Abstract
Background: Historically, fewer than half of American Indians and Alaska Natives (AI/AN) with diabetes received the annual diabetic retinopathy (DR) examination that is considered the minimum standard of care; this rate is similar to that of the general United States (U.S.) population with diabetes.
Solution: The Indian Health Service-Joslin Vision Network (IHS-JVN) Teleophthalmology Program in 2000 to increase compliance with DR standards of care among AI/AN through validated, primary care-based telemedicine. The IHS-JVN provides remote diagnosis of DR severity, with a report including management recommendations that is returned to the patient's primary care provider. The program conforms with the American Telemedicine Association (ATA) Practice Guidelines for Ocular Telehealth-Diabetic Retinopathy.
Outcomes: The IHS-JVN has been expanding incrementally since the first patients were recruited in 2000; this expansion coincides with large improvements in the annual DR examination rates reported as part of local, regional, and national regulatory compliance under the Government Performance and Results Act (GPRA). Currently, with 99 clinical implementations in 23 states, IHS-JVN is the largest primary care-based ATA validation category three telemedicine program in the U.S.
Summary: This article describes the program's workflow, imaging and reading technologies, diagnostic protocols, reports to providers, training, quality assurance processes, and geographical distribution. In addition to its clinical use, the program has been utilized in research on utilization of diabetic eye care, cost-effectiveness, technology development, and DR epidemiology of the AI/AN population. Potential next steps for this program are discussed.
Keywords: telemedicine, telehealth, teleophthalmology, ophthalmology
Introduction
At 15.1%, the age-adjusted rate of diagnosed diabetes is higher in American Indians and Alaska Natives (AI/AN) than any other major race/ethnic group in the United States (U.S.).1 AI/AN also tend to have higher rates of diabetes-related complications.2 Diabetic retinopathy (DR) is the most common microvascular complication of diabetes3 and is the leading cause of moderate and severe vision loss among working age adults.4 Timely diagnosis and treatment of DR is effective in substantially reducing vision loss due to DR, but approximately half of patients with diabetes in the United States do not receive the recommended annual DR examination.5,6 Many factors contribute to this low exam rate, including access to care and patient awareness.7,8
To increase the rate that AI/AN with diabetes receive DR examinations, the Indian Health Service launched the Joslin Vision Network (IHS-JVN) Teleophthalmology Program in 2000. The program arose from a federal, multicenter grant to support research for improved evaluation and management of diabetes and DR. Work leading to the IHS-JVN began in 1999 with the development of the technical infrastructure, Reading Center, and clinical protocols modeled after the JVN at the Joslin Diabetes Center (JDC).9 Discrete aspects of the IHS-JVN and the JDC JVN have been described.10–14 This article gives a broad overview of the program's main components and outcomes.
American Telemedicine Association Validation Categories
DR best practices combined with telemedicine standards have been used extensively in the IHS-JVN. In turn, the IHS-JVN has participated in standards development for telemedicine, particularly the American Telemedicine Association (ATA) Telehealth Practice Recommendations for Diabetic Retinopathy.15,16 The practice recommendations describe four validation categories, based on the Early Treatment Diabetic Retinopathy Study (ETDRS), the gold standard for DR diagnosis and treatment.15–17 The IHS-JVN is an ATA Category 3 program, meaning the program's clinicians identify the ETDRS defined clinical levels of DR and diabetic macular edema (DME; central involved and non-central involved) severity with a diagnostic accuracy that matches clinical retinal examination through dilated pupils or ETDRS photographs (Table 1, last column). Functionally, this means that levels of non-proliferative DR (NPDR) that are not yet considered sight-threatening can be found, referred for eye or other specialty care as needed, and medically managed appropriately before they progress to severe levels of DR. A Category 3 program also provides a management plan commensurate with the clinical recommendations that would have resulted from a traditional ophthalmology-based clinical retinal examination through dilated pupils. Category 1 programs differentiate between patients who have no DR and those who have any form of DR. Category 2 programs differentiate between patients who do or do not have potentially sight-threatening DR requiring prompt referral for eye care.
Table 1.
Classification Matrix
| MODIFIED AIRLIE HOUSE CLASSIFICATION FOR USE IN THE ETDRS |
CORRESPONDING CLINICAL SCALES FOR DR AND DME BY ATA VALIDATION CATEGORY |
|||
|---|---|---|---|---|
| NUMERIC LEVEL | CLINICAL SEVERITY SCALE FOR DR | CATEGORY 1 | CATEGORY 2 | CATEGORY 3 |
| 10 | DR absent | No or minimal DR | No or less severe DR | No DR |
| 12 | Non-DR abnormalities | |||
| 14 | DR questionable | |||
| 15 | DR questionable | |||
| 20 | Microaneurysms only | Minimal DR | ||
| 35 | Mild NPDR | More than minimal DR | Mild NPDR | |
| 43 | Moderate NPDR | Moderate NPDR | ||
| 47 | Moderately severe NPDR | |||
| 53 | Severe NPDR | Severe or worse levels of NPDR | Severe NPDR | |
| 53E | Very severe NPDR | Very severe NPDR | ||
| 60 | Inactive PDR | Quiescent PDR | ||
| 61 | Mild PDR | PDR | Less than high risk PDR | |
| 65 | Moderate PDR | |||
| 71/75 | High-risk PDR | High risk PDR | ||
| 81 | Advanced PDR: fundus partially obscured, center of macula attached | |||
| 85 | Advanced PDR: posterior fundus obscured, center of macula detached | |||
| 90 | Cannot grade, even for 81 or 85 | Cannot grade | Cannot grade | Cannot grade |
| NA | No DME | DME absent | DME absent | DME absent |
| NA | DME not central involved | DME present | DME present | DME not central involved |
| NA | DME central involved | DME central involved | ||
| NA | Cannot grade | Cannot grade | Cannot grade | Cannot grade |
Category 4 validation is for a system that matches or exceeds the ability of ETDRS photos to identify lesions of DR to determine levels of DR and DME.
No Category 4 programs currently exist, and, therefore, this category is not shown here.18
ATA, American Telemedicine Association; DME, diabetic macular edema; DR, diabetic retinopathy; ETDRS, Early Treatment Diabetic Retinopathy Study; NA, not applicable; NPDR, nonproliferative DR; PDR, proliferative DR.
The ATA validation categories do not constitute a quality continuum, but rather exist to optimize teleretinal services for a variety of settings. In the IHS, services are provided directly or indirectly through contracts or compacts with tribes or Tribal Organizations (TOs) and grants to Urban Indian Organizations (UIOs).19 The IHS currently includes 46 hospitals (24 are IHS operated, 22 are tribally operated) and 568 ambulatory facilities (92 are IHS operated, 476 are tribally operated) in 35 states,20 serving a user population (i.e., the number of patients who used IHS-funded services at least once in the most recent 3 years) of 1.6 million.19 Most of the ambulatory facilities are rural with limited availability of specialty providers.21 Given the largely rural context with limited access to specialists, the IHS-JVN program was designed to recruit patients opportunistically when they present for primary care and to minimize referrals for specialty care.
The ATA validation categories do not include measures for non-DR findings, but such findings are common and may be associated with severe vision loss and/or general health risks. Thus, the JVN protocol was studied to ensure its capacity to identify non-DR findings as well (e.g., cataract, age-related maculopathy choroidal lesions, etc.).22,23
A few telemedicine programs for DR are validated to ATA Category 3. The IHS-JVN is the largest primary care-based ATA Category 3 program in the U.S.
Government Performance and Results Act
The IHS-JVN conforms with Government Performance and Results Act (GPRA), which provides for annual, national reporting of defined clinical outcomes considered key indicators of health care quality.24 The GPRA defines a qualified retinal evaluation as: (1) a dilated retinal evaluation by an optometrist or ophthalmologist; (2) seven standard fields stereoscopic photos (ETDRS) evaluated by an optometrist or ophthalmologist; or (3) any photographic method formally validated to seven standard fields (ETDRS). The IHS-JVN satisfies the latter of these options.
Clinical Workflow
Clinical workflow of the IHS-JVN begins with opportunistic recruitment of patients during primary care encounters (Fig. 1). A certified Imager acquires a standardized series of retinal photographs specific to one of two imaging technologies (described below) and conducts limited diabetes and DR education during the encounter, using the patients' retinal images as conversation points. The Imager also looks at the patients' images to determine whether urgent assessment is needed from the Reading Center for possible urgent or sight-threatening findings (i.e., STAT read).
Fig. 1.
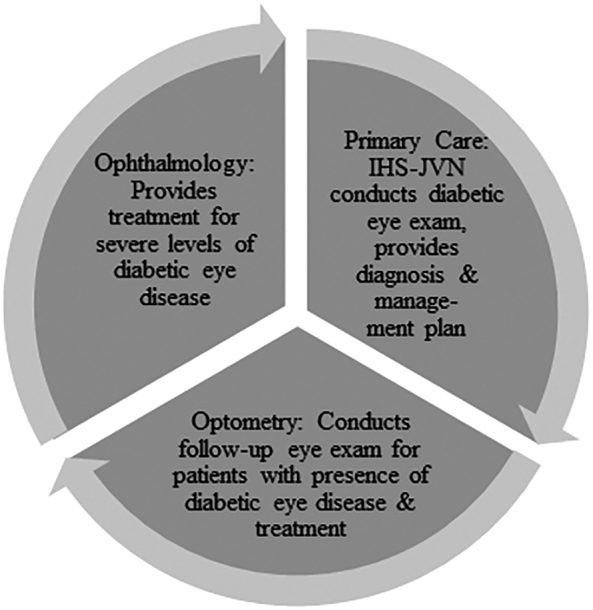
Intended clinical workflow of the IHS-JVN program. IHS-JVN, Indian Health Service-Joslin Vision Network.
The images are saved locally and then securely transmitted to the IHS-JVN National Reading Center at the Phoenix Indian Medical Center (PIMC) for assessment according to a standardized protocol performed by certified optometrist, teleretinal Readers with ophthalmologist oversight. The Reader diagnoses DR and DME severity level by using ETDRS rules-based, validated computer-assisted decision support and recommends a management plan in a report sent to the patient's primary care provider and imported into the electronic health record (EHR). If follow-up eye or other specialty care is needed, it is the responsibility of the primary care staff to make that referral. There are currently four Readers at PIMC.
Technologies and Protocols
The IHS-JVN technology has a modular architecture and a suite of applications for image acquisition, database management/monitoring/reporting, picture archiving and communication system, image display/post-imaging processing, study reading/reporting with computer-assisted decision support, and quality assurance (QA).
Image acquisition
The program uses two configurations of commercially available technology for image acquisition. The first configuration uses a low-illumination, nonmydriatic fundus photography (NMFP) digital imaging system (Topcon NW6S; Topcon Medical Systems, Inc., Paramus, NJ) with a custom digital camera back that provides low-light exposure capability to reduce reflexive pupillary constriction from multi-image light exposures (Megavision Retinal Image Capture; Santa Barbara, CA).25 Three non-simultaneous stereo pair 45° (degree) and two non-simultaneous stereo pair 30° digital images of the retina of each eye are obtained. One external image of the anterior segment of each eye is also obtained. The NMFP showed substantial agreement with ETDRS controls for diagnosis of DR severity level (unweighted κ = 0.81, 95% confidence interval = 0.73–0.89).25
The second configuration is nonmydriatic ultrawide-field imaging (UWFI) scanning laser ophthalmoscopy (Daytona, Optos, plc, Dunfermline, United Kingdom). The UWFI protocol includes non-simultaneous stereo pair 200° images from each eye, centered on the macula. The UWFI showed perfect agreement with ETDRS photography in 84% of cases, and agreement within one level of severity in 91% of cases (unweighted κ = 0.79).26
The IHS-JVN introduced UWFI to the program in 2014. It has become the default imaging system for new deployments and upgrades, because it has greater clinical accuracy, requires fewer images, incorporates automatic image acquisition, and lowers the proportion of poor images from which Readers cannot make a diagnosis of DR/DME severity level.27 However, the NMFP retinal imager is portable and durable, so it is still used in smaller and more remotely located settings requiring a durable and/or portable imager.
Image grading
The IHS-JVN images are transmitted to the IHS-JVN National Reading Center via an internet-based medical informatics program called the Comprehensive Diabetes Management Program.28 The software automatically imports patient demographics, diabetes duration, medications, laboratory data, blood pressure, and problem list from the EHR. The Imager manually supplements this information if needed.
The IHS-JVN DR grading details are shown in Table 1 (Category 3 column). In addition, grading for DME severity is based on stereoscopic assessment. Grades include: (1) absent; (2) not clinically significant, characterized by retinal thickening or hard exudates at or within 3,000 μm from the fovea or thickening in the posterior pole within the arcades, but outside the threshold for Clinically Significant Macular Edema (CSME); and (3) CSME, characterized by retinal thickening at or within 500 μm of the fovea, hard exudates at or within 500 μm of the fovea with adjacent retinal thickening, or one or more disk areas of retinal thickening, any part of which is within 1,500 μm of the fovea or with center involvement.29
If a conclusive determination of the level of DR or DME cannot be made, the Reader reports the study as ungradable for that condition. Stereo imaging and overlapping retinal fields provide redundancy of data within a single retinal field, so images may be ungradable for one condition but sufficient to grade for another. An ungradable outcome triggers a recommendation for referral. Usually, the recommended follow-up is within 3 months; however, the timeframe may be shorter depending on the basis for ungradability, whether other pathology is found, the patient's health status, and other factors.
Non-DR abnormalities evident in the images are included in the management recommendations.22,23
Image reporting
The Reader generates a report for each IHS-JVN study, which is sent to the originating site for communication to the patient via their primary care physician or any other member of the primary care team. The report includes available information on patient risk factors for progression of DR/DME, DR/DME severity, findings of nondiabetic eye disease, and the recommended management plan (Table 2). The recommended plan may suggest modification of identified DR risk factors, repeat IHS-JVN imaging, or referral to an eye care provider, primary care provider, or appropriate specialty provider.
Table 2.
Content from IHS-JVN Grading Report, Two Example Patients
| IHS-JVN REPORT DOMAINS | EXAMPLE PATIENT 1 | EXAMPLE PATIENT 2 |
|---|---|---|
| Background | ||
| Includes: name, gender, date of birth, age, Imager name, referring physician and contact, date location, etc. | Not shown here. | Not shown here. |
| Medical risk factors for DR | ||
| Duration of diabetes | 22 years | 1 year |
| Last eye exam | Date not shown here—calculated as 2 years ago | Date not shown here—calculated as 2 years ago |
| Lab studies: | ||
| A1c | 11.3% | 12.7% |
| LDL | 150 mg/dL | 400 mg/dL |
| HDL | 57 mg/dL | 19 mg/dL |
| Total cholesterol | 238 mg/dL | 298 mg/dL |
| Blood pressure | 120/88 mm Hg | 143/89 mm Hg |
| Imaging results | ||
| Level of NPDR | Right eye: moderate; left eye: moderate | Right eye: unable to grade; left eye: unable to grade |
| Level of PDR | Right eye: no evidence; left eye: no evidence | Right eye: unable to grade; left eye: unable to grade |
| Level of DME | Right eye: no evidence; left eye: no evidence | Right eye: no evidence; left eye: unable to grade |
| Additional findings | Right eye: hypertensive retinopathy, central vein occlusion, cotton wool spots; left eye: hypertensive retinopathy, cotton wool spots | Right eye: other; left eye: other |
| Management plan guidance | ||
| Risk level | High | Medium |
| Summary | This patient's A1c is very high (>10%). Initiation of intensive glycemic control in a gradual manner is recommended to reduce the risk of development and progression of DR. Reducing A1c to <7.0% or as low as medically appropriate to this patient's particular circumstances is recommended over time. | This patient's A1c is very high (>10%). Initiation of intensive glycemic control in a gradual manner is recommended to reduce the risk of development and progression of DR. Reducing A1c to <7.0% or as low as medically appropriate to this patient's particular circumstances is recommended over time. |
| DR evident by JVN examination; see Imaging Results. Non-DR pathology evident by JVN exam; see Imaging Results. | Elevated blood pressure (≥130/80) has been shown to increase the risk of development and progression of DR as well as cotton wool spot formation. Optimization of blood pressure control is recommended as medically appropriate to this patient's particular circumstances. | |
| Refer to eye clinic: based on the earlier findings, we recommend follow-up with an optometrist/ophthalmologist for central retinal vein occlusion within 3 weeks and with PCP for hypertension/diabetes control and cardiovascular work-up. | Dyslipidemia: elevated lipids have been associated with the presence and severity of hard exudates and moderate vision loss in patients with diabetes. Optimization of lipids is recommended as medically appropriate to this patient's particular circumstances. | |
| Non-DR finding evident by JVN exam; see Imaging Results. | ||
| Refer to eye clinic: based on the earlier findings, we recommend follow-up with an optometrist/ophthalmologist within 3 months for comprehensive eye exam (DR evaluation and lipemia retinalis follow-up). Patient should continue follow-up with his primary care doctor regarding hypertriglyceridemia. | ||
This information was obtained from real IHS-JVN Reading Center reports and reformatted for this table. Background information is not shown to protect patient privacy.
HDL, high-density lipoprotein; LDL, low-density lipoprotein; IHS-JVN, Indian Health Service-Joslin Vision Network; PCP, primary care provider.
Training
Standardized training of Imagers and Readers and structured QA protocols are used to promote ongoing fidelity with the validation studies by both existing and newly added sites.
Imager training begins with home-based, self-paced pre-training on ocular anatomy, DR, and telemedicine fundamentals before reporting to PIMC for a 2- or 3-day syllabus on UWFI or NMFP technology, respectively. This training includes structured exposure to Reading Center administrative and reading activities to facilitate the Imager's ability to request an urgent reading for possible urgent or sight-threatening findings. Provisional Imager certification is conveyed based on demonstrated technical, clinical, and administrative proficiency. Full certification is conveyed after 6 months of experience and 100 IHS-JVN patient encounters demonstrating successful quality reviews. Full certification is maintained by ongoing successful quality reviews or by formal retraining and recertification.
Reader training is provided to optometrist applicants with recent clinical experience. Most applicants come from IHS health care facilities. Home-based, self-paced pre-training emphasizes DR pathophysiology and foundational clinical trials.17,30,31 This is followed by 3 days of Reader training at JDC (Boston). Provisional Reader certification is conveyed on demonstrated proficiency of: (1) application of ETDRS-based interpretation of JVN digital images (NMFP and UWFI) in native stereoscopic format, with and without post-imaging processing enhancement, as compared with reference ETDRS image sets; and (2) post-imaging processing and other reading tools, computer-assisted decision support, and standardized reporting. Full Reader certification is conveyed after 6 months of successful interpretation of the images and use of the technology as determined by senior Reading Center staff. Full certification is maintained by ongoing successful quality reviews, focused training stemming from structured peer review, or by formal retraining and recertification.
Quality Assurance
Ongoing QA is a requirement of accreditation regulations and the ATA DR practice guidelines. The IHS-JVN is carefully monitored end-to-end, with the outcome used for performance improvement as described by ATA recommendations.15,16 Imagers and Readers are assessed for volume, recency, and proficiency of administrative and clinical performance. Technical support quality is similarly assessed. The overall program is assessed through monitoring of Reading Center latency (routine and STAT reads), reading queue, hosting site productivity, and hosting site annual DR examination rate. QA reporting is used internally to guide staff and provider education, provider re-credentialing, and regulatory compliance.
Outcomes
Outcomes to measure success of the program include: (1) geographical adoption by IHS and Tribal programs thus far and clinical volume; (2) improved DR surveillance rate with an associated improvement in DR treatment rate; (3) cost-effectiveness compared with a conventional examination; (4) technology testing for improved clinical performance and operational efficiency; and (5) expansion of epidemiologic data on DR and DME in AI/AN.
Geographical adoption and clinical volume
IHS health care services are administered through 12 administrative area offices and the IHS-JVN is currently active in 11: Alaska; Albuquerque; Bemidji; Billings; Great Plains; Nashville; Navajo; Oklahoma; Phoenix; Portland; and Tucson.32 As of the final quarter of fiscal year 2019, the IHS-JVN program had 99 active sites, distributed across 23 states (Fig. 2). In fiscal year 2019, the IHS-JVN imaged 29,958 unique patients. Since the program was initiated, it has conducted 226,333 studies cumulatively. In the past 3 years, during which the program cumulatively imaged 62,091 patients, we estimate that the program served about 25% of the IHS user population with diabetes.
Fig. 2.
Location of all IHS-JVN sites active in fiscal year 2019.
Facility participation in the IHS-JVN program is optional for IHS and tribal facilities. Facilities apply to participate and the program evaluates their eligibility, taking into consideration the facility's number of patients with diabetes, their existing annual DR examination rate (GPRA), and the clinical, technical, and business ability of the facility to support ongoing operations of the IHS-JVN. As facilities apply, the program will continue to expand to serve more patients.
DR examination rate
A retrospective study of the annual (1999–2003) rates of DR examinations and follow-up laser treatment was conducted at PIMC, the site of the first IHS-JVN deployment in 2000. A nearby PIMC satellite clinic without the IHS-JVN was used for comparison.33 Although the annual DR examination rates at the comparison clinic remained stable over the period of study, ranging from 51% to 59%, PIMC's annual DR examination rate increased from 50% in 1999 to 75% in 2003. The rate of laser treatment for the satellite clinic was not reported, but there was a parallel 51% increase in laser treatment for DR at PIMC in the same population during the same period.
There has been a similar trend in the national GPRA reports. Specifically, the national rate of annual DR examinations increased from 49.0% to 61.3% during 2007–2015.34 This 25% increase in exam rates was due to both IHS-JVN exams and conventional eye exams. Because there was not a significant change in conventional eye examination capacity within the IHS in this period,35 we believe that the IHS-JVN contributed substantially to the rate change.
Cost-effectiveness
A modeled economic analysis found that the IHS-JVN was more cost-effective than a conventional dilated retinal examination in detecting proliferative DR (PDR) and identifying patients requiring intervention to prevent vision loss.36 Specifically, the analysis showed that the IHS-JVN would detect an additional 148 cases of PDR over conventional eye exams while lowering costs by $525,690. One hundred thirty-nine more patients would receive laser treatment for their PDR, at a cost savings of $195,210. Five fewer patients would develop severe vision loss while saving another $324,810.
Technology testing
The performance of UWFI was compared with NMFP in the IHS-JVN over a 1-year period and 25,635 patients.37 The UWFI resulted in more than an 80% decrease in the image ungradable rate, doubled the rate of diagnosed DR, identified a more severe rate of DR in 9% of patients, and prevented unnecessary referrals in more than 4,000 patients.
DR/DME epidemiology
Prior reports of DR prevalence in AI/AN were dated, and research on DME in AI/AN was lacking. Thus, the IHS-JVN analyzed retrospective data from 53,998 consecutive patients imaged nationally by the program between November 1, 2011 and October 31, 2016 to determine the prevalence of: levels of DR and DME; presence/absence of any DR; and presence/absence of sight-threatening retinopathy (STR), defined as severe NPDR, any PDR, or any DME.38 The analysis found any level of DR in 17.7% of patients and STR in 4.2% of patients. A subset analysis of the UWFI images (n = 16,535) found any level of DR in 28.2% of patients and STR in 5.4%. This latter finding suggests that the wider field of view and lower ungradable rate of UWFI particularly make it easier for Readers to see mild and moderate NPDR. That analysis was reported in the most comprehensive, peer-reviewed publication describing DR and DME prevalence and severity in AI/AN to date.38
Discussion
The IHS-JVN is a large, nationally distributed, primary care-based, teleophthalmology program for AI/AN that is validated at ATA Validation Category 3 for the remote diagnosis and management of DR/DME severity levels and certain non-DR disease. Because Category 3 programs are complex and costly to operate, they are reserved for use in specific circumstances.14 The IHS circumstances are such that referred specialty care may be limited. This makes the higher DR severity referral threshold, lower referral rate, and specific management plan reported to the primary care staff particularly important in the IHS. Cost-avoidance is also critical in the IHS due to lower per capita funding of health care for AI/AN than that of the general U.S. population.20,39 Improving the timeliness of DR examinations with the IHS-JVN decreases DR/DME complications and allows for less costly and more effective interventions.
Adoption of innovation can be challenging for organizations wishing to improve processes and outcomes.40 Although the value of teleophthalmology for DR has been established,41,42 the IHS has shown less rapid adoption of the IHS-JVN than anticipated. This is unexpected since the program funds all costs of the equipment needed, the Imager training, the Reading Center services, and ongoing technical support. Sites pay their Imager's salary, usually a fraction of a full-time equivalent, and provide space for the imaging encounters. Imager salary costs can potentially be offset if sites bill third party payers for the technical component of the telemedicine services. Based on the literature and anecdote, we speculate that clinical inertia,43,44 professional resistance,45 the threat of workflow disruption to the clinic,46 and competition for staffing/space (anecdote) are likely barriers to program adoption.
Looking ahead, a next step for the IHS-JVN program is to quantify its public health impact. As mentioned, the annual DR examination rate among IHS tribal facilities (as tracked by GPRA) has increased annually, in parallel with expansion of the IHS-JVN. This implies a favorable correlation between the two historical trends. But various administrative barriers have precluded retrospective statistical tests of this correlation. In addition, after 2015, changes in the data collection process of this DR GPRA element limit comparison of current and prior (pre-2015) examination rates. Prospectively examining the DR examination rate at existing and new IHS-JVN sites and counting which annual DR exams at these sites are from the program versus a conventional eye exam is needed. This would give administrators and providers guidance on how the IHS-JVN can help clinical performance, regulatory compliance, and utilization at existing sites and improve public health overall.
Recently, artificial intelligence has gained attention as a way to increase access to cost-effective screening for DR, particularly in low- and middle-income countries.47 However, existing artificial intelligence systems for diagnosing DR are not validated at ATA Category 3, nor has the performance of these systems been evaluated in AI/AN populations.48 For the IHS-JVN context, artificial intelligence is an opportunity for the program to enhance Reading Center performance, rather than replace manual grading and interpretation of retinal images. Specifically, the program plans to use artificial intelligence algorithms to triage patients with no or mild DR so that patients with more severe DR can be prioritized in the Readers' queue, shortening the reading latency for these cases.
Acknowledgments
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the Indian Health Service.
Disclosure Statement
S.J.F. is Vice President for Research, Estenda Solutions, Inc.; S.-E.B. is a scientific consultant for SocialEyes Corp., and sub-contractor for Estenda Solutions, Inc.; D.G.L. is President, Estenda Solutions, Inc.; D.C. and D.S. are federal employees of the IHS; and M.B.H. developed and directed the IHS-JVN as a federal employee of the IHS 2000–2017 and is now retired from federal service. The authors have no other disclosures to report.
Funding Information
Estenda Solutions, Inc., is subcontracted by the IHS Tele-retinal program to provide required infrastructure, technology, and research support. This work was supported under that subcontract, HHSI236201600002C.
References
- 1. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services, 2017 [Google Scholar]
- 2. McLaughlin S. Traditions and diabetes prevention: A healthy plan for Native Americans. Diabetes Spectr 2010;23:271–277 [Google Scholar]
- 3. Frank RN. Diabetic retinopathy. N Engl J Med 2004;50:48–58 [DOI] [PubMed] [Google Scholar]
- 4. Klein BW. Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol 2007;14:179–183 [DOI] [PubMed] [Google Scholar]
- 5. Better Health Partnership. NCQA/HEDIS measures of comprehensive care for diabetes and high blood pressure 2016. Available at www.betterhealthpartnership.org/hedis_2016.asp (last accessed September24, 2019).
- 6. Hartnett ME, Key IJ, Loyacano NM, Horswell RL, Desalvo KB. Perceived barriers to diabetic eye care: Qualitative study of patients and physicians. Arch Ophthalmol 2005;123:387–391 [DOI] [PubMed] [Google Scholar]
- 7. Bressler NM, Varma R, Doan QV, Gleeson M, Danese M, Bower JK, Selvin E, Dolan C, Fine J, Colman S, Turpcu A. Underuse of the health care system by persons with diabetes mellitus and diabetic macular edema in the United States. JAMA Ophthalmol 2014;132:168–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leese GP, Boyle P, Feng Z, Emslie-Smith A, Ellis JD. Screening uptake in a well-established diabetic retinopathy screening program: The role of geographical access and deprivation. Diabetes Care 2008;31:2131–2135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Joslin Diabetes Center. Joslin Vision Network (JVN). Available at https://www.joslin.org/joslin_vision_network.html (last accessed July3, 2019)
- 10. Cavallerano AA, Cavallerano JD, Katalinic P, Blake B, Rynne M, Conlin PR, Hock K, Tolson AM, Aiello LP, Aiello LM; Joslin Vision Network Research Team. A telemedicine program for diabetic retinopathy in a Veterans Affairs Medical Center—The Joslin Vision Network Eye Health Care Model. Am J Ophthalmol 2005;139:597–604 [DOI] [PubMed] [Google Scholar]
- 11. Cavallerano AA, Conlin PR. Teleretinal imaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol 2008;2:33–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hays H, Carroll M, Ferguson S, Fore C, Horton M. The success of telehealth care in the Indian Health Service. Virtual Mentor 2014;16:986–996 [DOI] [PubMed] [Google Scholar]
- 13. Carroll M, Cullen T, Ferguson S, Hogge N, Horton M, Kokesh J. Innovation in Indian healthcare: Using health information technology to achieve health equity for American Indian and Alaska Native populations. Perspect Health Inf Manag 2011;8:1d. [PMC free article] [PubMed] [Google Scholar]
- 14. Horton MB, Silva PS, Cavallerano JD, Aiello LP. Operational components of telemedicine programs for diabetic retinopathy. Curr Diab Rep 2016;16:128. [DOI] [PubMed] [Google Scholar]
- 15. Li HK, Horton M, Bursell SE, Cavallerano J, Zimmer-Galler I, Tennant M, Abramoff M, Chaum E, Debuc DC, Leonard-Martin T, Winchester M; American Telemedicine Association Diabetic Retinopathy Telehealth Practice Recommendations Working Group, Lawrence MG, Bauman W, Gardner WK, Hildebran L, Federman J. Telehealth practice recommendations for diabetic retinopathy, second edition. Telemed J E Health 2011;17:814–837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Horton MB, Brady CJ, Cavallerano J, Abramoff M, Barker G, Blodi B, Chiang M, Crockett C, Garg S, Karth P, Liu Y, Maloney K, Newman C, Rathi S, Rosenson A, Sheth V, Silva PS, Stebbins K, Zimmer-Galler I. Practice guidelines for ocular telehealth-diabetic retinopathy, 3rd edition. Telemed J E Health 2020;26:495–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—And extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology 1991;98:786–806 [PubMed] [Google Scholar]
- 18. Tozer K, Woodward MA, Newman-Casey PA. Telemedicine and diabetic retinopathy: Review of published screening programs. J Endocrinol Diabetes 2015;2, DOI: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Congressional Research Service. CRS Report R43330. The Indian Health Service: An overview. Available at https://www.everycrsreport.com/reports/R43330.html (last accessed August9, 2019)
- 20. Indian Health Service. IHS profile. Available at https://www.ihs.gov/newsroom/factsheets/ihsprofile/ (last accessed September24, 2019)
- 21. US Department of Agriculture, Economic Research Service. American Indians remain disproportionally rural. Available at https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=77893 (last accessed August9, 2019)
- 22. Chow SP, Aiello LM, Cavallerano JD, Katalinic P, Hock K, Tolson A, Kirby R, Bursell SE, Aiello LP. Comparison of nonmydriatic digital retinal imaging versus dilated ophthalmic examination for nondiabetic eye disease in persons with diabetes. Ophthalmology 2006;113:833–840 [DOI] [PubMed] [Google Scholar]
- 23. Silva PS, Cavallerano JD, Haddad NM, Tolls D, Thakore K, Patel B, Sehizadeh M, Tolson AM, Sun JK, Aiello LP. Comparison of nondiabetic retinal findings identified with nonmydriatic fundus photography vs ultrawide field imaging in an ocular telehealth program. JAMA Ophthalmol 2016;134:330–334 [DOI] [PubMed] [Google Scholar]
- 24. Indian Health Service. IHS clinical reporting system. Available at https://www.ihs.gov/crs/includes/themes/responsive2017/display_objects/documents/crsv18/GPRAMeasuresV180.pdf (last accessed August9, 2019)
- 25. Silva PS, Walia S, Cavallerano JD, Sun JK, Dunn C, Bursell SE, Aiello LM, Aiello LP. Comparison of low-light nonmydriatic digital imaging with 35-mm ETDRS seven-standard field stereo color fundus photographs and clinical examination. Telemed J E Health 2012;18:492–499 [DOI] [PubMed] [Google Scholar]
- 26. Silva PS, Cavallerano JD, Sun JK, Noble J, Aiello LM, Aiello LP. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol 2012;154:549–559 [DOI] [PubMed] [Google Scholar]
- 27. Silva PS, Cavallerano JD, Tolls D, Omar A, Thakore K, Patel B, Sehizahah M, Tolson AM, Sun JK, Aiello LM, Aiello LP. Potential efficiency benefits of nonmydriatic ultrawide field retinal imaging in an ocular telehealth diabetic retinopathy program. Diabetes Care 2014;37:50–55 [DOI] [PubMed] [Google Scholar]
- 28. Fonda S, Birkmire-Peters D, Bursell SE. Comprehensive Diabetes Management Program (CDMP). Proceedings of the 4th IASTED International Conference on Telehealth and Assistive Technologies, Baltimore, MD, 2008;168–173 [Google Scholar]
- 29. Early Treatment Diabetic Retinopathy Study Research Group. Early Treatment Diabetic Retinopathy Study design and baseline characteristics. ETDRS report number 7. Ophthalmology 1991;98:741–756 [DOI] [PubMed] [Google Scholar]
- 30. Nathan DM, for the DCCT/EDIC Research Group. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study at 30 years: Overview. Diabetes Care 2014;37:9–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. American Diabetes Association. Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care 2002;25:s28–s32 [DOI] [PubMed] [Google Scholar]
- 32. IHS. Regional offices. Available at https://www.ihs.gov/dhr/regionaloffices/ (last accessed July3, 2019)
- 33. Wilson C, Horton M, Cavallerano J, Aiello LM. Addition of primary care–based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diabetes Care 2005;28:318–322 [DOI] [PubMed] [Google Scholar]
- 34. Indian Health Service. GPRA and other national reporting. Available at https://www.ihs.gov/crs/gprareporting/ (last accessed September24, 2019)
- 35. United States Government Accountability Office. Indian Health Service: Actions needed to improve oversight of patient wait times. GAO-16-333. Washington, DC. Available at https://www.gao.gov/assets/680/676120.pdf (last accessed December18, 2019)
- 36. Whited JD, Datta SK, Aiello LM, Aiello LP, Cavallerano JD, Conlin PR, Horton MB, Vigersky RA, Poropatich RK, Challa P, Darkins AW, Bursell SE. A modeled economic analysis of a digital tele-ophthalmology system as used by three federal health care agencies for detecting proliferative diabetic retinopathy. Telemed J E Health 2005;11:641–651 [DOI] [PubMed] [Google Scholar]
- 37. Silva PS, Horton MB, Clary D, Lewis DG, Sun JK, Cavallerano JD, Aiello LP. Identification of diabetic retinopathy and ungradable image rate with ultrawide field imaging in a national teleophthalmology program. Ophthalmology 2016;123:1360–1367 [DOI] [PubMed] [Google Scholar]
- 38. Bursell SE, Fonda SJ, Lewis DG, Horton MB. Prevalence of diabetic retinopathy and diabetic macular edema in a primary care-based teleophthalmology program for American Indians and Alaskan Natives. PLoS One 2018;13:e0198551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Board on Health Care Services; Institute of Medicine. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Washington (DC): National Academies Press (US), 2012. 11, Experiences of the VA and IHS. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207133/ (last accessed December17, 2019) [PubMed] [Google Scholar]
- 40. Rogers EM. Diffusion of innovations, 5th ed. New York: Free Press, 2003 [Google Scholar]
- 41. Silva PS, Cavallerano JD, Aiello LM, Aiello LP. Telemedicine and diabetic retinopathy: Moving beyond retinal screening. Arch Ophthalmol 2011;129:236–242 [DOI] [PubMed] [Google Scholar]
- 42. Surendran TS, Raman R. Teleophthalmology in diabetic retinopathy. J Diabetes Sci Technol 2014;8:262–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ziemer DC, Miller CD, Rhee MK, Doyle JP, Watkins C, Cook CB, Gallina DL, El-Kebbi IM, Barnes CS, Dunbar VG, Branch WT Jr, Phillips LS. Clinical inertia contributes to poor diabetes control in a primary care setting. Diabetes Educ 2005;31:564–571 [DOI] [PubMed] [Google Scholar]
- 44. Faria C, Wenzel M, Lee KW, Coderre K, Nichols J, Belletti DA. A narrative review of clinical inertia: Focus on hypertension. J Am Soc Hypertens 2009;3:267–276 [DOI] [PubMed] [Google Scholar]
- 45. Tang RA, Ricur G. The benefits, challenges and future of telehealth in ophthalmic care. Expert Rev Ophthalmol 2013;8:331–335 [Google Scholar]
- 46. Choi WS, Park J, Choi JYB, Yang JS. Stakeholders' resistance to telemedicine with focus on physicians: Utilizing the Delphi technique. J Telemed Telecare 2019;25:378–385 [DOI] [PubMed] [Google Scholar]
- 47. Wong TY, Sabanayagam C. Strategies to tackle the global burden of diabetic retinopathy: From epidemiology to artificial intelligence. Ophthalmologica 2019;13:1–12 [DOI] [PubMed] [Google Scholar]
- 48. Ting DSW, Cheung CY, Lim G, Tan GSW, Quang ND, Gan A, Hamzah H, Garcia-Franco R, San Yeo IY, Lee SY, Wong EYM, Sabanayagam C, Baskaran M, Ibrahim F, Tan NC, Finkelstein EA, Lamoureux EL, Wong IY, Bressler NM, Sivaprasad S, Varma R, Jonas JB, He MG, Cheng CY, Cheung GCM, Aung T, Hsu W, Lee ML, Wong TY. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA 2017;318:2211–2223 [DOI] [PMC free article] [PubMed] [Google Scholar]



