Abstract
Few, scalable, evidence-based psychosocial interventions exist for adolescent and young adult cancer survivors (AYAs, 18–39 years old). Using an existing, facilitated, online synchronous chat group-plus-education model (OSG+E), we replaced their educational workbook with an AYA-created film to stimulate an age-specific, emotion-focused group discussion (OSG+V). This randomized proof-of-concept trial compared the two models' content suitability, group processes, and feasibility over 9 months in 34 male and female AYAs with a range of cancers. AYAs rated the OSG + V model more suitable, cohesive, and as having higher levels of important group processes than the OSG+E. A larger randomized trial is feasible for this AYA-appropriate, emotion-focused OSG + V model.
Keywords: psychosocial oncology, online synchronous groups, proof-of-concept, adolescents and young adults
Background
Adolescents and Young Adults (AYAs; defined as both diagnosed and currently between ages 18 and 39 at the time of the study) are a distinct oncology subpopulation at higher risk of psychosocial distress than either their cancer-free peers or older adults with cancer.1 AYAs value technology-facilitated interventions2 and highlight unique, psychosocial unmet needs that are directly related to their developmental life stage, such as peer support, discussing emotions, and age-appropriate information.2,3
However, few age-appropriate interventions addressing these unique AYA concerns have been created and trialed4 because of the relatively small and geographically dispersed population5 and the high prevalence of practical barriers to research participation.6 Therefore, to effectively meet AYA-specific psychosocial needs, an ideal intervention would have to be easily accessible, reach a wide geographic population, combine peer and professional support, and be tailored to AYA concerns.
The CancerChatCanada (CCC; cancerchatcanada.ca) professionally facilitated, online, synchronous chat groups (OSGs, real-time text-only conversations) met the first three of these criteria7; however, we hypothesized that we could improve this model by specifically stimulating emotional discussions using AYA narratives that addressed transitions, fear and uncertainty, isolation, relationships, identity, reflection, and reintegration. This new model could thereby provide compelling and relevant discussion content to stimulate greater sharing of unique, AYA psychosocial challenges with peers during OSG sessions. Specifically, this OSG + V model focused on sharing feelings and building connections (emotion focused).
Instead, the OSG + E model focused on teaching coping skills (psychoeducational) such as mindfulness, relaxation, ways of thinking, communication, problem solving, social support, sexuality, and healthy lifestyle. The OSG + V model could thus potentially improve the efficacy of OSGs for AYAs by cultivating supportive peer relationships: a primary AYA developmental life task.2
The emergence of narrative-based psychotherapy,8 making therapeutic use of stories, and the increased ease of creating and viewing video content have facilitated beneficial engagement with AYAs through digital stories shared by peers.9 To leverage video-based narratives, peer connections, and technology-facilitated interventions for AYAs, we modified the existing OSG + E model and developed a phase II, randomized proof-of-concept trial.10 This trial explores a new narrative-informed emotion-focused model using video as a discussion stimulus for chat sessions (OSG+V). Although there have been other online, AYA psychosocial interventions developed, to our knowledge, only one previous AYA study examined a professionally facilitated, synchronous chat group modality11 with promising results.
This brief report presents a summary of our modifications of the Stephen et al.11 model and proof-of-concept results (full thesis available12), examining whether an AYA-specific OSG + V model would be more effective compared with an OSG + E model for AYAs. This trial had two primary aims:
-
(1)
Proof of concept—To examine whether (a) AYA-specific video content could enhance therapeutic discussions (by comparing participants' reports of use and suitability of E and V content) and (b) AYAs would experience group processes that may enhance intervention effectiveness (through comparisons of group cohesion and valued group experiences).
-
(2)
Study design feasibility—To explore the feasibility of randomized trial design and procedures (through measures of recruitment and retention, attendance, usability, and satisfaction, including a power calculation for outcomes).
Methods
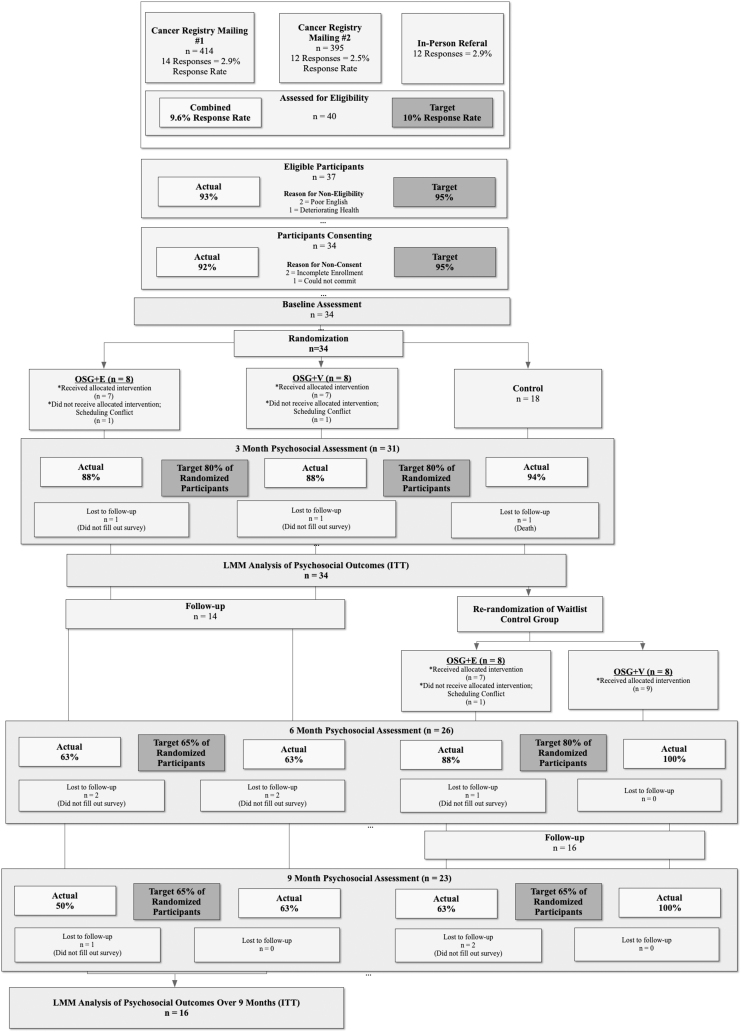
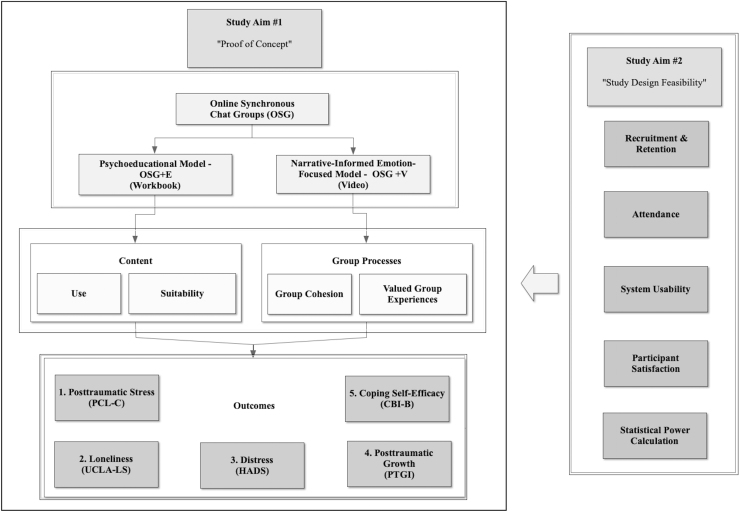
This exploratory trial used a three-arm randomized design, with crossover, to compare the two OSG models: a 10-week OSG + E model using a standard psychoeducational workbook12 versus the OSG + V model using clips from an AYA-created film, Wrong Way to Hope.13 CCC conducted all 90-minute OSG sessions with eight participants through their online platform using the same therapist. In-depth details of each intervention arm are provided in other articles.12 We randomized participants to the two treatment arms and a 10-week, treatment-as-usual, waitlist control group (Fig. 1). We collected psychosocial outcomes at four time points (baseline, 3, 6, and 9 months) and aggregated crossover groups with initial intervention groups for analysis of proof-of-concept and feasibility measures. We present the conceptual model used to organize the study aims in Figure 2.
FIG. 1.
CONSORT diagram with recruitment and retention targets. LMM, linear mixed model; ITT, intention-to-treat.
FIG. 2.
Conceptual model for the randomized proof-of-concept trial.
Study aim no. 1—proof-of-concept measures
Proof-of-concept measures focused on two primary areas: (1) intervention content and (2) group processes. Intervention content can impact participant outcomes.14 It was evaluated by participants reporting their use of the content each week (reading the workbook vs. watching the video) and postintervention, rating the overall suitability of the content to stimulate learning and discussion using a five-item Likert-type measure.
Group processes are the active ingredients in group psychotherapy15 and were measured using group cohesion16 and valued group experiences.17 Changes in group cohesion were measured using the Group Cohesiveness Scale18 (GCS; completed at weeks 1, 4, 7, and 9 across the 10-week intervention). Participants rated the cancer support group experiences they valued most by completing the Group Experience Questionnaire (GEQ; subscales: expressing true feelings, developing a new attitude, accessing information and advice, establishing supportive contact, and discussing sexual concerns) postintervention.17
Study aim no. 2—study design feasibility
The second study aim explored potential study protocol success using the following measures: (1) recruitment and retention, (2) attendance (intervention adherence), (3) participant satisfaction, and (4) system usability. We also included a power calculation to determine the appropriateness of outcome measures and estimate the required sample size.10 We based recruitment and retention targets (Fig. 2) on a similar published intervention19 and attendance targets on unpublished, CCC operational data (75% of the group attending each session). The recruitment and retention measures used the proportion of AYAs who were interested in the study, eligible to participate, consented to participate, and who completed the psychosocial outcome questionnaires (Fig. 2).
Attendance was assessed by reviewing attendance records and facilitator notes. Although participant satisfaction does not always correlate with psychosocial outcomes,20 it is an important feasibility measure to determine the likelihood of future participant recruitment, retention, and intervention adherence. Satisfaction was measured using a single, six-point Likert-type item immediately after the final chat group. We assessed the usability of the CCC online chat platform in conjunction with the OSG + E content and OSG + V content, using the System Usability Scale (SUS) delivered once, postintervention (passable SUS scores are >70).21
Finally, for the power calculation of the primary outcome measure, participants completed the PTSD Checklist–Civilian Version (PCL-C), with responses targeted to experiences with cancer. We used the pre/post (3-month) standard deviation (SD) in total score with a five-point change as the minimum threshold for response to treatment,22 a type I error level of 5%, and a power level of 80%. Additionally, we included other psychometrically validated tools to explore sensitivity to change over time (Fig. 2). There is disagreement around using proof-of-concept study data for power calculations in psycho-oncology intervention design23; however, a rough indication of sample size may provide some indication of study feasibility.
Due to this study's small sample size, tests of significance were inappropriate. Therefore, our analyses explored trajectories in psychosocial outcomes and assisted in characterizing participants' experiences for discussion. Data analysts used SPSS, v. 19 (2013), except for slope calculations for changes in the GCS, and linear mixed model (LMM) analysis of psychosocial outcome measures for power calculation using SAS Proc Mixed, v. 9.2 (2014).
Results
Table 1 presents demographic, medical, and psychosocial characteristics of the sample. No large differences in demographic characteristics between arms and study participants/nonparticipants appeared, indicating effective randomization and a representative sample. There was greater variance in several medical and psychosocial variables, which might be expected by chance.
Table 1.
Demographic, Medical, and Primary Outcome Characteristics of an Adolescent and Young Adult Sample (n = 34)
| Demographic | OSG + E (n = 8) | OSG + V (n = 8) | Control (n = 18) | Nonresponders (n = 383) |
|---|---|---|---|---|
| Age at baseline, mean, SD (range) | 34.5, 4.6 (27–39) | 28.9, 4.3 (23–35) | 29.8, 5.8 (21–39) | 32.0, 6.0 (18–39) |
| Female gender, n (%) | 6 (75.0) | 5 (62.5) | 12 (66.7) | 237 (61.9) |
| Married/partner, n (%) | 5 (62.5) | 3 (37.5) | 8 (44.4) | |
| Any postsecondary education, n (%) | 7 (87.5) | 8 (100) | 15 (83.3) | |
| Currently employed, n (%) | 2 (25.0) | 3 (37.5) | 9 (50) | |
| Geographic location—urban, n (%) | 6 (75.0) | 5 (62.5) | 11 (61.1) | |
| Medical | ||||
| Cancer type, n (%) | ||||
| Hematopoietic and reticuloendothelial systems | 2 (25.0) | 2 (25.0) | 9 (50.0) | 105 (27.4) |
| Breast | 3 (37.5) | 2 (25.0) | 3 (16.7) | 119 (31.1) |
| Melanoma | 0 | 1 (12.5) | 1 (5.6) | 13 (3.4) |
| Eye, brain, and other CNS | 2 (25.0) | 2 (25.0) | 2 (11.1) | 21 (5.5) |
| Male/female genital organs | 0 | 1 (12.5) | 2 (11.1) | 45 (11.7) |
| Digestive organs | 1 (12.5) | 0 | 1 (5.6) | 34 (8.9) |
| Bones and connective tissue | 0 | 0 | 0 | 23 (6.0) |
| Head and neck | 0 | 0 | 0 | 8 (2.1) |
| Thyroid and endocrine glands | 0 | 0 | 0 | 5 (1.3) |
| Other | 0 | 0 | 0 | 10 (2.6) |
| Metastatic (yes), n (%) | 4 (50.0) | 2 (25.0) | 5 (32.4) | |
| Current treatment status (yes), n (%) | 6 (75.0) | 4 (50.0) | 11 (61.1) | |
| Initial diag. to baseline (months), median (Q1–Q3) | 21.5 (2.3–38.3) | 7.5 (4.0–11.3) | 8.0 (5.0–17.0) | |
| Primary outcomes at baseline (mean, SD, 95% CI) | ||||
| 1. PCL-C (trauma) | 38.0, 13.9 (26.4–49.7) | 36.0, 9.5 (28.1–43.9) | 39.1, 13.9 (32.2–46.0) | |
| 2. UCLA-LS (loneliness) | 53.9, 7.0 (48.0–59.8) | 55.0, 4.6 (51.2–58.8) | 56.6, 3.7 (54.8–58.5) | |
| 3. HADS (distress) | 10.8, 6.2 (5.6–15.9) | 12, 6.6 (6.5–17.5) | 12.1, 7.1 (8.6–15.6) | |
| 4. CBI-B (self-efficacy) | 87.9, 10.1 (79.4–96.4) | 78.8, 18.3 (63.5–94.1) | 81.9, 13.2 (73.4–88.0) | |
| 5. PTGI (post-traumatic growth) | 75.9, 17.7 (61.1–90.7) | 73.7, 23.6 (53.9–93.3) | 60.3, 24.4 (48.1–72.4) | |
CI, confidence interval; OSG, online synchronous chat group; SD, standard deviation.
Study aim no. 1—proof-of-concept results
Overall, participants engaged with both OSG + E content and OSG + V content. The mean percentage of participants in the OSG + E arm who read the workbook before the chat group was 76.5% (range = 66.7%–91.7%), with 20.6% (range = 14.3%–33.3%) reading the chapter during the session. The mean percentage of participants in the OSG + V arm who viewed the video before the chat group was 88.2% (range = 75.0%–100.0%), with 11.8% (range = 7.7%–25.0%) viewing the video during the session.
Suitability for learning and discussion differed significantly between models (n = 20, Mann–Whitney U = 78.5, p = 0.029), with the video content deemed more suitable (OSG + E median = 2.9, interquartile range [IQR] = 2.35; OSG + V median = 4.1, IQR = 2.40). Both models appeared to increase group cohesiveness across the 10-week trajectory (OSG+E: slope = 0.66, SD = 2.87; OSG+V: slope = 1.66, SD = 3.49); however, OSG + V reported a greater increase in group cohesion (pre/post change score; 19.89, SD = 41.9) compared with OSG + E (7.92, SD = 34.4), with a moderate effect size (d = −0.31).
Overall, the distribution of valued group experiences was different between models, with participants in the OSG + E group endorsing all GEQ subscales at a lower level (median range = 1.00–3.39) compared with the OSG + V group (median range = 3.0–4.25). Two subscales were statistically different, with OSG + V participants rating Expressing True Feelings (n = 20, U = 86.5, p = 0.004) and Developing a New Attitude (n = 20, U = 77.5, p = 0.035) as more important aspects of their chat group experience.
Study aim no. 2—study design feasibility results
The modified CONSORT diagram provides a detailed description of the recruitment and retention results (Fig. 2). In all cases, except the 9-month follow-up of the initial OSG + E group, recruitment and retention percentages were within 5% of the target value. Each participant attended on average 6 (SD = 3, range = 0–10) weekly chat group sessions throughout the 10-week intervention, with an average of 5 AYAs (SD = 1, range = 3–8) participating. Categorically, 56% attended 7–10 sessions, 27% attended 3–6 sessions, and 17% attended 2 or less. OSG + V groups had stronger attendance overall, with 60% of participants attending 7 or more sessions compared with 53% for OSG+E; however, in neither model was the average weekly attendance target met (75% or 6 of 8 participants in attendance).
Overall, participant satisfaction did not differ significantly between models (n = 20, U = 42.0, p = 0.451), with 70% strongly agreeing, 25% agreeing, and 5% slightly agreeing with the statement that they were satisfied with their chat group experience. The overall mean SUS score was 88.0 (SD = 9.7, range = 0–100, higher value = higher ease of use) with no significant differences between models, and an estimated sample size of 90 participants (∼30 in each of the three study arms) would be necessary to find a significant difference in pre/post-PCL-C outcomes between models.
Discussion
We found that this study design is feasible for a larger RCT, with some modifications, having met most recruitment, retention, attendance, and participant satisfaction targets. The high participant satisfaction across models could lead to better retention regardless of intervention allocation. We also found that the OSG platform and both models' resources were usable and that participants rated the OSG + V content as more suitable than the standard OSG + E content.
This preliminary study may offer some guidance for future psycho-oncology group interventions targeting AYA-specific issues at a socioemotional level. Participants found the video content more suitable for their needs than the standard workbook. For many AYAs, differentiating and naming their emotions can be a difficult task2 and a peer-created video may help facilitate the process of entering their own story and naming their emotions by allowing them to directly reference the videos in weekly chat group discussions.8
Furthermore, the significantly higher group cohesion and endorsement of valued group experiences highlights another potential mechanism in the OSG + V model that could improve professionally facilitated OSGs for AYAs. Group cohesion is one of the most consistent and important precipitating factors in positive group psychotherapy outcomes as a feeling of belonging encourages greater openness, authenticity, and emotional expression within the group.17 AYAs with cancer are looking for meaningful peer interactions and support24 and therefore enhancing a sense of connection and belongingness could be considered a primary therapeutic objective. The emotion-focused, OSG + V intervention arm appeared to minimize the profound sense of isolation felt during a cancer experience by facilitating this sense of belonging and validated reports by others that it is possible to foster group cohesion in an online setting.25
Furthermore, participants in the OSG + V model endorsed one valued group experience specifically relevant to AYA psychosocial support, Expressing True Feelings, at a significantly higher level. AYAs report difficulty expressing true feelings to their friends and family and often reference the relief they experience when connecting with their cancer survivor peers.7 Continual refinement of psychosocial interventions so that they create a better environment for AYAs to share authentically with each other is an important future direction in AYA psycho-oncology.
This small pilot study had limitations such as small sample size, lower than expected weekly OSG attendance, and lower than expected 9-month follow-up. However, overall, it did meet most feasibility targets and provides modest proof-of-concept support for a larger trial of OSG + V with AYAs. Viewing personal video narratives as a main active ingredient in group psychotherapy with AYAs is a departure from the dominant psychoeducational model used in cancer care. In the AYA context, providing patient stories through videos may be of greater value than providing educational materials about coping skills. Future studies could use a wide variety of digital storytelling tools to stimulate discussion, foster a sense of belonging, and convey information more effectively.
Acknowledgments
Researchers obtained ethics approval from the Conjoint Health Research Ethics Board (REB13–0482) at the University of Calgary and were included under the CCC ethics approval through the BCCA Research Ethics Board at the University of British Columbia. The study was completed as Michael Lang's MSc thesis research and this article contains portions of the original text that is archived at the University of Calgary.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Funding for Michael Lang's Masters program was provided by the Western Regional Training Centre for Health Services Research and the Psychosocial Oncology Research Training (PORT) program at McGill University. Funding for Dr. Giese-Davis was provided by Alberta Cancer Research Institute (ACRI) Recruitment and Retention Grants #4739 and #24397, the Enbridge Research Chair in Psychosocial Oncology, and the Alberta Cancer Foundation.
References
- 1. Lang MJ, Giese-Davis J, Patton SB, Campbell DJT. Does age matter? Comparing post-treatment psychosocial outcomes in young adult and older adult cancer survivors with their cancer-free peers. Psychooncology. 2018;27(5):1404–11 [DOI] [PubMed] [Google Scholar]
- 2. Docherty SL, Kayle M, Maslow GR, Santacroce SJ. The adolescent and young adult with cancer: a developmental life course perspective. Sem Onc Nurs. 2015;31(3):186–96 [DOI] [PubMed] [Google Scholar]
- 3. Zebrack BJ, Block R, Hayes-Lattin B, et al. . Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer. 2013;119(1):201–14 [DOI] [PubMed] [Google Scholar]
- 4. Richter D, Koehler M, Friedrich M, et al. . Psychosocial interventions for adolescents and young adult cancer patients: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2015;95(3):370–86 [DOI] [PubMed] [Google Scholar]
- 5. Tonorezos ES, Oeffinger KC. Research challenges in adolescent and young adult cancer survivor research. Cancer. 2011;117(S10):2295–300 [DOI] [PubMed] [Google Scholar]
- 6. Rabin C, Simpson N, Morrow K, Pinto B. Behavioral and psychosocial program needs of young adult cancer survivors. Qual Health Res. 2011;21(6):796–806 [DOI] [PubMed] [Google Scholar]
- 7. Stephen J, MacGregor K, McLeod D, et al. . Evaluation of CancerChatCanada: a program of online support for Canadians affected by cancer. Curr Oncol. 2013;20:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Angus LE, Greenberg LS Working with narrative in emotion-focused therapy: changing stories, healing lives. American Psychological Association; 2011 [Google Scholar]
- 9. Laing CM, Moules NJ, Estefan A, Lang MJ. Stories that heal: understanding the effects of creating digital stories with pediatric and adolescent/young adult oncology patients. J Pediatr Oncol Nurs. 2017;34(4):272–82 [DOI] [PubMed] [Google Scholar]
- 10. Czajkowski SM, Powell LH, Adler N, et al. . From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015;34(10):971–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stephen J, Rojubally A, Linden W, et al. . Online support groups for young women with breast cancer: a proof-of-concept study. Support Care Cancer. 2017;25(7):2285–96 [DOI] [PubMed] [Google Scholar]
- 12. Lang MJ. Speaking their language: a randomized pilot study of synchronous online chat groups for young adults with cancer [master's thesis]. Calgary, AB: University of Calgary; 2015. p. 159 [Google Scholar]
- 13. Lang MJ, Bryant A Wrong Way to Hope: An Inspiring Story of Young Adults and Cancer [film]. 2010. [Cited 2020 June 24]. Available from: https://youtu.be/uzh9H-wBKeV
- 14. Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–12 [DOI] [PubMed] [Google Scholar]
- 15. Yalom ID. The theory and practice of group psychotherapy. New York: Basic Books; 1970 [Google Scholar]
- 16. Burlingame GM, McClendon DT, Alonso J. Cohesion in group therapy. Psychotherapy. 2011;48(1):34–42 [DOI] [PubMed] [Google Scholar]
- 17. Giese-Davis J, Brandelli Y, Kronenwetter C, et al. . Illustrating the multi-faceted dimensions of group therapy and support for cancer patients. Healthcare (Basel). 2016;4(3):E48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wongpakaran T, Wongpakaran N, Intachote-Sakamoto R, Boripuntakul T. The group cohesiveness scale (GCS) for psychiatric inpatients. Perspect Psychiatr Care. 2013;49(1):58–64 [DOI] [PubMed] [Google Scholar]
- 19. Zernicke KA, Campbell TS, Speca MP, et al. . A randomized wait-list controlled trial of feasibility and efficacy of an online mindfulness-based cancer recovery program: the eTherapy for cancer applying mindfulness trial. Psychosom Med. 2014;76(4):257–67 [DOI] [PubMed] [Google Scholar]
- 20. Andersen BL, Shelby RA, Golden-Kreutz DM. RCT of a psychological intervention for patients with cancer: mechanisms of change. J Consult Clin Psychol. 2007;75(6):927–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Hum Comput Int. 2008;24(6):574–94 [Google Scholar]
- 22. Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety. 2011;28(7):596–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kraemer H, Mintz J, Noda A, et al. . Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–9 [DOI] [PubMed] [Google Scholar]
- 24. Zebrack BJ. Psychological, social, and behavioral issues for young adults with cancer. Cancer. 2011;117(S10):2289–2294 [DOI] [PubMed] [Google Scholar]
- 25. McGill BC, Sansom-Daly UM, Wakefield CE, et al. . Therapeutic alliance and group cohesion in an online support program for adolescent and young adult cancer survivors: lessons from “Recapture Life.” J Adolesc Young Adult Oncol. 2017;6(4):568–72 [DOI] [PubMed] [Google Scholar]