Abstract
A Spigelian hernia is a rare hernia, making up approximately 0.1% of all abdominal wall hernias. This hernia goes through a defect in the Spigelian fascia which is the part of the transversus abdominis aponeurosis lateral to the rectus muscle, often at the level of the arcuate line, where the fascia is widest and weakest. Clinical diagnosis is difficult in patients without obvious abdominal mass but imaging can be a valuable adjunct in diagnosis.
We report the case of a 64-year-old male who presented to our hospital with small bowel obstruction secondary to an incarcerated Spigelian hernia who was pre-operatively diagnosed with ultrasound and computed tomography. At ultrasound and computed tomography a closed loop obstruction in a Spigelian Hernia was detected, resembling on both imaging modalities a “bulb-like“ appearance.
Keywords: Spigelian hernia, Small bowel obstruction, Incarceration, Ultrasound, CT
Introduction
Spigelian hernia is a type of interparietal abdominal wall hernia which is usually present at the level of the arcuate line in the area of “Spigelian belt.” It is also known as “spontaneous lateral ventral hernia” or “hernia of semilunar line.” Patients may present with a palpable lump with the classical findings of a hernia. In this case, the diagnosis is relatively straightforward. However, a number of patients present with no obvious hernia but a vague lump or tenderness along the region of the Spigelian fascia. However, in many cases incarceration or strangulation is the first clinical sign. In emergency settings, a number of radiological investigations have been used to diagnose Spigelian hernias. Ultrasonography has been shown to offer an accurate evaluation of suspected Spigelian hernias, it offers a noninvasive and dynamic assessment of soft tissues. Computed tomography (CT) has also been has also been shown to be of value in the diagnosis of Spigelian hernias. However, CT is associated with a radiation exposure, which limits its role as a first line imaging modality for noncomplicated hernia [1]. Small bowel obstruction in incarcerated Spigelian hernia is a rare event [2]. We present a rare case of an incarcerated Spigelian hernia causing a closed loop small bowel obstruction in a 64-year-old man presenting with nausea, vomiting, and abdominal pain that was preoperatively diagnosed with ultrasound (US) and CT. At US and CT a closed loop obstruction in a Spigelian hernia was detected, resembling on both imaging modalities a “bulb-like“ appearance.
Case summary
A 64-year-old male patient, affected by a severe form of Alzheimer's disease since age 52, presented at our Emergency Department complaining of 2 days history of nausea, vomiting, and abdominal pain. Clinical examination and anamnesis gathering were difficult given the compromised neurological status and required the patient's relatives. The patient reported a medical history of appendicectomy at the age of 18, diabetes mellitus and coronary artery disease, that required a left anterior descending artery stenting procedure almost a decade before. Prolonged use of laxatives was referred by the relatives. Physical examination of the patient revealed a nondistended abdomen with a palpable swelling in the right lower quadrant with mild tenderness to palpation. There was no rebound or guarding. Physical examination was otherwise unremarkable. A likely clinical diagnosis of incarcerated Spigelian hernia was formulated. The surgeon tried to reduce the hernia manually and the patient underwent clinical observation, but there were no signs of relief of symptoms. Laboratory findings documented neutrophilic leukocytosis and lymphocytopenia with no other remarkable findings. Arterial pressure, body temperature, heart rate, and blood oxygen saturation were within the normal range, the patient was afebrile.
Imaging findings and diagnosis
US and CT with intravenous contrast administration were performed.
US scans showed a breach, located along the linea semilunaris, of about 20 mm in maximum width and a hernial sac, containing a “bulb-like” multilayered image (Fig. 1). Small bowel loops were clearly visible through the defect and looping inside the hernial sac, resembling a close loop obstruction, with a “double beak sign” with tapering of bowel loops at the point of obstruction. Although the bowel loop was clearly incarcerated, the caliber was normal (<2.5 cm) and peristalsis was present but decreased. Within the incarcerated bowel loop, a hyperechoic layer of mesenteric fat was clearly visible, whereas a slightly disomogenous hypoechoic fluid collection was detected around the incarcerated bowel loop. This multilayered appearance resembles a “bulb-like” image. Further abdominal scans revealed distension of small bowel loops in proximity of the wall defect, with a maximum diameter >2,5 mm (30 mm, outer caliber measured on long axis) and decreased peristalsis (Fig. 2). No intrabdominal free fluid collections were documented. CT with intravenous contrast (Figs. 3a-c) confirmed the herniation of a small bowel loop through a 20 mm transversus muscle aponeurosis breach (measured on axial scans), located on the lateral margin of the right rectus muscle, close to the level of the arcuate line. The hernial content included bowel loops, mesentery, omental tissue and fluid. Both the afferent and efferent trapped loops were clearly visible on the CT scan (Fig. 3b), showing an image overlapping those obtained from the US scans, with a hypodense central layer determined by the presence of mesentery, and a mildly hypodense free fluid in the hernia sac, around the bowel loops (Fig. 3a). The herniated bowel loops were fluid filled, normal in caliber, and presented thinned walls with no signs of hypoperfusion. Mildly dilated afferent small bowel loops, were detected intrabadominally in proximity of the defect. CT confirmed the US diagnosis of mechanical small bowel obstruction due to incarcerated bowel loop in a Spigelian hernia, and consequently, due to the failure of conservative treatment, the patient underwent surgery. Intraoperatively the herniated content visualized at imaging was confirmed, including partial necrosis of the omentum and serum-blood fluid in the hernia sac. The sac was manually reduced and a polypropylene mesh was fixed, bridging the defect. The postoperative period showed no complications or major event and the patient was discharged 4 days later.
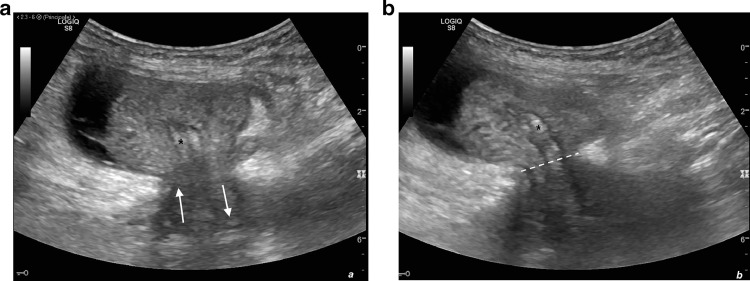
Fig. 1.
(a, b). Sonographic view of the right lower quadrant of the abdomen showing the interruption in the inferior margin of the spigelian fascia, the hernial defect is clearly visible (spotted line). Axial scan of the hernial sac, obtained in supine position, shows the “bulb-like” image determined by the presence of both the afferent and efferent loop (white arrows) tapered at the point of obstruction, the hyperechoic mesenteric and omental fat (*) and the inhomogeneous hypoechoic fluid collection (black arrow).
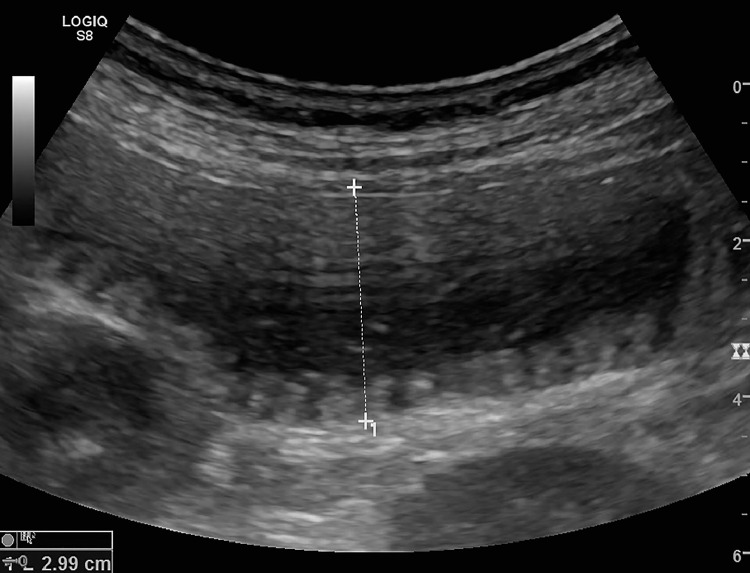
Fig. 2.
Sonographic view of the right lower quadrant of the abdomen, showing a dilated, hypokinetic, fluid-filled small bowel loop. Outer caliber, measured from wall to wall, was >25 mm.
Fig. 3.

(a, b). Axial (a) and sagittal MPR reconstruction (b) contrast enhanced CT shows a right-sided lower quadrant interstitial Spigelian hernia, through a 20-mm defect located between the rectus muscle and oblique muscles, superficially covered by external oblique aponeurosis and subcutaneous/cutaneous tissues. Inside the hernial sac the “bulb” (white arrow) is composed by hypodense mesenteric and omental fat and the small bowel loops, creating a multilayered image overlapping US findings. The mildly hypodense free fluid collection is visible around the loops.
Discussion
Spigelian hernia, also known as lateral ventral hernia, represents less than 1% of all abdominal wall hernias.
It shows no difference in gender distribution with higher incidence in the 5th-6th decade of life. It is usually unilateral, mostly affecting the left side [3], although other authors report the right side as the most frequent location [4]. Risk factors include multiple pregnancies, obesity, chronic cough, constipation, and sudden weigh loss [3].
The hernial defect can be congenital or acquired and it is located in the Spigelian fascia, part of the transversus abdominis muscle aponeurosis limited by the linea semilunaris laterally, which marks the transition between the aponeurotic to the muscular part of the transversus muscle, and the lateral edge of the rectus muscles medially. More than 90% of Spigelian hernias occur in the so called “Spigelian belt,” a 6-cm-wide area of the aponeurosis lying above the interspinal plane [5,6].
The intersection of the linea semilunaris and linea arcuata creates a physiological “weak spot,” determined by the absence, anteriorly, of the external oblique aponeurosis, while the cranial two thirds of the linea semilunaris are posteriorly reinforced by the muscular part of the transversus abdominis muscle that in the upper abdomen reaches almost the midline. It often starts as a protrusion of preperitoneal fat but common sac content includes greater omentum, small intestine or parts of the colon. A case where part of the sac is formed by the urinary bladder has been reported at least once [4]. There are two main hernia subtypes, interstitial if still covered by external oblique and subcutaneous if superficial [7]. Clinical examination forms the mainstay of diagnosis [8], although Spigelian hernias are elusive, sometimes concealed by the superficial layers, mostly in presence of obesity, pain, and scars [9].
The presence of a localized area of swelling or tenderness at palpation along the linea semilunaris can be decisive, considering that the great majority of patients are asymptomatic [1]. Clinical onset can be acute or chronic. In the first case, acute abdomen may be the main sign of complications, often requiring urgent investigation and surgery [10]. Chronic onset shows no characteristic or pathognomonic signs or symptoms. Noncomplicated hernias can cause a vague abdominal discomfort or bowel dysfunction as the only appreciable symptoms in often incidental diagnosis [2]. Imaging procedures such as US and CT are nowadays routinely used and integrated to diagnose bowel emergencies, including herniations [9]. The role of imaging is much important if the hernia is clinically occult [1] and in diagnosing complications such as incarceration, obstruction, strangulation and content necrosis, conditions that often require prompt surgical intervention.
Traditional radiological exams such as herniography are nowadays obsolete and not performed anymore. Ultrasonography can be diagnostic in the diagnosis of Spigelian hernia. Its advantages comprehend being a noninvasive, low cost, and widely spread methodic than can be performed in physiological positions such as supine or upright position, during Valsava maneuver or even bedside, and safely repeated after manual reduction. Sonographic findings of small bowel obstruction are represented by the presence of dilated small bowel loops >25 mm in outer caliber, abnormal peristalsis, parietal and valvulae conniventes bowel modifications and the presence of free abdominal fluid. US in the diagnosis of small bowel obstruction can speed up the management of patients and help in determining the correct timing of surgery [11].
There are no specific signs for detecting bowel vascular damage on US scans. This limit, and its consequences concerning the choice between surgical and conservative treatment most often leads to necessity of performing CT [11].
CT with its panoramic view and superior anatomical detail, is the most reliable method [9,10] in the diagnosis of SBO (small bowel obstruction), determining the cause, the level and the presence of vascular damage of bowel parietal wall. It can confirm US findings, integrate them or being a valid alternative in case of obese patients [9].
In our case, the “bulb-like appearance” of the incarcerated bowel loop in Spigelian hernia was detected on both US and CT, determined from the inner to the outer layer by the mesenteric fat (hyperechoic at US, hypodense at CT), the incarcerated bowel loop with a “double beak sign” with tapering of bowel loops at the point of obstruction (normal in caliber, fluid filled, hypoechoic at US, hypodense at CT), and the outer layer represented by inhomogeneous free fluid. On the other hand, each modality has its own capability, at US the real-time evaluation detected the presence of peristalsis in the incarcerated bowel loop, while CT determined the absence of vascular damage. In both case, the free fluid presented inhomogeneous characteristic that resulted at surgery in serum-blood fluid due to omental necrosis.
Conclusion
A complicated obstructed Spigelian hernia is an uncommon diagnosis. It is unusual to find mesentery of the small-bowel being incarcerated in this hernial defect leading to acute small-bowel obstruction. Nowadays small bowel obstruction is diagnosed with high accuracy with multimodality imaging US-CT, although US cannot always define the cause and determine the presence of vascular bowel parietal damage. In an emergency setting, reduction of the hernia is usually sufficient if the bowel loops appear viable. Post reduction and follow-up US scan confirms the diagnosis. In our case the manual reduction's failure detected at US, was confirmed at CT. The “bulb-like “appearance of the incarcerated hernia was equally detected at US and CT, confirming the emerging role of ultrasound in the diagnosis of small bowel obstruction but also the importance of the multimodality imaging and integration of each modality findings for a correct and accurate diagnosis.
References
- 1.Light D., Chattopadhyay D., Bawa S. Radiological and clinical examination in the diagnosis of Spigelian hernias. Ann R Coll Surg Engl. 2013;95:98–100. doi: 10.1308/003588413x13511609957092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lavin A., Gupta A., Lopez-Viego M., Buicko J.L. Incarcerated Spigelian hernias: a rare cause of a high-grade small bowel obstruction. Cureus. 2020;12:e7397. doi: 10.7759/cureus.7397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicolas G., Emmanuel N., Charbel C., Awdeh A., Bitar B., Abourafeh S.S. An unusual case of left spigelian hernia containing part of a fibroid uterus and the left adnexa in a 66-year-old woman. Am J Case Rep United States. 2019:1643–1647. doi: 10.12659/AJCR.917104. [DOI] [PubMed] [Google Scholar]
- 4.Igwe P.O., Ibrahim N.A. Strangulated sliding spigelian hernia: a case report. Int J Surg Case Rep. 2018;53:475–478. doi: 10.1016/j.ijscr.2018.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spangen L. Spigelian hernia. Surg Clin North Am. 1984;64:351–366. doi: 10.1016/s0039-6109(16)43290-1. [DOI] [PubMed] [Google Scholar]
- 6.Skandalakis P.N., Zoras O., Skandalakis J.E., Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72:42–48. [PubMed] [Google Scholar]
- 7.Serrado M.A., Dutra S., Barros J.M. An unusual case of right lower quadrant pain: Spigelian hernia. Eurorad. 2017 doi: 10.1594/EURORAD/CASE.144465. [DOI] [Google Scholar]
- 8.Montes I.S., Deysine M. Spigelian and other uncommon hernia repairs. Surg Clin North Am. 2003;83:1235–1253. doi: 10.1016/s0039-6109(03)00130-0. viii. [DOI] [PubMed] [Google Scholar]
- 9.Lassandro F., Iasiello F., Pizza N.L., Valente T., Stefano M.L., Grassi R. Abdominal hernias: radiological features. World J Gastrointest Endosc. 2011;3:110–117. doi: 10.4253/wjge.v3.i6.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mittal T., Kumar V., Khullar R., Sharma A., Soni V., Baijal M. Diagnosis and management of Spigelian hernia: a review of literature and our experience. J Minim Access Surg. 2008;4:95–98. doi: 10.4103/0972-9941.45204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tamburrini S., Lugarà M., Iaselli F., Saturnino P.P., Liguori C., Carbone R. Diagnostic accuracy of ultrasound in the diagnosis of small bowel obstruction. Diagnostics (Basel) 2019;9 doi: 10.3390/diagnostics9030088. [DOI] [PMC free article] [PubMed] [Google Scholar]