Summary
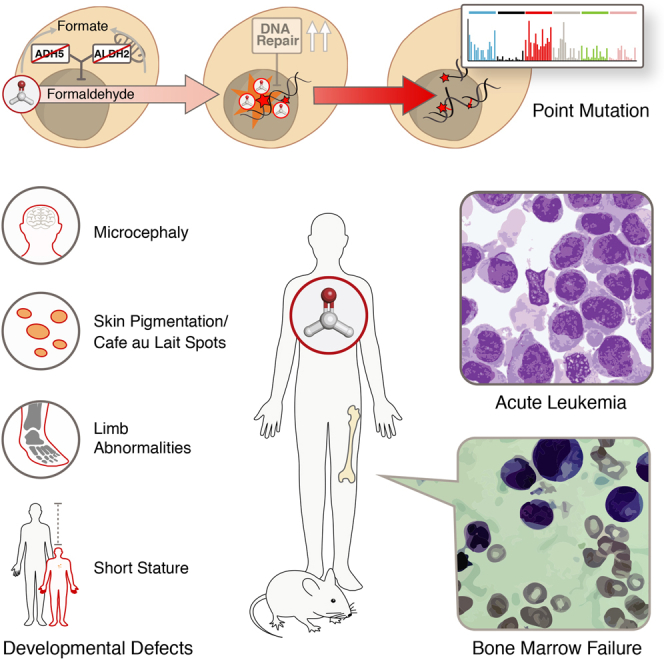
Reactive aldehydes arise as by-products of metabolism and are normally cleared by multiple families of enzymes. We find that mice lacking two aldehyde detoxifying enzymes, mitochondrial ALDH2 and cytoplasmic ADH5, have greatly shortened lifespans and develop leukemia. Hematopoiesis is disrupted profoundly, with a reduction of hematopoietic stem cells and common lymphoid progenitors causing a severely depleted acquired immune system. We show that formaldehyde is a common substrate of ALDH2 and ADH5 and establish methods to quantify elevated blood formaldehyde and formaldehyde-DNA adducts in tissues. Bone-marrow-derived progenitors actively engage DNA repair but also imprint a formaldehyde-driven mutation signature similar to aging-associated human cancer mutation signatures. Furthermore, we identify analogous genetic defects in children causing a previously uncharacterized inherited bone marrow failure and pre-leukemic syndrome. Endogenous formaldehyde clearance alone is therefore critical for hematopoiesis and in limiting mutagenesis in somatic tissues.
Keywords: hematopoietic stem cells, hematopoiesis, bone marrow failure, immunodeficiency, formaldehyde, oncometabolite, ageing, DNA damage, mutagenesis, cancer
Graphical Abstract
Highlights
-
•
Toxic levels of genotoxic formaldehyde are produced endogenously in mammals
-
•
Two enzymes, ADH5 and ALDH2, are critical for clearance of endogenous formaldehyde
-
•
Their loss in mice and humans causes defective hematopoiesis and increased cancer
-
•
Elevated formaldehyde causes DNA damage and mutation signature found in many cancers
Dingler et al. show that formaldehyde is produced endogenously at sufficient levels to induce and overwhelm DNA repair. Two enzymes, ADH5 and ALDH2, are critical in clearance of formaldehyde, whose loss results in a bone marrow failure and leukemia syndrome of purely metabolic origin.
Introduction
Reactive chemistry drives many fundamental metabolic processes of life. However, the reactive metabolites involved are often toxic because they can inappropriately attack cellular constituents, ultimately driving degenerative changes associated with aging and carcinogenesis. The best-studied group of such molecules are reactive oxygen species (ROS), which have been implicated in a wide range of (patho)physiological processes. A new and emerging group of reactive metabolites are endogenous aldehydes, and the threat they pose, combined with their molecular diversity, could explain why we possess so many enzymes to detoxify them. There are at least 19 distinct aldehyde dehydrogenases (ALDHs) as well as a number of enzymes that process aldehyde-glutathione conjugates (glutathione S-transferases [GSTs] and ADH5) (Jackson et al., 2011). However, we understand very little about the physiological importance of different aldehydes, which enzymes metabolize them, and whether these detoxifying enzymes are functionally linked to one another.
ALDH2 is a mitochondrial ALDH that utilizes NAD+ as a cofactor to oxidize acetaldehyde to acetate, which is then utilized in the Krebs cycle (Jacobson and Bernofsky, 1974). ALDH2 is important in ethanol metabolism, and deficiency of this enzyme is very common in humans, caused by a dominant-negative mutation in the ALDH2 gene (ALDH2∗2) that destabilizes the tetrameric enzyme, resulting in a red flushing reaction upon alcohol consumption because of buildup of acetaldehyde (Harada et al., 1981). In contrast to ALDH2, ADH5 is a cytosolic enzyme that does not act on free aldehydes but oxidizes the spontaneously formed glutathione (GSH) conjugate of formaldehyde to formate, which can be used in one-carbon metabolism. Formaldehyde likely originates from a variety of cellular sources, such as histone demethylation and folic acid decomposition (Burgos-Barragan et al., 2017; Uotila and Koivusalo, 1974). These two examples illustrate how aldehyde-processing enzymes convert the two simplest aldehydes into molecules useful for essential metabolism.
Recent research has established that aldehyde clearance constitutes just the first tier of protection against these molecules. If this is genetically ablated, as in Aldh2−/− or Adh5−/− mice, then DNA crosslink repair by Fanconi anemia (FA) genes provides an essential backup. Thus, the aldehydes detoxified by these respective enzymes are genotoxic and, in the case of acetaldehyde, cause DNA interstrand crosslinks (Hodskinson et al., 2020). This is why, when ALDH2 or ADH5 deficiency is combined with loss of the crosslink repair gene Fancd2, mice rapidly develop hematopoietic failure and acute leukemia (Garaycoechea et al., 2012, 2018; Langevin et al., 2011; Pontel et al., 2015). These findings lead to the proposal that aldehydes may be metabolic drivers for the human genetic disease FA, where patients lack the DNA repair pathway that provides the second tier of protection. An additional intriguing observation is that exposing cells to formaldehyde destabilizes the BRCA2 protein, the genotoxin itself causing DNA repair deficiency and genomic instability (Tan et al., 2017). This is postulated to explain why women haploinsufficient for BRCA2 might be predisposed to breast cancer without loss of their functional BRCA2 allele. What is absent in these studies is evidence to directly define which aldehyde(s) are driving these effects because of the lack of reliable methods to identify and quantify aldehydes in organisms. In this study, we discover that endogenous formaldehyde is the main physiological substrate for ALDH2 and ADH5. We define the severe hematopoietic consequences and explain what happens when this clearance fails in mice and humans.
Results
Genetic Redundancy between Aldh2 and Adh5 in Mice
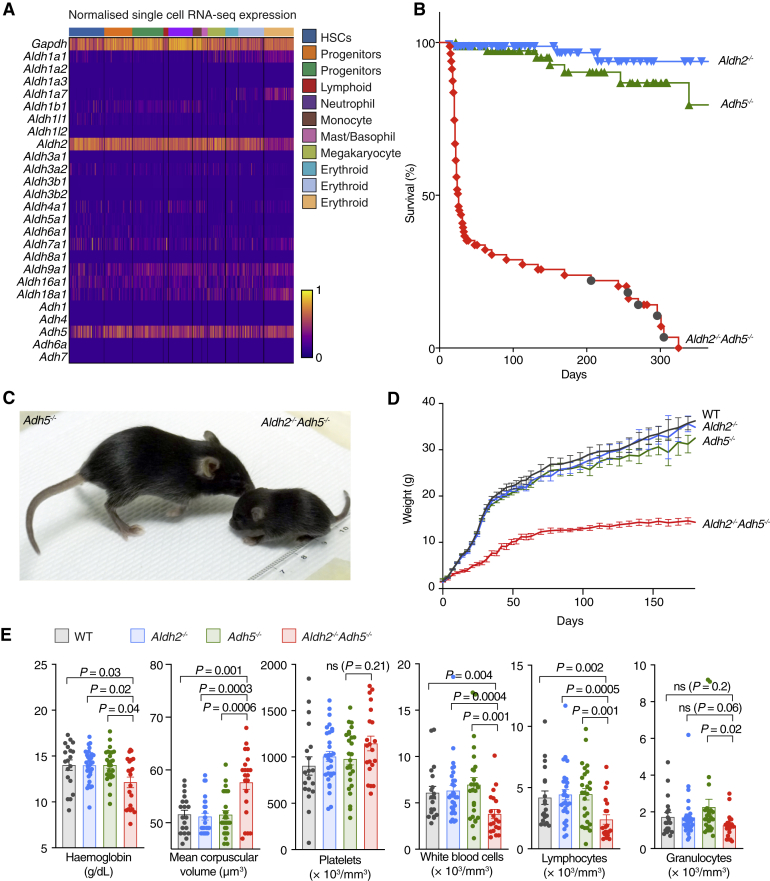
We first set out to determine the expression profile of the many aldehyde-detoxifying enzymes across hematopoietic lineages. Single-cell RNA sequencing (scRNA-seq) of primitive murine bone marrow cells shows that expression of two genes, Aldh2 and Adh5, stands out as being widespread across hematopoietic progenitors (Figure 1A). To find out whether these two enzymes functionally interact with each other, we crossed Aldh2−/− with Adh5−/− mice to obtain Aldh2−/−Adh5−/− mice. Although indistinguishable at birth (Figure S1A), their growth is severely compromised, and most die in the perinatal window without an obvious cause of death. Importantly, a small proportion of Aldh2−/−Adh5−/− mice survive into adulthood; these animals are significantly growth retarded, small, and lean (Figures 1B–1D, S1A, and S1B). Aged Aldh2−/−Adh5−/− mice continued to remain considerably smaller than wild-type littermate controls, and none lived longer than 47 weeks. This is due to a general decline in condition and predisposition to cancer, including thymic T cell leukemia (Figure 1B and S1C–S1E; Table S1). Furthermore, Aldh2−/−Adh5−/− mice are mildly anemic with macrocytosis (increased red cell mean corpuscular volume) and have depressed white blood cell counts, predominantly in the lymphocyte fraction (Figure 1E). In summary, combined inactivation of the aldehyde-clearing enzymes ALDH2 and ADH5 leads to perinatal lethality, growth failure, lymphopenia, and lymphoid malignancies.
Figure 1.
Postnatal Lethality, Stunted Growth, and Cancer Predisposition in Aldh2−/−Adh5−/− Mice
(A) Gene expression analysis of Aldh and Adh gene families by scRNA-seq in WT bone marrow progenitor cells (Lin− c-Kit+ Sca-1+). The colored bar at the top represents the assigned lineage of cell transcriptomes.
(B) Kaplan-Meier survival curve of Aldh2−/−, Adh5−/−, and Aldh2−/−Adh5−/− mice (n = 166, 89, 67). Dark gray circles indicate cancer deaths.
(C) Photograph of Aldh2−/−Adh5−/− mouse (right) and its littermate Adh5−/− control (left).
(D) Total body mass as mean ± SEM of WT, Aldh2−/−, Adh5−/−, and Aldh2−/−Adh5−/− mice (initial n = 35, 58, 60, 16).
(E) Blood parameters in Aldh2−/−Adh5−/− mice with controls (mean ± SEM; n = 21, 30, 26, 19, left to right).
The p values were determined by two-tailed Mann-Whitney U test. See also Figure S1 and Table S1.
Deficiency in Aldh2 and Adh5 Disrupts Hemato-lymphoid Development
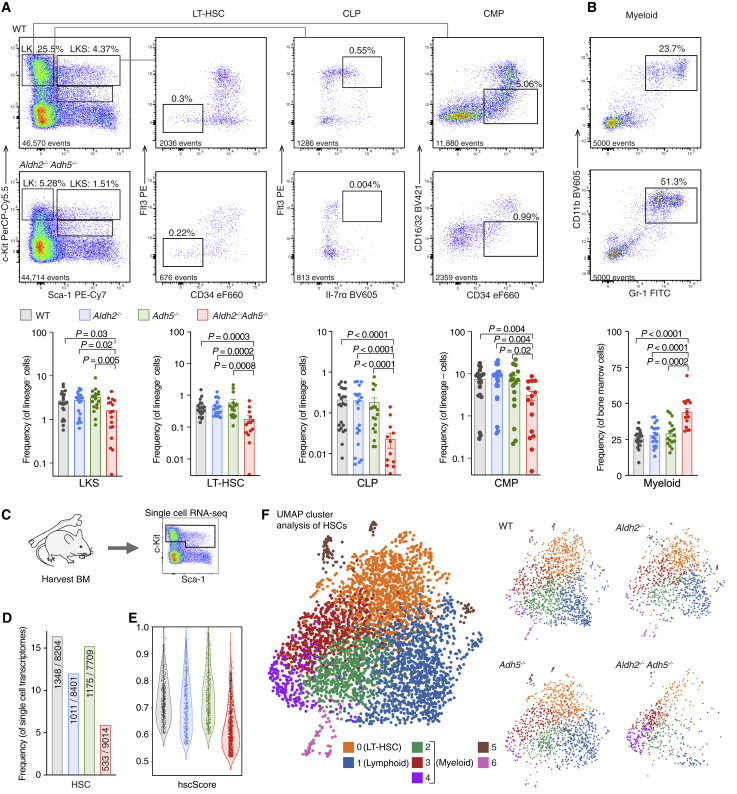
The reduced blood counts in Aldh2−/−Adh5−/− mice prompted us to carry out a detailed analysis of blood production. Flow cytometry analysis of the bone marrow indicates a reduced proportion of LKS (Lineage− [Lin−] c-Kit+ Sca-1+) cells, representing hematopoietic stem cells (HSCs) and progenitors in which we observe reduced long-term HSCs (LT-HSCs; Lin− c-Kit+ Sca-1+ Flt3− CD34− cells; Figure 2A) and multipotent progenitor cells (MPPs; Lin− c-Kit+ Sca-1+ Flt3+ CD34+ cells; Figure S2A). Among more differentiated progenitors, we find reduced common lymphoid progenitors (CLPs, Lin− c-Kitlo Sca-1+ Flt3+ interleukin-7Rα [IL-7R⍺]+ cells). Although the common myeloid progenitor (CMP) population (Lin− c-Kit+ Sca-1− CD34+ CD16/32lo cells) is mildly reduced, it is proportionately less affected so that the relative myeloid contribution in bone marrow and blood is increased significantly (Figure 2B; Figure S2A). To functionally validate the hematopoietic defect in Aldh2−/−Adh5−/−, we transplanted its bone marrow cells (CD45.2+) with wild-type competitor-derived cells (CD45.1+) into lethally irradiated recipients (CD45.1+ CD45.2+). Over a period of 4 months, Aldh2−/− Adh5−/−-transplanted bone marrow gave lower reconstitution across B220+ (B cells), CD4+/CD8+ (T cells), and Gr-1+/Mac-1+ (myeloid cells) in the blood, with the contribution to lymphoid lineages decreasing over time. Correspondingly, we also observed a reduced contribution to LT-HSC, LKS, and CLP compartments at 4 months (Figures S2B–S2D).
Figure 2.
Disrupted Aldehyde Catabolism Compromises Hematopoiesis
(A and B) Representative flow cytometry plots from Aldh2−/−Adh5−/− and WT mice showing bone marrow LK, LKS, LT-HSC, CLP, and CMP (A) and myeloid populations (B). Bottom: quantification of the respective populations assessed by flow cytometry in 2- to 30-week-old Aldh2−/−Adh5−/− mice with age-matched controls (mean ± SEM; n = 24, 20, 17, 17, left to right).
(C) scRNA-seq analysis of HSPCs from a 6-week-old female Aldh2−/−Adh5−/− mouse with age- and sex-matched controls.
(D) Fraction of single-cell transcriptomes assigned to the HSC cell identity (numerator) from total transcriptomes analyzed (denominator).
(E) hscScore analysis of single-cell transcriptomes identified as HSCs.
(F) UMAP visualization of HSC transcriptomes colored by cluster. On the left, all 4 genotypes are superimposed; on the right, individual genotypes are shown separately to highlight variation in distribution between the clusters.
The p values were determined by two-tailed Mann-Whitney U test. See also Figures S2 and S3 and Tables S2 and S5.
To further characterize hematopoiesis in Aldh2−/−Adh5−/− mice, we applied droplet-based scRNA-seq to LK (Lin− c-Kit+) and Lin− c-Kitlo Sca-1+ cells of Aldh2−/−Adh5−/− mice to profile the heterogeneous stem and progenitor populations in an unbiased fashion (Figures 2C–2F), sampling approximately 8,000 transcriptomes per genotype that were clustered using the Louvain algorithm. Each cluster was assigned a cell identity based on expression of marker genes (Figure S3A; see STAR Methods for details). Strikingly, hematopoietic stem and progenitor cells (HSPCs) and erythroid progenitors in Aldh2−/−Adh5−/− mice showed the greatest transcriptional change from controls (Figures S3B and S3D). Analysis of differentially expressed genes in Aldh2−/−Adh5−/− erythroid progenitors indicates more cells in the S and G2/M cell cycle phase as well as enrichment of genes regulating apoptosis (Figures S3E and S3F; Table S2). Focusing on the HSPCs, these are significantly under-represented in Aldh2−/−Adh5−/− bone marrow (Figure 2D) and rank lower in their hscScore (Hamey and Göttgens, 2019), a metric quantifying transcriptional similarity to reconstituting LT-HSCs (Figure 2E). To assess how the HSC population in Aldh2−/−Adh5−/− differed from controls, we submitted the differentially expressed genes to Gene Ontology (GO) term enrichment analysis to find multiple gene sets involved in lineage differentiation (Table S3). We proceeded to explore whether HSCs were lineage biased by fine clustering of this population. This generated 7 clusters (0–6), with cluster 0 containing the transcriptional signature associated with LT-HSCs (such as high Procr and Mecom expression), cluster 1 harboring lymphoid signature genes (such as Dntt [Tdt]), whereas clusters 2, 3, and 4 contain myeloid signature genes (such as Mpo) (for a full list of genes, see Table S4). Intriguingly, HSCs from Aldh2−/−Adh5−/− mice are mostly represented in clusters 3 and 4 (myeloid) and under-represented in clusters 0 (LT-HSCs) and 1 (lymphoid) (Figure 2F). In summary, scRNA-seq analysis of Aldh2−/−Adh5−/− bone marrow reveals a decreased frequency and qualitative score of HSCs with preferential loss of cells with LT-HSC and lymphoid profiles, in agreement with the characterization by cell-surface markers and transplantation experiments.
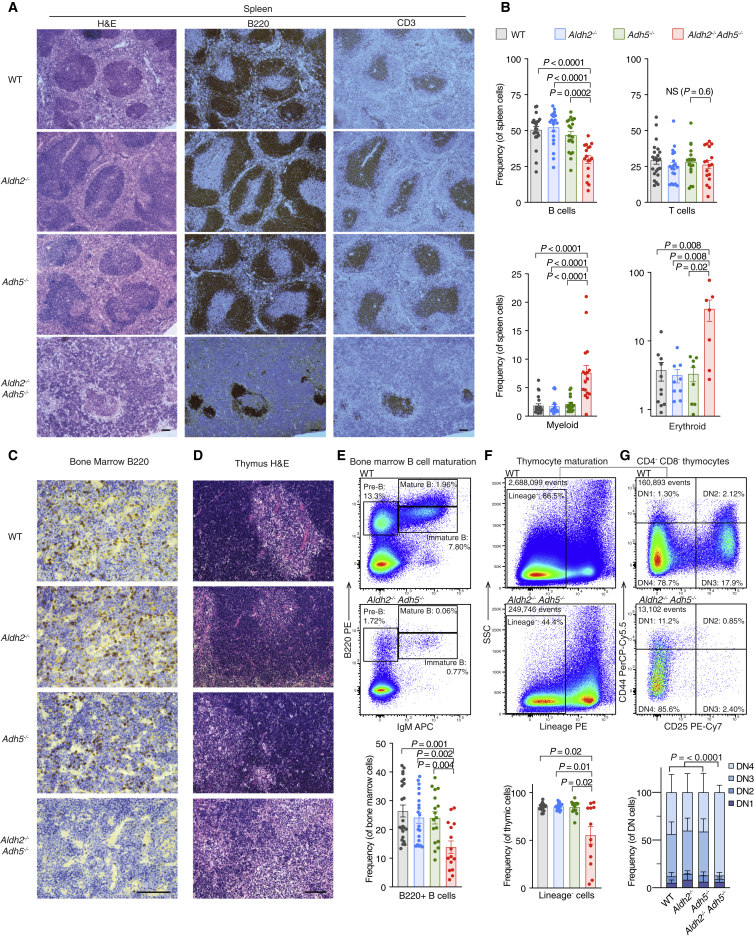
Although a CLP defect could account for reduced circulating lymphocytes, we wanted to assess for defects in T and B cell maturation in surviving Aldh2−/−Adh5−/− mice. Immunohistological analysis of the Aldh2−/−Adh5−/− spleens showed a gross disruption of lymphoid follicle architecture (Figure 3A), which is less numerous and depleted in B cells (Figure 3B). Indeed, we find a profound defect in B cell development with a reduction in total B220+ B cells in the bone marrow (Figures 3C and 3E). Attempts to narrow down the loss of B cells to a specific developmental stage revealed heterogeneity, with some animals exhibiting the strongest defect in the early pre-B cell (B220+ immunoglobulin M [IgM]−) population, whereas others had a near-normal proportions of pre-B cells in the bone marrow but were profoundly deficient in immature (B220+ IgM+) and mature (B220+ IgMhi) B cells (Figure S2E). The spleen also showed increased myeloid (CD11b+ Gr-1+) and erythroid (Ter-119+) cells (Figure 3B), likely representing stress-induced extramedullary hematopoiesis in response to insufficient blood production.
Figure 3.
Aldehyde Catabolism Is Essential for Lymphoid Development
(A) Spleen histology (hematoxylin and eosin [H&E stain]) and immunohistochemistry for B220 or CD3.
(B) Quantification of splenic B, T, myeloid, and erythroid precursors assessed by flow cytometry (n = 23, 20, 19, 17, left to right).
(C) Bone marrow immunohistochemistry for B220.
(D) Thymus histology (H&E stain).
(E) Representative flow cytometry plots showing bone marrow B cell development and quantification of total B220+ cells (mean ± SEM; n = 23, 20, 19, 15, left to right).
(F and G) Representative flow cytometry plots and quantification of the thymic Lin− population (F) and Lin− CD4− CD8− (DN) populations defined by CD44 and CD25 expression (G). Mice analyzed for thymic Lin− populations were 2–30 weeks old (n = 23, 20, 19, 15, left to right). Mice analyzed for thymic DN populations were older than 30 weeks (n = 7, 7, 5, 5 mice, left to right).
All bar graphs are shown with mean ± SEM. The p values were determined by two-tailed Mann-Whitney U test except for (G), where pairwise χ2 tests of average distributions were performed. Scale bars indicate 100 μm. See also Figures S2 and S3.
Despite normal T cell numbers in the peripheral blood and spleen (Figures 3B and S2A), thymi of Aldh2−/−Adh5−/− mice revealed marked atrophy and loss of cellularity (Figures 3D, 3F, and S2F). Thymocyte maturation was also perturbed, with specific loss of cells at the double-negative (DN, Lin− CD4− CD8−) DN2 (CD44+ CD25+) and DN3 (CD44− CD25+) stages of thymic development (Figure 3G). These thymic pathologies were most consistently observed in older (>30 weeks old) animals, whereas younger animals (<10 weeks old) exhibited considerable heterogeneity; some animals were enriched for earlier stages of thymic development (DN1–DN3), whereas others lacked early DN cells and were predominantly enriched for DN4 like the older mice (Figure S2G). Analysis of the competitive repopulation experiment showed a particularly low contribution of the Aldh2−/−Adh5−/− donor to the DN compartment (Figure S2H); recapitulating the heterogeneity in DN stages, about half of the recipients showed a strong DN1 bias (Figure S2I). In conclusion, accumulation of aldehyde(s) in Aldh2−/−Adh5−/− mice impairs hematopoiesis in several respects: early blood progenitors such as LT-HSCs and CLPs are depleted, but more striking defects are seen in the more committed cell populations of T and B cells, for which impaired maturation ultimately manifests in disordered secondary lymphoid structures.
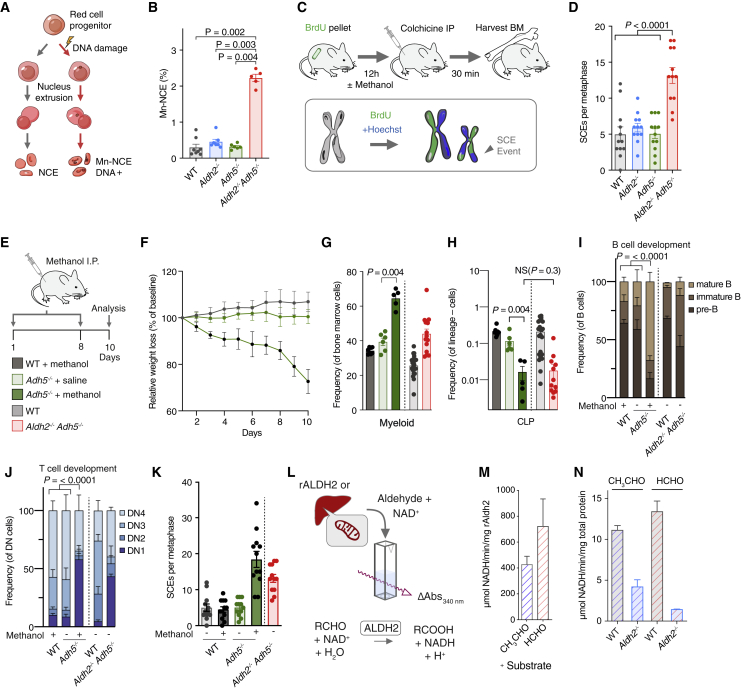
Induction of DNA Repair in Aldh2−/−Adh5−/− Mice and Consequences of Formaldehyde Challenge in Adh5−/− Mice
Aldehyde(s) detoxified by ALDH2 or ADH5 are genotoxic, and the DNA damage they cause necessitates crosslink repair (Langevin et al., 2011; Pontel et al., 2015). However, in Aldh2−/−Adh5−/− mice, DNA repair is genetically intact, so it is important to address whether these animals show any evidence of DNA damage and engagement of DNA repair. In the first instance, we investigated genome instability in the hematopoietic compartment of Aldh2−/−Adh5−/− mice. During the course of maturation, red blood cells (RBCs) extrude and lose their nucleus; however, broken chromosomes can partition into micronuclei that can persist in enucleated RBCs (Figure 4A; Bryce et al., 2007). Peripheral blood from single-mutant Aldh2−/− and Adh5−/− mice shows no strong increase in micronuclei over their wild-type controls. However, Aldh2−/−Adh5−/− RBCs contained increased numbers of micronucleated cells, indicating genome instability and chromosome breakage in these mice (Figure 4B). Next, we set out to assess the DNA repair response by quantifying sister chromatid exchanges (SCEs) in bone marrow using a protocol that assesses these events in vivo (Giri and Chatterjee, 1998; Orsburn et al., 2010). An SCE event requires crossover mediated by homologous recombination (HR) and is indicative of active DNA repair (Figure 4C). The mean number of SCE events per metaphase is 5 in the wild type (WT), 6 in Aldh2−/−, and 5 in Adh5−/−. In contrast, Aldh2−/−Adh5−/− mice show a more than 2-fold increase to an average of 13 SCE events (Figure 4D). Finally, by interrogating the single-cell transcriptomes of HSPCs, we observe increased expression of DNA repair genes in Aldh2−/−Adh5−/− mice (Figure S3G). Inspection of the most overexpressed DNA repair genes revealed a number of recognized DNA crosslink repair genes, including Brca1, Brca2, Fanci, Fancd2, Brip1, and Neil3 (Figures S3H and S3I). Importantly, DNA repair genes remained overrepresented after accounting for cell cycle phase (Table S5), which has been associated with expression of DNA repair genes (Walter et al., 2015). Overall, accumulation of endogenous aldehyde(s) in Aldh2−/−Adh5−/− mice elicits vigorous induction of HR-mediated DNA repair in hematopoietic cells.
Figure 4.
DNA Damage in Aldh2−/−Adh5−/− Mice and Methanol Challenge of Adh5−/− Mice Phenocopies the Double Mutant
(A) Scheme of the micronucleus assay.
(B) Micronuclei in Aldh2−/−Adh5−/− mice and controls. (mean ± SEM, n = 8, 7, 6, 5, left to right).
(C) SCE analysis in bone marrow cells.
(D) Quantification of SCE in Aldh2−/−Adh5−/− mice and controls. (mean ± SEM, n = 12 metaphases per group).
(E) Treatment of mice with intraperitoneal methanol injection.
(F) Percentage of weight loss relative to baseline weight on day 0 (mean ± SD, n = 10; WT + methanol, 6; Adh5−/− + saline and 6; Adh5−/− + methanol).
(G and H) Frequency of bone marrow myeloid (CD11b+ Gr-1+) and CLP cells (mean ± SEM, n = 8, 6, 5, left to right).
(I and J), Frequency of bone marrow B cell (pre-B, immature and mature) and thymus DN populations (DN1–DN4) (mean and SEM; n = 8, 6, 5 mice, left to right).
(K) Quantification of SCEs of methanol-treated mice and controls. n = 12 metaphases per group.
(L) ALDH activity assays on recombinant ALDH2 (rALDH2) or mitochondrial extracts from WT or Aldh2−/− liver.
(M and N) ALDH activity performed with acetaldehyde (CH3CHO) and formaldehyde (HCHO) substrates using rALDH2 (M); WT and Aldh2−/− liver mitochondrial extract (N). Activity is expressed as micromolar NADH per minute per milligram of total protein (mean and SD; n = 2).
The p values were determined by two-tailed Mann-Whitney U test, except for (I) and (J), where pairwise χ2 tests of average distributions were performed. See also Figures S3 and S4.
The fact that combined inactivation of Aldh2 and Adh5 causes such a severe phenotype suggests that they might have redundant aldehyde detoxification functions; many ALDH enzymes have overlapping substrate specificities. ADH5 is the main enzyme that detoxifies formaldehyde; nevertheless, Adh5−/− mice are largely normal. This could be because formaldehyde accumulation in these mice is restrained by ALDH2. A simple prediction is that challenging Adh5−/− mice with methanol would cause formaldehyde to accumulate (Pontel et al., 2015), which might elicit aspects of the phenotype seen in Aldh2−/−Adh5−/− mice. We therefore challenged WT and Adh5−/− mice with intraperitoneal methanol injections (Figure 4E), which results in significant weight loss (Figure 4F) and a marked reduction in the CLP fraction and increased myeloid representation in the bone marrow, as seen in Aldh2−/−Adh5−/− mice (Figures 4G and 4H). In addition, methanol challenge in Adh5−/− mice also leads to abnormal B cell development with loss of pre-B cells and defective thymic maturation with loss of DN2 and DN3 thymocytes, the same pattern of thymic defect observed in young Aldh2−/−Adh5−/− mice (Figures 4I and 4J). We next wanted to examine the engagement of DNA repair and found that methanol-challenged Adh5−/− mice, but not WT controls, showed a 2-fold induction of SCEs (Figure 4K).
Formaldehyde differs from acetaldehyde, the canonical substrate of ALDH2, by a single methyl group, so we assessed biochemically whether it can be detoxified by ALDH2 (Figure 4L). In the first instance, we expressed and purified recombinant murine ALDH2 (rALDH2) in E. coli (Figure S4) and confirmed that it can indeed metabolize acetaldehyde. We then tested whether rALDH2 could also metabolize formaldehyde, and it is clear that formaldehyde is an equally good substrate (Figure 4M). Wondering whether compensatory overexpression of one enzyme occurs in the absence of the other, we found no such compensation of Aldh2 or Adh5 expression in Adh5−/− or Aldh2−/− HSPCs by scRNA-seq analysis (Figure S3C). Next, we asked whether the formaldehyde-detoxifying activity of ALDH2 could be confirmed in tissues from WT or Aldh2−/− mice. To test this, we prepared mitochondrial extracts from livers of WT and Aldh2−/− mice. WT extracts have acetaldehyde- and formaldehyde-metabolizing activity, and both are greatly reduced in Aldh2−/− mice (Figure 4N). In conclusion, challenge of Adh5−/− mice with a formaldehyde precursor recapitulates DNA damage and hematological phenotypes of Aldh2−/−Adh5−/− mice, and the biochemical activity supports the notion of ALDH2 being responsible for formaldehyde detoxification in Adh5−/− mice.
Formaldehyde Accumulation in Blood and DNA Imprints a Mutation Signature in Hematopoietic Precursors
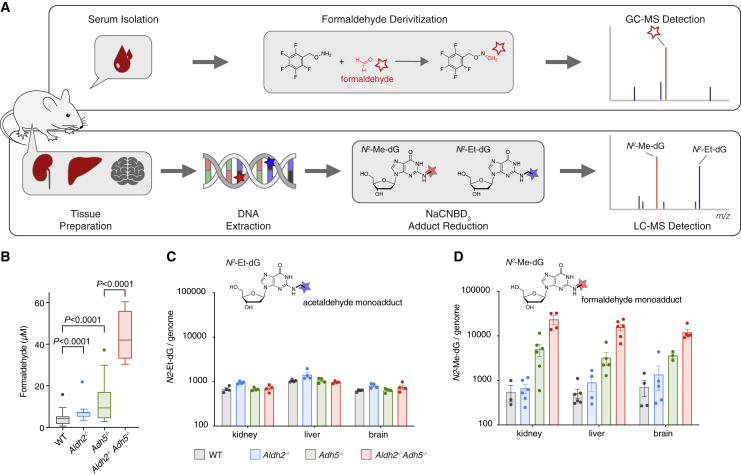
ALDH2 and ADH5 metabolize endogenous formaldehyde. Therefore, the drastic phenotype of Aldh2−/−Adh5−/− could be due to accumulation of reactive formaldehyde. To test this, we set out to directly quantify the formaldehyde concentration in mouse blood. There are many published studies using a range of methods that report blood formaldehyde levels of up to 100 μM in mammals (Heck et al., 1985; Luo et al., 2001; Martos and Pawliszyn, 1998), but, to date, we lack a reliably consistent value. This could be because measuring formaldehyde poses certain challenges; it is a volatile and reactive molecule. We therefore established a method to measure blood formaldehyde that is reliable and reproducible (Figure 5A). A blood sample is drawn and immediately processed to serum, spiked with an internal standard, and derivatized (Cancho et al., 2002). Samples are snap frozen and collected alongside a series of standards. Samples are then subjected to gas chromatography-mass spectrometry (GC-MS), and formaldehyde is detected and quantified. Using this method, we found that the mean blood formaldehyde level increased 11-fold in Aldh2−/−Adh5−/− compared with the WT (4 μM in the WT, 9 μM in Aldh2−/−, 11 μM in Adh5−/−, and 44 μM Aldh2−/−Adh5−/−) (Figure 5B).
Figure 5.
Aldh2 and Adh5 Act to Suppress Blood Formaldehyde Levels and Its DNA Adduct in Tissues
(A) Scheme of formaldehyde quantification in serum and as DNA adduct in tissues.
(B) Serum levels of formaldehyde (n = 43, 20, 51, 4, left to right). Boxes with lines indicate quartiles and median, and Tukey whiskers extend to 1.5 interquartile ranges. Two-tailed Mann-Whitney U test.
(C) Determination of the reduced genomic AA-deoxyguanine adduct N2-ethyl-deoxyguanosine from kidneys, liver, and brain (mean ± SEM; n = 4 per group).
(D) Determination of the reduced genomic formaldehyde-deoxyguanine adduct N2-methyl-deoxyguanosine from mouse kidneys, liver, and brain (mean ± SEM; n = 3–6 per group).
See also Figure S5.
We next wanted to assess whether the greatly increased levels of blood formaldehyde correlated with formaldehyde damage on DNA. A major acetaldehyde adduct is N2-ethylidene-deoxyguanosine (Garcia et al., 2011), and a major formaldehyde adduct is N2-hydroxymethyl-deoxyguanosine (HOMeG) (Moeller et al., 2011). However, both of these products are unstable and need to be reduced chemically (to N2-ethyl-deoxyguanosine, N2-EtG and N2-methyl-deoxyguanosine, N2-MeG) to be quantified. We then used ultra-sensitive liquid chromatography-tandem MS (LC-MS/MS) with synthetic chemical standards (Figure S5) to detect and quantify both adducts on DNA obtained from several tissues (Figures 5A and S5). Although the levels of the acetaldehyde adduct show little differences across genotypes (Figure 5C), there was a marked increase in the levels of N2-MeG in DNA extracted from livers, kidneys, and brains of Aldh2−/−Adh5−/− mice, to approximately 20-fold of WT levels (Figure 5D).
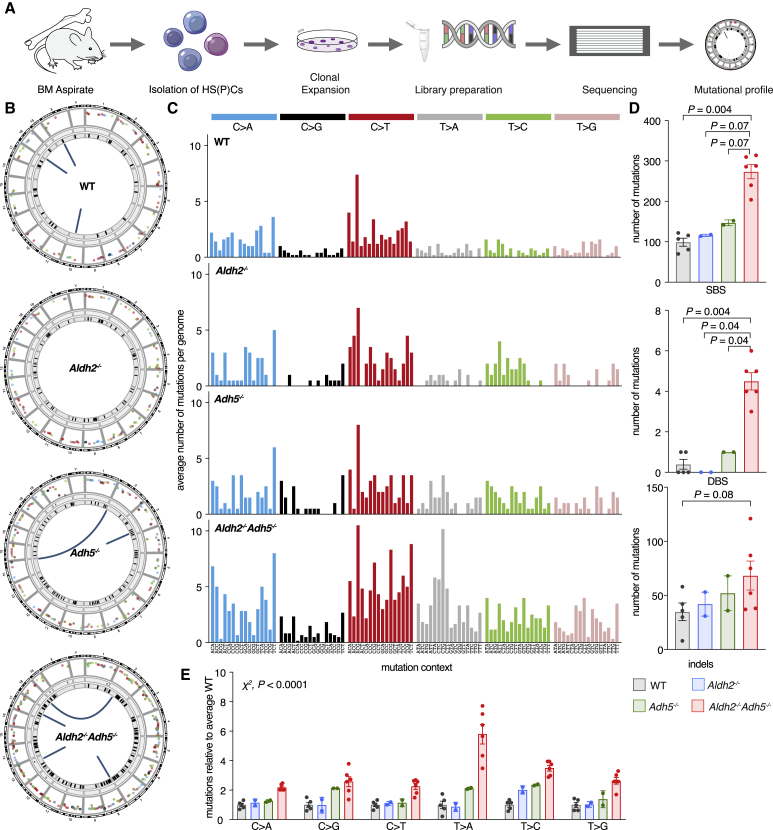
Although HOMeG may not be a mutagenic base adduct per se, it is noteworthy that Aldh2−/−Adh5−/− cells induce a very vigorous DNA repair response, part of which might be error prone. This could leave a distinct mutational imprint in their genome. We thus set out to determine the mutational landscape in bone marrow cells from 40-week-old Aldh2−/−Adh5−/− mice by whole-genome sequencing (Figure 6A). We found that Aldh2−/−Adh5−/− HSPCs contained a 3-fold increase in the number of single-nucleotide substitutions from approximately 100 to approximately 300 per genome, an increase in double-base substitutions from less than 1 to 4 per genome, and a 2-fold increase in insertions and deletions compared with the WT, with no obvious skew in size distribution (Figures 6B–6D, S6A, and S6B). We then analyzed the single-nucleotide substitutions in more detail. First, the mutation profile of the WT HSPCs is very similar to that extracted from human HSPCs from a 50-year-old man (Lee-Six et al., 2018), with C-to-T being the predominant change (about 40% of which are in a CpG context; Figure S6C). However, there is a notable and consistent increase in T-to-A transversions and, to a lesser extent, T-to-C transitions in Aldh2−/−Adh5−/− progenitors, which stand out (Figure 6E). By cosine similarity, the formaldehyde-induced mutational spectrum was most similar to the cancer-derived single-base substitution signatures SBS25, SBS40, SBS5, and SBS3 (Figure S6D; Alexandrov et al., 2020). Furthermore, T-to-A and T-to-G transversions showed a strong bias for an adenine base on the transcribed strand (Figure S6E), a feature shared with SBS40 that contributes to multiple cancers but is so far of unknown etiology. In summary, Aldh2−/−Adh5−/− mice show formaldehyde accumulation in their serum; this correlates with an increase in formaldehyde-modified DNA in tissues and mutational signatures with similarity to patterns observed in human cancers.
Figure 6.
Formaldehyde-Accumulating Aldh2−/−Adh5−/− Mice Reveal a Mutation Signature
(A) Whole-genome sequencing of HSPCs.
(B) Circos plots highlighting the different types and levels of mutations from a representative Aldh2−/−Adh5−/− mouse and controls. The outermost ring represents each chromosome, followed by sequential rings highlighting single-base substitutions (SBSs) as a rainfall plot (color-coding of substitution types as in C), tandem base substitutions (DBSs), and insertions or deletions (indels). Chromosomal rearrangements are represented by lines linking the translocated chromosomes at the center.
(C) Aggregated mutational profile of SBSs in HSPC genomes. Each mutation is assigned to the pyrimidine base of the originating base pair; within each of the 6 main mutation types, the sequence context of 5′ and 3′ flanking bases is shown in alphabetical order.
(D) Frequency of SBSs, DBSs, and indels (mean ± SEM; number of HSPC genomes analyzed = 5, 2, 2, 6 from left to right; two-tailed Mann-Whitney U test).
(E) Relative mutation number at each base, normalized to the average HSPC clone from WT litter-matched 40-week-old animals (mean ± SEM; n = 5, 2, 2, 6 from left to right; χ2 test comparing the aggregate number of mutations of each type between the WT and Aldh2−/−Adh5−/−).
See also Figure S6.
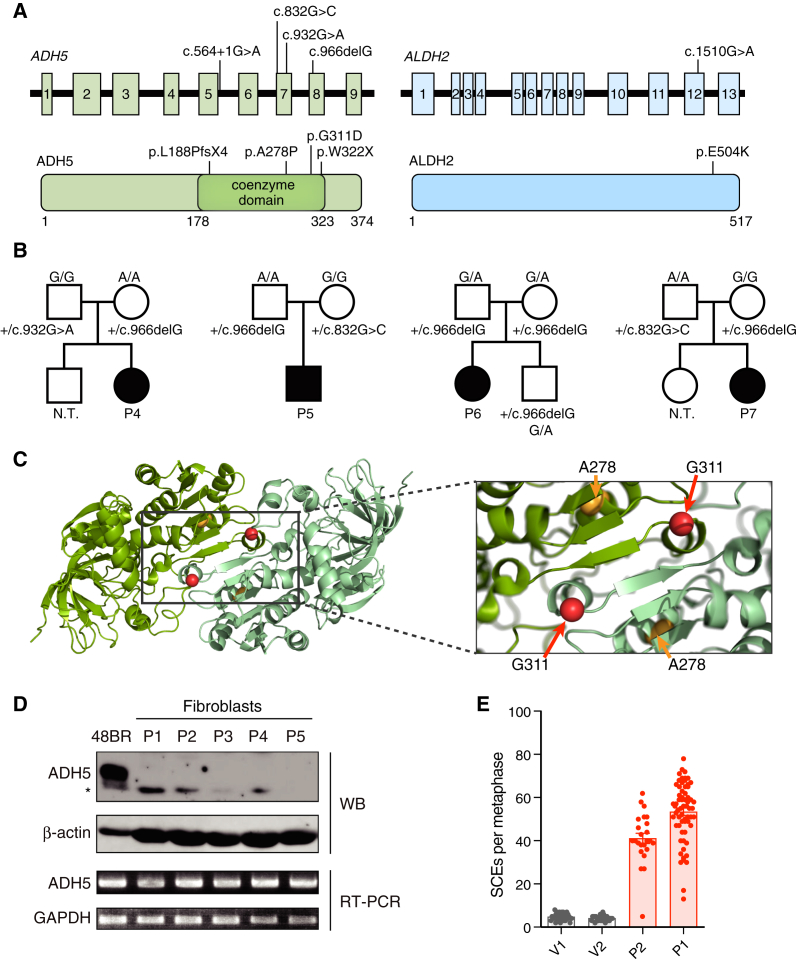
Inherited ALDH2 and ADH5 Deficiency in Humans Causes Bone Marrow Failure and Myelodysplasia
The devastating phenotype in mice resulting from failure of formaldehyde clearance prompted us to ask whether there are human diseases that could arise from loss of ALDH2 and ADH5. Based on our previous work suggesting that endogenous formaldehyde might be the genotoxin that causes FA, we predicted that a human disease analogous to Aldh2−/−Adh5−/− mice could present as early-onset bone marrow failure in children. We focused our search on the East Asian population, where a high proportion of people (40%–50%) already carry the ALDH2∗2 allele (Eng et al., 2007). This allele is defined by a functional SNP: rs671, the c.1510G > A mutation encoding a E504K amino acid substitution that reduces the enzymatic activity by ∼90% in a dominant-negative manner (Crabb et al., 1989). Individuals carrying the ALDH2∗2 allele develop facial flushing after consumption of alcohol and have an increased risk of esophageal cancer (Brooks et al., 2009).
Through a combination of whole-exome sequencing (WES) and targeted exome sequencing of the ADH5 gene, we sequenced children and young adults with bone marrow failure of unknown etiology from the Japanese Cancer Research Resources Bank (JCRB; Osaka, Japan) and our local centers. Of the 14 patients analyzed, seven harbored bi-allelic ADH5 mutations. Pathogenic alterations in genes known to be associated with other inherited bone marrow failure syndromes (IBMFS) (Bluteau et al., 2018) were not detected (data not shown). Interestingly, all seven of these IBMFS cases were also heterozygous for the ALDH2∗2 allele (the normal 1510G allele is called the ALDH2∗1 or G allele) (Figure 7A; Gross et al., 2015). Available clinical and laboratory data for these cases and the family pedigrees are summarized in Table 1 and Figure 7B. Detailed clinical information for the original three individuals was not available. However, all of them were adolescent patients with aplastic anemia (AA); moreover, the latter four developed myelodysplastic syndrome (MDS) that required HSC transplantation (HSCT), and in one patient, this progressed to acute myeloid leukemia (AML). Overall, their hematological phenotype (i.e., AA and MDS/AML), short stature, and skin pigmentation resembled FA. However, importantly, cells obtained from these patients did not show elevated chromosome breakage following exposure to the DNA crosslinking agents mitomycin C (MMC) or diepoxybutane (DEB) (Table 1). This indicates that DNA crosslink repair is intact in these individuals and that the cause of their bone marrow failure could not be a mutation in a new FA gene.
Figure 7.
Human Patients with Bone Marrow Failure Syndrome Caused by Inactivating Mutations in ALDH2 and ADH5
(A) Location of mutations in the ADH5 and ALDH2 genes (top) and proteins (bottom).
(B) Family pedigree of patients P4–P7. All parents were heterozygous for ADH5 mutations and reported to be healthy regardless of ALDH2 genotype. N.T., not tested.
(C) Localization of missense mutations near the ADH5 dimer interface.
(D) ADH5 gene expression in fibroblasts from patients P1–P5 by protein and RNA. An asterisk denotes a non-specific band recognized by the antibody.
(E) SCEs per metaphase (mean ± SEM) in patient-derived, PHA-stimulated lymphoblasts (P1 and P2) and two unrelated ALDH2∗1/∗2 heterozygous volunteers (V1 and V2).
See also Figure S7.
Table 1.
Summary of Japanese Patients Carrying Mutations in ADH5 and ALDH2 Genes
| Case No.: ID | Age (Years)/Gender | ADH5 Mutations | ALDH2 Genotype | Chromosome Breakage Test | Hematological Pathology | Bone Marrow Cytogenetics | Treatment and Outcome | Birth Weight and Stature | Other Clinical Features |
|---|---|---|---|---|---|---|---|---|---|
| P1: AP39P | 10/F | c.564+1G > A: p.L188PfsX4 c.832G > C: p.A278P (het) | G/A | 0.21 per cell (MMC) | – | – | – | ||
| P2: AP57P | 13/M | c.966delG: p.W322X c.832G > C: p.A278P (het) | G/A | 0.05 per cell (MMC) | – | – | – | ||
| P3: FA50P | 19/F | c.966delG: p.W322X (hom) | G/A | 0.11 per cell (MMC) | – | – | – | ||
| P4: TKFA-18 | 1/F | c.966delG: p.W322X c.932G > A: p.G311D (het) | G/A | 0.00 per cell (DEB) | AA progressing to MDS (RCMD) at age 10 years | 46,XX,der(22)t(1;22)(q12;q13),der(22)t(1;22)(q12;q13)[20] | HSCT at age 11 years, ongoing remission at 59 months post-HSCT | birthweight, 2,616 g; −1.48 SD; short stature, −4.9 SD at 138 months | skin pigmentation, café au lait spots, mild mental retardation |
| P5: TKFB-09 | 15/M | c.966delG: p.W322X c.832G > C: p.A278P (het) | G/A | 0.01 per cell (DEB) | AA progressing to AML | 46,XY,+1,der(1;15)(q10:q10),del(7)(q?),add(11)(q23)[19]/46,XY[1] | HSCT at age 16 years, died 60 months post-HSCT | birthweight, 2,784 g; −1.31 SD; short stature, −3.4 SD at 182 months | skin pigmentation, vitiligo, mild mental retardation |
| P6: KDFA-08 | 16/F | c.966delG: p.W322X (hom) | G/A | N.T. | AA with MDS (RCMD) | 46,XX,der(14)t(1;14)(q12;p11.2),der(21)t(1;21)(q12;p11.2)[19/20] | first and second HSCT at age 18 and 19 years, ongoing remission at 6 months after second HSCT | birthweight, 2,730 g; −0.37 SD; short stature, −2.4 SD at 194 months | short left fourth toe, microcephaly, mild mental retardation |
| P7: KDFA-13 | 4/F | c.966delG: p.W322X c.832G > C: p.A278P (Het) | G/A | 0.07 per cell (MMC) | AA with MDS (RAEB2) | 46,XX,+1,der(1;7)(q10;p10)[20/20] | HSCT at age 4 years, ongoing remission | birthweight, 2,935 g; −0.34 SD; short stature, −2.0 SD at 49 months | skin pigmentation, café au lait spots, microcephaly, mild mental retardation |
F, female; M, male; N.T., not tested; MMC, mitomycin C; DEB, diepoxybutane; AA, aplastic anemia; MDS, myelodysplastic syndrome; RCMD, refractory cytopenia with multi-lineage dysplasia; RAEB2, refractory anemia with excess blast 2; AML, acute myeloid leukemia; HSCT, hematopoietic stem cell transplant; SD, standard deviation from local population median. See also Table S7.
Among the four identified ADH5 variations (Figures 7A and 7B; Table S6), two were very rare and found only in a small number of East Asians in the genome aggregation database gnomAD (Karczewski et al., 2020), whereas the other two have not been described previously. No individuals homozygous or compound heterozygous for these variants were found in the databases or in our previous WES analysis in Japanese IBMFS patients (Muramatsu et al., 2017). Interestingly, the two missense variants were located close to the interface of the ADH5 dimer (Figure 7C). All variants abolish ADH5 protein expression; the corresponding fibroblast cultures had undetectable ADH5 protein by western blotting, but transcript levels were not affected severely (Figure 7D). The c.564+1G > A mutation in patient 1 (AP39P) affected splicing (Figure S7A). Exogenously expressed FLAG-tagged A278P ADH5 was barely detected in HEK293T cells, and neither the FLAG-tagged A278P ADH5 nor a missense G311D-FLAG ADH5 co-immunoprecipitated with co-expressed WT GFP-tagged ADH5 (Figure S7B). We wanted to assess whether DNA damage and repair was also elevated in these patients as in Aldh2−/−Adh5−/− mice by measuring the number of SCEs in phytohemagglutinin (PHA)-stimulated, patient-derived T lymphoblasts. Strikingly, the number of SCEs in patient cells was induced vigorously by about 10-fold (Figure 7E), which is similar to the levels seen in patients with Bloom syndrome (Chaganti et al., 1974), a genome instability syndrome where HR repair is induced. We found patients harboring mutations in ALDH2 and ADH5, resulting in a previously uncharacterized IBMFS, which highlights the essential requirement for metabolic clearance of formaldehyde in human hematopoiesis.
Discussion
This study establishes the scale of endogenous formaldehyde production and the routes through which it is removed. We identify two detoxifying enzymes, mitochondrial ALDH2 and cytosolic ADH5, that are jointly essential for removing formaldehyde. Loss of these detoxification mechanisms leads to hematopoietic failure and leukemia in mice and humans by overwhelming DNA repair, leading to genome instability and somatic mutations.
Formaldehyde-processing enzymes are widely expressed across tissues, including high expression in HSPCs (Figure 1A), but differ in their subcellular localization, which may point toward distinct sites of production of cellular formaldehyde. Given the level of formaldehyde that we detected in blood (4–44 μM), this is clearly an abundantly produced molecule. Decomposition of the vitamin folic acid (Burgos-Barragan et al., 2017), a cofactor of 1C metabolism, could be a mitochondrial source. Other likely sources could be oxidative demethylation reactions of DNA, RNA, and histones. Such epigenetic modification may be very active in developing hematopoietic cells, leading to spikes of endogenous formaldehyde being produced in the vicinity of DNA. For many years, formaldehyde has been considered an environmental carcinogen as a by-product of industrial processes, and exposure to such potential sources has been found to be associated with leukemia (Beane Freeman et al., 2009). However, environmental sources are very unlikely in our murine studies, indicating that 4 μM must be generated from within the animal. An important future area of research is to better define where within us all of this formaldehyde comes from.
The grave and diverse phenotype of Aldh2−/−Adh5−/− mice is very likely driven by accumulation of toxic formaldehyde, but it is not clear whether these features can be explained by genotoxicity alone. Perinatal lethality and growth retardation as observed in the Aldh2−/−Adh5−/− mice are common features of DNA repair-deficient mice and humans (Weeda et al., 1997), and it is tempting to speculate that endogenous formaldehyde may be responsible for at least some of the lesions these repair pathways deal with. Our analysis shows that formaldehyde accumulation has widespread consequences on blood production; there is significant perturbation of the transcriptomes of HSCs and early progenitors and a profound effect on development of the acquired immune system. Although these hematopoietic features could be due to DNA damage in this compartment, in good agreement with previous work showing specific depletion of lymphoid cells in response to exogenous DNA damage (Wang et al., 2016), it is also known that formaldehyde can modify RNA and proteins as well, which might add to the broad consequences of hematopoietic instruction.
An important aspect of our study is the emergence of a mutation signature associated with formaldehyde accumulation. Two particular aspects stand out. First, there is a marked increase across all classes of single-nucleotide substitutions in a profile that is similar to the cancer mutation signatures SBS5 and SBS40. This is a ubiquitous signature without known cause that is present in virtually all cancer genomes and certain normal somatic tissues, correlates with age, and has been speculated to reflect damage to DNA caused by ubiquitous metabolic driver(s) (Alexandrov et al., 2015, 2020; Blokzijl et al., 2016; Kim et al., 2016; Lee-Six et al., 2019; Moore et al., 2020). Formaldehyde thus seems to be a likely contributor shaping this common signature; this could be directly by causing DNA damage or indirectly by driving stem cell attrition and premature aging. However, previous work using an FA-deficient mouse model with a more severe stem cell defect and anemia showed that a more modest induction of point mutations and rescue of the stem cell defect via deletion of p53 did not reduce the mutation burden, arguing against stem cell attrition as the cause of mutation (Garaycoechea et al., 2018). Second, the number of T-to-A transversions and, to a lesser extent, T-to-C transitions stand out in Aldh2−/−Adh5−/− genomes. This suggests that formaldehyde may preferentially adduct adenine, possibly through attack to its exocyclic amine. A recent study implicated a novel mechanism by which formaldehyde exerts genotoxic activity. Cells were exposed to exogenous formaldehyde in excess of 100 μM, causing instability and inactivation of the key recombination and tumor suppressor protein BRCA2 (Tan et al., 2017). However, it is very unlikely that this is what occurs in Aldh2−/−Adh5−/− mice or in the deficient humans we describe here. First, we detected a striking induction of BRCA2-mediated DNA repair by rise of spontaneous SCEs in mice and humans. Second, the formaldehyde mutation signature we uncover here does not resemble that observed in BRCA2-deficient tumors. Third, our measurements of blood formaldehyde levels show that the physiological range is 4–10 μM when detoxification is intact, considerably lower than the dose range used in the published exposure studies.
Our previous work has shown that endogenous formaldehyde might be a driver for the phenotype of FA (Pontel et al., 2015; Rosado et al., 2011). We discovered seven human families carrying genetic defects in ALDH2 and ADH5, presenting as a new bone marrow failure syndrome that is solely driven by formaldehyde accumulation. Although the causes of IBMFS are diverse and include FA (Kottemann and Smogorzewska, 2013; Duxin and Walter, 2015; Ceccaldi et al., 2016), telomere biology disorders (Savage and Alter, 2009), and ribosome assembly defects (Kampen et al., 2020; Kennedy and Shimamura, 2019; Narla and Ebert, 2010), we believe that this is the first example of an IBMFS arising through a purely metabolic route. Given that formaldehyde is likely the common driver in FA and the IBMFS described in our work, it is not surprising that both diseases have common clinical features. As more cases of this new IBMFS are described, it will be of interest to assess any clinical features distinct from FA, indicating whether formaldehyde-driven pathologies can arise independent of failure of DNA crosslink repair. In our analysis, an unexpected finding was the high frequency (50%; 7 of 14 patients analyzed) of children and young adults with bone marrow failure of unknown etiology who carried mutations in ALDH2 and ADH5. We therefore recommend genotyping for these mutations as part of diagnostic investigations in future management of IBMFS patients of East Asian ethnicity. In addition, therapy aiming to lower endogenous formaldehyde could be a promising treatment strategy for this disease as well as for FA. Notably, ALDH2 deficiency has been associated with increased risk of esophageal, head and neck, and liver cancer in alcohol-consuming individuals (Brooks et al., 2009; Matsuo et al., 2001; Seo et al., 2019; Yokoyama et al., 2001). However, although FA patients with ALDH2 deficiency show more rapid disease progression (Hira et al., 2013), this effect is unlikely to be attributable to alcohol consumption because the patients are children. The present work raises the possibility that formaldehyde, rather than alcohol-derived acetaldehyde, might be responsible for this effect.
Finally, we establish reliable methods to track endogenous formaldehyde in blood and its adducts on DNA. These methods can now be used to probe in more detail how endogenous formaldehyde varies in humans and other mammals as well in other stressed physiological states. It is notable in this context that approximately 500 million humans are deficient in ALDH2 activity and may therefore accumulate endogenous formaldehyde (Oota et al., 2004), potentially in a manner that may interact with heritable polymorphisms in other loci or with specific environmental exposure. It is possible that this may have consequences for the long-term well-being of these individuals.
Limitations of Study
We find that strict adherence to the present protocol and rapid processing is essential for obtaining reliable formaldehyde quantification in serum. Although sequencing of HSPC-derived clones shows that DNA damage as mutations is increased in these cells, the assay does not discriminate between stem and progenitor cells, and our data suggest that both compartments are affected by formaldehyde accumulation. Furthermore, because the double-mutant mice show a defect in stem and progenitor populations, we cannot at present disentangle the direct effect of formaldehyde accumulation on the genome from its indirect effects mediated by the pathophysiological changes in Aldh2−/−Adh5−/− animals. Although we see induction of the DNA damage response and DNA repair gene expression in Aldh2−/−Adh5−/− stem and progenitor cells, the precise nature of formaldehyde-derived DNA damage and its sensing mechanism as well as the origin of endogenous formaldehyde remain areas of future study.
STAR★Methods
Key Resources Table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| CD45R/B220 (clone RA3-6B2) | R&D Systems | RRID:AB_357537 |
| c-Kit::APC-Cy7 (clone 2B8) | Biolegend | RRID:AB_1626278 |
| Sca-1::BV421 (clone D7) | Biolegend | RRID:AB_2563064 |
| CD45::FITC (clone 30-F11) | Biolegend | RRID:AB_312973 |
| Flt3::PE (clone A2F10) | Biolegend | RRID:AB_1877217 |
| Il-7R⍺::BV605 (clone A7R34) | Biolegend | RRID:AB_2572047 |
| Streptavidin::BV510 | Biolegend | Cat#405234 |
| CD4::FITC (clone H129.19) | BD Pharmingen | RRID:AB_394970 |
| CD3e::FITC (clone 145-2C11) | eBioscience | RRID:AB_464882 |
| Ly-6G/Gr-1::FITC (clone RB6-8C5) | eBioscience | RRID:AB_465314 |
| CD11b/Mac-1::FITC (clone M1/70) | BD PharMingen | RRID:AB_394774 |
| CD45R/B220::FITC (clone RA3-6B2) | BD PharMingen | RRID:AB_394618 |
| FcεR1α::FITC (clone MAR-1) | eBioscience | RRID:AB_465309 |
| CD8a::FITC (clone 53-6.7) | BD PharMingen | RRID:AB_394569 |
| CD11c::FITC (clone N418) | eBioscience | RRID:AB_464941 |
| TER-119::FITC (clone Ter119) | BD PharMingen | RRID:AB_396936 |
| c-Kit::PerCP-Cy5.5 (clone 2B8) | eBioscience | RRID:AB_2534338 |
| Sca-1::PE-Cy7 (clone D7) | eBioscience | RRID:AB_469669 |
| Flt3::PE (clone A2F10) | eBioscience | RRID:AB_465859 |
| CD34::eFluor660 (clone RAM34) | eBioscience | RRID:AB_10596826 |
| CD16/32::BV421 (clone 93) | Biolegend | RRID:AB_2650889 |
| Il-7R⍺::BV605 (clone A7R34) | Biolegend | RRID:AB_2572047 |
| CD3e::APC (clone 145-2C11) | eBioscience | RRID:AB_469315 |
| CD4::BV421 (clone H129.19) | BD PharMingen | RRID:AB_2739796 |
| CD8a::PE (clone 53-6.7) | BD PharMingen | RRID:AB_394571 |
| CD45R/B220::PerCP-Cy5.5 (clone RA3-6B2) | BD PharMingen | RRID:AB_394457 |
| Ly-6G/Gr-1::FITC (clone RB6-8C5) | eBioscience | RRID:AB_465315 |
| CD11b/Mac-1::BV605 (clone M1/70) | BD PharMingen | RRID:AB_2737951 |
| TER-119::PE-Cy7 (clone Ter119) | BD PharMingen | RRID:AB_396898 |
| B220::PE (clone RA3-6B2) | BD PharMingen | RRID:AB_394620 |
| IgM::APC (clone II/41) | BD PharMingen | RRID:AB_398464 |
| CD3e::PE (clone 145-2C11) | eBioscience | RRID:AB_465498 |
| Ly-6G/Gr-1::PE (clone RB6-8C5) | eBioscience | RRID:AB_466047 |
| CD11b/Mac-1::PE (clone M1/70) | BD PharMingen | RRID:AB_394775 |
| CD45R/B220::PE (clone RA3-6B2) | BD PharMingen | RRID:AB_394620 |
| TER-119::PE (clone Ter119) | BD PharMingen | RRID:AB_394986 |
| CD8a::APC (clone 53-6.7) | BD PharMingen | RRID:AB_398527 |
| CD44::PerCP-Cy5.5 (clone IM7) | eBioscience | RRID:AB_925746 |
| CD25::PE-Cy7 (clone PC61.5) | eBioscience | RRID:AB_469608 |
| CD4::FITC (clone H129.19) | Biolegend | RRID:AB_1279237 |
| CD45R/B220::PerCP-Cy5.5 (clone RA3-6B2) | Biolegend | RRID:AB_893354 |
| Gr-1::PE (clone 1A8) | BD PharMingen | RRID:AB_394208 |
| Mac-1::PE (clone M1/70) | Biolegend | RRID:AB_312791 |
| CD45.1::BV421 (clone A20) | Biolegend | RRID:AB_2562563 |
| CD45.2::APC (clone 104) | Biolegend | RRID:AB_389211 |
| TER-119::PE-Cy7 (clone Ter119) | Biolegend | RRID:AB_2281408 |
| CD45.1::BV605 (clone A20) | Biolegend | RRID:AB_2562565 |
| CD71::FITC (clone R17217.1.4) | eBioscience | RRID:AB_465124 |
| BrdU::FITC (clone B44) | BD PharMingen | RRID:AB_400327 |
| Goat-anti-mouse::AF488 | Invitrogen | RRID:AB_2534069 |
| rabbit polyclonal anti-ADH5 | Proteintech | RRID:AB_593422 |
| rabbit polyclonal anti-ALDH2 | Proteintech | RRID:AB_2224185 |
| mouse monoclonal anti-DDDDK tag (anti-FLAG) | MBL | RRID:AB_2687989 |
| Biological Samples | ||
| Patient cell lines | This study | N/A |
| Chemicals, Peptides, and Recombinant Proteins | ||
| O-(2,3,4,5,6-pentafluorobenzyl)hydroxylamine | Sigma-Aldrich | Cat#76735 |
| Formaldehyde solution | Thermo Fisher Pierce | Cat#28906 |
| 2′-Deoxy-N2-methylguanosine | Carbosynth | Cat#ND06236 |
| 15N-deoxyguanosine | Cambridge Isotope Laboratories | Cat#NLM-3899-CA-PK |
| BrdU slow release pellets, 50 mg/21 days | Innovative Research of America | Cat#N-231 |
| Critical Commercial Assays | ||
| Lineage Depletion Kit | StemCell Technologies, Inc. | Cat#19816A |
| Methocult GF M3434 | StemCell Technologies, Inc. | Cat#03434 |
| Deposited Data | ||
| Single-cell transcriptomes of murine HS(P)Cs | This study | GEO: GSE157832 |
| Genome sequencing data from HSPC clones | This study | ENA: PRJEB40375 |
| Patient exome sequencing data | This study | EGA: EGAS00001003809 |
| Experimental Models: Organisms/Strains | ||
| Mouse: Aldh2tm1a(EUCOMM)Wtsi | EUCOMM | RRID:MGI:5467969 |
| Mouse: Adh5tm1Stam | Liu et al., 2004 | RRID:MGI:3033876 |
| Mouse: C57BL/6J | The Jackson Laboratory | RRID:IMSR_JAX:000664 |
| Mouse: B6.SJL | Taconic | RRID:IMSR_TAC:b6sjl |
| Oligonucleotides | ||
| Primer sequences used in this study, see Table S7 | This study | N/A |
| Recombinant DNA | ||
| mmAldh2-pTrcHis-TOPO | This study | N/A |
| mmAldh2 cDNA | I.M.A.G.E., Source Bioscience | IMAGE ID 3600875 |
| Software and Algorithms | ||
| Scanpy | Wolf et al., 2018 | https://github.com/theislab/scanpy |
| GATK, version 4.1.0 | Van der Auwera et al., 2013 | RRID:SCR_001876; https://github.com/broadinstitute/gatk/releases |
| MassHunter GCMS Acquisition, version B.07.05.2479 | Agilent | N/A |
| MassHunter Quantitative Analysis for GCMS, version B.07.01 SP1/Build 7.1.524.1 | Agilent | N/A |
| Prism, version 8 | GraphPad | N/A |
Resource Availability
Lead Contact
Further information and requests for resources and reagents should be directed to KJ Patel, kjp@mrc-lmb.cam.ac.uk.
Materials Availability
This study did not generate new unique reagents; patient-derived cell lines have been deposited at JCRB cell bank and can be obtained from there.
Data and Code Availability
Single-cell RNA sequencing data have been deposited in Gene Expression Omnibus (accession GEO: GSE157832); genome sequencing data from HSPC clones have been deposited at the European Nucleotide Archive (accession ENA: PRJEB40375). Patient exome sequencing data have been deposited at the European Genome-Phenome Archive (accession EGA: EGAS00001003809). All other data and code are available upon reasonable request from the authors.
Experimental Model and Subject Details
Mice
All animals were maintained in specific pathogen-free conditions. In individual experiments mice were matched for gender and age. All animal experiments undertaken in this study were done so with the approval of the Animal Welfare Ethical Review Body and under project license authority granted by the UK Home Office. Aldh2−/−Adh5−/− mice were generated and bred into a C57BL/6J background. To this end, the previously reported Aldh2 allele (Aldh2tm1a(EUCOMM)Wtsi; MGI ID: 4431566, EUCOMM) was intercrossed with the previously reported Adh5 allele (Adh5tm1Stam; MGI ID: 3033711, a gift from Dr. Linmin Liu (Liu et al., 2004)). Some littermate Adh5+/− Aldh2+/− animals are included with the wild-type controls; they showed no noticeable difference from independently derived Adh5+/+ Aldh2+/+ animals.
For competitive repopulation experiments, C57BL/6Ola mice were intercrossed with B6.SJL (CD45.1) mice (Taconic) to generate CD45.1/CD45.2 recipients.
Research subjects
The overall research plan was approved by the Ethical Committee of Kyoto University and other participating institutions. Written informed consent was obtained from all subjects examined. Subjects’ age and sex are indicated in Table 1. The patient-derived cell cultures and information including SCE levels were originally deposited by Dr. Masao S. Sasaki (formerly at the Radiation Biology Center, Kyoto University) to the JCRB Cell Bank, and were provided to us with the consent of Dr. Sasaki. Genomic DNA was isolated from primary fibroblast cultures (P1-P5) or a buccal swab (P6) or peripheral blood mononuclear cells (family members and healthy PHA-blast donors) using Gentra Puregene kits. Chromosome breakage tests were carried out with MMC 0.02 μg per ml (50-72h) or with DEB 0.1 μg per ml (48h) as previously described (Sasaki and Tonomura, 1973; Yabe et al., 2007). Whole exome sequencing (WES) of genomic DNA and subsequent processing were done as described previously (Muramatsu et al., 2017). ALDH2 genotyping was done with Taqman PCR as described (Hira et al., 2013). Genome PCR and Sanger sequencing were done according to the standard procedure with primer sequences described in Table S7. Subjects in the HERPACC project were recruited between January 2001 and December 2005 from the Hospital-based Epidemiologic Research Program at Aichi Cancer Center (HERPACC)-2. The framework of HERPACC-2 has been described elsewhere (Hamajima et al., 2001). Non-cancer controls (n = 4206) were randomly selected from the HERPACC-2 database. DNA of each subject was extracted from the buffy coat fraction with a QIAamp DNA Blood Mini Kit (QIAGEN). Genotyping of ALDH2 (rs671) and three ADH5 variants (c.966delG, c.G832C, and c.564+1G > A) was conducted using TaqMan Assays with a 7500 Real-Time PCR System (Applied Biosystems).
Method Details
Blood counts
Total blood was collected in K3EDTA MiniCollect tubes (Greiner bio-one) and analyzed on a scil VetABC Plus+ blood counter (Horiba).
Histology and Immunohistochemistry
Dorsal skin was embedded in OCT medium and frozen on dry ice in a 2-methylbutane bath. Skin was cryosectioned at 20 μM at −30°C, and fixed in 10% formalin, then stained with oil red O and hematoxylin. Spleens and femurs were fixed in 10% neutral-buffered formalin for a minimum of 24 hours. Femurs were decalcified. Tissues were embedded in paraffin. After sectioning at 4 μm, tissues were deparaffinized and rehydrated using standard histological methods. Bone marrow was stained with anti-B220 antibody (R&D Systems, MAB1217, 1:500) for IHC. Spleens were stained with anti-B220 antibody and anti-CD3.
Single cell RNA-seq
The femurs, tibiae, iliac crest, humeri, and vertebrae of 6-16 weeks old mice were crushed, washed with 10 mL of PBS supplemented with 2% heat-inactivated FBS, and strained through 70-μm meshes. Cell suspension was depleted of red blood cells by ammonium chloride lysis (STEMCELL Technologies), and stained with the lineage depletion kit (19816A, STEMCELL Technologies) following the manufacturer’s instructions and passed through magnetic columns. Lineage-depleted cells were resuspended in 100 μl of PBS supplemented with 2% FCS containing the following antibodies against: c-Kit (APC-Cy7, clone 2B8, 105826, Biolegend), Sca-1 (BV421, clone D7, 108128, Biolegend), CD45 (FITC, clone 30-F11, 103108, Biolegend), Flt3 (PE, clone A2F10, 135306, Biolegend) and Il-7R⍺ (BV605, clone A7R34, 135041, Biolegend). Cells were incubated at 4°C for 30 minutes in the dark, washed, and resuspended in 100 μl of PBS supplemented with 2% FCS containing streptavidin (BV510, 405234, Biolegend). Cells were further incubated at 4°C for 15 minutes, washed and resuspended in 500 μl of PBS supplemented with 2% FCS containing 0.5 μl 7AAD (A1310, Life Technologies). Cells (lineage- c-Kit+ population, and lineage- c-Kitlo Sca-1+ population) were bulk sorted using a Becton Dickinson Influx sorter.
Single cell expression analysis
Sorted cells were processed using 10x Chromium (10x Genomics, Pleasanton, CA) according to the manufacturer’s protocol. Sample demultiplexing, barcodes processing, and gene counting was performed using the count commands from the Cell Ranger v1.3 pipeline. After Cell Ranger processing, each sample was filtered for potential doublets by simulating synthetic doublets from pairs of scRNaseq profiles and assigning scores based on a k-nearest-neighbor classifier on PCA transformed data. The 4.5% of cells with the highest doublets scores from each sample were removed from further analysis, respectively. Cells with > 10% of unique molecular identifier (UMI) counts mapping to mitochondrial genes, expressing fewer than 1200 genes, or with total number of UMI counts further than 3 standard deviations from the mean were excluded. After quality control, 8204 cells from WT, 7709 cells from Aldh2−/−, 8401 cells from Adh5−/−, and 9014 cells from Aldh2−/−Adh5−/− were retained for downstream analysis. These cells were then normalized to the same total count. All scRNaseq data was analyzed using the Scanpy Python Module (Wolf et al., 2018). Unsupervised UMAP clustering (Uniform Manifold Approximation and Projection) was carried out using the Louvain algorithm, and cell identity was manually annotated based on the following marker genes: Procr (HSC cluster), Dntt/Flt3 (Lymphoid cluster), Irf8/Ms4a6c (Monocyte cluster), Mpo/Elane/Ctsg (Neutrophil cluster), Itga2b/Pf4/Vwf (Megakaryocyte cluster), Gzmb/Cma3/Mcpt8 (Mast cell cluster), Klf1/Gata1 (Erythroid cluster).
Heatmap Visualization of Adh and Aldh Family Genes
WT cells from an independent experiment were clustered using the Louvain method and annotated based on their gene expression similarity to annotated clusters from previously published Lineage- c-Kit+ hematopoietic landscapes (Dahlin et al., 2018). The expression of Adh and Aldh family genes were then plotted on a heatmap grouped by their Louvain clustering. Each column was scaled independently between 0 and 1.
Quantification of HSC numbers across Genotypes
UMAP visualizations were calculated in Scanpy using default parameters. Each cell from the second experiment was mapped to the previously computed Louvain clusters using a KNN classifier in PCA space. Using these assigned clusters, the most immature cluster annotated through HSC-related gene expression markers as ‘HSPC’ was isolated and the proportion of cells in this cluster belonging to each genotype calculated.
Quantification of HSC state using hscScore
Each single cell transcriptome was scored using the recently published hscScore method (Hamey and Göttgens, 2019). Briefly, the transcriptome of each cell is compared to the transcriptomes of known HSCs using a MLP deep learning model to assign a score representing how likely the cell is to be a true HSC, with a score of 1 representing the most HSC-like cell in the dataset. Violin plots of the hscScore results for the ‘HSPC’ cluster were created using the Seaborn Python module.
Subclustering of HSPC cluster
Cells identified as belonging to the HSPC cluster were re-clustered and a new UMAP visualization was calculated. Seven clusters were found and a list of genes upregulated in each cluster compared to the union of all other clusters was calculated. The clusters were then annotated based on their differential expression of known HSC-, lineage- or cell cycle-related marker genes such as Procr, Mllt3, Mettl7a1 (HSC), Flt3, Dntt (Lymphoid) and Mpo, Ctsg, Cdk6 (Myeloid/Cycling).
Cell cycle profiling
Cell cycle assignment of erythroid progenitors was performed following the method established in Tirosh et al. (2016) for scoring cycling cells and implemented with Scanpy. Lists of 43 genes associated with S-phase and 55 genes associated with G2/M phases from Tirosh et al. (2016) were used to quantify the relative expression of these cell-cycle stages compared with a randomly chosen set of reference genes. Cells with high relative expression levels of either program were assigned to be in S-phase or G2/M phase respectively, while cells with no clear expression of either program were assigned to the G1 phase. No cells expressed relatively high levels of both S and G2/M phase programs.
Apoptosis module score
The apoptosis module score for the erythroid progenitors was calculated using the expression values of a set of 298 genes belonging to the ‘Intrinsic Apoptotic Signaling Pathway’ gene ontology term downloaded from http://www.informatics.jax.org/ (GO:0097193). For each cell, the score was given by
Where is the normalized expression of a gene , and is the size of the geneset.
DNA repair gene expression analysis
For each genotype, the list of DEGs in each cluster was intersected with the list of DNA repair genes belonging to the ‘DNA Repair’ gene ontology term (GO:006281). The resulting number of DNA repair DEGs and their median fold-change in each cluster was calculated and plotted as the size and color of circles respectively using the python module Matplotlib.
Flow cytometry
HSC and progenitor quantification
Bone marrow cells were isolated from femurs, tibiae and iliac crests with PBS supplemented with 2% FCS and strained through 70 μm meshes. Red cells were lysed by resuspending the cells in 10 mL red cell lysis buffer (130-094-183, MACS Miltenyi Biotec) for 10 min at room temperature. After centrifugation, the cell pellet was resuspended in PBS supplemented with 2% FCS and nucleated cells were counted with 3% acetic acid on a Vi-Cell XR cell viability counter (Beckman Coulter). 10 × 106 bone marrow cells were resuspended in 200 μL of PBS supplemented with 2% FCS containing the following antibody solution: FITC-conjugated lineage cocktail with antibodies against CD4 (clone H129.19, BD PharMingen), CD3e (clone 145-2C11, eBioscience), Ly-6G/Gr-1 (clone RB6-8C5, eBioscience), CD11b/Mac-1 (clone M1/70, BD PharMingen), CD45R/ B220 (clone RA3-6B2, BD PharMingen), FcεR1α (clone MAR-1, eBioscience), CD8a (clone 53-6.7, BD PharMingen), CD11c (clone N418, eBioscience), TER-119 (clone Ter119, BD PharMingen); c-Kit (PerCP-Cy5.5, clone 2B8, eBioscience), Sca-1 (PE-Cy7, clone D7, eBioscience), Flt3 (PE, clone A2F10, eBioscience), CD34 (eFluor660, clone RAM34, eBioscience), CD16/32 (BV421, clone 93, BioLegend) and Il-7R⍺ (BV605, clone A7R34, BioLegend).
Myeloid, erythroid, B and T lymphoid populations
Bone marrow cells (1 × 106) as prepared above were resuspended in 200 μL of PBS supplemented with 2% FCS containing a mature lineage cocktail that consist of antibodies against: CD3e (APC, clone 145-2C11, eBioscience), CD4 (BV421, clone H129.19, BD PharMingen), CD8a (PE, clone 53-6.7, BD PharMingen), CD45R/ B220 (PerCP-Cy5.5, clone RA3-6B2, BD PharMingen), Ly-6G/Gr-1 (FITC, clone RB6-8C5, eBioscience), CD11b/Mac-1 (BV605, clone M1/70, BD PharMingen), TER-119 (PE-Cy7, clone Ter119, BD PharMingen). Spleen cell suspensions in PBS supplemented with 2% FCS were prepared by gently washing and straining whole spleen through a 70 μm mesh. Red cell lysis, cell counting and staining with the mature lineage cocktail were as described above to quantify the myeloid, erythroid, B and T lymphoid populations. Myeloid, B and T lymphoid populations in the peripheral blood were quantified by red cell lysing 100 μl of whole blood with addition of 1 mL of ammonium chloride lysis buffer (155 mM NH4Cl, 10 mM KHCO3, 0.1 mM Na2EDTA, pH 7.2), incubated for 10 min at room temperature and washed with 3 mL of PBS supplemented with 2% FCS. Following centrifugation, cells were resuspended in 100 μl PBS supplemented with 2% FCS containing the mature lineage cocktail. Ter-119 was used to exclude unlysed red cells and red cell debris.
B cell maturation in the bone marrow
Bone marrow cells (1 × 106) as prepared above were stained with antibodies against CD45R/B220 (PE, clone RA3-6B2, BD PharMingen) and IgM (APC, clone II/41, BD PharMingen).
Thymic development
A whole thymus was gently washed and strained through a 70 μm mesh to prepare single cell suspensions. 10 × 106 thymic cells were stained in 200 μl PBS supplemented with 2% FCS containing the following antibody solution: PE-conjugated lineage cocktail with antibodies against CD3e (clone 145-2C11, eBioscience), Ly-6G/Gr-1 (clone RB6-8C5, eBioscience), CD11b/Mac-1 (clone M1/70, BD PharMingen), CD45R/ B220 (clone RA3-6B2, BD PharMingen) and TER-119 (clone Ter119, BD PharMingen); CD4 (BV421, clone H129.19, BD PharMingen), CD8a (APC, clone 53-6.7, BD PharMingen), CD44 (PerCP-Cy5.5, clone IM7, eBioscience), CD25 (PE-Cy7, clone PC61.5, eBioscience)
Competitive repopulation assay
This was performed essentially as described previously (Garaycoechea et al., 2018). Briefly, CD45.1+ CD45.2+ recipients were subjected to two doses of 5 Gy whole-body irradiation, three hours apart, before intravenous injection of a cell suspension containing 200 000 nucleated bone marrow cells from donor and 200 000 sex-matched nucleated bone marrow cells from a B6.SJL competitor in 200 μl IMDM. Blood samples were collected at 4-week intervals, red cells lysed and cells stained in 100 μl 2% FBS/PBS containing the following fluorochrome-conjugated antibodies: CD4 (FITC, clone H129.19, Biolegend), CD8 (FITC, clone 53-6.7, BD), B220 (PerCP-Cy5.5, clone RA3-6B2, Biolegend), Gr-1 (PE, clone 1A8, BD), Mac-1 (PE, clone M1/70, Biolegend), CD45.1 (BV421, clone A20, Biolegend), CD45.2 (APC, clone 104, Biolegend), TER-119 (PE-Cy7, clone TER-119, Biolegend). After four months, to determine long-term reconstitution, thymus was stained determine chimerism using the following antibodies: CD3e (PE, clone 145-2C11, eBioscience), B220 (PE, clone RA3-6B2, BD), Gr-1 (PE, clone 1A8, BD), Mac-1 (PE, clone M1/70, Biolegend), TER-119 (PE, clone TER-119, Biolegend), CD4 (BV421, clone RM4-5, Biolegend), CD8a (FITC, clone 53-6.7, BD), CD25 (PE-Cy7, clone PC61.5, eBioscience), CD44 (PerCP-Cy5.5, clone IM7, Biolegend), CD45.1 (BV605, clone A20, Biolegend), CD45.2 (APC, clone 104, Biolegend). Chimerism in the bone marrow was determined after red cell lysis using a cocktail containing antibodies against lineage antigens (FITC-conjugated, as above), c-Kit (PerCP-Cy5.5, clone 2B8, eBioscience), Sca-1 (PE-Cy7, clone D7, eBioscience), Flt3 (PE, clone A2F10, eBioscience). For enumeration of LT-HSCs, additional antibodies were used against CD34 (eFluor660, clone RAM34, eBioscience), CD45.1 (BV605, clone A20, Biolegend) and CD45.2 (BV421, clone 104, Biolegend). For enumeration of common lymphoid progenitors, Il-7R⍺ (BV605, clone A7R34, BioLegend), CD45.1 (BV421, clone A20, Biolegend) and CD45.2 (APC, clone 104, Biolegend) were added. Donor-derived chimerism was calculated as the fraction of CD45.2+CD45.1- cells among the sum of CD45.1+CD45.2- and CD45.2+CD45.1- cells in a population.
Micronucleus assay
Micronucleus assay was performed as previously described (Garaycoechea et al., 2018), with blood from mice 2-42 weeks of age (mean 8.7 weeks). 20 μl blood was added to 110 μl solution of heparin in PBS (1000 U ml-1). 120 μl of the blood suspension were added to 1.2 mL methanol at −80°C and stored for at least 12 hours at −80°C. Fixed blood was washed and resuspended in bicarbonate buffer (0.9%(w/v) NaCl, 5.3 mM NaHCO3). A volume corresponding to 2 μl blood in bicarbonate buffer was incubated with 1 μl anti-CD71 (FITC, clone R17217.1.4, eBioscience), 7 μl RNase A (Sigma) in a total volume of 100 μl for 45 min, washed with 1 mL bicarbonate buffer, and resuspended in 500 μl of a 5 μg ml-1 solution of propidium iodide in bicarbonate buffer and analyzed without delay.
Sister chromatid exchange assay
This was performed essentially as described previously (Garaycoechea et al., 2018). Mice were implanted with a 50 mg slow-release pellet of BrdU (Innovative Research of America, N-231) Where animals were treated with methanol, they received two doses of 1.5 g kg-1 via intraperitoneal injection of a 15% (w/v) solution in saline 16 and 12 hours before analysis. 30 min before femora were collected into ice-cold PBS, mice received an intraperitoneal injection of 100 μl colchicine 0.5% (w/v) in saline (Sigma). Bones were flushed with 10 mL of pre-warmed 75 mM KCl solution and incubated at 37°C for 15 min. Cells were spun down, resuspended in 3 mL Carnoy’s fixative (3:1 mixture of methanol:glacial acetic acid) drop-wise by gentle agitation and then topped up to 10 mL fixative. After 30 min at room temperature, cells were spun down, resuspended in 500 μl fixative and stored at −20°C until use. Cells were dropped onto chilled, humidified slides then dried for 1 hour at 60°C. Slides were washed in 2x SSC for 5 min, then stained for 15 min at room temperature with 1 μg ml-1 Hoechst 33258 (Thermo Fisher Scientific, H3569) in 2x SSC. Slides were subsequently transferred immersed in 2x SSC and crosslinked for 30 minutes in a Stratalinker crosslinker (Stratagene). Slides were dehydrated by passing through a 70%/96%/100% ethanol, placed in PBS at room temperature for 5 min, DNA was denatured by exposure to 70 mM NaOH for 2 min, then washed 3x 5 min in PBS. The slides were then blocked in blocking buffer (1% BSA, 0.5% Tween-20 in PBS) for 1 h at room temperature, then stained overnight with a FITC-conjugated mouse-anti-BrdU antibody (clone B44, BD PharMingen) diluted 1:1 in 3% BSA, 0.5% Tween-20/PBS. The slides were subsequently washed 3x 5 min in blocking buffer, then stained with AF488-conjugated goat-anti-mouse antibody (Invitrogen, A-11001) diluted 1:500 in blocking buffer for 6 h at room temperature. Slides were washed 3x 15 min in blocking buffer, then stained for 15 min in 5 μg ml-1 Hoechst 33342 in (H3570, Thermo Fisher Scientific) in PBS. The slides were then washed 3x 10 min in PBS, once in water for 5 min, and mounted with ProLong Gold Antifade mountant (P36930, Thermo Fisher Scientific).
Methanol treatment for hematopoietic development
Adh5−/− and WT mice aged between 7-12-week-old received intraperitoneal injections with 0.85 g kg-1 methanol (99.8% purity, HPLC grade, Fisher scientific) dose on days 1 and 8. Methanol was diluted to 8.5% v/v in saline, and injected at 12.6 mL kg-1. Weight was monitored daily, and on day 10, mice were culled by exposure to CO2 in rising concentration, followed by cardiac puncture. Blood, spleen, thymus and bones were harvested for analysis of hematopoiesis and lymphocyte development as described above.
ALDH2 biochemistry
Cloning and Expression of Aldh2
Mouse Aldh2 was cloned into a pTrcHis-TOPO expression vector (provided by D. Mochly-Rosen, Stanford University), containing a N-terminal uncleavable 6XHis tag. Mouse Aldh2 was amplified from full length cDNA (IRAV14-F04, IMAGE I.D. 3600875) using the following primers: 5′-TTATATGCTAGCTCAGCCGCCGCCACCAGCGCGGTG-3′ and 5′-GATGGCGGATCCAAGCTTGCATGATTCTTACGAGTTCTTCTGTGGCACTT-3′ and was cloned into the expression vector using NheI-HindIII sites. This removed the 19 amino acid N-terminal mitochondrial targeting signal peptide of ALDH2. The vector was transformed into E. coli BL21 E. coli and protein expression induced with 0.5 mM IPTG at 30°C for 5 hours. Cell pellets were harvested, resuspended in Buffer A (containing 25 mM Tris-HCl pH 8.0, 2 mM TCEP, 10% glycerol, 500 mM NaCl). Cells were lysed by the addition of 0.1% sodium deoxycholate, 200 μg ml-1 lysozyme with protease inhibitor cocktail (Roche) (50 mL Lysis Buffer per 10 g pellet). The extract was centrifuged at 43,000 × g, for 40 min at 4°C to obtain a soluble fraction for purification.
Purification of ALDH2
Mouse recombinant ALDH2 was purified using a 3-step purification strategy. The soluble fraction was first passed over a 1 mL HisTrap HP column, washed with 40 mM imidazole, and protein eluted with 250 mM imidazole. The pooled fractions were concentrated before being applied to a Superdex 200), eluted in buffer A (containing 50 mM NaCl). Fractions containing Aldh2 were then diluted three times with a 0 mM NaCl buffer and further purified using an Anion Exchange column (Q15, 3 ml) to yield pure mouse Aldh2 protein. Protein was stored in 50% glycerol at −20°C, or in 10% glycerol at −80°C, and used for enzymatic assays.
Liver mitochondria preparation and ALDH Assay
Mouse liver (0.5 g) was finely minced with scissors and homogenized with 500 μL of homogenization buffer (210 mM mannitol, 70 mM sucrose, 1 mM EDTA, 5 mM MOPS, pH = 7.4 in H2O) using a Dounce homogenizer. The homogenate was centrifuged at 700 × g for 10 min, the supernatant removed, and centrifuged again at 700 × g for 10 minutes. The supernatant was removed and centrifuged at 7000 × g for 20 min. The pellet was washed in homogenization buffer (centrifuged at 7000 × g for 10 min), then re-suspended in 300 μL of enzyme assay buffer (10 mM DTT, 20% glycerol, 0.1% Triton X-100 and 0.1 M Tris-HCl, pH = 8.0) and centrifuged at 100,000 × g for 30 minutes at 4°C to obtain a clear supernatant. Protein concentration was measured using a NanoDrop.
To perform the ALDH enzymatic activity assay, a 2 mL reaction was set up in a cuvette containing 50 mM NaPPi buffer (pH = 9.0), 2.5 mM NAD+, 10 mM acetaldehyde and 0.5 mg protein preparation in H2O. The absorbance at 340 nm was recorded using a Cary 5000 UV-Vis-NIR spectrophotometer, at RT for 300 s without the addition of the acetaldehyde substrate, in order to quench the reaction of endogenous aldehydes. After 3 minutes, acetaldehyde was added, and the absorbance recorded for a further 350 s. To calculate the NADH production in mol/min/mg total protein, we used: Absorbance = ε × c × L, where ε = 6220 M-1, L = path length (1 cm) and c = [NADH] in mol l-1. The assay was adapted from a protocol by D. Mochly-Rosen, Stanford University.
In vitro ALDH Activity assay
To perform ALDH enzymatic activity assays, a 2 mL reaction was set-up in a cuvette containing 50 mM NaPPi buffer (pH = 9.0), 2.5 mM NAD+, 10 μg recombinant protein and 1 mM subtstrate in H2O. As soon as the substrate was added, the absorbance at 340 nm was recorded using a Cary 5000 UV-Vis-NIR spectrophotometer, at RT for 300 s. To calculate the NADH production in mol/min/mg total protein, we used: Absorbance = ε × c × L, where ε = 6220 M-1, L = path length (1 cm) and c = [NADH] in mol l-1.
Mouse serum formaldehyde quantification by GC–MS
Mice were euthanized by exposure to CO2 in rising concentration, followed by cardiac puncture to collect 500 μl - 700 μl whole blood into Microvette 500 Z-gel tubes containing clotting activator (20.1344, Sarstedt). After centrifugation at 10,000 × g for 5 min at room temperature, 100 μl of the serum was transferred to glass crimp top vials (5182-0543, Agilent), followed by addition of internal standards: cyclohexanone (29140, Sigma) and n-Propanol (34871, Sigma) at a final concentration of 1 mg l−1 each respectively, and derivatization reagent O-(2,3,4,5,6-pentafluorobenzyl)hydroxylamine (PFBHA, 76735, Sigma) at a final concentration of 60 μg ml−1. The tube was sealed with magnetic crimp caps (5188-5386, Agilent), incubated overnight in the dark at room temperature, and stored at −80°C until analysis by GC–MS. A serum-formaldehyde calibration standard was prepared in parallel with each batch of serum sample collection. Following cardiac blood draw and transfer of the blood into the tube, dilutions of formaldehyde 16% (w/v, 28906, Thermo Fisher Pierce) in PBS were added to the blood sample at final concentrations ranging from 0 μM – 213 μM. Subsequent serum isolation and formaldehyde derivatization was identical to sample preparation as described above.
The mass spectrometer was operated in single ion monitoring mode for the ions m/z 181, 195 and 225 for formaldehyde-PFBHA oxime (retention time 11.47 min) and m/z 181, 195 and 293 for cyclohexanone-PFBHA oxime internal standard (retention time 16.73 min) with m/z 181 used for quantification for both compounds. A dwell time of 200 ms was used for each ion. The transfer line to the mass spectrometer was heated to 220°C, the source temperature was maintained at 230°C and the quadrupole at 150°C. The GC–MS data were acquired using MassHunter GCMS Acquisition B.07.05.2479. For quantification, all analyte integrated peak areas were ratioed to internal standard areas using MassHunter Quantitative Analysis Version B.07.01 SP1/Build 7.1.524.1 for GCMS. The method was calibrated across the range of 0.1 to 5 mg l−1 of formaldehyde: each calibration point was run in triplicate and a demonstrated precision of ≤ 15%.
Synthesis of nucleoside standards
Isotopically labeled nucleosides where purchased from Cambridge Isotope Laboratories, non-labeled from Sigma.
Synthesis of 15N-N2-MeG and N2-MeG
In a small glass vial with an air tight screw cap 15N-dG (1) or dG (5 mg) (3) was dissolved in formaldehyde (1 ml, MeOH free, 5.328 M (16%), Thermo Scientific). After 24 h the reaction was transferred to a round-bottom flask and evaporated twice with water (2 ml). The residue was then dissolved in a solution of NaOAc (pH = 4, 100 mM) with NaCNBH3 or NaCNBD3 respectively (1 ml, 100 mM) and left for another 24 h. The reaction was neutralized with PBS (20 ml) and purified by preparative HPLC on a Varian PrepStar using the following conditions: Buffer A: H2O Buffer B: MeCN, Gradient: 5%–12.5% Buffer B over 30 min. Column: Waters Atlantis Prep T3, 10 μM, 19 × 250 mm.
The product was obtained at retention time 12.5 min and yield < 1%, and its chemical identity confirmed by ESI mass spectrometry: 15N-N2-MeG (2) ESI+, 286.097 [M+H]+. Mw = 285.090 C11H1415N5O4. N2-MeG (4) 283.126 [M+H]+. Mw = 282.119 C11H14DN5O4.
Determination of the extinction coefficient for N2-MeG
2′-Deoxy-N2-methylguanosine (5 mg, Carbosynth) was re-purified on a Thermo Scientific Accela HPLC using the following conditions: Buffer A: H2O Buffer B: MeCN, Gradient: 5%–20% Buffer B over 30 min. Column: Agilent AdvanceBio Oligonucleotides, 4.6 × 150 mm. The product was evaporated to dryness. The resulting powder was then weighed out using an accurate balance (1-2 mg, Mettler Toledo, XS205). A 0.5 mg ml-1 solution was prepared in H2O. This solution was diluted 1:2 in PBS in quintuplicate, and the absorbance measured at 260 nm (Nanodrop). Using the Beer-Lambert law the extinction coefficient for N2-MeG was calculated to be 9277 l mol-1 cm-1. The same value was used for 15N-N2-MeG and N2-MeG.
Sample preparation for determination of N2-MeG in DNA
Organs were snap frozen and stored at −80°C until analysis. 10-30 mg of tissue was cut and lysed in a 2 mL Eppendorf, using 733 μL of Puregene cell lysis solution (QIAGEN), 4 μL of proteinase K (Fisher BioReagents) and a 7 mm stainless steel metal ball (QIAGEN). Samples where homogenized in a tissue lyser (QIAGEN/Retsch) for 3 min at 30 Hz, then incubated at 37°C for 30 min, 600 rpm. Then 4 μL of RNase A solution (QIAGEN) were added, vortexed and incubated at 37°C for 1 h at 600 rpm.
The supernatant was transferred to a new tube (1.5 ml) and cooled on ice for 1 min. Then 266 μL protein precipitation solution (QIAGEN, Puregene) and vortexed briefly, cooled on ice for 5 min, spun 21,300 × g, 3 min. The supernatant was transferred into a fresh tube containing 600 μL isopropanol, mixed by inversion 10 × and left at RT for 5 min for the DNA to precipitate. DNA was pelleted by spinning at 21,300 × g for 2 min. The supernatant was discarded and the DNA pellet washed with 600 μL of 70% ethanol, spun at 21,300 × g, 2 min. Again the supernatant was discarded and the pellet left to air-dry for 5 mins before dissolving the pellet by addition of 500 μL of 50 mM, NaCNBD3 in 200 mM NaOAc (pH = 5.2), and dissolved and reacted for 24 h at RT at 1000 RPM in an Eppendorf Thermomixer.
DNA was precipitated out of the NaCNBD3 solution by addition of 900 μl isopropanol, spun at 21,300 × g, 5 min and the supernatant discarded. This step was performed twice and the pellet left to air dry. The DNA was dissolved in 150 μl of ultra-pure water (Romil) and quantified by nanodrop.
DNA was digested in a total volume of 100 μl in reactions containing 5000 ng DNA, 2 U shrimp alkaline phosphatase, (New England Biolabs), 0.004 U snake venom phosphodiesterase I (Sigma, P3243) and 10 U DNase I (Roche) in 1 × DNase I digestion buffer.
Also added to the digest were the internal standards 15N-N2-MeG and 15N-dA. For standard curve generation a non-reduced sample of genomic liver DNA from a WT mouse was used and the standards 2′-deoxyadenosine (dA) and N2-MeG added at various concentrations. The range of the standard curves was as follows: 0.24 to 100 fmol for N2-MeG, 8.5 to 272 nmol for dA. The curves contained 6 points plus a zero control. The response ratio (non-labeled to labeled spike) was plotted versus the amount of non-labeled spike injected onto to the column.
After an overnight digest (> 16 h) samples were filtered with a 2000 MWCO Vivacon® 500 (Sartorius), 40 min, 16000 × g. Samples where then transferred to a MS vial and analyzed.
Online LC-MS2 determination of N2-MeG in DNA digests
Samples were analyzed on TSQ Altis Triple Quadrupole Mass Spectrometer in selected reaction monitoring mode (SRM) interfaced to an UltiMate 3000 uHPLC and. The uHPLC was fitted with a nanoEase M/Z Symmetry C18 Trap Column, 100Å, 5 μm, 180 μm × 20 mm (Waters) at RT and a reversed phase EASY-Spray HPLC analytical column (2 μm particle size, 75 μm × 250 mm, Thermo Fisher Scientific) connected to an EASY-Spray source at 35°C.
10 μl of sample (500 ng of digested DNA) was injected per run using a 10 μl sample loop and the full loop inject mode. Buffers used were from Romil and of Ultra LC standard. Buffer A: H2O (0.1% acetic acid), buffer B MeCN (0.1% acetic acid). The gradient was 0-2.5 min – 1% B, 22 min – 45% B, 23.5 min – 99% B. This was followed by 2 wash pulses (1%–99% B) and equilibration to 1% B (45 min total run time). The trap column was held at a constant 1% B and switching from the trap to the main column occurred at 1 min 24 s and back at 40 min.
Mass spectrometry conditions were as follows: source voltage of 2300V in positive ionisation mode; ion transfer tube temperature 250°C, CID gas pressure 2 mbar, scan widths for Q1 and Q3 at 0.7 m/z. Dwell times were 100 ms for N2-MeG and 15N-N2-MeG, 10 ms for dA. Collision energy voltage and RF voltage were optimized with authentic standards using the vendor-provided tune software for each fragment in the SRM, however the dA parameters were reduced to 10% of the optimal value due to their high abundance and consequently high ion current.
Detection of acetaldehyde mono-adduct N2-EtdG by MS
The determination was performed as described previously (Moeller et al., 2013) and performed in the Swenberg laboratory. DNA was isolated using a NucleoBond DNA isolation kit, with small modifications. DNA was then reduced and digested as described previously (Yu et al., 2015). Following digestion, hydrolysed DNA was filtered and injected onto an Agilent 1200 HPLC fraction collection system equipped with a diode-array detector. dG and N2-EtdG were separated and eluted. The amounts of dG were quantified according to the UV peak area with a calibration curve. The amounts of N2-EtdG were detected and quantified with a calibration curve on an AB SCIEX Triple Quad 6500 mass spectrometer interfaced with an Eksigent nanoLC Ultra 2D system. The internal standard 15N-N2-EtdG was synthesized by the Swenberg lab. Chemicals were from Sigma.
Genome sequencing of HSPC colonies
Total bone marrow was diluted in X-Vivo 20 (Lonza) supplemented with 5% (v/v) BIT9500 (Stem Cell Technologies), 10 ng ml-1 IL-3, 10 ng ml-1 IL-6, 50 ng ml-1 SCF and 50 ng ml-1 TPO (all Peprotech), and 1 volume of cells added to 10 volumes of Methocult GF M3434 (Stem Cell Technologies) semisolid medium. After 2 weeks, colonies were transferred to liquid culture in supplemented X-Vivo 20 for a further week. DNA from liquid cultures and mouse brain cortex as germline reference was extracted using Zymo Quick-gDNA microprep kit as per the manufacturer’s instructions. DNA was quantified fluorimetrically using AccuBlue High Sensitivity dsDNA Quantitation Kit (Biotium) and libraries prepared using NEBNext Ultra II FS DNA Library Preparation kit with unique dual indices (New England Biolabs) according to the manufacturer’s recommendation. Libraries were size-selected to peak around 500 bp, quality-controlled on Agilent Bioanalyzer 2100 and quantified by qPCR using Kapa library quantification kit for Illumina (Roche). Sequencing was performed as 150 bp paired end on NovaSeq S2 (Illumina). Raw sequence data was converted to unsorted BAM format and then fed into the Genome Analysis Toolkit v. 4.1.0 using the best practice pipelines for data preprocessing and somatic variant discovery (Van der Auwera et al., 2013). Alignment was performed against the Illumina mm10 reference genome using a set of single-nucleotide polymorphisms and indels from the Sanger Mouse Genome project as input for base quality score recalibration.
Mutect2 was invoked using matched brain sample as normal reference genome. Final passing variants were filtered to exclude multiallelic sites and sites identified by Mutect2 as normal_artifact, and further restricted to sites with coverage depth > = 20 and variant allele frequency > = 0.3 to limit the analysis to clonal mutations with good confidence. As a quality control step, using the same settings we asked Mutect2 to call mutations in the brain against matched HSPC genomes, but found none passing filters indicating non-clonal origin of the brain tissue.
Patient-derived cell culture and transfection
The patient-derived primary fibroblasts (JCRB Cell Bank, Osaka, Japan) and the 48BR cell lines were cultured in RPMI1640 supplemented with 20% FBS (GIBCO).
SCE assay on patient-derived cells
Peripheral blood mononuclear cells were separated by density gradient centrifugation and stimulated with 5 μg/ml phytohemagglutinin (PHA) (Sigma) in RPMI 1640 (Nacalai Tesque) supplemented with 10% FBS (GIBCO). The staining of metaphase spreads for the quantification of SCEs was performed according to a published protocol (Sonoda et al., 1999). For BrdU labeling, cells were cultured in the presence of 5 μM BrdU for 16 to 18 h (two cell cycle periods) and pulsed with 0.1 μg/ml Colcemid for the last 2 h. Harvested cells were treated with 75 mM KCl for 30 min and subsequently fixed with methanol: acetic acid (3:1) for 40 min. Cells were dropped onto wet (50% ethanol) glass slides and dried on a 42°C plate. Dried slides were incubated with 10 μg/ml Hoechst 33258 in phosphate buffer (pH 6.8) for 20 min, followed by rinsing with MacIlvaine solution (164 mM Na2HPO4, 16 mM citric acid, pH 7.0). Slides were irradiated with a black light (352 nm) for 1 h and incubated in 2 × SSC (0.3 M NaCl plus 0.3 M sodium citrate) solution at 62°C for 1 h before staining with 3% Giemsa solution (pH 6.8) and subsequent microscopy.
Immunoprecipitation and western blotting of patient-derived cells
Cells were washed once with PBS and lysed in NETN buffer (150 mM NaCl, 0.5 mM EDTA, 20 mM Tris-HCl pH = 8.0, 0.5% NP-40) supplemented with protease inhibitor cocktail (Roche) and 25 unit/mL Benzonase (Millipore) on ice for 30 min. Lysates were then briefly sonicated and centrifuged at 17,800 g for 10 min at 4°C. GFP-tagged proteins were captured using anti-GFP magnetic beads (Sigma) at 4°C, washed five times with NETN buffer, and eluted by adding 1 × Laemmli sample buffer and boiling. Samples were separated by SDS-PAGE, transferred to a PVDF membrane, and analyzed by western blotting. The antibodies used were rabbit polyclonal anti-ADH5 (Proteintech); rabbit polyclonal anti-ALDH2 (Proteintech), mouse monoclonal anti-DDDDK tag (anti-FLAG) (MBL).
Quantification and Statistical Analysis
Sample number (n) indicates the number of independent biological samples in each experiment and are indicated in figure legends or methods. Unless otherwise stated in the figure legends, data are shown as the mean ± SEM. Unless otherwise stated, statistical significance was assessed using two-tailed Mann-Whitney U test. Analysis was performed using GraphPad Prism (Version 8).
Acknowledgments
We thank the LMB ARES animal research staff and genotyping service, Emeritus Prof. M.S. Sasaki for deposition of the samples and data to the JCRB, T. Hirayama and Dr. A. Kohara at the JCRB Cell Bank for help, and Prof. G.S. Vassiliou and Prof. A.J. Warren for critical reading of the manuscript. This work was supported by funding to F.A.D. and M.W. (C60150/A23919) by CRUK, to L.P. and R.Y. by the FA Research Fund (5102402), to R.Y. in part by NIEHS grants P42 ES005948 and P30 ES010126 and TCEQ (582-12-21861), and to K.J.P. and group by the MRC, the Wellcome Trust, and the Jeffrey Cheah Foundation. This work was also supported by JSPS KAKENHI grants (JP23114010, JP26550026, and JP15H01738 to M.T. and 16K15243 to A.H.) and grants from The Ministry of Health, Labour and Welfare (to M.T., M.Y., H.Y., E.I., and S.K.), the Japan Leukemia Research Fund (to A.H.), the Takeda Science Foundation (to A.H.), the Uehara Memorial Foundation (to M.T.), the Astellas Foundation for Research on Metabolic Disorders (to M.T.), and The Kyoto University Research Fund (Core Stage Back-Up) (to M.T.). The Radiation Biology Center, Graduate School of Biostudies, Kyoto University, is a joint-usage research center certified by the MEXT and is also supported by the JSPS Core-to-Core Program (JPJSCCA20200009).
Author Contributions
K.J.P. conceived the project. F.A.D. and M.W. led the project with assistance from N.O., L.B.P., A.N.K.-L., F.L., C.N., and M.R.G.H. C.L.M., M.R.H.H., and R.Y. completed the adduct analysis. R.L.C. and P.S.M. measured serum formaldehyde. S.W., N.K.W., and B.G. performed scRNA-seq. The human study was planned by M.T., K.M., M.Y., H.Y., S.O., S.M., S.K., and E.I. K.Y., Y. Okuno, H.M., and Y.S. performed WES. M.Y., H.Y., M. Kobayashi, T.M., T.O., and M. Kato provided clinical samples and data. A.M. and A.H. completed the majority of the experiments on human samples with help from Y. Okamoto and M.M. K.J.P. wrote the manuscript with input from M.W., F.A.D., A.M., and M.T. All authors provided comments on the manuscript.
Declaration of Interests
The authors declare no competing interests.
Published: November 4, 2020
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.molcel.2020.10.012.
Contributor Information
Minoru Takata, Email: takata.minoru.8s@kyoto-u.ac.jp.
Ketan J. Patel, Email: kjp@mrc-lmb.cam.ac.uk.
Supplemental Information
References
- Alexandrov L.B., Jones P.H., Wedge D.C., Sale J.E., Campbell P.J., Nik-Zainal S., Stratton M.R. Clock-like mutational processes in human somatic cells. Nat. Genet. 2015;47:1402–1407. doi: 10.1038/ng.3441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexandrov L.B., Kim J., Haradhvala N.J., Huang M.N., Tian Ng A.W., Wu Y., Boot A., Covington K.R., Gordenin D.A., Bergstrom E.N., PCAWG Mutational Signatures Working Group; PCAWG Consortium The repertoire of mutational signatures in human cancer. Nature. 2020;578:94–101. doi: 10.1038/s41586-020-1943-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beane Freeman L.E., Blair A., Lubin J.H., Stewart P.A., Hayes R.B., Hoover R.N., Hauptmann M. Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries: the National Cancer Institute Cohort. J. Natl. Cancer Inst. 2009;101:751–761. doi: 10.1093/jnci/djp096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blokzijl F., de Ligt J., Jager M., Sasselli V., Roerink S., Sasaki N., Huch M., Boymans S., Kuijk E., Prins P. Tissue-specific mutation accumulation in human adult stem cells during life. Nature. 2016;538:260–264. doi: 10.1038/nature19768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluteau O., Sebert M., Leblanc T., Peffault de Latour R., Quentin S., Lainey E., Hernandez L., Dalle J.-H., Sicre de Fontbrune F., Lengline E. A landscape of germ line mutations in a cohort of inherited bone marrow failure patients. Blood. 2018;131:717–732. doi: 10.1182/blood-2017-09-806489. [DOI] [PubMed] [Google Scholar]
- Brooks P.J., Enoch M.-A., Goldman D., Li T.-K., Yokoyama A. The alcohol flushing response: an unrecognized risk factor for esophageal cancer from alcohol consumption. PLoS Med. 2009;6:e50. doi: 10.1371/journal.pmed.1000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryce S.M., Bemis J.C., Avlasevich S.L., Dertinger S.D. In vitro micronucleus assay scored by flow cytometry provides a comprehensive evaluation of cytogenetic damage and cytotoxicity. Mutat. Res. 2007;630:78–91. doi: 10.1016/j.mrgentox.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgos-Barragan G., Wit N., Meiser J., Dingler F.A., Pietzke M., Mulderrig L., Pontel L.B., Rosado I.V., Brewer T.F., Cordell R.L. Mammals divert endogenous genotoxic formaldehyde into one-carbon metabolism. Nature. 2017;548:549–554. doi: 10.1038/nature23481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancho B., Ventura F., Galceran M.T. Determination of aldehydes in drinking water using pentafluorobenzylhydroxylamine derivatization and solid-phase microextraction. J. Chromatogr. A. 2002;943:1–13. doi: 10.1016/s0021-9673(01)01437-6. [DOI] [PubMed] [Google Scholar]
- Ceccaldi R., Sarangi P., D’Andrea A.D. The Fanconi anaemia pathway: new players and new functions. Nat. Rev. Mol. Cell Biol. 2016;17:337–349. doi: 10.1038/nrm.2016.48. [DOI] [PubMed] [Google Scholar]
- Chaganti R.S., Schonberg S., German J. A manyfold increase in sister chromatid exchanges in Bloom’s syndrome lymphocytes. Proc. Natl. Acad. Sci. USA. 1974;71:4508–4512. doi: 10.1073/pnas.71.11.4508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crabb D.W., Edenberg H.J., Bosron W.F., Li T.K. Genotypes for aldehyde dehydrogenase deficiency and alcohol sensitivity. The inactive ALDH2(2) allele is dominant. J. Clin. Invest. 1989;83:314–316. doi: 10.1172/JCI113875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlin J.S., Hamey F.K., Pijuan-Sala B., Shepherd M., Lau W.W.Y., Nestorowa S., Weinreb C., Wolock S., Hannah R., Diamanti E. A single-cell hematopoietic landscape resolves 8 lineage trajectories and defects in Kit mutant mice. Blood. 2018;131:e1–e11. doi: 10.1182/blood-2017-12-821413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duxin J.P., Walter J.C. What is the DNA repair defect underlying Fanconi anemia? Curr. Opin. Cell Biol. 2015;37:49–60. doi: 10.1016/j.ceb.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng M.Y., Luczak S.E., Wall T.L. ALDH2, ADH1B, and ADH1C genotypes in Asians: a literature review. Alcohol Res. Health. 2007;30:22–27. [PMC free article] [PubMed] [Google Scholar]
- Garaycoechea J.I., Crossan G.P., Langevin F., Daly M., Arends M.J., Patel K.J. Genotoxic consequences of endogenous aldehydes on mouse haematopoietic stem cell function. Nature. 2012;489:571–575. doi: 10.1038/nature11368. [DOI] [PubMed] [Google Scholar]
- Garaycoechea J.I., Crossan G.P., Langevin F., Mulderrig L., Louzada S., Yang F., Guilbaud G., Park N., Roerink S., Nik-Zainal S. Alcohol and endogenous aldehydes damage chromosomes and mutate stem cells. Nature. 2018;553:171–177. doi: 10.1038/nature25154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia C.C.M., Angeli J.P.F., Freitas F.P., Gomes O.F., de Oliveira T.F., Loureiro A.P.M., Di Mascio P., Medeiros M.H.G. [13C2]-Acetaldehyde promotes unequivocal formation of 1,N2-propano-2′-deoxyguanosine in human cells. J. Am. Chem. Soc. 2011;133:9140–9143. doi: 10.1021/ja2004686. [DOI] [PubMed] [Google Scholar]
- Giri S.D., Chatterjee A. Modulation of mitomycin C-induced sister chromatid exchanges and cell cycle delay by buthionine sulfoximine and reduced glutathione in mouse bone marrow cells in vivo. Mutat. Res. 1998;413:227–234. doi: 10.1016/s1383-5718(98)00023-0. [DOI] [PubMed] [Google Scholar]
- Gross E.R., Zambelli V.O., Small B.A., Ferreira J.C.B., Chen C.-H., Mochly-Rosen D. A personalized medicine approach for Asian Americans with the aldehyde dehydrogenase 2∗2 variant. Annu. Rev. Pharmacol. Toxicol. 2015;55:107–127. doi: 10.1146/annurev-pharmtox-010814-124915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamajima N., Matsuo K., Saito T., Hirose K., Inoue M., Takezaki T., Kuroishi T., Tajima K. Gene-environment Interactions and Polymorphism Studies of Cancer Risk in the Hospital-based Epidemiologic Research Program at Aichi Cancer Center II (HERPACC-II) Asian Pac. J. Cancer Prev. 2001;2:99–107. [PubMed] [Google Scholar]
- Hamey F.K., Göttgens B. Machine learning predicts putative hematopoietic stem cells within large single-cell transcriptomics data sets. Exp. Hematol. 2019;78:11–20. doi: 10.1016/j.exphem.2019.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada S., Agarwal D.P., Goedde H.W. Aldehyde dehydrogenase deficiency as cause of facial flushing reaction to alcohol in Japanese. Lancet. 1981;2:982. doi: 10.1016/s0140-6736(81)91172-7. [DOI] [PubMed] [Google Scholar]
- Heck H.D., Casanova-Schmitz M., Dodd P.B., Schachter E.N., Witek T.J., Tosun T. Formaldehyde (CH2O) concentrations in the blood of humans and Fischer-344 rats exposed to CH2O under controlled conditions. Am. Ind. Hyg. Assoc. J. 1985;46:1–3. doi: 10.1080/15298668591394275. [DOI] [PubMed] [Google Scholar]
- Hira A., Yabe H., Yoshida K., Okuno Y., Shiraishi Y., Chiba K., Tanaka H., Miyano S., Nakamura J., Kojima S. Variant ALDH2 is associated with accelerated progression of bone marrow failure in Japanese Fanconi anemia patients. Blood. 2013;122:3206–3209. doi: 10.1182/blood-2013-06-507962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodskinson M.R., Bolner A., Sato K., Kamimae-Lanning A.N., Rooijers K., Witte M., Mahesh M., Silhan J., Petek M., Williams D.M. Alcohol-derived DNA crosslinks are repaired by two distinct mechanisms. Nature. 2020;579:603–608. doi: 10.1038/s41586-020-2059-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson B., Brocker C., Thompson D.C., Black W., Vasiliou K., Nebert D.W., Vasiliou V. Update on the aldehyde dehydrogenase gene (ALDH) superfamily. Hum. Genomics. 2011;5:283–303. doi: 10.1186/1479-7364-5-4-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson M.K., Bernofsky C. Mitochondrial acetaldehyde dehydrogenase from Saccharomyces cerevisiae. Biochim. Biophys. Acta. 1974;350:277–291. doi: 10.1016/0005-2744(74)90502-6. [DOI] [PubMed] [Google Scholar]
- Kampen K.R., Sulima S.O., Vereecke S., De Keersmaecker K. Hallmarks of ribosomopathies. Nucleic Acids Res. 2020;48:1013–1028. doi: 10.1093/nar/gkz637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karczewski K.J., Francioli L.C., Tiao G., Cummings B.B., Alföldi J., Wang Q., Collins R.L., Laricchia K.M., Ganna A., Birnbaum D.P. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–443. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy A.L., Shimamura A. Genetic predisposition to MDS: clinical features and clonal evolution. Blood. 2019;133:1071–1085. doi: 10.1182/blood-2018-10-844662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Mouw K.W., Polak P., Braunstein L.Z., Kamburov A., Kwiatkowski D.J., Rosenberg J.E., Van Allen E.M., D’Andrea A., Getz G. Somatic ERCC2 mutations are associated with a distinct genomic signature in urothelial tumors. Nat. Genet. 2016;48:600–606. doi: 10.1038/ng.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kottemann M.C., Smogorzewska A. Fanconi anaemia and the repair of Watson and Crick DNA crosslinks. Nature. 2013;493:356–363. doi: 10.1038/nature11863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langevin F., Crossan G.P., Rosado I.V., Arends M.J., Patel K.J. Fancd2 counteracts the toxic effects of naturally produced aldehydes in mice. Nature. 2011;475:53–58. doi: 10.1038/nature10192. [DOI] [PubMed] [Google Scholar]
- Lee-Six H., Øbro N.F., Shepherd M.S., Grossmann S., Dawson K., Belmonte M., Osborne R.J., Huntly B.J.P., Martincorena I., Anderson E. Population dynamics of normal human blood inferred from somatic mutations. Nature. 2018;561:473–478. doi: 10.1038/s41586-018-0497-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee-Six H., Olafsson S., Ellis P., Osborne R.J., Sanders M.A., Moore L., Georgakopoulos N., Torrente F., Noorani A., Goddard M. The landscape of somatic mutation in normal colorectal epithelial cells. Nature. 2019;574:532–537. doi: 10.1038/s41586-019-1672-7. [DOI] [PubMed] [Google Scholar]
- Liu L., Yan Y., Zeng M., Zhang J., Hanes M.A., Ahearn G., McMahon T.J., Dickfeld T., Marshall H.E., Que L.G., Stamler J.S. Essential roles of S-nitrosothiols in vascular homeostasis and endotoxic shock. Cell. 2004;116:617–628. doi: 10.1016/s0092-8674(04)00131-x. [DOI] [PubMed] [Google Scholar]
- Luo W., Li H., Zhang Y., Ang C.Y. Determination of formaldehyde in blood plasma by high-performance liquid chromatography with fluorescence detection. J. Chromatogr. B Biomed. Sci. Appl. 2001;753:253–257. doi: 10.1016/s0378-4347(00)00552-1. [DOI] [PubMed] [Google Scholar]
- Martos P.A., Pawliszyn J. Sampling and determination of formaldehyde using solid-phase microextraction with on-fiber derivatization. Anal. Chem. 1998;70:2311–2320. doi: 10.1021/ac9711394. [DOI] [PubMed] [Google Scholar]
- Matsuo K., Hamajima N., Shinoda M., Hatooka S., Inoue M., Takezaki T., Tajima K. Gene-environment interaction between an aldehyde dehydrogenase-2 (ALDH2) polymorphism and alcohol consumption for the risk of esophageal cancer. Carcinogenesis. 2001;22:913–916. doi: 10.1093/carcin/22.6.913. [DOI] [PubMed] [Google Scholar]
- Moeller B.C., Lu K., Doyle-Eisele M., McDonald J., Gigliotti A., Swenberg J.A. Determination of N2-hydroxymethyl-dG adducts in the nasal epithelium and bone marrow of nonhuman primates following 13CD2-formaldehyde inhalation exposure. Chem. Res. Toxicol. 2011;24:162–164. doi: 10.1021/tx1004166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller B.C., Recio L., Green A., Sun W., Wright F.A., Bodnar W.M., Swenberg J.A. Biomarkers of exposure and effect in human lymphoblastoid TK6 cells following [13C2]-acetaldehyde exposure. Toxicol. Sci. 2013;133:1–12. doi: 10.1093/toxsci/kft029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore L., Leongamornlert D., Coorens T.H.H., Sanders M.A., Ellis P., Dentro S.C., Dawson K.J., Butler T., Rahbari R., Mitchell T.J. The mutational landscape of normal human endometrial epithelium. Nature. 2020;580:640–646. doi: 10.1038/s41586-020-2214-z. [DOI] [PubMed] [Google Scholar]
- Muramatsu H., Okuno Y., Yoshida K., Shiraishi Y., Doisaki S., Narita A., Sakaguchi H., Kawashima N., Wang X., Xu Y. Clinical utility of next-generation sequencing for inherited bone marrow failure syndromes. Genet. Med. 2017;19:796–802. doi: 10.1038/gim.2016.197. [DOI] [PubMed] [Google Scholar]
- Narla A., Ebert B.L. Ribosomopathies: human disorders of ribosome dysfunction. Blood. 2010;115:3196–3205. doi: 10.1182/blood-2009-10-178129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oota H., Pakstis A.J., Bonne-Tamir B., Goldman D., Grigorenko E., Kajuna S.L.B., Karoma N.J., Kungulilo S., Lu R.-B., Odunsi K. The evolution and population genetics of the ALDH2 locus: random genetic drift, selection, and low levels of recombination. Ann. Hum. Genet. 2004;68:93–109. doi: 10.1046/j.1529-8817.2003.00060.x. [DOI] [PubMed] [Google Scholar]
- Orsburn B., Escudero B., Prakash M., Gesheva S., Liu G., Huso D.L., Franco S. Differential requirement for H2AX and 53BP1 in organismal development and genome maintenance in the absence of poly(ADP)ribosyl polymerase 1. Mol. Cell. Biol. 2010;30:2341–2352. doi: 10.1128/MCB.00091-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pontel L.B., Rosado I.V., Burgos-Barragan G., Garaycoechea J.I., Yu R., Arends M.J., Chandrasekaran G., Broecker V., Wei W., Liu L. Endogenous Formaldehyde Is a Hematopoietic Stem Cell Genotoxin and Metabolic Carcinogen. Mol. Cell. 2015;60:177–188. doi: 10.1016/j.molcel.2015.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosado I.V., Langevin F., Crossan G.P., Takata M., Patel K.J. Formaldehyde catabolism is essential in cells deficient for the Fanconi anemia DNA-repair pathway. Nat. Struct. Mol. Biol. 2011;18:1432–1434. doi: 10.1038/nsmb.2173. [DOI] [PubMed] [Google Scholar]
- Sasaki M.S., Tonomura A. A high susceptibility of Fanconi’s anemia to chromosome breakage by DNA cross-linking agents. Cancer Res. 1973;33:1829–1836. [PubMed] [Google Scholar]
- Savage S.A., Alter B.P. Dyskeratosis congenita. Hematol. Oncol. Clin. North Am. 2009;23:215–231. doi: 10.1016/j.hoc.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo W., Gao Y., He Y., Sun J., Xu H., Feng D., Park S.H., Cho Y.-E., Guillot A., Ren T. ALDH2 deficiency promotes alcohol-associated liver cancer by activating oncogenic pathways via oxidized DNA-enriched extracellular vesicles. J. Hepatol. 2019;71:1000–1011. doi: 10.1016/j.jhep.2019.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonoda E., Sasaki M.S., Morrison C., Yamaguchi-Iwai Y., Takata M., Takeda S. Sister chromatid exchanges are mediated by homologous recombination in vertebrate cells. Mol. Cell. Biol. 1999;19:5166–5169. doi: 10.1128/mcb.19.7.5166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan S.L.W., Chadha S., Liu Y., Gabasova E., Perera D., Ahmed K., Constantinou S., Renaudin X., Lee M., Aebersold R., Venkitaraman A.R. A Class of Environmental and Endogenous Toxins Induces BRCA2 Haploinsufficiency and Genome Instability. Cell. 2017;169:1105–1118.e15. doi: 10.1016/j.cell.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirosh I., Izar B., Prakadan S.M., Wadsworth M.H., 2nd, Treacy D., Trombetta J.J., Rotem A., Rodman C., Lian C., Murphy G. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-seq. Science. 2016;352:189–196. doi: 10.1126/science.aad0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uotila L., Koivusalo M. Formaldehyde dehydrogenase from human liver. Purification, properties, and evidence for the formation of glutathione thiol esters by the enzyme. J. Biol. Chem. 1974;249:7653–7663. [PubMed] [Google Scholar]
- Van der Auwera G.A., Carneiro M.O., Hartl C., Poplin R., Del Angel G., Levy-Moonshine A., Jordan T., Shakir K., Roazen D., Thibault J. From FastQ data to high confidence variant calls: the Genome Analysis Toolkit best practices pipeline. Curr. Protoc. Bioinformatics. 2013;43:11.10.1–11.10.33. doi: 10.1002/0471250953.bi1110s43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter D., Lier A., Geiselhart A., Thalheimer F.B., Huntscha S., Sobotta M.C., Moehrle B., Brocks D., Bayindir I., Kaschutnig P. Exit from dormancy provokes DNA-damage-induced attrition in haematopoietic stem cells. Nature. 2015;520:549–552. doi: 10.1038/nature14131. [DOI] [PubMed] [Google Scholar]
- Wang J., Morita Y., Han B., Niemann S., Löffler B., Rudolph K.L. Per2 induction limits lymphoid-biased haematopoietic stem cells and lymphopoiesis in the context of DNA damage and ageing. Nat. Cell Biol. 2016;18:480–490. doi: 10.1038/ncb3342. [DOI] [PubMed] [Google Scholar]
- Weeda G., Donker I., de Wit J., Morreau H., Janssens R., Vissers C.J., Nigg A., van Steeg H., Bootsma D., Hoeijmakers J.H. Disruption of mouse ERCC1 results in a novel repair syndrome with growth failure, nuclear abnormalities and senescence. Curr. Biol. 1997;7:427–439. doi: 10.1016/s0960-9822(06)00190-4. [DOI] [PubMed] [Google Scholar]
- Wolf F.A., Angerer P., Theis F.J. SCANPY: large-scale single-cell gene expression data analysis. Genome Biol. 2018;19:15. doi: 10.1186/s13059-017-1382-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabe M., Yabe H., Hamanoue S., Inoue H., Matsumoto M., Koike T., Ishiguro H., Morimoto T., Arakawa S., Ohshima T. In vitro effect of fludarabine, cyclophosphamide, and cytosine arabinoside on chromosome breakage in Fanconi anemia patients: relevance to stem cell transplantation. Int. J. Hematol. 2007;85:354–361. doi: 10.1532/IJH97.06191. [DOI] [PubMed] [Google Scholar]
- Yokoyama A., Muramatsu T., Omori T., Yokoyama T., Matsushita S., Higuchi S., Maruyama K., Ishii H. Alcohol and aldehyde dehydrogenase gene polymorphisms and oropharyngolaryngeal, esophageal and stomach cancers in Japanese alcoholics. Carcinogenesis. 2001;22:433–439. doi: 10.1093/carcin/22.3.433. [DOI] [PubMed] [Google Scholar]
- Yu R., Lai Y., Hartwell H.J., Moeller B.C., Doyle-Eisele M., Kracko D., Bodnar W.M., Starr T.B., Swenberg J.A. Formation, Accumulation, and Hydrolysis of Endogenous and Exogenous Formaldehyde-Induced DNA Damage. Toxicol. Sci. 2015;146:170–182. doi: 10.1093/toxsci/kfv079. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Single-cell RNA sequencing data have been deposited in Gene Expression Omnibus (accession GEO: GSE157832); genome sequencing data from HSPC clones have been deposited at the European Nucleotide Archive (accession ENA: PRJEB40375). Patient exome sequencing data have been deposited at the European Genome-Phenome Archive (accession EGA: EGAS00001003809). All other data and code are available upon reasonable request from the authors.