Abstract
In some regions, endodontists are increasingly placing implants in their daily practice. Endodontists have been proponents of the use of a dental dam during root canal treatment. It is beneficial to reduce the ingestion/aspiration of dental instruments during implant placement. It may be beneficial to reduce the bacterial load during implant placement procedures because biofilm formation on implants can lead to failure. A dental dam may help reduce the ingress of oral bacteria during implant placement. This case report demonstrates the use of a dental dam during the surgical placement of a dental implant. A literature review is presented that includes the history and rationale for the use of dental dams during various dental procedures. It also reviews the risks of aspirating/ingesting implant instruments. The use of a dental dam during implant placement offers certain operator conveniences, while also providing a safer field with less chance of instrument swallowing. It is expected that the technique offers a less bacteria-laden operating field due to the reduction in salivary ingress into the surgical site.
Keywords: Dental implants, endodontics, rubber dams
HIGHLIGHTS.
This is the first case report placing a dental implant using a dental dam to isolate the site.
A literature review discussing the benefits of dental dam use during endodontics is included.
Potential benefits and drawbacks of the use of a dental dam during implant placement are proposed and discussed.
INTRODUCTION
In 1864, Dr. Sanford C. Barnum introduced to dentistry the concept of isolation with the use of rubber dams* (1). Dental dam isolation is accepted as a standard procedure during endodontic treatment and has been endorsed by many professional organisations, including the American Association of Endodontists (AAE), the European Society of Endodontology (EES) and the American Academy of Pediatric Dentistry (AAPD) (2). In a recent American Dental Association (ADA) news article, former AAE President Gerald Glickman stressed on the importance of the use of a dental dam during endodontic treatment (3).
Despite the acceptance of and urging by associations such as the AAE and EES to use dental dams for endodontics as well as other dental procedures, the use of dental dams is not mentioned in the dental implant literature. It should be noted that despite recommendations to use dental dams, some practitioners avoid it nonetheless.
The benefits of the use of dental dams in endodontics could be expected to also be applicable during implant placement: improved visualisation of the crest of the ridge through isolation of the site from saliva, tongue and blood ingress and reduced risk of ingestion or aspiration of irrigation solutions and small instruments (2). Additional benefits would include improved view of the operating field by the retraction of soft tissues and enhanced visual contrast and increased ability of patients to keep their mouths open during treatment (4).
Endodontists, particularly those in the United States, are increasingly placing implants in their practices (5). However, this trend is not observed throughout all regions because some general dentists hold the belief that endodontists should not be placing implants (5). The value placed on a dental dam during endodontic treatments may also be transferrable to the advantageous use of dental dams during implant placement. The use of a dental dam during implant placement offers enhanced isolation of the surgical site, reduced ingress of oral fluids and microorganisms to the surgical site, as well as reduced chance of aspiration and swallowing of dental instruments. These advantages will be expanded upon later in this manuscript.
CASE PRESENTATION
A 60-year-old female patient presented with the chief complaint of a missing tooth (#21) that she wanted to have replaced with an implant. She was taking no medications, did not have any known allergies and had a non-contributory health history. She presented with a nearly full complement of teeth that were in good condition. She had a missing left mandibular second premolar and left mandibular first molar (#19). A supernumerary premolar occupied the space of the missing molar. The missing left mandibular second premolar had been extracted 20 years previously due to extensive caries.
The alveolar bone in the extraction site had resorbed and left a marginally compromised horizontal dimension, including a buccal concavity. However, cone-beam computed tomography (CBCT) revealed adequate horizontal (both bucco-lingual and mesio-distal) and vertical bony dimensions to enable endosseous implant placement. Adequate keratinised tissue was present for the planned procedure. All the risks, benefits, costs and alternative treatments were discussed, and the patient approved the treatment plan and signed the consent. The referring dentist, who had already planned with the patient for implant placement, had provided a surgical stent stored in 0.12% chlorhexidine gluconate (Peridex®, Zila Pharmaceuticals, USA), enabling a prosthetically driven implant placement. The stent had been fabricated using a computer-aided surgical guide, providing a guide tube for proper three-dimensional placement of the implant (Simplant, Dentsply, USA). The patient rinsed preoperatively for 90 seconds with Peridex and was prepared for surgery.
After 2-minute application of topical 5% benzocaine, 3.4 mL 2% lidocaine (Xylocaine, International Medication Systems Limited, Dentsply, Tulsa, Oklahoma, USA) with 1:100,000 epinephrine was buccally and lingually infiltrated to the surgery site. A disinfected non-latex dental dam (soaked for 5 minutes in 5.25% sodium hypochlorite and then rinsed with sterile saline) was placed in a split-dam format extending from the supernumerary premolar to the ipsilateral mandibular incisors and secured with #0 clamps (Figure 1). A rotary soft tissue punch (Rotary Tissue Punch for Latch Type Handpieces, Salvin, USA) was used in a slow-speed handpiece to expose the crestal bone. Tissue remnants were curetted with a spoon excavator. Implant placement was performed as a flapless procedure.
Figure 1.

Dental dam isolation of the implant site. The dental dam was mesially and distally anchored to allow adequate visualisation of the the implant site. Note the buccal concavity of the alveolar ridge resulting from the extraction
A pilot drill was used in an engine-driven rotary handpiece at 1.000 revolutions per minute at 35 Newton-centimetres to create the initial pathway into the bone. The angulation was not ideal and needed to be redirected in the mesio-distal plane to properly localise the osteotomy. At this point, the use of the guide was discontinued because of improper angulation, and the rest of the procedure was completed without the use of the guide. OraSeal® Calk & Putty (Ultradent Products, South Jordan, UT) was placed around the dam margins to further seal the edges of the dam from the oral fluids (this Oraseal was later removed after the cover screw was placed). A pilot drill (Nobel Biocare, Switzerland) was then used to redirect along the properly angulated pathway, following which the osteotomy was completed to enable the placement of a 4.3×11.5 mm Nobel Select Replace implant (Nobel Biocare, Switzerland) (Figure 2). The implant was placed with a hand torque driver to 35 Newton-centimetres, and a healing abutment was hand tightened. A clinical view of the implant in place with the cover screw attached and the site still isolated with the dental dam can is shown in Figure 3. The implant was placed completely within the bony envelope, as shown in the postoperative CBCT scan slices in the sagittal view and coronal view (Figure 4, 5). Because of the concavity of the buccal bone due to resorption of the ridge, it was paramount to ensure that the implant was entirely placed within the alveolar housing and was yet prosthetically driven. This was accomplished, as shown in Figure 5.
Figure 2.
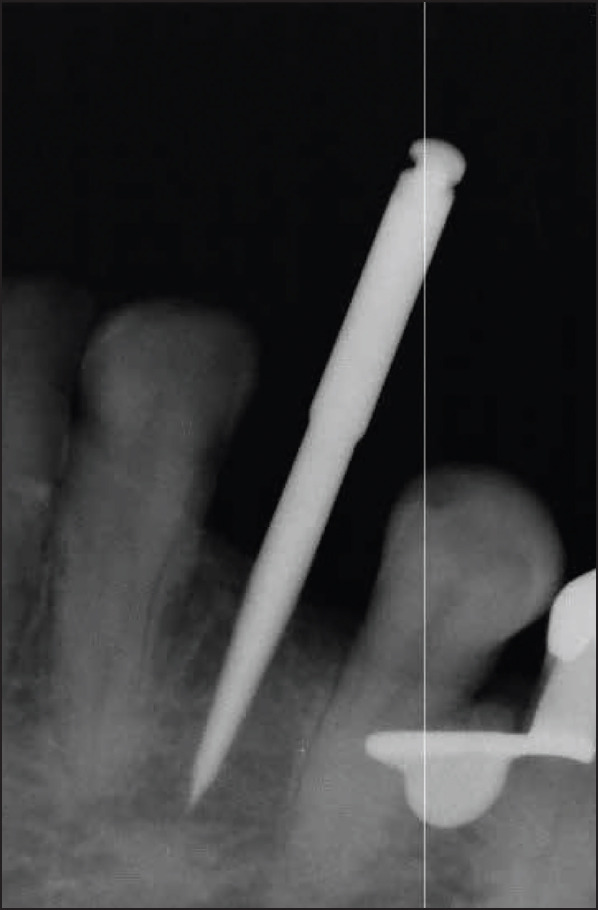
Intraoperative radiograph during the implant procedure. Radiograph shows pilot drill pathway after correction from the ill-fit surgical stent. The dental dam did not prevent the operator ability to diagnose an improperly angulated initial osteotomy. Correction of the angulation was done early in the implant placement procedure, as can be noted here
Figure 3.

The implant with attached healing abutment. The entire procedure, from tissue punch to osteotomy preparation and to healing abutment attachment to the implant, was performed under dental dam isolation
Figure 4.

The implant was placed entirely within the alveolar ridge. The CBCT scan shows the implant in a sagittal section spaced equidistant between the adjacent natural teeth
CBCT: cone-beam computed tomography
Figure 5.
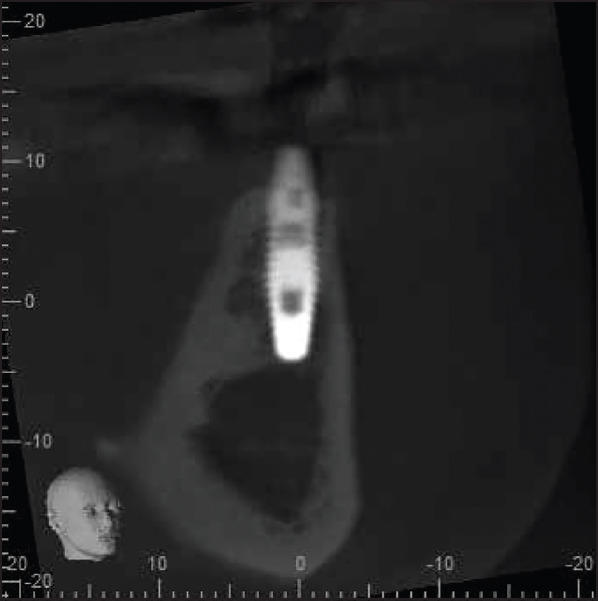
Coronal section of the CBCT scan shows the implant housed entirely within the alveolar bone. There was a buccal concavity in the bone from the resorption pattern of the alveolar ridge; thus, the implant was placed relatively closer to the buccal bone (but still entirely within the ridge) to enable prosthetically driven placement and future ease of restoration of the implant
CBCT: cone-beam computed tomography
Prescriptions for postoperative care included 21 tablets of 500 mg amoxicillin (t.i.d. for 7 days), 10 tablets of 5/325 mg hydrocodone/acetaminophen (Norco, Watson Pharmaceuticals, USA) (1-2 tablets every 6 hours, as needed for pain) and 1 bottle pf Peridex® to rinse the mouth (1 capful twice daily for 2 weeks). Postoperative evaluation showed satisfactory healing and no adverse signs or symptoms.
DISCUSSION
Benefits of dental dams
The use of a dental dam enables infection control by decreasing bacteria- and virus-laden aerosols (4). The failure to use a dam during non-surgical endodontic procedures can result in the aspiration or ingestion of dropped dental instruments with subsequent medical problems (6, 7).
Oral microorganisms play an essential role in the pathogenesis of apical periodontitis, a concept universally accepted in endodontics. It is also recognised in other disciplines (8). Goldfein et al. (9) evaluated the outcomes in patients who had posts placed either with or without the use of a dental dam; the success rate was 20% lower in the group without a dental dam than in the group with a dental dam, and the difference was statistically significant. Apparently, bacteria can, through salivary contamination, infect canal spaces even in the short periods of time during post placement and affect the treatment outcome. Could the same be true during the placement of dental implants?
Dental implants are susceptible to oral biofilms, similarly to teeth in case of periodontal disease (10). The presence of bacterial lipopolysaccharide and bacterial biofilms leads to peri-implant mucositis and peri-implantitis (10). Reducing the bacterial load in the surgical field appears to be beneficial because bacteria are able to form biofilms on the surface of many implant materials, and this can lead to implant failures (11).
A recent report on the effect of the use of dental dams on the survival of 517,234 endodontically treated teeth showed that after a mean observation period of 3.43 years, teeth treated with dental dam isolation had a higher survival probability (90.3%) than those treated without the same (88.8%) (12). Given the large sample size, the difference is statistically significant.
Confidence in the protective benefits of a dental dam may be an explanation why dentists who frequently use a dental dam also use higher concentrations of sodium hypochlorite and use ethylenediaminetetraacetic acid (EDTA) more often than dentists who do not. This can be extrapolated to implant placement, where implant screwdrivers and armamentarium instruments are often not tethered, which can lead to swallowing or aspirating the instruments by the patients. At the very least, operators using these untethered instruments may lack the confidence to use them properly without the use of a dental dam because they may worry about mishaps (e.g. swallowing, aspiration) and not pay attention to applying correct torque values.
Prevalence of dental dam use
Although it appears that dental dams are not currently used in implant dentistry, other dental disciplines use them more routinely. The use of dental dams during endodontic and restorative procedures is widely taught in dental schools. Despite learning to use dental dams during root canal treatment and expecting to routinely use dental dams after graduation, the rates of its use among dental school graduates are significantly lower in practice (13, 14).
An investigation found that only 44% of general dentists used a dental dam for all root canals procedures, 24% used it 51%-99% of the time, 17% used it less than 50% of the time and 15% never used it (14). Ireland (13) thus described the poor rate of use of a dental dam as follows: “Probably no other technique, treatment, or instrument used in dentistry is so universally accepted and advocated by the recognised authorities and so ignored by the practicing dentists”.
Common reasons for resistance to the use of a dental dam routinely include increased chair time necessary to apply the dam, lack of patient acceptance, insufficient training in its use (leading to difficulty in its application), insufficient emphasis placed on the necessity and application of the dam during dental school training, cost of equipment, as well as no increase in treatment fees (14). Avoiding the use of a dental dam due to the lack of patient acceptance has been challenged. Brookman (14) found that many patients prefer dams for dental treatment based on previous favourable experiences with them. Positive attitudes about the use of a dental dam by dentists and increased patient experience are major factors that could lead to increased acceptance (13).
Another negative view that dentists have about the use of a dental dam is often expressed in terms of being a “waste of time” rather than a valuable component of high-quality dental treatment. The application of a dental dam takes mere minutes, even in the hands of an inexperienced clinician, and the loss of time is compensated for by the many advantages inherent to the use of a dental dam, including increased visibility, decreased salivary contamination of the site, as well as retraction of soft tissues (4).
Use of dental dam during surgical implant placement
In this case report, the use of a dental dam sealed at the edges with Oraseal during the surgical placement of a dental implant provided convenient access to the surgical field, decreased the risk of aspiration or ingestion of a dropped instrument (such as an implant screwdriver, a cover screw, or an abutment) that could be aspirated or ingested and maintained a less contaminated environment. The dental dam did not present a problem during the exposure of treatment radiographs.
The literature is abundant with case reports of swallowed and aspirated dental instruments, including implant screwdrivers and implant crowns (6, 7). These procedural mishaps can be avoided with the use of a dental dam during implant placement. A clear benefit of using the dental dam during implant placement is providing a more safe surgical experience for the patient because an aspirated instrument can be life threatening and cause significant morbidity (7). In addition, the operator is better able to control the local conditions of the surgical site by reduction in ingress of oral fluids, decrease in aerosol formation and restriction of patient tongue movement (4).
In addition to the benefit of a dental dam reducing procedural mishaps during implant placement, there are biological reasons supporting its use as well. Implants may fail because of the loss of alveolar support, which has been attributed to the accumulation of biofilm and bacteria on the implant surfaces (similar to how periodontal disease negatively affects the periodontium) (10). Bacterial biofilms contain abundant lipopolysaccharides, which directly contribute to peri-implant mucositis and peri-implantitis (10). Biofilms formed on implant surfaces lead to implant failures (11). It is of clear benefit to attempt to reduce salivary and bacterial contact with the dental implant during surgical placement and manipulation. The use of a dental dam provides a potentially safer procedure for the patient and operator and may be beneficial to prevent salivary contamination of the dental implant during its surgical placement (4, 11).
The use of a dental dam during implant placement requires the presence of proximal teeth for dental dam clamps. Further, a dental dam may not provide a fluid-tight osteotomy site, similar to that accomplished during endodontic procedures; however, this problem can be addressed using a sealant such as OraSeal along the edges of the dam, similar to its use to create a fluid-tight seal during endodontic procedures.
It has been pointed out that there are situations in which the use of a dental dam may not be feasible during a dental procedure. Such a situation would be expected in an edentulous patient. However, if the value of having a dam in place during implant placement is important, one could consider providing a dental dam clamp anchor by temporarily placing orthodontic mini screws in suitable alveolar ridge locations.
As with all dental procedures, there are disadvantages as well as advantages. With a dental dam in place, the operator loses view of the entirety of the osseous structure revealed under the flap if a flap is used (although the view of the crestal region of the bone is enhanced via reduced ingress of saliva and blood into the surgical field) and loses the information about the position of the implant relative to the bucco-lingual width of the bone while progressing the osteotomy apically. The angulation of the alveolar housing, although often following the contour of the existing teeth, may be obscured when employing this clinical strategy. The use of a dental dam during implant placement could potentially lead to an altered view of critical anatomic landmarks and could lead to misangulation. Using guided surgery, employing the use of careful planning with CBCT, including adjacent teeth in dental dam isolation and other strategies to gain information about adjacent anatomic landmarks, can help facilitate the safe and predictable clinical use of a dental dam during implant placement.
While one would expect improved implant outcomes by reducing bacterial contamination with dental dam isolation, no study could be found addressing this issue. The value of reducing the risk of accidental swallowing/aspiration of small instruments can be recognised in that such events would open the dentist to performing litigation as well as dealing with the economic cost to resolve the acute and long-standing issues attributed to an accident. Recently, a patient sued her dentist after swallowing an untethered implant screwdriver that she was not able to regurgitate. In addition, the dentist failed to immediately refer the patient to a hospital emergency department, and subsequent surgery to remove it required a weeklong hospital stay (15). Treatment related to the aspiration or ingestion of a dental instrument can be very costly; therefore, increasing the use of dental dams should help prevent the untoward occurrence of aspirated or ingested instruments.
In response to the complaint that it is time-consuming to place a dental dam, Cragg pointed out that the most time-consuming aspect about the use of a dental dam is the amount of time necessary to convince dentists to use it (1). Many advantages exist, and this case report presents an example of its use during surgical endosseous implant placement. Preventing complications can best be accomplished with the routine use of a dental dam, but a throat screen when a dental dam is not possible and tethering floss through feasible dental instruments for retrieval if misplaced are alternative options.
Periapical radiographs are often exposed intraoperatively to assess the direction of the osteotomy procedure. Both the osteotomy depth and its mesio-distal angulation can be conveniently evaluated using periapical exposures, but the facio- lingual position of the implant is not adequately depicted on 2-dimensional periapical radiographs.
A postoperative CBCT scan was obtained to verify accurate alveolar bony housing of the implant. The value of postoperative CBCT scans must be weighed against the need to observe the principle of keeping the patient radiation dose “as low as reasonably achievable” (ALARA). This principle was part of the pre-treatment planning, and it was discussed with the patient.
CONCLUSION
Dental dam isolation during surgical implant placement provides a clean operating field, allowing clear visualisation of the crestal alveolar bone but not the entire alveolar housing of the implant, as mentioned previously, and prevented the gross ingress of saliva and bacteria into the surgical site that would otherwise contaminate the osteotomy site. It can also prevent the aspiration or ingestion of small instruments. Additional research is indicated to determine the biological benefits of the use of dental dams in surgical implant placement.
*Until recent decades, the dams were made from latex rubber, but in recent years, they have been made from non-latex vinyl to prevent latex allergy reactions and are now more accurately referred to as “dental dams.”
Footnotes
Ethical Approval: N/A.
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - T.S., L.B.; Design - T.S.; Supervision - T.S., L.B.; Resource - T.S., L.B.; Materials - T.S., L.B.; Data Collection and/or Processing - T.S.; Analysis and/or Interpretation - T.S., L.B.; Literature Search - T.S.; Writing - T.S., L.B.; Critical Reviews - T.S., L.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Cragg TK. The use of rubber dam in endodontics. J Can Dent Assoc. 1972;38(10):376–7. [PubMed] [Google Scholar]
- 2.American Association of Endodontists. AAE position statement:Dental dams. Available at:URL: www.aae.org 2010 .
- 3.Manchir M. AAE reminder:Dental dams help ensure patient safety. ADA News. 2015 May 18;:11. [Google Scholar]
- 4.Ahmad IA. Rubber dam usage for endodontic treatment:a review. Int Endod J. 2009;42(11):963–72. doi: 10.1111/j.1365-2591.2009.01623.x. [DOI] [PubMed] [Google Scholar]
- 5.Crawford JF, McQuistan MR, Williamson AE, Qian F, Potter KS. Should endodontists place dental implants? A national survey of general dentists. J Endod. 2011;37(10):1365–9. doi: 10.1016/j.joen.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Pingarrón Martín L, Morán Soto MJ, Sánchez Burgos R, Burgueño García M. Bronchial impaction of an implant screwdriver after accidental aspiration:report of a case and revision of the literature. Oral Maxillofac Surg. 2010;14(1):43–7. doi: 10.1007/s10006-009-0178-0. [DOI] [PubMed] [Google Scholar]
- 7.Zitzmann NU, Fried R, Elasser S, Marinello CP. The aspiration and swallowing of foreign bodies. The management of the aspiration or swallowing of foreign bodies during dental treatment. Schweiz Monatsschr Zahnmed. 2000;110(6):619–32. [PubMed] [Google Scholar]
- 8.Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965;20(3):340–9. doi: 10.1016/0030-4220(65)90166-0. [DOI] [PubMed] [Google Scholar]
- 9.Goldfein J, Speirs C, Finkelman M, Amato R. Rubber dam use during post placement influences the success of root canal-treated teeth. J Endod. 2013;39(12):1481–4. doi: 10.1016/j.joen.2013.07.036. [DOI] [PubMed] [Google Scholar]
- 10.Buddula A. Bacteria and dental implants:A review. J Dent Implants. 2013;3(1):58–61. [Google Scholar]
- 11.Hahnel S, Wieser A, Lang R, Rosentritt M. Biofilm formation on the surface of modern implant abutment materials. Clin Oral Implants Res. 2015;26(11):1297–301. doi: 10.1111/clr.12454. [DOI] [PubMed] [Google Scholar]
- 12.Lin PY, Huang SH, Chang HJ, Chi LY. The effect of rubber dam usage on the survival rate of teeth receiving initial root canal treatment:A nationwide population-based study. J Endod. 2014;40(11):1733–7. doi: 10.1016/j.joen.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Ireland EJ. The rubber dam - its advantages and application. Tex Dent J. 1962;80:10. [Google Scholar]
- 14.Brookman DJ. Vocational trainees'views of their undergraduate endodontic training and their vocational training experience. Int Endod J. 1991;24(4):178–86. doi: 10.1111/j.1365-2591.1991.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 15.Dental Tribune International. Dental patients receive $35 million in compensation. [Accessed July 22 2013]. Available at:URL: http://www.dentaltribune.com/articles/news/americas/13988_dental_patients_receive_35_million_in_compensation_ html .


