Abstract
Objectives
Adenomyosis is a common and refractory disease in gynecology. Preserving the uterus during treatment for adenomyosis remains a problem. High-intensity focused ultrasound (HIFU) is widely used in treatment of solid tumors. This study aimed to analyze patients with adenomyosis who were treated by HIFU and to preliminarily examine the characteristics of patients who are more suitable for HIFU to treat adenomyosis with reliable efficacy.
Methods
Over 2 years, 67 women who were diagnosed with adenomyosis and treated with HIFU at our gynecology department were included in this study. We investigated outcomes of their symptoms (dysmenorrhea and hypermenorrhea) and the volume of their uterine lesions. We also compared the patients’ clinical profiles.
Results
The women had a mean follow-up duration of 11.6 ± 0.46 months. In the numerical rating scale, used to assess the degree of dysmenorrhea, the score was significantly lower (mean difference: −1.94, 95% confidence interval: −2.704 to −1.176) 3 months after HIFU treatment compared with before treatment, then it remained stable for 3 to 12 months. Hypermenorrhea was reduced to a certain degree, with a mean difference of −0.54 (−1.01–0.02).
Conclusions
HIFU is a new noninvasive treatment method for adenomyosis that may help relieve dysmenorrhea.
Keywords: Adenomyosis, high-intensity focused ultrasound, dysmenorrhea, hypermenorrhea, uterus, lesion
Introduction
Adenomyosis is a disease of the endometrium, including the glands and interstitium. Adenomyosis invades the uterine muscle and is accompanied by compensatory hypertrophy and hyperplasia of peripheral myocytes.1 Adenomyosis frequently occurs in women of reproductive age. Approximately two thirds of women with this disease are symptomatic with hypermenorrhea and dysmenorrhea.2 Adenomyosis has a major adverse effect on quality of life, causing pain and subfertility. Historically, hysterectomy is considered the definitive treatment for adenomyosis. However, for women who wish to preserve their uterus, there is a lack of effective treatments involving conservative therapies. Clinical studies have shown that hormonal medications and the levonorgestrel-releasing intrauterine system (LNG-IUS) alleviate the symptoms of adenomyosis, but relapse can occur.3,4 Previous small-sample studies have reported that high-intensity focused ultrasound (HIFU) is a safe and effective treatment for adenomyosis,5–10 but without long-term relief of clinical symptoms. However, the literature is inconclusive regarding the benefits of HIFU. Therefore, further evaluation of the therapeutic efficacy of HIFU is required to identify patients with adenomyosis who may benefit from treatment. This study aimed to analyze patients with adenomyosis who were treated by HIFU and to preliminarily investigate the characteristics of patients who are more suitable for HIFU for treating adenomyosis with reliable efficacy.
Methods
Patients
The Ethics Committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University (approval number: 753 [2020]) approved this study. Written informed consent was obtained from each patient. Patients who were diagnosed with adenomyosis by magnetic resonance imaging (MRI) and had typical symptoms, such as dysmenorrhea and/or menorrhagia, and were treated at the Gynecology Department (Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China) from May 2015 to May 2017 were included in this single-institution study.
Inclusion criteria were as follows: all patients (1) had menorrhagia and/or dysmenorrhea, (2) received HIFU therapy, (3) had no serious systemic diseases, and (4) could communicate clearly with a nurse or physician during the duration of treatment and follow-up. Exclusion criteria were as follows: patients (1) with adenomyotic lesions that could not be visualized; (2) those who were pregnant, lactating, or menopausal; (3) those with suspected or confirmed uterine malignancy; and (4) those with contraindications to magnetic resonance imaging.
Endpoints and evaluation
The outcome was the level of dysmenorrhea and hypermenorrhea. The intensity of dysmenorrhea was assessed by a numerical rating scale (NRS) score ranging from 0 to 10. A score of 1 to 3 indicated mild pain, 4 to 6 indicated moderate pain, and 7 to 10 indicated severe pain. Hypermenorrhea was defined as a period of menstrual flow for more than 7 days, with a hemoglobin level <100 g/L and anemia.11 Hypermenorrhea was graded on a 5-point scale (FPS) on the basis of the duration of menses and the degree of anemia as follows: 0, no anemia and menses for <4 days; 1, no anemia and menses for 4 to 7 days; 2, no anemia and menses for >1 week; 3, anemia and menses for <4 days; 4, anemia and menses for 4 to 7 days; and 5, anemia and menses for >7 days. The volume of uterine lesions was evaluated by examination of pelvic MRI. The uterus and targeted lesions were measured in three dimensions of longitudinal (D1), anteroposterior (D2), and axial (D3). The volume was calculated using the following equation: V = 0.5233 × D1 × D2 × D3.11
HIFU treatment
A PRO-2008 focused ultrasound ablation machine (Shenzhen Prohuiren Medical Technology Co., Ltd., Shenzhen, China) was used to perform the HIFU ablations in this study. This equipment consisted of an ultrasonic treatment system, a vacuum water treatment system, a central treatment system, and an ultrasonic diagnostic unit, including a central ultrasound diagnostic probe and an adjacent ultrasound therapeutic transducer. The system was equipped with a sensor with a focal length of 16.5 cm, a frequency of 1.0 MHz, an acoustic emission power of 0 to 3000 W/cm2, which generated therapeutic focusing ultrasound energy, and six therapeutic transducers. The launch time was 0.15 s, the interval time was 0.25 s, and the number of launches was 10 to 12. The central probe monitored and guided the entire HIFU treatment process in real time during surgery. The high-intensity ultrasonic focus (focal area) emitted by the treatment probe was approximately 3 × 3×8 mm, and the treatment was completed by the point-to-line and line-to-surface procedure. Before treatment, the patients were placed in the supine position and the lesions were located using an external ultrasound probe and laser light. Treatment was initiated after precise localization of the lesions by the internal ultrasound probe.
After HIFU treatment, patients were followed up with telephone inquiries every 3 months. The endpoint was set at 18 months after treatment.
Data analysis
Statistical analyses were performed using IBM SPSS Statistics software version 20 (IBM Corp., Armonk, NY, USA). Data with a normal distribution are shown as mean ± standard deviation. The Student’s t-test was used to analyze the lesion data and uterine volume changes. The independent sample Kruskal–Wallis test was used to analyze the NRS and FPS scores. All of the statistical tests were two sided and considered significant when P ≤ 0.05.
Results
Patients’ demographic characteristics
From May 2015 to July 2015, 94 patients with adenomyosis underwent HIFU treatment. During the follow-up period, 2 patients became pregnant and 25 were lost to follow-up (Figure 1). Among the 67 patients, the mean age was 38.6 ± 5.3 years, the mean course of disease was 6.37 ± 5.01 years, and the mean number of births was 1.22 ± 0.76. All of the patients had a history of dysmenorrhea and 27 also had hypermenorrhea. Twelve patients were treated with HIFU combined with a gonadotropin-releasing hormone agonist and LNG-IUS (seven were treated with a gonadotropin-releasing hormone agonist and five were treated with LNG-IUS). A summary of the patients’ characteristics is shown in Table 1.
Figure 1.
Flowchart of the study.
Table 1.
Baseline characteristics of the patients.
| Characteristic | Mean ± SD (n=67) |
|---|---|
| Age (years) | 38.6 ± 5.3 |
| BMI (kg/m2) | 23.02 ± 3.09 |
| Number of births | 1.22 ± 0.76 |
| Times of therapy | 2 ± 0.82 |
| Pre-therapy NRS score | 6.46 ± 2.03 |
| Pre-therapy FPS score | 2.69 ± 1.81 |
| Pre-therapy lesion volume (mm3) | 247.7 ± 155.2 |
| Disease duration (years) | 6.37 ± 5.01 |
| Follow-up duration (months) | 11.6 ± 0.46 |
SD, standard deviation; BMI, body mass index; NRS, numerical rating scale; FPS, five-point scale.
Symptom relief
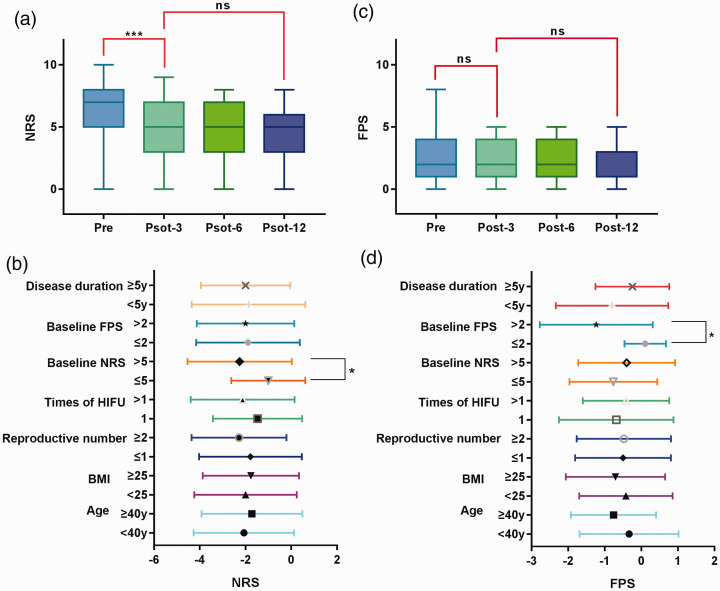
The degree of dysmenorrhea decreased from severe pain before HIFU treatment to moderate pain, and remained at a moderate or low level 6 months after treatment. The NRS score was significantly decreased 3 months after treatment compared with before treatment (P<0.0001) and then remained stable for 3 to 12 months. Age, body mass index, number of births, preoperative period, and duration of illness had no effect on HIFU (Supplemental Table). HIFU was more effective in patients with severe preoperative dysmenorrhea. Patients with a high NRS score before treatment obtained good results (Table 2 and Figure 2a, b).
Table 2.
Effect of high-intensity focused ultrasound for dysmenorrhea, hypermenorrhea, and uterine lesion volume.
| Pre-treatment | 3 months post-treatment | 6 months post-treatment | 12 months post-treatment | ||
|---|---|---|---|---|---|
| NRS score | Mean ± SEM | 6.46 ± 0.248 | 4.52 ± 0.29 | 4.55 ± 0.297 | 4.59 ± 0.29 |
| MD, 95% CI | −1.94 (−2.70 to −1.18) | −1.91 (−2.68 to −1.14) | −1.87 (−2.62 to −1.11) | ||
| FPS score | Mean ± SEM | 2.69 ± 0.22 | 2.15 ± 0.18 | 2.16 ± 0.18 | 2.03 ± 0.18 |
| MD, 95% CI | −0.54 (−1.01–0.02) | −0.52 (−1.08–0.036) | −0.66 (−1.22 to −0.09) | ||
| Lesion volume (mm3) | Mean ± SEM | 247.7 ± 34.69 | 226.7 ± 34.26 | ||
| MD, 95% CI | −20.95 (−119.6–77.76) |
SEM, standard error of the mean; MD, mean difference; CI, confidence interval; NRS, numerical rating scale; FPS, five-point scale.
Figure 2.
Effect of HIFU on dysmenorrheal and hypermenorrhea.
(a) Box plot showing the changes in the NRS score before and after treatment. (B) Graph showing the effect of the underlying features on NRS. (C) Box plot showing the changes in the FPS before and after treatment. (D) Graph showing the effect of the underlying features of the FPS. *P<0.05, ***P<0.001. NRS, numerical rating scale; FPS, five-point scale; HIFU, high-intensity focused ultrasound; BMI, body mass index.
The FPS was applied to assess hypermenorrhea, which is one of the most common symptoms of adenomyosis. The mean pre-therapy FPS score was 2.69 ± 0.22. After treatment, the FPS score decreased to 2.15 ± 0.18, which was not significantly different to that before treatment. However, in subgroup analysis, patients with a high pre-therapy FPS score obtained therapeutic benefits (Table 2 and Figure 2c, d).
Evaluation of uterine lesion volume
Before HIFU, the mean uterine lesion volume was 247.7 ± 34.69 mm3. After treatment for 6 months, the mean lesion volume was 226.7 ± 34.26 mm3, which was not significantly different to that before treatment (Table 3 and Figure 3a). Uterine lesion volume before treatment did not affect relief of dysmenorrhea by HIFU. However, the FPS score was significantly lower for a lesion volume ≥200 mm3 than that for a lesion volume <200 mm3 (P<0.05) (Figure 3b).
Table 3.
Effect of uterine lesion volume on high-intensity focused ultrasound for dysmenorrhea and hypermenorrhea.
| Lesion volume (mm3) | <200 (n = 11) | ≥200 (n = 9) | MD ± SEM, P |
|---|---|---|---|
| NRS score | −2.18 ± 0.58 | −3.11 ± 0.66 | −0.93 ± 0.88, P = 0.31 |
| FPS score | −1.18 ± 0.40 | −0.11 ± 0.19 | 1.07 ± 0.48, P = 0.03 |
MD, mean difference; SEM, standard error of the mean; NRS, numerical rating scale; FPS, five-point scale.
Figure 3.
Effect of HIFU on uterine lesion volume.
NRS, numerical rating scale; FPS, five-point scale.
Analysis of combined therapy
At present, many conservative methods are used to treat adenomyosis. In this study, 12 patients received HIFU combined with Mirena or a gonadotropin-releasing hormone agonist. Neither treatment improved HIFU treatment outcomes (Figure 4).
Figure 4.
Effect of Mirena and a GnRHa on the outcome of HIFU for dysmenorrhea and hypermenorrhea.
NRS, numerical rating scale; FPS, five-point scale; HIFU, high-intensity focused ultrasound; GnRHa, gonadotropin-releasing hormone agonist.
Discussion
To the best of our knowledge, this is the first study to evaluate relief of symptoms by HIFU for adenomyosis. In this study, 67 cases of adenomyosis were treated with HIFU and successfully followed up. Our study showed that HIFU improved dysmenorrhea in uterine adenomyosis, especially in those with severe dysmenorrhea. However, HIFU had no significant effect on menses of adenomyosis, but it appeared to affect those with a severe increase in menses (based on some individual observations) and relatively small uterine lesions.
There are many adverse factors leading to uterine adenomyosis, such as inflammation, cesarean section, multiple pregnancies and childbirth, invasion of the intima by the muscle layer, an increase of the effect of the endometrium and other factors, occurrence of moderate or severe dysmenorrhea, and an increase in menstrual volume. A preliminary diagnosis of adenomyosis can be made according to the typical clinical symptoms and signs, with or without increased levels of serum cancer antigen 125, with confirmation by ultrasound and MRI. MRI shows that the junctional zone is widened, usually >12 mm, as the diagnostic criterion for adenomyosis.12,13 However, the final diagnosis for adenomyosis requires a histopathological examination. Although the histology of adenomyosis is benign, it has obvious infiltration, metastasis, relapse, and other malignant biological behaviors.
Treatment for adenomyosis should be determined by the patient’s age, her desire to have children, clinical symptoms, and signs. The majority of patients with adenomyosis have had children, the clinical symptoms of the disease are often severe, and the lesion boundaries can be difficult to define.14 For many years, hysterectomy was considered the most effective method for treating adenomyosis. HIFU, which is a non-invasive treatment, offers safety, efficacy, no radiation injury, and a rapid recovery, and is painless. HIFU retains organ function, its clinical value has been gradually recognized, and its application is becoming more extensive. Dysmenorrhea is a major symptom of adenomyosis. Therefore, the extent of relief of dysmenorrhea after treatment is an important indicator of the treatment’s effectiveness.15 We found that HIFU improved dysmenorrhea in uterine adenomyosis as shown by a significant decrease in the NRS score 3 months after treatment compared with before treatment. However, the FPS score did not change after treatment. Most of the patients in this study had fertility requirements, and some had never given birth before treatment. Therefore, the endometrium needs to be protected during HIFU treatment. This could be the reason the symptoms of menorrhagia did not significantly improve.
There are several limitations to this study. The sample size was small with only 67 patients. Additionally, this was a retrospective study. Therefore, there may have been selection bias. We need to design a prospective, observational study to evaluate HIFU for treating adenomyosis. Finally, and most importantly, HIFU’s effect on fertility was not assessed. Further research on this topic is expected in the near future.
Conclusion
HIFU is a new noninvasive treatment for adenomyosis. HIFU can significantly relieve dysmenorrhea in patients with adenomyosis and shows borderline effectiveness for hypermenorrhea and uterine lesion volume. HIFU can be used as a clinical application for adenomyosis.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_0300060520976492 for Clinical effectiveness and potential long-term benefits of high-intensity focused ultrasound therapy for patients with adenomyosis by Wei Li, Jiayu Mao, Yang Liu, Ying Zhu, Xiaojing Li, Zhigang Zhang, Xuechai Bai, Wei Zheng and Liang Wang in Journal of International Medical Research
Acknowledgments
The authors would like to thank the members of the research group for useful discussions.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This work was supported by a grant from the Natural Science Foundation of China (No. 81472422).
Author contributions: Wei Li, Yang Liu, Jiayu Mao, and Ying Zhu analyzed and interpreted the data and drafted the manuscript. Zhigang Zhang, Xuechai Bai, and Xiaojing Li acquired the data. Wei Zheng and Liang Wang contributed to conception and design of the study. All authors approved the final content of the manuscript.
ORCID iD: Liang Wang https://orcid.org/0000-0001-6047-5284
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Wang L, Zheng W, Ding X, et al. Identification biomarkers of eutopic endometrium in endometriosis using artificial neural networks and protein fingerprinting. Fertil Steril 2010; 93: 2460–2462. [DOI] [PubMed] [Google Scholar]
- 2.Xinmei Z, Xinfeng H, Min H. Adenomyosis. ISBN 978-7-117-26152-4.
- 3.Garcia L, Isaacson K. Adenomyosis: review of the literature. J Minim Invasive Gynecol 2011; 18: 428–437. [DOI] [PubMed] [Google Scholar]
- 4.Tsui KH, Lee WL, Chen CY, et al. Medical treatment for adenomyosis and/or adenomyoma. Taiwan J Obstet Gynecol 2014; 53: 459–465. [DOI] [PubMed] [Google Scholar]
- 5.Kim KA, Yoon SW, Lee C, et al. Short-term results of magnetic resonance imaging-guided focused ultrasound surgery for patients with adenomyosis: symptomatic relief and pain reduction. Fertil Steril 2011; 95: 1152–1155. [DOI] [PubMed] [Google Scholar]
- 6.Zhou M, Chen JY, Tang LD, et al. Ultrasound-guided high-intensity focused ultrasound ablation for adenomyosis: the clinical experience of a single center. Fertil Steril 2011; 95: 900–905. [DOI] [PubMed] [Google Scholar]
- 7.Wang W, Wang Y, Tang J. Safety and efficacy of high intensity focused ultrasound ablation therapy for adenomyosis. Acad Radiol 2009; 16: 1416–1423. [DOI] [PubMed] [Google Scholar]
- 8.Yoon SW, Kim KA, Cha SH, et al. Successful use of magnetic resonance-guided focused ultrasound surgery to relieve symptoms in a patient with symptomatic focal adenomyosis. Fertil Steril 2008; 90: 2018.e13-5. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Li K, Xie B, et al. Effective ablation therapy of adenomyosis with ultrasound-guided high-intensity focused ultrasound. Int J Gynaecol Obstet 2014; 124: 207–211. [DOI] [PubMed] [Google Scholar]
- 10.Shui L, Mao S, Wu Q, et al. High-intensity focused ultrasound (HIFU) for adenomyosis: two-year follow-up results. Ultrason Sonochem 2015; 27: 677–681. [DOI] [PubMed] [Google Scholar]
- 11.Chong GO ,Lee YH ,Hong DG, et al. Long-term efficacy of laparoscopic or robotic adenomyomectomy with or without medical treatment for severely symptomatic adenomyosis. Gynecol Obstet Invest 2016; 81: 346–352. [DOI] [PubMed] [Google Scholar]
- 12.Tamai K, Togashi K, Ito T, et al. MR imaging findings of adenomyosis: correlation with histopathologic features and diagnostic pitfalls. Radiographics 2005; 25: 21–40. [DOI] [PubMed] [Google Scholar]
- 13.Sudderuddin S, Helbren E, Telesca M, et al. MRI appearances of benign uterine disease. Clin Radiol 2014; 69: 1095–1104. [DOI] [PubMed] [Google Scholar]
- 14.Wood C. Adenomyosis: difficult to diagnose, and difficult to treat. Diagn Ther Endosc 2001; 7: 89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu X, Wang W, Wang Y, et al. Clinical predictors of long-term success in ultrasound-guided high-intensity focused ultrasound ablation treatment for adenomyosis: a retrospective study. Medicine (Baltimore) 2016; 95: e2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_0300060520976492 for Clinical effectiveness and potential long-term benefits of high-intensity focused ultrasound therapy for patients with adenomyosis by Wei Li, Jiayu Mao, Yang Liu, Ying Zhu, Xiaojing Li, Zhigang Zhang, Xuechai Bai, Wei Zheng and Liang Wang in Journal of International Medical Research