Abstract
Background: In neonatal respiratory distress syndrome, breathing support and surfactant therapy are commonly used to enable the alveoli to expand. Surfactants are typically delivered through liquid instillation. However, liquid instillation does not specifically target the small airways. We have developed an excipient enhanced growth (EEG) powder aerosol formulation using Survanta®.
Methods: EEG Survanta powder aerosol was delivered using a novel dry powder inhaler via tracheal insufflation to surfactant depleted rats at nominal doses of 3, 5, 10, and 20 mg of powder containing 0.61, 0.97, 1.73, and 3.46 mg of phospholipids (PL), whereas liquid Survanta was delivered via syringe instillation at doses of 2 and 4 mL/kg containing 18.6 and 34 mg of PL. Ventilation mechanics were measured before and after depletion, and after treatment. We hypothesized that EEG Survanta powder aerosol would improve lung mechanics compared with instilled liquid Survanta in surfactant depleted rats.
Results and Conclusion: EEG Survanta powder aerosol at a dose of 0.61 mg PL significantly improved lung compliance and elastance compared with the liquid Survanta at a dose of 18.6 mg, which represents improved primary efficacy of the aerosol at a 30-fold lower dose of PL. There was no significant difference in white blood cell count of the lavage from the EEG Survanta group compared with liquid Survanta. These results provide an in vivo proof-of-concept for EEG Survanta powder aerosol as a promising method of surfactant replacement therapy.
Keywords: compliance, EEG Survanta powder aerosol, elastance, inflammation, resistance, surfactant depletion, ventilation mechanics
Introduction
The main function of the lungs is to facilitate gas exchange between the capillary blood and the alveoli sacs. To accomplish this function, the lungs have a large surface area. Lining the alveoli at the air to liquid interface is a complex surfactant mixture consisting of phospholipids (PL) and proteins that lower the surface tension, thereby increasing the compliance of the lungs during respiration.(1) The surfactant PL are mainly composed of dipalmitoylphosphatidylcholine (DPPC), which functions to reduce surface tension and four surfactant associated proteins (SP-A, SP-B, SP-C, and SP-D) that regulate surfactant function.(2) Together, the PL and proteins ensure the stability of the alveoli and allow for alveolar expansion and diffusional transport across the alveolar interface.(3) Deficiency of surfactant due to the immaturity of the lungs in premature infants or disruption of surfactant composition due to surfactant protein gene mutations can lead to respiratory distress syndrome (RDS).(4,5)
Premature infants are prone to RDS as surfactant production does not mature until the last weeks of gestation.(6) RDS accounts for about 20% of all neonatal deaths(7) and 50%–70% of death in premature infants(8) (about 1.1 million premature infant die each year(9)). Numerous therapies used in the treatment of RDS include breathing support and surfactant replacement therapy that enable the alveoli to expand and prevent their collapse.(10) Surfactant replacements include Alveofact®, Curosurf®, and Survanta®.(11) Treatments are delivered by instillation of the liquid(12) in volumes ranging from 2 to 8 mL/kg of body weight to reach the distal airways. However, adding more fluid to an already distressed lung may complicate the injury by hindering gas exchange and causing inflammation.(13) Administering these drugs as an aerosol is an alternative method that could deliver functional lipids and proteins to the distal airways to effectively replace the deficient surfactant.(14) However, efficiently delivering sufficient aerosolized medication to the lungs of infants using conventional inhalers and nebulizer has proven challenging.(3)
High-efficiency aerosol drug delivery using excipient enhanced growth (EEG) methods have been recently described.(15) This technology was employed to produce a dry powder aerosol formulation of EEG Survanta.(16) The EEG Survanta formulation consists of micrometer-sized combination particles containing Survanta, mannitol (which acts as a hygroscopic excipient), and leucine (dry powder dispersion enhancer) prepared by spray drying. Powder aerosols are formed by dispersing the particles using a new low-dispersion-air-volume dry powder inhaler.
In the EEG aerosol delivery method, a relatively small aerosol with a mass median aerodynamic diameter (MMAD) approximately ≤1.5 μm is initially created through a combination of high-efficiency aerosolization and a highly dispersible spray-dried formulation.(17,18) The small aerosol size enables low upper airway loss and efficient penetration to the lower regions of the lungs.(19) However, at this small aerosol size, a majority of the particles would typically not deposit and be exhaled,(20) especially with the quick respiration cycle of infants and test animals. A novel component of EEG delivery that enables hygroscopic growth is inclusion of mannitol or another hygroscopic excipient, which absorbs water vapor in the warm and humid respiratory airways rapidly increasing the size of the aerosol(21) as it travels to the deep lung and may foster enhanced deposition.(19,22)
To study the efficacy of surfactant therapies, surfactant depletion (SD) animal models have been used previously.(23,24) Successive lavage of the alveoli with warm saline solution is used for SD followed by delivery of the surfactant replacement therapies. In this study, we have used a modified SD model to evaluate the efficacy of delivering EEG Survanta powder aerosols in Sprague Dawley rats. We hypothesized that EEG Survanta powder aerosol would improve lung mechanics compared with instilled liquid Survanta in surfactant depleted rats.
Materials and Methods
Novel dry powder inhaler
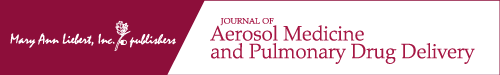
The custom dry powder inhaler device (Fig. 1) was created using Autodesk Inventor and exported as .STL files to be prototyped. The files were then prepared using Objet Studio preparation software and were built using an in-house Stratasys Objet24 3D Printer (Stratasys Ltd., Eden Prairie, MN) using VeroWhitePlus material at a 32 μm resolution. Support material was cleaned away from the model material using a Stratasys waterjet and the devices were allowed to fully dry before use. The capillaries used in the dry powder inhaler (DPI) were custom cut from lengths of stainless steel (SAE 304) capillary tubing and epoxy was used to secure them in place. An o-ring was used to seal the two halves of the device to prevent leaks. A Luer-lock style connection was used to seal the device to both the air syringe and the blunt needle used as the tracheostomy tube. Powder aerosol was delivered from the device using a 5 mL actuation air volume.
FIG. 1.
Custom dry powder inhaler device used for EEG Survanta® delivery. EEG, excipient enhanced growth.
The aerosolization device separates into two parts with a twisting motion and powder is directly loaded into the powder chamber. Hand actuation of the 10 mL syringe supplies the necessary air volume to aerosolize the powder and deliver the aerosol into the rat lungs. Within the aerosolization device, the inlet capillaries form three high-velocity air jets that enter the powder chamber. These air jets initially fluidize the powder and then break apart the aggregates through particle interactions with turbulent eddies.(25) The aerosol is then carried through the outlet hollow capillary and to the trachea of the rat. Further description of the air-jet aerosolization concept and the effects of turbulence can be found in our previous work.(26,27) The custom novel dry powder inhaler used in this study was developed by Virginia Commonwealth University (VCU) College of Engineering(28,29) for aerosolizing surfactant powders with low air volumes (3–10 mL). Aerosolization testing with surfactant powder indicated that emitted dose remains proportional to loaded dose through a fill mass of 10 mg.(28,29) However, optimal aerosolization of the powder occurs at a 3 mg powder mass (producing the smallest MMAD) and aerosolization efficiency decreases with larger fill masses (producing larger MMADs).(28,29) It is well known that smaller MMAD values will better penetrate the upper airways and thereby reach the deep lung at higher efficiencies.
EEG formulation
Survanta EEG spray-dried powders were prepared from dispersions containing Survanta, mannitol, and leucine in a ratio of 45:33:22% w/w in a 5% ethanol in water mixture with a solid concentration of 0.125% w/v. Powders were spray dried using the Büchi Nano Spray Dryer B-90 HP (Büchi Labortechnik AG, Flawil, Switzerland). Spray drying parameters were as follows: 70°C inlet temperature (outlet temperatures of 37°C–41°C), pump speed of 3%, spray intensity of 80%, and a gas inlet flow of 120 L/min (drying chamber pressure of 40–42 mbar). Powders were collected from the electrostatic particle collector into vials and stored in a desiccator at 2°C–4°C when not in use. For the deposition visualization study, 0.5% w/w of Texas Red® dye (1,2-dihexadecanoyl-sn-glycero-3-phosphoethanolamine, triethylammonium salt; Texas Red DHPE; ThermoFisher Scientific, Waltham, MA) was added to the spray drying dispersion to enable labeling of the PL powder aerosol.
Powder formulation particle size characterization
The primary particle size of the spray-dried powder was determined using a laser diffraction method with a Sympatec ASPIROS dry dispersing unit and HELOS laser diffraction sensor (Sympatec GmbH, Clausthal-Zellerfeld, Germany). A pressure drop of 4.5 bar was used to disperse a small amount of powder for analysis.
Animal use
Sprague Dawley rats were purchased from Hilltop Laboratory (Scottdale, PA) and were housed at VCU vivarium. The protocol was approved by the VCU Institutional Animal Care and Use Committee (IACUC), and all procedures were performed according to their guidelines.
In vivo imaging system imaging
To qualitatively assess the deposition of the EEG Survanta powder aerosol in the lungs, SD was performed as described in the Depletion and Lung Mechanics section; surfactant depleted rats were then treated with 10 mg of EEG powder aerosol labeled with Texas Red dye as described in the treatment methods followed by 10 minutes of mechanical ventilation. At the end of the mechanical ventilation, the lungs were isolated and imaged using an in vivo imaging system (IVIS) spectrum from VCU Cancer Mouse Models Core to determine the local distribution of aerosol. The IVIS spectrum uses two-dimensional (2D) and three-dimensional (3D) optical tomography to show 2D- and 3D-like structure of the location of the fluorescent dye in the lung.
Depletion and lung mechanics
The rats (0.3–0.5 kg) were anesthetized with 60 mg/kg of sodium pentobarbital (Sigma, St. Louis, MO) with 50% redosing when necessary. To assess the condition of the rats at baseline, initial lung mechanics were measured as healthy controls. Lungs mechanics were measured using a FlexiVent FX4 system and FlexiWare software (Scireq, Montreal, Canada). The perturbations performed included deep inflation for alveolar recruitment and Snapshot 150 for mechanics of the respiratory system. FlexiWare then used Snapshot 150 to fit the data onto a single compartment math model to determine the lung mechanics of resistance (resistance assesses how constricted the lungs are to airflow), elastance (elastance is the elastic property of the lungs or the ease of the lungs to return to their original state after inflation), and compliance (compliance measures the ease of the respiratory system to stretch and expand). In the SD group, warmed phosphate-buffered saline (PBS; 10 mL/kg) was perfused and quickly withdrawn from the lungs via the trachea and repeated once. Lung mechanics were normalized to individual rats. The SD mechanics were determined by normalizing to the healthy lung mechanics before depletion for each rat. Finally, the lung mechanics for each treatment (liquid Survanta and EEG Survanta) were determined by dividing mechanics taken following treatment of the surfactant depleted rats by the healthy ventilation mechanics of each rat taken at baseline.
Treatments
Following depletion and ventilation mechanics measurements, the animals were taken off the mechanical ventilator to allow spontaneous breathing and were treated with EEG Survanta powder or liquid Survanta. Treatment arms consisted of liquid instillation of Survanta (Abbvie, North Chicago, IL) at doses of 2 and 4 mL/kg (18.6 and 34 mg PL, respectively). Dry powder aerosol delivery of EEG Survanta powder at nominal loaded doses of 3, 5, 10, and 20 mg (0.61, 0.97, 1.73, and 3.46 mg PL, respectively; Table 1) was accomplished via the novel dry powder inhaler. Liquid treatments were administered via a syringe connected to a tracheal cannula, whereas aerosol treatments were loaded into the dry powder inhaler and were administered via a syringe connected to the dry powder inhaler (Fig. 1) and connected to a tracheal cannula. The inhaler was actuated using 5 mL of air delivered from a syringe connected to the inhaler. For the 20 mg dose, two inhalers were used each containing 10 mg of EEG Survanta. In separate studies, the delivered mass of powder emitted from the DPI was determined by measuring the weight of the inhaler before and after actuation. The mass of PL delivered was calculated from the measured DPPC content of the EEG Survanta powder. The DPPC content was determined by a validated liquid chromatography-mass spectrometry (LC-MS) method.
Table 1.
Administered Doses of Survanta and Aerosol Excipient Enhanced Growth Survanta
| Administration method | Dose of Survanta®or EEG Survanta | Aerosol emitted dose (%) | PL dose (mg) |
|---|---|---|---|
| Instillation | 0.75 (0.1) mL | NA | 18.6 (2.6) |
| Instillation | 1.36 (0.1) mL | NA | 34.0 (2.0) |
| Aerosol | 3.05 (0.03) mg | 73.7 (9.3) | 0.61 (0.08) |
| Aerosol | 5.02 (0.04) mg | 71.4 (6.6) | 0.97 (0.09) |
| Aerosol | 10.04 (0.04) mg | 63.6 (6.3) | 1.73 (0.17) |
| Aerosol | 20.08 mga | NA | 3.46a |
Liquid and EEG Survanta aerosol doses are represented as mean and standard deviation (in parentheses) of loaded doses where applicable with their corresponding delivery percentage and PL content, n = 5–7.
Calculated as 2 × 10.04 mg dose.
EEG, excipient enhanced growth; PL, phospholipid.
Mechanical ventilation
Treatments were followed by injection of a paralytic agent pancuronium bromide (MP Biomedicals, Santa Ana, CA) at 1 mg/kg to prevent spontaneous breathing, and mechanical ventilation of the rats at 8 mL/kg, 90 bpm, and 3 cm H2O positive end-expiratory pressure was performed. Lung mechanics were recorded after 10 minutes of ventilation. Five rats were used for liquid Survanta and 10 mg dose treatments groups each, whereas three rats each were used for other EEG Survanta groups.
Bronchoalveolar lavage
Bronchoalveolar lavage (BAL) was performed as described before with minor modification and adapted for rats.(30) Briefly, at the end of mechanical ventilation, the rats were euthanized via the snipping of the inferior vena cava. A gravity-assisted lavage was then performed by letting PBS flow into the lungs until full inflation and raising the rats to recover the fluid with no repeat. The BAL fluid (BALF) was then recovered for downstream processing.
BALF cytology
BALF cytology was performed as previously described with minor modifications.(30) Staining of the microscope slides was performed with a 3 Diff-Quik solutions staining kit. Neutrophil, monocyte, and lymphocyte counts were then accessed by microscopy to assess inflammation.
Histology
Lungs were fixed with a gravity-assisted flow of 4% paraformaldehyde in the lungs via the trachea at the end of each procedure. Fixed lungs were dehydrated using increasing percentages of ethanol, after being placed in running tap water for 45 minutes, fixed lungs were placed in 50% ethanol overnight, then 70%, 80%, 90%, 95%, and 100% ethanol for 30 minutes each with a repeat of 100% followed by 30 minutes submersion in xylene. The lung tissues were then embedded into paraffin cassettes and 20 μm slices were made with a microtome and transferred onto microscope slides. The slides were then rehydrated and stained with hematoxylin and eosin (H&E) stain. An Olympus microscope was then used to take color images of the slides with a 10 × objective.
Statistics
The power analysis was estimated based on our previous work in this model. Different treatment groups were compared by analysis of variance, followed by post hoc Tukey's multiple comparison test. GraphPad Prism 6 was used for statistical analyses. p-Values <0.05 were considered significant and ≥3 replicates were performed for each experiment. The data were normally distributed.
Results
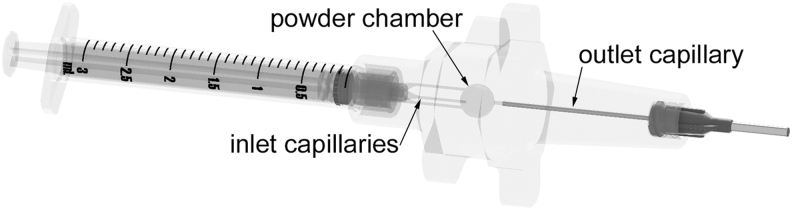
Powder formulation particle size characterization
EEG Survanta powder aerosols from different spray-dried batches used in this study were found to be monodisperse with an overall mean ± standard deviation geometric diameter of 1.0 ± 0.04 μm at 4.5 bar dispersion pressure (Fig. 2). This resulted in coefficients of variation of <6% across the 10 batches, indicating good reproducibility of the spray drying process.
FIG. 2.
Particle size characterization of EEG Survanta revealing significant fraction of particle <1.5 μm. Cumulative distribution percentage of particles less than the size reported on the y-axis. Density distribution shows the frequency of particles at each size reported on the x-axis. Error bars are standard deviation with n = 3.
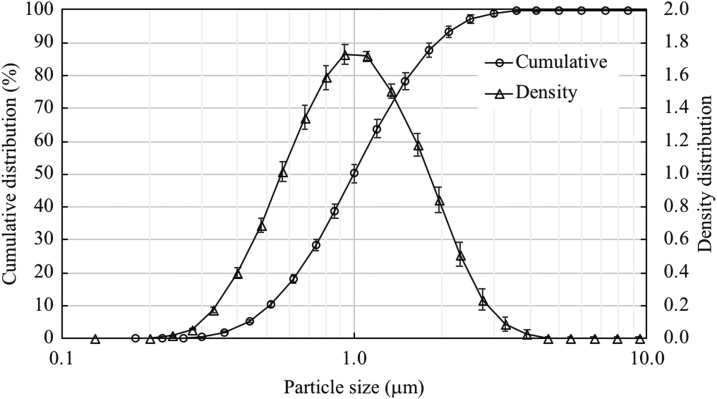
Particle deposition
Figure 3 shows fluorescent IVIS images of the whole lung following deposition of the Texas Red-labeled EEG Survanta powder aerosol. The distribution of the aerosol appears to be throughout almost the entire lung compared with control, which did not receive the fluorescent dye (Fig. 3A). Moreover, the image mixing, which appears as a 3D-like structure, shows that the red fluorescent dye has reached the deep lung region (Fig. 3B).
FIG. 3.
Fluorescent images of EEG powder deposition (10 mg). (A) Fluorescence image for control and EEG Survanta powder-labeled aerosol and (B) 3D overlay of the fluorescence with light image mixed for control and EEG Survanta powder-labeled aerosol. Image mixing shows Quasi-complete deposition of EEG Survanta in the distal lung. 3D, three-dimensional. Color images are available online.
Compliance
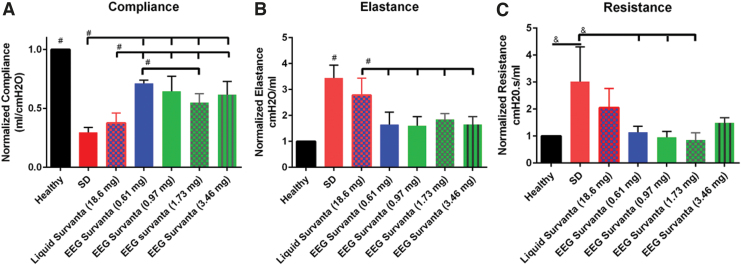
There was a significant decrease in the normalized compliance following SD compared with the healthy control. Figure 4 shows the normalized compliance values for the SD groups compared with the treatment groups. Each of the aerosol EEG-Survanta treatment groups had significant increases in compliance compared with the SD group. There was no significant difference in compliance between the SD and liquid Survanta groups. Dosing with 0.61 mg PL in the EEG Survanta aerosol group produced the most improved compliance and was significantly greater than the SD and liquid Survanta groups (Fig. 4A). Each of the aerosol doses administered produced significantly greater compliance following treatment compared with the 18.6 mg PL liquid instillation. Importantly, this improved compliance was observed at PL doses that were ∼10-fold lower compared with the liquid dosing. Within the aerosol EEG Survanta groups, an effect of administered dose was observed with a significant difference between dosing with 0.61 mg PL compared with 1.73 mg PL. There were no other differences between the 0.61 mg PL dose and the other aerosol EEG Survanta doses (0.97 mg of PL and 3.46 mg PL).
FIG. 4.
Compliance, elastance, and resistance measurements for rats before and after treatments of 0.61, 0.97, 1.73, and 3.46 mg PL (3, 5, 10, and 20 mg EEG Survanta) and 2 mL/kg of liquid Survanta (18.6 mg PL). (A) Compliance: compliance of groups receiving EEG Survanta of 1.73 mg PL was higher than the compliance of groups receiving liquid Survanta treatment at 18.6 mg PL; EEG Survanta treatment of 0.61 mg PL had the highest compliance of all treatments. (B) Elastance: elastance for all EEG Survanta group was significantly lower than elastance of liquid Survanta. SD group had significantly higher elastance than other groups. (C) Resistance: no significant difference between the EEG Survanta group and liquid Survanta, although the trend of EEG Survanta was lower than liquid Survanta and closer to the healthy state. Bar graphs are mean ± standard deviation. #p < 0.05; &p < 0.01. n ≥ 3. PL, phospholipids; SD, surfactant depletion. Color images are available online.
Elastance
There was a significant increase in the normalized elastance following SD. Figure 4B shows a significant difference between the groups that were treated with EEG Survanta aerosol compared with the group that received liquid Survanta as treatment with the EEG Survanta group having a better elastance (Fig. 4B). These results were confirmed with all the EEG Survanta groups being not statistically different from the healthy group, whereas the group that received liquid Survanta as treatment was significantly different from the healthy group. Moreover, there was no difference between the liquid Survanta as treatment and the SD group while all EEG treatment groups were statistically different from the SD group. Finally, there was a significant difference between the healthy and the SD group elastance. These results show the efficacy of the EEG Survanta at effectively improving elastance.
Resistance
The only groups that were statistically different from each other were the healthy and SD, SD and 1.73 mg of PL EEG Survanta, SD and 0.97 mg of PL EEG Survanta, SD and 0.61 mg of PL EEG Survanta (Fig. 4C). Although there was not any significant statistical difference between the healthy, liquid, and EEG Survanta, the groups that received EEG Survanta at different doses had a closer resistance to the healthy group compared with the ones that received liquid Survanta as treatment. The trend also shows a similar resistance among all EEG Survanta cases at different doses. Additionally, there was no significant difference between the SD group and the group that received liquid Survanta as treatment. Although we did not record any statistical difference in change of resistance between the two main treatment groups, EEG Survanta treatments at all dose levels appear to be better options in terms of reducing resistance than liquid Survanta.
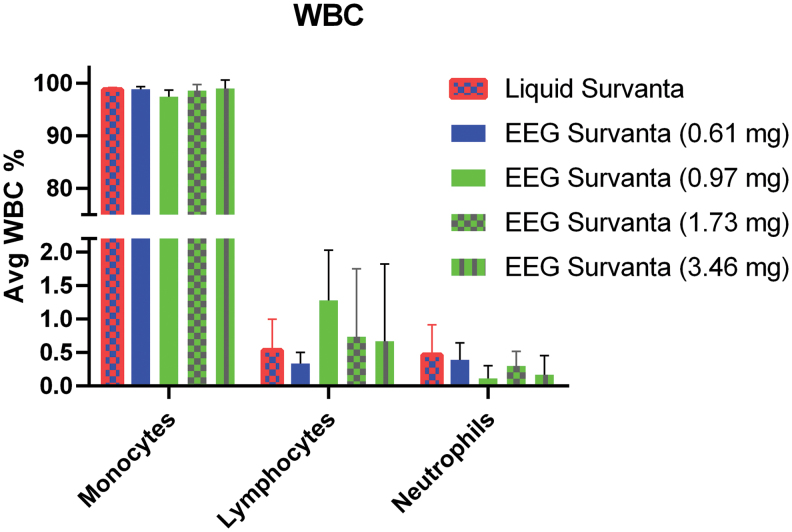
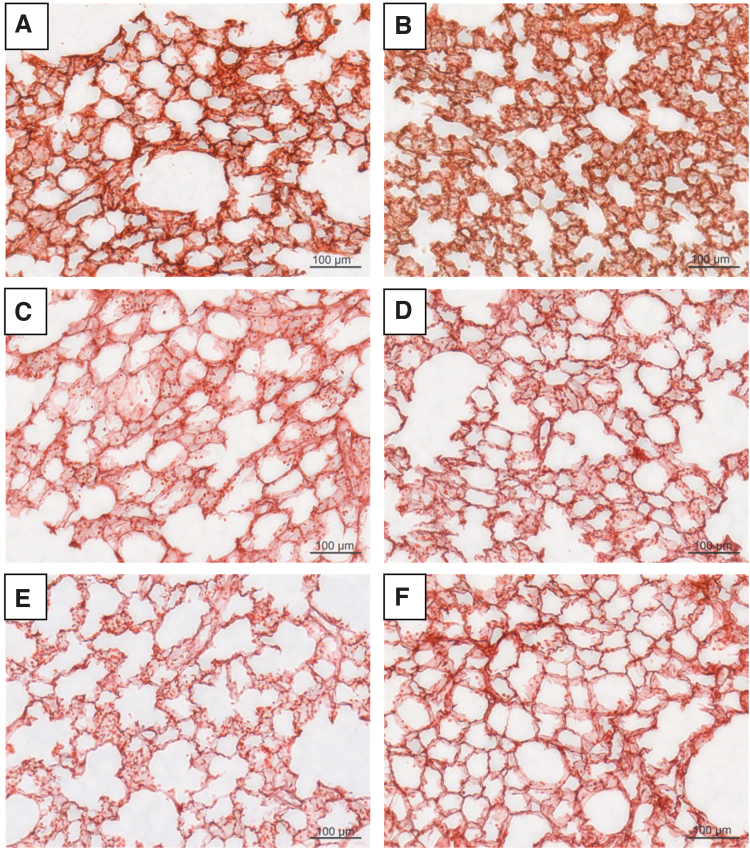
Inflammatory assessment
White blood cells (WBC) were counted in lavages obtained from different experimental groups. We specifically counted monocytes, lymphocytes, and neutrophils. There were similar percentages of monocytes (97%–99%) per 300 WBC count in cytospin slides of rats that received liquid Survanta and rats that received EEG Survanta. The same trend was observed when assessing the lymphocytes level. There was no statistically significant difference in the number of lymphocytes among any of the groups. Finally, the neutrophil count, which is characteristic of acute inflammation in the lungs, did not significantly change among all experimental groups (Fig. 5). Moreover, H&E stain yielded no visible signs of inflammation (Fig. 6), although the group receiving liquid Survanta showed signs of alveoli collapse (Fig. 6B).
FIG. 5.
Percent neutrophils, monocytes, and lymphocytes obtained per 300 WBC count of cytospin slides. No significant difference in all groups for all treatments. Bar graphs are mean ± standard deviation. n ≥ 4. WBC, white blood cell. Color images are available online.
FIG. 6.
Hematoxylin and eosin staining of (A) control rat with no treatment and no SD, (B) 18.6 mg PL liquid Survanta treatment, (C) 0.61 mg PL EEG Survanta, (D) 0.97 mg PL EEG Survanta, (E) 1.73 mg PL EEG Survanta treatment, and (F) 3.46 mg PL EEG Survanta showing no clear signs of neutrophils influx (i.e., inflammation), although liquid Survanta treatment group (B) shows signs of structural alveoli collapse. Color images are available online.
Discussion
This study has characterized the efficacy of a spray-dried powder aerosol formulation of Survanta. The spray-dried powder contained mannitol and leucine in addition to commercially available Survanta liquid and disperses into micrometer size particles upon aerosolization with a MMAD in the range of 1.0 μm. The small particle size allows for high-efficiency aerosol delivery to the lungs and enables the aerosol to reach the distal airways. Size increase during flight from the hygroscopic excipient helps target the site of deposition and prevents exhalation of the aerosol. A new aerosolization device, originally developed by Boc et al.(16,28,29) using an air-jet concept,(26,27) was used that is capable of efficient lung delivery to a small animal model using only 5 mL of air. The study implemented a new rat lung SD model to compare the efficacy of liquid bolus surfactant instillation at a clinically implemented rate of 2 mL/kg of surfactant versus different doses of the surfactant EEG aerosol. The standard of care instillation method delivered a significantly higher dose of PL (18.6 mg) than the aerosol approach, which delivered a range of PL doses between 0.61 and 1.73 mg. Overall, the aerosolization approach significantly improved lung mechanics better than the standard-of-care liquid instillation. Little difference in lung mechanics was observed among the aerosol surfactant doses making the 0.61 mg dose the preferred dose in this model. The aerosolized surfactant formulation significantly improved lung mechanics compared with the standard-of-care liquid formulation and delivery approach at a PL dose (0.61 mg) that was a factor of 30-fold lower than with instillation.
Surfactant is composed of PL (mainly DPPC) and proteins, and this functions to reduce surface tension between the air and liquid interface in the alveoli.(31) The absence of surfactant is the underlying cause of RDS in premature neonates. To remedy RDS, surfactant replacement is available in both synthetic and natural formulations. Survanta is primarily a naturally derived surfactant product that is formulated from minced porcine lungs with added DPPC(32) and is widely used in the treatment of RDS.(11) Survanta is administered by instillation as a liquid(33) in volumes of up to 7 mL/kg, which adds to the fluid burden already present in the alveolar space due to RDS and may not be efficiently distributed to the peripheral lung during instillation.
As an alternative to liquid instillation, a powder aerosol formulation of Survanta has been developed for high-efficiency lung delivery using the EEG approach.(15) For this method, excipients have been formulated with Survanta and spray dried into a powder containing micrometer-sized particles for inhalation. The EEG formulation contains mannitol as a hygroscopic excipient, which functions to absorb water during transit through the airways, turning the particles into droplets with increasing mass. This engineered size increase during flight can be controlled to target the region of deposition and prevent the exhalation of the aerosol, which is a significant problem when delivering small particles to infant airways. Leucine was used as a dry powder dispersion enhancer to facilitate aerosolization of the spray-dried particles.
Lung mechanics, especially the compliance of all animals receiving EEG Survanta aerosol, were significantly improved compared to animals that received liquid Survanta containing 18.6 mg of PL. Initial studies using 4 mL/kg of liquid Survanta, the clinically suggested dose in premature infants, resulted in the death of the animals during the post-dose mechanical ventilation. This was probably due to excess fluid in the alveoli that hindered the ability of the rats to effectively perform gas exchange. Subsequent control studies with liquid Survanta were performed at the 2 mL/kg dose level. We believe that this result confirms that liquid bolus instillation of surfactant, which is the current Food and Drug Administration-approved method for all surfactant replacement therapies, may be in need of significant improvement and that aerosol delivery may be an effective alternative.
An important component of this study relates to the amount of PL that is delivered with each approach. The liquid surfactant formulation of 2 mL/kg contained 18.6 mg of PL, whereas the EEG aerosol doses contained 0.61–3.46 mg of PL. The aerosol formulations delivered 5- to 30-fold less PL than the liquid formulation. Surprisingly, even with this significantly reduced dose of PL, the liquid surfactant was significantly better at improving lung mechanics than the liquid formulation. We theorize that this improved response at a lower administered dose is because of a combination of (1) improved targeting of PL dose to the alveolar region with the aerosol and (2) the absence of the large liquid bolus and associated negative impacts on lung mechanics.
Of the aerosolized surfactant doses, the lowest dose of 0.61 mg was as effective as the higher dose levels. This is surprising because the response to surfactants is expected to be dose-dependent. The limited response to the escalated aerosol dose may be due to two reasons. First, the 0.61 mg of PL may be sufficiently high to restore lung mechanics as much as possible in the selected model. A dose–response relationship may be seen if lower doses are considered instead of higher. Second, we have observed that the aerosolization device is most efficient, producing the smallest MMAD, with lower mass loadings of ∼3 mg of powder.(16,28,29) Increasing the loaded mass in the range of 5–10 mg increases the MMAD size, thereby limiting the amount of aerosol delivered to the distal airways. This limitation will require an improved design of the aerosol generation device for small animal experiments. However, for infants, this problem may be more easily overcome as delivered air volumes are increased beyond what can be administered to a rat, which improves aerosolization of higher mass powders. For example, a reasonable tidal volume for a 1600 g infant is ∼10 mL.(34) Our group has recently developed several inline DPIs that can effectively aerosolize 10 mg and higher doses of EEG powder with 10 mL of air-producing aerosols with MMADs in the range of 1.5 μm.(26,27,35)
Liquid surfactant has also been used in the form of a nebulized solution to treat surfactant deficiency or lack of surfactant in preterm infants; however, those studies remain inconclusive due to the difficulty of getting the nebulized drug to the airways.(14,36) Berggren et al.(36) observed no benefit in nebulized surfactant delivered to spontaneously breathing newborns with RDS despite the fact that 480 mg of surfactant was administered in each case. Potential reasons for the lack of response were cited as poor lung delivery efficiency, estimated to be <1% of the administered dose, and very long delivery times, on the order of hours. One recently published study (under evaluation in Phase II clinical trial) observed an equivalent response in terms of lung mechanics of rabbits that received nebulized poractant alfa (brand name Curosurf) at 200 and 400 mg/kg to the ones that were treated with instilled surfactant at 200 mg/kg.(37) These results indicate that potential advantages of EEG powder as surfactant replacement need to be investigated further to unlock its full potential in the clinic.
Limitations
While the results of this study were promising, there were some limitations. As described above, the emitted aerosol size changes with the mass of loaded dose. Therefore, drug dose delivered to the lungs is not necessarily consistent with the loaded drug mass. Furthermore, it is currently not certain which powder mass formulation delivered the most PL mass to the alveolar region. The current washout model is different from experiments with preterm animal models that are naturally surfactant deficient. Rey-Santano et al.(38) considered both acute and sustained effects of surfactant delivery to premature lambs with RDS. While the preterm model may be more realistic, there is currently no evidence to prove that preterm animal models better predict efficacy in human neonates with RDS compared with SD models. In all animal models, the airway structure is significantly different from that of humans. The next recommended step is the application of the developed therapy in a larger animal closer to the size of a preterm infant, as with a ferret or rabbit model. Finally, we were not able to measure arterial partial pressure of oxygen (PaO2) to confirm a drop in PaO2 as some surfactant depleted methods have done in the past.(23) However, we observed a substantial decreased in compliance in the SD groups compared with the healthy group similar to RDS disease characteristic.(39)
Conclusion
We demonstrated that an EEG Survanta formulation can be effectively aerosolized with 5 mL of air and delivered to a rat SD model in a way that benefits lung mechanics. The SD model was sensitive to different deliver approaches (instillation vs. aerosolization) and dosages of surfactant. Aerosol delivery significantly improved lung mechanics compared with no treatment in surfactant depleted rats. Aerosol delivery improved lung mechanics better than a 30-fold higher dose of PL administered through liquid bolus, which is the current standard-of-care method for administering surfactants to humans. Of the aerosol doses administered, there was little change in the lung mechanics, which may imply that the administered dose may be reduced below the lowest considered dose of 0.61 mg PL. Histology highlighted that liquid delivery resulted in some alveolar collapse, whereas this was not observed with aerosol delivery. Finally, none of the treatments caused observable inflammation in the lungs. While these results are promising, longer studies need to be performed to evaluate the potential for side effects of the EEG powder delivery technique.
Acknowledgment
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
Virginia Commonwealth University is currently pursuing patent protection of devices and methods described in this study, which, if licensed and commercialized, may provide a future financial interest to the authors.
Funding Information
This work was supported by the National Institutes of Health grant R01HL139673. Services and products in support of the research project spray-dried by the Virginia Commonwealth University Cancer Mouse Models Core Laboratory, supported, in part, with funding from NIH-NCI Cancer Center Support Grant P30 CA016059.
Reviewed by:
Qi (Tony) Zhou
Robert DiBlasi
References
- 1. Sardesai S, Biniwale M, Wertheimer F, Garingo A, and Ramanathan R: Evolution of surfactant therapy for respiratory distress syndrome: Past, present, and future. Pediatr Res. 2017;81:240–248 [DOI] [PubMed] [Google Scholar]
- 2. Glasser JR, and Mallampalli RK: Surfactant and its role in the pathobiology of pulmonary infection. Microbes Infect. 2012;14:17–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andersson JM, Grey C, Larsson M, Ferreira TM, and Sparr E: Effect of cholesterol on the molecular structure and transitions in a clinical-grade lung surfactant extract. Proc Natl Acad Sci U S A. 2017;114:E3592–E3601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ricci F, Catozzi C, Murgia X, Rosa B, Amidani D, Lorenzini L, Bianco F, Rivetti C, Catinella S, Villetti G, Civelli M, Pioselli B, Dani C, and Salomone F: Physiological, biochemical, and biophysical characterization of the lung-lavaged spontaneously-breathing rabbit as a model for respiratory distress syndrome. PLoS One. 2017;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tsitoura M-EI, Stavrou EF, Maraziotis IA, Sarafidis K, Athanassiadou A, and Dimitriou G: Surfactant protein A and B gene polymorphisms and risk of respiratory distress syndrome in late-preterm neonates. PLoS One. 2016;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pérez-Gil J: Structure of pulmonary surfactant membranes and films: The role of proteins and lipid–protein interactions. Biochim Biophys Acta. 2008;1778:1676–1695 [DOI] [PubMed] [Google Scholar]
- 7. Lu H, Li W, Shao G, and Wang H: Expression of SP-C and Ki67 in lungs of preterm infants dying from respiratory distress syndrome. Eur J Histochem. 2012;56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang C, and Zhu X: Clinical effects of pulmonary surfactant in combination with nasal continuous positive airway pressure therapy on neonatal respiratory distress syndrome. Pak J Med Sci. 2017;33:621–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kinney MV, Lawn JE, Howson CP, and Belizan J: 15 Million preterm births annually: What has changed this year? Reprod Health. 2012;9:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sankar MJ, Gupta N, Jain K, Agarwal R, and Paul VK: Efficacy and safety of surfactant replacement therapy for preterm neonates with respiratory distress syndrome in low- and middle-income countries: A systematic review. J Perinatol. 2016;36(Suppl 1):S36–S48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mussavi M, Mirnia K, and Asadollahi K: Comparison of the efficacy of three natural surfactants (Curosurf, Survanta, and Alveofact) in the treatment of respiratory distress syndrome among neonates: A randomized controlled trial. Iran J Pediatr. 2016;26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moen A, Yu X-Q, Almaas R, Curstedt T, and Saugstad OD: Acute effects on systemic circulation after intratracheal instillation of Curosurf or Survanta in surfactant-depleted newborn piglets. Acta Paediatr. 1998;87:297–303 [DOI] [PubMed] [Google Scholar]
- 13. Ruppert C, Kuchenbuch T, Boensch M, Schmidt S, Mathes U, Hillebrand V, Henneke I, Markart P, Reiss I, Schermuly RT, Seeger W, and Günther A: Dry powder aerosolization of a recombinant surfactant protein-C–based surfactant for inhalative treatment of the acutely inflamed lung. Crit Care Med. 2010;38:1584–1591 [DOI] [PubMed] [Google Scholar]
- 14. Willson DF: Aerosolized surfactants, anti-inflammatory drugs, and analgesics. Respir Care. 2015;60:774–793 [DOI] [PubMed] [Google Scholar]
- 15. Longest PW, and Hindle M: Numerical model to characterize the size increase of combination drug and hygroscopic excipient nanoparticle aerosols. Aerosol Sci Technol. 2011;45:884–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Boc S: Aerosolized surfactants: Formulation development and evaluation of aerosol drug delivery to the lungs of infants. Theses Dissertation. 2018. Virginia Commonwealth University, Richmond, VA, USA [Google Scholar]
- 17. Son Y-J, Longest PW, and Hindle M: Aerosolization characteristics of dry powder inhaler formulations for the excipient enhanced growth (EEG) application: Effect of spray drying process conditions on aerosol performance. Int J Pharm. 2013;443:137–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Son Y-J, Longest PW, Tian G, and Hindle M: Evaluation and modification of commercial dry powder inhalers for the aerosolization of a submicrometer excipient enhanced growth (EEG) formulation. Eur J Pharm. 2013;49:390–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tian G, Longest PW, Li X, and Hindle M: Targeting aerosol deposition to and within the lung airways using excipient enhanced growth. J Aerosol Med Pulm Drug Deliv. 2013;26:248–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kim CS: Deposition of aerosol particles in human lungs: In vivo measurement and modeling. Biomarkers. 2009;14(Suppl 1):54–58 [DOI] [PubMed] [Google Scholar]
- 21. Hindle M, and Longest PW: Condensational growth of combination drug-excipient submicrometer particles for targeted high efficiency pulmonary delivery: Evaluation of formulation and delivery device. J Pharm Pharmacol. 2012;64:1254–1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Longest PW, and Tian G: Development of a new technique for the efficient delivery of aerosolized medications to infants on mechanical ventilation. Pharm Res. 2015;32:321–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ricci F, Casiraghi C, Storti M, D'Alò F, Catozzi C, Ciccimarra R, Ravanetti F, Cacchioli A, Villetti G, Civelli M, Murgia X, Carnielli V, and Salomone F: Surfactant replacement therapy in combination with different non-invasive ventilation techniques in spontaneously-breathing, surfactant-depleted adult rabbits. PLoS One. 2018;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Russ M, Kronfeldt S, Boemke W, Busch T, Francis RCE, and Pickerodt PA: Lavage-induced surfactant depletion in pigs as a model of the acute respiratory distress syndrome (ARDS). J Vis Exp. 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Longest PW, Son Y-J, Holbrook L, and Hindle M: Aerodynamic factors responsible for the deaggregation of carrier-free drug powders to form micrometer and submicrometer aerosols. Pharm Res. 2013;30:1608–1627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Longest W, and Farkas D: Development of a new inhaler for high-efficiency dispersion of spray-dried powders using computational fluid dynamics (CFD) modeling. AAPS J. 2019;21:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Longest W, Farkas D, Bass K, and Hindle M: Use of computational fluid dynamics (CFD) dispersion parameters in the development of a new DPI actuated with low air volumes. Pharm Res. 2019;36:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Boc ST, Farkas DR, Longest PW, and Hindle M: Spray dried pulmonary surfactant powder formulations: Development and characterization. Respir Drug Deliv. 2018;2:635–638 [Google Scholar]
- 29. Boc ST, Farkas DR, Longest PW, and Hindle M: Aerosolization of spray dried pulmonary surfactant powder using a novel low air volume actuated dry powder inhaler. Respir Drug Deliv. 2018;2:639–642 [Google Scholar]
- 30. Herbert JA, Valentine MS, Saravanan N, Schneck MB, Pidaparti R, Fowler AA, Reynolds AM, and Heise RL: Conservative fluid management prevents age-associated ventilator induced mortality. Exp Gerontol. 2016;81:101–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nkadi PO, Merritt TA, and Pillers D-AM: An overview of pulmonary surfactant in the neonate: Genetics, metabolism, and the role of surfactant in health and disease. Mol Genet Metab. 2009;97:95–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ma CC-H, and Ma S: The role of surfactant in respiratory distress syndrome. Open Respir Med J. 2012;6:44–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bloom BT, and Clark RH: Comparison of Infasurf (calfactant) and Survanta (beractant) in the prevention and treatment of respiratory distress syndrome. Pediatrics. 2005;116:392–399 [DOI] [PubMed] [Google Scholar]
- 34. Walsh BK, and Diblasi RM: Mechanical ventilation of the neonate and pediatric patient. In: BK Walsh, MP Czervinske, and RM DiBlasi, (eds). Perinatal and Pediatric Respiratory Care. Saunders Elsevier, St. Louis; pp. 325–347, 2010 [Google Scholar]
- 35. Farkas D, Hindle M, and Longest PW: Development of an inline dry powder inhaler that requires low air volume. J Aerosol Med Pulm Drug Deliv. 2018;31:255–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Berggren E, Liljedahl M, Winbladh B, Andreasson B, Curstedt T, Robertson B, and Schollin J: Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Paediatr. 2000;89:460–464 [DOI] [PubMed] [Google Scholar]
- 37. Bianco F, Ricci F, Catozzi C, Murgia X, Schlun M, Bucholski A, Hetzer U, Bonelli S, Lombardini M, Pasini E, Nutini M, Pertile M, Minocchieri S, Simonato M, Rosa B, Pieraccini G, Moneti G, Lorenzini L, Catinella S, Villetti G, Civelli M, Pioselli B, Cogo P, Carnielli V, Dani C, and Salomone F: From bench to bedside: In vitro and in vivo evaluation of a neonate-focused nebulized surfactant delivery strategy. Respir Res. 2019;20:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rey-Santano C, Mielgo VE, Andres L, Ruiz-del-Yerro E, Valls-i-Soler A, and Murgia X: Acute and sustained effects of aerosolized vs. bolus surfactant therapy in premature lambs with respiratory distress syndrome. Pediatr Res. 2013;73:639–646 [DOI] [PubMed] [Google Scholar]
- 39. Caminita F, van der Merwe M, Hance B, Krishnan R, Miller S, Buddington K, and Buddington RK: A preterm pig model of lung immaturity and spontaneous infant respiratory distress syndrome. Am J Physiol Lung Cell Mol Physiol. 2014;308:L118–L129 [DOI] [PubMed] [Google Scholar]