Abstract
Objective:
The purpose of this study was to assess the restorative choices for pulpal therapy by members of the Australian and New Zealand Society of Paediatric Dentistry (ANZSPD).
Methods:
Members of the ANZSPD were sent an online survey asking about the procedures that they performed and their choice of dental materials.
Results:
The respondents were 31 general dentists (GD) and 55 specialist paediatric dentists (PD). Materials used for indirect pulp capping included calcium hydroxide [Ca(OH)2] cement (CHC), glass ionomer cement or resin-modified glass ionomer cement (GIC/RMGIC), Ca(OH)2 paste (CHP) and mineral trioxide aggregate (MTA). Materials for direct pulp capping included MTA, CHP and CHC. Materials and techniques used for pulpotomy included MTA, ferric sulphate, formocresol and diathermy, CHP and CHC. GD and PD were similar in their choice of materials. However, there was no preferred product for pulp therapy. Most GD learnt how to use MTA from CPD lectures, while some PD learnt how to use MTA from their postgraduate training as well as CPD lectures. Many GD and PD did not have hands-on training from their education on how to use MTA (GD: 80%, PD: 43%). Most would like to attend hands-on MTA courses (GD: 86%, PD: 65%).
Conclusion:
There was no clear preferred product for the various types of pulp therapy in paediatric dentistry. Education appears to be the major barrier to the use of MTA rather than the cost of MTA.
Keywords: Calcium hydroxide, ferric sulphate, formocresol, glass ionomer cements, mineral trioxide aggregate, permanent teeth, primary teeth, pulp capping, pulpotomy
INTRODUCTION
Mineral trioxide aggregate (MTA) is a dental material that has been advocated for various paediatric dental indications such as vital pulp therapy and pulpotomy in primary and permanent teeth (1). When MTA is used in permanent teeth, there is a 97.6% success rate for direct pulp caps (DPCs) and a 79% success rate for pulpotomy (2, 3). In primary teeth, the corresponding success rates are 100% for DPCs (4) and 97% for pulpotomy (5). Despite these high success rates, MTA is not widely used. The high cost of the material is considered to be the major barrier to its use in clinical practice; however, it is also possible that lack of knowledge regarding how to use MTA could be another significant issue (6).
The extent of teaching regarding the use of MTA has been limited. In 2009, across the UK and Ireland, only 2 of 14 postgraduate paediatric dentistry departments taught the use of MTA for pulp therapy in primary molars (7). A similar study in the UK in 2005 involving 13 dental schools reported that calcium hydroxide [Ca(OH)2] was routinely used for pulp capping and ferric sulphate (FS) for pulpotomy, with only 1 school teaching the use of MTA as an alternative material (8). In Europe, the use of MTA is becoming more widespread as training regarding the use of the material has extended further. A 2013 survey of 29 postgraduate departments in Europe reported that 6 used MTA for pulp capping and 17 used MTA for pulpotomy (6).
There are no published data on the use of MTA in paediatric dentistry in Australia or New Zealand. Accordingly, the aim of the present study was to assess the use of MTA by members of the Australian and New Zealand Society of Paediatric Dentistry (ANZSPD). This society consists of both general dentists (GD) with an interest in paediatric dentistry and specialist paediatric dentists (PD). The study examined the choices of clinicians and assessed how well patterns of clinical use of MTA aligned with the scientific literature, focusing on pulp capping and pulpotomy, grouping both partial and complete pulpotomies into a single category.
MATERIALS AND METHODS
The national office of the ANZSPD distributed information regarding a survey to all society members on 28 November 2014, and this was followed by a reminder email sent on 15 April 2015. The survey was conducted online using www.surveymonkey. com. The final response was received on 21 May 2015.
The survey sought information from respondents on the following:
Whether the respondent was GD, PD, or a dentist undergoing specialty training in paediatric dentistry.
Material handling and placement preferences.
Education and training received on MTA.
Preferences for materials used for indirect pulp caps (IPCs), DPCs and pulpotomy in anterior and posterior primary and permanent teeth.
For each survey question, respondents were supplied with a menu of options, including an ‘other’ option to enable short written responses. If the ‘other’ was a listing of single responses, the first single response replaced their response. If the ‘other’ response was equivalent to another single response, their answer was grouped with that single response. The least popular responses (i.e. <10% of respondents or single unique responses) were grouped together under ‘other’.
For the purpose of the study, responses indicating the use of Biodentine (Septodont, Saint Maur des Fausses, France) or various commercial MTA products were grouped under the classification of MTA. A typical MTA cement contains Portland cement with a radiopaque additive, with the major ingredients of the Portland cement being calcium silicates and calcium aluminates (9). This has many similarities to the composition of Biodentine, which is primarily calcium silicates with a radiopacifier (10).
Differences in the patterns of responses between GD and PD were assessed according to their distribution frequency using Fisher’s exact test with GraphPad™ statistical software (http://graphpad.com/quickcalcs/catMenu/). P values of less than 0.05 were regarded as significant.
RESULTS
Respondent characteristics
A total of 103 of 280 members of the ANZSPD completed the survey, giving an overall response rate of 37%. As the respondents included 17 dental therapists, but none of these used MTA, there was no further analysis was conducted for this group. Responses from dentists undergoing specialty training in paediatric dentistry were grouped with those from specialist PD, giving 31 GD and 55 PD.
Overall, MTA was used by more PD than GD (69% vs. 35%). This difference was statistically significant (P<0.05). The choice of MTA product brand was similar in GD (64% ProRoot MTA, 36% MTA Angelus) and PD (70% ProRoot MTA, 27% MTA Angelus).
MTA usage
As illustrated in Table 1, most GD and PD preferred to permanently restore teeth immediately after MTA placement, while others waited for an arbitrary period of time and a minority placed a temporary restoration after MTA placement and then returned to permanently restore the tooth in a subsequent appointment.
TABLE 1.
MTA usage and training patterns of respondents
| GD | PD | |||
|---|---|---|---|---|
| n | % | n | % | |
| Do you use MTA or MTA like cements? | ||||
| Yes (*) | 11 | 35% | 37 | 69% |
| No | 20 | 65% | 17 | 31% |
| Which MTA do you use? | ||||
| ProRoot MTA | 7 | 64% | 26 | 70% |
| MTA Angelus | 4 | 36% | 10 | 27% |
| Other | 0 | 0% | 1 | >1% |
| After placing MTA how long do you wait before permanently restoring the tooth? | ||||
| Don’t wait | 1 | 20% | 8 | 47% |
| 5 minutes | 2 | 40% | 6 | 35% |
| 15 minutes | 0 | 0% | 1 | 6% |
| Temporise the tooth and restore another day Where do you store your MTA? In the refrigerator? | 2 | 40% | 2 | 12% |
| In the refrigerator | 0 | 0% | 3 | 19% |
| In the drawer | 5 | 100% | 13 | 81% |
| If you use ProRoot MTA, do you use the satchels for multiple applications? | ||||
| Yes | 2 | 50% | 5 | 71% |
| No | 2 | 50% | 2 | 29% |
| Where did you learn to use MTA? | ||||
| Training as a general dentist | 2 | 13% | 2 | 5% |
| Training as a specialist paediatric dentist (*) | 0 | 0% | 19 | 44% |
| Continuing education lectures (*) | 13 | 87% | 15 | 35% |
| Other | 0 | 0% | 7 | 16% |
| Did this education include a hands-on component with MTA or PC | ||||
| Yes (*) | 3 | 20% | 24 | 57% |
| No | 12 | 80% | 18 | 43% |
| Would you be interested in sitting hands on MTA courses? | ||||
| Yes | 18 | 86% | 32 | 65% |
| No | 3 | 14% | 17 | 35% |
Statistically significant difference between general dentists (GD) and paediatric dentists (PD), P<0.05.
Some respondents stored their MTA in the refrigerator and some used single-use satchels of ProRoot MTA for multiple applications. Both these actions are against the manufacturer’s instructions. Although minor differences existed between GD and PD for these aspects, these were not statistically significant.
Education on MTA usage
Attendance at continuing professional development (CPD) lectures was the major way in which GD had learnt how to use MTA (87%). This significantly differed for PD; nearly half (44%) learnt how to use MTA during their specialist training and only one-third (35%) learnt how to use MTA from CPD. The courses attended by GD rarely included hands-on training in the use of MTA (20%), while the specialist training of PD often included hands-on training in the use of MTA (57%). The majority of respondents in both the groups wanted to attend hands-on courses on the use of MTA (GD: 86%; PD: 65%).
The types of clinical procedures undertaken by respondents are shown in Figure 1 (indirect pulp capping), Figure 2 (direct pulp capping) and Figure 3 (pulpotomy).
Figure 1.
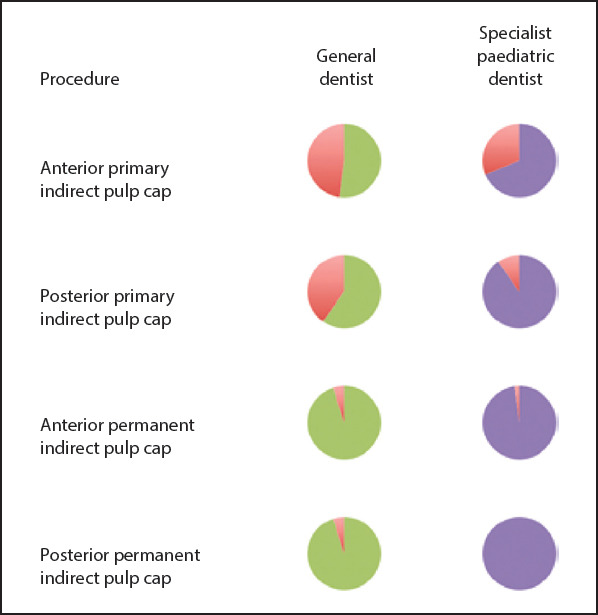
Proportions of clinicians who perform indirect pulp capping. Red segments show proportions of those who do not perform these procedures
Figure 2.
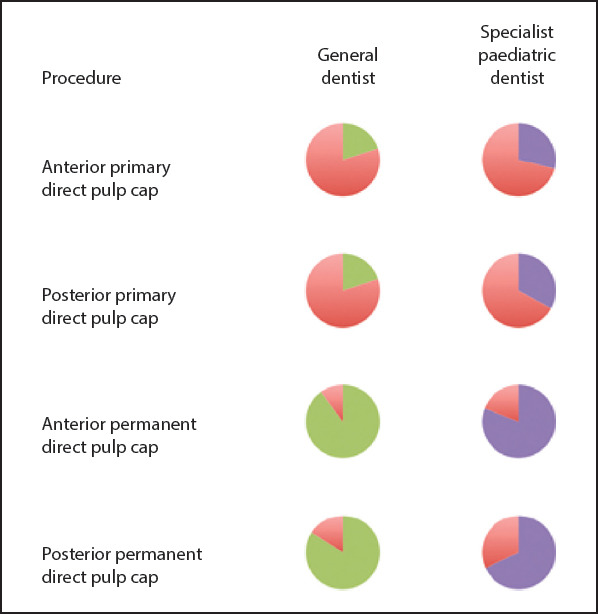
Proportions of clinicians who perform direct pulp capping. Red segments show proportions of those who do not perform these procedures
Figure 3.
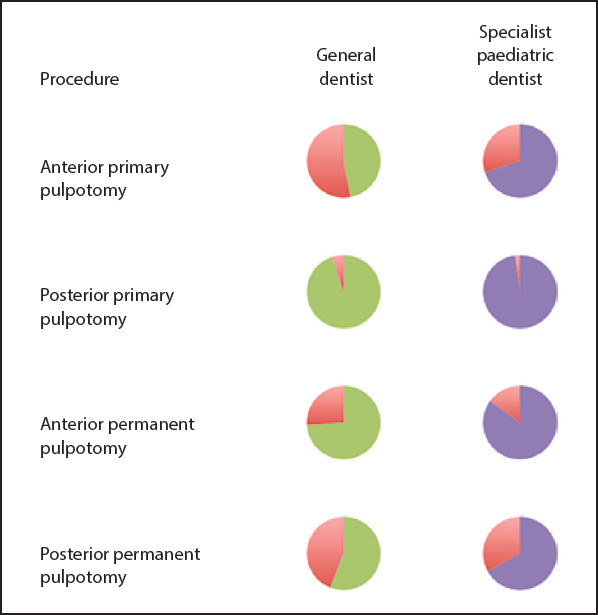
Proportions of clinicians who perform pulpotomy procedures. Red segments show proportions of those who do not perform these procedures
Indirect pulp capping (IPC)
Primary teeth
Popular choices for IPC were Ca(OH)2 cement (CHC) (GD: 45%; PD: 18%) and either glass ionomer cement or resin-modified glass ionomer cement (GIC/RMGIC) (GD: 45%; PD: 58%).
In case of posterior teeth, many clinicians preferred GIC/RMGIC (GD 50%; PD 65%) or CHC (GD: 42%; PD 9%) rather than MTA. Detailed results are presented in Table 2.
TABLE 2.
Preferred materials for indirect pulp capping (IPCs)
| GD | PD | |||
|---|---|---|---|---|
| n | % | n | % | |
| For IPCs in anterior primary teeth, what is your preferred material? | ||||
| GIC/RMGIC | 5 | 45% | 19 | 58% |
| Calcium hydroxide cements | 5 | 45% | 6 | 18% |
| Other | 1 | 9% | 8 | 24% |
| For IPCs in posterior primary teeth, what is your preferred material? | ||||
| GIC/RMGIC | 6 | 50% | 28 | 65% |
| Calcium hydroxide cements (*) | 5 | 42% | 4 | 9% |
| Other | 1 | 8% | 11 | 26% |
| For IPCs in anterior permanent teeth, what is your preferred material? | ||||
| GIC/RMGIC | 6 | 30% | 22 | 47% |
| Calcium hydroxide cements | 8 | 40% | 16 | 34% |
| Calcium hydroxide pastes | 4 | 20% | 4 | 9% |
| Other | 2 | 10% | 5 | 11% |
| For IPCs in posterior permanent teeth, what is your preferred material? | ||||
| Calcium hydroxide cements | 8 | 42% | 14 | 29% |
| GIC/RMGIC | 5 | 26% | 18 | 38% |
| MTA | 3 | 16% | 7 | 15% |
| Other | 3 | 16% | 9 | 19% |
Statistically significant difference between general dentists (GD) and paediatric dentists (PD), P<0.05
Permanent teeth
In case of anterior teeth, popular choices for IPC were CHC (GD: 40%; PD 34%), GIC/RMGIC (GD: 30%; PD: 47%) and Ca(OH)2 paste (CHP) (GD: 20%; PD: 9%) rather than MTA. Likewise, in case of posterior teeth, popular choices for IPC were CHC (GD: 42%; PD: 29%) and GIC/RMGIC (GD: 26%; PD 38%), followed by MTA (GD: 16%; PD: 15%) (Table 2).
Direct pulp capping (DPCs)
Primary teeth
In anterior teeth, the most common choice for DPC was MTA (GD: 50%; PD: 42%), and the same was observed for DPC in posterior teeth (GD: 50%; PD: 43%) (Table 3).
TABLE 3.
Preferred materials for direct pulp capping (DPCs)
| GD | PD | |||
|---|---|---|---|---|
| n | % | n | % | |
| For DPCs in anterior primary teeth, what is your preferred material? | ||||
| MTA | 2 | 50% | 5 | 42% |
| Other | 2 | 50% | 7 | 58% |
| For DPCs in posterior primary teeth, what is your preferred material? | ||||
| MTA | 2 | 50% | 6 | 43% |
| Other | 2 | 50% | 8 | 57% |
| For DPCs in anterior permanent teeth, what is your preferred material? | ||||
| Calcium hydroxide pastes | 6 | 33% | 20 | 51% |
| Calcium hydroxide cements | 8 | 44% | 9 | 23% |
| MTA | 3 | 17% | 7 | 18% |
| Other | 1 | 6% | 3 | 8% |
| For DPCs in posterior permanent teeth, what is your preferred material? | ||||
| MTA | 5 | 31% | 14 | 44% |
| Calcium hydroxide pastes | 4 | 25% | 10 | 31% |
| Calcium hydroxide cements | 7 | 44% | 5 | 16% |
| Other | 0 | 0% | 3 | 9% |
Permanent teeth
Popular choices for DPC in anterior teeth were CHC (GD: 44%; PD 23%) and CHP (GD: 33%, PD: 51%), followed by MTA (GD: 17%; PD: 18%). In contrast, in posterior teeth, the preferred material was CHC (GD: 44%; PD 16%), followed by MTA (GD: 31%; PD 44%) and CHP (GD 25%; PD: 31%) (Table 3).
Pulpotomy
Primary teeth
In anterior teeth, the most popular material for pulpotomy was FS (GD: 33%; PD: 45%), followed by MTA (GD: 33%; 26%), diathermy (GD: 11%; PD: 13%) and formocresol (FC) (GD: 11%, PD: 10%).
In posterior teeth, the most popular material was pulpotomy again FS (GD: 61%; PD: 36%), followed by MTA (GD: 11%; PD 40%) and FC (GD: 11%; PD: 11%) (Table 4).
TABLE 4.
Preferred materials for pulpotomies
| GD | PD | |||
|---|---|---|---|---|
| n | % | n | % | |
| For pulpotomies in anterior primary teeth, what is your preferred material? | ||||
| MTA | 3 | 33% | 8 | 26% |
| Ferric sulfate | 3 | 33% | 14 | 45% |
| Formocresol | 1 | 11% | 3 | 10% |
| Diathermy | 1 | 11% | 4 | 13% |
| Other | 1 | 11% | 2 | 6% |
| For pulpotomies in posterior primary teeth, what is your preferred material? | ||||
| MTA (*) | 2 | 11% | 18 | 40% |
| Ferric Sulfate | 11 | 61% | 16 | 36% |
| Formocresol | 2 | 11% | 5 | 11% |
| Diathermy | 1 | 6% | 4 | 9% |
| Other | 2 | 11% | 2 | 4% |
| For pulpotomies in anterior permanent teeth, what is your preferred material? | ||||
| MTA | 2 | 14% | 7 | 18% |
| Calcium hydroxide pastes | 8 | 57% | 21 | 54% |
| Calcium hydroxide cements | 3 | 21% | 7 | 18% |
| Other | 1 | 7% | 4 | 10% |
| For pulpotomies in posterior permanent teeth, what is your preferred material? | ||||
| MTA | 3 | 21% | 16 | 41% |
| Calcium hydroxide pastes | 6 | 43% | 7 | 18% |
| Other | 1 | 7% | 8 | 21% |
Statistically significant difference between general dentists (GD) and paediatric dentists (PD), P<0.05
Permanent teeth
In anterior permanent teeth, the most popular choice for pulpotomy was CHP (GD: 57%; PD: 54%), followed by CHC (GD: 21%; PD: 18%) and MTA (GD: 14%; PD: 18%). In contrast, in posterior permanent teeth, MTA was the most popular material for pulpotomy (GD: 21%; PD: 41%), followed by CHP (GD: 43%; PD: 18%) (Table 4).
DISCUSSION
Although literature shows that MTA is successful when used in various scenarios in restorative dentistry and endodontics, in Australia and New Zealand, this material is not used frequently in clinical practice (11). The results of the present study show that clinicians working with paediatric dental patients use a range of materials for pulp capping and pulpotomy procedures, with MTA not being used frequently for pulp capping and pulpotomy despite its suitability for these procedures. In Australia and New Zealand, MTA is mainly used as an apical barrier and this application is popular among GD treating adult patients and among endodontists (12). Notably, all the GD respondents in the present study are members of the ANZSPD and therefore have a special interest in paediatric dentistry. However, they may not be completely representative of the wider population of GD in Australia and New Zealand.
The literature often cites the high cost of MTA being a major barrier to its use in clinical practice despite a widely held view that for procedures such as direct pulp capping, it is the material of choice (6, 13-17). The mismatch between the evidence from the literature and the patterns of clinical practice suggests that there may be factors other than cost that influence the material selection by GD and PD. A recent survey of GD and endodontists in Australia and New Zealand showed that lack of education on the use of MTA was a greater barrier than the cost of MTA (12). This aligns with the observations of the present study, where education on MTA was desired by the majority of respondents. A further point supporting this is product brand selection.
In the dental market in Australia and New Zealand, there is a limited range of MTA products available; yet, clinicians most often used ProRoot MTA, which is the most expensive brand; this contradicts that cost has the strongest influence on the use of MTA. A preference to use ProRoot MTA has also been noted in other surveys on MTA product usage (6, 12). In the present study, CHC and glass ionomer cement were preferred over MTA for indirect pulp capping in both primary teeth and permanent teeth, which is in line with the evidence for effectiveness (18). In contrast, for direct pulp capping in primary teeth, MTA was the most popular material choice, even though this procedure was not performed commonly, even by specialists. The use of MTA for DPC is supported by clinical studies, which show success after 2 to 9 years of follow-up (2, 4).
For direct pulp capping in permanent teeth, clinicians used MTA, CHP or CHC. When considering clinical studies with a follow-up of at least 5 years as being sufficient to cover eventual pulpal necrosis, the selection of both MTA and CHP is supported in the literature (2, 19). There is, on the other hand, evidence for failure if CHC is used for direct pulp capping in permanent teeth (20). A study by Barthel et al. reported a 44.5% failure rate at 5 years and a 79.7% failure rate at 10 years (21). These results are in contrast to those for MTA in the same clinical situation, with 98% success at 9 years (2). Although studies that directly compare long-term clinical outcomes of direct pulp capping with MTA with those of direct pulp capping with CHC are lacking, a 2-year study reported 31.5% failure with CHC and only 19.7% failure with MTA (22).
In the present study, when direct pulp capping with MTA was performed in permanent teeth, there was a clear preference for MTA to be used less often in anterior teeth. This likely reflects concerns of tooth discolouration, particularly from the bismuth trioxide radiopacifier, which is problematic for teeth in the aesthetic zone. Instead, clinicians were choosing CHP, which avoids long-term staining problems. To date, there are limited data on outcomes from CHP versus MTA over the long term (23).
For pulpotomy in primary teeth, the clinicians in this survey preferred either FS or MTA. This finding agrees with that of a recent Cochrane review, in which similar successful clinical outcomes at 6 and 12 months were illustrated for both materials, with a trend for better outcomes for MTA at 2 years, although the difference was not statistically significant (24). It was surprising to find that some clinicians were still using FC for pulpotomy in primary teeth because this has become a very difficult dental material to obtain.
The need to use MTA in indirect pulp capping when managing vital teeth with deep carious lesions is limited because of the widespread use of alternatives such as glass ionomer cement. Selective caries excavation and a focus on sealing the margins are designed to reduce iatrogenic pulpal exposure during caries removal. Some infected carious dentine may intentionally be left, and this is then entombed using a well-sealed restoration (17). In the Hall technique, preformed metal crowns filled with viscous GIC are placed onto teeth without local anaesthesia and without caries removal or approximal enamel preparation (25).
In cases where the vitality of the coronal pulp is in question because of irreversible pulpitis, options include pulpotomy and pulpectomy, which can give respectable clinical success rates for pulpotomy (26). In the present study, in case of permanent anterior teeth, CHC and CHP were the most popular products for pulpotomy, while in case of posterior teeth, MTA was more popular, followed by CHP. This pattern of use aligns with evidence that supports the use of CHP for partial pulpotomy in permanent teeth, with a reported success rate of 93.5% over 4 years (27). There are similar reported success rates for CHP and MTA for partial pulpotomy, although the situation is less clear for complete pulpotomy because many studies do not clarify the type of Ca(OH)2 used (24, 28, 29). In the present study, the preference of CHP over MTA for pulpotomy in anterior teeth and the corresponding preference for MTA for pulpotomy in posterior teeth most likely reflects concerns regarding the discolouration of treated teeth rather than concerns regarding effectiveness (23).
CONCLUSION
The choices to use MTA and other dental materials were similar between GD and PD. There were situations in which MTA was not being used despite strong clinical evidence in the literature, and this reflects several factors including training, concerns regarding discolouration and relative cost. The expressed desire of clinicians to undergo further training in the use and handling of MTA suggests that lack of education and awareness remains the major obstacle to its wider use. The same lack of knowledge explains why some clinicians store MTA in an incorrect manner.
Acknowledgements:
The authors would like to thank the Members of the Australian and New Zealand Society of Paediatric Dentistry.
Footnotes
Ethical Approval: The authors declare that this article does not contain any studies with human participants and does not require ethics committee approval.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Authorship Contributions: Concept - R.Z.; Design - I.H.; Supervision - R.Z.; Materials - Z.S., T.T.; Data Collection and/or Processing - R.Z., T.T.; Analysis and/or Interpretation - R.Z.; Literature Review - T.T.; Writer - I.H.; Critical Review - R.Z., I.H.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review - Part III:Clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36(3):400–13. doi: 10.1016/j.joen.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Bogen G, Kim JS, Bakland LK. Direct pulp capping with mineral trioxide aggregate:an observational study. J Am Dent Assoc. 2008;139(3):305–15. doi: 10.14219/jada.archive.2008.0160. [DOI] [PubMed] [Google Scholar]
- 3.Witherspoon DE, Small JC, Harris GZ. Mineral trioxide aggregate pulpotomies:a case series outcomes assessment. J Am Dent Assoc. 2006;137(5):610–8. doi: 10.14219/jada.archive.2006.0256. [DOI] [PubMed] [Google Scholar]
- 4.Tuna D, Olmez A. Clinical long-term evaluation of MTA as a direct pulp capping material in primary teeth. Int Endod J. 2008;41(4):273–8. doi: 10.1111/j.1365-2591.2007.01339.x. [DOI] [PubMed] [Google Scholar]
- 5.Holan G, Eidelman E, Fuks AB. Long-term evaluation of pulpotomy in primary molars using mineral trioxide aggregate or formocresol. Pediatr Dent. 2005;27(2):129–36. [PubMed] [Google Scholar]
- 6.Foley JI. A pan-European comparison of the use of mineral trioxide aggregate (MTA) by postgraduates in paediatric dentistry. Eur Arch Paediatr Dent. 2013;14(2):113–6. doi: 10.1007/s40368-013-0018-7. [DOI] [PubMed] [Google Scholar]
- 7.Ni Chaollai A, Monteiro J, Duggal MS. The teaching of management of the pulp in primary molars in Europe:a preliminary investigation in Ireland and the UK. Eur Arch Paediatr Dent. 2009;10(2):98–103. doi: 10.1007/BF03321609. [DOI] [PubMed] [Google Scholar]
- 8.Pitt Ford T, Mannocci F, Woolford M. Survey on the teaching and use of mineral trioxide aggregate in UK dental schools. Eur J Dent Educ. 2007;11(3):155–9. doi: 10.1111/j.1600-0579.2007.00440.x. [DOI] [PubMed] [Google Scholar]
- 9.Torabinejad J, White DJ. Inventors;Tooth filling material and method of use. US patent publication US. 1995;5:415–547. [Google Scholar]
- 10.Malkondu Ö, Karapinar Kazandağ M, Kazazoğlu E. A review on biodentine, a contemporary dentine replacement and repair material. Biomed Res Int. 2014;2014:160951. doi: 10.1155/2014/160951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srinivasan V, Waterhouse P, Whitworth J. Mineral trioxide aggregate in paediatric dentistry. Int J Paediatr Dent. 2009;19(1):34–47. doi: 10.1111/j.1365-263X.2008.00959.x. [DOI] [PubMed] [Google Scholar]
- 12.Ha WN, Duckmanton P, Kahler B, Walsh LJ. A survey of various endodontic procedures related to mineral trioxide aggregate usage by members of the Australian Society of Endodontology. Aust Endod J. 2016;42(3):132–8. doi: 10.1111/aej.12170. [DOI] [PubMed] [Google Scholar]
- 13.Seale NS, Glickman GN. Contemporary perspectives on vital pulp therapy:views from the endodontists and pediatric dentists. J Endod. 2008;34:S57–61. doi: 10.1016/j.joen.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 14.Mooney GC, North S. The current opinions and use of MTA for apical barrier formation of non-vital immature permanent incisors by consultants in paediatric dentistry in the UK. Dent Traumatol. 2008;24(1):65–9. doi: 10.1111/j.1600-9657.2006.00495.x. [DOI] [PubMed] [Google Scholar]
- 15.Schwendicke F, Brouwer F, Stolpe M. Calcium hydroxide versus mineral trioxide aggregate for direct pulp capping:A cost-effectiveness analysis. J Endod. 2015;41(12):1969–74. doi: 10.1016/j.joen.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 16.Friedlander L, McElroy K, Daniel B, Cullinan M, Hanlin S. Direct pulp capping of permanent teeth in New Zealand general dental practice--a practice based research study. N Z Dent J. 2015;111(2):58–64. [PubMed] [Google Scholar]
- 17.Seale NS, Glickman GN. Contemporary perspectives on vital pulp therapy:views from the endodontists and pediatric dentists. Pediatr Dent. 2008;30(3):261–7. [PubMed] [Google Scholar]
- 18.Marchi JJ, de Araujo FB, Fröner AM, Straffon LH, Nör JE. Indirect pulp capping in the primary dentition:a 4 year follow-up study. J Clin Pediatr Dent. 2006;31(2):68–71. doi: 10.17796/jcpd.31.2.y4um5076341226m5. [DOI] [PubMed] [Google Scholar]
- 19.Miyashita H, Worthington HV, Qualtrough A, Plasschaert A. Pulp management for caries in adults:maintaining pulp vitality. Cochrane Database Syst Rev. 2007:CD004484. doi: 10.1002/14651858.CD004484.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Dammaschke T, Leidinger J, Schäfer E. Long-term evaluation of direct pulp capping--treatment outcomes over an average period of 6.1 years. Clin Oral Investig. 2010;14(5):559–67. doi: 10.1007/s00784-009-0326-9. [DOI] [PubMed] [Google Scholar]
- 21.Barthel CR, Rosenkranz B, Leuenberg A, Roulet JF. Pulp capping of carious exposures:treatment outcome after 5 and 10 years:a retrospective study. J Endod. 2000;26(9):525–8. doi: 10.1097/00004770-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Hilton TJ, Ferracane JL, Mancl L. Northwest Practice-based Research Collaborative in Evidence-based Dentistry (NWP). Comparison of CaOH with MTA for direct pulp capping:a PBRN randomized clinical trial. J Dent Res. 2013;92:16S–22S. doi: 10.1177/0022034513484336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Belobrov I, Parashos P. Treatment of tooth discoloration after the use of white mineral trioxide aggregate. J Endod. 2011;37(7):1017–20. doi: 10.1016/j.joen.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Smaïl-Faugeron V, Courson F, Durieux P, Muller-Bolla M, Glenny AM, Fron Chabouis H. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst Rev. 2014:CD003220. doi: 10.1002/14651858.CD003220.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Innes NP, Evans DJ, Stirrups DR. The Hall Technique;a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice:acceptability of the technique and outcomes at 23 months. BMC Oral Health. 2007;7:18. doi: 10.1186/1472-6831-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barja-Fidalgo F, Moutinho-Ribeiro M, Oliveira MA, de Oliveira BH. A systematic review of root canal filling materials for deciduous teeth:is there an alternative for zinc oxide-eugenol? ISRN dent. 2011;2011:367318. doi: 10.5402/2011/367318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mejare I, Cvek M. Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol. 1993;9(6):238–42. doi: 10.1111/j.1600-9657.1993.tb00279.x. [DOI] [PubMed] [Google Scholar]
- 28.Qudeimat MA, Barrieshi-Nusair KM, Owais AI. Calcium hydroxide vs mineral trioxide aggregates for partial pulpotomy of permanent molars with deep caries. Eur Arch Paediatr Dent. 2007;8(2):99–104. doi: 10.1007/BF03262577. [DOI] [PubMed] [Google Scholar]
- 29.Fong CD, Davis MJ. Partial pulpotomy for immature permanent teeth, its present and future. Pediatr Dent. 2002;24(1):29–32. [PubMed] [Google Scholar]


