Abstract
Introduction
Telehealth is gaining more attention in multiple specialties, including urology. Video visits in particular have shown high satisfaction and cost-saving for patients. However, there has been little investigation into how video visits compare to traditional clinic visits on measures of clinical efficiency and reimbursement.
Methods
Our dataset included 250 video visits of established patients at Michigan Medicine Department of Urology and 250 in-person clinic visits with the same providers completed between July 2016 and July 2017. Information on visit completion and cancellation rates; cycle time (time from check in to check out); reimbursement; and patient out-of-pocket expenses was collected using the electronic medical record and billing data.
Results
Completion rates were similar between video and clinic visits (58% versus 61%, respectively; p=0.24). Average cycle time for video visits was significantly shorter compared to clinic visits (24 min vs 80 min, respectively; p<0.01). Neither average commercial payer reimbursement (p=0.21) nor average out-of-pocket expense (p=0.22) was statistically different between video and traditional visits. More video visits than clinic visits were billed as level 3 encounters (85% and 63%, respectively, p=0.002).
Conclusions
Our study demonstrates that video visits have the potential to reduce the time patients spend on follow-up care without negatively impacting reimbursement rates. However, these visits could reduce average billing levels. These findings suggest that the incorporation of video visits into practice may be more efficient for patients but may also reduce billing levels.
Keywords: telemedicine, telehealth, reimbursement, practice patterns
INTRODUCTION
Telehealth continues to be a subject of interest for urologists. Telehealth growth has been fueled by the expectation that it will be an efficient, accessible, and cost-effective way to deliver care to patients.1 In the field of urology, recent literature has demonstrated both high levels of patient enthusiasm and cost-savings for patients who participate in video visits.2-7
While this enthusiasm continues to drive the use of telehealth, little is known about how video visits compare on measures of clinical efficiency and reimbursement. For instance, it is plausible that video visits can improve the clinical productivity of providers, allowing physicians to see more patients in clinic and potentially improve financial metrics. Data in the field of ophthalmology suggests that the use of telehealth can improve clinical efficiency by reducing the time patients spent in the clinic thereby increasing the number of patients seen.8 On the other hand, due to implementation of new technology, it is possible that these visits can result in increased burden on providers and patients and be detrimental to clinic workflow, negatively affecting productivity. The wide-spread adoption of new technology does not always translate to immediate benefits. Studies across multiple specialties in ambulatory care settings revealed that clinic productivity decreased after implementation of electronic medical records (EMRs).9-11 The implementation of video visits as a new technology could impact existing workflows or increase the burden of documentation for providers thereby decreasing clinical efficiency.
Previous investigators have demonstrated the benefits and value of telehealth to patients, namely decreased travel time, decreased cost, and increased convenience.3,4,7,12 In recent years, health policy surrounding reimbursement for telehealth has been driven by state-level adoption of telemedicine parity laws. These laws regulate reimbursement by private payers for visits completed from patients’ home or work. In 2019, 37 states had private payer parity laws allowing commercial insurers to reimburse for telehealth services, primarily video visits.13 Herein, we build on the existing body of work by studying synchronous telehealth visits with established patients to measure clinical efficiency and compare reimbursement rates to clinic encounters in a state with telemedicine parity laws.
METHODS
Our dataset was developed from billing data obtained from our department coupled with de-identified patient information obtained through chart review. This included video visits, performed through a video communication system integrated in the EMR, and clinic appointments at an outpatient urology clinic. Patients were offered video visits if it was determined that an in-person physical exam would not impact clinical management. This study was deemed exempt from review by the University of Michigan Institutional Research Board.
Our study population included all established, adult patients (age >18) who were scheduled for a video visit or in-person visit between July 2016 and July 2017. We identified 250 video visit appointments with four different urologists. A stratified, random sample of 250 established patients scheduled for clinic visits with these same providers was selected as a comparison during this timeframe. Travel distance was calculated using Google Maps from patients’ hometowns to Ann Arbor, MI. Statistical analysis included point estimates (simple proportions) and t-test for comparison of reimbursement and out-of-pocket expenses. We excluded duplicated patient data which was identified by reviewing our institution’s EPIC EMR and comparing visit information to available billing data.
Completion, Cancellation and No-show rates
Our first outcome of interest was the percentage of appointments that were completed as scheduled. We identified and calculated the number of visits that were canceled or labeled as no-show. For a visit to be classified as a cancellation, the patient had to notify the clinic that they were unable to make that appointment. For video visits, cancellation included converting to a telephone encounter. No-show visits were visits for which patients were unable to make their appointment and the clinic staff was not notified ahead of time.
Cycle time
We used clinic metrics to calculate cycle time, a measure of clinical efficiency, which is defined as the amount of time in minutes that a patient spends at an office visit.14 We were able to obtain check-in and check-out time for in-person visits which included waiting time, rooming time, time spent with their Urologist, and time spent checking-out. For video visits, the cycle time was a measure of when patients logged in and logged out of their video appointment.
EM billing, Reimbursement, Patient Expenses
Finally, we used billing data to identify billing levels, private payer reimbursement, and patient out-of-pocket expenses incurred through their insurance. Billing level was determined by the urology provider and documented in the EMR. Private payer reimbursement was listed in billing database and cross checked for accuracy in the EMR. A similar process was used to determine patient out-of-pocket expenses from their insurance. This did not include expenses such as parking, fuel, food or other costs incurred during a visit.
RESULTS
We identified 250 established patients who were scheduled for a video visit between July 2016 through July 2017 and matched them to a random sample of 250 established patients with clinic visits during this time period, stratified by provider. Demographic information is listed on Table 1. Diagnoses for which these patients sought care included benign prostatic hyperplasia (BPH), nephrolithiasis, prostate cancer, renal mass, urinary tract infection (UTI), postop visits, and a small number of other miscellaneous diagnoses.
Table 1 -.
Demographics
| Video Visit | Clinic Visits | ||
|---|---|---|---|
| Age, Median (IQR) | 55 (38 – 65) | 65 (52 – 72) | |
| Sex, No. (%) | Female | 117 (47%) | 77 (31%) |
| Male | 133 (53%) | 173 (69%) | |
| Travel Distance in Miles, Median (IQR, Max) | 38 (17 – 98, 446) | 33 (17 – 65, 843) | |
Completion, Cancellation and No-show rates
58% (n=146) patients completed their video visit as scheduled compared to 61% (n=154) of patients seen in clinic. This difference was not statistically significant (p=0.24). The cancellation rate of 33% was the same (n=83) for video and clinic visits and only 1.2% (n=3) of video visits were converted to telephone encounters. The no-show rate for video visits was 8% (n=21) which was higher than that the 5% rate of clinic visit (n=13); however, this difference was not statistically significant (p=0.14, Figure 1).
Figure 1 -.
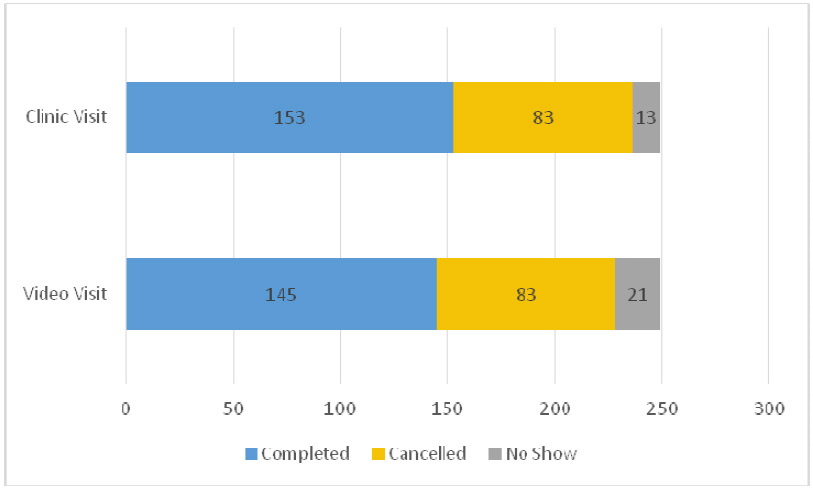
Cancellation and No-show Rates for Video Visits and Clinic Visits
Cycle time
We calculated cycle time for 40% (n=99) of video visits and 60% (n=150) of clinic visits based on completed appointments and availability of check-in/check-out data. For these visits we found that the average cycle time for video visits was 24 minutes and significantly lower than the 80-minute average cycle time of clinic visits (p<0.01, Figure 2).
Figure 2 -.
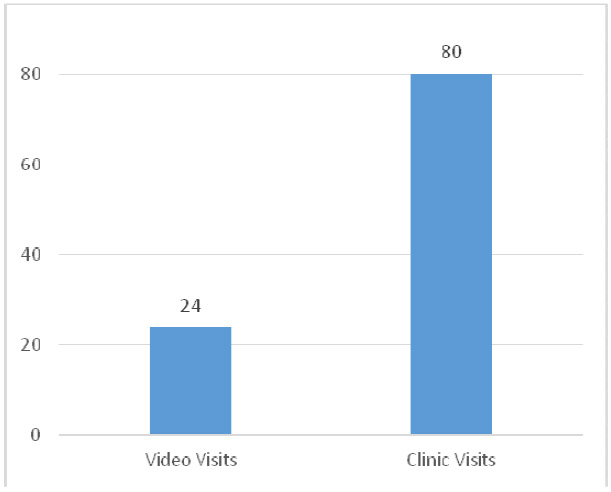
Average Cycle Time (minutes) for Video Visits and Clinic Visits
EM billing, Reimbursement, Patient Expenses
EM billing data was available for 74% (n=105) of completed video and 76% (n=116) of clinic visits. 85% (n=89) of video visits were billed as level 3 encounters (CPT code 99213) and the remaining 15% (n=16) as level 1 encounters (CPT code 99211). In comparison, 63% (n=73) of traditional clinic visits were billed as a level 3 encounters. Video visits had a proportionally larger number of visits billed as level 3 encounters (p=0.002). Of the remaining clinic visits, 1% (n=1) was billed as level 2 (CPT 99212), 35% (n=41) as level 4 (CPT code 99214) and 1% (n=1) billed as level 5 encounters (CPT code 99215).
Reimbursement and insurance-related expenses data was more limited. 48% (n=69) of completed video and 44% (n=67) of clinic visits had finalized reimbursement data. Average commercial payer reimbursement was similar for video visits compared to traditional visits ($48.89 vs. $52.64, p=0.21; Table 2). This included Level 3 video and Level 2 through 4 clinic visits. Level 3 visit reimbursement was $48.89 for video visits (n=69) and $44.37 for clinic visits (n=42). Additional reimbursement numbers for different billing levels are available for review in Table 3.
Table 2 -.
Reimbursement and Out-of-Pocket Expenses for Both Visit Types
| Video Visit | Clinic Visits | ||
|---|---|---|---|
| Commercial Payer | $48.89 | $52.64 | |
| p=0.21 | |||
| Out-of-Pocket Expenses | $29.07 | $33.10 | |
| p=0.22 |
Table 3 -.
Billing level for Video Visits and Clinic Visits
| E/M Coding | Video Visit | Clinic Visits | |
|---|---|---|---|
| Level 2 | -- | $32.71 | |
| Level 3 | $48.89 | $46.11 | |
| p=0.35 | |||
| Level 4 | -- | $69.48 |
Data regarding patient out-of-pocket expenses was only available for 21% (n=30) of completed video visits and 26% (n=40) of completed clinic visits. Similar to reimbursement rates, the average out-of-pocket expense was similar for video visits compared to traditional visits ($29.07 vs. $33.10, p=0.22; Table 2). Available data for video visits included expenses for a level 2 encounter of $7.39 (n=1) and $29.8, on average, for level 3 encounters (n=29). Patient expenses for clinic visits were, on average, $32.06 for level 3 (n=24) and $34.66 for level 4 encounters (n=16).
DISCUSSION
At our institution, video visits were completed at similar rates but billed at lower levels than clinic visits. However, video visits enhanced clinical efficiency through reduced cycle time while maintaining similar rates of reimbursement. Collectively, these findings suggest that, in states where telehealth parity laws allow for comparable reimbursement, there is a business case for the implementation of video visits for encounters that do not require a physical exam.
Our finding that video and clinic visits have similar no-show and cancellation rates is consistent with the findings of a Mayo clinic randomized control trial of post-operative follow-up after prostatectomy.3 While our analysis does not explain why video visits were cancelled, our initial experience did require adjustments in clinic workflow to address technical issues related to the implementation of this new technology. Video visit cycle time was 56 minutes shorter than cycle time for clinic visits (24 vs 80 minutes). Previous work in ophthalmology found that cycle time, defined as the amount of time in minutes that a patient spends at an office visit, for teleglaucoma visits was 34 minutes shorter than an in-person evaluation (82 vs 116 minutes); however, these programs use asynchronous telehealth to store of images for review at a later time.8,15 Our work with video visits represents one of the first evaluations of the efficiency of synchronous telehealth, highlighting that on average up to three video visits could potentially be completed in the same time one patient spends in clinic. The current literature on the financial evaluation of telehealth has focused on costs incurred by patients and health systems through traveling for care.3-5,7 We build on their work by revealing that, in a state with telehealth parity laws, video visit reimbursement and insurance expenses are similar to clinic visits. Notably, the vast majority of video visits were billed as level 3 encounters. We hypothesize that the lack of an in-person physical exam resulted in decreased billing levels and that time-based billing was the primary driver of E/M coding level rather than clinical complexity.
This study has several limitations. This was a single institution, single specialty study in an outpatient setting. These results are therefore not generalizable to inpatient, emergency urological care or other outpatient specialty clinics, especially in scenarios where physical exam findings will impact decision making. Completion rates and cycle times are specific to our institution’s existing clinic workflow and operations. Additionally, we only looked at cycle time as a metric of clinical efficiency. Without a randomized, prospective comparison of these visits, it is impossible to conclude that the difference in cycle time translates to significant change in number of patients seen. Finally, the generalizability of our findings is limited by differences in state-level telemedicine reimbursement laws as well as the policies of commercial insurers. In the state of Michigan, telemedicine reimbursement parity laws allow for video visits performed from a patient’s home or work to be reimbursed similarly to in-person appointments, based on billing level. These limitations notwithstanding, our findings are relevant for clinic visits for routine post-operative follow-up or common health conditions for which there are evaluation and management guidelines that do not include a physical exam.
As we continue to incorporate the use of telehealth within the field of urology, future research will be required to identify the ideal metrics for evaluating video visits through the progression from feasibility, to viability and finally, sustainability. These metrics could include measuring differences in number of patients seen, clinic procedures, or operative cases scheduled after implementation of video visits. As time-driven, activity-based cost accounting is translated from business applications to healthcare, there is a potential to better understand the true costs of video visits compared to clinic visits across different healthcare settings. Moreover, our work does not touch upon one of the potential promises of telehealth – improved access to specialty care. In other fields, such as ophthalmology, the use of asynchronous telemedicine has been shown to improve access to care.8,15 With an aging population and a limitation on physical space and staff, telehealth provides a path for expanding capacity while maintaining safety and appropriateness of care.16,17 Future work will be required to determine whether access to urological care is improved with the use of telehealth services. Answering these questions will have a significant impact on providers, insurers, and policy makers given the existing barriers in licensure and reimbursement for these services.
CONCLUSION
Our study demonstrates that video visits have the potential to reduce the time patients spend on follow-up care without negatively impacting reimbursement rates. However, these visits could reduce average billing levels. These findings suggest that the incorporation of video visits into practice may be more efficient for patients but may also reduce billing levels.
Further research is necessary to understand the optimal implementation of telehealth services like video visits into urology clinic workflows and what metrics should be used to define success. This will ultimately help determine not whether but where and how telehealth can live up to its potential.
Footnotes
Publisher's Disclaimer: DISCLAIMER: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our subscribers we are providing this early version of the article. The paper will be copy edited and typeset, and proof will be reviewed before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to The Journal pertain.
References
- 1.Bashshur RL, Shannon G, Krupinski EA, Grigsby J. Sustaining and Realizing the Promise of Telemedicine. Telemed e-Health. 2013;19(5):339–345. doi: 10.1089/tmj.2012.0282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viers BR, Pruthi S, Rivera ME, et al. Are patients willing to engage in telemedicine for their care: A survey of preuse perceptions and acceptance of remote video visits in a urological patient population. Urology. 2015;85(6):1233–1240. doi: 10.1016/j.urology.2014.12.064 [DOI] [PubMed] [Google Scholar]
- 3.Viers BR, Lightner DJ, Rivera ME, et al. Efficiency , Satisfaction , and Costs for Remote Video Visits Following Radical Prostatectomy: A Randomized Controlled Trial. Eur Urol. 2015;68(4):729–735. doi: 10.1016/j.eururo.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 4.Andino JJ, Guduguntla V, Weizer A, et al. Examining the Value of Video Visits to Patients in an Outpatient Urology Clinic. Urology. August 2017. doi: 10.1016/j.urology.2017.07.050 [DOI] [PubMed] [Google Scholar]
- 5.Russo JE, Mccool RR, Davies L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed e-Health. 2016;22(3):209–215. doi: 10.1089/tmj.2015.0055 [DOI] [PubMed] [Google Scholar]
- 6.Ellimoottil C Video visits in urology: How clinicians, patients benefit. Urol Times. October 2017. http://urologytimes.modernmedicine.com/urology-times/news/video-visits-urology-how-clinicians-patients-benefit?page=0,1. Accessed October 19, 2017. [Google Scholar]
- 7.Finkelstein JB, Cahill D, Kurtz MP, et al. The Use of Telemedicine for the Postoperative Urological Care of Children: Results of a Pilot Program. J Urol. 2019;202(1):159–163. doi: 10.1097/JU.0000000000000109 [DOI] [PubMed] [Google Scholar]
- 8.Arora S, Rudnisky CJ, Damji KF. Improved Access and Cycle Time with an “In-House” Patient-Centered Teleglaucoma Program Versus Traditional In-Person Assessment. Telemed e-Health. 2014;20(5):439–445. doi: 10.1089/tmj.2013.0241 [DOI] [PubMed] [Google Scholar]
- 9.Fleming NS, Becker ER, Culler SD, et al. The Impact of Electronic Health Records on Workflow and Financial Measures in Primary Care Practices. Health Serv Res. 2014;49(1pt2):405–420. doi: 10.1111/1475-6773.12133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haidar YM, Moshtaghi O, Mahboubi H, et al. Association Between Electronic Medical Record Implementation and Otolaryngologist Productivity in the Ambulatory Setting. JAMA Otolaryngol Neck Surg. 2017;143(1):20. doi: 10.1001/jamaoto.2016.2528 [DOI] [PubMed] [Google Scholar]
- 11.Scott DJ, Labro E, Penrose CT, Bolognesi MP, Wellman SS, Mather RC. The Impact of Electronic Medical Record Implementation on Labor Cost and Productivity at an Outpatient Orthopaedic Clinic. J Bone Jt Surg. 2018; 100(18):1549–1556. doi: 10.2106/JBJS.17.01339 [DOI] [PubMed] [Google Scholar]
- 12.Nikolian VC, Williams AM, Jacobs BN, et al. Pilot Study to Evaluate the Safety , Feasibility , and Financial Implications of a Postoperative Telemedicine Program. Ann Surg. 2018;268(4):700–707. doi: 10.1097/SLA.0000000000002931 [DOI] [PubMed] [Google Scholar]
- 13.American Telemedicine Association. 2019 State of the States Report: Coverage and Reimbursement.; 2019. https://cdn2.hubspot.net/hubfs/5096139/Files/ThoughtLeadership_ATA/2019StateoftheStatessummary_final.pdf.
- 14.Institute for Healthcare Improvement: Office Visit Cycle Time. http://www.ihi.org/resources/Pages/Measures/OfficeVisitCycleTime.aspx. Accessed February 10, 2018.
- 15.Thomas S-M, Jeyaraman M, Hodge WG, Hutnik C, Costella J, Malvankar-Mehta MS. The Effectiveness of Teleglaucoma versus In-Patient Examination for Glaucoma Screening: A Systematic Review and Meta-Analysis Acott TS, ed. PLoS One. 2014;9(12):e113779. doi: 10.1371/journal.pone.0113779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ellimoottil C, Boxer RJ. Bringing Surgical Care to the Home Through Video Visits. JAMA Surg. 2018;153(2):177. doi: 10.1001/jamasurg.2017.4926 [DOI] [PubMed] [Google Scholar]
- 17.Modi PK, Portney D, Hollenbeck BK, Ellimoottil C. Engaging telehealth to drive value-based urology. Curr Opin Urol. 2018;4(28):342–347. doi: 10.1097/MOU.0000000000000508 [DOI] [PubMed] [Google Scholar]


