Abstract
Background:
Missed or delayed follow-up of abnormal subcritical tests, i.e., tests that do not require immediate medical attention, can lead to poor patient outcomes. Safety-net health systems with limited resources and socially complex patients are vulnerable to safety gaps resulting from delayed management. We sought clinician perspectives to identify system challenges, vulnerable situations, and potential solutions.
Methods:
We conducted a series of 5 semi-structured focus groups with purposefully sampled clinicians from radiology, hospital medicine, emergency medicine, risk management, and ambulatory care from an urban, academic, integrated, safety-net health system. Thematic analysis identified challenges of current management of abnormal subcritical tests, vulnerable situations, and solution characteristics.
Results:
43 clinicians participated in focus groups May and June, 2015. Clinicians cited challenges in assigning responsibility for follow-up in the context of rotating providers and differing beliefs about who should take responsibility. Clinicians identified tests pending at discharge and tests requiring delayed follow-up as vulnerable situations. The lack of tracking systems and missing contact information for patients and providers exacerbated these challenges. Proposed solution characteristics involved protocols to aid in assigning responsibility, reliable paths of communication, and systems to track the status of tests. Clinicians noted a strong desire for integration of the workflow and technology solutions into existing structures.
Conclusion:
In an urban safety net setting, clinicians recommended outlining clear chains of responsibility and communication in the management of subcritical test results, and employing simple, integrated technological solutions that allow for tracking and management of tests. Existing test management solutions should be adapted to work within safety net systems, which often have fewer resources, more complex patients, and may function in the absence of integrated technology systems.
INTRODUCTION
Missed and delayed diagnoses are major patient safety and malpractice concerns that can result in serious harm and even death.1, 2 Previous literature has shown that inadequate management of clinical tests can result in missed and delayed diagnosis or treatment.3–6 Many of these tests may be considered abnormal and subcritical. Abnormal subcritical tests are tests which, when resulted, may not require immediate medical attention but could result in patient harm without appropriate follow-up at a later time. Previous literature has shown variability in subcritical test management across departments, inconsistent practices within departments, and few documented protocols.5, 7 In addition, both patients8 and physicians report dissatisfaction with current test notification systems.9, 10
The existing literature indicates a need for integrated technology and workflow solutions to address subcritical test management.4, 5, 7, 9–13 Care transitions between healthcare settings have been shown to be particularly problematic for test management.14 However, the majority of this research has been conducted in the outpatient setting, and little, if any, assesses test management in a safety net health system where enterprise electronic health records are infrequently used and providers have fewer resources to adopt new solutions.15
To understand the barriers to managing abnormal subcritical tests in the context of an integrated safety net health system and to assess potential solutions for the management of abnormal subcritical tests within this system, we sought perspectives from a diverse group of clinicians in the inpatient, emergency department, and ambulatory care setting an urban academic safety-net health system.
METHODS
We conducted and analyzed a series of 5 focus groups of clinicians in an integrated, safety-net health system in San Francisco in 2015. We chose qualitative methodology because it is useful to explore in-depth complex phenomena and for areas in which there is limited previous literature.16 This study was approved by the Institutional Review Board at the University of California, San Francisco.
Setting and context
This study occurred in an urban health system in San Francisco, which includes a large public hospital with comprehensive ambulatory specialty care and four hospital-based primary care clinics, in addition to more than 20 free-standing primary care clinics. The health system did not have an enterprise electronic health record (EHR) at the time of the study, but did have separate electronic health records for the ambulatory, inpatient, and emergency departments. The radiology and laboratory test results were resulted into all three electronic health records.
Study subjects
Focus group participants were recruited using purposeful sampling of multidisciplinary clinicians from radiology, hospital medicine, emergency medicine, risk management, and ambulatory care leadership (n=43), which rely on several different electronic health systems. The groups included physicians, nurses and nurse practitioners (Table 1). The study team emailed potential participants based on their operational leadership or educational roles with trainees in risk management, hospital medicine, emergency department, ambulatory specialty care, pediatrics, family medicine, internal medicine, and radiology. Introductory emails were sent twice if there was no response to the initial email. The email informed potential participants of the study. No compensation was given for participation. Through snowballing, invitations were extended to additional clinicians recommended by the initial contacts. Ambulatory care leadership invited research staff to a standing ambulatory care leadership committee that consisted of nursing, medical, and pharmacy leadership. Radiology invited the research staff to a standing departmental meeting that included radiology faculty and fellows. Consent was emailed prior to the meeting. Verbal consent from all participants was obtained prior to each focus group.
Table 1 –
Characterization of focus group participants (n = 43)
| Characteristic | N (%) |
|---|---|
| Gender | |
| Male | 22 (51) |
| Female | 21 (49) |
| Clinical roles | |
| Physician | 33 (77) |
| Nurse practitioner | 1 (2) |
| Registered nurse | 6 (14) |
| Other | 3 (7) |
| Department | |
| Emergency department | 3 (7) |
| Quality and risk management | 5 (12) |
| Radiology | 16 (37) |
| Inpatient services | 9 (21) |
| Ambulatory care team | 10 (23) |
Data collection
Two researchers (LG, US) trained in qualitative research methods conducted focus groups using a semi-structured focus group guide. The focus group guide was informed by current patient safety literature and team members’ health system knowledge. The goals of the focus groups were to characterize and understand current challenges in managing abnormal subcritical tests by different stakeholders and to identify solution characteristics. Specific discussion probes included questions on assigning responsibility and technology systems. Focus groups lasted approximately 1 hour, were facilitated by one or more authors, and were audio recorded and professionally transcribed to facilitate analysis (Appendix A). Themes were presented to representatives from radiology, hospital medicine, primary care and ambulatory subspecialists for confirmation.
Data analysis
We used thematic analysis with an inductive framework to identify emergent themes from the focus group transcripts17 and then deductively applied transcript excerpts to the SEIPS, or Systems Engineering Initiative for Patient Safety, model. The SEIPS model was selected as it was specifically developed to help understand patient safety issues related to healthcare structures, processes, and outcomes.18 The SEIPS model develops the work systems into the Donebedian structure-process-outpatient relationship, recognizing the role of human factors engineering and systems approaches to patient safety improvements. The model identifies structural domains and their inter-relationships including person, tasks, technology, organization, and the environment and processes and patient-quality of care and patient safety outcomes and employee and organizational outcomes.
We selected a qualitative approach to analyze our data as our goal was to understand key themes that emerged from the data, not to determine explicitly validate whether the SEIPS model was appropriate in this circumstance. Each focus group transcript was initially coded independently by 2 researchers (CC and JL) using Dedoose software.19 The codes were then iteratively refined by a multidisciplinary team (CC, JL, LG, and MH) to establish consensus and develop a coding structure. We then grouped codes into major themes and identified relationships between the emergent themes.
RESULTS
We identified several themes that mapped to domains in the SEIPS model and represented barriers to safe management of abnormal subcritical tests (Table 2). A common barrier discussed across focus groups was the lack of health information technology (IT) system integration. This health system had no enterprise EHR and almost all of the 5 departments used different EHRs to manage patient information. Few providers were open to the addition of new tools that would not be integrated into the current tools, as one hospital provider noted, “We’ve also been hearing really strongly that people are pretty maxed out and the idea of going to a new system is pretty stressful, too.”
Table 2.
Reported Barriers to Safe Management of Abnormal Subcritical Tests
| SEIPS sub-domain | Study-specific theme | Quote | Clinical Example |
|---|---|---|---|
| Health IT system integration | “I think adding another system when people are reaching a breaking point with managing multiple systems …I think it would not be well received.” – Inpatient | ||
| Technology and Tools | Tracking test and results | “So it’s a handoff, but there is not a… population-based tracking process.” – Primary care | No electronic tracking system for pulmonary nodule follow-up |
| Rotating providers | “There is no continuity with physicians.” - Radiology | ||
| Beliefs about who is responsible | ‘…I think if someone orders a study they’re responsible for the findings…– Radiology | Ordering clinician in ED or PCP? | |
| Clear paths of communication | “The problem is when you spend hours to try to track who to call.” – Radiology | ||
| Organization | Adequate staffing to allow for a reliable point of contact | “Our issue is personnel. We don’t have a staff who are dedicated (to test management), people to access that registry and then people to act upon it…”– Primary care | |
| Population served |
‘…there are patients that we serve in the specialty care clinics that don’t have primary care…I think those processes and making sure that those patients get the care they need is another population to focus on.” – Primary care ‘We do get a lot of the patients that are brought back quickly where there is no update, there is zero information in their contact information, so that makes it really challenging.” |
||
| Care transition | Some of these…are tests pending, right? So there’s no result at all…it isn’t until you actually get somebody who’s interpreted the result to determine if its critical or subcritical” – Risk management | Pulmonary nodules incidentally discovered during ED visits& hospitalizations & require outpatient follow-up | |
| Task and Test Characteristics | Time/acuity of result | ‘I think you could make a pretty clear line that if it needs to be followed up within days, it’s on the inpatient person. If it needs to be followed within weeks, then it’s reasonable to expect the PCP to do it.” – Inpatient | Follow-up time period for nodules requires handoff of care |
Many participants reported lacking the ability to track test results. The few departments that did track usually used home-grown electronic or paper registries that were not integrated or shareable and required manual updating to be functional. The lack of reliable tools and integrated technologies significantly impeded providers’ trust in the system to identify and address abnormal subcritical test results in a consistent and timely manner, and represented major gaps in the structures needed for reliable test management. A need for reliable tracking tools was particularly important to close the loop on tests requiring delayed action, and for tests pending at discharge from hospitalization. A clinical example would be the development of a tracking system to follow pulmonary nodules requiring repeat imaging months later to identify enlarging masses. This system could help address the challenge ordering providers in the emergency department face if unable to reach a patient within a particular timeframe. A workflow or technology tool could assist staff to make sure the patient, or primary care provider, is aware of the results, and receives appropriate recommended follow-up.
The majority of participants highlighted that certain organizational characteristics contributed to the challenges of test management. Participants perceived the rotation of providers on and off services in the inpatient, ED, and ambulatory settings where there were trainees, as a vulnerability and contributor to missed follow-up of abnormal subcritical tests. Participants noted that this lack of provider continuity made it difficult to assign responsibility and develop safeguards, and the necessity to hand off test management responsibility created a vulnerable situation that could result in lost information.
Participant beliefs about who is ultimately responsible for managing a given test varied based on the participants’ department. The inpatient, emergency, and radiology departments often designated primary care providers (PCPs) or the ordering provider as the responsible party. The variable acuity and time required until follow-up for a given subcritical test drove beliefs regarding who should be responsible for the test. For instance, one hospitalist said, “I think you could make a pretty clear line that if it needs to be followed up within days, it’s on the inpatient person. If it needs to be followed within weeks, then it’s reasonable to expect the PCP to do it.” For example, blood culture results need to be followed-up within days where an abnormal thyroid test could be follow-up within weeks.
However, the process of assigning responsibility was often complicated by difficulties communicating between clinicians. Many participants cited inaccurate clinician contact information and the lack of a protocol identifying who should be called as reasons communication was difficult. Also, participants stressed the importance of verifying that the information had been appropriately received. This was especially true when communication was conducted via email, as one radiologist said, “The challenge of emails for me is closing the loop because you guys also want to be able to document officially that you have closed the loop.”
Another barrier to assigning responsibility and communicating successfully was a lack of staff resources. Checking and managing a test registry, calling patients and providers, and ensuring appropriate clinical follow-up take time and staff that many departments do not have. As one ambulatory care provider stated, “I’m sure everyone can agree we’re all understaffed in all of our clinics wherever we are, and so even if we go, can we utilize it? Do we have a staff to actually be able to act up on it?”
Participants also discussed barriers related to the unique populations they serve as safety net healthcare providers, such as assigning follow-up for patients that do not have a PCP and the lack of patient contact information in the clinical record.
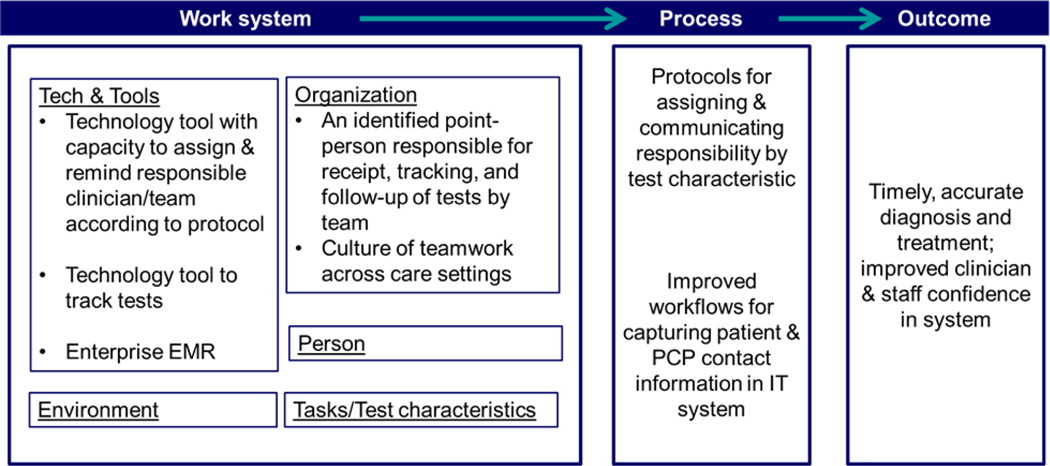
Solution characteristics
Participants discussed health information technology solutions such as a tool with the capacity to assign responsibility for test management and follow-up and to remind responsible providers in the case of tests that require delayed follow-up. They also believed a tool that could track the status of tests and was integrated into existing technology tools, would significantly decrease the risks of missed tests. Full integration of technology systems across departments as an enterprise EHR were considered important characteristics of a solution, “I would argue that if you create a new system that…say these need to be tracked and followed and it’s somehow a database that is inherently part of (the EHR), it has to integrate with (the EHR). It has to be a seamless click over.”
Another suggested solution was a dedicated staff member or members for each department who would be responsible for the receipt, tracking, and follow-up of tests, “You could have someone at each clinic who is going to be there, whose job it is to longitudinally transmit information, lab results, X-ray results to the provider.”
Participants highlighted the need for protocols for communicating and assigning responsibility based on acuity and time to follow-up of tests, as well as improved workflows for capturing patient and PCP contact information in an integrated IT system. They also discussed a more uniform culture of responsibility across care settings.
Participants believed that the implementation of these solutions would improve the timely and accurate diagnosis and treatment as well as staff and provider confidence in the system.
DISCUSSION
In a safety-net health system without an integrated electronic health record, the perception of responsibility for subcritical tests differed by department and characteristics of the test itself. Providers believed integrated IT systems with tracking capabilities would prevent missed follow-up of abnormal tests. Rotating providers, common in an academic setting, contributed to challenges in following-up on tests, especially pending tests at discharge. Missing patient contact information was also cited as a barrier. None of these issues seem distinct to safety-net systems, though lacking a PCP and/or reliable contact information are likely more common issues in safety net settings 20. The SEIPS model served as a useful framework to organize structural needs identified by the clinicians, and helped provide an organizational framework for potential systems solutions. Our study identified both technology and organization approaches necessary to address safety gaps and vulnerable situations identified by safety-net clinicians in this integrated healthcare system.
While participants noted the need for a technology solution, an established domain in the SEIPS model, many participants also expressed concern about adding new electronic systems, citing an overload of disparate systems already in use. IT solutions must consider this technology fatigue by integrating into or replacing an existing system rather than creating a new system. System burnout and change fatigue have been reported with the implementation of new information technology 21,22, and represents an important consideration when implementing any new change in safety net health systems 23. There have been technology solutions developed for the management of clinical tests. These solutions rely on an enterprise EHR, something that this and many safety net health systems do not have. 13
Moreover, while integrated technology systems with tracking and automated notification would likely improve test result management, they are not able to entirely resolve gaps in management.24, 25 Some barriers that participants discussed related to systemic characteristics that are less easy to change particularly in resource limited safety-net settings such as the availability of staff resources to assist with tracking and follow-up. A health system may require additional staffing or staffing responsibilities and new workflows to address subcritical abnormal tests even with the adoption of new tracking and notification systems. For example, if a pulmonary nodule requiring 12-month follow-up was identified in the emergency department, the staff and workflows may differ from the workflow to address an abnormal gonorrheal test which requires more immediate follow-up.
In academic health systems, residents and trainees rotate regularly, often on monthly blocks in the inpatient setting. Rotating providers represents an example of staffing structures, a domain in the SEIPS model that increases risks of missed and dropped tests, that is often not modifiable .Workflows in need to account for these rotating providers. Health systems can develop protocols and workflows to aid in transferring patient information when a hand-off occurs.26, 27 Implementation of such systems specifically for results management could mitigate the negative patient safety impacts of rotating providers. Other studies have cited workflow redesign as a way to improving test result management.4,12
Communication among staff within and across health system departments is an important domain affecting patient safety, and critical for successful handoffs regarding follow-up of an abnormal test. We found that participants reported difficulty in assigning responsibility for test management, with inconsistent in expectations across departments. This finding has been noted in other studies.5, 28 To address this challenge, protocols could be developed that include information on how to assign responsibility for a test based on variables such as test type, time to follow-up, and acuity 29 that would standardize expectations and permit more consistent workflow applications. Building consensus across stakeholders about who should be responsible for tests in certain situations, while potentially challenging, may permit a uniform protocol across departments would be helpful in decreasing variability through standardization of assignments. These instructions would outline clear chains of reliable communication including accurate contact information for the parties involved.
Particular situations were identified as particularly vulnerable for missed test follow-up. Pending tests at hospital discharge and tests requiring delayed follow-up remain a challenge that may be mitigated via an integrated tracking tool. This tracking tool could also contain accurate patient and provider contact information. Workflow interventions to encourage updating of contact information would improve tool utility. Furthermore, many studies have indicated the desire for and usefulness of automated reminder systems to aid in resulting pending tests and tests that require delayed follow-up.4, 12, 28
Our findings, which demonstrate vulnerabilities for test result management in each domain of the SEIPS model, are remarkably consistent with prior studies. Indeed, the themes that emerged from our interviews demonstrate a lack of progress despite long-standing awareness of the safety gap in test results management.
This study has several limitations. Participation in the study was voluntary; the attitudes and practices of respondents may differ from non-participants. Additional demographic information and practice experience of participants was not available. One of the researchers who conducted the focus groups also participated in the analyses of the transcripts. We attempted to limit inherent biases by having a larger research group develop the coding manual and identify themes. We collected limited demographic information about our participants. Our findings may not be generalizable to providers practicing in other health systems or regions. This qualitative research is exploratory by nature; the findings will need to be confirmed in future studies.
On the ground in a safety-net health care setting, providers across departments and settings share awareness of the risk inherent in suboptimal test results management processes and express a desire for improvement, echoing earlier studies. Our results will inform the design and implementation of an intervention which will provide a technological approach integrated with the electronic health record, in tandem with workflow redesigns and protocols to improve the management of abnormal subcritical tests. This multi-prong solution is consistent with the SEIPS model which recognizes the various structural domains that influence the processes and patient safety-outcomes. We are not aware of existing health care systems utilizing comprehensive ambulatory abnormal test results management processes. Our findings from our focus group analysis suggest that safety-net health systems have many similar operational and structural challenges in managing subcritical abnormal tests as non-safety-net settings. These challenges are further exacerbated by limited health-system resources, lack of adequate technology infrastructure, and patient populations with communication challenges and frequent lacking stable housing, contact information, and health care access.
Figure 1:
Proposed solutions for managing abnormal subcritical tests using an adapted SEIPS model
Acknowledgments
This study was funded by the Agency for Healthcare Research and Quality P30HS023558 as part of the San Francisco Ambulatory Safety Center for Innovation (ASCENT)
Contributor Information
Cassidy Clarity, University of California, San Francisco, Division of General Medicine.
Urmimala Sarkar, University of California San Francisco, Division of General Medicine, Center for Vulnerable Populations.
Jonathan Lee, University of California San Francisco, Division of Hospital Medicine.
Margaret Handley, University of California San Francisco, Division of General Internal Medicine, Center for Vulnerable Populations.
L. Elizabeth Goldman, University of California San Francisco, Division of General Internal Medicine, Affiliate Faculty Philip R. Lee Institute for Health Policy Studies, University of California San Francisco.
REFERENCES
- 1.Gandhi TK Fumbled handoffs: one dropped ball after another, Ann Intern Med. 2005, 142, 352–358. [DOI] [PubMed] [Google Scholar]
- 2.Gandhi TK; Kachalia A; Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims, Ann Intern Med. 2006, 145, 488–496. [DOI] [PubMed] [Google Scholar]
- 3.Giardina TD; King BJ; Ignaczak AP, et al. Root cause analysis reports help identify common factors in delayed diagnosis and treatment of outpatients, Health Aff (Millwood). 2013, 32, 1368–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore C SO, Trikha A, Lin J Timely follow-up of abnormal outpatient test results: Perceived barriers and impact on patient safety, Journal of Patient Safety. 2008, 4, 241–244. [Google Scholar]
- 5.Callen JL; Westbrook JI; Georgiou A; Li J. Failure to follow-up test results for ambulatory patients: a systematic review, J Gen Intern Med. 2012, 27, 1334–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cram P; Rosenthal GE; Ohsfeldt R; Wallace RB; Schlechte J; Schiff GD Failure to recognize and act on abnormal test results: the case of screening bone densitometry, Jt Comm J Qual Patient Saf. 2005, 31, 90–97. [DOI] [PubMed] [Google Scholar]
- 7.Elder NC; McEwen TR; Flach JM; Gallimore JJ Management of test results in family medicine offices, Ann Fam Med. 2009, 7, 343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meza JP; Webster DS Patient preferences for laboratory test results notification, Am J Manag Care. 2000, 6, 1297–1300. [PubMed] [Google Scholar]
- 9.Poon EG; Gandhi TK; Sequist TD; Murff HJ; Karson AS; Bates DW “I wish I had seen this test result earlier!”: Dissatisfaction with test result management systems in primary care, Arch Intern Med. 2004, 164, 2223–2228. [DOI] [PubMed] [Google Scholar]
- 10.Murff HJ; Gandhi TK; Karson AK, et al. Primary care physician attitudes concerning follow-up of abnormal test results and ambulatory decision support systems, Int J Med Inform. 2003, 71, 137–149. [DOI] [PubMed] [Google Scholar]
- 11.Singh H; Graber M. Reducing diagnostic error through medical home-based primary care reform, Jama. 2010, 304, 463–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hysong SJ; Sawhney MK; Wilson L, et al. Understanding the management of electronic test result notifications in the outpatient setting, BMC Med Inform Decis Mak. 2011, 11, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poon EG; Blumenfeld B; Hamann C, et al. Design and implementation of an application and associated services to support interdisciplinary medication reconciliation efforts at an integrated healthcare delivery network, J Am Med Inform Assoc. 2006, 13, 581–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Callen J; Georgiou A; Li J; Westbrook JI The safety implications of missed test results for hospitalised patients: a systematic review, BMJ Qual Saf. 2011, 20, 194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Institute of Medicine America’s Health Care Safety Net Intact but Endangered, Washington D.C: : National Academy Press, 2000. [PubMed] [Google Scholar]
- 16.Pope C; Mays N. Reaching the Parts Other Methods Cannot Reach - an Introduction to Qualitative Methods in Health and Health-Services Research, Brit Med J. 1995, 311, 42–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Braun V CC Using thematic analysis in psychology, Qualitative Research in Psychology. 2006, 3, 77–101. [Google Scholar]
- 18.Carayon P; Hundt AS; Karsh B-T, et al. Work system design for patient safety: the SEIPS model, Qual Saf Health Care. 2006, 15, i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dedoose.). Los Angeles: SocioCultural Research Consultants, LLC, 2015, web application for managing, analyzing, and presenting qualitative and mixed method research data [Google Scholar]
- 20.Cheung PT; Wiler JL; Lowe RA; Ginde AA National study of barriers to timely primary care and emergency department utilization among Medicaid beneficiaries, Ann Emerg Med. 2012, 60, 4–10 e12. [DOI] [PubMed] [Google Scholar]
- 21.Hanauer DA; Branford GL; Greenberg G, et al. Two-year longitudinal assessment of physicians’ perceptions after replacement of a longstanding homegrown electronic health record: does a J-curve of satisfaction really exist?, J Am Med Inform Assoc. 2016, DOI 10.1093/jamia/ocw077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ford EW; Silvera GA; Kazley AS; Diana ML; Huerta TR Assessing the relationship between patient safety culture and EHR strategy, International journal of health care quality assurance. 2016, 29, 614–627. [DOI] [PubMed] [Google Scholar]
- 23.Lyles CR; Aulakh V; Jameson W; Schillinger D; Yee H; Sarkar U. Innovation and transformation in California’s safety net health care settings: an inside perspective, Am J Med Qual. 2014, 29, 538–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh H; Thomas EJ; Sittig DF, et al. Notification of abnormal lab test results in an electronic medical record: do any safety concerns remain?, Am J Med. 2010, 123, 238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wahls T; Haugen T; Cram P. The continuing problem of missed test results in an integrated health system with an advanced electronic medical record, Jt Comm J Qual Patient Saf. 2007, 33, 485–492. [DOI] [PubMed] [Google Scholar]
- 26.Lee SH; Phan PH; Dorman T; Weaver SJ; Pronovost PJ Handoffs, safety culture, and practices: evidence from the hospital survey on patient safety culture, BMC Health Serv Res. 2016, 16, 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheu L; Fung K; Mourad M; Ranji S; Wu E. We need to talk: Primary care provider communication at discharge in the era of a shared electronic medical record, J Hosp Med. 2015, 10, 307–310. [DOI] [PubMed] [Google Scholar]
- 28.Lin JJ; Dunn A; Moore C. Follow-up of outpatient test results: a survey of house-staff practices and perceptions, Am J Med Qual. 2006, 21, 178–184. [DOI] [PubMed] [Google Scholar]
- 29.Brigham and Women’s Hospital internal protocol.). personal communications.