Abstract
Objectives
This study aims to evaluate and compare the cost-effectiveness of inpatient physical therapy, outpatient physical therapy applications, and back school education in low back pain (LBP) treatment.
Patients and methods
Between March 2011 and September 2011, a total of 105 patients (43 males, 62 females; mean age 44.8±12.7 years; range, 27 to 58 years) who were treated for chronic LBP were included in this prospective study. Of the patients, 34 received inpatient physical therapy consisting of electrotherapy, superficial-deep heat application, and basic back exercise program, 35 received the same treatment in the outpatient setting, and 36 received back school education. Each patient was evaluated five times during the study using pain intensity Visual Analog Scale (VAS), spinal mobility measurements (inclinometer), general evaluation (VAS), functional disability measurement (Roland-Morris Disability Questionnaire [RMDQ]), and quality of life (Short Form-36 [SF-36]). All expenses and costs for treatment of LBP were estimated.
Results
At the end of six months of follow-up, all study groups had a statistically significant improvement in all variables. Improvements in spinal mobility, RMDQ, and SF-36 scores were significantly higher in the inpatient physical therapy group (p<0.001). Direct and total costs were the highest in the inpatient treatment group and were the lowest in the back school education group (p<0.001). No statistically significant differences were observed in terms of additional cost of one-unit improvement in these variables among the study groups.
Conclusion
Our study results suggest that all three treatment modalities are effective in chronic LBP. In patients with LBP-related impairment in functional status and quality of life, inpatient physical therapy and rehabilitation should be preferred.
Keywords: Back school, cost-effectiveness, low back pain, physical therapy
Introduction
Low back pain (LBP) is a very common musculoskeletal problem with deleterious impacts on quality of life (QoL). The disability which results from the chronicity of the pain is considered one of the most important factors leading to absenteeism from work and a decrease in work productivity. Also, LBP is an important healthcare problem resulting in significant costs for the community. It has direct (diagnostic and therapeutic) and indirect (absenteeism from work) economic burden.[1,2]
In the United States, LBP causes 33 to 41% of workmen’s compensations, and 16 to 19% of disability payments.[3] It has been reported that LBP is the main cause of 25% of all workday losses and nine days of failure to attend to work per patient.[4] Within all direct medical costs spent for LBP, 17% is constituted by physical therapy, 17% by hospital expenses, 13% by medications, and 13% by primary care services.[5] In Switzerland, the total cost of treatment of LBP was reported as 7.4 million Euros, of which 3.4 million Euros (6.7% of all of Switzerland's total healthcare costs) are direct costs, 4 million Euros are indirect costs.[6] In addition, it has been reported that chronic LBP is an important cause of permanent disability and absenteeism from work. Also, between 1990 and 2005, workers' compensation for LBP has increased by 215%.[6,7]
As it is unlikely to identify the exact etiological factors in the majority of patients with LBP, it is aimed to determine whether the pain is mechanical at the time of diagnosis and to alleviate functional disability and pain during treatment. Since it is well known that not any treatment modality alone is effective for the treatment of LBP, multidisciplinary modalities comprising intensive exercise programs and back protection education are needed.[8,9]
In the present study, we aimed to compare the cost-effectiveness of inpatient and outpatient physical therapy applications and back school education for the treatment of patients with chronic and mechanical LBP to present our mid-term follow-up results.
Patients and Methods
This prospective study was conducted at Ufuk University School of Medicine, Department of Physical Medicine and Rehabilitation (PMR), Ankara, Turkey between March 2011 and September 2011. A total of 108 patients who presented to the PMR outpatient clinics complaining of LBP lasting for more than three months and who were subsequently diagnosed with chronic mechanical LBP were included in the study. For each participant, after obtaining a detailed history, a systematic physical examination was performed. Laboratory tests including a complete blood count (CBC), biochemistry panel, conventional X-ray studies, magnetic resonance imaging (MRI), and computed tomography (CT) scans were also performed, where necessary. Patients having spinal surgery, root compression, spine fracture, neurological findings, inflammatory, infectious, metabolic disease or malignancy, severe osteoporosis or osteomalacia, spinal deformity or congenital malformations were excluded from study. Data including sociodemographic status (age, sex, weight, height, and marital, educational and occupational status), pain duration and intensity, and occupational intensity levels were recorded.
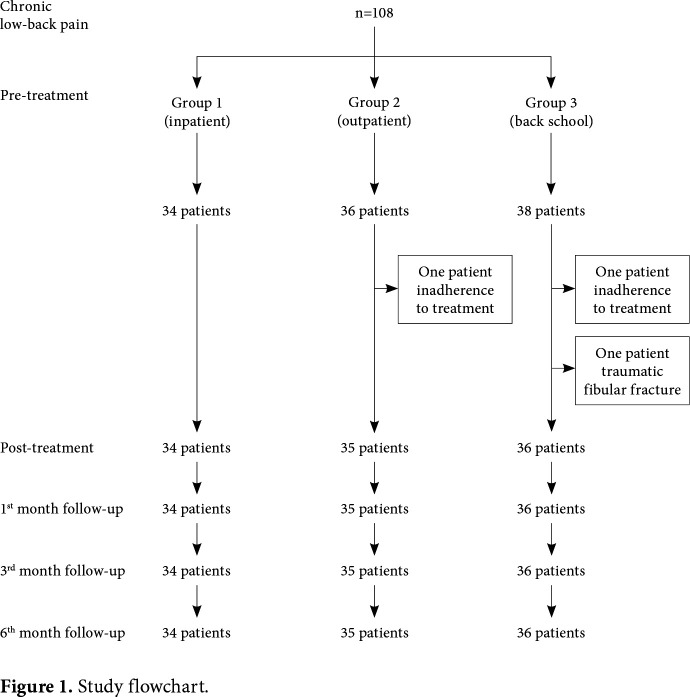
The patients were allocated into one of the three study groups: Group 1 (inpatient physical therapy), Group 2 (outpatient physical therapy), and Group 3 (back school program). Group 1 had five inpatient therapy sessions per week for a total duration of three weeks. The therapy regimen consisted of 45-min hot pack, ultrasound (1 MHz, 1 to 1.5 Watt/cm2, 10 min), transcutaneous electrical nerve stimulation (TENS, 30 to 40 Hz, 15 min conventional), and basic back exercises. Group 2 received the same treatment in the outpatient setting. Group 3 received back school education for a total of four 45-min sessions, which was provided in classes of 10 to 12 participants. In these classes, alongside with slide presentations, anatomical education was given with clinical models. Moreover, a program information booklet with pictures was also provided to each participant. One patient from Group 2 and one patient from Group 3 were excluded due to non-adherence to treatment. Also, one patient from Group 3 was unable to complete the assigned treatment protocol and was excluded from the study due to a fibular fracture. Finally, a total of 105 patients (43 males, 62 females; mean age 44.8±12.7 years; range, 27 to 58 years) who were treated for chronic LBP were included. The study flow chart is shown in Figure 1.
Figure 1. Study flowchart.
A written informed consent was obtained from each patient. The study protocol was approved by the Ufuk University School of Medicine Ethics Committee. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Assessment tools
All study participants were evaluated for a total of five times: immediately before and after the assigned therapy, and at one, three, and six months after the completion of the therapy. Medical treatment including paracetamol, non-steroid anti-inflammatory drugs (NSAIDs), myorelaxants, and opioids in an algorithmic fashion, therapeutic equipment such as girdles and back pillow, and paravertebral injections were performed, as indicated. During the six-month follow-up, there were no restrictions for the number of applications to seek medical treatment for recurrent LBP, medication and equipment use, or other treatments.
Among the surveillance variables, pain was evaluated with the Visual Analog Scale (VAS). A 100-mm scale was used, where a point of 0 indicates absence of pain, and a score of 100 indicates maximal pain. The patients were asked to mark a point on the scale that reflects their pain. The VAS scale was used also for the Patient Global Assessment (PGA) and Physician Global Assessment (MDGA). Lumbar mobility (flexion, extension and lateral flexion) was evaluated with Baseline® 12-1057 digital inclinometer (Fabrication Enterprises Inc., NY, USA), which is the most commonly used method to assess mobility.[10] The T12-L1 equaled to the total lumbar mobility, and subtraction of the sacral value from this equaled to true lumbar mobility. The Roland-Morris Disability Questionnaire (RMDQ) was used to determine functional disability. The Turkish version of this form has been shown to be valid and reliable.[11] The questionnaire consists of 24 questions which are either answered as “Yes” or “No”, giving a total score between 0 and 24 points. In this system, 0 indicates "No disability", whereas any point of >1 indicates the presence of disability. The QoL was also assessed using the Short Form-36 (SF-36) which consists of 36 questions. It has also eight subscales to assess vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning, and mental health. There are two summary scales: the mental component summary (MCS) and physical component summary (PCS). Each of these are separately scored between 0 and 100, where a higher score indicates higher QoL.
Calculation of costs
Health expenses were grouped as direct and indirect costs. The patients were asked to fill out a daily log for all the expenses they made regarding treatment of LBP. Costs per units of tests and treatment measures were acquired from the Turkish Social Security Institution (SGK) reimbursement rates. Treatment costs were determined as the sum of physical therapy costs, costs of medications and equipment used during treatment, transportation costs (for patients receiving outpatient treatment), and cost of days-off-work (for occupied participants). Direct costs included all costs within the six months post-treatment period such as re-examinations, tests, physical therapies, paravertebral muscle injections, hospitalizations, medications, equipment and alternative therapies. Indirect costs were calculated as days-off-work multiplied by daily wage/income.
For cost-effectiveness analysis, cost per one-unit change in VAS, RMDS, SF-36 MCS and SF-36 PCS, as well as the changes in these variables proportional to total therapy costs were analyzed.
Statistical analysis
Statistical analysis was performed using the PASW for Windows version 17.0 software (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed in mean ± standard deviation (SD), median (min-max), while categorical variables were expressed in number and percentage. The chi-square, Mann-Whitney U, and Kruskal-Wallis tests were used to compare the groups, where appropriate. The Kolmogorov-Smirnov test was used to assess normal data distribution. A p value of <0.05 was considered statistically significant.
Results
Baseline socio-demographic characteristics of the patients are presented in Table 1. In the pretreatment period, there were no statistically significant differences among the study groups in terms of VAS, PGA, and MDGA. Compared to the other groups, spinal mobility and SF-36 summary scores were significantly lower, whereas the RMDS was significantly higher in the inpatient physical therapy group (p<0.05) (Table 2).
Table 1. Socio-demographic characteristics of patients.
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | P | |||||||
| n | % | Mean±SD | n | % | Mean±SD | n | % | Mean±SD | ||
| Age (year) | 50.8±7.9 | 44±13.6 | 39.4±11.5 | 0.001 | ||||||
| Sex | 0.011 | |||||||||
| Female | 27 | 79.4 | 16 | 45.7 | 19 | 52.8 | ||||
| Marital status | 0.015 | |||||||||
| Married | 33 | 97 | 30 | 85 | 26 | 72 | ||||
| Education | <0.001 | |||||||||
| Illiterate | 1 | 2.9 | 0 | 0 | 0 | 0 | ||||
| Elementary school | 17 | 50 | 3 | 8.6 | 22 | 21 | ||||
| Middle school | 6 | 17.6 | 1 | 2.9 | 15 | 14.3 | ||||
| High school | 8 | 23.5 | 14 | 40 | 29 | 27.6 | ||||
| University | 2 | 5.9 | 17 | 48.6 | 38 | 36.2 | ||||
| Body mass index (kg/m2) | 30.2±5.06 | 26.5±4.2 | 24.3±4.7 | <0.001 | ||||||
| Disease duration (month) | 60.1±43 | 42±52 | 27±32 | 0.003 | ||||||
| Occupation working | 4 | 11.8 | 19 | 54.3 | 29 | 80.6 | <0.001 | |||
| Occupational intensity | 0.132 | |||||||||
| Heavy | 2 | 5.9 | 2 | 5.7 | 5 | 13.9 | ||||
| Moderate | 10 | 29.4 | 12 | 34.3 | 18 | 50 | ||||
| Light | 22 | 64.7 | 21 | 60 | 13 | 36.1 | ||||
| SD: Standard deviation. | ||||||||||
Table 2. Pre-treatment values of assessment variables including pain, spinal mobility, patient and physician global assessment, functional status, and disability.
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | ||
| Parameter | Mean±SD | Mean±SD | Mean±SD | P |
| VAS (0-100 mm) | 50.9±23 | 61.4±25 | 49.7±18.5 | 0.072 |
| Lumbar flexion angle | 49.1±6.2 | 52±6.2 | 53.3±5.3 | 0.007 |
| Lumbar extension angle | 17.2±4.6 | 22±5 | 2.6±4.5 | <0.001 |
| Right lateral flexion angle | 17.7±4 | 20.7±3.1 | 21.3±2.3 | <0.001 |
| Left lateral flexion angle | 17.8±4 | 20.8±3.1 | 21.5±2.3 | <0.001 |
| PGA (0-100 mm) | 47.3±24.7 | 47.1±27.5 | 45.9±19.1 | 0.941 |
| MDGA (0-100 mm) | 41.2±22.2 | 35.2±20.9 | 36.1±17.9 | 0.452 |
| RMDS score (0-24) | 17.4±4.7 | 12±6 | 10±8.2 | <0.001 |
| SF-36 PCS | 33.1±17.9 | 52.9±19.9 | 54.7±23.4 | <0.001 |
| SF-36 MCS | 48.5±18.2 | 57±19.3 | 65.3±19.9 | 0.002 |
| SD: Standard deviation; VAS: Visual Analog Scale; PGA: Patient global assessment; MDGA: Physician global assessment; RMDS: Roland Morris Disability Score; SF-36 MCS: Short Form 36 Mental Component Summary; SF-36 PCS: Short Form 36 Physical Component Summary. | ||||
In all treatment groups, the VAS, spinal mobility, PGA, MDGA, RMDS, and SF-36 PCS and MCS scores were significantly improved in the immediate post- treatment period and at one, three, and six months (p<0.001). In terms of VAS, PGA, and MDGA score changes, pre-treatment and six-month evaluations showed no statistically significant difference (p>0.05). In terms of improvement in spinal mobility, RMDS, and SF-36 summary scores, there was a statistically significant difference among the treatment groups (p<0.05). Improvement in the inpatient physical therapy group was significantly higher compared to other treatment groups (p<0.05) (Table 3).
Table 3. The results of pre-treatment and six-month assessment of pain, mobility, functional capacity, and disability.
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | ||
| Parameter | Mean±SD | Mean±SD | Mean±SD | P |
| VAS (0-100 mm) | 31.5±33.8 | 31.9±30 | 25.6±21.5 | 0.227 |
| Lumbar flexion angle | -5.2±5.5 | -2.6±4.3 | -2.1±2.3 | 0.008 |
| Lumbar extension angle | -4.2±4.3 | -2.1±3.3 | -2.5±3 | 0.015 |
| Right lateral flexion angle | -3.7±3.5 | -1.6±2.6 | -1.4±1.5 | <0.001 |
| Left lateral flexion angle | -3.3±3.4 | -1.5±2.5 | -1.4±1.7 | 0.001 |
| PGA (0-100 mm) | 28.8±34.3 | 22.5±32.4 | 25.3±22 | 0.358 |
| MDGA (0-100 mm) | 31.6±24.1 | 17.6±25.5 | 22.1±20 | 0.053 |
| RMDS score (0-24) | 11±7.2 | 6.9±5.6 | 4±4.8 | <0.001 |
| SF-36 PCS | -34 ±27 | -18.3±21.8 | -15.9±16.4 | 0.003 |
| SF-36 MCS | -18.9±19 | -13.6±18.3 | -2.9±12.3 | <0.001 |
| SD: Standard deviation; VAS: Visual Analog Scale; PGA: Patient global assessment; MDGA: Physician global assessment; RMDS: Roland Morris Disability Score; SF-36 MCS: Short Form 36 Mental Component Summary; SF-36 PCS: Short Form 36 Physical Component Summary. | ||||
In the post-treatment six-month follow-up, other treatment resources that the patients resorted, and the patient numbers using these modalities were compared among the treatment groups. Patient numbers who needed hospitalization, attending to outpatient clinics, laboratory and imaging tests, paravertebral intramuscular injections, medical equipment and complementary medical interventions were similar among the groups (p>0.05). The number of patients in whom physical therapy was applied was higher in the back school education group than the other treatment groups (p=0.011), while the number of patients who required medication was lower (p=0.006) (Table 4). Baseline and mean total costs of 14-day physical therapy/back school were the highest in the inpatient treatment group and was the lowest in the back school group (p<0.001) (Table 5). Direct medical costs which were calculated at the end of six months was the highest in the inpatient physical therapy group and was the lowest in the back school group (p<0.001). In terms of indirect costs, there were statistically significant differences among the study groups (p>0.05). Total costs were the highest in the inpatient physical therapy group and were the lowest in the back school group (p<0.001) (Table 6).
Table 4. Utilization of healthcare resources during follow-up.
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | P | ||||
| n | % | n | % | n | % | ||
| Physical therapy | 0 | 0 | 1 | 2.9 | 6 | 16.7 | 0.011 |
| Hospitalization | 0 | 0 | 0 | 0 | 0 | 0 | NA |
| Outpatient clinics | 10 | 29.4 | 8 | 22.9 | 8 | 22.2 | 0.746 |
| Imaging tests (MRI/CT) | 3 | 8.8 | 4 | 11.4 | 5 | 13.9 | 0.801 |
| Paravertebral muscle injection | 7 | 20.6 | 10 | 28.6 | 7 | 19.4 | 0.611 |
| Medication | 31 | 91.7 | 32 | 91.4 | 24 | 66.7 | 0.006 |
| Medical equipment | 19 | 55.9 | 20 | 57.1 | 15 | 41.7 | 0.350 |
| Complementary medical interventions* | 12 | 35.3 | 12 | 34.3 | 17 | 47.2 | 0.462 |
| Balneotherapy | 6 | 6 | 4 | ||||
| Massage | 6 | 6 | 7 | ||||
| Acupuncture | 0 | 1 | 1 | ||||
| Aromatherapy/herbal therapy | 3 | 2 | 9 | ||||
| Neural therapy | 0 | 0 | 1 | ||||
| Ozone therapy | 0 | 1 | 2 | ||||
| G therapy | 0 | 0 | 1 | ||||
| Absenteeism from work (days) | 10 | 38 | 48 | ||||
| MRI: Magnetic resonance imaging; CT: Computerized tomography;* Some patients received more than one complementary medical intervention. | |||||||
Table 5. The cost of physical therapy and back school (14 days) (TL).
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | ||||||||
| Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | P | |
| Initial cost (TL) | 700 | 280 | 32 | <0.001 | ||||||
| Medication | 22.9±10.3 | 23.2 | 5-46.6 | 20.1±10.4 | 21.7 | 0-39.7 | 13±11.5 | 11.8 | 0-37.9 | 0.004 |
| Medical equipment | 22.1±27.7 | 0 | 0-70 | 5.2±14.9 | 0 | 0-68 | 0.030 | |||
| Transportation costs | 14±25.6 | 0 | 0-70 | 106.5±46 | 98 | 49-280 | 39±33.3 | 35 | 14-210 | <0.001 |
| Absenteeism from work | 0 | 118.1±395 | 0 | 0-1866.6 | 19.1±60.9 | 0 | 0-250 | 0.970 | ||
| Total (TL) | 81.6±257.1 | 0 | 0-1,166.6 | 547 ± 429 | 439.9 | 334-2366.4 | 108.4±77.6 | 87.6 | 46-389.7 | <0.001 |
| TL: Turkish Liras; SD: Standard deviation; Min: Minimum; Max: Maximum. | ||||||||||
Table 6. Mean total costs for all groups.
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | p | |||||||
| Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | ||
| Direct medical costs | 960.8±320.9 | 802.4 | 706-1,731 | 488.3±268.3 | 386.1 | 280-1,327 | 247.5±347.1 | 74 | 32-1,532 | <0.001 |
| Physical therapy | 702.3±5.5 | 700 | 700-726 | 283±5.2 | 280 | 280-297 | 80.5±108.3 | 32 | 32-329 | <0.001 |
| Medication | 39.6±19.1 | 40.4 | 5-90 | 34.8±17.2 | 31.7 | 0-87 | 24±20.5 | 19.9 | 0-68 | 0.003 |
| Outpatient clinics | 19.4±32.8 | 0 | 0-110 | 14.1±27.7 | 0 | 0-110 | 12.2±23.1 | 0 | 0-55 | 0.687 |
| Imaging tests | 6.9±22.7 | 0 | 0-79 | 7.9±23 | 0 | 0-79 | 10.9±27.7 | 0 | 0-79 | 0.799 |
| Medical equipment | 192.4±311.4 | 58 | 0-1, 000 | 148.4±265.6 | 60 | 0-1,030 | 119.7±307.3 | 15 | 0-1,500 | 0.110 |
| Complementary medical interventions | 180.2±342 | 0 | 0-1,098 | 211.9±383.4 | 0 | 0-1,307 | 241.3±396.9 | 0 | 0-1,200 | 0.510 |
| Direct non-medical costs transportation | 0 | 0 | 0 | 106.5±46 | 98 | 49-280 | 39±33.3 | 35 | 14-210 | <0.001 |
| Indirect costs | 89.5±270 | 0 | 0-1166 | 213.1±695.7 | 0 | 0-3,866 | 108.1±228.3 | 0 | 0-850 | 0.208 |
| Total costs | 1,050.4±432.5 | 806 | 706-2,451 | 808±794.1 | 525.9 | 336-4,636 | 394.7±495.8 | 124 | 57-1,869 | <0.001 |
| TL: Turkish Liras; SD: Standard deviation; Min: Minimum; Max: Maximum. | ||||||||||
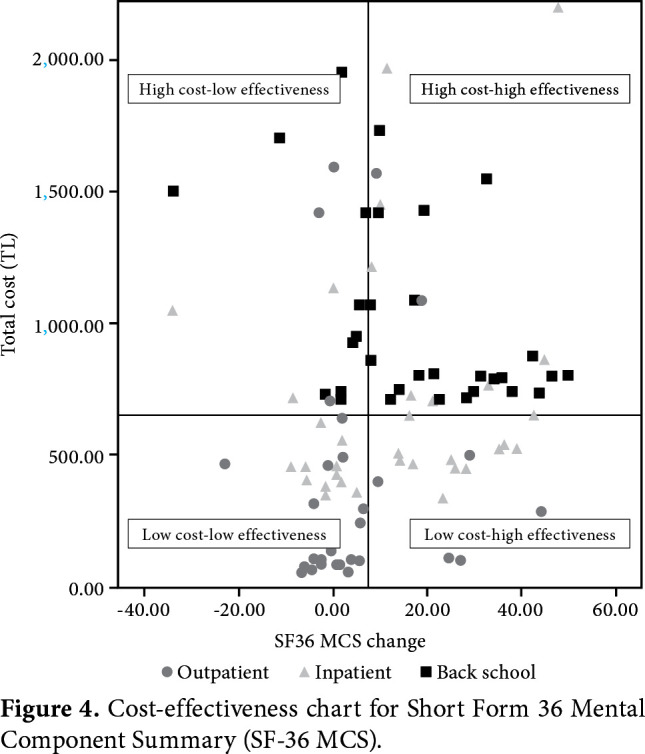
After six months of follow-up, when the costs of one unit of improvement in the study variables (VAS, RMDS, SF-36 summary scores) were compared between the groups, the cost of one unit decrease in the VAS value was significantly lower in the back school group (p=0.001). Although the improvement in the pre-treatment and six-month RMOS and SF-36 summary scores was significantly higher in the inpatient physical therapy group, there were no significant differences among the groups in terms of the cost of one-unit improvement (p>0.05) (Table 7). Cost-effectiveness graphics regarding the RMDS and SF-36 summary scores of the groups are presented in Figures 2, 3 and 4 respectively.
Table 7. Cost-effectiveness ratios (TL cost per one-unit improvement).
| Group 1 (n=34) (inpatient therapy) | Group 2 (n=35) (outpatient therapy) | Group 3 (n=36) (back school) | ||||||||
| Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | P | |
| VAS (0-100 mm) | 33.2±32.1 | 22.6 | 9-155 | 29.9±44.1 | 16,8 | 5-231 | 29.5±62.2 | 4 7 | 1-318 | 0.001 |
| RMDS score (0-24) | 123.2±146.5 | 65.9 | 36-716 | 235.8±303.4 | 109,8 | 34-1 159 | 147.7±310 | 64 6 | 5-1 592 | 0.143 |
| SF-36 PCS | 118.8±472.7 | 22.6 | 10-2 482 | 50.9±93.7 | 26,2 | 9-506 | 71.6±172.6 | 10 6 | 1-821 | 0.117 |
| SF-36 MCS | 125.7±194.6 | 47.6 | 16-987 | 268.4±825.7 | 36.4 | 13-4 315 | 531.9±1 954.9 | 40 3 | 3-8 358 | 0.611 |
| TL: Turkish Liras; SD: Standard deviation; Min: Minimum; Max: Maximum; VAS: Visual Analog Scale; RMDS: Roland Morris Disability Score; SF-36: Short Form 36; PCS: Physical component summary; MCS: Mental component summary. | ||||||||||
Figure 2. Cost-effectiveness chart for Roland Morris Disability Score (RMDS).
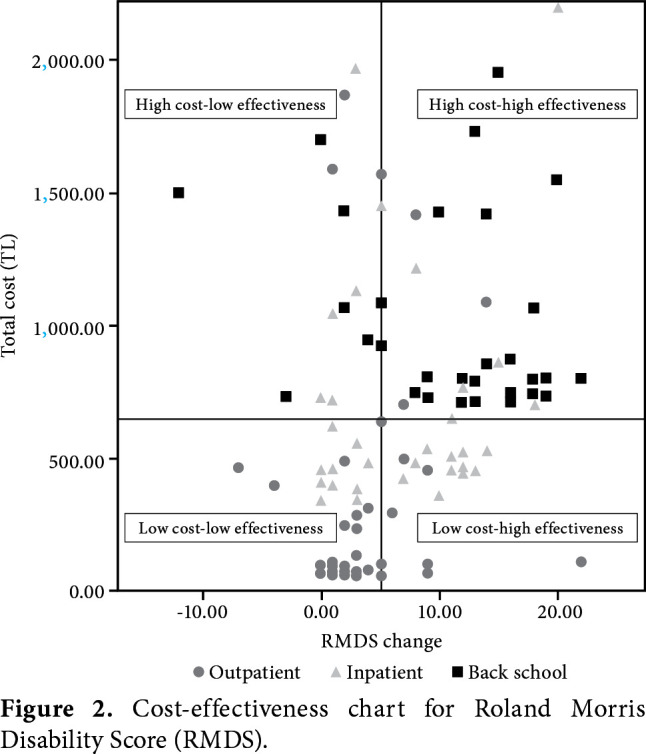
Figure 3. Cost-effectiveness chart for Short Form 36 Physical Component Summary (SF-36 PCS).
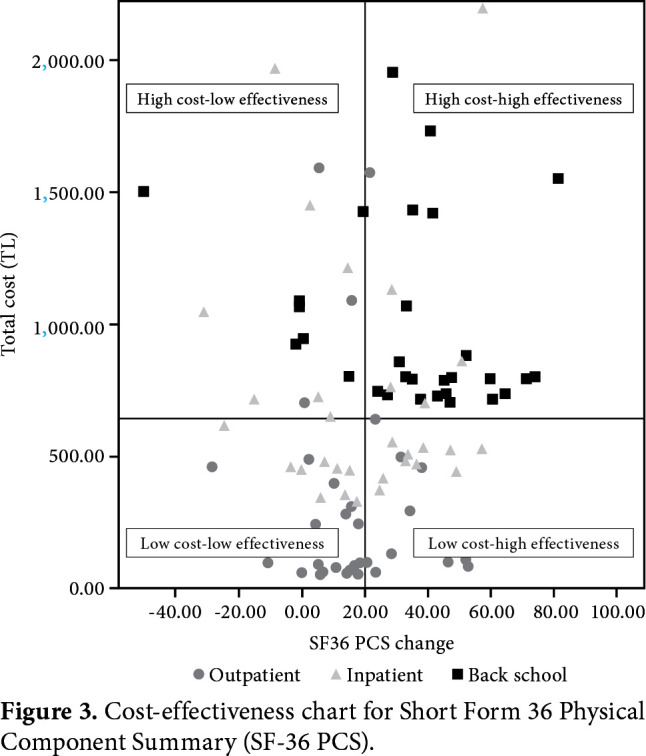
Figure 4. Cost-effectiveness chart for Short Form 36 Mental Component Summary (SF-36 MCS).
Discussion
In the present study, we compared the cost- effectiveness of inpatient and outpatient physical therapy, and back school programs for the treatment of chronic mechanical LBP. After six months of follow-up, there was an improvement in all study variables for all treatment groups. However, as our main objective was to conduct a cost analysis of all healthcare resources that these patients resorted to in the mid- and long-term, and no restrictions were applied in the use of medications, medical equipment, complementary medicine and balneotherapy, which may significantly increase the treatment costs. Hence, the cost-effectiveness analysis included not only the baseline costs, but also other treatments that the patients received during the six-month follow-up period. In the pre-treatment evaluation, spinal mobility and SF-36 summary scores were significantly lower and RMOS was significantly higher in the inpatient physical therapy group compared to the other groups. These findings indicate that, when the duration of pain prolongs, the impairment in functional status and QoL becomes more evident; therefore, these patients are more likely to request inpatient treatment program. After the treatment, there were no significant differences in the variables, except for spinal mobility, RMDS and SF-36 scores which were all significantly higher in the inpatient physical therapy group. This improvement can be attributed to the fact that inpatient physical therapy was performed under continuous supervision of the physician and physiotherapist during the exercise sessions which might have improved the motivation and compliance of the patients. During daily clinical visits, the communication between the rehabilitation team such as physician, physiotherapist, and the patient may have positive effects on the patients' misconceptions, misconducts, and additional problems which can be easily recognized and corrected by this way. On the other hand, in the outpatient group, treatment might have been interrupted due to environmental issues, the patients' inability to keep the treatment area warm after hot pack application during the winter season, inability to check the compliance of home-based exercise program, and patients' daily life issues which reduce the adherence to the prescribed home-based program and, thus, it might have led to lesser improvement in the functional status. Back school group also had lower functional scores due to similar reasons to the outpatient group, as well as the lack of physician’s visit and the belief of the common concept that physical therapy is the most effective treatment in the LBP patient population.
In a previous study, the effects of inpatient and outpatient physical therapy programs on QoL and functional status in chronic LBP were compared.[12] In the pre-treatment and post-treatment (1 week after completion) QoL, Nottingham Health Profile (NHP), functional evaluation scales, modified Oswestry, RMDS, and Beck Depression Inventory (BDI) scores were evaluated. Both groups had significant improvement in the post-treatment evaluation. In the inter-group comparison, the inpatient group had an improvement in the NHP subscales of energy, sleep and emotional reaction. However, no significant improvements were observed in the outpatient group. In psychological evaluation, there were no significant differences in the inpatient group, while a significant improvement was observed in the outpatient group.
Another study conducted in the United Kingdom compared physical therapy and physiotherapy recommendations in terms of cost-utility in subacute and chronic LBP patients.[13] In this randomized study, one of the groups received five sessions of physical therapy including hot pack application, joint mobilization, soft tissue techniques, and personal exercise program, whereas the other group received recommendations of a physiotherapist. The patients were evaluated at 2,612 months using the Oswestry Disability Index and EuroQoL 5D (EQ-5D) QoL index by using surveys. There were no significant differences in terms of total costs; however, the patients’ expenses were significantly higher in the physical therapy group. The authors concluded that receiving recommendations by a physiotherapist should be considered as the initial approach in these patients.
In this study, we calculated every single expense for the treatment of LBP during the six-month follow-up and compared the study groups. According to the SGK reimbursement costs, the mean total cost of 14-day treatment was the highest for the inpatient group and was the lowest in the back school group (p<0.001). When the groups were compared in terms of the utilization of healthcare resources, there was no significant difference among the groups in terms of the rates of readmission to outpatient clinics for pain management during follow-up period (p>0.05). This finding suggests that inpatient or outpatient physical therapy programs have no superiority to prevent the recurrence of LBP and to decrease the utilization of healthcare resources, compared to the back school program.
Furthermore, during the six-month follow-up, we found direct medical costs to be the highest in the inpatient group, whereas it was the lowest in the back school group. Direct non-medical costs mainly included transportation costs and, as expected, these costs were the highest in the outpatient physical therapy group. When we compared indirect costs, there was no significant difference among the groups in terms of the cost of absenteeism from work (p>0.05). The ratio of employed patients was 11.8% in the inpatient group, whereas it was 80.6% in the back school group, and absenteeism from work was also lower in the inpatient group and higher in the back school group. This contradictory finding can be explained by the fact that the calculation of indirect costs was based on the mean wage/income of the patients, which was the highest in the employed inpatient physical therapy group. In a recent study conducted in Turkey, the total economic burden of chronic LBP was examined in 211 patients.[14] A questionnaire was used to assess the utilization of healthcare resources and direct and indirect costs within the past six months. Direct and indirect costs included similar items to ours and the authors found that indirect costs were higher than the direct costs which was related to the productivity loss. However, directs costs in our study seem to be higher than the indirect cost, which may be due to the inpatient physical therapy cost.
In their study, Critchley et al.[15] compared the effectiveness of outpatient physical therapy, spinal stabilization exercise, and pain management class to decrease disability due to chronic LBP. A total of 212 patients were followed for 18 months and were compared in terms of the VAS, RMDS, EQ-5D, and absenteeism from work. All of the three approaches were found to be effective; however, pain management class was found to be the most cost-effective and alternative approach. In another study from Switzerland, the cost of function-oriented and pain-oriented rehabilitation approaches were analyzed for a three-year period.[6] A total of 174 patients were randomized into either functional-oriented treatment group consisting of a functional restoration program, 4 h per day for a total of three weeks, or pain-oriented treatment group in groups of eight participants, 2.5 h per day, which consisted of physical therapy modalities, exercises, and back school. After three years of follow-up, the cost analyses of the two study groups were found to be similar. In Germany, among 409 patients, the cost-effectiveness of three-week standard inpatient rehabilitation versus additional cognitive behavioral treatment was compared, and the additional behavioral therapy group were found to be more effective on absenteeism from work and indirect costs.[16] Hahne et al.[17] also investigated the cost-effectiveness of individualized physical therapy (IPT) program and guideline-based advice for patients with LBP and/or referred leg pain during a six-month follow-up using questionnaires. Totally, 300 patients were randomized to either 10 sessions of IPT or two sessions of guideline-based advice. The IPT was found to be more cost-effective with less work absence. Another randomized study including 159 patients evaluated the cost-effectiveness of medical yoga therapy as an early intervention versus exercise and self-care advice in non-specific LBP patients during 12 months.[18] The health outcome measure EQ-5D, health-related quality of life, and incremental cost per quality-adjusted life year (QALY) were assessed and medical yoga therapy was found to be cost-effective. In this study, direct and indirect costs were higher in the exercise group.
Nonetheless, there are some limitations to the present study. A six-month follow-up is relatively short and further long-term studies may provide additional data. Also, the pre-treatment spinal mobility and disability scores were higher in the inpatient patients, and it is predictable to have higher costs due to the SGK reimbursement package for inpatient patients.
In conclusion, the main goals of treatment in chronic LBP should be to prevent and decrease disability and to improve the QoL and functional status. According to our study findings, all treatments seem to be effective for LBP patients. Although back school has the lowest and the inpatient therapy has the highest cost, the additional cost of inpatient treatment can be considered acceptable for patients with concomitant impaired functional status and QoL. Further large-scale, prospective studies are needed to evaluate and elucidate the cost-effectiveness of various physical therapy modalities in the treatment of chronic LBP.
Acknowledgments.
We would like to thank Prof. Cengizhan Açıkel, MD for his valuable contributions to the statistical analysis of the study.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64:2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol. 2010;24:155–165. doi: 10.1016/j.berh.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Williams DA, Feuerstein M, Durbin D, Pezzullo J. Health care and indemnity costs across the natural history of disability in occupational low back pain. Spine (Phila Pa 1976) 1998;23:2329–2336. doi: 10.1097/00007632-199811010-00016. [DOI] [PubMed] [Google Scholar]
- 4.Riihimaki H. Back and limb disorders. In: McDonald JC, editor. Epidemiology of work related diseases. London: BMJ Publishing Group; 1995. pp. 207–238. [Google Scholar]
- 5.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Bachmann S, Wieser S, Oesch P, Schmidhauser S, Knüsel O, Kool J. Three-year cost analysis of function-centred versus pain-centred inpatient rehabilitation in patients with chronic non-specific low back pain. J Rehabil Med. 2009;41:919–923. doi: 10.2340/16501977-0449. [DOI] [PubMed] [Google Scholar]
- 7.Hemmilä HM. Quality of life and cost of care of back pain patients in Finnish general practice. Spine (Phila Pa 1976) 2002;27:647–653. doi: 10.1097/00007632-200203150-00015. [DOI] [PubMed] [Google Scholar]
- 8.Özcan E. Bel ağrılı hastaların konservatif tedavisi. In: Özcan E, Ketenci A, editors. Bel Ağrısı Tanı ve Tedavi. İstanbul: Nobel Kitabevi; 2002. pp. 187–219. [Google Scholar]
- 9.Wewege MA, Booth J, Parmenter BJ. Aerobic vs. resistance exercise for chronic non-specific low back pain: A systematic review and meta-analysis. J Back Musculoskelet Rehabil. 2018;31:889–899. doi: 10.3233/BMR-170920. [DOI] [PubMed] [Google Scholar]
- 10.Flores L, Gatchel RJ, Polatin PB. Objectification of functional improvement after nonoperative care. Spine (Phila Pa 1976) 1997;22:1622–1633. doi: 10.1097/00007632-199707150-00020. [DOI] [PubMed] [Google Scholar]
- 11.Küçükdeveci AA, Tennant A, Elhan AH, Niyazoglu H. Validation of the Turkish version of the Roland-Morris Disability Questionnaire for use in low back pain. Spine (Phila Pa 1976) 2001;26:2738–2743. doi: 10.1097/00007632-200112150-00024. [DOI] [PubMed] [Google Scholar]
- 12.Yedeler E. Kronik mekanik bel ağrısında yatarak veya ayaktan uygulanan fizik tedavinin yaşam kalitesi ve fonksiyonel durum üzerine etkileri [Yüksek Lisans Tezi] Edirne: Trakya Üniversitesi Sağlık Bilimleri Enstitüsü; 2006. [Google Scholar]
- 13.Rivero-Arias O, Gray A, Frost H, Lamb SE, Stewart-Brown S. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Spine (Phila Pa 1976) 2006;31:1381–1387. doi: 10.1097/01.brs.0000218486.13659.d5. [DOI] [PubMed] [Google Scholar]
- 14.Yumusakhuylu Y, Baklacıoglu H, Aras H, Haliloglu S, Selimoglu E, İçağasıoğlu A. The economic cost of chronic low back pain. Bozok Tıp Dergisi. 2018;8:66–74. [Google Scholar]
- 15.Critchley DJ, Ratcliffe J, Noonan S, Jones RH, Hurley MV. Effectiveness and cost-effectiveness of three types of physiotherapy used to reduce chronic low back pain disability: a pragmatic randomized trial with economic evaluation. Spine (Phila Pa 1976) 2007;32:1474–1481. doi: 10.1097/BRS.0b013e318067dc26. [DOI] [PubMed] [Google Scholar]
- 16.Schweikert B, Jacobi E, Seitz R, Cziske R, Ehlert A, Knab J, et al. Effectiveness and cost-effectiveness of adding a cognitive behavioral treatment to the rehabilitation of chronic low back pain. J Rheumatol. 2006;33:2519–2526. [PubMed] [Google Scholar]
- 17.Hahne AJ, Ford JJ, Surkitt LD, Richards MC, Chan AY, Slater SL, et al. Individualized Physical Therapy Is Cost- Effective Compared With Guideline-Based Advice for People With Low Back Disorders. E169-E76Spine (Phila Pa 1976) 2017;42 doi: 10.1097/BRS.0000000000001734. [DOI] [PubMed] [Google Scholar]
- 18.Aboagye E, Karlsson ML, Hagberg J, Jensen I. Cost- effectiveness of early interventions for non-specific low back pain: a randomized controlled study investigating medical yoga, exercise therapy and self-care advice. J Rehabil Med. 2015;47:167–173. doi: 10.2340/16501977-1910. [DOI] [PubMed] [Google Scholar]