Summary
Multiple professional groups and societies worldwide have produced airway management guidelines. These are typically targeted at the process of tracheal intubation by a particular provider group in a restricted category of patients and reflect practice preferences in a particular geographical region. The existence of multiple distinct guidelines for some (but not other) closely related circumstances, increases complexity and may obscure the underlying principles that are common to all of them. This has the potential to increase cognitive load; promote the grouping of ideas in silos; impair teamwork; and ultimately compromise patient care. Development of a single set of airway management guidelines that can be applied across and beyond these domains may improve implementation; promote standardisation; and facilitate collaboration between airway practitioners from diverse backgrounds. A global multidisciplinary group of both airway operators and assistants was assembled. Over a 3‐year period, a review of the existing airway guidelines and multiple reviews of the primary literature were combined with a structured process for determining expert consensus. Any discrepancies between these were analysed and reconciled. Where evidence in the literature was lacking, recommendations were made by expert consensus. Using the above process, a set of evidence‐based airway management guidelines was developed in consultation with airway practitioners from a broad spectrum of disciplines and geographical locations. While consistent with the recommendations of the existing English language guidelines, these universal guidelines also incorporate the most recent concepts in airway management as well as statements on areas not widely addressed by the existing guidelines. The recommendations will be published in four parts that respectively address: airway evaluation; airway strategy; airway rescue and communication of airway outcomes. Together, these universal guidelines will provide a single, comprehensive approach to airway management that can be consistently applied by airway practitioners globally, independent of their clinical background or the circumstances in which airway management occurs.
Keywords: airway management, anaesthesia, emergency medicine, intensive care, prehospital
What other guidelines are available on this topic?
Worldwide, several professional groups and societies have produced airway management guidelines. Most of these efforts have targeted a particular provider group and category of patients, and reflect practice preferences in a particular geographical region. Typically, application of these guidelines is restricted to circumstances where the intended airway is a tracheal tube and management challenges are either anticipated or have already been encountered.
Why is this guideline being developed?
Irrespective of the discipline of practitioners conducting airway management or the context in which this is being performed, the underlying principles governing airway decision‐making remain constant. The universal airway guidelines aim to promote safe and effective management of airways by application of these principles to all episodes of airway management by teams of airway practitioners across all disciplines. In addition to making recommendations easier to recall and implement, emphasising common principles is intended to facilitate standardisation and collaboration across disciplines and locations as well as providing consistent guidance to airway practitioners, regardless of context. This includes circumstances for which no specific guidelines currently exist. These universal airway guidelines also aim to highlight areas where evidence for best practice is incomplete and guide future research.
Consistent with previous publications, the term ‘airway management’ in these guidelines refers to techniques that predominantly relate to the extrathoracic airway, performed by specially trained airway practitioners.
How will this differ from existing guidelines?
This guideline has been developed to be consistently applied to any episode of airway management undertaken by trained airway practitioners, whether routine or challenging, without restriction to a specific provider background, patient type or geographical region and independent of the intended airway type or other contextual factors (Table 1). It incorporates the most recent concepts in airway management, including statements on areas not widely addressed by the existing guidelines.
Table 1.
Domains across which the Project for Universal Management of Airways (PUMA) guidelines are intended to be applied.
| Domain | Examples | |
|---|---|---|
| Geography | Country of practice | |
| Provider | Anaesthetists; emergency physicians; pre‐hospital physicians; intensivists; neonatologists; paramedics; surgeons; respiratory therapists; nurse anaesthetists; airway assistants (both qualified and trainees) | |
| Patient | Adult; paediatric; obstetric; trauma; critically ill; requiring precautions against airborne pathogen transmission | |
| Context | Location | Emergency department; intensive care unit; operating room; non‐operating room anaesthesia locations (e.g. radiology; cardiology; endoscopy); wards, prehospital |
| Indication | Surgery; procedures; resuscitation; transport; diagnostic imaging; respiratory compromise; decreased conscious state | |
| Urgency | Emergency; urgent; elective | |
| Complexity | Straightforward; challenging (both anticipated and unanticipated) | |
| Intended airway | Facemask; supraglottic airway; tracheal tube; front‐of‐neck airway | |
Disclaimer
These guidelines do not represent minimum standards of practice nor are they a substitute for sound clinical judgement. Although they articulate key principles to inform clinical practice, there may be legitimate reasons that providers select alternative approaches in certain contexts. All recommendations assume that airway practitioners have appropriate training and experience with the relevant devices and techniques.
Introduction
Guidelines for cardiopulmonary resuscitation practice have long been co‐ordinated by groups of global experts leading to relative standardisation of care across all geographies, providers, patient types and clinical circumstances. More recently, a similar approach has been taken to the management of sepsis [1]. In contrast, guidelines for airway management have traditionally been independently developed by professional groups or societies representing a particular geographical region and/or practitioner group, with different guidelines being intended for application to specific patient types or contexts [2, 3]. Since the ASA published its original Practice Guidelines for Management of the Difficult Airway in 1993 [4], there has been a profusion of distinct guidelines, each targeting specific patient groups (adult; paediatric; obstetric; trauma; critically ill; obese), particular clinical disciplines (anaesthesia; emergency medicine; intensive care medicine; prehospital care) and reflecting practice preferences in discrete geographical regions [3]. Typically, each addresses the circumstance in which challenges managing the airway are anticipated or have arisen, without necessarily explicitly reinforcing standard principles to be embedded in routine episodes of airway management.
Limitations of context‐specific guidelines
Individually, the current airway guidelines are valuable tools promoting safe, effective care in the defined contexts that each addresses. However, by approaching each distinct airway management situation in isolation, collectively these documents have the potential to obscure the common principles each advocates, that are applicable to all airway management decisions. This may impede shared learning between specialty areas and compromise cognitive efficiency. The human brain seeks pattern recognition, particularly in time‐pressured situations [5]. Attempts to memorise, recall and implement multiple separate protocols for closely related circumstances as if they were unique events creates the potential for confusion and contributes to cognitive overload [3, 6, 7]. Embedding the common themes present in existing guidelines [3] into a single resource and highlighting a limited number of situation‐specific caveats and exceptions should help optimise real‐world performance.
The specificity of traditional guidelines also restricts their application beyond the circumstances for which they have been developed. References to ‘induction of general anaesthesia’ and ‘surgery’ in anaesthesia‐oriented guidelines [8] for example, can diminish their perceived relevance to airway practitioners working in other disciplines. This specificity also provides a potential source of ambiguity in situations to which multiple guidelines could reasonably apply [9]. Conversely, the existing guidelines do not address several common circumstances, most notably use of a supraglottic airway rather than a tracheal tube as the intended device in elective operating room airway management. With rare exceptions, current guidelines deal exclusively with the situation where the goal of airway management is tracheal intubation. This focus on tracheal intubation dates back to the original published failed tracheal intubation drill by Tunstall in 1976 [10]. Furthermore, the designation of most current guidelines as applying to management of the ‘difficult’ airway implies, perhaps unintentionally, that they do not relate to more routine situations. As ‘difficulty’ is a subjective concept, this may compromise the ability of an airway management team to identify the trigger for implementing the guideline. An emphasis on the core principles of airway management in both straightforward and challenging situations avoids this unnecessary distinction. Reinforcing familiarity with safe practice in everyday settings not only makes recall and implementation easier during evolving airway crises but may contribute to prevention of such incidents.
While providers from different disciplines often practice airway management independently, they may be called upon to collaborate at short notice in the most challenging of circumstances. The requirement for airway practitioners from disparate backgrounds to be able to work together effectively under stressful circumstances has been starkly highlighted by the severe acute respiratory syndrome coronavirus disease‐2 (SARS‐CoV‐2) pandemic. It is also apparent in more routine circumstances, however, particularly when patient, team or situational challenges complicate airway management. In the absence of a shared underlying framework for managing the airway, such interactions can be seriously impeded. Having distinct guidelines for providers practising in different clinical situations may also contribute to the development of silos between disciplines and risks promoting tribalism by reinforcing the idea that the principles of airway management fundamentally differ in each of these contexts [9]. Options phrased as ‘waking’ the patient [8, 11] in anaesthesia‐oriented guidelines may conceal the applicability of the broader principle to which such statements refer, in contexts where return to full consciousness is less likely or not possible. This is particularly so when ‘waking’ is linked to actions such as ‘cancelling surgery’ [8] with the implication that the impending requirement for airway management can be circumvented, an option typically unavailable in critically unwell patients. As a result, when referring to such guidelines, the opportunity and value of restoring the patient’s ability to maintain their own airway and ventilation, even temporarily, may be underappreciated by disciplines exclusively involved in emergency airway management, leading this to be dismissed as ‘never an option for us’. Even within a specialty, practitioners working as airway assistants may be unfamiliar with the decision‐making algorithms employed by the airway operators working alongside them.
Airway practitioners from a given clinical background also commonly practice in multiple settings either contemporaneously or over the course of their career. This might involve working in different institutions; different geographical regions; or different contexts for care (e.g. in‐hospital versus retrieval). It is recognised that even within a given discipline working in a single geographical region, significant heterogeneity may exist in the algorithms used for airway management [12, 13]. Standardised practice improves outcomes [14] and it is reasonable to expect that creating a mutual template for all episodes of airway management that encourages consistent practice across all these domains could improve performance.
Variations in the format of the regional guidelines may provide another source of confusion. The familiar ‘Plan ABCD’ nomenclature used in some guidelines [11, 15, 16], prioritises sequencing over clarity regarding the category of airway device being attempted. For example, when addressing airway rescue, reference to ‘Plan B’ in the Difficult Airway Society guidelines is synonymous with use of a supraglottic airway [11, 16] whereas ‘Plan B’ in the 2013 Canadian Airway Focus Group Guidelines refers to an “alternative approach to intubation” [15]. This inconsistency is even more pertinent in the situation referred to above, when ‘Plan A’ is to use a supraglottic airway. The broader impact of variations in terminology between different guidelines has been discussed in detail elsewhere [9, 13, 17, 18, 19].
The geographical specificity of guidelines creates other challenges. Many countries have not developed their own national guidelines and the assumption that those from other regions are readily transferrable ignores regional differences in processes and resource availability. Access to pulse oximetry; waveform capnography; videolaryngoscopy; or even flexible bronchoscopy might be assumed in most airway management settings in high‐ and upper‐middle–income countries but recommendations regarding use of such items in lower‐middle–income or low‐income countries may need to be recognised as aspirational. By enhancing the relevance of recommendations to current airway practice in these settings, such an acknowledgment may also provide a mechanism for airway practitioners in resource‐poor environments to promote access to these technologies in the future. This aligns with the goals of programs such as the Global Oximetry Initiative [20] and Global Capnography Project [21] to create international standards for safe patient care.
Developing universal principles
The mission of the Project for Universal Management of Airways (PUMA) is to elucidate a set of principles that are not only internationally consistent but can be applied by trained airway practitioners across all disciplines and in all contexts, during both routine and more challenging episodes of airway management (Table 1). With the exception of the context of skill‐acquisition (by either fully qualified airway practitioners or trainees), which may demand judicious modification of some principles under expert supervision or in carefully selected patients, the intention is for the PUMA recommendations to have utility for all airway practitioners. This includes trainees, particularly when they are practising independent of direct supervision. Note that while some principles relating to use of a facemask or supraglottic airway may be relevant to clinicians with limited airway experience who are called upon to provide emergency airway support in the context of urgent resuscitation situations (e.g. respiratory or cardiac arrest), these guidelines have not been developed for this purpose. Rather they are intended exclusively for use by specially trained airway practitioners (Table 1) for whom advanced airway management forms a regular part of their practice.
To address the complete scope of airway management scenarios encompassing both elective and emergency situations, a universal resource must be applicable regardless of the intended airway (facemask; supraglottic airway; tracheal tube; or front‐of‐neck airway), the initial airway (e.g. facemask ventilation before tracheal intubation) or the sequence in which rescue attempts are made if airway management becomes challenging. A traditional linear algorithm cannot accomplish this. Furthermore, identical approaches cannot be advocated in all contexts. Different patient populations are predisposed to requiring certain interventions (e.g. rapid sequence intubation) while some interventions are often impractical in particular scenarios (e.g. awake tracheal intubation in children; deferring airway management in emergency situations). Conversely, variations in skill, resources and other factors may result in airway practitioners legitimately adopting different approaches despite being faced with similar patient‐related challenges. Finding common ground between these varied contexts on which to base universal recommendations is less reliant on making compromises than on understanding the reasons behind such distinctions. It is the principles of management and not the specific interventions undertaken in a particular clinical circumstance that must be standardised. Accordingly, while emphasising consistent principles, a universal airway resource must retain the flexibility to allow variations in practice in different contexts based on good clinical judgement. The PUMA guidelines aim to be a unifying resource that complements, rather than competes, with the existing guidelines.
Human factors (ergonomics) refers to the science of understanding and optimising the interactions between humans and other elements in a system [22]. Non‐technical (‘teamwork’) skills represent only one component of this area of study [23]. In recognition of the importance of human factors considerations to safe airway management [23, 24, 25, 26] and their interplay with technical issues, statements on this area stand alongside those addressing the technical aspects of airway management in relation to each topic covered, rather than being relegated to a discrete human factors section.
The PUMA guidelines will be presented across five separate documents as outlined in Table 2.
Table 2.
Components of the universal airway guidelines.
| Part 1: concept and methods | Why and how were the guidelines developed? |
| Part 2: universal guidelines for evaluating risks of airway management | What are the issues? |
| Part 3: universal guidelines for airway strategy | What approach should be used? |
| Part 4: universal guidelines for airway rescue | What if things go wrong? |
| Part 5: universal guidelines for communication of airway outcomes | What and how should the next person be told? |
Limits on scope
The primary goal of PUMA is to reconcile apparent conflicts and identify consensus among the existing guidelines. As such, in areas such as awake tracheal intubation and airway emergencies occurring in patients with existing tracheostomies/laryngectomies, for which only a limited number of dedicated guidelines exist [27, 28], statements are confined to addressing gaps in the existing recommendations or providing comments to facilitate their universal application. For more detailed information in relation to these areas, readers are referred to the original guidelines. Recommendations in relation to fasting, tracheostomy care, lung isolation or mandatory equipment lists are beyond the scope of this project.
While standardisation of the terminology used in airway management represents an important area [17], the diverse language used in the existing guidelines [3, 13] provided little basis for identifying consensus. Formulating universal terminology requires a methodology distinct from that adopted for this project. As such, the PUMA guidelines have used the dominant legacy terms from the literature whenever possible, only introducing novel terms in select cases when it was considered that legacy terms were unsatisfactory due to their potential to compromise the clarity of communication and impact the safety or efficacy of patient care. Use of legacy terms perceived to predispose to divergence of the language of the academic literature from that most suited to clinical practice has also been avoided. All key terms used in the PUMA guidelines are defined in an online PUMA glossary (https://www.UniversalAirway.org/glossary) which will be available once the final manuscripts are published. Each term in the glossary is supplemented by a list of any other terms in common use in the literature that the PUMA working group would consider equivalent in meaning and comments on their relative merits as ‘critical language’ [17]. This glossary is intended to model a desirable template for airway terminology but does not reflect universal consensus in relation to this. It is hoped it will be a useful resource for future projects attempting to develop a universal lexicon for airway management [9].
Methods
The 14‐member PUMA working group (https://www.UniversalAirway.org/workinggroup) was assembled in 2016. Members were selected to ensure representation by widely published airway clinicians with backgrounds in anaesthesia, intensive care medicine, emergency medicine and pre‐hospital care from Asia, Australasia, Europe and North America – regions from which the existing published guidelines have originated. To complement the working group, a larger and more diverse advisory group of over 60 individuals was also recruited. The advisory group included airway assistants; human factors experts; neonatologists; nurse anaesthetists; surgeons; respiratory therapists; and paramedics, as well as incorporating airway practitioners across multiple disciplines from additional locations, including Africa and South America (https://www.UniversalAirway.org/advisorygroup). Many of the working and advisory group members were contributing authors of the reviewed guidelines, but for the purposes of this project, none acted as representatives of their respective societies.
Working group members met on average every two weeks via videoconference as well as several face‐to‐face meetings over a 3‐year period from 2017 to 2020. A quorum required at least 50% of working group members, including the presence of the executive chair (CH) or project director (NC) as well as a member representing each of anaesthesia, intensive care medicine and emergency medicine. All videoconferences were recorded and made available for review by the working group members.
The process for developing the PUMA guidelines (Fig. 1) conforms to most of the criteria specified in the appraisal of guidelines research and evaluation checklist [29]. Following an initial series of meetings to define terms of reference and methodology, 24 international English‐language airway management guidelines authored by national professional airway groups and published in peer reviewed journals since 2005 were reviewed (the ‘existing guidelines’ – online Supporting Information, Appendix S1). A white paper was drafted listing common themes, recommendations and decisions identified in these guidelines and specifying areas of consensus and divergence between them. Issues addressed by only a minority of the guidelines and areas where divergent recommendations existed were also noted. This white paper was used as the basis from which to generate a series of ‘normalised statements’ articulating consensus between the guidelines. Wherever divergence was identified between the existing guidelines, an attempt was made to delineate a broader unifying principle on which consensus existed from which to develop a normalised statement. Finally, working group members were invited to submit any additional issues that they felt should be addressed on which the existing guidelines were silent. Using these and issues in the white paper that were only addressed by a minority of guidelines, a series of ‘novel statements’ were also developed.
Figure 1.
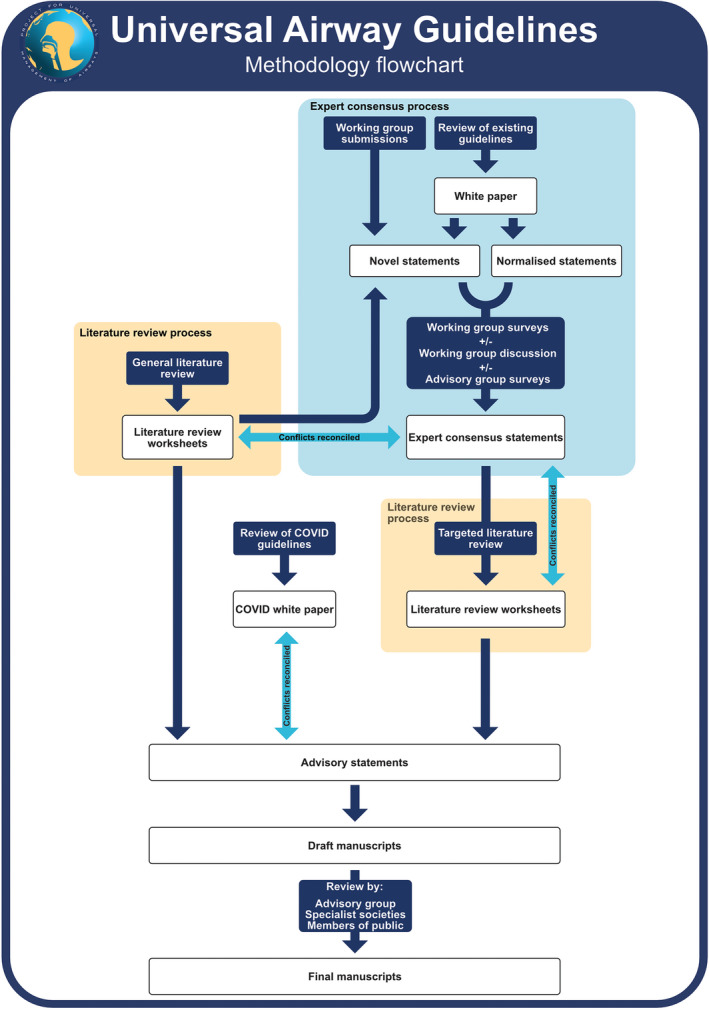
Summary flowchart of the methodology used in the development of these guidelines. COVID, coronavirus disease 2019.
Following the outbreak of the SARS‐CoV‐2 pandemic, six additional coronavirus disease 2019 (COVID‐19) guidelines relating specifically to airway management in patients requiring precautions against airborne pathogen transmission were identified and reviewed (‘COVID‐19 guidelines’; online Supporting Information, Appendix S2). A ‘COVID‐19 white paper’ was drafted incorporating these COVID‐19‐specific guidelines and reconciled against previously generated advisory statements to ensure that no conflicts existed.
There are many areas of airway practice on which providers seek guidance where evidence for best practice is lacking or highly context specific. In recognition of this, a formal process to establish expert consensus among the PUMA working group on each of these statements was conducted to supplement the literature review.
Expert consensus process
Over a period of 2 years, statements derived from the above process were incorporated into detailed, themed electronic surveys and circulated to working group members. Agreement was rated on a Likert scale from 1 (strongly disagree) to 5 (strongly agree). Additional free text comments, including relevant references, could also be submitted. All responses were reviewed and collated by the project director and at least one other member of the working group. On the basis of the feedback provided, the circulated statements were categorised as ‘accepted’ (mean Likert score ≥4 and ≥70% of working group members rating ≥4) or ‘requiring further review’. Some statements that would otherwise have been regarded as accepted according to Likert scores alone were also subjected to further review based on the free text comments received or when a skewed distribution of responses among clinicians from different geographies or specialties was observed.
During scheduled videoconferences, statements requiring review were discussed in an effort to achieve consensus. This discussion was supplemented by extensive text‐based debate between videoconferences, using email or electronic collaboration platforms to allow input from working group members unable to attend a particular videoconference. Both videoconference and electronic text‐based discussions were moderated by the project director. Where issues were identified with content or phrasing, statements were either refined or rejected according to the consensus of the working group. If necessary, statements were subjected to repeat rounds of feedback via the above electronic survey process. When consensus among the working group could not be reached or where consensus in the guidelines could not be identified in relation to a statement (which by definition included statements on novel areas), the input of advisory group members was obtained using similar electronic surveys to those described above before making a final decision to accept, modify or reject a statement. Even in areas where the existing guidelines demonstrated widespread consensus in relation to tracheal intubation, they were often silent on the same issue in relation to facemask ventilation or placement of a supraglottic airway, necessitating advisory group review. As such, the majority of statements drafted met these criteria and were subjected to review by members of the advisory group. All feedback from the advisory group was reviewed by members of the working group and any significant discrepancies between the advisory group opinion and a working group expert consensus statement prompted further working group discussion before the decision to accept, reject or modify the statement was finalised. If the working group experienced particular difficulty in achieving consensus, internationally recognised experts in that area, drawn from the advisory group, were invited to discuss the issue with the working group at specially convened videoconferences. The above process yielded expert consensus statements on areas commonly addressed in guidelines as well as on novel areas.
Literature review process
A directed rather than systematic review of the literature was conducted. The first component of this process was performance of a general literature review, directed at terms related to major airway‐related topics and analogous to that outlined in the methods of many of the existing guidelines. This was supplemented by a more targeted literature search, using search terms directed at each individual expert consensus statement, to evaluate their validity. The initial literature search was conducted in December 2018 and repeated periodically until October 2020, incorporating additional search terms relevant to the targeted component of the review, as expert consensus statements were generated.
Topics addressed in the existing guidelines [8, 11, 15, 54] were taken to be supported by the evidence on which these guidelines were based. The release of the 2013 ASA guidelines [8] marked the onset of an acceleration in the publication of airway guidelines, with between one and seven guidelines being published annually and only four of the existing guidelines having been published before this. As such it was determined that the overwhelming majority of the existing guidelines could be relied upon to have thoroughly reviewed the literature before the publication date of papers captured by the literature review performed for the 2013 ASA guidelines. Each year beyond this, however, the rapid rate of guideline publication resulted in a significant decline in the proportion of the existing guidelines that had reviewed the more recent literature. Based on a conservative estimate, this provided an inherited literature review before the start of 2012 for topics derived from the existing guidelines. For these topics, the literature search was therefore limited to articles published from January 2012 to October 2020. For specific issues on which the existing guidelines were silent and for which there was therefore no inherited literature review, however, no restriction was placed on the publication date for the literature review. The databases used for literature searches were chosen by individual reviewers and included Medline; PubMed; EMBASE; Ovid; ResearchGate; Google Scholar and the Cochrane Central Register of Controlled Trials.
Topics identified in the white paper as the common areas addressed by the existing guidelines were assigned to members of the working group in pairs, comprised where possible of clinicians with different geographical and clinical backgrounds. Expert consensus statements were also categorised according to these topics and provided to the reviewing pairs. Searches were conducted using terms chosen by each reviewing pair based on their allocated topics and the expert consensus statements relevant to these. In addition to the restrictions on publication date outlined above, a number of other filters were placed on searches (online Supporting Information, Appendix S3). Reviewers were also instructed to hand search the references of the existing guidelines, as well as any retrieved airway‐related review articles, for papers relevant to their assigned topics. Articles retrieved that were potentially relevant to another pair of reviewers were sent to them for consideration.
The abstracts retrieved were screened by the working group pairs and relevant full‐text articles were retrieved for review. Additional articles were retrieved by cross‐referencing of articles from both the topic‐based and targeted literature reviews, as well as by hand searching of references in retrieved articles. Full‐text articles were reviewed using a purpose‐generated standardised template for critical appraisal (online Supporting Information, Appendix S4) to ensure a consistent process for critical evaluation of the literature between reviewers. Where a reviewer was the author of a retrieved paper, it was referred to the project lead for allocation to an alternate reviewer. Worksheets containing the results of the literature review as well as full copies of the papers reviewed were made available to the whole working group using a file hosting service. This process produced a detailed review of the literature in relation to all areas in which the evidence base of the of the existing guidelines could not be relied upon. Where literature review identified any areas on which an expert consensus statement had not previously been made, a statement was drafted and subjected to the expert consensus process described above.
Having independent processes for performing a general topic‐based literature review, determination of expert consensus on drafted statements and literature‐based evaluation of these statements allowed for discrepancies between any of these to be readily identified. This was used as an additional mechanism to identify potential areas of misinterpretation or bias. Such discrepancies prompted a process to reconcile them based on further critical appraisal of the literature via circulation of the relevant articles and the associated critical appraisal worksheets to the whole working group for further review. Specific questions pertinent to the discrepancy were also posed to relevant members of the advisory group. Subsequent videoconference debate taking into account this information was then undertaken by the working group before arriving at a final statement. From the above processes, manuscripts were drafted and the advisory statements therein were categorised according to level of evidence and strength of recommendation using the American Heart Association classification system [55]. Areas where evidence is lacking have been highlighted as potential areas for future research.
A draft of the manuscripts will be distributed to members of the advisory group, chosen to reflect an appropriate clinical and geographical diversity, as well as to representatives of relevant professional airway organisations for comment. Input will also be sought from human factors experts in the advisory group. Public consultation will be undertaken in accordance with the Royal College of Anaesthetists process for obtaining lay person review. All feedback was reviewed by members of the working group before completion of the final manuscripts.
Limitations
While every effort was made to ensure the guideline development process was as robust as possible, a number of limitations must be acknowledged. First, the working group is self‐selected, anaesthesia‐dominated and does not include representation by practitioners from a number of clinical disciplines involved in airway management or all countries. While more diverse than the authorship groups of most of the existing guidelines, this remains a potential source of bias. Consultation with the larger and more diverse advisory group aimed to limit this. Second, no formal process was adopted for selecting or ensuring diversity in the advisory group. As such, practitioners from certain regions and/or clinical disciplines may have been overlooked, further resulting in bias. Third, while a structured process was used to generate expert consensus statements, this involved a customised approach rather than a formal Delphi technique. Fourth, the development of expert consensus statements before the targeted literature review could potentially have biased the evidence generated from this review. The parallel performance of a general topic‐based literature review and a structured process for reconciling any conflicts between this and the expert consensus statements was intended to minimise this. Fifth, consistent with the methodology of most of the existing guidelines, a directed rather than structured, methodologically rigorous systematic review of the literature was performed. For issues addressed by the existing guidelines, the literature reviews performed for the 19 existing guidelines published after January 2013 were relied on as the evidence base before January 2012. Sixth, the use of impact factor as a filter during the literature search (online Supporting Information, Appendix S3) could potentially have excluded relevant papers from lower impact factor journals. Seventh, challenges in conducting high‐quality research on airway emergencies and lack of generalisability or flawed methodology of some studies resulted in gaps in the literature that required some recommendations to be based on expert consensus rather than being evidence‐based. Finally, for logistical reasons it will only be feasible to consult with members of the public in the UK, biasing the feedback on a document intended for international application.
Conclusion
The PUMA guidelines address four core areas: evaluation; strategy; rescue; and communication of outcomes. Together, these comprise a comprehensive approach to airway management. Over a 3‐year period, a review of the existing guidelines and primary literature was combined with a structured process for achieving expert consensus, involving consultation with airway practitioners (both operators and assistants) from a wide spectrum of clinical and geographical backgrounds worldwide. It is hoped that providing a single set of guidelines that can be universally applied across clinical discipline, patient type, geographical region and context of care will clarify core management principles, increase opportunities for shared learning between airway practitioners from different backgrounds and improve safe and effective patient care.
Translation of management principles into practice is recognised by the PUMA working group to be an important factor in improving safe patient care. A second phase of the PUMA initiative, directed at developing a free, universally accessible education program to train airway management teams in the implementation of the PUMA guidelines is planned.
It is hoped that future iterations of the PUMA guidelines will at minimum involve formal representation from the national professional airway groups who have produced the existing guidelines. Ideally, organisations representing additional disciplines and geographical locations will also be engaged. The first review is intended to be undertaken no later than 2030.
Supporting information
Appendix S1. Reviewed airway management guidelines (existing guidelines).
Appendix S2. Reviewed COVID‐19 airway management guidelines (COVID‐19 guidelines).
Appendix S3. Details of the search strategies.
Appendix S4. Standardised critical appraisal template.
Acknowledgements
Additional information on the project is available at https://www.UniversalAirway.org. The authors would like to thank Dr C. Noonan for his input into development of the standardised critical appraisal template (online Supporting Information, Appendix S4). NC is the creator of the ‘Vortex Approach’ but has no financial interest in this material, which is licensed under a Creative Commons Attribution‐NonCommercial‐NoDerivatives 4.0 International License. NC has undertaken unpaid consultancy work for Verathon Inc. NC’s partner is employed by Verathon Inc. and he has accompanied her to a corporate retreat funded by Verathon Inc. AH is Treasurer of the Difficult Airway Society. RG is past president of the European Airway Management Society. PAB is the owner of Airway Simulation Ltd which manufactures the ORSIM® bronchoscopy simulator. CR is an independent contractor for Teleflex Inc. and also assists in the development and teaching of procedural skills labs. JS is faculty on The Difficult Airway Course; Associate Editor of Walls Manual of Emergency Airway Management; Associate Editor, Airway Management in Emergencies, Author UpToDate Chapter: RSI for Adults Outside the Operating Room; Author UpToDate Chapter: Emergency Cricothyrotomy; Consultant to Verathon Inc. MS has received paid consultancy from Teleflex Medical, Verathon Medical and DEAS Italia, is a patent co‐owner (no royalties) of DEAS Italia and has received lecture grants and travel reimbursements from MSD Italia, MSD USA. CAH has received research support from Ambu, Karl Storz Endoscopy and Vyaire Medical. She has been a speaker for Karl Storz Endoscopy and has received honoraria from UpToDate and Elsevier. No other external funding or competing interests declared.
This article accompanies an editorial by Ahmad et al. Anaesthesia 2020; 75: 1570–3
The copyright line for this article was changed on 3 December 2020 after original online publication.
Contributor Information
N. Chrimes, Email: nicholaschrimes@gmail.com, @NicholasChrimes.
A. Higgs, @AndyHiggsGAA.
J. A. Law, @jadamlaw.
P. A. Baker, @PaulBakerORSIM.
R. M. Cooper, @gaspasser.
G. Kovacs, @kovacsgj.
S. N. Myatra, @SheilaMyatra.
E. P. O'Sullivan, @ProfEllenO.
W. H. Rosenblatt, @AirwayOnDemand.
C. H. Ross, @crossermed.
J. C. Sakles, @JohnCSakles.
M. Sorbello, @SorbelloMax.
C. A. Hagberg, @CarinHagberg.
References
- 1. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Critical Care Medicine 2017; 45: 486–552. [DOI] [PubMed] [Google Scholar]
- 2. Frova G, Sorbello M. Algorithms for difficult airway management: a review. Minerva Anestesiologica 2009; 75: 201–9. [PubMed] [Google Scholar]
- 3. Edelman DA, Perkins EJ, Brewster DJ. Difficult airway management algorithms: a directed review. Anaesthesia 2019; 74: 1175–85. [DOI] [PubMed] [Google Scholar]
- 4. Practice guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 1993; 78: 597–602. [PubMed] [Google Scholar]
- 5. Tay SW, Ryan P, Ryan CA. Systems 1 and 2 thinking processes and cognitive reflection testing in medical students. Canadian Medical Education Journal 2016; 7: e97–e103. [PMC free article] [PubMed] [Google Scholar]
- 6. LeBlanc V. The effects of acute stress on performance: implications for health professions education. Academic Medicine 2009; 84: S25–33. [DOI] [PubMed] [Google Scholar]
- 7. Szulewski A, Howes D, van Merrienboer JJG, Sweller J. From theory to practice: the application of cognitive load theory to the practice of medicine. Academic Medicine 2020. 10.1097/ACM.0000000000003524 [DOI] [PubMed] [Google Scholar]
- 8. Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251–70. [DOI] [PubMed] [Google Scholar]
- 9. Chrimes N, Higgs A, Sakles JC. Welcome to the era of universal airway management. Anaesthesia 2020; 75: 711–5. [DOI] [PubMed] [Google Scholar]
- 10. Tunstall M. Failed intubation drill. Anaesthesia 1976; 31: 850. [Google Scholar]
- 11. Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. British Journal of Anaesthesia 2015; 115: 827–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brewster DJ, Nickson CP, Gatward JJ, Staples M, Hawker F. Should ongoing airway education be a mandatory component of continuing professional development for College of Intensive Care Medicine Fellows? Anaesthesia and Intensive Care 2018; 46: 190–6. [DOI] [PubMed] [Google Scholar]
- 13. Rehak A, Watterson LM. Institutional preparedness to prevent and manage anaesthesia‐related 'can't intubate, can't oxygenate' events in Australian and New Zealand teaching hospitals. Anaesthesia 2019; 75: 767–74. [DOI] [PubMed] [Google Scholar]
- 14. Shah R, Barksfield R. Fostering patient safety through health policy innovation: a case study of implementation of the WHO Surgical Checklist in the UK. Journal of Perioperative Practice 2019; 30: 315–9. [DOI] [PubMed] [Google Scholar]
- 15. Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management – part 1 – difficult tracheal intubation encountered in an unconscious/induced patient. Canadian Journal of Anesthesia 2013; 60: 1089–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. British Journal of Anaesthesia 2018; 120: 323–52. [DOI] [PubMed] [Google Scholar]
- 17. Chrimes N, Cook TM. Critical airways, critical language. British Journal of Anaesthesia 2017; 118: 649–54. [DOI] [PubMed] [Google Scholar]
- 18. Chrimes N, Higgs A, Rehak A. Lost in transition: the challenges of getting airway clinicians to move from the upper airway to the neck during an airway crisis. British Journal of Anaesthesia 2020; 125: e38–e46. [DOI] [PubMed] [Google Scholar]
- 19. Myatra SN, Patwa A, Divatia JV. Critical language during an airway emergency: time to rethink terminology? Indian Journal of Anaesthesia 2020; 64: 275–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thoms GMM, McHugh GA, O'Sullivan EP. The global oximetry initiative. Anaesthesia 2007; 62: 75–7. [DOI] [PubMed] [Google Scholar]
- 21. Jooste R, Roberts F, Mndolo S, et al. Global Capnography Project (GCAP): implementation of capnography in Malawi – an international anaesthesia quality improvement project. Anaesthesia 2019; 74: 158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chrimes N, Bradley WPL, Gatward JJ, Weatherall AD. Human factors and the 'next generation' airway trolley. Anaesthesia 2019; 74: 427–33. [DOI] [PubMed] [Google Scholar]
- 23. Schnittker R, Marshall S, Horberry T, Young KL. Human factors enablers and barriers for successful airway management – an in‐depth interview study. Anaesthesia 2018; 73: 980–9. [DOI] [PubMed] [Google Scholar]
- 24. Jones CPL, Fawker‐Corbett J, Groom P, Morton B, Lister C, Mercer SJ. Human factors in preventing complications in anaesthesia: a systematic review. Anaesthesia 2018; 73(Suppl. 1): 12–24. [DOI] [PubMed] [Google Scholar]
- 25. Cook TM, Woodall N, Frerk C. 4th National Audit Project of The Royal College of Anaesthetists and The Difficult Airway Society. Major complications of airway management in the United Kingdom, Report and Findings, 2011. https://www.nationalauditprojects.org.uk/downloads/NAP4%20Full%20Report.pdf (accessed 11/04/2020). [DOI] [PubMed]
- 26. Cook TM. Strategies for the prevention of airway complications – a narrative review. Anaesthesia 2018; 73: 93–111. [DOI] [PubMed] [Google Scholar]
- 27. Ahmad I, El‐Boghdadly K, Bhagrath R, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 2020; 75: 509–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McGrath BA, Bates L, Atkinson D, Moore JA; National Tracheostomy Safety P . Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia 2012; 67: 1025–41. [DOI] [PubMed] [Google Scholar]
- 29. Brouwers MC, Kerkvliet K, Spithoff K, Consortium ANS . The AGREE reporting checklist: a tool to improve reporting of clinical practice guidelines. British Medical Journal 2016; 352: i1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Petrini F, Accorsi A, Adrario E, et al. Recommendations for airway control and difficult airway management. Minerva Anestesiologica 2005; 71: 617–57. [PubMed] [Google Scholar]
- 31. Frova G, Guarino A, Petrini F, Merli G, Sorbello M. Recommendations for airway control and difficult airway management in paediatric patients. Minerva Anestesiologica 2006; 72: 723–48. [PubMed] [Google Scholar]
- 32. Jensen AG, Callesen T, Hagemo JS, et al. Scandinavian clinical practice guidelines on general anaesthesia for emergency situations. Acta Anaesthesiologica Scandinavica 2010; 54: 922–50. [DOI] [PubMed] [Google Scholar]
- 33. Popat M, Mitchell V, Dravid R, Patel A, Swampillai C, Higgs A. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia 2012; 67: 318–40. [DOI] [PubMed] [Google Scholar]
- 34. Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management–part 2–the anticipated difficult airway. Canadian Journal of Anesthesia 2013; 60: 1119–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Japanese Society of A . JSA airway management guideline 2014: to improve the safety of induction of anesthesia. Journal of Anesthesia 2014; 28: 482–93. [DOI] [PubMed] [Google Scholar]
- 36. Black AE, Flynn PE, Smith HL, Thomas ML, Wilkinson KA. Development of a guideline for the management of the unanticipated difficult airway in pediatric practice. Pediatric Anesthesia 2015; 25: 346–62. [DOI] [PubMed] [Google Scholar]
- 37. Mushambi MC, Kinsella SM, Popat M, et al. Obstetric Anaesthetists' Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia 2015; 70: 1286–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Piepho T, Cavus E, Noppens R, et al. S1 guidelines on airway management : Guideline of the German Society of Anesthesiology and Intensive Care Medicine. Der Anaesthetist 2015; 64(Suppl. 1): 27–40. [DOI] [PubMed] [Google Scholar]
- 39. Rehn M, Hyldmo PK, Magnusson V, et al. Scandinavian SSAI clinical practice guideline on pre‐hospital airway management. Acta Anaesthesiologica Scandinavica 2016; 60: 852–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Petrini F, Di Giacinto I, Cataldo R, et al. Perioperative and periprocedural airway management and respiratory safety for the obese patient: 2016 SIAARTI Consensus. Minerva Anestesiologica 2016; 82: 1314–35. [PubMed] [Google Scholar]
- 41. Myatra SN, Shah A, Kundra P, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian Journal of Anaesthesia 2016; 60: 885–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ramkumar V, Dinesh E, Shetty SR, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in obstetrics. Indian Journal of Anaesthesia 2016; 60: 899–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pawar DK, Doctor JR, Raveendra US, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in Paediatrics. Indian Journal of Anaesthesia 2016; 60: 906–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kundra P, Garg R, Patwa A, et al. All India Difficult Airway Association 2016 guidelines for the management of anticipated difficult extubation. Indian Journal of Anaesthesia 2016; 60: 915–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Myatra SN, Ahmed SM, Kundra P, et al. The All India Difficult Airway Association 2016 guidelines for tracheal intubation in the Intensive Care Unit. Indian Journal of Anaesthesia 2016; 60: 922–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sun F, Wang Y, Ma S, et al. Clinical consensus of emergency airway management. Journal of Thoracic Disease 2017; 9: 4599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Langeron O, Bourgain JL, Francon D, et al. Difficult intubation and extubation in adult anaesthesia. Anaesthesia Critical Care and Pain Medicine 2018; 37: 639–51. [DOI] [PubMed] [Google Scholar]
- 48. Dadure C, Sabourdin N, Veyckemans F, et al. Management of the child's airway under anaesthesia: the French guidelines. Anaesthesia Critical Care and Pain Medicine 2019; 38: 681–93. [DOI] [PubMed] [Google Scholar]
- 49. Brewster DJ, Chrimes N, Do TB, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group. Medical Journal of Australia 2020; 212: 472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cook TM, El‐Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID‐19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020; 75: 785–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Garg R, Patwa A, Shah A, et al. All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID‐19 pandemic. Indian Journal of Anaesthesia 2020; 64: 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Matava CT, Kovatsis PG, Lee JK, et al. Pediatric Airway Management in COVID‐19 Patients: Consensus Guidelines from the Society for Pediatric Anesthesia's Pediatric Difficult Intubation Collaborative and the Canadian Pediatric Anesthesia Society. Anesthesia and Analgesia 2020; 131: 61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sorbello M, El‐Boghdadly K, Di Giacinto I, et al. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia 2020; 75: 724–32. [DOI] [PubMed] [Google Scholar]
- 54. Zuo MZ, Huang YG, Ma WH, et al. Expert recommendations for tracheal intubation in critically Ill patients with noval coronavirus disease 2019. Chinese Medical Sciences Journal 2020; 35: 105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Halperin JL, Levine GN, Al‐Khatib SM, et al. Further evolution of the ACC/AHA clinical practice guideline recommendation classification system: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology 2016; 67: 1572–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Reviewed airway management guidelines (existing guidelines).
Appendix S2. Reviewed COVID‐19 airway management guidelines (COVID‐19 guidelines).
Appendix S3. Details of the search strategies.
Appendix S4. Standardised critical appraisal template.


