Abstract
[Purpose] This study aimed to investigate a cross-cultural adaptation of the 40-item Healthcare Provider-Patient Activation Scale (HP-PAS). [Participants and Methods] We followed a guideline for cross-cultural adaptation that recommended using two forward and backward translations. In pilot testing, participants were Japanese physical therapists who provided comments about expression readability. Two authors independently categorized each comment as either “unable to understand” or “suggestion to enhance clarity”, after which Cohen κ and % agreement were used to assess agreement. We then assessed the flooring and ceiling effects, internal consistency, and Spearman ρ between the factor scores of the patient-activation-approach and non-patient-activation-approach. [Results] A total of 58 Japanese physical therapists participated in the pilot test. The agreement on comments was κ=0.44 and 86.5%. We identified the flooring and ceiling effects for most items. In addition, the internal consistency was acceptable for each factor; however, the Spearman ρ between the patient-activation-approach and non-patient-activation-approach factor scores was positive when it should have been negative. [Conclusion] We developed a Japanese version of the HP-PAS which will serve as a foundation for future studies to establish a measurement method for the magnitude of patient activation in the physical therapist population.
Key words: Patient activation, Patient centered approach, Self-management
INTRODUCTION
Patient-activation (PA), which allows the patient to actively take control of the consultation and/or in the management of their condition1), is an important factor in the patient-centered approach (PCA)2, 3). PA increases patient satisfaction from medical services1, 4). Importance of PCA has been recognized in physical therapy; however, the therapist-centered biomedical approach has been actually provided5). Therefore, further studies are needed to facilitate PCA in physical therapy.
In 2019, the Healthcare Providers Patient-Activation Scale (HP-PAS) has been developed through factor analysis and sensitivity to change analysis6). The HP-PAS is a self-reported questionnaire for healthcare providers using a 5-point Likert scale (1, not important; and 5, very important) and evaluates their attitude toward the importance of PA. Shand et al.6) reported that the factor analysis demonstrated two-factor structures with 20 items each of PA-approach and non-PA-approach. In the sensitivity to change analysis with 105 Australian healthcare providers comprising mostly of nurses (75 nurses and 10 physical therapists), the total scores in both factors decreased after an online training program to support chronic disease self-management. Therefore, Shand et al.6) suggested the use of the 20-item non-PA-approach for the assessment of PA.
The HP-PAS is a promising tool to evaluate attitudes of physical therapists toward PA and to facilitate PCA. However, no Japanese version of the HP-PAS has been reported yet. Therefore, this study aimed to investigate the cross-cultural adaptation of the 40-item HP-PAS.
PARTICIPANTS AND METHODS
This study was approved by the institutional research committee (Saitama Prefectural University No. 20011), and written informed consent was obtained from each participant. An approval of the HP-PAS translation into Japanese was obtained from the developer a priori. We followed a guideline of cross-cultural adaptation7), which includes forward translation, synthesize meeting with forward translations, backward translation, expert committee review, and pilot testing.
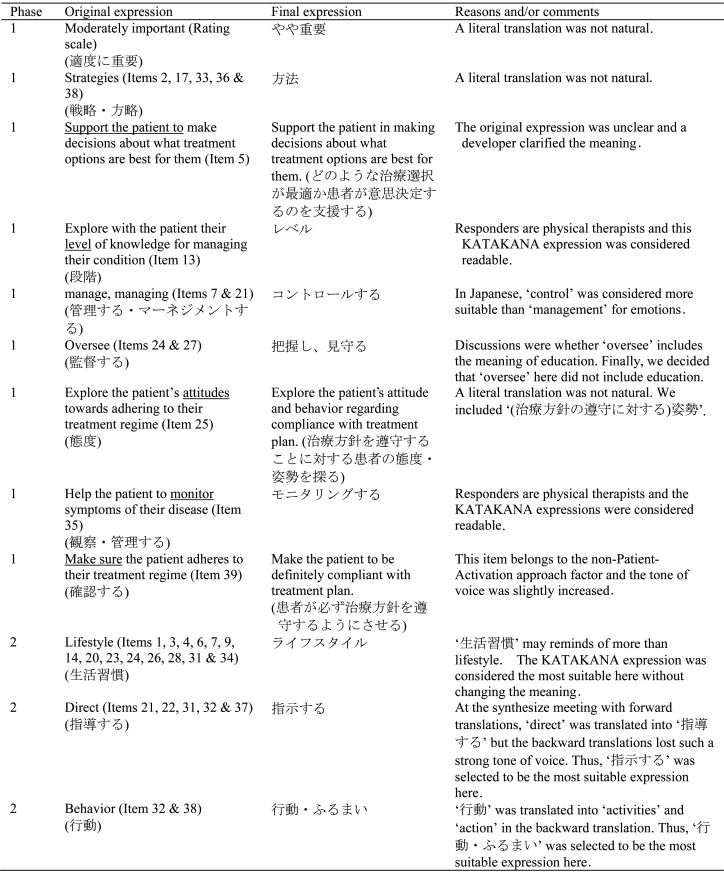
In the forward translation process, two English-Japanese bilingual translators independently translated 40 items including the instruction into Japanese. One translator was a physical therapist aware of the aim of the HP-PAS, whereas the other translator was an English scholar unaware of the aim of the HP-PAS. In the synthesize meeting with forward translations, a combined Japanese draft was developed with discussions among two forward translators and two authors. The combined Japanese draft was then translated into English independently by two physical therapists who were blinded to the aim of the HP-PAS. An expert committee review was held with 6 members included in the forward and backward translations. Modifications to ensure semantic, idiomatic, experiential, and conceptual equivalences were recorded7), and a pre-final draft to be tested in the pilot testing was developed with one consent among 6 expert committee members.
In the pilot testing, all participants were Japanese physical therapists. The guideline7) recommends 30–40 samples; however, data collection was continued until 50–60 samples were obtained to further understand data distribution. Data collection was carried out via an online survey on the home page of an author in July 2020. Participants were asked to provide free comments for each of 40 items including the instruction message in terms of expression readability. Each comment was independently categorized by two authors into “unable to understand” and “suggestion to enhance clarity”. Agreement between authors was assessed with Cohen κ and % agreement, where κ-value of <0.4 was interpreted as poor agreement, 0.41–0.60 as moderate agreement, 0.61–0.80 as good agreement, and 0.81–1.0 as very good agreement8). Disagreement between authors was resolved with discussion. Although criteria for the acceptance of missing data are not yet established, 5% can be used9). Thus, the pilot test was repeated by modifying the expression with >5% of “unable to understand” until all items satisfied the criteria.
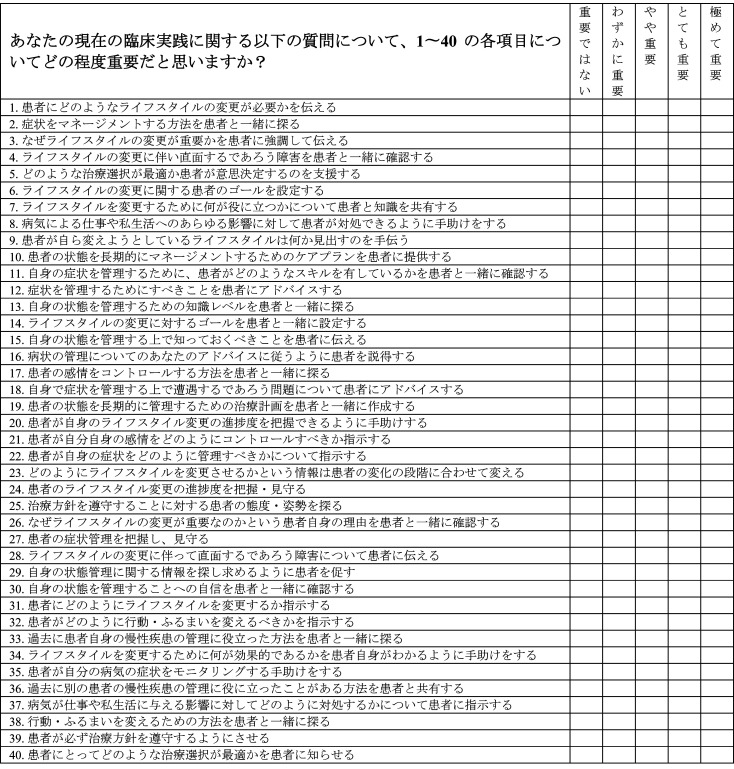
In the final version, participants completed the 40-item HP-PAS and reported the time to complete. The research utilized the 20-item PA-approach and 20-item non-PA-approach using the Cronbach α to assess internal consistency. Data distributions were assessed in each item, where flooring or ceiling effects were considered when >15% of the responses were the minimum or maximum response10,11,12). Furthermore, Spearman ρ was calculated between sum scores in PA-approach and non-PA-approach factors. Statistical analysis was conducted using the Statistical Package for the Social Sciences (version 21.0, IBM Corporation, New York, USA) using a statistical significance of 5%.
RESULTS
Appendix Table 1 summarizes reasons and/or comments for developing a pre-final draft to be tested in the pilot testing (Appendix 1), which included 58 physical therapists (45 males and 13 females) with a mean ± standard deviation (SD) of age and years after physical therapy license as 1.0 ± 10.6 years and 9.2 ± 9.0 years, respectively. The pilot testing was conducted once with the moderate agreement in the category of comments (0.44 [p<0.001], 86.5%). Table 1 presents proportions of categories in the comments for each item. The mean ± SD of time to complete 40 items was 390.3 ± 221.9 s. Cronbach α for the PA-approach and non-PA-approach was 0.94 and 0.89, respectively. Four items demonstrated the flooring effect and 35 items for the ceiling effect. The Spearman ρ between the PA-approach and non-PA-approach factors was 0.64 (p<0.001).
Table 1. Proportions of the categories of comments and proportions of response distributions.
| Item No. | Proportions of the categories of comments | Proportions of responses (%) | |||||
| Unable to understand | Suggestion to enhance clarity | Not important | Slightly important | Moderately important | Very important | Extremely important | |
| Instructions | 1.7 | 6.9 | – | – | – | – | – |
| 1n | 0 | 6.9 | 0 | 3.5 | 20.7 | 48.3 | 27.6 |
| 2p | 0 | 3.4 | 0 | 1.7 | 8.6 | 31.0 | 58.6 |
| 3 n | 0 | 5.3 | 1.7 | 10.3 | 20.7 | 32.8 | 34.5 |
| 4 p | 1.7 | 5.3 | 0 | 1.7 | 17.2 | 41.4 | 39.7 |
| 5 p | 0 | 5.3 | 0 | 3.5 | 20.7 | 31.0 | 44.8 |
| 6 n | 3.4 | 1.7 | 0 | 5.2 | 20.7 | 36.2 | 37.9 |
| 7 n | 1.7 | 3.4 | 0 | 3.5 | 19.0 | 37.9 | 39.7 |
| 8 p | 0 | 1.7 | 1.7 | 5.2 | 22.4 | 29.3 | 41.4 |
| 9 p | 3.4 | 1.7 | 3.5 | 6.9 | 24.1 | 24.1 | 41.4 |
| 10 n | 0 | 1.7 | 0 | 6.9 | 19.0 | 43.1 | 31.0 |
| 11 p | 1.7 | 8.6 | 0 | 12.1 | 22.4 | 31.0 | 34.5 |
| 12 n | 0 | 3.4 | 0 | 1.7 | 15.5 | 32.8 | 50.0 |
| 13 p | 3.4 | 10.3 | 1.7 | 19.0 | 25.9 | 29.3 | 24.1 |
| 14 p | 0 | 1.7 | 0 | 3.5 | 17.2 | 39.7 | 39.7 |
| 15 n | 0 | 3.4 | 0 | 5.2 | 10.3 | 39.7 | 44.8 |
| 16 n | 1.7 | 3.4 | 19.0 | 29.3 | 39.7 | 5.2 | 6.9 |
| 17 p | 0 | 3.4 | 1.7 | 13.8 | 41.4 | 20.7 | 22.4 |
| 18 n | 3.4 | 1.7 | 0 | 5.2 | 27.6 | 41.4 | 25.9 |
| 19 p | 0 | 3.4 | 3.5 | 5.2 | 27.6 | 39.7 | 24.1 |
| 20 p | 0 | 5.3 | 1.7 | 3.5 | 34.5 | 34.5 | 25.9 |
| 21 n | 0 | 3.4 | 27.6 | 22.4 | 31.0 | 13.8 | 5.2 |
| 22 n | 0 | 3.4 | 12.1 | 15.5 | 32.8 | 24.1 | 15.5 |
| 23 p | 3.4 | 5.3 | 0 | 8.6 | 15.5 | 46.6 | 29.3 |
| 24 n | 1.7 | 0 | 0 | 12.1 | 24.1 | 32.8 | 31.0 |
| 25 p | 0 | 1.7 | 8.6 | 10.3 | 25.9 | 25.9 | 29.3 |
| 26 p | 0 | 1.7 | 0 | 1.7 | 24.1 | 43.1 | 31.0 |
| 27 n | 0 | 6.9 | 0 | 3.5 | 32.8 | 34.5 | 29.3 |
| 28 n | 0 | 5.3 | 1.7 | 10.3 | 22.4 | 37.9 | 27.6 |
| 29 p | 1.7 | 1.7 | 6.9 | 13.8 | 29.3 | 25.9 | 24.1 |
| 30 p | 0 | 3.4 | 5.2 | 5.2 | 32.8 | 25.9 | 31.0 |
| 31 n | 0 | 5.3 | 12.1 | 29.3 | 34.5 | 13.8 | 10.3 |
| 32 n | 0 | 3.4 | 15.5 | 27.6 | 36.2 | 15.5 | 5.2 |
| 33 p | 1.7 | 1.7 | 1.7 | 10.3 | 29.3 | 36.2 | 22.4 |
| 34 p | 1.7 | 0 | 0 | 3.5 | 20.7 | 46.6 | 29.3 |
| 35 p | 0 | 6.9 | 3.5 | 3.5 | 20.7 | 36.2 | 36.2 |
| 36 n | 0 | 1.7 | 5.2 | 17.2 | 34.5 | 22.4 | 20.7 |
| 37 n | 1.7 | 1.7 | 10.3 | 12.1 | 29.3 | 36.2 | 12.1 |
| 38 p | 1.7 | 0 | 0 | 5.2 | 31.0 | 31.0 | 32.8 |
| 39 n | 0 | 3.4 | 27.6 | 32.8 | 22.4 | 13.8 | 3.5 |
| 40 n | 0 | 1.7 | 3.5 | 19.0 | 24.1 | 27.6 | 25.9 |
–: Not applicable; p: Patient-Activation approach factor; n: non-Patient-Activation approach factor.
DISCUSSION
This study investigated the cross-cultural adaptation of the 40-item HP-PAS into Japanese, which will be a foundation for future studies to develop an established measurement method for the magnitude of the PA in the population of physical therapists.
This study indicates that interpretability would be acceptable as the proportion of the “unable to understand” for each item was <5%. Furthermore, the ideal length of a web survey was median of 10 min13); thus, the HP-PAS with the maximum of 40 items would be feasible for a web survey and can be conducted with other measures.
The Cronbach α demonstrated an acceptable internal consistency14) in both PA-approach and non-PA-approach factors. However, most items demonstrated the flooring or ceiling effect, indicating the need to modify the rating scale when the HP-PAS is used in the physical therapist population. The potential reason for flooring or ceiling effect is the lack of a neutral response option, where the 5-point response option may be acceptable15). The Rasch analysis enables to inspect appropriateness of the rating scale and scale options can be combined to enhance the psychometric property10, 11, 16, 17). Shand et al.6) proposed an idea on the use of the “How often do you…” rather than “How important is it to…,” and these psychometric properties are considered similar. This change of the rating scale can solve the potential concern of the lack of a neutral response option. Therefore, a future study would be required to investigate whether the flooring and ceiling effects can be improved using the % scale or the 11-point % Likert scale and asking the frequency for each item.
The Spearman ρ between the PA-approach and non-PA-approach factors was statistically significant and positive, which should be theoretically negative. This indicates a problem in the content validity of the PA-approach and non-PA-approach factors, which is the most important validity to be inspected first18). Item generation of the PA-approach factor was undertaken by the author panels in the previous study6) based on literature19, 20) and the non-PA-approach items were generated to have the opposite meaning of the PA-approach items. No comprehensive content validity analysis has been undertaken; thus, further studies of the content analysis are warranted.
Limitation of this study includes findings of the internal consistency and the correlation between the PA-approach and non-PA-approach factors as preliminary, and robust findings are achieved with a larger cohort.
Funding
This work was supported by JSPS KAKENHI Grant Number 19K19912 for publication.
Conflict of interest
There is no conflict of interest.
Appendix Table 1. Summary of reasons and/or comments for developing a pre-final draft to be tested in the pilot testing
Appendix 1. Healthcare Providers Patient-Activation Scale (Japanese version).
REFERENCES
- 1.Michie S, Miles J, Weinman J: Patient-centredness in chronic illness: what is it and does it matter? Patient Educ Couns, 2003, 51: 197–206. [DOI] [PubMed] [Google Scholar]
- 2.Kitson A, Marshall A, Bassett K, et al. : What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs, 2013, 69: 4–15. [DOI] [PubMed] [Google Scholar]
- 3.Pelzang R: Time to learn: understanding patient-centred care. Br J Nurs, 2010, 19: 912–917. [DOI] [PubMed] [Google Scholar]
- 4.May SJ: Patient satisfaction with management of back pain. Part 1: What is satisfaction? Review of satisfaction with medical management. Physiotherapy, 2001, 87: 4–20. [Google Scholar]
- 5.Hammond R, Stenner R, Palmer S: What matters most—a qualitative study of person-centred physiotherapy practice in community rehabilitation. Physiotherapy, 2020, 107: e205–e206. [DOI] [PubMed] [Google Scholar]
- 6.Shand L, Higgins R, Murphy B, et al. : Development and validation of the healthcare providers patient-activation scale. Patient Educ Couns, 2019, 102: 1550–1557. [DOI] [PubMed] [Google Scholar]
- 7.Beaton DE, Bombardier C, Guillemin F, et al. : Guidelines for the process of cross-cultural adaptation of self-report measures. Spine, 2000, 25: 3186–3191. [DOI] [PubMed] [Google Scholar]
- 8.Altman DG: Practical statistics for medical researched. London: Chapman & Hall, 1991. [Google Scholar]
- 9.Leong FT, Austin JT: The psychology research handbook: a guide for graduate students and research assistants, 2nd ed. Thousand Oaks: SAGE Publications, 2006. [Google Scholar]
- 10.Takasaki H, Treleaven J: Construct validity and test-retest reliability of the Fatigue Severity Scale in people with chronic neck pain. Arch Phys Med Rehabil, 2013, 94: 1328–1334. [DOI] [PubMed] [Google Scholar]
- 11.Takasaki H, Chien CW, Johnston V, et al. : Validity and reliability of the perceived deficit questionnaire to assess cognitive symptoms in people with chronic whiplash-associated disorders. Arch Phys Med Rehabil, 2012, 93: 1774–1781. [DOI] [PubMed] [Google Scholar]
- 12.Hobart JC, Thompson AJ: The five item Barthel index. J Neurol Neurosurg Psychiatry, 2001, 71: 225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Revilla M, Ochoa C: Ideal and maximum length for a web survey. Int J Mark Res, 2017, 59: 557–565. [Google Scholar]
- 14.Andresen EM: Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil, 2000, 81: S15–S20. [DOI] [PubMed] [Google Scholar]
- 15.Simms LJ, Zelazny K, Williams TF, et al. : Does the number of response options matter? Psychometric perspectives using personality questionnaire data. Psychol Assess, 2019, 31: 557–566. [DOI] [PubMed] [Google Scholar]
- 16.Takasaki H, Hall T: A Japanese version of the Patient Attitudes and Beliefs Scale for patients with musculoskeletal disorders. Physiother Theory Pract, 2019, 1–9. [DOI] [PubMed] [Google Scholar]
- 17.Takasaki H, Johnston V, Treleaven J, et al. : Neck pain driving index: appropriateness of the rating scale and unidimensionality of the strategic, tactical, and operational levels. Arch Phys Med Rehabil, 2013, 94: 1842–1846. [DOI] [PubMed] [Google Scholar]
- 18.Terwee CB, Prinsen CA, Chiarotto A, et al. : COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res, 2018, 27: 1159–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher EB, Brownson CA, O’Toole ML, et al. : Ecological approaches to self-management: the case of diabetes. Am J Public Health, 2005, 95: 1523–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawn S, Battersby M. Capabilities for supporting prevention and chronic condition self-management: a resource for educators of primary health care professionals. Adelaide: Commonwealth of Australia, 2009.