Abstract
Introduction:
Abdominal masses in children constitute a spectrum of lesions of diverse origin, nature and significance. In a low-income setting with limited investigative facilities, accurate diagnosis of abdominal masses can be very challenging. However, ultrasound has been used preferentially as a diagnostic tool in evaluating abdominal masses in children. This study aimed to determine the accuracy of ultrasound evaluation of abdominal masses in children.
Materials and Methods:
This was a prospective descriptive study of 135 consecutive children presenting with palpable and/or suspected abdominal masses over a 1-year period at a tertiary hospital. Data analyses were done using SPSS version 17 software and level of significance was set at P < 0.05.
Results:
Abdominal mass was located in the kidney in 40 (32.3%) patients. Definitive diagnoses of abdominal masses were confirmed intraoperatively in 33 (24.4%) and by histopathological examination in 102 (75.6%) cases. Abdominal masses were detected in 124/135 (91.9%) of the participants. Ultrasound (US) correctly identified 109/124 (87.9%) of the pathologies. The sensitivity and specificity of USS were 87.9% and 81.8%, respectively. Positive predictive value (PPV) and negative predictive value (NPV) were 97.2%–98.2% and 37.5%–45.7%, respectively. The overall US diagnostic accuracy was 87.4%. The predictive value of US for intussusceptions, Wilms' tumour and hydronephrosis was high (sensitivity was 92.0%, 95.8% and 81.1% and PPV was 90.0%, 83.0% and 93.8%, respectively). On the other hand, the sensitivity indices for appendiceal mass/abscess, lymphoma and neuroblastoma were low (28.6%, 66.7% and 57.1%, respectively), while their PPV was low too (66.7%, 42.9% and 77.7%, respectively). The PPV was especially poor for lymphoma. The specificity and NPV indices for these six disease conditions were good.
Conclusion:
Ultrasound is a reliable tool in the evaluation of abdominal masses in children in this setting.
Keywords: Abdominal masses, histopathological, negative predictive value, positive predictive value, sensitivity, specificity, ultrasound
INTRODUCTION
The management of an abdominal mass in a child requires a holistic approach which commonly entails clinical, radiological, surgical and/or histopathological evaluations.[1] Clinicians are usually desirous of a cost-effective imaging tool to facilitate the diagnostic process. A widely available, affordable and easily accessible imaging modality is indispensable to prompt management.[2] Ultrasonography is the most readily available imaging modality in Nigeria.
The aim of this study is to determine the sensitivity, specificity and predictive indices of Ultrasound (US) in the management of childhood abdominal masses in this setting.
MATERIALS AND METHODS
This study was a prospective descriptive study of 135 consecutive children presenting with abdominal masses at the Ahmadu Bello University Teaching Hospital, Zaria, within a 12-month period (from 5th August 2013 to 5th August 2014).
Study protocol
Written/informed consent was obtained from parents/guardians of all participants included in this study and ethical approval was obtained from the institution's Ethics and Research Committee.
Clinical assessment of each child at presentation included detailed clinical history and thorough physical examination, following which provisional diagnoses were made. All patients were then sent for ultrasonographic evaluation. All participants had real-time ultrasonographic evaluation using 3.5–7.5MHz frequency transducer (Mind ray [DC-8] ultrasound system). The evaluations were performed by consultant radiologists or senior registrar of at least 6-month supervised training in ultrasonographic scanning.
All patients had US done as the first-line diagnostic modality. The evaluation focused on the anatomical region of lesion, organ of origin of the mass and pathological description with diagnosis. The correct description of the mass with a presumptive diagnosis was noted.
Data analysis
Data were entered into a structured study pro forma and subsequently analysed using Statistical Package for the Social Sciences (SPSS) version 17 software (SPSS Chicago IL, USA). Level of statistical significance was set at P < 0.05.
Participants designated as 'true positive' (TP) had masses that were detected by USS. 'False negative' (FN) represented subjects with masses undetected by USS but were confirmed to be present, while 'false positive' (FP) was assigned to participants with masses seen at USS evaluation but confirmed to be absent. True negative (TN) represented participants with masses that were not detected by USS and actually confirmed to be absent.[3]
The accuracy indices were determined using the following formulae such as: Sensitivity (TP/TP + FN), specificity (TN/TN + FP), positive predictive value (TP/TP + FP), negative predictive value (NPV) (TN/TN + FN) and accuracy (TP + TN/TP + TN + FP + FN).[3,4,5]
RESULTS
Demographics
Of 135 study participants, 60.7% (82) were male and 39.3% (53) were female. The patients were aged 5 weeks–12 years (median 3 years), and distribution of abdominal masses in the 135 participants by age and sex is as shown in Table 1.
Table 1.
Distribution of abdominal masses in 135 children (age, sex and mass consistency)
| Diagnosis | Age group (years) | Male | Female | Total | Consistency | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| <1 | 1-4 | 5-8 | 9-12 | Total (%) | Cystic | Mixed | Solid | ||||
| Intussusceptions | 23 | 11 | 0 | 25 (18.5) | 13 | 12 | 25 | - | - | 25 | |
| Wilms’ tumour | 1 | 9 | 10 | 2 | 22 (16.3) | 10 | 12 | 22 | 2 | 18 | 2 |
| Hydronephrosis | 7 | 8 | 2 | 1 | 18 (13.3) | 15 | 3 | 18 | 17 | 1 | - |
| Lymphoma | 0 | 1 | 2 | 4 | 7 (5.2) | 4 | 3 | 7 | 1 | 2 | 4 |
| Appendiceal mass/abscess* | 0 | 1 | 1 | 57 (5.2) | 6 | 1 | 7 | 3 | 1 | - | |
| Neuroblastoma | 0 | 4 | 1 | 2 | 7 (5.2) | 1 | 6 | 7 | 0 | 2 | 4 |
| Hepatic tumour | 1 | 2 | 1 | 2 | 6 (4.4) | 5 | 1 | 6 | 1 | 2 | 3 |
| Sarcomas | 0 | 1 | 2 | 3 | 6 (4.4) | 5 | 1 | 6 | 0 | 4 | 2 |
| Omental/mesenteric cyst | 0 | 2 | 2 | 0 | 4 (3.0) | 2 | 2 | 4 | 2 | 2 | 0 |
| Other malignant tumours* | 1 | 0 | 0 | 3 | 4 (3.0) | 1 | 3 | 4 | 0 | 2 | 0 |
| Hypertrophic pyloric stenosis | 3 | 0 | 0 | 0 | 3 (2.2) | 3 | 0 | 3 | - | - | 3 |
| Female genital tract | 0 | 2 | 0 | 1 | 3 (2.2) | 0 | 3 | 3 | 1 | 2 | 0 |
| Pancreatic pseudocyst | 0 | 2 | 1 | 0 | 3 (2.2) | 3 | 0 | 3 | 3 | 0 | 0 |
| Choledochal cyst | 0 | 2 | 0 | 0 | 2 (1.5) | 1 | 1 | 2 | 2 | 0 | 0 |
| Other benign lesions* | 2 | 1 | 3 | 1 | 7 (5.2) | 7 | 0 | 7 | 4 | 2 | 0 |
| No pathological lesion* | 6 | 1 | 0 | 4 | 11 (8.1) | 6 | 5 | 11 | - | - | - |
| Total | 44 | 37 | 26 | 28 | 135 | 82 | 53 | 135 | 36 | 38 | 43 |
No pathological lesions→2 FP and 9 TN results. *Consistencies of 7 pathologies were not recorded as they constituted part of the false negative results and were not described ultrasonographically- 3 appendiceal lesions, 2 malignant conditions, 1 benign condition and 1 neuroblastoma. Consistencies for the other 8 FN pathologies were described. Total participants with recorded consistency (117), no description (7) and no pathological lesions (11) added up to 135. This was used as the denominator in the calculations involving. TN: True negative, FP: False positive, FN: False negative
Clinical presentation
The various clinical presentations in these patients were abdominal swelling (85 [52.1%]), abdominal pain (28 [17.2%]), incidentally detected masses (23 [14.1%]), vomiting (8 [4.9%]), passage of bloody mucoid stool (7 [4.3%]), fever (5 [3.1%]), haematuria (4 [2.5%]) and weight loss (3 [1.8%]). Duration of symptoms was 1 day–7 years (median 1 month) [Figure 1].
Figure 1.
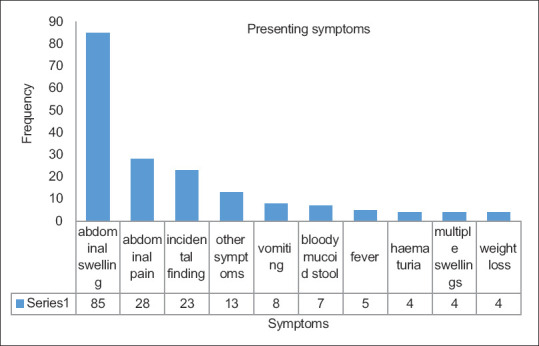
Presentation of 135 children with abdominal masses
Ultrasound scan correlated to clinical findings
Benign lesions accounted for 63.7% (79/124) of children, whereas 36.3% (45/124) had malignant lesions. Abdominal masses in the age group <5 years were mostly benign. Malignant masses were found commonly in those over 5 years, accounting for 53.7% (29/54) (χ2=30.6, df −3, P<0.05).
Cystic masses accounted for 36/135 (26.7%), mixed 38/135 (28.1%) and solid 43/135 (31.8%). In 11/135 (8.2%) participants who had no pathological lesions and in 7/135 (5.2%) participants that constituted part of the FN cases, there was no description for the masses.
The origin of abdominal masses was renal in 40 (32.3%), gastrointestinal tract (GIT) in 35 (28.2%), intraperitoneal (extra-GIT) in 22 (17.7%), retroperitoneal (extrarenal) in 12 (9.7%), appendiceal in 7 (5.7%), intrapelvic in 5 (4.0%) and female genital tract in 3 (2.4%).
Histopathological examination confirmed the diagnosis for 102/135 (75.6%) patients. In 33/135 (24.4%) patients, diagnoses were confirmed by intra-operative findings alone.
As shown in Figure 2, 85 (63%) participants required further investigative evaluation by use of other imaging modalities. Investigative modalities such as contrast-enhanced computed tomography (CECT) scan (26), IVU (17), US-guided percutaneous Trucut needle biopsy (14), VCUG (6), plain X-ray (6), radioisotope scanning (4), magnetic resonance imaging (MRI) (2) and others (10) were done in addition to US examination [Figure 2].
Figure 2.
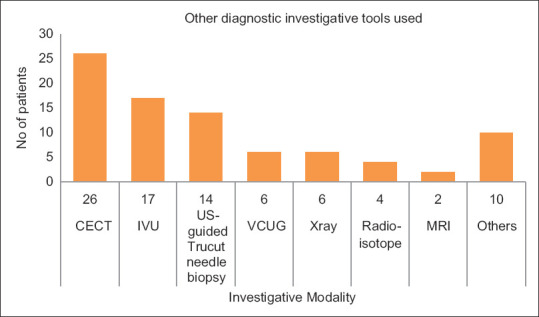
Various diagnostic tools employed
Definitive diagnoses of abdominal masses were confirmed intraoperatively in 33 (24.4%) and by histopathological examination in 102 (75.6%) cases. Abdominal masses were detected in 124/135 (91.9%) of the patients. USS pathological diagnosis was accurate in109 cases (TP). USS pathological diagnosis was incorrect in 15 cases (FN). In 9 patients, USS did not detect any lesions (TN), whereas 2 patients were wrongly tagged as having a pathological lesion (FP).
Ultrasound scan findings correlated to pathology
The overall diagnostic accuracy, sensitivity and specificity of ultrasound were found to be 87.4%, 87.9% and 81.8%, respectively. The accuracy of USS evaluation in making diagnosis of an abdominal mass with respect to PPV and NPV was 97.2%–98.2% and 37.5%–45.7%, respectively. (χ2=33.6, df =1, P≤0.05).
Diagnostic accuracy parameters were also calculated for the first six diagnoses (intussusceptions, Wilms' tumour, hydronephrosis, appendiceal mass/abscess, lymphoma and neuroblastoma). The specificity and NPV indices for these pathologies were good and encouraging. On one hand, the sensitivity and PPV for the first three diagnoses (intussusceptions, Wilms' tumour and hydronephrosis) ranged as follows: 81.8%–92.0% and 90.0%–95.8%, respectively. On the other hand, the sensitivity and the PPV for the next three diagnoses were notably low (appendiceal mass/abscess 28.6% and 66.7%, lymphoma 57.1% and 66.7% and neuroblastoma 42.9% and 77.7%, respectively) [Table 2]. All the above values were found to be statistically significant. Initial evaluation in two cases each for lymphoma and neuroblastoma was inconclusive.
Table 2.
The diagnostic indices of abdominal masses in 135 children
| Disease | Sensitivity (%) | Specificity (%) | PPV (%) | NPV% | χ2 | df | P |
|---|---|---|---|---|---|---|---|
| 1. Intussusception | 92.0 | 98.2 | 95.8 | 98.2 | 109.0 | 1 | <0.05 |
| 2. Wilms’ tumour | 81.8 | 96.5 | 90.0 | 97.4 | 93.5 | 1 | <0.05 |
| 3. Hydronephrosis | 83.0 | 99.0 | 93.8 | 98.3 | 93.5 | 4 | <0.05 |
| 4. Lymphoma | 57.1 | 98.4 | 66.7 | 97.7 | 48.3 | 1 | <0.05 |
| 5.Appendiceal mass/abscess | 28.6 | 99.2 | 66.7 | 96.2 | 16.8 | 1 | <0.05 |
| 6. Neuroblastoma | 42.9 | 97.7 | 77.7 | 96.9 | 30.4 | 2 | <0.05 |
| Overall accuracy (87.4%) | 87.9 | 81.8 | 97.2-98.2 | 37.5-45.7 | 33.6 | 1 | <0.05 |
PPV: Positive predictive value, NPV: Negative predictive value
DISCUSSION
An abdominal mass in a child constitutes a worry for the parent and a dilemma for the attending clinician. The ability of an investigative tool to make an accurate diagnosis within the shortest time is mostly desirable.
All the participants had ultrasonographic examination as the primary imaging investigative tool after clinical assessment. The diagnosis, however, changed in only 26/85 (30.6%) of the patients. CECT, IVU and US-guided biopsy were the most frequent alternative investigative modalities employed (in that order). MRI was done in only two participants. CECT considered the most versatile and creditable modality by some authors;[3,6] this was not supported report by other authors that discouraged the exposure of ionising radiation and the use of contrast media in children, affirming that US should still remain the modality of choice.[7,8] Our report also support this view.
The estimated overall diagnostic accuracy of US in detecting a pathological abdominal mass was high. This is comparable to reports in an Ethiopian study showing diagnostic accuracy at 88.9%.[9] Reports by other authors in separate studies show similar but slightly lower values (78%,[10] 82%[11] and 85%[12]). Sensitivity, specificity and positive predictive values were equally high and encouraging in our study as compared to other studies.[9,11] This is also similar to reports by Barker and Lindsell[11] and Kebede and Nigussie[9] However, NPV in this report was low (37.5%–45.7%), compared to high values recorded by other authors (97%[11] and 98.8%[9]). The reason for this difference from findings in the present study is not clear.
While the diagnostic accuracy in specific disease conditions showed good results for the diagnosis of conditions such as intussusceptions, Wilms' tumour and hydronephrosis, it was low in appendiceal abscess/mass, lymphoma and neuroblastoma. In accordance with current teaching, ultrasound has proven to detect intussusceptions with a high certainty of up to 100%,[13,14] this is relatively similar to the result of 92% in this study. This study found US to be very useful in diagnosing renal pathologies. Report by Annuar et al.[10] had 100% accuracy on detection of hydronephrosis. Report by Kebede and Nigussie[9] was also similar. Indices obtained for Wilms' tumour show that at least eight out of ten patients with this condition can correctly be diagnosed. The diagnostic accuracy of US of appendiceal mass/abscess was low (28.6%) in this study. This is comparable with another Nigerian study which gave a diagnostic accuracy of 24.4%.[15] Other studies showed varying reports. One author recorded 100%[11] accuracy for appendiceal abscess; another recorded a poor result, concluding that ultrasonographic appearances of GIT pathology are generally nonspecific.[16]
The diagnostic accuracy for lymphomas and neuroblastomas was also relatively low; this is contrary to other reports.[9,10] One report found US alone to be specifically insufficient in identifying the adrenal gland in children and providing pathological diagnosis and staging of adrenal neoplasm.[17] It was concluded, however, that US in a patient with adrenal neoplasm is useful as a guide to further diagnostic workup or can sometimes obviate the need for CT scan or MRI.[17,18]
The overall low NPV (37.5%–45.7%) observed in this study implies that clinicians should be careful in order not to miss an abdominal mass in 6 out of 10 normal children. In other words, if no mass was felt with high certainty amongst a group of normal children, then it will only be true in about 40% of the children. A case–control study may be required to further validate this concern. The low sensitivities observed for appendiceal abscess/mass, lymphoma and neuroblastoma should alert clinicians and sonologists to the possibility of missing these pathologies.
CONCLUSION
With the good and encouraging indices of ultrasonographic accuracy and the practical lessons obtained from this study, US should be given a priority in the diagnostic evaluation of abdominal masses in children in low-resource settings as ours. A multicentre randomised controlled study will be necessary to validate the result of this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
In the preparation of this research, I have received aid from my teachers, mentors, supervisors and many others. I must, however, make exceptions by expressing my particular gratitude to Prof Garba, Drs Abdulrahman, Igoche, Anyanwu and Dr Kajogbola, for their valuable suggestions, moral supports, guidance and patience.
I'm grateful to my family members for their sacrifices, attending to the needs (in cash, in kind, emotionally and spiritually) of my wife and children when it mattered most. Topmost on my list are my Mothers (Mrs B J A Adedayo, Mrs V. A. Towobola and Mrs Fatounde) and my Fathers (Mr F. A. Adedayo, Major R. A. Towobola(rtd) and Hon. R. F. Adedayo). To my siblings and in-laws, 'I doff my hat'.
To my sweetheart, Dr(Mrs) Grace Adedamola Adedayo, and my lovely children: Adedimeji and Ti-kristi-ni and Ayodele l dedicate this article.
REFERENCES
- 1.Ahmed I, Nazir R, Chaudhary MY, Kundi S. Triple Assessment of Breast Lump. J Coll Physicians Surg Pak. 2007;17:535–8. [PubMed] [Google Scholar]
- 2.Altman DG, Bland JM. Diagnostic tests 1: Sensitivity and specificity. BMJ. 1994;308:1552. doi: 10.1136/bmj.308.6943.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crane GL, Hernanz-Schulman M. Current imaging assessment of congenital abdominal masses in pediatric patients. Semin Roentgenol. 2012;47:32–44. doi: 10.1053/j.ro.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Wong HB, Lim GH. Measures of Diagnostic Accuracy: Sensitivity, Specificity, PPV, NPV Statistics. [Last accessed on 2014 Jun 26]. Available from: http://wwwsinghealthacademyedusg/Documents/Publications/vol20No420011/11_stats_032-0911WongHBpdf .
- 5.Glaros AG, Kline RB. Understanding the accuracy of tests with cutting scores: The sensitivity, specificity, and predictive value model. J Clin Psychol. 1988;44:1013–23. doi: 10.1002/1097-4679(198811)44:6<1013::aid-jclp2270440627>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 6.Peng Y, Jia L, Sun N, Li J, Fu L, Zeng J, et al. Assessment of cystic renal masses in children: Comparison of multislice computed tomography and ultrasound imaging using the Bosniak classification system. Eur J Radiol. 2010;75:287–92. doi: 10.1016/j.ejrad.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 7.Elder JE. Abdominal masses in children. In: Resnick MI, Novick CA, editors. Urology Secrets. 2nd ed. New Delhi: Jaypee Brothers Med Publishers (P) Ltd; 1999. pp. 27–8. [Google Scholar]
- 8.Onur MR, Bakal U, Kocakoc E, Tartar T, Kazeez A. Cystic abdominal masses in children: A pictorial essay. J Clin Imaging. 2012;3:1–9. doi: 10.1016/j.clinimag.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Kebede AG, Nigussie Y. Ultrasound evaluation of abdominal masses in Ethiopian child patients. Trop Doct. 2011;41:157–9. doi: 10.1258/td.2011.100253. [DOI] [PubMed] [Google Scholar]
- 10.Annuar Z, Sakijan AS, Annuar N, Kooi GH. Ultrasound in the diagnosis of palpable abdominal masses in children. Med J Malaysia. 1990;45:281–7. [PubMed] [Google Scholar]
- 11.Barker CS, Lindsell DR. Ultrasound of the palpable abdominal mass. Clin Radiol. 1990;41:98–9. doi: 10.1016/s0009-9260(05)80137-0. [DOI] [PubMed] [Google Scholar]
- 12.Hill BA, Yamaguchi K, Flynn JJ, Miller DR. Diagnostic sonography in general surgery. Arch Surg. 1975;110:1089–94. doi: 10.1001/archsurg.1975.01360150033006. [DOI] [PubMed] [Google Scholar]
- 13.Hesse AA, Abantanga FA, Lakhoo K. Intussusceptions. In: Ameh EA, Bickler SW, Nwomeh BC, Poenaru D, editors. Paediatric Surgery: A Comprehensive Text for Africa. Vol. 2. Seattle, WA USA: Global HELP Organization; 2012. pp. 405–11. [Google Scholar]
- 14.Ko HS, Schenk JP, Tröger J, Rohrschneider WK. Current radiological management of intussusception in children. Eur Radiol. 2007;17:2411–21. doi: 10.1007/s00330-007-0589-y. [DOI] [PubMed] [Google Scholar]
- 15.Garba ES, Chom ND. Ultrasound in the diagnosis of appendicitis: A plea for caution. Niger J Surg Res. 2006;8:3–4. [Google Scholar]
- 16.Salem S, O'Malley BP, Hitz CW. Ultrasonographic appearances of gastrointestinal masses. J Can Assoc Radiol. 1980;31:163–7. [PubMed] [Google Scholar]
- 17.Petrus LV, Hall TR, Ines B, Westra SJ, Curran JG, Steckel RJ, Kangarloo H. The paediatric patient with suspected adrenal neoplasm: Which radiological test to use? Med Paediatr Oncol. 1992;20:53–7. doi: 10.1002/mpo.2950200111. [DOI] [PubMed] [Google Scholar]
- 18.Wicks JD, Silver TM, Bree RL. Giant cystic abdominal masses in children and adolescents: Ultrasonic differential diagnosis. AJR Am J Roentgenol. 1978;130:853–7. doi: 10.2214/ajr.130.5.853. [DOI] [PubMed] [Google Scholar]


