there are still other events (e.g., death of siblings or close friends) that are not measured in HRS. Many participants were also missing data for several events, often due to noncompletion of the LBQ. Variance in timing and severity of SLEs was also constrained by the binary “presence/absence” event coding. Furthermore, the brevity of the MIDI may have limited our power to detect effects of Big Five traits. We attempted to address these issues through sensitivity analyses. Encouragingly, the vast majority of specifications pointed to the same substantive conclusions. Nonetheless, future research may improve on these measurement concerns. “Gold standard” SLE assessments involve semistructured interviews to thoroughly explore participants’ exposure to stressors, which are subsequently scored by blind raters (Harkness & Monroe, 2016). Such methods could be used to test whether our results replicate with an even more exhaustive measure of SLEs, and more precise assessment of event timing and severity. Exploration of the effects of different types of stressors, such as daily hassles and chronic stress, are also warranted. Replication efforts using a longer Big Five measure may also be valuable.
Like many longitudinal studies of aging, the present study is subject to selection effects. However, attrition was not strongly related to neuroticism (see Supplementary Table S2). To mitigate selection bias, we used FIML and controlled for variables that were significantly associated with attrition. Furthermore, when examining change only between Waves 1 and 2 (when 93% of the current sample was retained), the results were consistent with the main analysis. In LGM models that did not constrain interaction parameters to be equal across waves, the N × SLE interaction for Wave 2 was B = 0.033, p = .171 for depressive symptoms, and B = −0.043, p = .003 (ns after applying Holm correction) for self-rated health. Testing diverse samples, including individuals with relatively high neuroticism (e.g., clinical samples), and using more frequent assessments may further mitigate selection bias in future research.
Our results may not generalize to earlier times of life, as the present sample included only older adults. That said, the size and national reach of the HRS sample is an important strength, and we expect that our findings represent American older adults reasonably well.
Conclusion
The present study found little evidence that Big Five traits, and neuroticism in particular, moderate the health impacts of SLEs on a 2-year time frame. Though past research has strongly supported the hypothesis that neuroticism represents greater reactivity to stress, this heightened response to stressors may dissipate and become undetectable over the course of several months. Older adults with high neuroticism may also have effective coping mechanisms to limit the severity of their reaction to SLEs. Though we did not find that neuroticism moderated the effect of SLEs, the main effects of Big Five traits and SLEs were substantial in many instances, suggesting that these factors are important predictors of older adults’ health outcomes in their own right, and should be considered in the context of interventions to promote older adults’ mental and physical health.
Supplementary Material
Acknowledgments
The authors thank Zachary G. Baker, Siamak Noorbaloochi, and Nidhi Kohli for feedback on the study preregistration and analysis plan.
Funding
The Health and Retirement Study is sponsored by the National Institute on Aging (NIA U01AG009740) and is conducted by the University of Michigan. This material is based on work supported by the Office of Academic Affiliations, Department of Veterans Affairs.
Conflict of Interest
None declared.
References
- Aldwin C. (2011). Stress and coping across the lifespan. In Folkman S. (Ed.), The Oxford handbook of stress, health, and coping (pp. 15–34). Oxford University Press. New York. [Google Scholar]
- Anusic I., Yap S. C., & Lucas R. E (2014). Does personality moderate reaction and adaptation to major life events? Analysis of life satisfaction and affect in an Australian national sample. Journal of Research in Personality, 51, 69–77. doi: 10.1016/j.jrp.2014.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagby R. M., Gralnick T. M., Al‐Dajani N., & Uliaszek A. A (2016). The role of the five‐factor model in personality assessment and treatment planning. Clinical Psychology: Science and Practice, 23(4), 365–381. doi: 10.1111/cpsp.12175 [DOI] [Google Scholar]
- Bleidorn W., Hill P. L., Back M. D., Denissen J. J. A., Hennecke M., Hopwood C. J., . . . Roberts B (2019). The policy relevance of personality traits. The American Psychologist, 74(9), 1056–1067. doi: 10.1037/amp0000503 [DOI] [PubMed] [Google Scholar]
- Bolger N., & Schilling E. A (1991). Personality and the problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of Personality, 59(3), 355–386. doi.org/ 10.1111/j.1467-6494.1991.tb00253.x [DOI] [PubMed] [Google Scholar]
- Bogg T., & Roberts B. W (2004). Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin, 130(6), 887–919. doi: 10.1037/0033-2909.130.6.887 [DOI] [PubMed] [Google Scholar]
- Bryant C., Jackson H., & Ames D (2008). The prevalence of anxiety in older adults: Methodological issues and a review of the literature. Journal of Affective Disorders, 109(3), 233–250. doi: 10.1016/j.jad.2007.11.008 [DOI] [PubMed] [Google Scholar]
- Bucher M. A., Suzuki T., & Samuel D. B (2019). A meta-analytic review of personality traits and their associations with mental health treatment outcomes. Clinical Psychology Review, 70, 51–63. doi: 10.1016/j.cpr.2019.04.002 [DOI] [PubMed] [Google Scholar]
- Chapman B., Duberstein P., Tindle H. A., Sink K. M., Robbins J., Tancredi D. J., . . . Franks P.; Gingko Evaluation of Memory Study Investigators (2012). Personality predicts cognitive function over 7 years in older persons. The American Journal of Geriatric Psychiatry, 20(7), 612–621. doi: 10.1097/JGP.0b013e31822cc9cb [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg L. R., Johnson J. A., Eber H. W., Hogan R., Ashton M. C., Cloninger C. R., & Gough H. G.(2006). The international personality item pool and the future of public-domain personality measures. Journal of Research in Personality, 40(1), 84–96. doi: 10.1016/j.jrp.2005.08.007 [DOI] [Google Scholar]
- Gross J. J., Sutton S. K., & Ketelaar T (1998). Relations between affect and personality: Support for the affect-level and affective-reactivity views. Personality and Social Psychology Bulletin, 24(3), 279–288. doi: 10.1177/0146167298243005 [DOI] [Google Scholar]
- Hahn E., Specht J., Gottschling J., & Spinath F. M.(2015). Coping with unemployment: The impact of unemployment duration and personality on trajectories of life satisfaction. European Journal of Personality, 29(6), 635–646. doi: 10.1002/per.2034 [DOI] [Google Scholar]
- Hakulinen C., Elovainio M., Pulkki-Råback L., Virtanen M., Kivimäki M., & Jokela M (2015). Personality and depressive symptoms: Individual participant meta-analysis of 10 cohort studies. Depression and Anxiety, 32(7), 461–470. doi: 10.1002/da.22376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938 [DOI] [PubMed] [Google Scholar]
- Hampson S. E. (2012). Personality processes: mechanisms by which personality traits “get outside the skin”. Annual Review of Psychology, 63, 315–339. doi: 10.1146/annurev-psych-120710-100419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness A. R., & Lilienfeld S. O (1997). Individual differences science for treatment planning: Personality traits. Psychological Assessment, 9(4), 349. doi: 10.1037/1040-3590.9.4.349 [DOI] [Google Scholar]
- Harkness K. L., & Monroe S. M (2016). The assessment and measurement of adult life stress: Basic premises, operational principles, and design requirements. Journal of Abnormal Psychology, 125(5), 727–745. doi: 10.1037/abn0000178 [DOI] [PubMed] [Google Scholar]
- Hatch S. L., & Dohrenwend B. P (2007). Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. American Journal of Community Psychology, 40(3-4), 313–332. doi: 10.1007/s10464-007-9134-z [DOI] [PubMed] [Google Scholar]
- Hill P. L., & Roberts B. W (2016). Personality and health: Reviewing recent research and setting a directive for the future. In K. W. Schaie & S. L. Willis (Eds), Handbook of the Psychology of Aging (pp. 205–218). Academic Press: London. doi: 10.1016/B978-0-12-411469-2.00011-X [DOI] [Google Scholar]
- Holm S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6, 67–70. [Google Scholar]
- Holmes T. H., & Rahe R. H (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11(2), 213–218. doi: 10.1016/0022-3999(67)90010-4 [DOI] [PubMed] [Google Scholar]
- Hu L., & Bentler P. M (1999). Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hutchinson J. G., & Williams P. G (2007). Neuroticism, daily hassles, and depressive symptoms: An examination of moderating and mediating effects. Personality and Individual Differences, 42, 1367–1378. doi: 10.1016/j.paid.2006.10.014 [DOI] [Google Scholar]
- Iacovino J. M., Bogdan R., & Oltmanns T. F (2016). Personality predicts health declines through stressful life events during late mid-life. Journal of Personality, 84(4), 536–546. doi: 10.1111/jopy.12179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. L., & Benyamini Y (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38(1), 21–37. doi: 10.2307/2955359 [DOI] [PubMed] [Google Scholar]
- Juster R. P., McEwen B. S., & Lupien S. J (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews, 35(1), 2–16. doi: 10.1016/j.neubiorev.2009.10.002 [DOI] [PubMed] [Google Scholar]
- Kendler K. S., Gardner C. O., & Prescott C. A (2003). Personality and the experience of environmental adversity. Psychological Medicine, 33(7), 1193–1202. doi: 10.1017/s0033291703008298 [DOI] [PubMed] [Google Scholar]
- Kendler K. S., Karkowski L. M., & Prescott C. A (1999). Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry, 156(6), 837–841. doi.org/ 10.1176/ajp.156.6.837 [DOI] [PubMed] [Google Scholar]
- Kendler K. S., Kuhn J., & Prescott C. A (2004). The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. The American Journal of psychiatry, 161(4), 631–636. doi: 10.1176/appi.ajp.161.4.631 [DOI] [PubMed] [Google Scholar]
- Lachman M. E., & Weaver S. L (1997). The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Waltham, MA: Brandeis University. [Google Scholar]
- Lahey B. B. (2009). Public health significance of neuroticism. The American Psychologist, 64(4), 241–256. doi: 10.1037/a0015309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J. E., Neylan T. C., Epel E., & O’Donovan A (2016). Associations of childhood adversity and adulthood trauma with C-reactive protein: A cross-sectional population-based study. Brain, Behavior, and Immunity, 53, 105–112. doi: 10.1016/j.bbi.2015.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire L. M., Schulz R., Helgeson V. S., Small B. J., & Saghafi E. M (2010). Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine, 40(3), 325–342. doi: 10.1007/s12160-010-9216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae R. R., & Costa P. T. Jr. (2008). The five-factor theory of personality. In John O. P., Robins R. W., & Pervin L. A. (Eds.), Handbook of personality: Theory and research (pp. 159–181). The Guilford Press: New York. [Google Scholar]
- Mroczek D. K., & Almeida D. M (2004). The effect of daily stress, personality, and age on daily negative affect. Journal of Personality, 72(2), 355–378. doi: 10.1111/j.0022-3506.2004.00265.x [DOI] [PubMed] [Google Scholar]
- Musliner K. L., Seifuddin F., Judy J. A., Pirooznia M., Goes F. S., & Zandi P. P (2015). Polygenic risk, stressful life events and depressive symptoms in older adults: A polygenic score analysis. Psychological Medicine, 45(8), 1709–1720. doi: 10.1017/S0033291714002839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neupert S. D., Almeida D. M., & Charles S. T (2007). Age differences in reactivity to daily stressors: The role of personal control. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62(4), P216–P225. doi: 10.1093/geronb/62.4.p216 [DOI] [PubMed] [Google Scholar]
- Ogle C. M., Rubin D. C., Berntsen D., & Siegler I. C (2013). The frequency and impact of exposure to potentially traumatic events over the life course. Clinical Psychological Science, 1(4), 426–434. doi: 10.1177/2167702613485076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle C. M., Rubin D. C., & Siegler I. C (2014). Cumulative exposure to traumatic events in older adults. Aging & Mental Health, 18(3), 316–325. doi: 10.1080/13607863.2013.832730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai M., & Carr D (2010). Do personality traits moderate the effect of late-life spousal loss on psychological distress? Journal of Health and Social Behavior, 51(2), 183–199. doi: 10.1177/0022146510368933 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Renzaho A. M., Houng B., Oldroyd J., Nicholson J. M., D’Esposito F., & Oldenburg B (2014). Stressful life events and the onset of chronic diseases among Australian adults: Findings from a longitudinal survey. European Journal of Public Health, 24(1), 57–62. doi: 10.1093/eurpub/ckt007 [DOI] [PubMed] [Google Scholar]
- Roberts B. W., Kuncel N. R., Shiner R., Caspi A., & Goldberg L. R (2007). The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science, 2(4), 313–345. doi: 10.1111/j.1745-6916.2007.00047.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer J. D., & Willett J. B (2003). Applied longitudinal data analysis. New York, NY: Oxford University Press. [Google Scholar]
- Smith T. W. (2006). Personality as risk and resilience in physical health. Current Directions in Psychological Science, 15(5), 227–231. doi: 10.1111/j.1467-8721.2006.00441.x [DOI] [Google Scholar]
- Sonnega A., Faul J. D., Ofstedal M. B., Langa K. M., Phillips J. W., & Weir D. R (2014). Cohort profile: the Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. doi: 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J., & Martin R (2005). The daily life of the garden-variety neurotic: Reactivity, stressor exposure, mood spillover, and maladaptive coping. Journal of Personality, 73(6), 1485–1509. doi: 10.1111/j.1467-6494.2005.00356.x [DOI] [PubMed] [Google Scholar]
- Sutin A. R., Terracciano A., Milaneschi Y., An Y., Ferrucci L., & Zonderman A. B (2013). The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry, 70(8), 803–811. doi: 10.1001/jamapsychiatry.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano N. A., Pitzer L., Armour C., Karlamangla A., Ryff C. D., & Mroczek D. K (2012). Personality trait level and change as predictors of health outcomes: Findings from a national study of Americans (MIDUS). The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67(1), 4–12. doi: 10.1093/geronb/gbr072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman S. E., & Siegel J. M (1996). Traumatic events and physical health in a community sample. Journal of Traumatic Stress, 9(4), 703–720. doi: 10.1007/BF02104098 [DOI] [PubMed] [Google Scholar]
- Weston S. J., Hill P. L., & Jackson J. J (2015). Personality traits predict the onset of disease. Social Psychological and Personality Science, 6(3), 309–317. doi: 10.1177/1948550614553248 [DOI] [Google Scholar]
- Yap S. C., Anusic I., & Lucas R. E (2012). Does personality moderate reaction and adaptation to major life events? Evidence from the British household panel survey. Journal of Research in Personality, 46(5), 477–488. doi: 10.1016/j.jrp.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.