Key Points
Question
What is the association of sex with the relative outcomes of multiple vs single arterial grafting during coronary artery bypass grafting?
Findings
In a statewide cohort study of 63 402 patients undergoing coronary artery bypass grafting, at 7 years’ follow-up, outcomes with multiple arterial grafting were better among low-risk, but not high-risk, patients. Mortality at 7 years was lower among men, but not women, undergoing multiple arterial grafting.
Meaning
Multiple arterial grafting was associated with better outcomes among low-risk, but not high-risk, men and women at different thresholds; studies of multiple arterial grafting specifically directed at women are needed.
Abstract
Importance
Sex-related differences in the outcome of using multiple arterial grafts during coronary artery bypass grafting (CABG) remain uncertain.
Objective
To compare the outcomes of the use of multiple arterial grafts vs a single arterial graft during CABG for women and men.
Design, Setting, and Participants
This statewide cohort study used data from New York’s Cardiac Surgery Reporting System and New York’s Vital Statistics file on 63 402 patients undergoing CABG from January 1, 2005, to December 31, 2014. Statistical analysis was performed from January 10 to August 20, 2020.
Exposures
Multiple arterial grafting or single arterial grafting.
Main Outcomes and Measures
Mortality, acute myocardial infarction (AMI), stroke, repeated revascularization, major adverse cardiac and cerebrovascular event (composite of mortality, AMI, and stroke), and major adverse cardiac event (composite of mortality, AMI, or repeated revascularization) were compared among propensity-matched patients and stratified by the risk of long-term mortality.
Results
Of the 63 402 patients (48 155 men [76.0%]; mean [SD] age, 69.9 [10.5] years) in the study, women had worse baseline characteristics than men for most of the explored variables. Propensity matching yielded a total of 9512 male pairs and 1860 female pairs. At 7 years of follow-up, mortality was lower among men who underwent multiple arterial grafting (adjusted hazard ratio, 0.80; 95% CI, 0.73-0.87) but not women who underwent multiple arterial grafting (adjusted hazard ratio, 0.99; 95% CI, 0.84-1.15). When stratified by the estimated risk of death, the use of multiple arterial grafts was associated with better survival and a lower rate of a major adverse cardiac event among low-risk, but not high-risk, patients of both sexes, and the risk cutoff was different for men and women.
Conclusions and Relevance
This study suggests that women have a worse preoperative risk profile than men. Multiple arterial grafting is associated with better outcomes among low-risk, but not high-risk, patients, and the risk cutoffs differ between sexes. These data highlight the need for new studies on the outcome of multiple arterial grafts in women.
This cohort study compares the outcomes of the use of multiple arterial grafts vs a single arterial graft during coronary artery bypass grafting for women and men.
Introduction
The association of sex with the outcomes of coronary artery bypass grafting (CABG) is controversial. Women presenting for CABG have different disease characteristics and worse risk profiles compared with men.1,2,3 However, in most CABG observational studies and randomized clinical trials, women represent only a minority of the patient population, so the reported findings represent the predominantly male cohort and may not be applicable to women.4,5,6,7,8
The benefit associated with using multiple arterial grafts during CABG for women also remains uncertain. Although there is observational evidence demonstrating better clinical outcomes and graft patency with multiple arterial grafting (MAG) in the general population of patients undergoing CABG,9,10,11,12 few studies have evaluated the benefit associated with MAG for women, and the results have been contradictory.13,14,15 Conduits and target vessels are typically smaller in women, which may increase the complexity of MAG and probably explains some of the reported discrepancies.16,17
In this study, we evaluate the association of sex with the relative outcomes of MAG vs single arterial grafting (SAG) for women and men in New York state. We hypothesize that the treatment effect may be different between the 2 sexes.
Methods
Databases
This cohort study used data from New York’s Cardiac Surgery Reporting System (CSRS) and New York’s Vital Statistics file on patients undergoing CABG from January 1, 2005, to December 31, 2014. The CSRS database includes information on patient demographic characteristics, hospital and physician identifiers, preoperative risk factors, and outcomes. Procedural information includes the total number of conduits and the number of arterial conduits. Data from the CSRS are checked annually for completeness and accuracy by matching the records to the Statewide Planning and Research Cooperative System (SPARCS), New York’s administrative acute care database. The accuracy of risk factors in the system is checked by using New York’s utilization review agent to audit samples of cases from selected hospitals each year. Institutional review board approval was not required by University at Albany, State University of New York, given the retrospective nature of the study and the fact that patient identification data were encrypted.
The data from New York’s Vital Statistics file were matched to the CSRS data using unique patient identifiers to obtain information on postdischarge deaths that occurred after the index procedure. The SPARCS data were used to obtain information on hospitalizations for acute myocardial infarction (AMI) or stroke after the index hospitalization. Information on repeated revascularization was obtained by matching the CABG and percutaneous coronary intervention registries and developing a longitudinal data file. The study was limited to New York state residents to minimize the chance of postdischarge outcomes occurring outside of New York. Data were also collected on surgeons’ annual CABG case volumes, which were stratified as low (<75 cases), moderate (75-150 cases), and high (>150 cases). All patients with multivessel coronary artery disease who underwent nonemergency multigraft CABG with at least 1 arterial conduit and could be followed up for at least 2 years using registry data were included in the study.
Outcomes
The incidence rates of mortality, AMI, stroke, repeated revascularization, a major adverse cardiac and cerebrovascular event (MACCE; composite of mortality, AMI, or stroke), and a major adverse cardiac event (MACE; composite of mortality, AMI, or repeated revascularization) were compared separately for male and female patients between MAG and SAG procedures at 1 year and 7 years after the index procedure.
Statistical Analysis
Statistical analysis was performed from January 10 to August 20, 2020. Propensity score matching was used to minimize selection bias due to lack of randomization of patients to MAG and SAG by decreasing heterogeneity in baseline risk factors. Propensity matching was based on important patient risk factors, including diseased vessels, completeness of revascularization, number of conduits, total surgeon CABG volume, and type of surgery (off pump or on pump) (Table 1; eTables 1 and 2 in the Supplement).
Table 1. Surgeon Volume and Baseline Patient Characteristics of Patients Undergoing Single Arterial and Multiple Arterial Isolated Coronary Artery Bypass Grafting Surgery in New York State From 2005 to 2014a.
| Variable | Patients, No. (%) | Standardized difference | ||
|---|---|---|---|---|
| Overall | Single arterial grafting | Multiple arterial grafting | ||
| Men | ||||
| No. of patients | 48 155 (100) | 37 627 (78.1) | 10 528 (21.9) | NA |
| Age, mean (SD), y | 65.1 (10.4) | 66.3 (10.2) | 60.6 (9.9) | 56.8 |
| Body surface area, mean (SD), m2 | 2.1 (0.2) | 2.1 (0.2) | 2.1 (0.2) | 10.1 |
| Risk score, mean (SD) | 6.3 (3.0) | 6.7 (2.9) | 4.9 (2.6) | 63.0 |
| High risk (score ≥9) | 10 419 (21.6) | 9402 (25.0) | 1017 (9.7) | 41.4 |
| Low risk (score <9) | 37 736 (78.4) | 28 225 (75.0) | 9511 (90.3) | 41.4 |
| Off-pump surgery | 10 354 (21.5) | 8266 (22.0) | 2088 (19.8) | 5.3 |
| Incomplete revascularization | 10 554 (21.9) | 8505 (22.6) | 2049 (19.5) | 7.7 |
| ≤3 Conduits | 10 803 (22.4) | 8627 (22.9) | 2176 (20.7) | 5.5 |
| Aged ≥70 y | 16 962 (35.2) | 15 006 (39.9) | 1956 (18.6) | 48.2 |
| Peripheral vascular disease | 5604 (11.6) | 4611 (12.3) | 993 (9.4) | 9.1 |
| Cerebrovascular disease | 8006 (16.6) | 6746 (17.9) | 1260 (12.0) | 16.8 |
| COPD | 10 001 (20.8) | 8561 (22.8) | 1440 (13.7) | 23.7 |
| Type 1 or 2 diabetes | 17 545 (36.4) | 14 403 (38.3) | 3142 (29.8) | 17.9 |
| Previous cardiac surgery | 789 (1.6) | 617 (1.6) | 172 (1.6) | 0.0 |
| Women | ||||
| No. of patients | 15 247 (100) | 13 146 (86.2) | 2101 (13.8) | NA |
| Age, mean (SD), y | 68.6 (10.3) | 69.2 (10.1) | 64.8 (10.8) | 42.3 |
| Body surface area, mean (SD), m2 | 1.9 (0.2) | 1.9 (0.2) | 1.9 (0.2) | 10.6 |
| Risk score, mean (SD) | 7.4 (2.8) | 7.6 (2.8) | 6.2 (2.9) | 48.3 |
| High risk (score ≥9) | 5022 (32.9) | 4594 (34.9) | 428 (20.4) | 33.0 |
| Low risk (score <9) | 10 225 (67.1) | 8552 (65.1) | 1673 (79.6) | 33.0 |
| Off-pump surgery | 3527 (23.1) | 3062 (23.3) | 465 (22.1) | 2.8 |
| Incomplete revascularization | 3702 (24.3) | 3228 (24.6) | 474 (22.6) | 4.7 |
| ≤3 Conduits | 4210 (27.6) | 3659 (27.8) | 551 (26.2) | 3.6 |
| Aged ≥70 y | 7599 (49.8) | 6881 (52.3) | 718 (34.2) | 37.3 |
| Peripheral vascular disease | 2147 (14.1) | 1830 (13.9) | 317 (15.1) | 3.3 |
| Cerebrovascular disease | 3585 (23.5) | 3179 (24.2) | 406 (19.3) | 11.8 |
| COPD | 3863 (25.3) | 3451 (26.3) | 412 (19.6) | 15.8 |
| Diabetes | 7389 (48.5) | 6491 (49.4) | 898 (42.7) | 13.3 |
| Previous cardiac surgery | 198 (1.3) | 166 (1.3) | 32 (1.5) | 2.2 |
Abbreviations: COPD, chronic obstructive pulmonary disease; NA, not applicable.
Additional details are provided in eTables 1 and 2 in the Supplement.
The propensity scores were derived separately for male and female patients by developing nonparsimonious logistic regression models that estimated the probability of a given patient receiving multiple arterial grafts based on all of the risk factors available in the registry. Then, the propensity score was used to match patients on a 1-to-1 basis to minimize the overall distance in propensity scores between the groups. Patients were matched exactly for year of surgery to ensure similar follow-up periods for patients who underwent MAG and those who underwent SAG. Patients were also matched exactly for complete revascularization (using a proxy of number of total conduits equal to or greater than the number of diseased vessels because no better information was available), left main coronary artery disease, 3-vessel disease, 2-vessel disease with right coronary artery involvement, previous AMI within 7 days, left ventricular ejection fraction less than 50%, kidney failure (serum creatinine level >1.5 mg/dL [to convert to micromoles per liter, multiply by 88.4] or undergoing dialysis), and age (≥70 years). Patients were also matched with respect to other factors as long as their estimated log odds from the logistic regression model were no more than 0.2 SDs apart. Standardized differences in the prevalence of propensity model variables were then calculated.
The propensity-matched pairs were used to analyze differences in adverse outcomes between patients undergoing MAG and those undergoing SAG. To eliminate further differences within the matched pairs, a Cox proportional hazards regression model was used to calculate the adjusted hazard ratio (AHR) for the 2 procedures after adjusting for all risk factors in the propensity score.
Because we hypothesized that differences in MAG vs SAG outcomes by sex may be associated with differences in patients’ preoperative risk profile, we performed separate propensity score–matched comparisons for men and women based on the preoperative risk factors, including a long-term mortality risk score developed by our group.18 That risk score was developed using the New York state CSRS data from 8597 patients who underwent isolated CABG in 2000. Variables independently associated with 7-year survival at multivariable analysis (age, body mass index, ejection fraction, unstable hemodynamic state or shock, left main coronary artery disease, cerebrovascular disease, peripheral arterial disease, congestive heart failure, malignant ventricular arrhythmia, chronic obstructive pulmonary disease, type 1 or 2 diabetes, kidney failure, and history of open heart surgery) were assigned 1 to 7 points, with the maximum point total for each patient aged 28 years. Patients aged 70 to 79 years and 80 years or more had the highest weight (5 and 7 points, respectively). Female and male patients were divided into low-risk (<10% 1-year mortality, corresponding to a risk score of 0-8) and high-risk (≥10% 1-year mortality, corresponding to a risk score of ≥9) categories, and the outcomes were compared. The robustness of the results was tested for different risk cutoffs.
In a sensitivity analysis, a fully adjusted Cox proportional hazards regression model (including the risk score as a continuous variable) was used instead of propensity matching for risk adjustment, and the interactions between female sex and MAG and between female sex and risk score were tested.
A landmark analysis including only patients who were alive 30 days after surgery was performed. Mortality was also compared between female and male patients receiving SAG and female and male patients receiving MAG in separate fully adjusted Cox proportional hazards regression models. Gamma testing and the E-value were used to evaluate the association of unmeasured confounding with the results of the main analysis.19,20,21 All P values were from 2-sided tests, and results were deemed statistically significant at P < .05. All analyses were conducted in SAS, version 9.4 (SAS Institute Inc) and R, version 3.5.2 (R Foundation for Statistical Computing).
Results
Patient Characteristics
In total, 71 706 New York state residents underwent nonemergency multigraft CABG with at least 1 arterial conduit in 42 New York state nonfederal hospitals between January 1, 2005, and December 31, 2014. Out-of-state residents (n = 2757) and patients with an invalid Social Security number (n = 5547) were excluded because their deaths or subsequent hospitalizations could not be ascertained using New York Vital Statistics and SPARCS data. The final study sample comprised 63 402 patients (48 155 men [76.0%] and 15 247 women [24.0%]; mean [SD] age, 69.9 [10.5] years) (eFigure in the Supplement).
The baseline characteristics of the male and female patients before and after propensity score matching are summarized in Table 1 and eTables 1, 2, 3, and 4 in the Supplement. Female patients had worse baseline risk profiles (overall mean [SD] risk score, 7.4 [2.8]; mean [SD] risk score for women undergoing SAG, 7.6 [2.8]; mean [SD] risk score for women undergoing MAG, 6.2 [2.9]) compared with male patients (overall mean [SD] risk score, 6.3 [3.0]; mean [SD] risk score for men undergoing SAG, 6.7 [2.9]; mean [SD] risk score for men undergoing MAG, 4.9 [2.6]).
Among male patients, 37 627 (78.1%) received a single arterial graft, and 10 528 (21.9%) received multiple arterial grafts (Table 1; eTable 1 in the Supplement). The median follow-up was 6.5 years (range, 3.9-9.2 years) for all male patients, 6.4 years (range, 3.8-9.0 years) for men undergoing SAG, and 7.2 years (range, 4.4-9.6 years) for men undergoing MAG. The median number of grafts per male patient was 3 (interquartile range, 3-4), and the median number of arterial grafts per male patient was 1 (interquartile range, 1-1). Male patients undergoing MAG were younger than those undergoing SAG and had a lower prevalence of diabetes, cerebrovascular disease, congestive heart failure, chronic obstructive pulmonary disease, kidney dialysis, elevated serum creatinine level (>1.5 mg/dL), and/or low left ventricular ejection fraction (<40%). Men receiving multiple arterial grafts were also more likely than those receiving a single arterial graft to be undergoing an elective procedure and to have a higher body surface area. Patients undergoing off-pump SAG and patients undergoing off-pump MAG had similar rates of incomplete revascularization (2121 of 8266 [25.7%] vs 504 of 2088 [24.1%]; P = .15). Surgeons with low (<75 cases), moderate (75-150 cases), or high (>150) annual CABG volumes were all more likely to perform SAG than MAG for male patients (low, 14 358 of 17 477 [82.2%] vs 3119 of 17 477 [17.8%]; moderate, 16 075 of 22 329 [72.0%] vs 6254 of 22 329 [28.0%]; high, 7194 of 8349 [86.2%] vs 1155 of 8349 [13.8%]).
Among female patients, 13 146 (86.2%) received a single arterial graft, and 2101 (13.8%) received multiple arterial grafts (Table 1; eTable 2 in the Supplement). The median follow-up was 6.3 years (range, 3.7-8.8 years) for all female patients, 6.2 years (range, 3.6-8.7 years) for women undergoing SAG, and 6.8 years (range, 4.1-9.4 years) for women undergoing MAG. The median number of grafts per female patient was 3 (interquartile range, 2-3), and the median number of arterial grafts per female patient was 1 (interquartile range, 1-1). Female patients undergoing MAG were younger than those undergoing SAG and had lower a prevalence of diabetes, cerebrovascular disease, congestive heart failure, chronic obstructive pulmonary disease, and/or kidney dialysis. Female patients undergoing MAG also had higher body surface areas and higher left ventricular ejection fraction (≥40%) compared with those undergoing SAG. Patients undergoing off-pump SAG and patients undergoing off-pump MAG had similar rates of incomplete revascularization (899 of 3062 [29.4%] vs 139 of 465 [29.9%]; P = .81). Surgeons with low (<75 cases), moderate (75-150 cases), or high (>150 cases) annual CABG volumes were all more likely to perform SAG than MAG for female patients (low, 4976 of 5555 [89.6%] vs 579 of 5555 [10.4%]; moderate, 5716 of 7050 [81.1%] vs 1334 of 7050 [18.9%]; high, 2454 of 2642 [92.9%] vs 188 of 2642 [7.1%]).
Propensity Matching
Propensity matching yielded a total of 9512 propensity-matched male pairs and 1860 propensity-matched female pairs. Both the male and female propensity-matched pairs were similar with respect to prevalence of risk factors, with no patient characteristic having a standardized difference exceeding 10% (eTables 3 and 4 in the Supplement). There were no significant differences by sex in mortality between patients undergoing SAG and those undergoing MAG (eTable 5 in the Supplement).
Outcomes in Propensity-Matched Male Patients by Number of Arterial Grafts
The 1-year and 7-year outcomes of propensity-matched male patients who underwent MAG or SAG are summarized in Table 2. At 1 year, the incidence of mortality was similar for male patients who underwent MAG and those who underwent SAG (Kaplan-Meier estimates: 195 of 9512 [2.1%] vs 185 of 9512 [1.9%]; AHR, 1.06; 95% CI, 0.87-1.30). The incidences of AMI, stroke, and MACCE were also not different, but male patients who underwent MAG had lower incidences of repeated revascularization (Kaplan-Meier estimates: 220 of 9512 [2.3%] vs 310 of 9512 [3.3%]; AHR, 0.72; 95% CI, 0.61-0.86) and MACE (Kaplan-Meier estimates: 500 of 9512 [5.3%] vs 601 of 9512 [6.3%]; AHR, 0.84; 95% CI, 0.75-0.94) than those who underwent SAG.
Table 2. One- and 7-Year Outcomes of Propensity-Matched Patients Undergoing Multiple Arterial vs Single Arterial Isolated Coronary Artery Bypass Grafting in New York State From 2005 to 2014.
| Outcome | Multiple arterial grafting | Single arterial grafting | AHR (95% CI) | P value | ||
|---|---|---|---|---|---|---|
| Patients at risk at the end of the follow-up period, No. | Adverse event, No. (%)a | Patients at risk at the end of the follow-up period, No. | Adverse event, No. (%)a | |||
| Men | ||||||
| 1-y Outcome | ||||||
| Mortality | 9317 | 195 (2.1) | 9327 | 185 (1.9) | 1.06 (0.87-1.30) | .56 |
| AMI | 9182 | 142 (1.5) | 9160 | 179 (1.9) | 0.80 (0.64-1.00) | .05 |
| Stroke | 9184 | 156 (1.6) | 9205 | 146 (1.5) | 1.06 (0.85-1.33) | .60 |
| Repeated revascularization | 9098 | 220 (2.3) | 9020 | 310 (3.3) | 0.72 (0.61-0.86) | <.001 |
| MACCE | 9053 | 459 (4.8) | 9041 | 471 (5.0) | 0.99 (0.87-1.12) | .83 |
| MACE | 9012 | 500 (5.3) | 8911 | 601 (6.3) | 0.84 (0.75-0.94) | .004 |
| 7-y Outcome | ||||||
| Mortality | 4892 | 933 (11.6) | 4741 | 1133 (14.1) | 0.80 (0.73-0.87) | <.001 |
| AMI | 4685 | 420 (5.3) | 4490 | 498 (6.3) | 0.84 (0.74-0.96) | .01 |
| Stroke | 4705 | 421 (5.3) | 4555 | 418 (5.2) | 0.99 (0.86-1.13) | .89 |
| Repeated revascularization | 4411 | 890 (11.3) | 4141 | 1111 (14.2) | 0.80 (0.73-0.87) | <.001 |
| MACCE | 4513 | 1565 (19.1) | 4320 | 1804 (21.9) | 0.85 (0.80-0.91) | <.001 |
| MACE | 4301 | 1930 (23.4) | 4023 | 2336 (28.2) | 0.81 (0.76-0.86) | <.001 |
| Women | ||||||
| 1-y Outcome | ||||||
| Mortality | 1769 | 91 (4.9) | 1794 | 66 (3.5) | 1.34 (0.97-1.84) | .07 |
| AMI | 1732 | 43 (2.4) | 1745 | 54 (2.9) | 0.80 (0.53-1.19) | .27 |
| Stroke | 1725 | 55 (3.0) | 1757 | 46 (2.5) | 1.18 (0.80-1.74) | .41 |
| Repeated revascularization | 1707 | 62 (3.4) | 1738 | 57 (3.1) | 1.06 (0.74-1.52) | .74 |
| MACCE | 1688 | 172 (9.2) | 1711 | 149 (8.0) | 1.13 (0.91-1.41) | .25 |
| MACE | 1681 | 179 (9.6) | 1705 | 15 (8.3) | 1.14 (0.92-1.41) | .24 |
| 7-y Outcome | ||||||
| Mortality | 886 | 316 (19.6) | 881 | 310 (19.5) | 0.99 (0.84-1.15) | .85 |
| AMI | 836 | 120 (8.0) | 807 | 154 (10.2) | 0.77 (0.60-0.97) | .03 |
| Stroke | 834 | 126 (8.2) | 835 | 106 (6.9) | 1.19 (0.92-1.54) | .18 |
| Repeated revascularization | 774 | 222 (14.8) | 755 | 250 (16.6) | 0.90 (0.75-1.08) | .25 |
| MACCE | 789 | 478 (29.0) | 765 | 486 (29.9) | 0.97 (0.86-1.10) | .65 |
| MACE | 745 | 560 (33.9) | 713 | 585 (35.8) | 0.94 (0.84-1.06) | .29 |
Abbreviations: AHR, adjusted hazard ratio; AMI, acute myocardial infarction; MACCE, mortality, AMI, stroke, repeated revascularization, major adverse cardiac event, and cerebrovascular event (composite of mortality, AMI, and stroke); MACE, major adverse cardiac event (composite of mortality, AMI, or repeated revascularization).
Kaplan-Meier estimate at the end of 1- and 7- year periods.
At 7 years, the incidence of mortality was significantly lower for male patients who underwent MAG (Kaplan-Meier estimates: 933 of 9512 [11.6%] vs 1133 of 9512 [14.1%]; AHR, 0.80; 95% CI, 0.73-0.87) (Figure 1A). The incidences of AMI, repeated revascularization, MACCE, and MACE were also lower for male patients who underwent MAG (Kaplan-Meier estimates: AMI, 430 of 9512 [5.3%] vs 498 of 9512 [6.3%]; AHR,0.84; 95% CI, 0.74-0.96; repeated revascularization, 890 of 9512 [11.3%] vs 1111 of 9512 [14.2%]; AHR, 0.80; 95% CI, 0.73-0.87; MACCE, 1565 of 9512 [19.1%] vs 1804 of 9512 [21.9%]; AHR, 0.85; 95% CI, 0.80-0.91; MACE, 1930 of 9512 [23.4%] vs 2336 of 9512 [28.2%]; AHR, 0.81; 95% CI, 0.76-0.86). The incidence of stroke was similar for male patients who underwent MAG and those who underwent SAG.
Figure 1. Seven-Year Mortality of Propensity-Matched Patients Undergoing Multiple Arterial Grafting (MAG) vs Single Arterial Grafting (SAG) for Coronary Artery Bypass Grafting in New York State From 2005 to 2014.
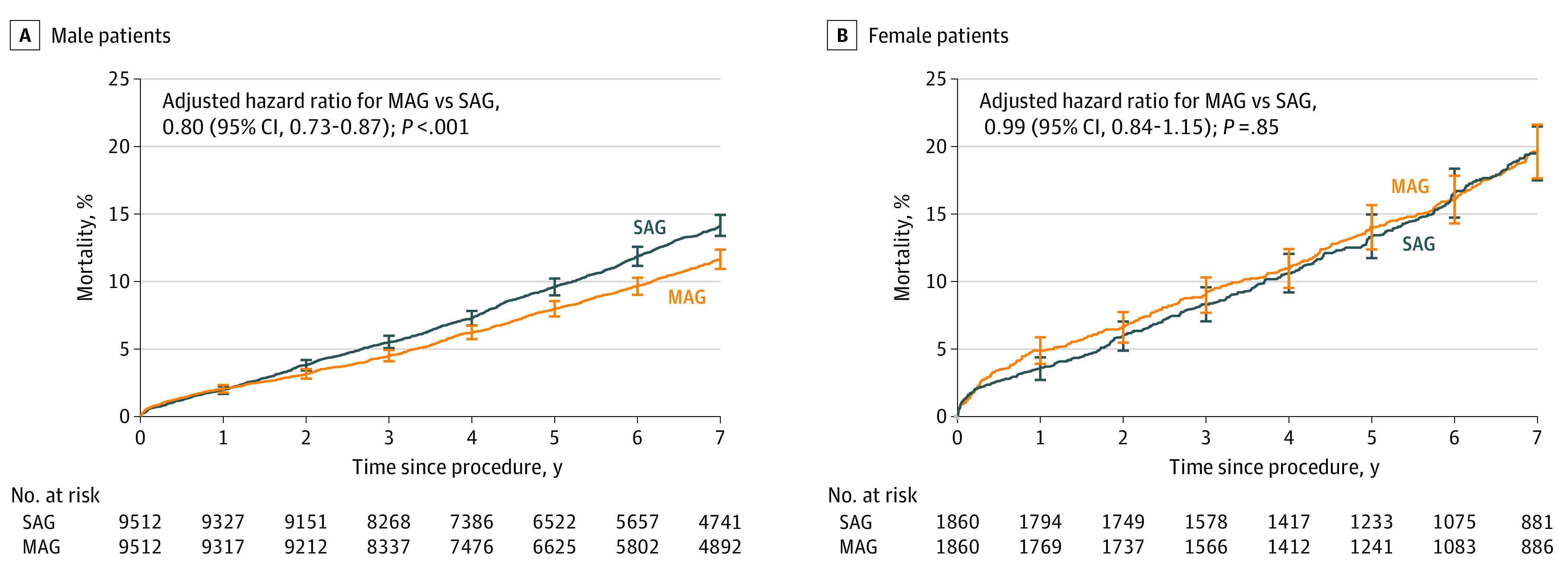
A, Male patients. B, Female patients. Vertical lines indicate 95% CIs.
Outcomes in Propensity-Matched Female Patients by Number of Arterial Grafts
The 1-year and 7-year outcomes for MAG and SAG propensity-matched female patients are summarized in Table 2. At 1 year, the incidence of mortality was similar for female patients who underwent MAG vs those who underwent SAG (91 of 1860 [4.9%] vs 66 of 1860 [3.5%]; AHR, 1.34; 95% CI, 0.97-1.84). The incidences of AMI, stroke, MACE, repeated revascularization, and MACCE were also similar between groups.
At 7 years, the incidence of mortality was similar for female patients who underwent MAG and those who underwent SAG (Kaplan-Meier estimates: 316 of 1860 [19.6%] vs 310 of 1860 [19.5%]; AHR, 0.99; 95% CI, 0.84-1.15) (Figure 1B). The incidences of stroke, repeated revascularization, MACCE, and MACE were also similar for female patients who underwent MAG and those who underwent SAG (Kaplan-Meier estimates: stroke, 126 of 1860 [8.2%] vs 106 of 1860 [6.9%]; AHR, 1.19; 95% CI, 0.92-1.54; repeated revascularization, 222 of 1860 [14.8%] vs 250 of 1860 [16.6%]; AHR 0.90; 95% CI, 0.75-1.08; MACCE, 478 of 1860 [29.0%] vs 486 of 1860 [29.9%]; AHR, 0.97; 95% CI, 0.86-1.10; MACE, 560 of 1860 [33.9%] vs 585 of 1860 [35.8%]; AHR, 0.94; 95% CI, 0.84-1.06). Female patients who underwent MAG had a significantly lower incidence of AMI at 7 years follow-up (Kaplan-Meier estimates: 120 of 1860 [8.0%] vs 154 of 1860 [10.2%]; AHR, 0.77; 95% CI, 0.60-0.97).
Analysis by Estimated Risk of Mortality
At 7 years, the incidence of mortality was lower for MAG vs SAG among low-risk male and female patients (Kaplan-Meier estimates: male, 681 of 9467 [8.6%] vs 882 of 9467 [11.1%]; AHR, 0.80; 95% CI, 0.73-0.89; female, 183 of 1669 [13.0%] vs 233 of 1669 [16.3%]; AHR, 0.80; 95% CI, 0.65-0.97) (Table 3, Figure 2A and B). Among high-risk male and female patients, the incidence of 7-year mortality was similar for MAG vs SAG (Kaplan-Meier estimates: male, 377 of 1013 [43.7%] vs 381 of 1013 [44.3%]; AHR, 0.95; 95% CI, 0.82-1.10; female, 179 of 424 [47.9%] vs 153 of 424 [42.3%]; AHR, 1.14; 95% CI, 0.91-1.42) (Table 3; Figure 2C and D).
Table 3. Seven-Year Mortality Rates of Propensity-Matched Risk-Stratified Patients After Multiple Arterial vs Single Arterial Coronary Artery Bypass Grafting in New York State From 2005 to 2014.
| Patient group | Multiple arterial grafting | Single arterial grafting | AHR (95% CI) | P value | ||
|---|---|---|---|---|---|---|
| Patients at risk at the end of the follow-up period, No. | Adverse event, No. (%)a | Patients at risk at the end of the follow-up period, No. | Adverse event, No. (%)a | |||
| Women | ||||||
| Overall | 999 | 362 (20.0) | 972 | 386 (21.5) | 0.92 (0.80-1.07) | .29 |
| Low risk (score <9) | 869 | 183 (13.0) | 834 | 233 (16.3) | 0.80 (0.65-0.97) | .02 |
| High risk (score ≥9) | 130 | 179 (47.9) | 138 | 153 (42.3) | 1.14 (0.91-1.42) | .26 |
| Men | ||||||
| Overall | 5408 | 1058 (11.9) | 5301 | 1263 (14.2) | 0.83 (0.77-0.90) | <.001 |
| Low risk (score ≤8) | 5081 | 681 (8.6) | 4980 | 882 (11.1) | 0.80 (0.73-0.89) | <.001 |
| High risk (score ≥9) | 327 | 377 (43.7) | 321 | 381 (44.3) | 0.95 (0.82-1.10) | .47 |
Abbreviation: AHR, adjusted hazard ratio.
Kaplan-Meier estimate.
Figure 2. Seven-Year Mortality of Propensity-Matched Patients Undergoing Multiple Arterial Grafting (MAG) vs Single Arterial Grafting (SAG) Coronary Artery Bypass Grafting in New York State From 2005 to 2014.
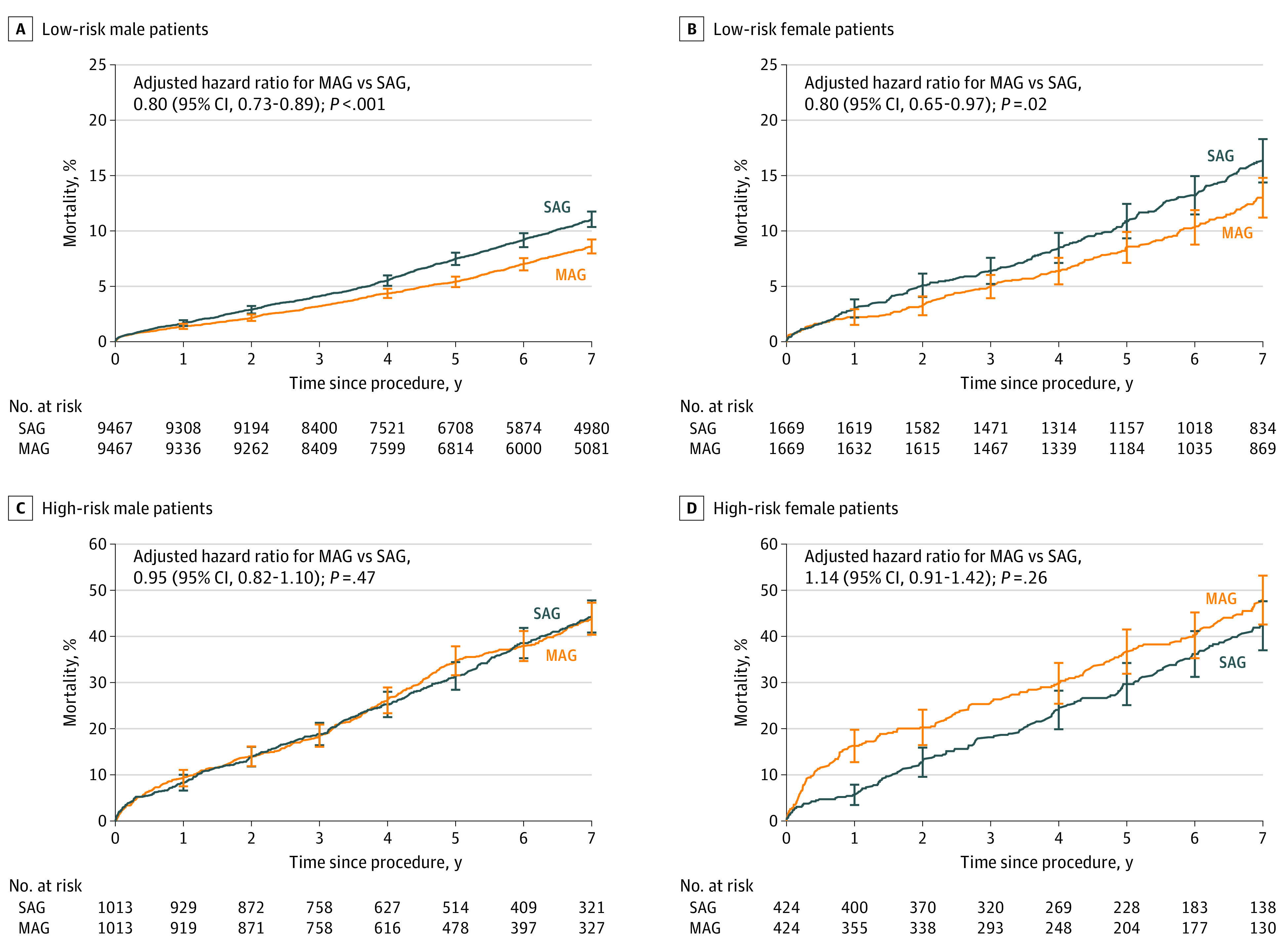
A, Low-risk male patients. B, Low-risk female patients. C, High-risk male patients. D, High-risk female patients. Vertical lines indicate 95% CIs.
Similar to mortality, at 7 years, low-risk male and female patients undergoing MAG had a significantly lower incidence of MACE compared with those undergoing SAG (Kaplan-Meier estimates: male, 1693 of 9467 [20.7%] vs 2139 of 9467 [25.8%]; AHR, 0.79; 95% CI, 0.74-0.84; female, 421 of 1669 [28.6%] vs 495 of 1669 [33.6%]; AHR, 0.84; 95% CI, 0.74-0.98). For high-risk patients, the incidence of 7-year MACE was similar for MAG and SAG for both male and female patients (Kaplan-Meier estimates: male, 459 of 1013 [52.0%] vs 457 of 1013 [52.3%]; AHR, 0.97; 95% CI, 0.85-1.11; female, 215 of 424 [56.1%] vs 184 of 424 [49.1%]; AHR, 1.20; 95% CI, 0.98-1.46).
Results of the analysis using different low-risk cutoffs showed that MAG was associated with lower mortality for all the explored low-risk levels in men, while for women, no differences between MAG and SAG were seen when cases with a risk score higher than 11 (corresponding to a 1-year mortality of 17.5%) were included (eTable 6 in the Supplement). In a fully adjusted model (including the risk score), MAG was inversely associated with mortality (AHR, 0.53; 95% CI, 0.46-0.61), while female sex (AHR, 1.44; 95% CI, 1.26-1.64; P < .001) and the risk score (AHR, 1.28; 95% CI, 1.27-1.29; P < .001) were positively associated with it (eTable 7 in the Supplement).
The results of the landmark analysis were consistent with the results of the main analysis (eTable 8 in the Supplement). Results of the analysis using gamma testing and the E-value are reported in eTable 9 and eTable 10 in the Supplement and show that only unmeasured confounders with moderate to high association with the treatment and the outcome would explain the reported results. Female patients receiving a single arterial graft and female patients receiving multiple arterial grafts had higher mortality than their male counterparts in separate fully adjusted Cox proportional hazards regression models (eTable 11 in the Supplement).
Discussion
In this study of patients undergoing CABG in New York state from 2005 to 2014, MAG was associated with longer survival and a lower rate of MACE for low-risk, but not high-risk, men and women. The risk thresholds at which the association of MAG with improved outcomes was lost differed between men and women.
Although a large body of observational evidence has compared follow-up data of patients undergoing SAG vs MAG, few studies, to our knowledge, have examined sex-related differences or have stratified the outcomes based on the preoperative risk profile of the patients. Our findings of a clear difference in the outcome of MAG between high-risk and low-risk patients is consistent with studies that have reported an age cutoff for the survival advantage associated with MAG11,22,23,24 and is biologically plausible because a shorter life expectancy may minimize any cardiac survival benefit associated with MAG.
The current literature on the sex-specific outcomes of MAG is based mainly on subanalyses of studies with a predominantly male population. The few observational studies that have focused specifically on women have reported conflicting results.13,14,25,26
In our study, similar to most previous literature, women had more baseline comorbidities than men, and the apparent lack of benefit associated with MAG in the overall female cohort may be due to the higher percentage of women in the high-risk category (13.0% vs 6.0% of men). However, we cannot exclude that other factors associated with sex and not measured in our database may have played a role in determining the observed differences. Also, women have a higher rate of postoperative sternal complications after bilateral internal thoracic artery grafting.14
Limitations
This analysis has important limitations. The granularity of the data in our database is limited for the purposes of this study. We had no data on the type and quality of the conduit used, the severity of target-vessel stenosis, or the location and quality of the target vessel. These data and other unmeasured variables may be important determinants of MAG outcomes, so our analysis cannot clarify whether the differences found between men and women are associated entirely with differences in baseline characteristics or with other sex-related confounders. Further investigations using more granular data sources are needed to address this important question.
In addition, we used a score developed from our database and not one of the more widely adopted surgical scores for risk stratification, which limits the generalizability of our findings. As in most observational comparative studies in surgery, it is possible that, despite extensive adjustment, unmeasured confounders and treatment allocation bias were present.27 Data on postoperative adherence with medical therapy were not available, and prescription and medication adherence may be different between men and women. Clinical follow-up data were limited to hospital visits and deaths within the state, which could have introduced a bias. Finally, the percentage of patients included in the high-risk group was relatively small, so an inability to identify significant treatment differences among the high-risk patients may be due to power limitations.
Conclusions
In this analysis of New York’s CSRS from 2005 to 2014, MAG was associated with longer survival and lower incidence of MACE among low-risk, but not high-risk, men and women. The threshold at which MAG was not associated with improved outcome was different in the 2 sexes, suggesting that important differences in the association of MAG may exist between sexes and that data derived from studies with a predominantly male population may not be applicable to women.
New studies, including randomized clinical trials, specifically designed to test the outcome of MAG vs SAG for women are needed. Our data also highlight the importance of a grafting strategy tailored to the risk profile of the individual patient.
eFigure. Details of Patient Inclusion and Exclusion
eTable 1. Provider Volume and Baseline Patient Characteristics of Male Patients Undergoing Single-Arterial and Multiple-Arterial Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 2. Provider Volume and Baseline Patient Characteristics of Female Patients Undergoing Single-Arterial (SAG) and Multiple-Arterial (MAG) Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 3. Provider Volume and Baseline Characteristics of Propensity-Matched Male Patients Undergoing Single-Arterial and Multiple-Arterial Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 4. Provider Volume and Baseline Characteristics of Propensity-Matched Female Patients Undergoing Single-Arterial (SAG) and Multiple-Arterial (MAG) Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 5. Operative (In-Hospital/30 day) Mortality Rates of Female and Male Propensity Matched Patients
eTable 6. Seven-Year Mortality Rates of Propensity-Matched Risk-Stratified Female and Male Patients According to Different Low Risk Score Cut-Offs After Multiple- (MAG) vs Single-Arterial (SAG) Coronary Artery Bypass Grafting in New York State Between 2005-2014
eTable 7. Fully Adjusted Cox Regression Models Evaluating the Effect of Multiple Arterial Grafting (MAG) on Death in the Overall Population
eTable 8. Landmark Analysis of Alive Female and Male Low- and High-Risk Patients at 30 Days
eTable 9. Sensitivity Analysis Using Gamma Testing
eTable 10. Sensitivity Analysis Using E-Value
eTable 11. Fully Adjusted Cox Regression Models Comparing Mortality Between Female and Male Patients Receiving Single Arterial Grafts (SAG), and Female and Male Patients Receiving Multiple Arterial Grafts (MAG)
References
- 1.Abramov D, Tamariz MG, Sever JY, et al. The influence of gender on the outcome of coronary artery bypass surgery. Ann Thorac Surg. 2000;70(3):800-805. doi: 10.1016/S0003-4975(00)01563-0 [DOI] [PubMed] [Google Scholar]
- 2.Ahmed WA, Tully PJ, Knight JL, Baker RA. Female sex as an independent predictor of morbidity and survival after isolated coronary artery bypass grafting. Ann Thorac Surg. 2011;92(1):59-67. doi: 10.1016/j.athoracsur.2011.02.033 [DOI] [PubMed] [Google Scholar]
- 3.Koch CG, Khandwala F, Nussmeier N, Blackstone EH. Gender and outcomes after coronary artery bypass grafting: a propensity-matched comparison. J Thorac Cardiovasc Surg. 2003;126(6):2032-2043. doi: 10.1016/S0022-5223(03)00950-4 [DOI] [PubMed] [Google Scholar]
- 4.Fukui T, Takanashi S. Gender differences in clinical and angiographic outcomes after coronary artery bypass surgery. Circ J. 2010;74(10):2103-2108. doi: 10.1253/circj.CJ-10-0275 [DOI] [PubMed] [Google Scholar]
- 5.Alam M, Lee V-V, Elayda MA, et al. Association of gender with morbidity and mortality after isolated coronary artery bypass grafting: a propensity score matched analysis. Int J Cardiol. 2013;167(1):180-184. doi: 10.1016/j.ijcard.2011.12.047 [DOI] [PubMed] [Google Scholar]
- 6.Alam M, Bandeali SJ, Kayani WT, et al. Comparison by meta-analysis of mortality after isolated coronary artery bypass grafting in women versus men. Am J Cardiol. 2013;112(3):309-317. doi: 10.1016/j.amjcard.2013.03.034 [DOI] [PubMed] [Google Scholar]
- 7.Ennker IC, Albert A, Pietrowski D, Bauer K, Ennker J, Florath I. Impact of gender on outcome after coronary artery bypass surgery. Asian Cardiovasc Thorac Ann. 2009;17(3):253-258. doi: 10.1177/0218492309104746 [DOI] [PubMed] [Google Scholar]
- 8.Humphries KH, Gao M, Pu A, Lichtenstein S, Thompson CR. Significant improvement in short-term mortality in women undergoing coronary artery bypass surgery (1991 to 2004). J Am Coll Cardiol. 2007;49(14):1552-1558. doi: 10.1016/j.jacc.2006.08.068 [DOI] [PubMed] [Google Scholar]
- 9.Gaudino M, Puskas JD, Di Franco A, et al. Three arterial grafts improve late survival: a meta-analysis of propensity-matched studies. Circulation. 2017;135(11):1036-1044. doi: 10.1161/CIRCULATIONAHA.116.025453 [DOI] [PubMed] [Google Scholar]
- 10.Gaudino M, Benedetto U, Fremes S, et al. ; RADIAL Investigators . Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-2077. doi: 10.1056/NEJMoa1716026 [DOI] [PubMed] [Google Scholar]
- 11.Chikwe J, Sun E, Hannan EL, et al. Outcomes of second arterial conduits in patients undergoing multivessel coronary artery bypass graft surgery. J Am Coll Cardiol. 2019;74(18):2238-2248. doi: 10.1016/j.jacc.2019.08.1043 [DOI] [PubMed] [Google Scholar]
- 12.Samadashvili Z, Sundt TM III, Wechsler A, et al. Multiple versus single arterial coronary bypass graft surgery for multivessel disease. J Am Coll Cardiol. 2019;74(10):1275-1285. doi: 10.1016/j.jacc.2019.06.067 [DOI] [PubMed] [Google Scholar]
- 13.Schwann TA, Engoren M, Bonnell M, Clancy C, Habib RH. Comparison of late coronary artery bypass graft survival effects of radial artery versus saphenous vein grafting in male and female patients. Ann Thorac Surg. 2012;94(5):1485-1491. doi: 10.1016/j.athoracsur.2012.05.029 [DOI] [PubMed] [Google Scholar]
- 14.Dimitrova KR, Hoffman DM, Geller CM, et al. Radial artery grafting in women improves 15-year survival. J Thorac Cardiovasc Surg. 2013;146(6):1467-1473. doi: 10.1016/j.jtcvs.2012.10.004 [DOI] [PubMed] [Google Scholar]
- 15.Jabagi H, Tran DT, Hessian R, Glineur D, Rubens FD. Impact of gender on arterial revascularization strategies for coronary artery bypass grafting. Ann Thorac Surg. 2018;105(1):62-68. doi: 10.1016/j.athoracsur.2017.06.054 [DOI] [PubMed] [Google Scholar]
- 16.Sheifer SE, Canos MR, Weinfurt KP, et al. Sex differences in coronary artery size assessed by intravascular ultrasound. Am Heart J. 2000;139(4):649-653. doi: 10.1016/S0002-8703(00)90043-7 [DOI] [PubMed] [Google Scholar]
- 17.O’Connor NJ, Morton JR, Birkmeyer JD, Olmstead EM, O’Connor GT; Northern New England Cardiovascular Disease Study Group . Effect of coronary artery diameter in patients undergoing coronary bypass surgery. Circulation. 1996;93(4):652-655. doi: 10.1161/01.CIR.93.4.652 [DOI] [PubMed] [Google Scholar]
- 18.Wu C, Camacho FT, Wechsler AS, et al. Risk score for predicting long-term mortality after coronary artery bypass graft surgery. Circulation. 2012;125(20):2423-2430. doi: 10.1161/CIRCULATIONAHA.111.055939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenbaum PR, Rubin DB. Assessing sensitivity to an unobserved binary covariate in an observational study with binary outcome. J Royal Stat Soc Ser B (Methodological). 1983;45(2):212-218. doi: 10.1111/j.2517-6161.1983.tb01242.x [DOI] [Google Scholar]
- 20.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 21.Faries DE, Leon AC, Haro JM, Obenchain RL, eds. Analysis of Observational Health Care Data Using SAS. SAS Institute Inc; 2010. [Google Scholar]
- 22.Kieser TM, Lewin AM, Graham MM, et al. ; APPROACH Investigators . Outcomes associated with bilateral internal thoracic artery grafting: the importance of age. Ann Thorac Surg. 2011;92(4):1269-1275. doi: 10.1016/j.athoracsur.2011.05.083 [DOI] [PubMed] [Google Scholar]
- 23.Benedetto U, Codispoti M. Age cutoff for the loss of survival benefit from use of radial artery in coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2013;146(5):1078-1084. doi: 10.1016/j.jtcvs.2013.07.025 [DOI] [PubMed] [Google Scholar]
- 24.Benedetto U, Amrani M, Raja SG; Harefield Cardiac Outcomes Research Group . Guidance for the use of bilateral internal thoracic arteries according to survival benefit across age groups. J Thorac Cardiovasc Surg. 2014;148(6):2706-2711. doi: 10.1016/j.jtcvs.2014.07.088 [DOI] [PubMed] [Google Scholar]
- 25.Lawton JS, Barner HB, Bailey MS, et al. Radial artery grafts in women: utilization and results. Ann Thorac Surg. 2005;80(2):559-563. doi: 10.1016/j.athoracsur.2005.02.055 [DOI] [PubMed] [Google Scholar]
- 26.Pullan M, Kirmani BH, Conley T, et al. The effect of patient sex on survival in patients undergoing isolated coronary artery bypass surgery receiving a radial artery. Eur J Cardiothorac Surg. 2015;47(2):324-330. doi: 10.1093/ejcts/ezu100 [DOI] [PubMed] [Google Scholar]
- 27.Gaudino M, Di Franco A, Rahouma M, et al. Unmeasured confounders in observational studies comparing bilateral versus single internal thoracic artery for coronary artery bypass grafting: a meta-analysis. J Am Heart Assoc. 2018;7(1):e008010. doi: 10.1161/JAHA.117.008010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Details of Patient Inclusion and Exclusion
eTable 1. Provider Volume and Baseline Patient Characteristics of Male Patients Undergoing Single-Arterial and Multiple-Arterial Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 2. Provider Volume and Baseline Patient Characteristics of Female Patients Undergoing Single-Arterial (SAG) and Multiple-Arterial (MAG) Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 3. Provider Volume and Baseline Characteristics of Propensity-Matched Male Patients Undergoing Single-Arterial and Multiple-Arterial Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 4. Provider Volume and Baseline Characteristics of Propensity-Matched Female Patients Undergoing Single-Arterial (SAG) and Multiple-Arterial (MAG) Isolated-Coronary Artery Bypass Grafting (CABG) Surgery in New York State From 2005-2014
eTable 5. Operative (In-Hospital/30 day) Mortality Rates of Female and Male Propensity Matched Patients
eTable 6. Seven-Year Mortality Rates of Propensity-Matched Risk-Stratified Female and Male Patients According to Different Low Risk Score Cut-Offs After Multiple- (MAG) vs Single-Arterial (SAG) Coronary Artery Bypass Grafting in New York State Between 2005-2014
eTable 7. Fully Adjusted Cox Regression Models Evaluating the Effect of Multiple Arterial Grafting (MAG) on Death in the Overall Population
eTable 8. Landmark Analysis of Alive Female and Male Low- and High-Risk Patients at 30 Days
eTable 9. Sensitivity Analysis Using Gamma Testing
eTable 10. Sensitivity Analysis Using E-Value
eTable 11. Fully Adjusted Cox Regression Models Comparing Mortality Between Female and Male Patients Receiving Single Arterial Grafts (SAG), and Female and Male Patients Receiving Multiple Arterial Grafts (MAG)


