Abstract
Objectives
Inequities in access to and utilization of health care greatly influence the health and quality of life of American Indian elders (AIEs). This study explores the importance and perceived prevalence of factors affecting health care use within this population and assesses the changeability of these factors to produce a list of action items that are timely and relevant to improving health care access and utilization.
Method
Concept mapping was conducted with AIEs (n = 65) and professional stakeholders (n = 50), including tribal leaders, administrators of public-sector health systems, outreach workers, and health care providers. Data were analyzed using multidimensional scaling and cluster analyses.
Results
The final concept-map model comprised nine thematic clusters related to factors affecting elder health care: Difficulties Obtaining and Using Insurance; Insecurity from Lack of Knowledge; Limited Availability of Services; Scheduling Challenges; Provider Issues and Relationships; Family and Emotional Challenges; Health-Related Self-Efficacy and Knowledge; Accessibility and Transportation Barriers; and Tribal/National Policy.
Discussion
Findings suggest that improvements in access to and utilization of health care among AIEs will require actions across multiple domains, including health system navigation services, workforce improvements, and tribal, state, and federal policy. A multilevel socioecological approach is necessary to organize and undertake these actions.
Keywords: Health disparities, Health services use, Insurance, Minority aging (race/ethnicity)
Published reports describe American Indians (AIs) as experiencing some of the worst health disparities in the United States, including higher rates of physical and mental illness, and a lower life expectancy than other U.S. populations (Espey et al., 2014; Indian Health Service, 2015). Although members of federally recognized tribes are entitled to health care as a treaty-guaranteed right, AIs are more likely to go without health care than non-Hispanic Whites (Boccuti, Swoope, & Artiga, 2014). These disparities greatly influence the health and quality of life of American Indian elders (AIEs), defined as individuals aged 55 and older. Inequities in access to and utilization of health care among AIEs are due to intersecting factors at multiple levels of influence, including personal and interpersonal circumstances, community and organizational dynamics, and tribal, state, and national policy. This study uses concept mapping (CM), a participatory mixed-method approach to data collection and analysis, to gain a multilevel understanding of the factors influencing AIE health care.
Background
Compared to their non-Hispanic White counterparts, AIs live with disproportionately high rates of health problems, such as cardiovascular disease, diabetes, heart disease, hypertension, and obesity (Espey et al., 2014; Indian Health Service, 2015; Kim, Bryant, Goins, Worley, & Chiriboga, 2012; Schieb, Ayala, Valderrama, & Veazie, 2014; Veazie et al., 2014), as well as mental health concerns (Beals et al., 2005). Among AIEs with chronic illnesses, comorbidities are common and increase with age (Goins & Pilkerton, 2010; John, Kerby, & Hennessy, 2003). Almost one fourth of AIs have a disability (Smith-Kaprosy, Martin, & Whitman, 2012). Adults who are AI are also less likely to see a medical doctor or have a usual source of care than Whites (Kim et al., 2012). Many AIEs lack health insurance, which negatively affects their access to health care (Upper Midwest Rural Health Research Center, 2007; Willging, Waitzkin, & Wagner, 2005). Although the 2010 Patient Protection and Affordable Care Act (ACA) expanded access to health insurance for AIs, reports estimate that 25% of elders under age 65 remain uninsured (Boccuti et al., 2014).
Numerous intersecting factors affect AIE access to and use of health care at multiple levels: individual, interpersonal, organizational, community, and policy (McLeroy, Bibeau, Steckler, & Glanz, 1988). Individual-level factors include race, ethnicity, age, and education, as well as employment and housing status, income, and health and mental health history. Low health literacy is also common among both AIs and older adults (White, 2008), and is correlated with poor health-related self-efficacy, less use of preventative care, and higher morbidity and mortality, especially in seniors (Baker, Wolf, Feinglass, & Thompson, 2008; Cho, Lee, Arozullah, & Crittenden, 2008). Additional individual factors likely to affect the health literacy of older adults include difficulty processing information due to cognitive aging and vision and hearing impairments (Centers for Disease Control and Prevention, 2009; Verney et al., 2008). Older adults may also be reluctant to ask questions in health care settings (Rubin, Freimuth, Johnson, Kaley, & Parmer, 2014). Increasingly, comfort with technology is an integral component of health literacy (Kim & Xie, 2016). At the interpersonal level, positive social interactions and emotional support affect the health and quality of life of AIEs, including their resilience, mental health, and experiences of chronic pain (Conte, Schure, & Goins, 2015; Roh et al., 2015). Yet, AIEs may be negatively affected by unsupportive family or social relationships. Their likelihood to access health care may also be influenced by the time commitment and financial responsibility of caring for children and grandchildren (Jaramillo, Willging, Haozous, Verney, & Lujan, 2019).
At the organizational and community levels, the majority of AIEs rely on the Indian Health Service (IHS), where they are entitled to receive available health care services at no cost without health insurance (Adamsen, 2015). However, the Fiscal Year 2017 IHS per capita health care expenditure was $3,851, far less than the $10,348 per capita health care expenditure for the U.S. population in 2016 (Indian Health Service, 2019). Because the IHS is a health service delivery system, not an insurance provider, it cannot protect against unforeseen medical expenses and it is not uncommon for health care demands to exceed available funding, increasing the likelihood that AIEs face major medical bills or go without recommended treatments (Fox, 2011). Another important organizational-level factor is the provider–patient relationship. Studies show that AIs may feel less trust in their providers and health care organizations than their non-AI counterparts, affecting their decisions to access health care (Canales, Weiner, Samos, & Wampler, 2011; Simonds, Goins, Krantz, & Garroutte, 2014). Geography is an additional community-level factor affecting AIEs. Geographic areas with high concentrations of AIs report disparities in access to and use of health services, especially preventative care (Towne, Smith, & Ory, 2014). Elders who live on reservations are also more likely to be uninsured than urban AIEs as high unemployment affects their access to private health insurance (Upper Midwest Rural Health Research Center, 2007). However, the nearly 60% of AI people in the United States who live in nonreservation settings may not be able to obtain health care for which they would otherwise be eligible at IHS or tribally run programs (Artiga, Arguello, & Duckett, 2013).
Finally, various tribal, state, and national policies influence the ability of AIEs to access and use health care. For example, efforts to use the IHS can be complicated for individuals who do not meet tribe-specific criteria regarding tribal affiliation or who reside outside their tribe’s IHS service area (Artiga et al., 2013). Scholars also point to widespread confusion and inconsistency regarding AI policy at state and federal levels, as well as an overall paucity of public funding, as major contributors to AI health disparities (Dyste, 2014; Skinner, 2016). In addition to reauthorizing the 1976 Indian Health Care Improvement Act (IHCIA), the ACA increased access to health insurance for AIs via AI-specific provisions, such as an unlimited enrollment period to purchase private insurance. Additionally, in the states that accepted the expansion of Medicaid eligibility for most low-income adults, this benefit affected large numbers of AIs (Warne, Delrow, Angus-Hornbuckle, & Shelton, 2017). The IHS and tribally-run health care programs provide services to AI patients without insurance. However, these programs do bill the health insurance of patients with coverage; consequently, the increase in insured users has infused these programs with new funding (Artiga, Ubri, & Foutz, 2017; Skinner, 2016; Warne et al., 2017). Notably, the ongoing national debate over the ACA and public insurance programs in general has increased uncertainty for AIs, particularly the 96% of AIEs over the age of 65 who rely on public health insurance, 24% of whom depend on both Medicaid and Medicare (Boccuti et al., 2014).
The purpose of this study is to further examine these multilevel factors from the perspectives of AIEs and other relevant stakeholders in AIE health, including tribal leaders, administrators of public-sector systems, outreach workers, and health care providers. The CM approach has been used in community-driven, participatory research to engage participants in generating theory and determining locally relevant intervention strategies (Kane & Trochim, 2007; Kelly, Baker, Brownson, & Schootman, 2007; Windsor, 2013). In this study, we used CM to: (a) explore the importance and perceived prevalence of multilevel factors affecting AIE health care access from the viewpoints of diverse stakeholders who may hold different perspectives, and (b) assess the changeability of these factors to produce a list of action items that are timely and relevant to improving health care access and utilization among AIEs.
Method
In keeping with community-engaged approaches to research with indigenous peoples (Brave Heart et al., 2016), the study was conceptualized and designed in consultation with a group of AIEs and allies comprising the Seasons of Care Community Action Board (CAB). The members of the CAB have overseen each aspect of the research, including reviewing data collection instruments, assisting with recruitment, and strategizing efforts to promote elder health. The study design and written informed consent protocols were reviewed and approved by the Institutional Review Board of the Southwest Tribal Native American Research Center for Health.
Participants
This CM initiative was conducted between June and December 2017 as part of a larger study on access to and utilization of health care and health insurance among AIEs in two states in the U.S. Southwest (Willging et al., 2018). We used a purposive sampling strategy to represent a range of knowledge, beliefs, and experiences related to health care. The AIE participants were recruited through in-person outreach during regular visits to AI senior centers, health clinics, and meetings of health-focused AI groups and organizations. Additionally, we used reputational case selection to solicit recommendations from CAB members and other local experts on AIE health for professional stakeholder participants, consisting of individuals who played roles in conceptualizing and enacting health policy affecting AIEs, or delivering health-related services to AIEs (Schensul, Schensul, & LeCompte, 1999). The professional participants were invited to participate via phone and e-mail.
A total of 65 AIEs and 50 professional stakeholder participants (n = 115) completed at least one of the CM sorting or rating activities discussed below. The AIE participants identified as AI and had an average age of 68.7 years. A total of 69.2% (n = 45) of AIE participants were female and 9.2% (n = 6) also reported having Hispanic or Latina/o heritage. Outreach workers or health care providers (e.g., physicians, public health nurses, benefits coordinators; n = 35; 30.4%) and tribal leaders or public-sector health system administrators (e.g., state-level health agency staff, hospital administrators; n = 15; 13.0%) comprised the remaining participants. The average age of these professional stakeholder participants was 50.2 years; the majority were female (n = 39; 78%) and identified as AI (n = 47; 94%), with the remaining professional participants identifying as White. Four percent (n = 2) of professional participants reported that they had Hispanic or Latina/o heritage. Informed consent was obtained from all participants.
CM Approach
The CM process typically consists of six phases: (a) preparation—researchers identify participants and develop a focus question; (b) generation—participants contribute statements in response to the focus question; (c) structuring—participants sort statements into thematic groups based on similarity and rate each statement on several a priori dimensions (e.g., importance, changeability); (d) representation—researchers conduct multidimensional scaling (MDS) and cluster analyses to create a “concept map” placing statements that were sorted together in closer proximity to each other; (e) interpretation—researchers and participants assess the resulting potential concept maps to determine which is perceived to best represent the data and develop cluster labels and interpretations; and (f) utilization—researchers and participants use results to better understand the perspectives of stakeholders and identify potential action items. Below, we describe how we applied this process in the present study.
In the preparation phase, the study team and CAB developed a single focus question: What factors make it easy or hard for Native American elders to get good health care? The focus question was asked in individual, in-depth interviews with the larger sample of the parent study on AIE health care access and utilization that were conducted prior to the remaining CM activities. This parent sample included 96 AIEs and 47 professional stakeholders. Of these participants, nine AIEs and 10 professionals also took part in the CM portion of the study described here.
The generation phase included a range of activities to elicit a thorough representation of factors perceived to affect whether AIEs obtained good health care. In the first step, the research team identified 106 unique factors generated from the interviews. Slightly revised and consolidated factor lists were then presented to 20 individuals, including the 10 members of the CAB and the attendees of two small group forums (one consisting of five AIEs and one of five health care administrators/providers) to get feedback on the interpretability of the statements and identify other key factors to consider for inclusion. The demographics of these individuals mirrored the larger CM sample. These individuals reviewed, added, and consolidated factor statements to reduce conceptual overlap/redundancy, resulting in a final list of 61 distinct statements.
In the structuring phase, each of the 115 CM participants were first asked to sort the 61 factor statements into separate thematic groups (or “clusters”) in a manner that was meaningful to her/him. Each statement was listed on a separate card and each participant was asked to physically group together statements that s/he thought were related. After all cards were grouped into different thematic piles, participants suggested a name to describe the general content of each grouping (e.g., “Transportation issues,” “Insurance”). When researchers observed stakeholders sorting statements according to their personal relationships to the factors (i.e., “Things that are hard for me”), participants were redirected to label piles thematically.
Second, we asked each participant to individually rate each factor statement (using a Likert scale) on the following dimensions: “How much do you think this factor affects the health of Native American elders?” (1 = no effect; 10 = very large effect); “How common do you think this factor is among Native American elders?” (1 = not common at all; 10 = very common); “How easy do you think it is to change this factor?” (1 = very difficult to change; 10 = very easy to change). Participants marked ratings for each dimension on separate worksheets.
Analysis
Analysis was conducted using specialized Concept Systems software (Concept Systems Inc., 2018). One member of the research team manually entered the sorting and rating data into the software; two additional team members reviewed the data for accuracy and excluded four invalid or incomplete cases (e.g., respondents indicating no variability in ratings). The sorting data from the remaining cases were analyzed using MDS and hierarchical cluster analysis (Davison, 1983). These procedures resulted in the creation of visual representations (i.e., concept maps) for how statements were typically clustered across all participants. Multiple concept-map outcomes were considered based on interpretability of each potential solution, with the ideal model considered to include the fewest number of clusters that also represented distinct key concepts (Rosas & Kane, 2012). We first considered a large number of potential clusters (e.g., 20) and then, in stepwise fashion, consolidated groups that were most thematically similar based on participant responses. To arrive at the final cluster solution, we presented potential solutions ranging from 15 to 8 clusters to the CAB members, who collaboratively settled on the nine-cluster solution to best represent the data without loss of important distinct thematic areas. The CAB also examined each cluster in this final model to ensure that the label assigned to it accurately reflected the nature of the statements that it contained.
Next, we used the three different ratings of each factor separately to calculate an average score for the factor’s perceived: (a) impact on AIE health, (b) prevalence among AIEs, and (c) changeability, respectively. Following the identification of the nine thematic statement clusters, we calculated the rating of each cluster for these three dimensions by computing the average ratings of the individual statements contained within each cluster. To identify “important” clusters that were rated as having high impact on AIE health, high prevalence among AIEs, and high changeability, we created a rank cluster order for each dimension (with the highest cluster rating ranked as #1, second highest as #2, etc.), and then summed the three separate rank orders to calculate a total rank score for each cluster.
Results
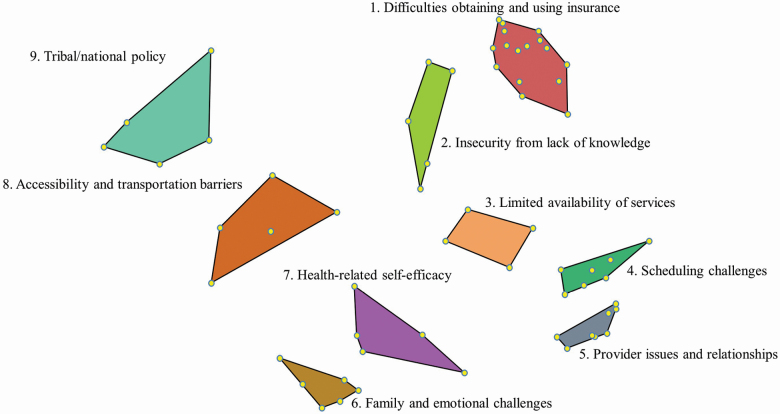
The final model comprised nine thematic clusters, each representing a key domain related to factors affecting whether AIEs can obtain good health care, as illustrated in Figure 1. These clusters were: Difficulties Obtaining and Using Insurance; Insecurity from Lack of Knowledge; Limited Availability of Services; Scheduling Challenges; Provider Issues and Relationships; Family and Emotional Challenges; Health-Related Self-Efficacy and Knowledge; Accessibility and Transportation Barriers; and Tribal/National Policy. The research team and CAB members evaluated these clusters as having good face validity.
Figure 1.
Thematic cluster map of factors perceived to affect American Indian elder health care.
Per Figure 1, each dot within a cluster represents a statement that was sorted into similar categories by participants. The stress value is a measure of how well the point map represents the original data. The value should range from 0.10 to 0.35, with lower values indicating a better fit (Concept Systems Inc., 2018). When the map did not fit the original data (i.e., the stress value was too high), this meant that the distances of statements on the point map were more discrepant from the values in the similarity matrix derived from the sorting activity (Kane & Trochim, 2007). The stress value of 0.23 for our analyses indicate good model fit for the underlying concept point map from which the final cluster solution was determined. Table 1 lists each of the nine clusters and individual factor statements.
Table 1.
Cluster Themes and Factors Affecting American Indian Elder Health Care
| Cluster name | Statements included in cluster |
|---|---|
| 1. Difficulties Obtaining and Using Insurance | Uncertainty about what health care services/medications are covered by insurance |
| Insurance or Indian Health Service won’t cover enough health care costs | |
| Difficulty communicating with insurance company (including rude or unhelpful insurance representatives, understanding insurance lingo) | |
| Having to deal with billing departments and debt collectors | |
| Not knowing how to report or appeal health care/insurance decisions | |
| Needing to change insurance companies | |
| Difficulties using insurance at Indian Health Service | |
| Too many forms to fill out to get insurance | |
| Difficulties using multiple types of insurance | |
| Difficulties paying for the cost of insurance | |
| Lack of education about insurance plan choices | |
| Doctors/health care professionals not accepting insurance plan | |
| Insurance or Indian Health Service refusing to cover certain health care services or prescriptions | |
| Not having insurance/prescription card to show for services | |
| Too many forms to fill out when getting health care services | |
| Not being aware of Purchased Referred Care or how to use it | |
| 2. Insecurity from Lack of Knowledge | Not knowing where to find health care information |
| Limited knowledge of computers or the Internet to obtain information about insurance | |
| Not having access to Native language interpreters/translators to help with insurance enrollment | |
| Difficulties paying for health care costs | |
| Getting inaccurate health care/insurance advice from Indian Health Service and/or Tribal services | |
| 3. Limited Availability of Services | Not having a health facility open on weekends or after hours in or near my community |
| Not knowing where to obtain good health care | |
| Health services/providers being shut down | |
| Not having access to Native language interpreters/translators when communicating with health care professionals | |
| 4. Scheduling Challenges | Needing to change to a new doctor and/or health care facility |
| Difficulty communicating with health care professionals (including rude or unhelpful providers, not understanding medical “lingo” or terminology) | |
| No same-day appointments available or walk-in access | |
| Long waits at health care facilities | |
| Doctors/health care professionals cancelling/rescheduling appointments | |
| Difficulty scheduling appointments (i.e., being told to call back at a later date when trying to schedule an appointment or having to schedule appointments more than a month in the future) | |
| Difficulties getting medication prescriptions filled/refilled | |
| 5. Provider Issues and Relationships | Not having a qualified/skilled doctor who can be trusted |
| Rushed appointments with the doctor (e.g., 5-min visit) | |
| Not being able to see the desired doctor or health care professional | |
| Not having all your doctors, nurses, pharmacists, and facilities know the right information about you | |
| Not having a “regular” doctor that knows your personal health history | |
| Concerns about doctors or health care professionals not maintaining privacy/confidentiality | |
| Not knowing how to choose the right doctor | |
| Being overprescribed too many drugs | |
| 6. Family and Emotional Challenges | Family being unwilling or unavailable to advocate on behalf of the elder |
| Difficulties dealing with emotions related to health care (e.g., feeling like a burden on family | |
| Living alone | |
| Not wanting to tell others about personal health issues | |
| Not being able to be honest with family about health care-related wants and needs | |
| Denying the need for care (“tough guy” mentality) | |
| 7. Health-Related Self-Efficacy | Not being comfortable/confident enough to ask questions |
| Not knowing how to advocate for own personal health care | |
| Reluctance to use services provided by Indian Health Service or Tribe | |
| Not being able to read or understand instructions for taking medicines correctly | |
| Not knowing when to go to the doctor (i.e., knowing the “warning signs”) | |
| 8. Accessibility and Transportation Barriers | Limited availability of elder-specific services (including home health caregivers) |
| High cost of transportation to obtain health care | |
| Needing to travel long distances to obtain care (e.g., doctors or emergency care) | |
| Not having reliable transportation to get to health care appointments | |
| Not having access to community health programs (e.g., senior center or clinics) that provide transportation | |
| 9. Tribal/National Policy | Health care is a low priority for Tribal leadership |
| Information not shared with the community or general meetings | |
| Tribal affiliations or blood quantum restrictions make it hard to get good health care | |
| Not knowing how to influence Tribal leadership | |
| Health care is a low priority for national politicians |
Table 2 shows AIE and professional stakeholder ratings for each of the nine thematic clusters (as determined by the average of the ratings of the individual factor statements per cluster), and the relative rank order of the cluster for (a) impact on AIE health, (b) prevalence among AIEs, and (c) changeability. The average ratings for each cluster indicate that both AIEs and professionals perceived all domains to have a large impact on AIE health (i.e., all rating values were above a value of 7 on the 10-point scale). The AIE ratings ranged from 7.17 (Family and Emotional Challenges) to 7.75 (Provider Issues and Relationships) and professional ratings ranged from 7.73 (Tribal/National Policy) to 8.15 (Insecurity from Lack of Knowledge). Likewise, the prevalence ratings for both AIEs and professionals indicate that all factors were perceived as fairly common among AIEs. The AIE ratings ranged from 7.35 (Scheduling Challenges) to 7.98 (Tribal/National Policy) and professional ratings ranged from 7.31 (Limited Availability of Services) to 7.80 (Insecurity from Lack of Knowledge). Both AIE and professional participants were more ambivalent regarding the changeability of factors, with average ratings varying from slightly below to slightly above the midpoint of the scale. For AIEs, the changeability ratings ranged from 4.89 (Tribal/National Policy) to 5.47 (Health-Related Self-Efficacy) and for professionals, ratings ranged from 4.52 (Family and Emotional Challenges) to 5.20 (Health-Related Self-Efficacy).
Table 2.
Cluster Rating Averages and Ranks for Factors That Affect AIE Health Care, by AIE and Professional Stakeholder Participants
| Impact on AIE health | Prevalence among AIEs | Changeability | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AIE | Professional | AIE | Professional | AIE | Professional | AIE | Professional | |||||||
| Cluster theme (# in Figure 1) | Ratinga | Rank | Ratinga | Rank | Ratinga | Rank | Ratinga | Rank | Ratinga | Rank | Ratinga | Rank | Rank score | Rank score |
| Insecurity from Lack of Knowledge (#2) | 7.56 | 3 | 8.15 | 1 | 7.60 | 3 | 7.80 | 1 | 5.35 | 2 | 5.10 | 4 | 8 | 6 |
| Tribal/National Policy (#9) | 7.75 | 1 | 7.73 | 9 | 7.98 | 1 | 7.49 | 4 | 4.89 | 9 | 4.79 | 7 | 11 | 20 |
| Accessibility and Transportation Barriers (#8) | 7.51 | 4 | 7.79 | 8 | 7.43 | 7 | 7.46 | 5 | 5.30 | 3 | 5.12 | 2 | 14 | 15 |
| Provider Issues and Relationships (#5) | 7.72 | 2 | 7.86 | 7 | 7.53 | 5 | 7.35 | 7 | 4.98 | 7 | 5.07 | 5 | 14 | 19 |
| Health-Related Self-Efficacy (#7) | 7.20 | 8 | 8.17 | 2 | 7.47 | 6 | 7.73 | 2 | 5.47 | 1 | 5.20 | 1 | 15 | 5 |
| Family and Emotional Challenges (#6) | 7.17 | 9 | 7.95 | 5 | 7.83 | 2 | 7.54 | 3 | 5.23 | 4 | 4.52 | 9 | 15 | 17 |
| Limited Availability of Services (#3) | 7.50 | 5 | 8.15 | 3 | 7.57 | 4 | 7.31 | 9 | 4.91 | 8 | 4.76 | 8 | 17 | 20 |
| Difficulties Obtaining and Using Insurance (#1) | 7.28 | 7 | 7.93 | 6 | 7.36 | 8 | 7.34 | 8 | 5.12 | 5 | 4.92 | 6 | 20 | 20 |
| Scheduling Challenges (#4) | 7.37 | 6 | 7.94 | 4 | 7.35 | 9 | 7.45 | 6 | 5.09 | 6 | 5.12 | 3 | 21 | 13 |
Note. AIE = American Indian elder.
aRatings were completed on a 10-point scale (1–10), with higher scores indicating more impact on AIE health, greater prevalence among AIEs, or easier changeability, respectively
The cluster rankings facilitated a comparison of the relative perspectives between AIE and professional participants. For example, while the impact ratings for Tribal/National Policy were nearly identical for AIEs and professionals (7.75 and 7.73, respectively), Tribal/National Policy was ranked first on impact for AIEs, but last for professional stakeholders. Conversely, Health-Related Self-Efficacy was ranked high on impact by professionals (rank order of 2), but relatively low by AIEs (rank order of 8). An area of some agreement between AIEs and professionals was found in the high rank order of Insecurity from Lack of Knowledge (3 and 1, respectively). Overall, there was a negative correlation between the impact ratings of AIEs and professional participants (−0.44).
While some variations existed, rankings were generally more consistent between AIEs and professionals on the domains of prevalence and factor changeability, as evidenced by positive correlations of 0.19 and 0.44, respectively. The theme of Family and Emotional Challenges was identified as prevalent among AIEs by both AIE and professional participants (rank orders of 2 and 3, respectively). However, AIEs rated these factors as more malleable than professionals (rank orders of 4 and 9, respectively). In general, for both AIEs and professionals, individual-level factors such as those sorted into the Health-Related Self-Efficacy cluster were perceived to be more easily changeable than system-level factors that included those sorted into Tribal/National Policy and Limited Availability of Services.
An examination of the total rank score indicated that Insecurity from Lack of Knowledge was the overall highest-ranked cluster among AIEs and second highest among professional participants (total rank scores of 8 and 6, respectively). The highest total rank score among professional stakeholders was Health-Related Self-Efficacy (total rank score of 5). Despite having the lowest changeability rank order possible, Tribal/National Policy had the second-highest total rank score among AIEs (total rank score of 11) but was tied for the lowest total rank score among professionals (total rank score of 20).
Discussion
Concept mapping is a community-based mixed-method approach to understanding the perspectives of multiple stakeholders and acting on complex phenomena—in this case: health systems serving AIEs. This methodology integrates both quantitative and qualitative data from diverse perspectives to organize multifaceted problems and identify priority areas for intervention. Our use of this approach facilitated systematic collection and analysis of data about factors affecting AIE access to and utilization of health care from a range of relevant stakeholder groups. Using CM techniques, we collaboratively identified nine key domains perceived to affect whether AIEs can obtain good health care (Figure 1). While conceptually overlapping and intersecting, the domains reflect factors that operate primarily at distinct socioecological levels. The Health-Related Self-Efficacy theme focuses on how individuals navigate health care systems and organizations. Social dynamics with family and health care professionals are reflected in the Family and Emotional Challenges and the Provider Issues and Relationships themes. While tied to larger systems and resource issues, Limited Availability of Services, Accessibility and Transportation Barriers, and Scheduling Challenges relate to community and organizational barriers that AIEs face when trying to access services. System-level factors include Tribal/National Policy and Difficulties Obtaining and Using Insurance. The final domain identified, Insecurity from Lack of Knowledge, spans multiple levels of influence, accentuating the limitations of individual health literacy and the organization- and system-level barriers that make it difficult for AIEs to find, understand, and act on information regarding their health, and health care and insurance options.
Our findings demonstrate limited variability in absolute rating values across participant groups. While not quite as narrow as the current study, a small range of rating scores is common in our previous CM studies (e.g., Aarons et al., 2016). Despite their limited variation, the rating and rank order findings provide valuable information from which to better understand needs and opportunities for improving AIE health care. Overall, the ratings indicate that all nine thematic domains were perceived by both AIE and professional participants as having a large impact on AIEs and their ability to access health care. Likewise, all participants thought the factors associated with each domain were commonly experienced by AIEs.
While there was overall agreement as to the importance and prevalence of all domains, there were some differences in their relative ranking or prioritization between AIE and professional participants, although these differences should be interpreted cautiously given the narrow absolute range of rating values. For example, the top two areas perceived to affect AIE health as rated by AIEs themselves were Tribal/National Policy and Provider Issues and Relationships. Among professionals, the rank orders of those issues were 9 and 7, respectively. Such disparities confirm the importance of considering AIE perspectives separate from those of professional stakeholders, both in understanding AIE access to health care and in prioritizing areas for intervention.
A nexus of agreement between AIEs and professionals was the need to address the theme of Insecurity from Lack of Knowledge. The total rank score among both AIE and professional participants indicated that this theme was viewed as having a high impact on AIE health, very prevalent among AIEs, and relatively changeable compared to other domains. These findings suggest that efforts that target Insecurity from Lack of Knowledge by facilitating navigation of the health system have the potential to make a big impact on AIE health and will likely be favorably received by both AIEs and professional stakeholders. Recent efforts to provide culturally relevant navigation to AI cancer patients feature assistance with decision making, scheduling, transportation, and communication with health care providers and caretakers (Grimes, Dankovchik, Cahn, & Warren-Mears, 2017; Harjo, Burhansstipanov, & Lindstrom, 2014). These efforts have been well received by patients and show promise in increasing community knowledge about health and health care, improving access to care, and avoiding significant delays in diagnosis of serious health conditions (Burhansstipanov et al., 2014). Our CM data are now guiding development of a web-based guide that professional stakeholders (e.g., community health workers), informal social supporters (e.g., family and friends of AIEs), and AIEs themselves can access to obtain tailored and culturally relevant information that may contribute to enhanced access to and use of health care for AIEs. However, research indicates that in-person assistance from trusted individuals who are embedded within communities is indispensable, especially for older adults (Krebs et al., 2013). Tools like our web-based guide are useful in enhancing, rather than replacing, this interpersonal support. Researchers and policymakers must also continue to advocate for the necessary resources to fund, train, and staff in-person support for AIEs.
Apart from prioritizing issues to address in the web-based guide, our findings suggest that substantial improvements in AIE access to and utilization of health care will require actions across multiple domains to allow for organizational or system changes. Efforts to influence Tribal/National Policy, for example, must involve educating tribal leaders about health care and insurance systems and encouraging them to deploy tribal resources to pay for benefits coordination, ombudsmen, and related services that aid elders. Such efforts must also entail advocating for state and federal governments to honor treaty-guaranteed obligations to dedicate resources to AI health, including funding for long-term services and other supports that AIEs need. Likewise, improvements to Accessibility and Transportation Barriers, Scheduling Challenges, and Provider Issues and Relationships must involve multilevel efforts aimed at cultivating health literacy and advocacy skills among AIEs and their caregivers, educating health care providers and staff about the needs of AIEs and best practices to build trust, and demanding system-level investments in workforce and services.
Limitations
This CM study examines factors pertaining to health care access and utilization among AIEs. We did not examine the broader range of factors affecting AIE health using CM methods, although we assess these factors qualitatively elsewhere (Jaramillo, Willging, Haozous, Verney, & Lujan, 2019).
While efforts were made to include many different stakeholders throughout the CM process and to obtain input from the CAB to promote accurate interpretation of findings, the sample sizes are relatively small and there may be biases in the sample of participants such that the findings do not reflect the perspectives of all AIEs or the breadth of professional stakeholders involved in developing and implementing policy or delivering outreach and health care services that affect AIEs. Because participation was based on interest among AIEs recruited in health-focused venues, we likely oversampled AIEs who were not only more likely to access health care, but who also were more willing to voice their opinions about health care than their peers. These were overwhelmingly women. Indeed, reluctance to discuss health concerns among elders in general and men specifically is a common concern (Jaramillo et al., 2019). For this reason, our results may underestimate the impact and prevalence of factors in the Health-Related Self-Efficacy theme, such as “Not being comfortable/confident enough to ask questions.” However, this effect was likely mitigated by the fact that participants were asked to assess each factor among elders in general, rather than for themselves alone. Similarly, the composition of the sample of professional stakeholder participants does not reflect a random selection of persons but resulted from a conscious effort to tap into the viewpoints of a wide range of professionals who provide services or are involved in tribal or administrative leadership. Furthermore, although many professional participants were close relatives of AIEs, we did not specifically sample the informal social supports of AIEs. Overall, limitations of representativeness were likely to be moderated by participants’ familiarity with and concern for AIEs in general.
The multistage CM process requires an intensive commitment of time and attention from both researchers and participants, especially among elderly populations. Although CM studies often assess 80 or more factor statements, we minimized these burdens on participants by utilizing the smallest number of statements possible without dropping factors that were commonly endorsed in the generation phase. This may have contributed to the relatively narrow range of variability evident on the rating scales, since there was already some implicit exclusion of items that were likely lower in perceived importance or prevalence.
Due to the linguistic diversity of AI communities and their proximity to English-speaking populations, individuals targeted for recruitment were generally fluent in English. However, because the CM activities involved reading and writing in English, AIEs who were not completely literate in written English may have declined to participate. Researchers were prepared to administer the MINI-COG (2017) to test for cognitive impairment of potential participants. Although no participants were identified as potentially having cognitive impairment, it is possible that individuals with cognitive or other limitations (e.g., of hearing or vision) may have declined to participate. Finally, the need to redirect some participants to label piles thematically, rather than according to their personal experiences with those factors, may present a limitation of this research.
Conclusion
There is an urgent need to prioritize improvements in health care and health insurance systems for AIEs, a population that is expected to quadruple in size to about 2 million individuals by 2060 (Boccuti et al., 2014). Findings from this CM study underscore the importance of promoting enhancements in health system navigation services, the health care workforce, and state and federal consideration of and consultation with tribal communities. Moreover, this research points to a persistent gap in understandings of the impact and prevalence of factors affecting the health of AIEs and their perceived changeability. This gap is reflected in the majority of existing health policy interventions for this population, which focus predominately on individual-level knowledge (i.e., health literacy) and behavior (e.g., Centers for Disease Control and Prevention, 2009). In contrast, AIE participants in this study emphasized the impact and prevalence of community-, organizational-, and policy-level barriers to accessing health care, indicating the limitations of individually focused improvements. Finally, these findings highlight the value of using the multilevel socioecological perspective to understand the perspectives and experiences of AIEs. Such a perspective is imperative to examining and addressing the complex challenges that affect AIE health.
Funding
This work was supported by a grant from the National Institute on Minority Health and Health Disparities (R01 MD010292-01).
Acknowledgments
The authors wish to thank the Seasons of Care Community Action Board for their valuable contributions to this manuscript.
Author Contributions
D. H. Sommerfeld conceptualized and conducted the concept-mapping analyses, and contributed to the drafting of the manuscript. E. T. Jaramillo and E. Haozous contributed to the drafting of the manuscript. E. Lujan made significant contributions to the conceptualization of the study. E. Lujan and C. E. Willging collected the concept-mapping data presented in this study. C. E. Willging conceptualized the study and contributed to the drafting of the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
None reported.
References
- Aarons G. A., Sommerfeld D. H., Chi B. H., Ezeanolue E. E., Sturke R., Guay L., & Siberry G. K (2016). Concept mapping of PMTCT implementation challenges and solutions across 6 Sub-Saharan African countries in the NIH-PEPFAR PMTCT implementation science alliance. Journal of Acquired Immune Deficiency Syndromes (1999), 72(Suppl. 2), S202–S206. doi:10.1097/QAI.0000000000001064 [DOI] [PubMed] [Google Scholar]
- Adamsen C. (2015). Native fact sheet: Health care coverage by age for American Indian/Alaska Native elders [PDF file]. Retrieved from https://ruralhealth.und.edu/pdf/native-health-care-coverage.pdf
- Artiga S., Arguello R., & Duckett P (2013). Health coverage and care for American Indians and Alaska Natives [PDF file]. Retrieved from https://www.kff.org/disparities-policy/issue-brief/health-coverage-and-care-for-american-indians-and-alaska-natives/
- Artiga S., Ubri P., & Foutz J (2017). Medicaid and American Indians and Alaska Natives [PDF file]. Retrieved from http://files.kff.org/attachment/issue-brief-medicaid-and-american-indians-and-alaska-natives
- Baker D. W., Wolf M. S., Feinglass J., & Thompson J. A (2008). Health literacy, cognitive abilities, and mortality among elderly persons. Journal of General Internal Medicine, 23, 723–726. doi:10.1007/s11606-008-0566-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J., Novins D. K., Whitesell N. R., Spicer P., Mitchell C. M., Manson S. M., & American Indian Service Utilization Psychiatric Epidemiology Risk and Protective Factors Project Team. (2005). Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: Mental health disparities in a national context. American Journal of Psychiatry, 162, 1723–1732. doi:10.1176/appi.ajp.162.9.1723 [DOI] [PubMed] [Google Scholar]
- Boccuti C., Swoope C., & Artiga S (2014). The role of medicare and the Indian Health Service for American Indians and Alaska natives: Health, access and coverage [PDF file]. Retrieved from https://www.kff.org/medicare/report/the-role-of-medicare-and-the-indian-health-service-for-american-indians-and-alaska-natives-health-access-and-coverage/
- Brave Heart M. Y., Chase J., Elkins J., Martin J., Nanez J. X., & Mootz J. J (2016). Women finding the way: American Indian women leading intervention research in Native communities. American Indian and Alaska Native Mental Health Research, 23, 24–47. doi:10.5820/aian.2303.2016.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhansstipanov L., Krebs L. U., Dignan M. B., Jones K., Harjo L. D., Watanabe-Galloway S., … Isham D (2014). Findings from the Native Navigators and the Cancer Continuum (NNACC) study. Journal of Cancer Education, 29, 420–427. doi:10.1007/s13187-014-0694-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canales M. K., Weiner D., Samos M., & Wampler N. S (2011). Multi-generational perspectives on health, cancer, and biomedicine: Northeastern native American perspectives shaped by mistrust. Journal of Healthcare for the Poor and Underserved, 22, 894–911. doi:10.1353/hpu.2011.0096 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2009). Improving health literacy for older adults: Expert panel report 2009 [PDF file]. Retrieved from https://www.cdc.gov/healthliteracy/pdf/olderadults-508.pdf
- Cho Y. I., Lee S. Y., Arozullah A. M., & Crittenden K. S (2008). Effects of health literacy on health status and health service utilization amongst the elderly. Social Science & Medicine, 66, 1809–1816. doi:10.1016/j.socscimed.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Concept Systems Inc (2018). The Concept System (version 2018.284.23) [computer software]. Retrieved from https://conceptsystemsglobal.com
- Conte K. P., Schure M. B., & Goins R. T (2015). Correlates of social support in older American Indians: The Native Elder Care Study. Aging & Mental Health, 19, 835–843. doi:10.1080/13607863.2014.967171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison M. L. (1983). Multi-dimensional scaling. New York: John Wiley & Sons. [Google Scholar]
- Dyste A. (2014). It’s hard out here for an American Indian: Implications of the Patient Protection and Affordable Care Act for the American Indian population. Law & Inequity, 32, 95–133. [Google Scholar]
- Espey D. K., Jim M. A., Cobb N., Bartholomew M., Becker T., Haverkamp D., & Plescia M (2014). Leading causes of death and all-cause mortality in American Indians and Alaska natives. American Journal of Public Health, 104(S3), S303–S311. doi:10.2105/AJPH.2013.301798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox E. (2011). Health care reform: Tracking tribal, federal, and state implementation [PDF file]. Retrieved from http://www.cms.gov/Outreach-and-Education/American-Indian-Alaska-Native/AIAN/Downloads/CMSHealthCareReform5202011.pdf
- Goins R. T., & Pilkerton C. S (2010). Comorbidity among older American Indians: The Native Elder Care Study. Journal of Cross-Cultural Gerontology, 25, 343–354. doi:10.1007/s10823-010-9119-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimes C., Dankovchik J., Cahn M., & Warren-Mears V (2017). American Indian and Alaska Native cancer patients’ perceptions of a culturally specific patient navigator program. The Journal of Primary Prevention, 38, 121–135. doi:10.1007/s10935-016-0458-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harjo L., Burhansstipanov L., & Lindstrom D (2014). Rationale for “cultural” native patient navigators in Indian country. Journal of Cancer Education, 29, 414–419. doi:10.1007/s13187-014-0684-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indian Health Service (2015). Trends in Indian health, 2014 edition [PDF file]. Retrieved from https://www.ihs.gov/dps/includes/themes/newihstheme/display_objects/documents/Trends2014Book508.pdf
- Indian Health Service (2019). IHS profile Retrieved from https://www.ihs.gov/newsroom/factsheets/ihsprofile/
- Jaramillo E. T., Willging C. E., Haozous E., Verney S. P., & Lujan E (2019). ‘Speak your mind and heart in the Indian way’: Wellness and agency among American Indian elders. In Page-Reeves J. (Ed.), Wellness as a multidimensional concept: Understanding connections between culture, community, and health (pp. 193–212). Lanham, MD: Lexington Books of Rowman & Littlefield. [Google Scholar]
- John R., Kerby D. S., & Hennessy C. H (2003). Patterns and impact of comorbidity and multimorbidity among community-resident American Indian elders. The Gerontologist, 43, 649–660. doi:10.1093/geront/43.5.649 [DOI] [PubMed] [Google Scholar]
- Kane M., & Trochim W. M. K (2007). Concept mapping for planning and evaluation. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Kelly C. M., Baker E. A., Brownson R. C., & Schootman M (2007). Translating research into practice: Using concept mapping to determine locally relevant intervention strategies to increase physical activity. Evaluation and Program Planning, 30, 282–293. doi:10.1016/j.evalprogplan.2007.05.007 [DOI] [PubMed] [Google Scholar]
- Kim G., Bryant A. N., Goins R. T., Worley C. B., & Chiriboga D. A (2012). Disparities in health status and health care access and use among older American Indians and Alaska natives and non-Hispanic Whites in California. Journal of Aging and Health, 24, 799–811. doi:10.1177/0898264312444309 [DOI] [PubMed] [Google Scholar]
- Kim H., & Xie B (2016). Health literacy and internet- and mobile app-based health services: A systematic review of the literature. Computer Science, 52, 1–4. doi:10.1002/pra2.2015.145052010075 [Google Scholar]
- Krebs L., Burhansstipanov L., Watanabe-Galloway S., Pingatore N., Petereit D., & Isham D (2013). Navigation as an intervention to eliminate disparities in American Indian communities. Seminars in Oncology Nursing, 29, 118–127. doi:10.1016/j.soncn.2013.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy K. R., Bibeau D., Steckler A., & Glanz K (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351–377. doi:10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- Roh S., Burnette C. E., Lee K. H., Lee Y. S., Easton S. D., & Lawler M. J (2015). Risk and protective factors for depressive symptoms among American Indian older adults: Adverse childhood experiences and social support. Aging & Mental Health, 19, 371–380. doi:10.1080/13607863.2014.938603 [DOI] [PubMed] [Google Scholar]
- Rosas S. R., & Kane M (2012). Quality and rigor of the concept mapping methodology: A pooled study analysis. Evaluation and Program Planning, 35, 236–245. doi:10.1016/j.evalprogplan.2011.10.003 [DOI] [PubMed] [Google Scholar]
- Rubin D. L., Freimuth V. S., Johnson S. D., Kaley T., & Parmer J (2014). Training meals on wheels volunteers as health literacy coaches for older adults. Health Promotion Practice, 15, 448–454. doi:10.1177/1524839913494786 [DOI] [PubMed] [Google Scholar]
- Schensul S. L., Schensul J. J., & LeCompte M. D (1999). Essential ethnographic methods: Observations, interviews, and questionnaires. New York: Altamira Press. [Google Scholar]
- Schieb L. J., Ayala C., Valderrama A. L., & Veazie M. A (2014). Trends and disparities in stroke mortality by region for American Indians and Alaska natives. American Journal of Public Health, 104(S3), S368–S376. doi:10.2105/AJPH.2013.301698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonds V. W., Goins R. T., Krantz E. M., & Garroutte E. M (2014). Cultural identity and patient trust among older American Indians. Journal of General Internal Medicine, 29, 500–506. doi:10.1007/s11606-013-2578-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner D. (2016). The politics of native American Health Care and the Affordable Care Act. Journal of Health Politics, Policy and Law, 41, 41–71. doi:10.1215/03616878-3445601 [DOI] [PubMed] [Google Scholar]
- Smith-Kaprosy N., Martin P. P., & Whitman K (2012). An overview of American Indians and Alaska natives in the context of social security and supplemental security income. Social Security Bulletin, 72, 1–10. [PubMed] [Google Scholar]
- Towne S. D. Jr., Smith M. L., & Ory M. G (2014). Geographic variations in access and utilization of cancer screening services: Examining disparities among American Indian and Alaska native elders. International Journal of Health Geographics, 13, 18. doi:10.1186/1476-072X-13-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upper Midwest Rural Health Research Center (2007). Health insurance coverage and access to health care for American Indian and Alaska Native Elders [PDF file]. Retrieved from http://ruralhealth.und.edu/pdf/umrhrc_policybrief1007.pdf
- Veazie M., Ayala C., Schieb L., Dai S., Henderson J. A., & Cho P (2014). Trends and disparities in heart disease mortality among American Indians/Alaska Natives, 1990–2009. American Journal of Public Health, 104(S3), S359–S367. doi:10.2105/AJPH.2013.301715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verney S. P., Jervis L. L., Fickenscher A., Roubideaux Y., Bogart A., & Goldberg J (2008). Symptoms of depression and cognitive functioning in older American Indians. Aging & Mental Health, 12, 108–115. doi:10.1080/13607860701529957 [DOI] [PubMed] [Google Scholar]
- Warne D., Delrow D., Angus-Hornbuckle C., & Shelton B. L (2017). Impact of ACA repeal on American Indians and Alaska natives [PDF file]. Retrieved from http://files.constantcontact.com/a3c45cb9201/38e0f51f-647b-4ed6-a79b-2e55f2afa6d6.pdf
- White S. (2008). Assessing the nation’s health literacy: Key concepts and findings of the National Assessment of Adult Literacy (NAAL) [PDF file]. Retrieved from http://www.ama-assn.org/ama1/pub/upload/mm/367/hl_report_2008.pdf
- Willging C. E., Sommerfeld D. H., Jaramillo E. T., Lujan E., Bly R. S., Devenport E. K., … Lujan R (2018). Improving native American elder access to and use of health care through effective health system navigation. BMC Health Services Research, 18, 464. doi:10.1186/s12913-018-3182-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willging C. E., Waitzkin H., & Wagner W (2005). Medicaid managed care for mental health services in a rural state. Journal of Healthcare for the Poor and Underserved, 16, 497–514. doi:10.1353/hpu.2005.0060 [DOI] [PubMed] [Google Scholar]
- Windsor L. C. (2013). Using concept mapping in community-based participatory research: A mixed methods approach. Journal of Mixed Methods Research, 7, 274–293. doi:10.1177/1558689813479175 [DOI] [PMC free article] [PubMed] [Google Scholar]