Abstract
Background:
Combined transfer of the gluteus maximus and tensor fasciae latae (TFL) has been acknowledged as a treatment for irreparable full-thickness gluteus medius tears; yet, there is a paucity of reports on outcomes for this topic in the current literature. The purpose of the present study was to report short-term patient-reported outcome scores in patients who underwent combined transfer of the gluteus maximus and TFL in the setting of an irreparable gluteus medius tear.
Methods:
Data for patients who underwent hip preservation and hip arthroplasty between July 2011 and November 2017 were prospectively collected and retrospectively reviewed. Patients were considered for this study if they had undergone combined transfer of the gluteus maximus and TFL for irreparable gluteus medius tears. Inclusion criteria consisted of patients who had a minimum 1-year follow-up for the modified Harris hip score, Non-Arthritic Hip Score, Hip Outcome Score Sports Specific Subscale, visual analog scale score for pain, and patient satisfaction. The exclusion criterion was Workers’ Compensation status.
Results:
The study included 18 hips in 18 patients who underwent combined transfer of the gluteus maximus and TFL, with a mean follow-up of 39.75 months (range, 12.04 to 93.88 months). The average age was 68.48 ± 11.05 years, the average body mass index was 29.54 ± 6.23 kg/m2, and 13 patients were female. Abductor strength improved in 7 of 17 patients, with abduction data unavailable for 1 patient. Significant improvements were observed in modified Harris hip score from 49.73 ± 16.85 to 74.94 ± 17.91 (p < 0.001), Non-Arthritic Hip Score from 55.02 ± 22.53 to 72.78 ± 19.17 (p = 0.032), and visual analog scale for pain from 5.42 ± 3.42 to 1.57 ± 1.68 (p = 0.0004). No secondary surgeries were reported.
Conclusions:
Significant improvements in patient-reported outcomes were observed in patients who underwent combined transfer of the gluteus maximus and TFL for the treatment of irreparable full-thickness gluteus medius tears at short-term follow-up.
Level of Evidence:
Level IV. See Instructions for Authors for a complete description of levels of evidence.
Greater trochanteric pain syndrome, a common clinical complaint among individuals over 60 years old, usually precedes abductor tendon tears and tendinopathy as trochanteric bursitis1. With nonoperative treatment, approximately 90% of cases are resolved2; however, in patients who experience continuous and recalcitrant lateral hip pain, abductor weakness, and a Trendelenburg gait, clinical suspicion should be raised for spontaneous avulsion of the gluteus medius tendon3. Open repair of the gluteus medius is often successful; however, the failure rate can be high if what remains is a deficient muscle or tendon4-8. Moreover, even successful repairs may show fatty degeneration on magnetic resonance imaging (MRI), a predisposing factor for retears7,9. With the ever-increasing number of surgical procedures being performed for greater trochanteric pain syndrome, a notable solution for irreparable gluteus medius tears becomes imperative. When facing irreparable gluteus medius tears, combined transfer of the gluteus maximus and tensor fasciae latae (TFL) has been described as an option10,11.
Although the gluteus maximus and TFL are not hip abductors themselves on account of their attachment to the fascia lata as opposed to the osseous surface of the greater trochanter, the anterior portion of the gluteus maximus passes over the greater trochanter, and the muscle fibers of the gluteus maximus and of the TFL are found to closely align in direction. This allows for the transfer of the gluteus maximus and TFL to the greater trochanter, permitting them to function as abductors of the hip12. Nonetheless, combined gluteus maximus and TFL transfer for irreparable gluteus medius tears is an uncommon procedure; therefore, there is a lack of data on outcomes in patients who have undergone this procedure. The purposes of the present study were to report short-term patient-reported outcomes in patients who underwent combined transfer of the gluteus maximus and TFL in the setting of an irreparable gluteus medius tear. We hypothesized that patients who underwent this surgical procedure for this particular indication would demonstrate significant improvement in postoperative patient-reported outcomes at short-term follow-up.
Materials and Methods
Patient Selection
Data for all patients who underwent a hip-preservation procedure and/or hip arthroplasty by the senior surgeon (B.G.D.) between July 2011 and November 2017 were prospectively collected and retrospectively reviewed. Patients were considered for this study if they had undergone combined transfer of the gluteus maximus and TFL for irreparable gluteus medius tears. Irreparable tears were defined as those that were largely retracted or atrophied. The classification system proposed by Lall et al. for greater trochanteric pain syndrome was used to classify these Type-V gluteus medius tears1. Patients were included if they had a minimum of 1 year of follow-up for the modified Harris hip score (mHHS)13, Non-Arthritic Hip Score (NAHS)14, Hip Outcome Score Sports Specific Subscale (HOS-SSS)15, and visual analog scale (VAS) score for pain and satisfaction16. The only exclusion criterion was Workers’ Compensation status in order to limit confounding effects. The institution began collection of the International Hip Outcome Score 12-item questionnaire (iHOT-12) in early 2014, and thus because of incomplete data, preoperative iHOT-12 scores were not recorded for the study.
Participation in the American Hip Institute Hip Preservation/Reconstruction Registry
Patients in this study were part of the American Hip Institute hip preservation and reconstruction patient registry. Some patients may have been evaluated in a previous study; however, the present study represents an updated cohort11. This study received institutional review board approval.
Preoperative Physical Examination and Assessment
All patients underwent preoperative physical examination by the senior author (B.G.D.) to evaluate gait11. Points of tenderness near the greater trochanter were checked bilaterally. Abductor strength was assessed by the senior surgeon through extension of the hip and knee and through internal rotation at the hip while the patient was lying laterally. Hip strength was evaluated with the Medical Research Council grading scale from 0 (complete weakness) to 5 (full strength)17,18.
Surgical Indication for Combined Transfer of Gluteus Maximus and TFL
Patients were recommended for surgical treatment if they had pain that was recalcitrant to nonoperative treatment, including physical therapy and/or gait training, for at least 3 months. Patients suspected to present with a gluteus medius tear underwent further diagnostic MRI preoperatively. Patients were considered as having a possible irreparable gluteus medius tear if there was >2 cm of retraction or >50% fatty muscle infiltration1,11,19.
Surgical Technique
Exposure of Gluteus Maximus and TFL Triangular Muscle Flap
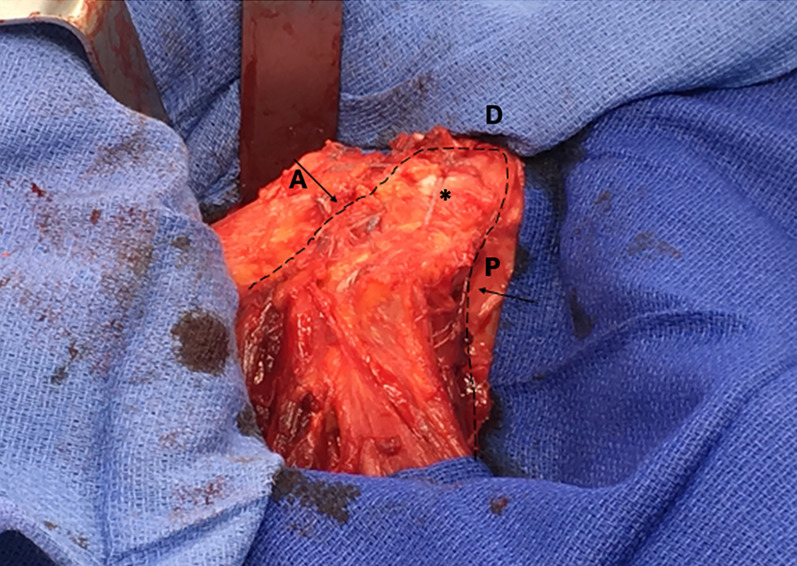
Patients were placed in the lateral decubitus position, and the skin was prepared and draped in sterile fashion prior to incision. A longitudinal incision was made directly centered over the posterior third of the greater trochanter11. The fascia lata and iliotibial band were identified (Fig. 1), and a triangular flap including the anterior third of the gluteus maximus and the posterior third of the TFL was created and mobilized (Fig. 2). Care was taken to not injure the lateral femoral circumflex artery and superior gluteal nerve.
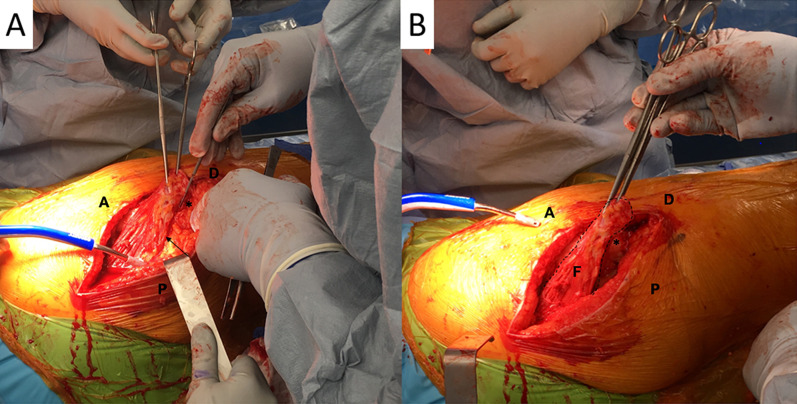
Fig. 1.
Figs. 1-A and 1-B Intraoperative photographs showing a right hip with the patient in the lateral decubitus position. A = anterior, P = posterior, D = distal, and * = greater trochanter. Fig. 1-A The posterior border of the triangular flap is marked by the black arrow. Fig. 1-B The complete triangular flap (F) is indicated with a dotted line.
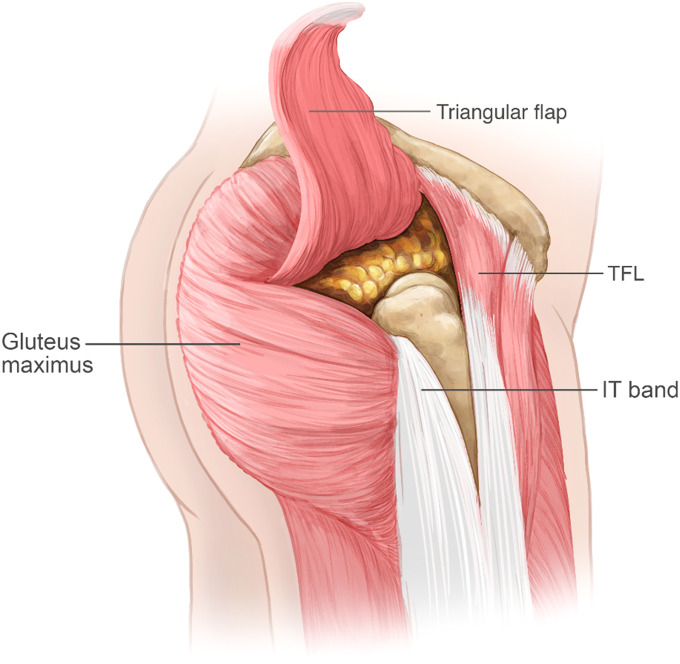
Fig. 2.
Illustration of a right hip showing the triangular flap including the anterior third of the gluteus maximus and the posterior third of the TFL for the combined transfer technique. IT = iliotibial.
Preparation of the Greater Trochanter and Triangular Muscle Flap Transfer
To provide a bleeding bone bed to enhance biologic healing of the triangular muscle flap transfer, the exposed greater trochanter was prepared and decorticated with use of a 5.5-mm arthroscopic round burr (Fig. 3). Two 5.5-mm polyetheretherketone corkscrew suture anchors (Arthrex) were placed at the superolateral edge of the greater trochanter. The triangular flap—i.e., the anterior third of the gluteus maximus and posterior third of the TFL—was then transferred to the greater trochanter to restore the abductor mechanism. The adjoining edges of the transferred flap were sutured together with absorbable sutures (No. 1 Vicryl; Ethicon), and the vastus lateralis edges were closed over the transferred flap (Fig. 4). The final construct is shown in Figure 5.
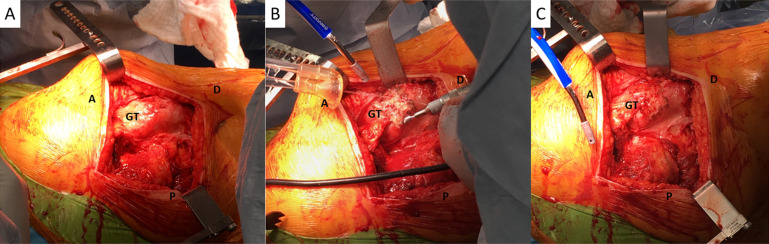
Fig. 3.
Figs. 3-A, 3-B, and 3-C Intraoperative photographs showing a right hip with the patient in the lateral decubitus position. A = anterior, P = posterior, D = distal, and GT = greater trochanter. Fig. 3-A The GT is shown prior to osseous-bed preparation. Fig. 3-B The gluteus medius footprint was prepared with use of a burr. Fig. 3-C The gluteus medius footprint osseous-bed preparation is shown.
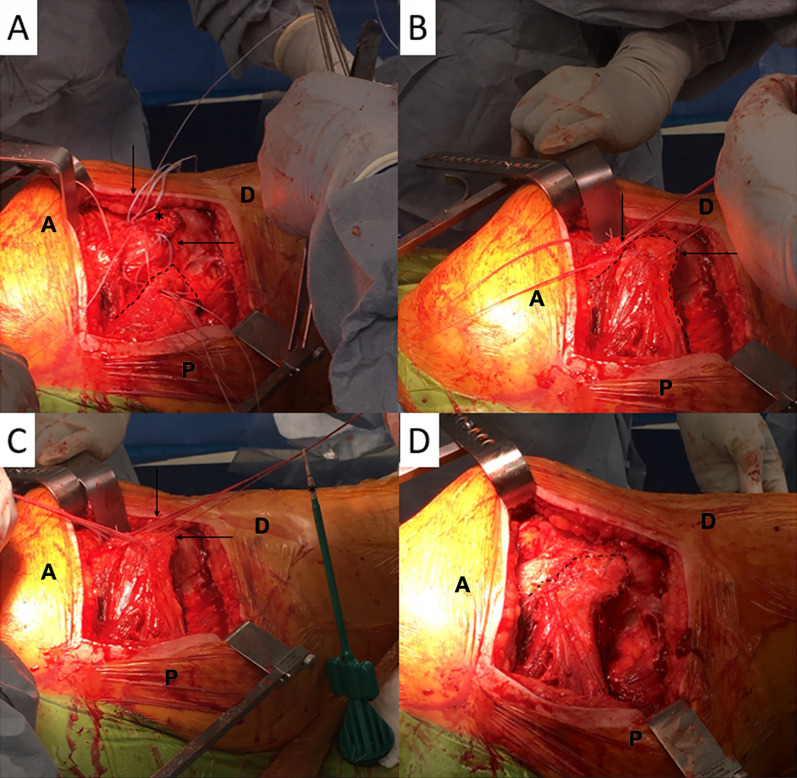
Fig. 4.
Figs. 4-A through 4-D Intraoperative photographs showing a right hip with the patient in the lateral decubitus position. A = anterior, P = posterior, and D = distal. Fig. 4-A Two knotless anchors had already been put in place for the first row (black arrows). * = greater trochanter. The combined gluteus maximus and TFL flap is identified by a dotted line. Fig. 4-B Sutures from each knotless anchor (black arrows) were passed through the triangular flap (dotted line). Fig. 4-C For the distal row of the construct, limbs from each knotless anchor (black arrows) were passed through 2 additional knotless anchors in a suture-bridge transosseous-equivalent fashion. Fig. 4-D The final construct with completion of the gluteus maximus transfer (dotted line).
Fig. 5.
Intraoperative photograph of a right hip with the patient in the lateral decubitus position showing the final construct for the combined transfer of the gluteus maximus and TFL. The dotted line indicates the flap border, and the arrows point to the anterior and posterior flap borders. A = anterior flap border, P = posterior flap border, D = distal end of the incision, and * = level of the greater trochanter.
Rehabilitation
All patients were instructed to remain 20-lb (9-kg) flat-foot weight-bearing with crutches or a walker for 8 weeks. Abduction exercises while standing were introduced under physical therapy guidance after 6 weeks and steadily increased for another 6 weeks. Abduction against gravity while lying on the nonoperative side was initiated 8 weeks postoperatively. Gait training was initiated 3 months postoperatively.
Patient-Reported Outcomes
Preoperative and latest postoperative patient-reported outcomes were evaluated, including the mHHS, NAHS, HOS-SSS, and iHOT-12. VAS pain and patient satisfaction were recorded on a 10-point scale, with 0 representing no pain and low satisfaction and 10 representing high pain and high satisfaction, respectively. The proportions of patients who attained the minimal clinically important difference and the patient-acceptable symptomatic state for the mHHS and iHOT-12 were also reported20,21. iHOT-12 scores were available for 10 patients. The questionnaires were completed either during a clinic appointment, through encrypted email, or over the telephone.
Statistical Analysis
Microsoft Excel was used to perform all analyses. The Shapiro-Wilk test was used to determine if data were normally distributed (p > 0.05) by testing the parametricity of continuous outcomes. A paired 2-tailed t test was then used to compare preoperative and postoperative results. Significance was set at 0.05.
Results
Patient Demographics
The study included 18 hips in 18 patients who underwent combined transfer of the gluteus maximus and TFL for the treatment of an irreparable gluteus medius tear, with a mean follow-up of 39.75 months (range, 12.04 to 93.88 months) (Table I). The average age (and standard deviation) was 68.48 ± 11.05 years, the average body mass index was 29.54 ± 6.23 kg/m2, and 13 patients were female. Three patients received concomitant arthroscopic procedures to address hip intra-articular pathologies such as labral tears and femoroacetabular impingement syndrome, whereas the remaining patients exclusively underwent open procedures with isolated gluteus maximus and TFL transfer. One patient had an ipsilateral total hip arthroplasty 2 weeks prior to the index procedure.
TABLE I.
Patient Demographics
| Hip* | |
| Left | 13 (72%) |
| Right | 5 (28%) |
| Sex* | |
| Female | 13 (72%) |
| Male | 5 (28%) |
| Age† (yr) | 68.48 ± 11.05 (71.25; 30.50-78.66) |
| Body mass index† (kg/m2) | 29.54 ± 6.23 (27.7; 21.92-44.39) |
| Follow-up time† (mo) | 39.75 (32.20; 12.04-93.88) |
| Follow-up rate* | 18 (100%) |
| Procedure type* | |
| Open | 15 (83%) |
| Intra-articular (arthroscopy) and open | 3 (17%) |
| Future reoperations and end points* | |
| Arthroscopy/endoscopy/open | 0 (0%) |
| Conversion to total hip arthroplasty | 0 (0%) |
| Death | 0 (0%) |
Values are given as the number of patients, with the percentage in parentheses.
Values are given as the mean and standard deviation, with the median and range in parentheses.
Abduction Strength Test
Seventeen of 18 patients included in the study underwent preoperative and postoperative abduction strength testing, ranging from 3 to 6 months postoperatively. Scores were improved by at least 1 grade in 7 patients and remained unchanged from preoperatively to postoperatively in 10 patients. All 10 patients had a preoperative strength deficit and did not show abductor strength improvement on physical examination at 3 to 6 months postoperatively.
Patient-Reported Outcomes
Significant improvements were observed in the following patient-reported outcomes from preoperatively to 2 years postoperatively (Table II): mHHS from 49.73 ± 16.85 to 74.94 ± 17.91 (p < 0.001), NAHS from 55.02 ± 22.53 to 72.78 ± 19.17 (p = 0.032), and VAS for pain from 5.42 ± 3.42 to 1.57 ± 1.68 (p = 0.0004). Although HOS-SSS improved from 18.76 ± 18.39 preoperatively to 38.08 ± 35.71 at 2 years postoperatively, this difference did not reach significance (p = 0.086). Among the 10 patients for whom iHOT-12 data were available, scores improved from 32.24 ± 15.5 to 54.37 ± 12.61 (p < 0.0001). Furthermore, 12 (67%) of 18 hips demonstrated improvements in the mHHS that surpassed the minimal clinically important difference (8 points) as reported in the literature, and 9 patients (50%) had a postoperative mHHS that surpassed the patient-acceptable symptomatic state (74 points)20,21. Eight (80%) of 10 patients with iHOT data surpassed the patient-acceptable symptomatic state. Patient satisfaction was 6.78 out of 10 overall.
TABLE II.
Patient-Reported Outcomes*
| Patient-Reported Outcomes | Preoperative | Latest | P Value |
| mHHS | 49.73 ± 16.85 (44.00; 32.90-68.00) | 74.94 ± 17.91 (75.50; 60.50-92.00) | <0.001 |
| NAHS | 55.02 ± 22.53 (53.88; 31.88-78.13) | 72.78 ± 19.17 (73.13; 56.25-90) | 0.032 |
| HOS-SSS | 18.76 ± 18.39 (8.00; 3.57-30.56) | 38.08 ± 35.71 (37.13; 21.04-44.19) | 0.086 |
| iHOT-12 | 32.24 ± 15.5 (31.67; 17.39-49.00) | 54.37 ± 12.61 (57.47; 48.64-64.85) | <0.0001 |
| VAS pain | 5.42 ± 3.42 (6.86; 0.00-9.96) | 1.57 ± 1.68 (1.08; 0.00-6.21) | 0.0004 |
| Patient satisfaction | — | 6.78 ± 2.55 (7; 5-9) |
Values are given as the mean and standard deviation, with the median and range in parentheses. Bolding indicates a significant p value (<0.05).
Discussion
The present study demonstrated significant improvement in multiple validated patient-reported hip-function measures as well as VAS pain at short-term follow-up in patients who underwent combined transfer of the gluteus maximus and TFL in the setting of irreparable gluteus medius tears. Twelve (67%) of 18 patients demonstrated improvements in mHHS that surpassed the minimal clinically important difference, and 9 patients (50%) had a postoperative mHHS that surpassed the patient-acceptable symptomatic state. Eight (80%) of 10 patients with iHOT-12 data met the patient-acceptable symptomatic state for the measure. Patient satisfaction, on average, was 6.78 out of 10. Abductor strength grades increased by at least 1 grade in 7 (41%) of 17 patients and was unchanged in 10 patients.
Gluteus medius tears have increasingly been shown to contribute to chronic lateral hip pain8,22. Once diagnosed on physical examination and MRI, the modalities to treat gluteus medius tears that are large and retracted with signs of major fatty atrophy are scarce11,12,23. Tendon transfer for the treatment of such tears is an option in these difficult cases12. Combined transfer of the gluteus maximus and TFL follows the general principles of tendon transfers, aiming to reproduce the line of pull of the deficient muscle without substantial loss of power at the donor site, which can be achieved because the transferred muscle fibers closely approximate the direction of pull of the deficient abductor muscles24. Whiteside examined the effects of gluteus maximus and TFL transfer on patients with gluteus medius rupture at the time of total hip arthroplasty10. Although no patient-reported outcomes were recorded in that study, 4 of 5 patients showed improvement in pain on abduction and gait. In another study by Whiteside, hips with complete gluteus medius avulsion and poor muscle quality underwent abductor muscle repair or gluteus maximus flap transfer25. Of the 35 hips with good muscle tissue that underwent gluteus maximus flap transfer, all 35 had good abduction against gravity, a negative Trendelenburg sign, and no lateral hip pain at 2 and 5 years postoperatively. These patients fared better than those who underwent simple gluteus medius repair for mild abductor tendon damage and those with poor muscle quality who underwent gluteus maximus flap transfer. Whiteside concluded that augmented repair with a gluteus maximus flap provided stable reconstruction, whereas simple repair did not prevent progressive abductor weakness in some hips.
Other tendons, such as the vastus lateralis and the Achilles, have been used as a source for abductor tendon transfers. Kohl et al. reported significant improvement in Merle d’Aubigné-Postel hip scoring system and pain scores for 11 patients who underwent a vastus lateralis muscle shift26,27. Similarly, Wang et al. also found that 3 out of 4 patients who underwent vastus lateralis transfer displayed dramatically improved VAS pain scores and hip-abduction power, as well as extremely high patient-reported satisfaction and improvements in walking23.
In contrast to the aforementioned studies above, which show a mixture of results, the present study adds to the existing literature by demonstrating a significant improvement in widely accepted patient-reported outcomes for patients who underwent combined transfer of the gluteus maximus and TFL for irreparable gluteus medius tears. Previously, Chandrasekaran et al.11 presented a small case series (3 patients) showing improvements in patient-reported outcomes and abductor strength following combined transfer of the gluteus maximus and TFL for irreparable gluteus medius tears at a minimum 1-year follow-up. The present study included a larger patient population and longer follow-up time than the aforementioned study, showing the sustainability of these favorable patient-reported outcomes. Patients with large gluteus medius tear but with minimal to no fatty muscle infiltration are most likely to undergo gluteus medius tear repair. However, more severe abductor deficiency associated with advanced fatty muscle infiltration may require gluteus maximus and TFL transfer28,29. Patients with irreparable gluteus medius tears with advanced fatty atrophy may benefit from the combined transfer of the gluteus maximus and TFL as the present study has reported.
It is important to note, however, that this is a salvage procedure for patients with irreparable gluteus medius tears and as such, some patients may not benefit clinically. Ten (41%) of the 17 patients for whom abductor strength data were available did not show any improvement in abductor strength postoperatively. However, this result may be attributed to the timing of evaluation because 3 to 6 months may not have been adequate for complete assessment of abductor strength. Nonetheless, patient satisfaction with the procedure was high, pain improved, and functional outcome scores increased significantly from preoperatively, which signifies success in this difficult-to-treat cohort.
Strengths
The present study had several noteworthy strengths. First, this is one of only a few studies to report multiple validated functional hip patient-reported outcomes in a group of patients who underwent combined transfer of the gluteus maximus and TFL in the setting of irreparable gluteus medius tears. Moreover, as significance does not equate to clinical relevance, the present study also reported on the proportion of patients who achieved the minimal clinically important difference and patient-acceptable symptomatic state for not only the mHHS but also the iHOT-1221.
Limitations
This study had some limitations. First, it has no control group. Second, although data collection was performed prospectively, this was a retrospective study, which introduces bias. Third, despite this study including one of the largest cohorts with short-term follow-up reported in the literature, there was still a minimal sample size. Fourth, longer follow-up is required to determine the sustainability of results. Fifth, the intra-articular pathologies that were addressed in 3 patients with concomitant arthroscopy may have had a potential confounding effect on the results. Sixth, the decision to classify a gluteus medius tear as irreparable, the selection of performing a combined transfer of the gluteus maximus and TFL, and the technique used for such a task are centered on the expertise of the senior author, which may create bias. Seventh, postoperative abductor strength was not consistently documented after the 6-month window period. Finally, the potential detrimental effect on function and due to removal of the transferred muscle from the donor site could not be addressed in the current investigation.
Conclusions
Patients who underwent combined transfer of the gluteus maximus and TFL in the setting of an irreparable full-thickness gluteus medius tear reported significant improvements in patient-reported outcomes and VAS pain at short-term follow-up.
Footnotes
Investigation performed at the American Hip Institute Research Foundation, Chicago, Illinois
Disclosure: One author (B.J.D.) was partially supported by the American Orthopaedic Association. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work; “yes” to indicate that the author had a patent and/or copyright, planned, pending, or issued, broadly relevant to this work; and “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJSOA/A225).
References
- 1.Lall AC, Schwarzman GR, Battaglia MR, Chen SL, Maldonado DR, Domb BG. Greater trochanteric pain syndrome: an intraoperative endoscopic classification system with pearls to surgical techniques and rehabilitation protocols. Arthrosc Tech. 2019. Aug 1;8(8):e889-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooker AF, Jr. The surgical approach to refractory trochanteric bursitis. Johns Hopkins Med J. 1979. Sep;145(3):98-100. [PubMed] [Google Scholar]
- 3.Chandrasekaran S, Vemula SP, Gui C, Suarez-Ahedo C, Lodhia P, Domb BG. Clinical features that predict the need for operative intervention in gluteus medius tears. Orthop J Sports Med. 2015. Feb 20;3(2):2325967115571079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies H, Zhaeentan S, Tavakkolizadeh A, Janes G. Surgical repair of chronic tears of the hip abductor mechanism. Hip Int. 2009. Oct-Dec;19(4):372-6. [DOI] [PubMed] [Google Scholar]
- 5.Lübbeke A, Kampfen S, Stern R, Hoffmeyer P. Results of surgical repair of abductor avulsion after primary total hip arthroplasty. J Arthroplasty. 2008. Aug;23(5):694-8. Epub 2008 Mar 4. [DOI] [PubMed] [Google Scholar]
- 6.Chandrasekaran S, Gui C, Hutchinson MR, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of endoscopic gluteus medius repair: study of thirty-four patients with minimum two-year follow-up. J Bone Joint Surg Am. 2015. Aug 19;97(16):1340-7. [DOI] [PubMed] [Google Scholar]
- 7.Alpaugh K, Chilelli BJ, Xu S, Martin SD. Outcomes after primary open or endoscopic abductor tendon repair in the hip: a systematic review of the literature. Arthroscopy. 2015. Mar;31(3):530-40. Epub 2014 Nov 1. [DOI] [PubMed] [Google Scholar]
- 8.Maldonado DR, Annin S, Chen JW, Rosinsky PJ, Shapira J, Lall AC, Domb BG. Full-thickness gluteus medius tears with or without concomitant hip arthroscopy: minimum 2-year outcomes using an open approach and contemporary tendon repair techniques. Orthop J Sports Med. 2020. Jul 10;8(7):2325967120929330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thaunat M, Clowez G, Desseaux A, Murphy CG, Sbiyaa M, Noël E, Sonnery-Cottet B. Influence of muscle fatty degeneration on functional outcomes after endoscopic gluteus medius repair. Arthroscopy. 2018. Jun;34(6):1816-24. Epub 2018 Mar 21. [DOI] [PubMed] [Google Scholar]
- 10.Whiteside LA. Surgical technique: gluteus maximus and tensor fascia lata transfer for primary deficiency of the abductors of the hip. Clin Orthop Relat Res. 2014. Feb;472(2):645-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chandrasekaran S, Darwish N, Vemula SP, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of gluteus maximus and tensor fascia lata transfer for primary deficiency of the abductors of the hip. Hip Int. 2017. Nov 21;27(6):567-72. Epub 2017 Jun 6. [DOI] [PubMed] [Google Scholar]
- 12.Whiteside LA. Surgical technique: transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop Relat Res. 2012. Feb;470(2):503-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aprato A, Jayasekera N, Villar RN. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy? Am J Sports Med. 2012. Nov;40(11):2557-60. Epub 2012 Sep 28. [DOI] [PubMed] [Google Scholar]
- 14.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The Nonarthritic Hip Score: reliable and validated. Clin Orthop Relat Res. 2003. Jan;406:75-83. [DOI] [PubMed] [Google Scholar]
- 15.Martin RL, Philippon MJ. Evidence of validity for the Hip Outcome Score in hip arthroscopy. Arthroscopy. 2007. Aug;23(8):822-6. [DOI] [PubMed] [Google Scholar]
- 16.Chandrasekaran S, Gui C, Walsh JP, Lodhia P, Suarez-Ahedo C, Domb BG. Correlation between changes in visual analog scale and patient-reported outcome scores and patient satisfaction after hip arthroscopic surgery. Orthop J Sports Med. 2017. Sep 13;5(9):2325967117724772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dyck PJ, Boes CJ, Mulder D, Millikan C, Windebank AJ, Dyck PJ, Espinosa R. History of standard scoring, notation, and summation of neuromuscular signs. A current survey and recommendation. J Peripher Nerv Syst. 2005. Jun;10(2):158-73. [DOI] [PubMed] [Google Scholar]
- 18.Vanhoutte EK, Faber CG, van Nes SI, Jacobs BC, van Doorn PA, van Koningsveld R, Cornblath DR, van der Kooi AJ, Cats EA, van den Berg LH, Notermans NC, van der Pol WL, Hermans MC, van der Beek NA, Gorson KC, Eurelings M, Engelsman J, Boot H, Meijer RJ, Lauria G, Tennant A, Merkies IS; PeriNomS Study Group. Modifying the Medical Research Council grading system through Rasch analyses. Brain. 2012. May;135(Pt 5):1639-49. Epub 2011 Dec 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bogunovic L, Lee SX, Haro MS, Frank JM, Mather RC, 3rd, Bush-Joseph CA, Nho SJ. Application of the Goutallier/Fuchs rotator cuff classification to the evaluation of hip abductor tendon tears and the clinical correlation with outcome after repair. Arthroscopy. 2015. Nov;31(11):2145-51. Epub 2015 Jul 15. [DOI] [PubMed] [Google Scholar]
- 20.Kivlan BR, Martin RL, Christoforetti JJ, Wolff AB, Nho SJ, Salvo JP, Jr, Ellis TJ, Van Thiel G, Matsuda D, Carreira DS. The patient acceptable symptomatic state of the 12-item International Hip Outcome Tool at 1-year follow-up of hip-preservation surgery. Arthroscopy. 2019. May;35(5):1457-62. Epub 2019 Apr 15. [DOI] [PubMed] [Google Scholar]
- 21.Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A. Research pearls: the significance of statistics and perils of pooling. Part 1: clinical versus statistical significance. Arthroscopy. 2017. Jun;33(6):1102-12. Epub 2017 Apr 25. [DOI] [PubMed] [Google Scholar]
- 22.Chi AS, Long SS, Zoga AC, Read PJ, Deely DM, Parker L, Morrison WB. Prevalence and pattern of gluteus medius and minimus tendon pathology and muscle atrophy in older individuals using MRI. Skeletal Radiol. 2015. Dec;44(12):1727-33. Epub 2015 Aug 11. [DOI] [PubMed] [Google Scholar]
- 23.Wang K, Cole S, White DC, Armstrong MS. Vastus lateralis transfer for severe hip abductor deficiency: a salvage procedure. Hip Int. 2014. Mar-Apr;24(2):180-6. Epub 2013 Oct 10. [DOI] [PubMed] [Google Scholar]
- 24.Sammer DM, Chung KC. Tendon transfers: part I. Principles of transfer and transfers for radial nerve palsy. Plast Reconstr Surg. 2009. May;123(5):169e-77e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whiteside LA. Gluteus transfer technique restores abductor deficiency in total hip arthroplasty. Orthop Proc. 2018;100-B(SUPP_13):43. [Google Scholar]
- 26.Kohl S, Evangelopoulos DS, Siebenrock KA, Beck M. Hip abductor defect repair by means of a vastus lateralis muscle shift. J Arthroplasty. 2012. Apr;27(4):625-9. Epub 2011 Sep 9. [DOI] [PubMed] [Google Scholar]
- 27.d’Aubigné RM, Postel M. The classic: functional results of hip arthroplasty with acrylic prosthesis. 1954. Clin Orthop Relat Res. 2009. Jan;467(1):7-27. Epub 2008 Oct 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davies JF, Stiehl JB, Davies JA, Geiger PB. Surgical treatment of hip abductor tendon tears. J Bone Joint Surg Am. 2013. Aug 7;95(15):1420-5. [DOI] [PubMed] [Google Scholar]
- 29.Betz M, Zingg PO, Hirschmann A, Alireza A, Dora C. Primary total hip arthroplasty (THA) in patients with incomplete hip abductor tears: does hip abductor repair improve outcome? Hip Int. 2014. Jul-Aug;24(4):399-404. Epub 2014 Apr 17. [DOI] [PubMed] [Google Scholar]