Abstract
Objective:
To evaluate the fracture resistance of different intra-radicular post systems in flared root canals.
Methods:
Sixty human canines were used. The coronal portion was removed and the root length was standardized at 17 mm. Canals were prepared and filled with gutta-percha/AH Plus sealer. Roots were embedded in self-polymerising acrylic resin blocks. According to the material used, the teeth were randomly divided into three groups (n=20): glass fibre post (GFP): GFP and Z350 resin composite core; pre-fabricated metal post (PMP): PMP and Z350 resin composite core; and cast metal core (CMC): CMC with silver-tin alloy. Coronal reconstruction involved fabrication of metal copings. Samples were submitted to mechanical compression testing at 45º in a universal test machine. Fracture pattern was evaluated under a stereoscope. The fracture strength values were submitted to one-way analysis of variance (ANOVA) and Tukey tests (α=0.05).
Results:
There was no statistically significant difference between the resistance values among groups (P=0.193). With regard to fracture pattern, GFP showed 55% and PMP 45% of Type I fractures, which considered repairable or favourable, whereas MCC presented 50% of Type V, which was considered irreparable or unfavourable.
Conclusion:
Glass fibre and pre-fabricated metal posts have good fracture resistance to compression and may be used for restoring flared root canals, since they presented fractures mainly involving the filling core, thus facilitating later repair.
Keywords: Endodontic post, endodontically treated teeth, fracture resistance, tooth preparation
HIGHLIGHTS.
In this study, no significant difference was observed in the fracture strength among the groups. This may be explained because of the use of flared root canals.
Glass fibre posts and pre-fabricated metal posts showed more reparable fractures compared to cast metal core posts, which allowed restoration of the teeth.
Glass fibre posts and pre-fabricated metal posts should be used in flared root canals.
INTRODUCTION
There are many options for reconstructing endodontically treated teeth; however, when the teeth are very fragile, it is difficult to decide which material should be used. This situation occurs with open apices, teeth that were prepared for previous post-retained restorations, inadequate post removal, fractures, or internal resorption. These flared root canals with thin dentine walls may require reinforcement and restoration using dentine bonding agents and composite, posts, and/or cores (1).
In cases where most of the coronal portion is lost, a common method to restore such teeth is the use of a post and core, onto which a full crown is cemented (2). The post functions primarily to aid the retention of the restoration and to protect the tooth by dissipating or distributing forces along the tooth (3).
The type of post to be used depends on various factors, including tooth location in the arch; root morphology; degree of tooth destruction; periodontal conditions; occlusal stress and opposing tooth (4). The post design and material; adhesion capacity of the cementing agent; coronal reconstruction material; crown material and aesthetics directly interfere with selecting the intra-radicular retention system (5).
There are two types of posts in use, the custom-made (such as cast metal posts) and pre-fabricated type. Pre-fabricated posts are usually made of metals, such as stainless steel, titanium and noble metal alloys, or they are non-metal types, such as ceramic and fibre posts.
Pre-fabricated metal posts (PMPs) have been used for restoring endodontically treated teeth. However, roots are prone to fracture with metal posts due to the high elastic modulus of metals compared with that of dentin (6). Glass fibre posts (GFPs) have anelasticity modulus similar to that of dentin, which allow more uniform stress absorption and distribution on the remaining root (5). Moreover, these posts are resistant to corrosion; have good tensile strength; are retentive due to their conformity and have shown favourable results relative to root fracture strength or more favourable fracture modes (7, 8).
Other benefits of GFPs are that they allow to prepare the intra-canal post space and perform post cementation in the same clinical session, because these procedures require no laboratory step, thereby reducing both working time and risk of root canal contamination (9).
However, cast metal post fabrication demands a minimum of two clinical consultations to perform post moulding, casting and then post cementation; in case of aesthetic rehabilitation, these posts may change the shade of the final restoration, either due to corrosion, or because they inherently form a dark background (10). They may also induce stress in the apical root third when lateral forces are exerted on the tooth, because their elasticity modulus is higher than that of dentin, thus leading to fracture (5).
The complex set of forces that are concentrated on intra-radicular posts inserted into endodontically treated teeth may contribute to the increased risk for vertical cracks and fractures, which are not only difficult to diagnose, but are irreparable and irreversible. They frequently lead to frustrated attempts to perform endodontic re-treatment and invariably lead to loss of the tooth (11).
Thus, the aim of this study was to evaluate the strength and failure pattern of structurally weakened roots, restored with different intra-radicular post systems.
MATERIALS AND METHODS
The present study complied with the rules and demands of the Research Ethics committee of Federal University of Juiz de Fora (Protocol 173.290). The 60 canines with similar coronal and radicular (diameter) measurements used in the study were donated by Federal University of Juiz de Fora.
Statistical analysis
The coronal portion of all the teeth was removed, and root canals were standardised to a length of 17 mm with a carborundum disc (Dentoruim, New York, USA)mounted in a straight hand piece (Kavo do Brasil IND, Santa Catarina, Brazil).
Subsequently, endodontic treatment was performed. The canals were instrumented with the rotary system Protaper Universal (Dentsply/Maillefer, Ballaigues, Switzerland). During instrumentation, the root canals were irrigated with 5.25% sodium hypochlorite solution (Fórmula&Ação, São Paulo, Brazil). The root canal filling was performed with M and MF gutta-percha cones (Dentsply/Maillefer, Ballaigues, Switzerland) and AH Plus sealer (Dentsply/Maillefer, Konstanz, Germany) using the thermomechanical condensation technique with Gutta Condensers #45 (Dentsply/Maillefer,Ballaigues, Switzerland). The teeth were stored in saline solution at 37ºC for 15 days.
After 15 days, the roots were fixed in a rigid structure to simulate their implantation in the alveolar bone. They were then covered with a layer of self-vulcanizing silicone (Polystic/Pulvitec, São Paulo, Brazil) sealing adhesive to obtain a space corresponding to that occupied by the periodontal ligament. Subsequently, the test specimens were fabricated by embedding the roots in a cylindrical polyvinyl chloride (PVC) ring, a round- shaped plastic tube, (Tigre, Rio Claro, São Paulo, Brazil) measuring three-fourth inches, with the use of self-polymerising acrylic resin (Jet, Classico Products Odontológicos, Rio de Janeiro, Brazil). To debilitate the roots, root preparation was performed with a diamond bur No.4137 (KG Sorensen, Cotia, Brazil) introduced up to the depth of 8 mm. Subsequently, the canals were unobstructed and prepared for intra-radicular retainer placement at a length of 11 mm, corresponding to two-third of the root canal length, and maintaining 6 mm of the remaining filling material (Fig. 1). After the flaring procedure, all roots had similar wall thickness (volume). The roots were measured in a coronal portion, in buccolingual and mesiodistal direction with a pachymeter.
Figure 1.
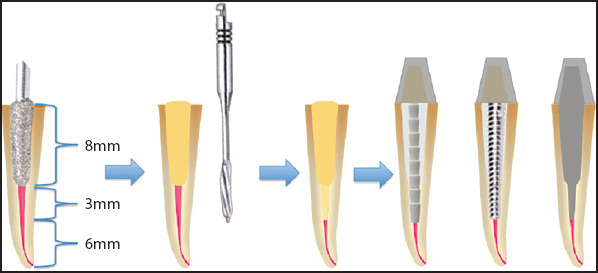
Schematic setup of sample preparation
The roots were then randomly divided into three groups (n=20) as follows:
Glass fibre post group
Root canals were prepared using Largo burs No. 1, 2 and 3 (Dentsply/Maillefer, Ballaigues, Switzerland) at a length of 11 mm. They were rinsed with water and the space was dried with paper points (Tanariman, Amazonas, Brazil).
For post treatment, the GFPs (# 2 Angelus, Londrina, Brazil) were cleaned with 70% ethanol. Subsequently, one layer of Monobond S (Ivoclar/Vivadent, Schaan, Liechtenstein) was applied and dried with air, according to the manufacturer’s recommendations.
Multilink N Primer A/B (Ivoclar /Vivadent, Schaan, Liechtenstein) was applied on the root canal surface for about 15 seconds using thin microbrushes and then dried with air. The excess material was removed from the canal with a paper point. The fibre post surface was coated with the mixed resin cement Multilink System Pack dispensed from the automix syringe, according to the manufacturer’s recommendations. The post was inserted into the root canal space at 11mm. Filling cores were fabricated using nanofilled resin composite Z350 (3M/ESPE, Sumaré, Brazil), with an acetate matrix obtained from the coronal portion of a pilot sample.
Pre-fabricated metal posts group
Root canal preparation was performed using a bur specifically for the post (Angelus, Londrina, Brazil) at a length of 11 mm.
Reforpost I metal (Angelus, Londrina, Brazil)posts with the dimensions of 11 mm of active partand 1.5 mm in diameter were used. Posts were cleaned with 70% ethanol and the Metal/Zirconia Primer (Ivoclar/Vivadent, Schaan, Liechtenstein) was applied on the post surface, waiting 3 minutes to allow it to set. The post was cemented with resin cement Multilink System Pack (Ivoclar/Vivadent, Schaan, Liechtenstein), as described for the GFP group.
Cast metal core group
The root canals were prepared using Largo burs No. 1, 2, and 3 (Dentsply/Maillefer, Ballaigues, Switzerland) at a length of 11 mm. The cores were modelled using the nucleojet kit (Angelus, Londrina, Brazil), pre-fabricated acrylic resin posts in radicular and coronal portion. The radicular portion was re-lined, and the coronal portion was standardised relative to size and diameter; the posts were then cast in a silver-tin alloy (80% silver, 1% copper and 19% tin; Maxally Matalms, Arujá, Brazil). The canals were cleaned and dried as described previously and the post was cemented using zinc phosphate (Lee Smith-Vigodent/Coltene, Rio de Janeiro, Brazil), thus concluding the post cementation procedure. This cement was used because it is indicated for CMC cementation.
For the reconstruction of the coronal portion in all the groups, the post preparation impressions were taken with composite resin, 3-dimensional addition silicon (Angelus, Londrina, Brazil) using the re-lining technique to obtain the dies. The casting pattern of the copings was constructed in wax and then casted with a nickel-chromium alloy. All the copings were cemented using zinc phosphate (Lee Smith-Vigodent/Coltene, Rio de Janeiro, Brazil), and a No.8 carbide bur (KG Sorensen, Cotia, Brazil) was used to make a niche in the cingulum region of the lingual surface for supporting the load of force during the test.
Fracture resistance test
To evaluate the fracture strength, the test specimens were submitted to the compressive load test in a universal test machine (EMIC DL 2000, São José dos Pinhais, Brazil) at an angle of 45° to the long axis of the roots, with constant force loading at a speed of 0.5 mm/min. The force required to cause fracture (rupture), recorded in units of kilogram/force (Kgf), was measured using a load cell of 500 N connected to Tesc Software version 3.04.
The fracture patterns were classified as proposed by Santos-Filho et al. (12): I- Fracture involving the filling core or intra-radicular retainer; II- Root canal fracture in the cervical third; III-Root canal fracture in the middle third; IV- Root canal fracture in the apical third; and V- Longitudinal root canal fracture.
Statistical analysis
The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) version 23.0 (IBM Corp.; Armonk, NY, USA) program at a 5% level of significance. The mean fracture resistance values were compared among the three groups using the one-way analysis of variance (ANOVA) associated with Tukey multiple comparison tests among the groups. However, the fracture types were described using descriptive frequency.
RESULTS
The mean and standard deviation of the fracture strength values are presented in Table 1. The statistical analysis of the data revealed no significant differences among the groups (P=0.193).
TABLE 1.
Fracture strength values (Kgf) of groups; Mean and (standard deviation)
GFP: glass fibre posts; PMP: pre-fabricated metal posts; CMC: cast metal core
Difference between the means was not statistically significant according to the one-way ANOVAand Tukey Tests (P>0.05)
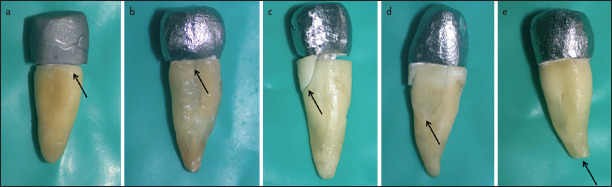
When the groups were compared with regard to the fracture type, it was observed that the CMC group presented 50% of Type V fracture, which was considered irreparable. However, the GFP and PMP groups predominantly presented Type I fractures (45% and 50%, respectively), that is, fractures involving the filling core or intra-radicular retainer, with the possibility of replacing the restoration without compromising the root. The distribution of the fracture types is described in Table 2. Figure 2 illustrates the fracture patterns.
TABLE 2.
Fracture pattern distribution of groups tested Fracture
| Fracture | ||||||
|---|---|---|---|---|---|---|
| Group*d | Type I | Type II | Type III | Type IV | Type V | Total |
| GFP | 11(55.0%) | 4 (20.0%) | 3 (15.0%) | 0 (0%) | 2 (10%) | 20 (100%) |
| PMP | 9 (45.0%) | 4 (20.0%) | 1 (5.0%) | 1 (5.0%) | 5 (25.0%) | 20 (100%) |
| CMC | 0 (0%) | 4 (20.0%) | 5 (25.0%) | 1 (5.0%) | 10 (50.0%) | 20 (100%) |
GFP: glass fibre posts; PMP: pre-fabricated metal posts; CMC: cast metal core
Figure 2.
(a-e) Photograph of each type of fracture classified; (a) fracture type I, (b) fracture type II, (c) fracture type IV and (e) fracture type V
DISCUSSION
Intra-radicular posts have been widely used to restore endodontically treated teeth with extensive loss of structure, such as an insufficient coronal remainder (13). Therefore, prosthetic restoration would be required with the use of this type of post to retain the restoration, and the choice of retainer is a decisive factor for successful treatment (7, 12, 13-15). The present study evaluated the strength and failure pattern of structurally weakened roots restored with different intra-radicular post systems.
CMPs were compared with pre-fabricated (metal and glass fibre) posts. Despite the advances in adhesive dentistry, the use of cast metal post is still a reality. They are indicated when the tooth has little or no coronal remainder to serve as a support for a prosthetic crown to be adapted on it (16).
GFPs have a modulus of elasticity similar to that of dentin that allows more uniform stress absorption and distribution on the remaining root (7). In this study, chemically activated Multilink System resin cement was used for cementing both GFPs and PMPs. This material was chosen because there was little passage of light into the interior of the canal, rendering the use of light-activated or dual polymerisation cements difficult. Furthermore, Uzun et al. (17) compared Multilink N with Maxcem Elite and Superbond C&B resin cements and observed that Multilink N showed the least void surface and volume. The authors associated the positive results with the use of the automix syringe (in comparison with hand mixing).
Post-related factors, such as diameter and material, may influence the fracture strength (6). In the present study, no significant difference was observed in the fracture strength among groups. The data are in agreement with those of Barcellos et al. (18) who observed statistically similar fracture strength values between GFPs and cast posts. In addition, other studies observed similar fracture loads between fibre posts and PMPs (3, 19, 20).
In this study, the CMC exhibited the lowest fracture resistance, which corroborates with that presented by Makade et al. (3). However, Makade et al. (3) found significant difference between CMC and PFP groups, unlike the present study. These differences can be explained because in the present study, the roots were already severely damaged during root preparation that it made no difference which type of post was inserted.
Relative to fracture mode, some studies showed less favourable fractures in the CMC post group fractures, because they involved a larger extent of root, while the fractures in the GFP and PFP groups involved the filling core and were capable of being restored again (1, 3, 18). This fact corroborated the findings of this study because in the CMC group, 80% of samples presented irreparable fractures. In the GFP group, 75% of fractures were reparable; and in the PMP group, 65% of fractures were reparable (limited to the cervical third).
Santos-Filho et al. (12) observed a large number of longitudinal fractures for CMC posts and few longitudinal fractures for GFP, because human teeth were used and all roots were also damaged during preparation. Santos-Filho et al. (12) used bovine teeth that were not damaged with burs during preparation.
For GFP, Jung et al. (6) observed that the fracture line was limited to the cervical third of the root, while fractures extending into the middle-third were found in the cast posts. These results partly corroborate the finding of this study, because the presence of longitudinal fractures in this study could be associated with the use of flared root canals.
The positive results for the GFP group relative to reparable fractures can be justified by the low modulus of elasticity similar to that of dentin, allowing deformation of the restorative complex similar to that of the healthy tooth, dissipating stresses throughout the entire restored tooth structure (7).
The use of crowns was a relevant factor with regard to the compression test. To evaluate the fracture strength of endodontically treated teeth, some laboratory trials have placed the action of the load directly on the post (6, 21, 22). However, the fabrication of crowns on filling cores may improve the distribution of forces (1, 21, 23,24). In this research, the authors fabricated and cemented metal Ni-Cr copings on all the test specimens to perform the mechanical test.
From the results presented in this study, the authors considered that it might be feasible to propose the use GFP and PMP cemented with chemically activated cement, as alternative procedures for restoring flared root canals because when compared with CMCs, the GFPs and PMPs showed statistically superior fracture mode results. Further clinical studies are necessary to confirm these findings.
The authors emphasize that when selecting the type of intra-radicular retainer system and material for cementation, it is important for clinicians to base themselves on technical and scientific knowledge of dental materials and carefully evaluate each case. Therefore, a balance must be sought between attaining ideal biomechanical characteristics and how to establish the aesthetics and function of the tooth.
Some factors, such as the lack of a standard root and structural differences in dentin; presence or absence of microcracks; and different degrees of tooth mineralization, imposed limitations on the study. In addition, methodology of this study did not simulate the clinical situation of cyclic forces and the presence of different angulated forces, especially in the lateral direction. In view of the foregoing, further studies simulating clinical conditions should be conducted.
CONCLUSION
The authors concluded that the compressive strength of the root was similar irrespective of the type of intra-radicular retainer used. However, in relation to the type of fracture, the cast metal cores (CMC) showed more type V fractures, which were considered irreparable and frequently led to loss of the tooth.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Ethical Approval: Ethics committee approval was received for this study from Federal University of Juiz de Fora (Decision No: 173.290).
Informed Consent: This work was done in vitro, no informed consent was necessary. The teeth were donated by Human Teeth Bank of Federal University of Juiz de Fora.
Peer-review: Externally peer-reviewed.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship Contributions: Concept – V.G., F.A., M.O., C.N.C.; Design – V.G., F.A., M.O., C.N.C.; Supervision – M.O., C.N.C.; Materials - V.G.; Data collection &/or processing – V.G., M.P., C.O.L.; Analysis and/or interpretation – M.P., C.O.L.; Literature search – M.P., C.O.L.; Writing – V.G., M.P., C.O.L.; Critical Reviews - M.P., C.O.L.
REFERENCES
- 1.Maccari PC, Cosme DC, Oshima HM, Burnett LH Jr, Shinkai RS. Fracture strength of endodontically treated teeth with flared root canals and restored with different post systems. J EsthetRestor Dent. 2007;19(1):30–6. doi: 10.1111/j.1708-8240.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- 2.Wadhwani KK, Jindal R, Shrivastava S, Nigam P. Comparative evaluation of fracture resistance of various post systems:An in vitro study. J Conserv Dent. 2003;6(2):56–61. [Google Scholar]
- 3.Mekade CS, Meshram GK, Warhadpande M, Patil PG. A comparative evaluation of fracture resistance of endodontically treated teeth restored with different post core systems - an in-vitro study. J AdvProsthodont. 2011;3(2):90–5. doi: 10.4047/jap.2011.3.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36(4):609–17. doi: 10.1016/j.joen.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Fernandes AS, Shetty S, Coutinho I. Factors determining post selection:a literature review. J ProsthetDent. 2003;90(6):556–62. doi: 10.1016/j.prosdent.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Jung SH, Min KS, Chang HS, Park SD, Kwon SN, Bae JM. Microleakage and fracture patterns of teeth restored with different posts under dynamic loading. J Prosthet Dent. 2007;98(4):270–6. doi: 10.1016/S0022-3913(07)60100-0. [DOI] [PubMed] [Google Scholar]
- 7.Dallari A, Rovatti L, Dallari B, Mason PN, Suh BI. Translucent quartz-fiber post luted in vivo with self-curing composite cement:case report and microscopic examination at a two-year clinical follow-up. J Adhes Dent. 2006;8(3):189–95. [PubMed] [Google Scholar]
- 8.Salameh Z, Sorrentino R, Papacchini F, Ounsi HF, Tashkandi E, Goracci C. et al. Fracture resistance and failure patterns of endodontically treated mandibular molars restored using resin composite with or without translucent glass fiber posts. J Endod. 2006;32(8):752–5. doi: 10.1016/j.joen.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Martelli HJr, Pellizzer EP, Rosa BT, Lopes MB, Gonini A Jr. Fracture resistance of structurally compromised root filled bovine teeth restored with accessory glass fibre posts. Int Endod J. 2008;41(8):685–92. doi: 10.1111/j.1365-2591.2008.01424.x. [DOI] [PubMed] [Google Scholar]
- 10.Torabi K, Fattahi F. Fracture resistance of endodontically treated teeth restored by different FRC posts:an in vitro study. Indian J Dent Res. 2009;20(3):282–7. doi: 10.4103/0970-9290.57359. [DOI] [PubMed] [Google Scholar]
- 11.Santos AF, Tanaka CB, Lima RG, Espósito CO, Ballester RY, Braga RR, et al. Vertical root fracture in upper premolars with endodontic posts:finite element analysis. J Endod. 2009;35(1):117–20. doi: 10.1016/j.joen.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 12.Santos-Filho PC, Castro CG, Silva GR, Campos RE, Soares CJ. Effects of post system and length on the strain and fracture resistance of root filled bovine teeth. Int Endod J. 2008;41(6):493–501. doi: 10.1111/j.1365-2591.2008.01383.x. [DOI] [PubMed] [Google Scholar]
- 13.Cailleteau JG, Rieger MR, Akin JE. A comparison of intracanal stresses in a post-restored tooth utilizing the finite element method. J Endod. 1992;18(11):540–4. doi: 10.1016/S0099-2399(06)81210-0. [DOI] [PubMed] [Google Scholar]
- 14.Adanir N, Belli S. Evaluation of different post lengths'effect on fracture resistance of a glass fiber post system. Eur J Dent. 2008;2(1):23–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Morgano SM, Milot P. Clinical success of cast metal posts and cores. J Prosthet Dent. 1993;70(1):11–6. doi: 10.1016/0022-3913(93)90030-r. [DOI] [PubMed] [Google Scholar]
- 16.Ferrari M, Vichi A, Grandini S, Goracci C. Efficacy of a self-curing adhesive-resin cement system on luting glass-fiber posts into root canals:an SEM investigation. Int J Prosthodont. 2001;14(6):543–9. [PubMed] [Google Scholar]
- 17.Uzun İ H, Malkoç MA, Keleş A, Öğreten AT. 3D micro-CT analysis of void formations and push-out bonding strength of resin cements used for fiber post cementation. J Adv Prosthodont. 2016;8(2):101–9. doi: 10.4047/jap.2016.8.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.BarcellosRR Correia DP, Farina AP, Mesquita MF, Ferraz CC, Cecchin D. Fracture resistance of endodontically treated teeth restored with intra-radicular post:the effects of post system and dentine thickness. J Biomech. 2013;46(15):2572–7. doi: 10.1016/j.jbiomech.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 19.Gu XH, Kern M. Fracture resistance of crowned incisors with different post systems and luting agents. J Oral Rehabil. 2006;33(12):918–23. doi: 10.1111/j.1365-2842.2006.01672.x. [DOI] [PubMed] [Google Scholar]
- 20.Chuang SF, Yaman P, Herrero A, Dennison JB, Chang CH. Influence of post material and length on endodontically treated incisors:an in vitro and finite element study. J Prosthet Dent. 2010;104(6):379–88. doi: 10.1016/S0022-3913(10)60171-0. [DOI] [PubMed] [Google Scholar]
- 21.Scotti R, Valandro LF, Galhano GA, Baldissara P, Bottino MA. Effect of post length on the fatigue resistance of bovine teeth restored with bonded fiber posts:a pilot study. Int J Prosthodont. 2006;19(5):504–6. [PubMed] [Google Scholar]
- 22.Costa RG, De Morais EC, Campos EA, Michel MD, Gonzaga CC, Correr GM. Customized fiber glass posts. Fatigue and fracture resistance. Am J Dent. 2012;25(1):35–8. [PubMed] [Google Scholar]
- 23.Bergoli CD, Amaral M, Boaro LC, Braga RR, Valandro LF. Fiber post cementation strategies:effect of mechanical cycling on push-out bond strength and cement polymerization stress. J Adhes Dent. 2012;14(5):471–8. doi: 10.3290/j.jad.a28389. [DOI] [PubMed] [Google Scholar]
- 24.Franco È B, Valle AL, Almeida ALPF, Ruba JH, Pereira JR. Fracture resistance of endodontically treated teeth restored with glass fiber posts of different lengths. J Prosthet Dent. 2014;111(1):30–4. doi: 10.1016/j.prosdent.2013.09.013. [DOI] [PubMed] [Google Scholar]