Abstract
Objective
To report pregnancy outcomes and disease activity (DA) in women with MS, neuromyelitis optica spectrum disorders (NMOSDs), and other neuroimmunologic diseases (ONID) after treatment with rituximab (RTX)/ocrelizumab (OCR) 12 months before or during pregnancy.
Methods
Data were collected in the German MS and pregnancy registry and centers from the Neuromyelitis Optica Study Group. Sixty-eight known outcomes of 88 pregnancies from 81 women (64 MS, 10 NMOSD, and 7 ONID) were included and stratified in 3 exposure groups: >6M-group = RTX/OCR >6 but ≤12 months before the last menstrual period (LMP) (n = 8); <6M group = RTX/OCR <6 months before the LMP (n = 47); preg group = RTX/OCR after the LMP (n = 13).
Results
Pregnancy outcomes were similar between groups, but significantly more preterm births (9.8% vs 45%) occurred after exposure during pregnancy. Overall, 2 major congenital abnormalities (3.3%), both in the preg group, were observed. Three women had severe infections during pregnancy. All women with MS (35) and 12/13 women with NMOSD, RTX/OCR exposure before the LMP and known pregnancy outcomes after gestational week 22 were relapse free during pregnancy. Five of 29 (17.2%) women with relapsing-remitting MS (RRMS) and 1 of 12 (8.3%) with NMOSD and at least 6 months postpartum follow-up experienced a relapse postpartum. Duration of RTX/OCR and early retreatment but not detection of B-cells were possible predictors for postpartum relapses in patients with RRMS/NMOSD.
Conclusions
Although RTX/OCR might be an interesting option for women with RRMS/NMOSD who plan to become pregnant to control DA, more data on pregnancy outcomes and rare risks are needed.
Only limited (<200) data on pregnancy outcomes after anti-CD20 monoclonal antibodies (mAbs) exposure—mainly focusing on rituximab (RTX)—in women with neuroimmunologic diseases have been published.1–3 Because of the fear of potential fetal B-cell depletion, the label is conservative and recommends to discontinue anti-CD20 mAbs at least 6 (US Food and Drug Administration) to 12 months (European Medicine Agency) before planned conception.
With the introduction of highly effective disease-modifying therapies (DMTs), women with relapsing-remitting MS (RRMS) or neuromyelitis optica spectrum disorders (NMOSDs) might consider pregnancy after stabilization of active disease courses,4–6 but reoccurrence or even rebound of disease activity (DA) has been reported in patients with MS after discontinuation of DMTs such as natalizumab and fingolimod.7–12 Thus, women may be confronted weighing the risk of relapses against potential risks of fetal DMT exposure.13 In NMOSD, relapses during pregnancy and postpartum have been reported, particularly in patients who stopped immunosuppressive therapy, and maintenance of immunotherapy has been discussed.14,15 Anti-CD20 mAbs could be an interesting option as in contrast to other drugs, no rebound has been reported so far.2,16
Therefore, the objective of this cohort study was to investigate the safety of RTX/ocrelizumab (OCR) during the last 12 months before or during pregnancy in women with neuroimmunologic diseases and to assess DA in a subcohort of women with RRMS or NMOSDs.
Methods
Participants and data collection
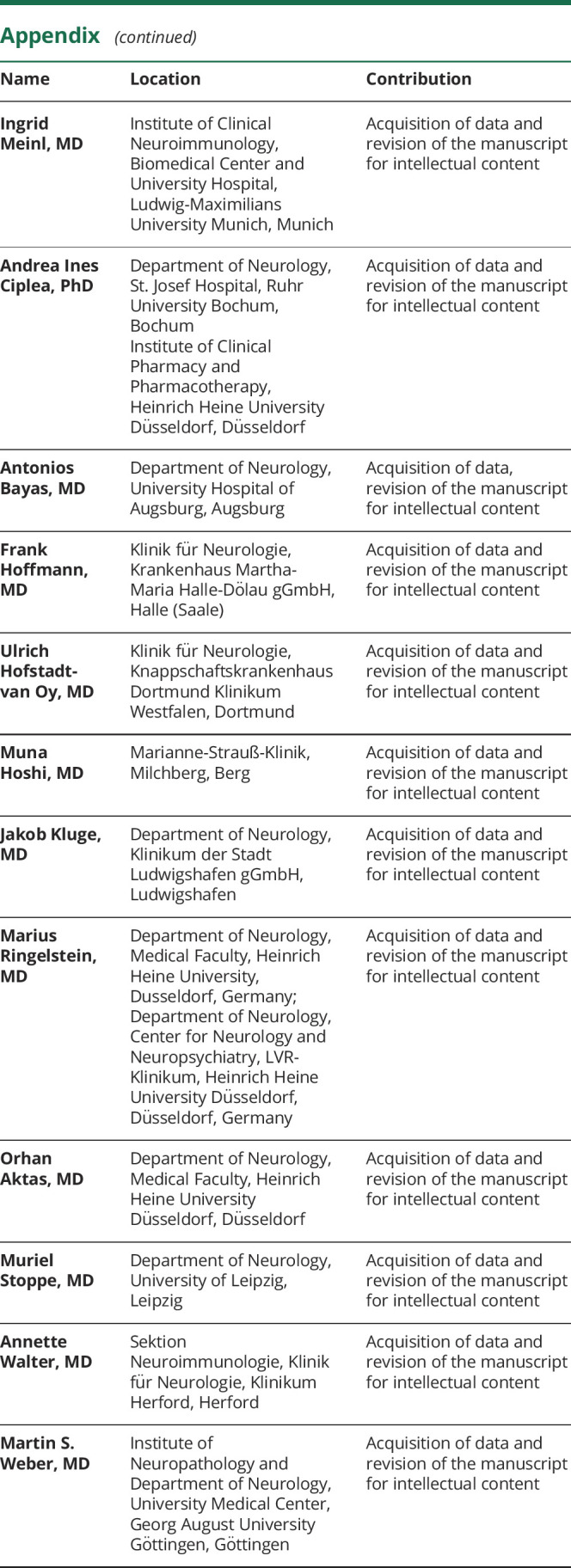
We identified 88 pregnancies of 81 women with neuroimmunologic diseases treated with RTX or OCR ≤12 months before the last menstrual period (LMP) through the German MS and pregnancy registry (DMSKW) and centers from the Neuromyelitis Optica Study Group (NEMOS) network between November 2004 and February 2020 (figure). In the DMSKW, pregnant women with MS or other neuroimmunologic diseases (ONID) are enrolled at any time point during pregnancy and followed up prospectively with a standardized questionnaire.17 For pregnancies reported from NEMOS centers, we used a core minimal data set from the DMSKW consisting of the following variables: diagnosis, age, LMP, date of last RTX/OCR infusion before or after the LMP, pregnancy outcome, severe maternal and infant infections, relapses during pregnancy, and postpartum in patients with RRMS/NMOSD. Four pregnancies (1 PPMS, 1 NMOSD, and 2 ONID) from NEMOS centers were included retrospectively (all 4 with healthy newborns). Available B-cell counts from mothers and babies were collected. We stratified our cohort according to exposure to anti-CD20 mAbs before or after the LMP into 3 groups: >6M group = RTX/OCR >6 but ≤12 months before the LMP; <6M group = RTX/OCR <6 months before the LMP; preg group = RTX/OCR after the LMP.
Figure. Flowchart of the pregnancies enrolled in the study.
*ONID included in this cohort: 1 myasthenia gravis, 1 autoimmune myositis, 1 neurosarcoidosis, 1 MOG disease, 1 CRION, 2 NMDA-Ab encephalitis. CRION = chronic relapsing inflammatory optic neuropathy; DMSKW = German MS and pregnancy registry (Deutsches Multiple Sklerose und Kinderwunsch Register); DMT = disease-modifying therapy; GW = gestational week; mAb = monoclonal antibody; MOG = myelin oligodendrocyte glycoprotein; NEMOS = Neuromyelitis Optica Study Group; NMOSD = neuromyelitis optica spectrum disorder; ONID = other neuroimmunologic diseases; PPMS = primary progressive MS; RRMS = relapsing-remitting MS; SPMS = secondary progressive MS
Outcomes
Spontaneous abortion (SA) was defined as fetal loss before 22 completed gestational weeks (GWs). Congenital anomalies (CA) were rated and classified in accordance with the guidelines of EUROCAT and confirmed by the treating pediatrician/obstetrician. Birth weight and length and preterm birth (PB, live birth before 37 completed GWs) were analyzed as reported in mothers' maternity logs. Elective abortions (EAs) and ectopic pregnancies were also documented. B-cells, depletion in newborns was defined as not detectable B-cells, borderline as detectable but under the lower range of the reference.
In the subgroup of women with RRMS/NMOSD, the number of relapses before, during, and after pregnancy (follow-up 6 months) was analyzed using the current McDonald criteria relapse definition18 and disability progression12 by using the Expanded Disability Status Scale (EDSS).19 Except one, the EDSS was taken outside relapse (≥2 months). The baseline EDSS was the last available EDSS during the last year before pregnancy and without the occurrence of a relapse between the EDSS date and the LMP. Relapses were confirmed, and the EDSS was obtained by the treating neurologist.
Standard protocol approvals, registrations, and patient consents
All patients gave their informed consent. The DMSKW is approved by the review board of the Ruhr University in Bochum (Reg Nr.: 18-6474-BR). All patients who participated in the NEMOS gave written informed consent, and each local institutional review board of participating centers approved the study.
Statistical analysis
To compare pregnancy outcomes as well as relapses and disability progression during pregnancy and postpartum between groups, we used the Kruskal-Wallis rank-sum test for continuous and the χ2 test or Fisher exact test for categorical variables. A 2-sided p < 0.05 was considered as statistically significant.
Pregnancy outcomes were analyzed regardless of the underlying disease. To account for the difference in being at risk, we used different denominators: all known pregnancy outcomes for the outcomes live birth, SA, and EA and all live births for the outcomes CA and PB. In addition, we performed four sensitivity analysis with (i) prospective pregnancies and (ii) patients with MS and NMOSD (ONID excluded). We also stratified exposure (iii) by drug RTX/ OCR or (iv) by timing <3 months, >3 but ≤12 months before the LMP, or after LMP.
For all analysis of DA, we stratified our cohort into patients with RRMS and NMOSD. The analysis of DA during pregnancy only includes pregnancies with outcome after 22 GWs and treated with anti-CD20 mAbs already before pregnancy. The analysis of DA postpartum includes all pregnancies with anti-CD20 mAbs before or during pregnancy and a postpartum follow-up of 6 months (figure). Statistical analysis was performed using RStudio Version 1.2.5019.
Data availability
No deidentified patient data will be shared. No study-related documents will be shared. Reasonable requests from any qualified investigator for anonymized data will be considered by the corresponding author.
Results
Baseline characteristics
We analyzed 49 (55.7%) pregnancies after treatment with RTX and 39 (44.3%) after therapy with OCR. Most pregnancies occurred in women with MS (n = 64, 72.7%; n = 39 OCR and n = 25 RTX) or NMOSD (n = 17, 19.3%), and 7 (8.0%) in women with ONID (figure), the majority (n = 64, 72.7%) within 6 months after the last infusion administered with a median of 67 days before the LMP (range 4–169 days).
Fourteen pregnancies (15.9%) were exposed after the LMP (median 39 days, range 2–148 days), but only 4 because of worsening of the underlying autoimmune disease (RRMS, NMOSD, and chronic relapsing inflammatory optic neuropathy and myositis). One woman (NMOSD) followed her routine infusion scheme, and the remaining (n = 9) were infused during early pregnancy because pregnancy was undetected. Five of these 14 (35.7%) were treated with anti-CD20 mAbs for the first time during pregnancy: 2 because of a relapse, 1 due to worsening of myositis, and 2 due to undetected pregnancies.
Two pregnancies (1 RRMS and 1 NMOSD) were exposed simultaneously to another DMT (1 fingolimod and 1 azathioprine). Two (1 NMOSD and 1 myositis) received concomitant low-dose steroid therapy during pregnancy and 3 (1 RRMS and 2 NMOSD) high-dose corticosteroids for relapse treatment during pregnancy. Baseline characteristics of all pregnancies are shown in table 1.
Table 1.
Baseline characteristics of all 88 pregnancies
Pregnancy outcomes
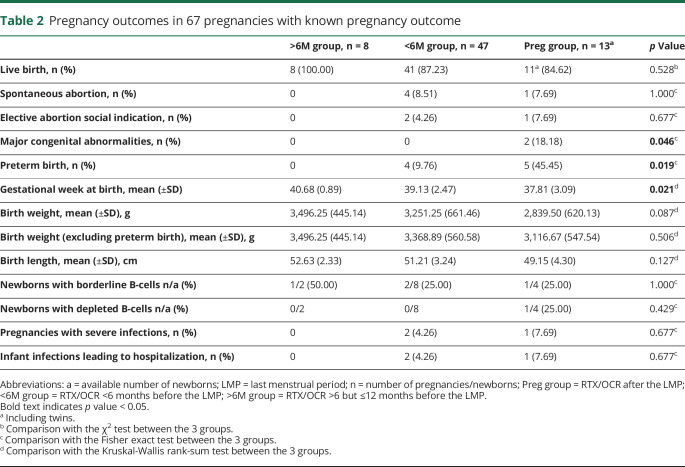
We analyzed the outcomes of 67 pregnancies (76.1%) including 1 twin pregnancy, most resulting in live births (n = 60/68; 88.2%) (table 2). Twenty-one (23.9%) pregnancies are still ongoing. The overall number of SAs (n = 5/68; 7.4%) was low regardless if reported by the DMSKW or by NEMOS centers. Overall, 15% of pregnancies ended in PB, significantly more often in those exposed during pregnancy (>6M group: 0/8; <6M group: 4/41 9.76%; preg group: 5/11 45.45%: p value: 0.019, table 2). Excluding PB, the birth weight was statistically not significantly lower in the preg group. PB occurred in median GW 35 (range 29.14–36.14), and preterm newborns had a mean birth weight of 2,308.13 ± 534.50 g. Potential reasons for PB are shown in table e-1, links.lww.com/NXI/A338.
Table 2.
Pregnancy outcomes in 67 pregnancies with known pregnancy outcome
Two of 60 live births (3.3%) were born with a major CA, both (a ventricular septum defect and an atrium septum defect with pulmonary stenosis) in the preg group (2/11, 18.2%, p value = 0.046) (table e-1, links.lww.com/NXI/A338). Three (4.4%) EAs due to social indication were performed.
Additional sensitivity analysis with a more conservative exposure cutoff of 3 months (see above Statistical analysis) replicated our findings concerning major CA (>3M group: 0/19; <3M group: 0/30; preg group: 2/11 18.2%: p value: 0.034) and PB (>3M group: 1/19 5.3%; <3M group: 3/30 10.0%; preg group: 5/11 45.4%: p value: 0.020). Excluding retrospective cases and ONID does not change the results. After stratification of exposure by drug (RTX or OCR), no statistically significant differences can be observed for major CA and PB (data not shown).
B-cell counts in newborns
B-cell counts were available for 14 babies (23.4%), 12 with 1 (9 cord blood, 2 during the first weeks of live, and 1 at age 3 months) and 2 with 2 B-cell counts (cord blood/2 and 5 months postpartum, respectively). B-cells according to anti-CD20 mAb exposure are shown in table 2. Despite exposure 6 months before the LMP (n = 8) or during pregnancy (n = 4), most had normal B-cell counts. Four (28.6%) newborns showed borderline B-cell counts (RTX 50 days before the LMP, 325 (ref. 600–1,000)/μL, 10 (ref. 13–39)%; OCR 99 days before the LMP, 420 (ref. 150–1,200)/μL, 9.1 (ref. 15–40)%; RTX 200 days before the LMP, 47 (ref. 50–631)/μL, 2 (ref. 5–24)%; and OCR 131 days after the LMP 339 (ref. 600–1,900)/μL, 12 (ref. 4–26)%). In the OCR-exposed baby, B-cells normalized at age 2 months (1,107 [ref. 600–3,000]/μL, 15 [ref. 13–39]%) despite OCR exposed breastfeeding.20 The B-cell–depleted newborn was exposed to RTX 141 days after the LMP and azathioprine until GW 7. At age 5 months, the B-cell count was normal and no serious infections were observed in 20 months of follow-up.
Breastfeeding
Of 57 women with available information on breastfeeding, 38 breastfed exclusively (n = 20/52.6%) or partly (n = 18/47.4%) for a median duration of 119 days (range 1–205 days). Three of them received anti-CD20 mAbs during breastfeeding, with a duration of exposed breastfeeding of 82, 54, and 53 days recently reported in Ref. 20.
Infections in mothers and infants
Severe infections during pregnancies occurred in 3 mothers (2 with decreased/depleted B-cells) and infections leading to hospitalization in 3 newborns (table 2 and table e-2, links.lww.com/NXI/A338).
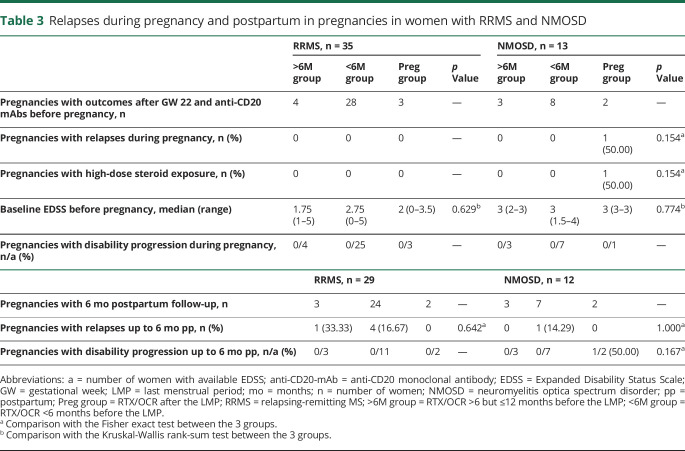
Relapses and disability progression during pregnancy and postpartum in women with RRMS
All pregnancies in women with RRMS (n = 35), anti-CD20 mAbs before conception, and known pregnancy outcomes after GW 22 were relapse free (table 3).
Table 3.
Relapses during pregnancy and postpartum in pregnancies in women with RRMS and NMOSD
For 5 of 29 pregnancies (17.2%), a relapse during the first 6 months postpartum (median time to first relapse postpartum 2.3 months; range 0.1–4.9 months) was documented. The majority (n = 21, 72.4%) restarted DMT (all anti-CD20 mAbs) with a median time of 3.0 months (range 0.3–26.0 months) after birth (median DMT-free interval 14.1 months, range 5.2–35.6). Only 1 woman had a relapse 44 days after the infusion with OCR, 69 days after delivery (table e-3, links.lww.com/NXI/A338). The median time between the last RTX/OCR and the relapse postpartum was 16.3 months (range 1.5–21 months).
The baseline EDSS (median 2.5, range 0–5) was evaluated median 33 days before the LMP (range 17–250) and the delta EDSS analyzed in 32/35 (91.4%; median 0, range −2 to 0) during pregnancy and 16/29 (55.2%; median 0 range −2 to 0.5) postpartum (table 3 and table e-3, links.lww.com/NXI/A338). All but 1 woman (autoimmune myositis) with ONID showed a stable DA during pregnancy without change of therapy.
Relapses and disability progression during pregnancy and postpartum in women with NMOSD
Most pregnancies (n = 12/13; 92.3%) in women with NMOSD, anti-CD20 mAbs before conception, and known pregnancy outcomes after GW 22 were relapse free (table 3). Only 1 woman had a relapse in GW 33 despite having received RTX before and during pregnancy. She had reduced her previous concomitant prednisolone therapy after notice of pregnancy. One woman started anti-CD20 mAbs during pregnancy because of a disastrous relapse with an EDSS increase from 2 to 7 after withdrawal of azathioprine at the beginning of pregnancy.
For one of 12 pregnancies (8.3%), 2 relapses during the first 6 months postpartum (time to first relapse postpartum 0.3 months) were documented (table 3 and table e-3, links.lww.com/NXI/A338). All restarted anti-CD20 mAbs with a median time of 0.45 months (range 0–4.2 months) after birth (median DMT-free interval 13.2 months, range 6.3–18.8).
The baseline EDSS (median 3; range 1.5–4) was evaluated median 120 days before the LMP (range 5–308) and delta EDSS analyzed in 11/13 (84.6%, median 0 range −1 to 0.5) during pregnancy and 12/12 (100%; median 0 range −0.5 to 2.5) postpartum. The EDSS remained stable during pregnancy in all patients. Postpartum, all but 1 (11/12; 91.7%) patients with NMOSD showed a stable EDSS. This patient received RTX for the first time during pregnancy due to a disastrous relapse and had 2 relapses during the second half of the postpartum year (table 3).
Relapses in patients with RRMS and NMOSD depending on the B-cell count
For analysis of DA during pregnancy, we had 12 (25.0%) B-cell counts of 48 included pregnancies available. Most (9; 75.0%) had detectable B-cells in peripheral blood during pregnancy, only 1 (NMOSD) of them relapsed. Postpartum, 9 (22.0%) B-cell counts—all of them before the first anti-CD20 mAb infusion after delivery—from 41 pregnancies were available and detectable in all of them, 3 (2 RRMS and 1 NMOSD) of these women relapsed. In 3 women with MS with postpartum relapses, B-cell counts were not available.
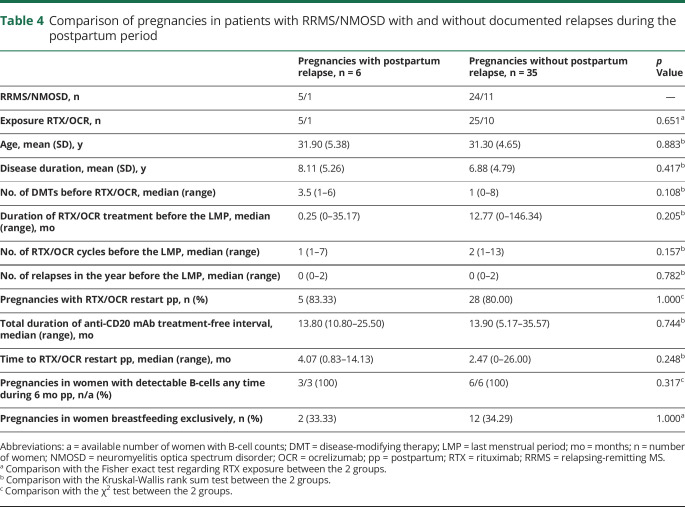
Predictors for postpartum relapses in patients with RRMS and NMOSD
Women (RRMS/NMOSD) without postpartum relapses had received anti-CD20 mAbs for a longer time with more cycles and were retreated earlier postpartum than those who relapsed (table 4). However, this difference was not statistically significant.
Table 4.
Comparison of pregnancies in patients with RRMS/NMOSD with and without documented relapses during the postpartum period
Discussion
In our cohort study, we found that pregnancy outcomes after treatment with anti-CD20 mAbs in the year before pregnancy in women with neuroimmunologic diseases were within the range what is expected for the general population. If anti-CD20 mAbs were given during pregnancy, we observed significantly more PBs and 2 major CAs. Another important finding of our study is the good control of DA during pregnancy (98%) and postpartum (85%), observed in most pregnancies in women with RRMS/NMOSD, although treatment was generally suspended during pregnancy.
In contrast to a recently published study from southern California with similar sample size, where 27% of the women had SA,2 we did not observe an increased risk. In this population-based study of a health insurance where data linkage to the gynecologic records is possible, pregnancies are captured very early. In our study, first contact was at the beginning of the second trimester, after the risk for SA is already decreasing, a common limitation in pregnancy registries.21
The overall prevalence of major CA was 3.3% (n = 2), both in women who were treated with OCR during pregnancy, which is in line with outcomes from unexposed pregnancies from our DMSKW registry.17 RTX or OCR exposure was not associated with teratogenicity in humans,1,3 nor in animal studies22,23 so far, and we believe that it is a chance finding.
Although the overall risk of PB was similar to other studies,2,24 we found a higher risk for PB (45%) and lower birth weight when anti-CD20 mAb was given during pregnancy. This might be partially related to the underlying disease and/or concomitant autoimmune diseases,25 especially in NMOSD, to the previous DMT exposure and/or other concomitant medication with steroids, and deserves further investigation. To what extent long-term treatment with anti-CD20 mAbs may lead to hypogammaglobulinemia, which in turn could increase the risk of neonatal and maternal infections26,27 including chorioamnionitis—another potential underlying mechanism of PB—is still unknown. Recently, it was shown that treatment with RTX increases the risk of infections in the general MS population.28 We did not collect systematically information on IgG levels, but 3 women experienced severe infections potentially attributable to B-cell depletion.
In most women who were treated during pregnancy, anti-CD20 mAbs were given early during the first trimester, suggesting that only limited amounts of the drugs passed through the placental barrier and fetal exposure was low.29 So far, data on B-cell counts in the newborn, especially from mothers with MS or NMOSD, are based on single case reports.30 In our study, B-cell counts were normal in the majority (73%) of the babies, of note also in 2 first trimester exposed babies. Four babies were born with borderline values, but determination of B-cell counts in those newborns was not standardized and the exact methods used unknown. The fact that one newborn was B-cell depleted after pregnancy exposure to RTX during the second trimester is in line with previous reports and indicates that treatment after the second trimester is a risk factor for neonatal B-cell reduction. This should require the measurement of B-cells at birth and a close interaction with pediatricians to time vaccinations accordingly.1,31
Our data that all women with RRMS who had been treated with anti-CD20 mAbs before pregnancy experienced a stable DA during pregnancy are very reassuring and in line with a recent observation in a retrospective cohort of 27 patients with MS from Sweden16 and both Californian studies.1,2 Of note, women who were treated >6 months before the LMP were effectively untreated by the end of pregnancy.
Although more women with RRMS in our cohort (17,2%) relapsed postpartum compared with the southern Californian study (2.7%), our results still demonstrate a very good control of DA specially in comparison to other active MS pregnancies, e.g., after the suspension of natalizumab (36.5% relapsed during pregnancy and 21.7% in the first postpartum year).12 Reasons for the higher number of postpartum relapses in our patients with RRMS may include the close prospective follow-up of our patients as well as a more active disease cohort, which is reflected by the high number of previous DMTs in 4 RRMS patients with relapses. As B-cells were detectable in 2 women with RRMS who relapsed but also in 4 women without postpartum relapses, the reoccurrence of B-cells did not seem to predict these relapses.
In our cohort, women with NMOSD had a surprisingly low relapse risk, although relapse rates are known to increase after delivery in this disease spectrum15,32,33 or perhaps already during pregnancy.14 Because of the low number of relapses, we were not able to identify significant risk factors for recurrent DA. So far, suspension of immunosuppression has been identified as the main risk factor for relapses during pregnancy and postpartum,14 which is reflected by the 1 case in our cohort with the disastrous relapse during pregnancy after withdrawal of azathioprine and before start with RTX. In addition, the presence of B-cells in the peripheral blood has been associated with NMOSD relapses in previous studies,34 which is partly supported by our observations because 3 relapses occurred all in women with detectable B-cells.
Although nonsignificant, we identified the overall treatment duration with anti-CD20 mAbs and number of RTX/OCR cycles before pregnancy and the later reinfusion postpartum as possible risk factors for postpartum relapses in patients with RRMS/NMOSD. Thus, women with active disease before pregnancy might benefit from postponing pregnancy until stabilization of DA and resuming anti-CD20 mAbs early after delivery, but more data are needed to give a definite advice.
Recent publications deliver reassurance for the use of mAbs during breastfeeding in neuroimmunologic diseases.35 The amount of RTX in the breast milk was shown to be minimal. Data on OCR transfer are not available yet but can be anticipated to be very low.36 Even if not officially labeled, we believe that women should not forego nursing of mature newborns because of anti-CD20 mAbs, but again, more data with a longer follow-up of the children are needed.
Beside the short follow-up time, our study has other limitations: importantly, our data are limited by a relatively small sample size, which precluded a more detailed, multivariable adjusted analysis, especially as adverse pregnancy outcomes and in our cohort also relapses were rare events. The fact that 2 neonatal strokes have been reported recently after anti-CD20 mAb therapy2,37 underlines the importance of a systematic collection of data and if possible a combined analysis between different registries to increase sample size in the future. In our cohort, the treatment duration with OCR before pregnancy is still short because it was only approved in Germany for RRMS in early 2018, an important limitation if the risk for infection increases with longer use. In addition, we only have limited information on the health status of the infants at birth such as the Apgar score and long-term outcomes of the babies including developmental milestones, all infections, vaccinations, and systematic data on B-cells.
Nonetheless, our study has strengths, among them is the inclusion of the largest cohort of RTX-treated women with NMOSD, the possibility to stratify for 3 different exposure groups, and at least in some women and babies, the availability of B-cell counts.
Our findings demonstrate that anti-CD20 mAbs are highly effective for disease control in women with RRMS and NMOSD during and also partly after pregnancy and no major safety signal was observed after use within 6 months before conception. This finding is biologically plausible as the placental transfer for mAbs during the first trimester is negligible.38 Anti-CD20 mAbs offer advantages for women with neuroimmunologic diseases, especially with active RRMS/NMOSD who want to get pregnant due to its long-lasting effects. Both RTX and OCR are interesting options as the drugs themselves are cleared within 4–6 months after exposure, but the biological effect seems to continue. Besides, B-cell monitoring for the mothers and newborns long-term data and data from larger patient cohorts are necessary to determine the safety profile and identify the best time point when to restart after delivery. Especially more information on the infection risk during and after pregnancy in association with serum immunoglobulin levels in the mother and child is needed. Therefore, most importantly, outcome on pregnancies after anti-CD20 mAbs should be all carefully documented in registries, especially in rare diseases such as NMOSD.
Glossary
- CA
congenital anomalies
- DA
disease activity
- DMT
disease-modifying therapy
- EA
elective abortion
- EDSS
Expanded Disability Status Scale
- GW
gestational week
- LMP
last menstrual period
- mAb
monoclonal antibody
- NEMOS
Neuromyelitis Optica Study Group
- NMOSD
neuromyelitis optica spectrum disorder
- OCR
ocrelizumab
- ONID
other neuroimmunologic diseases
- RRMS
relapsing-remitting MS
- RTX
rituximab
- SA
spontaneous abortion
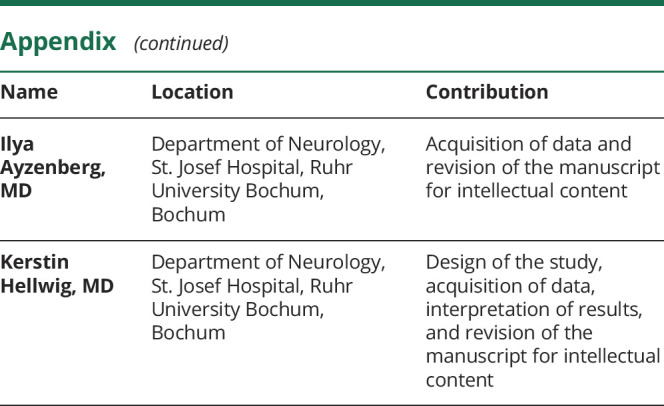
Appendix. Authors
Study funding
The German Multiple Sclerosis and Pregnancy Registry (DMSKW) is partly supported by the Innovation Fund of the Federal Joint Committee, Bayer Vital GmbH, Biogen GmbH Germany, Teva GmbH, Novartis Pharma GmbH, Merck Serono GmbH, and Sanofi Genzyme. The Neuromyelitis Optica Study Group (NEMOS) is partially funded by the German Ministry for Education and Research (BMBF) as part of the German Competence Network Multiple Sclerosis (KKNMS; for NEMOS NationNMO-DAB FKZ 01GI1602).
Disclosure
T. Kümpfel received speaker honoraria from Bayer HealthCare, Merck, Novartis Pharma, Roche Pharma, and Biogen as well as grant support from Novartis. S. Thiel received speaker honoraria from Bayer HealthCare. I. Meinl received travel expenses from MedDay and Roche Pharma and compensation from Serono and Roche Pharma. A.I. Ciplea received speaker honoraria from Bayer HealthCare and travel grants from Sanofi Genzyme, Teva, and Novartis. A. Bayas received personal compensation from Merck Serono, Biogen, Bayer, Novartis, Teva, Roche, Sanofi/Genzyme, Celgene, and Alexion and grants for congress trips and participation from Biogen, Teva, Novartis, Sanofi/Genzyme, Merck Serono, and Celgene. F. Hoffmann received speaker honoraria and grant support from Alexion, Bayer Vital, Biogen, CSL Behring, DIAMED Medizintechnik, Genzyme, Grifols, Ipsen, Merck Serono, Novartis, Roche, and Teva. U. Hofstadt-van Oy received speaker honoraria from Merck and Bayer HealthCare and research support by unrestricted grants from Bayer Schering, Novartis, and Merck. M. Hoshi received travel expenses and speaker honoraria from Bayer HealthCare, Merck, Sanofi-Aventis/Genzyme, and Biogen. J. Kluge declares no potential conflicts of interest with respect to this article. M. Ringelstein received speaker honoraria from Novartis, Bayer Vital GmbH, Roche, Alexion, and Ipsen and travel reimbursement from Bayer Schering, Biogen Idec, Merz, Genzyme, Teva, Roche, and Merck, none related to this study. O. Aktas reports grants from the German Ministry of Education and Research (BMBF), outside of the submitted work, and personal fees from Bayer HealthCare, Biogen, Merck Serono, Novartis, Roche, Teva, Alexion, and MedImmune, outside of the submitted work. M. Stoppe declares no potential conflicts of interest with respect to this article. A. Walter received travel expenses and speaker honoraria from Bayer HealthCare, Teva Pharma, Merck, Novartis Pharma, Sanofi-Aventis/Genzyme, Biogen, and Roche Pharma. M.S. Weber receives research support from the Deutsche Forschungsgemeinschaft (DFG; WE 3547/5-1), Novartis, Teva, Biogen Idec, Roche, Merck, and the ProFutura Programm of the Universitätsmedizin Göttingen. M.S. Weber is serving as an editor for PLoS One. He received travel funding and/or speaker honoraria from Biogen Idec, Merck Serono, Novartis, Roche, Teva, Bayer, and Genzyme. I. Ayzenberg received travel grants from Biogen Idec and Guthy-Jackson Charitable Foundation, served on scientific advisory boards for Roche and Alexion, and received research support from Diamed, none related to thisarticle. K. Hellwig has received travel grants from Biogen, Novartis, and Merck and received speaker and research honoraria from Biogen Idec Germany, Teva, Sanofi Genzyme, Novartis, Bayer HealthCare, Merck Serono, and Roche. Go to Neurology.org/NN for full disclosures.
References
- 1.Das G, Damotte V, Gelfand JM, et al. Rituximab before and during pregnancy: a systematic review, and a case series in MS and NMOSD. Neurol Neuroimmunol Neuroinflamm 2018;5:e453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith JB, Hellwig K, Fink K, Lyell DJ, Piehl F, Langer-Gould A. Rituximab, MS, and pregnancy. Neurol Neuroimmunol Neuroinflamm 2020;7:e734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chakravarty EF, Murray ER, Kelman A, Farmer P. Pregnancy outcomes after maternal exposure to rituximab. Blood 2011;117:1499–1506. [DOI] [PubMed] [Google Scholar]
- 4.Krysko KM, Graves JS, Dobson R, et al. Sex effects across the lifespan in women with multiple sclerosis. Ther Adv Neurol Disord 2020;13:1756286420936166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dobson R, Dassan P, Roberts M, Giovannoni G, Nelson-Piercy C, Brex PA. UK consensus on pregnancy in multiple sclerosis: “Association of British Neurologists” guidelines. Pract Neurol 2019;19:106–114. [DOI] [PubMed] [Google Scholar]
- 6.Thone J, Thiel S, Gold R, Hellwig K. Treatment of multiple sclerosis during pregnancy–safety considerations. Expert Opin Drug Saf 2017;16:523–534. [DOI] [PubMed] [Google Scholar]
- 7.Meinl I, Havla J, Hohlfeld R, Kumpfel T. Recurrence of disease activity during pregnancy after cessation of fingolimod in multiple sclerosis. Mult Scler 2018;24:991–994. [DOI] [PubMed] [Google Scholar]
- 8.Rigau V, Mania A, Befort P, et al. Lethal multiple sclerosis relapse after natalizumab withdrawal. Neurology 2012;79:2214–2216. [DOI] [PubMed] [Google Scholar]
- 9.Hellwig K, Gold R. Immune reconstitution inflammatory syndrome after withdrawal of natalizumab? Neurology 2011;76:1362–1363. [DOI] [PubMed] [Google Scholar]
- 10.Barry B, Erwin AA, Stevens J, Tornatore C. Fingolimod rebound: a review of the clinical experience and management considerations. Neurol Ther 2019;8:241–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canibaño B, Ali M, Mesraoua B, et al. Severe rebound disease activity after fingolimod withdrawal in a pregnant woman with multiple sclerosis managed with rituximab: a case study. Case Rep Womens Health 2020;25:e00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Portaccio E, Moiola L, Martinelli V, et al. Pregnancy decision-making in women with multiple sclerosis treated with natalizumab: II: maternal risks. Neurology 2018;90:e832–e839. [DOI] [PubMed] [Google Scholar]
- 13.Portaccio E, Annovazzi P, Ghezzi A, et al. Pregnancy decision-making in women with multiple sclerosis treated with natalizumab: I: fetal risks. Neurology 2018;90:e823–e831. [DOI] [PubMed] [Google Scholar]
- 14.Mao-Draayer Y, Thiel S, Mills EA, et al. Neuromyelitis optica spectrum disorders and pregnancy: therapeutic considerations. Nat Rev Neurol 2020;16:154–170. [DOI] [PubMed] [Google Scholar]
- 15.Klawiter EC, Bove R, Elsone L, et al. High risk of postpartum relapses in neuromyelitis optica spectrum disorder. Neurology 2017;89:2238–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Juto A, Fink K, Al Nimer F, Piehl F. Interrupting rituximab treatment in relapsing-remitting multiple sclerosis; no evidence of rebound disease activity. Mult Scler Relat Disord 2020;37:101468. [DOI] [PubMed] [Google Scholar]
- 17.Thiel S, Langer-Gould A, Rockhoff M, et al. Interferon-beta exposure during first trimester is safe in women with multiple sclerosis-A prospective cohort study from the German Multiple Sclerosis and Pregnancy Registry. Mult Scler 2016;22:801–809. [DOI] [PubMed] [Google Scholar]
- 18.Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 2018;17:162–173. [DOI] [PubMed] [Google Scholar]
- 19.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983;33:1444–1452. [DOI] [PubMed] [Google Scholar]
- 20.Ciplea AI, Langer-Gould A, de Vries A, et al. Monoclonal antibody treatment during pregnancy and/or lactation in women with MS or neuromyelitis optica spectrum disorder. Neurol Neuroimmunol Neuroinflamm 2020;7:e723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Margulis AV, Mittleman MA, Glynn RJ, Holmes LB, Hernández-Díaz S. Effects of gestational age at enrollment in pregnancy exposure registries. Pharmacoepidemiol Drug Saf 2015;24:343–352. [DOI] [PubMed] [Google Scholar]
- 22.EMA. Ocrevus (ocrelizumab)–EPAR summary of product characteristics 2018. Available at: ema.europa.eu/en/documents/product-information/ocrevus-epar-product-information_en.pdf. Accessed June 5, 2020.
- 23.EMA. MabThera (rituximab)–EPAR summary of product characteristics 2008. Available at: ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000165/WC500025821.pdf. Accessed March 25, 2020.
- 24.Lopez-Leon S, Geissbühler Y, Sabidó M, Turkson M, Wahlich C, Morris JK. A systematic review and meta-analyses of pregnancy and fetal outcomes in women with multiple sclerosis: a contribution from the IMI2 ConcePTION project. J Neurol 2020;267:2721–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.He WR, Wei H. Maternal and fetal complications associated with systemic lupus erythematosus: an updated meta-analysis of the most recent studies (2017–2019). Medicine (Baltimore) 2020;99:e19797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roberts DM, Jones RB, Smith RM, et al. Rituximab-associated hypogammaglobulinemia: incidence, predictors and outcomes in patients with multi-system autoimmune disease. J Autoimmun 2015;57:60–65. [DOI] [PubMed] [Google Scholar]
- 27.Derfuss T, Weber MS, Hughes R, et al. Serum Immunoglobulin Levels and Risk of Serious Infections in the Pivotal Phase III Trials of Ocrelizumab in Multiple Sclerosis and Their Open-Label Extensions. ECTRIMS 2019 Congress; September 11–13 2019. Stockholm: ECTRIMS Online Library; 2019. [Google Scholar]
- 28.Luna G, Alping P, Burman J, et al. Infection risks among patients with multiple sclerosis treated with fingolimod, natalizumab, rituximab, and injectable therapies. JAMA Neurol 2020;77:184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ciobanu AM, Dumitru AE, Gica N, Botezatu R, Peltecu G, Panaitescu AM. Benefits and risks of IgG transplacental transfer. Diagnostics (Basel) 2020;10:583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ringelstein M, Harmel J, Distelmaier F, et al. Neuromyelitis optica and pregnancy during therapeutic B cell depletion: infant exposure to anti-AQP4 antibody and prevention of rebound relapses with low-dose rituximab postpartum. Mult Scler 2013;19:1544–1547. [DOI] [PubMed] [Google Scholar]
- 31.Ostensen M. Safety issues of biologics in pregnant patients with rheumatic diseases. Ann N Y Acad Sci 2014;1317:32–38. [DOI] [PubMed] [Google Scholar]
- 32.Kim W, Kim SH, Nakashima I, et al. Influence of pregnancy on neuromyelitis optica spectrum disorder. Neurology 2012;78:1264–1267. [DOI] [PubMed] [Google Scholar]
- 33.Fragoso YD, Adoni T, Bichuetti DB, et al. Neuromyelitis optica and pregnancy. J Neurol 2013;260:2614–2619. [DOI] [PubMed] [Google Scholar]
- 34.Pellkofer HL, Krumbholz M, Berthele A, et al. Long-term follow-up of patients with neuromyelitis optica after repeated therapy with rituximab. Neurology 2011;76:1310–1315. [DOI] [PubMed] [Google Scholar]
- 35.LaHue SC, Anderson A, Krysko KM, et al. Transfer of monoclonal antibodies into breastmilk in neurologic and non-neurologic diseases. Neurol Neuroimmunol Neuroinflamm 2020;7:e769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krysko KM, LaHue SC, Anderson A, et al. Minimal breast milk transfer of rituximab, a monoclonal antibody used in neurological conditions. Neurol Neuroimmunol Neuroinflamm 2020;7:e637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rolfes M, Rutatangwa A, Waubant E, Krysko KM. Ocrelizumab exposure in the second trimester of pregnancy without neonatal B-cell depletion. Mult Scler Relat Disord 2020;45:102398. [DOI] [PubMed] [Google Scholar]
- 38.Palmeira P, Quinello C, Silveira-Lessa AL, Zago CA, Carneiro-Sampaio M. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol 2012;2012:985646. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No deidentified patient data will be shared. No study-related documents will be shared. Reasonable requests from any qualified investigator for anonymized data will be considered by the corresponding author.