Abstract
Cholecystocolonic fistula with associated idiopathic megabowel (megacolon and megarectum) is a rare presentation as acute large bowel obstruction. Frequently presenting with chronic constipation, acute bowel obstruction is rarely encountered in the presence of concomitant cholecystocolonic fistula. This presents diagnostic and management difficulties with no consensus on appropriate surgical approach. This case highlights the outcomes following emergency total colectomy and subtotal cholecystectomy as a single-stage procedure for a 68-year-old man presenting with cholecystocolonic fistula secondary to idiopathic megabowel as acute large bowel obstruction.
Keywords: surgery, general surgery
Background
Idiopathic megabowel comprises megarectum and megacolon with no underlying cause identified.1 Although persistently dilated bowel leads to intractable constipation, this seldom presents in the acute surgical setting. In addition, a cholecystocolonic fistula is formed by an abnormal communication between the gallbladder and right-sided colon. This is the second most common form of cholecystoenteric fistula following cholecystoduodenal fistula and is present in approximately 0.1% of cholecystectomies.2 However, variable clinical features make preoperative diagnosis difficult. We present a rare occurrence and treatment outcomes of cholecystocolonic fistula associated with idiopathic megabowel causing large bowel obstruction.
Case presentation
A 68-year-old man presented as a surgical emergency with a history of confusion, central abdominal pain, a single episode of bilious vomiting, abdominal distension and unspecified weight loss. He had not opened his bowel or passed flatus for 5 days but usually maintained a once daily bowel habit. He had an open appendicectomy aged 14 and suffered with mild chronic obstructive pulmonary disease (COPD) controlled with Ellipsis and Salbutamol inhalers. A CT scan had diagnosed a megarectum in 2014. He had smoked 20 cigarettes per day for 53 years since aged 15 but had stopped 1 month prior to admission and drank one measure of whiskey per night. He had an exercise tolerance of 20 yards. On examination, he was pale with generalised abdominal pain and peritonism with no masses. Per rectal examination revealed a capacious, empty rectum.
Investigations
A baseline haematology and biochemistry profile was obtained which revealed a haemoglobin of 81 g/L, a C reactive protein of 97 mg/L, white cell count of 2.7×109/L (neutrophils 1.79×109/L, lymphocytes 0.67×109/L), procalcitonin 3.63 ng/mL, albumin of 17 IU/L, glomemular filtration rate (GFR) of 76 mL/min/1.73 m2. Furthermore, serum folate was 2.2 µg/L, serum iron was 2.3 μmol/L with a low total iron-binding capacity of 33.9 μmol/L. His liver and renal function tests were within normal limits.
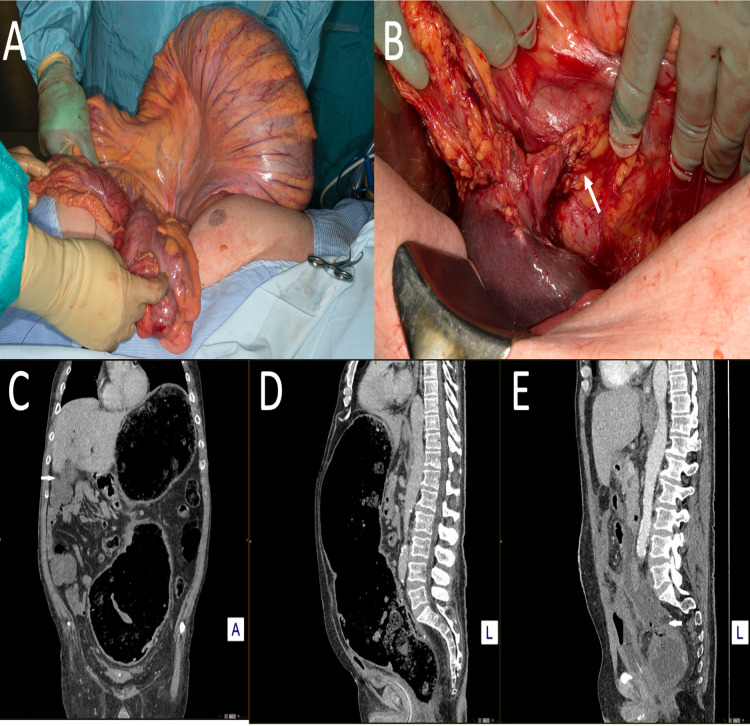
A CT scan of the abdomen and pelvis performed showed a megarectum and megacolon with a reported maximum diameter reaching 22 cm with the calibre change to normal colon in the left hypochondrium. In the rectosigmoid junction there was submucosal gas with oedema but no perforation was identified. Air densities were noted in the left lobe of the liver (figure 1). There were no reported gallstones, common bile duct (CBD) stones or intrahepatic duct dilatation on the CT scan.
Figure 1.
Radiological and intraoperative findings of idiopathic megabowel and cholecystocolonic fistula presenting as acute large bowel obstruction. (A) Chronic dilated colon. (B) Cholecystocolonic fistula (white arrow). (C) Coronal CT scan showing evidence of pneumobilia. (D) Saggital CT scan showing chronic megabowel. (E) Saggital CT scan view showing rectal stump blowout and intra-abdominal collection (white arrow).
Treatment
The patient was transferred to the operating theatre for an emergency exploratory laparotomy. Intraoperatively the megarectum and megacolon were confirmed with obstruction of the large bowel at the hepatic flexure (figure 1). Moreover, the gallbladder was found to be fistulating into the colon at the hepatic flexure (figure 1). Subsequently, a total colectomy and end ileostomy was formed. The dilated rectal stump was not amenable to standard surgical stapling, so was oversewn with 2-0 prolene in double layers. In addition, a subtotal cholecystectomy was performed to treat the cholecystocolonic fistula because of difficulty identifying the biliary anatomy. After washout of the abdomen with 0.9% normal saline, a 20 Ch Robinsons Drain was left in the hepatic bed along with a 30 Ch Foley’s catheter in the rectal stump to reduce the risk of rectal stump blowout. The patient was transferred for observation on the surgical high-dependency unit (level II bed). Histology confirmed a maximal circumference of 32 cm for the sigmoid colon stercoral ulcerations extending to the muscularis propria were identified distally. However, the proximal colon was thin and dilated consistent with recent obstruction. The gallbladder demonstrated acute-on-chronic cholecystitis eroding into the colon at the hepatic flexure, fistulating to the muscularis propria. Microscopically, reduced autonomic nerves of the myenteric plexus were shown in the megacolon region but not in to the proximal obstructed large bowel (figure 2).
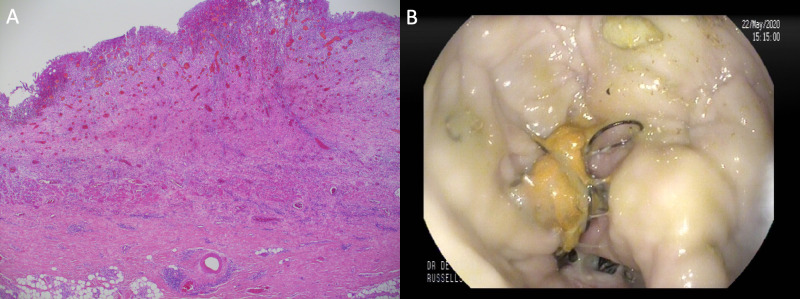
Figure 2.
: Histological confirmation of reduction of autonomic nerves of myenteric plexus and absence of ganglion cells with a 1 cm thick rectal wall precluding use of stapling devices (A). Endoscopic washout of rectal stump blowout (B).
Outcome and follow-up
The patient remained on the surgical high-dependency unit for 2 weeks requiring total parenteral nutritional support. During this stay, he developed paralytic ileus and on the sixth postoperative day an intra-abdominal collection was identified which was radiologically drained with appearances consistent with bile and an output of 400 mL/ per day was noted. Antibiotic therapy was guided by the microbiologist for initial treatment of intra-abdominal collection.
He later developed a rectal stump blowout which was managed with repeated endoscopic rectal stump washouts as an alternative to endosponge Vaccum Assisted Closure (VAC) therapy (figure 2). After confirming high bilirubin levels of 703 μmol/L on the 40th postoperative day in the drain fluid, an Endoscopic Retrograde Cholangiopancreatography (ERCP) was performed along with sphincterotomy whereby a CBD stone was extracted and a plastic stent placed in the CBD. The abdominal drain was subsequently removed. The patient thereafter tested positive for COVID-19 on the 42nd postoperative day for which he required supportive ward-based care with supplemental oxygen. He was discharged after a 2-month stay.
Discussion
Chronic idiopathic megabowel is defined by a persistent rectal diameter greater than 6.5 cm at the pelvic brim leading to intractable constipation and faecal impaction with negative consequences on quality of life.3 4 The condition equally affects men and women and can occur in children as well as adults.4 5 The cause may be Hirschsprung disease, anorectal obstruction, neurological disorders or endocrine disorders although it is often unknown.6 The pathological features are characterised by colonic hypomobility, rectal sensory dysfunction and hypoganglionosis as well as reduced resting anal canal pressure which may reflect impaired internal sphincter function.4 7 8 Presentation of idiopathic megabowel is uncommon in the emergency setting with few reports of acute presentation. These include isolated hypoganglionosis causing megarectum, toxic megacolon, phytobezoar obstruction and sigmoid volvulus.9–12 Thus, this rare occurrence of acute large bowel obstruction may in part be due to poor functioning enlarged colon and rectum. The histology from our patient confirmed reduction of myenteric plexus autonomic neurons which would support hypoganglionosis as part of the pathophysiology in this case. Moreover, managing his persistent hypoalbuminemia and hypotension was challenging and may explain the rectal stump blowout and this possibility needs to be anticipated and mitigated by rectal tubes and surgical drains.
In addition, cholecystocolonic fistula has an incidence of 0.06%–0.14% and is the second most frequent cholecystoenteric fistula representing 8%–26.5% of such fistulas.2 Common presenting features include chronic diarrhoea, right upper quadrant pain, vitamin K malabsorption and pneumobilia.2 13 The most common cause is chronic inflammation from gallstone disease, colonic diverticular disease, infectious colitis and trauma.2 14 Treatment options are divided into uncomplicated or complicated emergency situations.2 In uncomplicated situations, a staged colonic resection with cholecystectomy is performed with no consensus on the order of resection.2 Furthermore, there is no consensus on emergency operations which are dependent on the complexity of the fistula, presence of bleeding or obstruction.2
The approach adopted in the present case is justified on the basis of the complex presentation where the priority was colonic resection and so a partial cholecystectomy was performed to avoid risking damage to critical biliary structures due to unclear anatomy. As in our patient, there is a possibility of migrating stones to the CBD which can safely be managed post surgery and this should be actively monitored for. Furthermore, CT scans have a reported sensitivity of 65%–88% for identifying CBD stones; however, the need for emergent management did not allow for preoperative Magnetic Resonance Cholangiopancretography (MRCP).15 If the patient had deranged Liver Function Test (LFTs), or CT scan evidence of CBD stones or a dilated biliary tree, a preoperative or intraoperative ERCP could have been considered although not without risk, exacerbated by aberrant anatomy.
The treatment options for idiopathic megabowel also lack consensus and have been extensively reviewed.1 These include subtotal colectomy, segmental colectomy, anterior resection, proctectomy, Duhamel procedure, internal sphincterotomy, division of puborectalis or stoma.1 Treatment options are tailored to the degree or bowel involvement. However, there are reports of recurrent constipation with some treatment options as well as complications.1 Overall success has been reported in 101 out of 142 patients treated with subtotal colectomy with a morbidity rate of 23.6%.1 In addition, management of the rectal stump to reduce the risk of complications is not clear given the chronic dilatation. Studies in ulcerative colitis patients undergoing emergency subtotal colectomy suggest leaving an intra-abdominal rectal stump is safe.16 Moreover, emergency surgery and subcutaneous rectal stump are associated with increased risk of complications.16 The rectal stump blowout was anticipated; hence, a hand-sewn technique as commercial stapling devices are not adequate to safely staple thickened tissue and in addition a large rectal catheter was secured in the rectal stump for decompression. Moreover, the added complexity of an acute bowel obstruction in the presence of a cholecystocolonic fistula necessitated a total colectomy and partial cholecystectomy which we have shown to be an appropriate and safe emergency treatment option.
Learning points.
Idiopathic megabowel is a rare presentation of large bowel obstruction.
Concomitant pathology such as cholecystocolonic fistula adds to the complexity of management.
We advocate a single procedure to manage dual pathologies in the acute setting in the form of a cholecystectomy and subtotal colectomy.
Rectal stump blowout should be anticipated in patients undergoing subtotal colectomy for complicated megabowel.
The use of endosponge VAC therapy has become popular recently but not widely available; hence, repeated endoscopic rectal stump washout could be an alternative management technique.
Footnotes
Twitter: @fembimps
Contributors: FM drafted the manuscript, obtained consent and reviewed the notes. OA reviewed and advised on radiological imaging as well as proof read manuscript. MA helped revise the manuscript and proofreading. AAA managed the patient involved, originated the idea for the case report, proof-read manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gladman MA, Scott SM, Lunniss PJ, et al. Systematic review of surgical options for idiopathic megarectum and megacolon. Ann Surg 2005;241:562–74. 10.1097/01.sla.0000157140.69695.d3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costi R, Randone B, Violi V, et al. Cholecystocolonic fistula: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg 2009;16:8–18. 10.1007/s00534-008-0014-1 [DOI] [PubMed] [Google Scholar]
- 3.Todd IP. Discussion on megacolon and megarectum with the emphasis on conditions other than Hirschsprung's disease. Proc R Soc Med 1961;54:1035–10. [PubMed] [Google Scholar]
- 4.Gattuso JM, Kamm MA. Clinical features of idiopathic megarectum and idiopathic megacolon. Gut 1997;41:93–9. 10.1136/gut.41.1.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnes PR, Lennard-Jones JE, Hawley PR, et al. Hirschsprung's disease and idiopathic megacolon in adults and adolescents. Gut 1986;27:534–41. 10.1136/gut.27.5.534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehrenpreis T. Megacolon and megarectum in older children and young adults. classification and terminology. Proc R Soc Med 1967;60:799–80. [PMC free article] [PubMed] [Google Scholar]
- 7.Chiarioni G, Bassotti G, Germani U, et al. Idiopathic megarectum in adults. An assessment of manometric and radiologic variables. Dig Dis Sci 1995;40:2286–22. 10.1007/BF02209019 [DOI] [PubMed] [Google Scholar]
- 8.Verduron A, Devroede G, Bouchoucha M. Megarectum. Dig Dis Sci 1988;33:1164–1. [DOI] [PubMed] [Google Scholar]
- 9.Aldossary MY, Privitera A, Elzamzami O, et al. A rare case of adult-onset rectosigmoid hypoganglionosis. Am J Case Rep 2018;19:557–61. 10.12659/AJCR.907109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qadir I, Salick MM, Barakzai A, et al. Isolated adult hypoganglionosis presenting as sigmoid volvulus: a case report. J Med Case Rep. 2011;5:44. 10.1186/1752-1947-5-445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pescatori M, Mattana C, Castiglioni GC. Adult megacolon due to total hypoganglionosis. Br J Surg 1986;73:765. 10.1002/bjs.1800730930 [DOI] [PubMed] [Google Scholar]
- 12.Karpagam B, Vinayagam S, Kishore J, et al. Isolated adult hypoganglionosis presenting as sigmoid phytobezoar: a case report. Int J Sci Stud 2015;2pp.:139. [Google Scholar]
- 13.Savvidou S, Goulis J, Gantzarou A, et al. Pneumobilia, chronic diarrhea, vitamin K malabsorption: a pathognomonic triad for cholecystocolonic fistulas. World J Gastroenterol 2009;15:4077. 10.3748/wjg.15.4077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glenn F, Reed C, Grafe WR. Biliary enteric fistula. Surg Gynecol Obstet 1981;153:527–31. [PubMed] [Google Scholar]
- 15.Miller FH, Hwang CM, Gabriel H, et al. Contrast-enhanced helical CT of choledocholithiasis. AJR Am J Roentgenol 2003;181:125–30. 10.2214/ajr.181.1.1810125 [DOI] [PubMed] [Google Scholar]
- 16.Lissel M, Omidy S, Myrelid P, et al. The handling of the rectal stump does not affect severe morbidity after subtotal colectomy for ulcerative colitis: a retrospective cohort study. Scand J Surg 2020;109:238–43. 10.1177/1457496919857269 [DOI] [PubMed] [Google Scholar]