Abstract
Background/Aims
Stress, in its various forms, plays an important role in the development and evolution of inflammatory bowel disease (IBD). For patients with IBD, the evidence related to the effects of various types of psychological therapies remains inconclusive. This study aimed to evaluate whether cognitive behavioral therapy, in combination with educational counseling, influenced disease activity and quality of life (QoL) among patients with IBD.
Materials and Methods
We conducted a randomized controlled trial with 60 patients diagnosed with IBD. All patients completed the IBD questionnaire-32 (IBDQ-32) and the Big Five Inventory. Group A (experimental group) received specialized educational and psychological counseling (SEPC), and group B (control group) was treated according to the current medical practice. All patients were reassessed after 12 months.
Results
After the SEPC, there was no improvement in disease activity as estimated by fecal calprotectin levels. However, the QoL of patients in group A was significantly improved. The highest mean difference between the initial and final IBDQ scores was found among patients whose main personality trait was openness to experience (48.58±28.80), and the lowest mean difference between these 2 scores was found among patients whose main personality trait was closedness to experience (3.33±2.97, p=0.009).
Conclusion
Although there was no improvement in disease activity after the SEPC, this therapy improved patients’ QoL in terms of both emotional and social functions, especially among patients whose dominant personality trait was openness to experience or neuroticism.
Keywords: Inflammatory bowel disease, cognitive behavioral therapy, quality of life, personality trait
INTRODUCTION
In the 21st century, inflammatory bowel disease (IBD) has become globally prevalent (1). Over the past 2 decades, ulcerative colitis and Crohn’s disease have emerged as debilitating chronic conditions associated with complications, surgery, and high hospitalization costs. There is a growing body of evidence indicating that the incidence and prevalence rates of IBD are expanding worldwide, with IBD currently affecting over 2.2 million people in Europe and over 1.5 million in the United States (2). IBD currently affects the most active segment of the population, that is, usually those aged 20–30 years for Crohn’s disease and those aged 30–40 years for ulcerative colitis. The disease is infrequent among patients over the age of 65 years (2). Despite having a low mortality rate, IBD has significant effects on quality of life (QoL), educational performance, and workplace participation (3).
Novel therapies targeting several immune pathways have been developed for the treatment and disease management of patients with IBD. New and emerging therapies have improved the overall outcomes, symptoms, and mucosal healing, altering the natural history of the disease (3). Stress, in its various forms, plays an important role in the development and evolution of IBD. Emotional disorders have a higher incidence among patients with IBD than the general population (4). Moreover, depression and anxiety may negatively influence the natural course of the disease (5).
Psychological interventions have been found to benefit patients suffering from chronic diseases. Recent studies have demonstrated improvements in QoL among patients with chronic kidney disease who had undergone hemodialysis (6) and those with chronic rheumatic diseases (7), neoplasia (8), and chronic hepatic diseases who were registered in support groups (9).
For patients with IBD, the evidence related to the effects of various types of psychological therapies remains inconclusive (10). Numerous clinical studies support the idea that psychosocial aspects represent an important dimension of IBD. A meta-analysis referring to the assessment of patients living with IBD has shown the harmful influence of the disease on QoL (11). Furthermore, recent studies have concluded that psychological therapies, especially cognitive behavioral therapy (CBT), might have small short-term beneficial effects on depression scores and QoL among patients with IBD (12).
Therefore, we designed and created a support group for patients with IBD to provide easy access to CBT. We aimed to evaluate whether CBT, in combination with educational counseling, influences disease activity and QoL among patients with IBD.
MATERIALS AND METHODS
We conducted a randomized controlled trial with 60 patients diagnosed with IBD. We included adult patients with previously diagnosed IBD (clinical, biological, endoscopic, imagistic, or histological diagnosis). Patients with undetermined colitis, colorectal cancer, other neoplasia, or psychiatric disorders were not included in the study. After enrollment, the patients’ medical records, including fecal calprotectin levels and demographic data, were collected and compiled into a database. All patients also completed 2 questionnaires: the IBD questionnaire-32 (IBDQ-32) and the Big Five Inventory (BFI). Patients were randomized (1:1) into 2 groups. Group A (experimental group) included 30 patients who received specialized educational and psychological counseling (SEPC), and group B (control group) included 30 patients treated according to the current medical practices. All patients were reassessed after 12 months (using medical records, fecal calprotectin levels, and the IBDQ-32).
Measurements
Disease activity was estimated using the level of fecal calprotectin. Patients avoided nonsteroidal anti-inflammatory drugs for 2 days before stool collection. Approximately 2 g of stool was collected (irrespective of the time of day) in a disposable container, which was sealed with a cap. These samples were kept in a refrigerator at 2°C–8°C for up to 7 days if they could not be treated immediately. The results were obtained using the fluoro-immunoenzymatic method. Fecal calprotectin values >50 mg/kg (μg/g) were considered to indicate intestinal inflammation.
QoL was quantified using the IBDQ-32. This well-validated, disease-specific instrument for measuring QoL among patients with IBD has previously been translated and validated for patients in Romania (12). The questionnaire includes 32 items structured into 4 fields: IBDQ1, gastrointestinal symptoms (diarrheic stools, abdominal pain, rectorrhagia, and rectal tenesmus); IBDQ2, systemic symptoms (fatigue and sleep disorders), IBDQ3, emotional functions (depression, irritability, anger, and sexual activity); and IBDQ4, social functions (absenteeism and changes in social status). The questionnaire responses ranged from 1 (worst) to 7 (best), with total scores ranging from 32 to 224. We also computed a sub-score for each distinct field (emotional functions: 12–84, gastrointestinal symptoms: 10–70, systemic symptoms: 5–35, and social functions: 5–35). Lower scores indicate more affected QoL (13).
Personality traits were evaluated using the BFI, which is a self-report inventory including 44 items designed to measure the 5 dimensions of personality (14). Each factor is then further divided into personality facets (Table 1). In the BFI analysis, a patient can show several personality traits in various proportions. In the statistical analysis, we used the dominant personality trait of each patient.
Table 1.
The big five factors.
| Big 5 dimensions | Facet (and correlated trait adjective) |
| Extraversion vs. introversion | Gregariousness (sociable) |
| Assertiveness (forceful) | |
| Activity (energetic) | |
| Excitement seeking (adventurous) | |
| Positive emotions (enthusiastic) | |
| Warmth (outgoing) | |
| Agreeableness vs. antagonism | Trust (forgiving) |
| Straightforwardness (not demanding) | |
| Altruism (warm) | |
| Compliance (not stubborn) | |
| Modesty (not a show-off) | |
| Tender mindedness (sympathetic) | |
| Conscientiousness vs. lack of direction | Competence (efficient) |
| Order (organized) | |
| Dutifulness (not careless) | |
| Achievement striving (thorough) | |
| Self-discipline (not lazy) | |
| Deliberation (not impulsive) | |
| Neuroticism vs. emotional stability | Anxiety (tense) |
| Anger/hostility (irritable) | |
| Depression (not contented) | |
| Self-consciousness (shy) | |
| Impulsiveness (moody) | |
| Vulnerability (not self-confident) | |
| Openness vs. closedness to experience | Ideas (curious) |
| Fantasy (imaginative) | |
| Esthetics (artistic) | |
| Actions (wide interests) | |
| Feelings (excitable) | |
| Values (unconventional) |
This table was recreated from the work of John and Srivastava, 1999 (15).
Intervention
The educational counseling consisted of 1 session per month for 6 months for each group of 7–8 patients. In these sessions, issues related to etiopathogenesis, symptomatology, diagnosis, paraclinical diagnosis complications, nutrition, and treatment of IBD were presented to patients by gastroenterologists in an accessible manner. Psychological counseling was based on cognitive behavioral techniques. The SEPC group met weekly at a tertiary hospital for 6 months for 2-hour sessions carried out by a qualified clinical psychologist. The psychologist’s training and supervision were provided by Alexandru I Cuza University. This program focused on improving coping among patients with IBD. The interventional plan is detailed in Table 2.
Table 2.
Interventional plan.
|
Session 1: 90 minutes Introduction and self-introduction, CBT training, CBT conceptualization, drafting a list of needs and issues related to IBD, inventory of the psychological effects of IBD, and assessment of medical treatment needs Completion of the BFI and IBDQ-32 questionnaires Homework: Daily activity record |
|
Session 2: 90 minutes Behavioral assessment, behavioral ABCs, behavioral activation, and activity planning Psychoeducation on the psychological manifestations of chronic digestive diseases Homework: Daily activity record and reward planning |
|
Session 3: 90 minutes Cognitive assessment, cognitive therapy: role of thoughts in experiences with depression and/or anxiety and identification of automatic negative thoughts Monitoring stressful situations and managing stress and negative emotions Psychoeducation on diet Homework: Daily record of automatic dysfunctional thoughts and daily activity record |
|
Session 4: 90 minutes Social skills development and monitoring dysfunctional negative thoughts Behavioral activation and assertiveness development Cognitive ABCs: doubting dysfunctional negative thoughts Homework: Daily record of automatic dysfunctional thoughts and daily activity record |
|
Session 5: 90 minutes ABCs of realistic thinking: formulation of alternative thoughts Identifying and debating dysfunctional beliefs Optimization and personal development: assertive communication, time management, stress management, and negative emotions management Psychoeducation on couple/family relationships Homework: Daily record of automatic dysfunctional thoughts and their replacement with alternative, realistic thoughts, and continuing debate of dysfunctional beliefs. |
|
Session 6: 90 minutes Optimization and personal development: increased frequency of positive social contacts and problem solving Assessment of the extent to which negative schemes have influenced important life experiences Identification of more realistic beliefs and patterns Homework: Continuing to identify and discuss automatic thoughts, dysfunctional beliefs, and negative patterns and to replace them with adaptive thoughts and patterns |
|
Session 7: 90 minutes Follow-up and prevention of relapses Completion of the IBDQ-32 questionnaire Identification of effective interventions used Plans for possible depressive and/or anxious episodes in the future |
BFI: Big Five Inventory; CBT: cognitive behavioral therapy; IBD: inflammatory bowel disease; IBDQ-32: inflammatory bowel disease questionnaire-32
All patients enrolled in the study signed an informed consent form, which explained the details of the purpose of the study, study methods, and the risks and benefits involved in the study and provided information regarding the confidentiality of the results. The study was approved by the local ethical committee.
RESULTS
There were no statistically significant differences in the demographic characteristics between groups A and B (Table 3).
Table 3.
Characteristics of the experimental and control groups before SEPC.
| Characteristic | Group A (n=30) | Group B (n=30) | p |
|---|---|---|---|
| Male, n (%) | 20 (66.7) | 17 (56.7) | 0.425* |
| Female, n (%) | 10 (33.3) | 13 (43.3) | |
| Age, years, mean±standard deviation | 43.27±14.21 | 44.67±11.16 | 0.673** |
| Urban, n (%) | 20 (66.7) | 20 (66.7) | nc |
| Rural, n (%) | 10 (33.3) | 10 (33.3) | |
| UC | 21 (70.0) | 25 (83.3) | 0.220* |
| CD | 9 (30.0) | 5 (16.7) | |
| Activity | 17 (56.7) | 16 (53.3) | 0.797* |
| Remission | 13 (43.3) | 14 (46.7) | |
| IBDQ total, means±standard deviations | 144.23±31.14 | 141.57±34.54 | 0.790** |
| IBDQ1, means±standard deviations | 49.93±13.18 | 46.67±13.76 | 0.351** |
| IBDQ2, means±standard deviations | 23.93±7.16 | 22.07±6.87 | 0.307** |
| IBDQ3, means±standard deviations | 50.77±16.10 | 54.60±16.04 | 0.359** |
| IBDQ4, means±standard deviations | 21.63±5.71 | 22.70±6.10 | 0.503** |
| Calprotectin, μg/g, means±standard deviations | 149.10±120.79 | 174.40±149.98 | 0.475** |
IBDQ: inflammatory bowel disease questionnaire; IBDQ1: inflammatory bowel disease questionnaire-1 score, gastrointestinal symptoms; IBDQ2: inflammatory bowel disease questionnaire-2 score, systemic symptoms; IBDQ3: inflammatory bowel disease questionnaire-3 score, emotional functions; IBDQ4: inflammatory bowel disease questionnaire-4 score, social functions; SPEC: specialized educational and psychological counseling
Chi-squared test;
Student’s t test; nc; group A (experimental group); group B (control group)
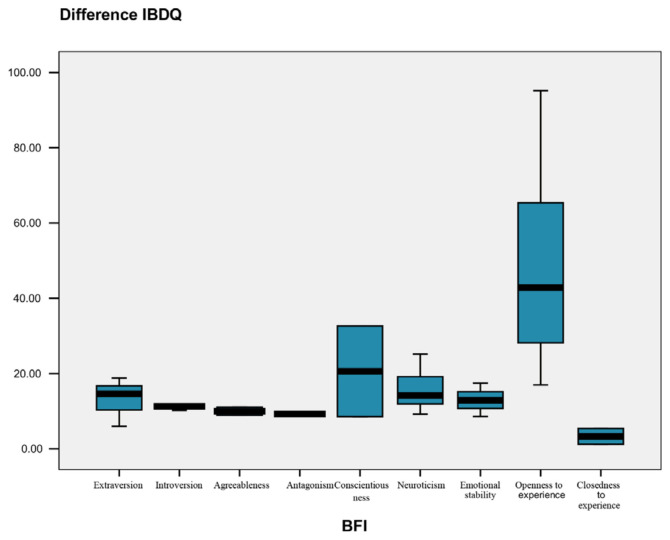
According to the BFI evaluation, only 9 of the 10 personality traits were found dominantly in the study groups. The most frequent dominant personality traits were openness to experience and neuroticism (Figure 1).
Figure 1.
Study groups by dominant personality trait. Group A (experimental group) and group B (control group).
After SEPC, there was no improvement in disease activity as estimated by fecal calprotectin levels (Table 4). However, the QoL of patients in group A was significantly improved (Table 5).
Table 4.
Fecal calprotectin evaluation in the study groups.
| Group A | pa | Group B | p | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| First evaluation (n=30) | Re-evaluation (n=30) | First evaluation (n=30) | Re-evaluation (n=30) | |||
| Fecal calprotectin (μg/g) | 149.10±120.79 | 95.30±69.41 | 0.002 | 174.40±149.98 | 140.70±130.26 | 0.096 |
Group A (experimental group); group B (control group); p=0.002a statistically significant.
Table 5.
Evaluation of the IBDQ score.
| Characteristic | Group A | P | Group B | p | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| First evaluation (n=30) | Re-evaluation (n=30) | First evaluation (n=30) | Re-evaluation (n=30) | |||
| IBDQ total means±standard deviations | 144.23±31.14 | 168.90±24.47 | 0.001a | 141.57±34.54 | 138.43±34.04 | 0.852 |
| IBDQ1 means±standard deviations | 49.93±13.18 | 53.67±12.33 | 0.061 | 46.67±13.76 | 46.87±13.74 | 0.909 |
| IBDQ2 means±standard deviations | 23.93±7.16 | 27.17±6.46 | 0.101 | 22.07±6.87 | 22.83±6.31 | 0.923 |
| IBDQ3 means±standard deviations | 50.77±16.10 | 62.27±10.24 | 0.001a | 54.60±16.04 | 51.17±15.87 | 0.426 |
| IBDQ4 means±standard deviations | 21.63±5.71 | 26.83±5.13 | 0.001a | 22.70±6.10 | 21.00±5.82 | 0.372 |
IBDQ: inflammatory bowel disease questionnaire score
Group A (experimental group); group B (control group); p=0.001a statistically very significant.
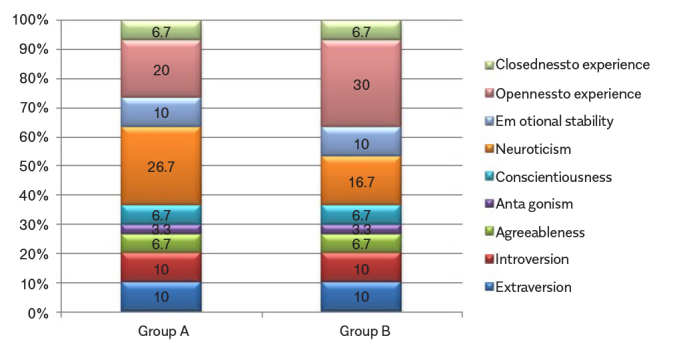
The effect of SEPC on QoL was later analyzed by patient’s dominant personality trait in the BFI questionnaire. The highest mean difference between the initial and final IBDQ scores was found among patients whose main personality trait was openness to experience (48.58±28.80), and the lowest mean difference between these 2 scores was found among patients whose main personality trait was closedness to experience (3.33±2.97); this difference was statistically significant (p=0.009; Figure 2).
Figure 2.
Average difference between the initial and final inflammatory bowel disease questionnaire scores.
DISCUSSION
IBD, which is associated with physical, social, and emotional dysfunction, has a significant impact on QoL. Disease activity is one of the most important factors contributing to the decreased QoL (15).
In this study, QoL was assessed using a specific instrument, the IBDQ-32. To the best of our knowledge, there is little information related to defining an IBDQ-32 score threshold for considering a patient’s QoL as normal. In this study, the overall score obtained was similar to that reported in previous studies (16). QoL was evaluated both among patients who received SEPC and among those who were treated according to the current medical practice. There were no significant differences between the 2 groups at the start of the study.
Most of the previous studies have used activity scores, which may include subjective items, to evaluate disease activity. In our research, disease activity was estimated using the level of fecal calprotectin, which is a non-invasive biomarker known for its ability to assess disease activity among patients with IBD (17).
Several studies available in literature evaluate the efficacy of CBT among patients with IBD (18, 19). However, this study included specialized psychological therapy and an educational component. Patients were trained monthly on the medical implications of IBD. Educational materials included information on disease etiopathogenesis, paraclinical tests, treatment, and nutrition for individuals with IBD.
Previous studies have shown that psychological stress is an important predictor of disease activity (20). Therefore, we assumed that psychosocial education would help the patients to cope with day-to-day stress and reduce the number of activity breaks. However, previous studies described no improvement in disease activity (21). This may be because of short follow-up periods and also because few patients experienced activity during this period. These findings were similar to those of a recent study that used CBT (18). In our study, 1 patient had serious complications, with the appearance of a toxic megacolon-requiring total proctocolectomy. Excluding this patient, no statistically significant difference was observed in the activity assessed by the specific scores at the start and end of the study. In addition, the level of calprotectin used to evaluate endoscopic activity did not vary significantly.
QoL was significantly improved by the SEPC. No statistically significant differences were observed in the IBDQ1 (gastrointestinal symptoms) or IBDQ2 (systemic symptoms) sub-scores. This can be explained by the fact that the SEPC had a low impact on disease activity in general. In contrast, statistically significant differences were found in the IBDQ3 (emotional functions) and IBDQ4 (social functions) sub-scores. We noticed that at the end of the therapy, patients were much more aware of what it meant to live with IBD, more easily accepted the permanence of this disease in their lives, and were better prepared to coexist with the disease. In addition, social activities improved with patients becoming more active in their social lives.
Existing findings regarding the role of psychological stress management methods for the evolution of IBD are controversial (19). Eccleston et al. (22) evaluated the effectiveness of psychological interventions among adolescents with IBD and reported promising results. CBT and counseling have played a crucial role in treatment of various psychological disorders because of a solid conceptual grounding, and there is convincing scientific literature referring to the effectiveness of these therapies (23). These therapies include a variety of techniques and methods that focus on the role of cognitive, behavioral, and environmental factors in the presence or absence of the disease. Additional findings by Schoultz et al. (24) showed the effectiveness of this therapy for patients with IBD. Although the psychological component of the etiology of IBD is currently uncertain, the disease is associated with significant psychological disorders. However, despite the association between IBD and psychological disorders, which has been demonstrated by many studies, very few patients with IBD who also have mental disorders or psychiatric symptoms undergo psychotherapy. A Dutch study showed that <40% of patients with IBD received psychotherapy because of low addressability and limited access to psychotherapists (25). Similarly, a recent national audit in the United Kingdom reported that only 12% of patients with IBD were referred to a psychotherapist by their general practitioner or gastroenterologist (26). After reviewing 17 studies, Goodhand et al. (27) concluded that CBT was effective for mood disorders and for improving patients’ QoL. McCombie et al. (28) analyzed all relevant Cochrane reviews and selected 18 final studies to identify different types of therapy treatments. CBT was found to be the most efficient, by far, with more positive outcomes than those of counseling and psychotherapy.
Our study had 2 major limitations, which were the small group of patients involved and the short follow-up period. However, existing studies on CBT among patients with IBD have had similar follow-up periods and numbers of patients comparable to that in this study (12).
The main strength and novelty of this study is the stratification of patients by personality traits, allowing for identification of the subgroup for whom CBT and educational counseling were the most effective. The results obtained show that this type of intervention is especially effective for patients with a dominant personality trait of openness to experience or neuroticism. To the best of our knowledge, this is the first prospective study to stratify patients using the BFI. Some existing studies have used QoL assessment questionnaires to identify patients who may respond to psychological therapies (29, 30). Apart from these aspects, our study showed that CBT did not influence the activity of IBD as evaluated objectively using fecal calprotectin levels.
In conclusion, patients with IBD have an impaired QoL. Although there was no improvement in disease activity after the SEPC, this therapy improved patients’ QoL in terms of both emotional and social functions, especially among patients who have the dominant personality trait of openness to experience or neuroticism. The effect of these therapies on disease activity may have been low because of the short period of application. Future studies are needed to assess the long-term effects and identify patients who may benefit from CBT and educational counseling as an integral part of their therapeutic management.
MAIN POINTS.
This study aimed to evaluate whether cognitive behavioral therapy, in combination with educational counseling, influenced disease activity and quality of life among patients with inflammatory bowel disease.
Although there was no improvement in disease activity after the therapy and counseling sessions, this therapy improved patients’ quality of life in terms of both emotional and social functions, especially among patients whose dominant personality trait was openness to experience or neuroticism.
Acknowledgements
We thank Jennifer Barrett, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Footnotes
Ethics Committee Approval: Ethics committee approval was received fort his study from the Research Ethics Commission of UMF “Grigore T. Popa” Iasi (decision date – 29.12.2016).
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – O.G., M.D., C.M.; Design – O.G., C.S., C.M.; Supervision – C.C.P., C.M., M.D.; Resource – O.G., C.C.P., C.M.; Materials – O.G., C.S., C.C.P.; Data Collection and/or Processing – O.G., M.D., C.M.; Analysis and/or Interpretation – O.G., M.D., C.M.; Literature Search – O.G., M.D., C.M.; Writing - O.G., M.D., C.M.; Critical Reviews – C.C.P., C.S., C.M.
Conflict of Interest: The auhtors have no conflict of interest to declare.
Financial Disclosure: This work was supported by the “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania – Grant 29026/28.11.2016.
REFERENCES
- 1.Ng SC, Shi HY, Hamidi N. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390:2769–78. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 2.Burisch J, Munkholm P. The epidemiology of inflammatory bowel disease. Scand J Gastroenterol. 2015;50:942–51. doi: 10.3109/00365521.2015.1014407. [DOI] [PubMed] [Google Scholar]
- 3.Lonnfors S, Vermeire S, Greco M, Hommes D, Bell C, Avedano L. IBD and health-related quality of life-discovering the true impact. J Crohns Colitis. 2014;8:1281–6. doi: 10.1016/j.crohns.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Neurath MF, Travis SP. Mucosal healing in inflammatory bowel diseases: a systematic review. Gut. 2012;61:1619–35. doi: 10.1136/gutjnl-2012-302830. [DOI] [PubMed] [Google Scholar]
- 5.Brzozowski B, Mazur-Bialy A, Pajdo R, et al. Mechanisms by which stress affects the experimental and clinical inflammatory bowel disease (IBD): role of brain-gut axis. Curr Neuropharmacol. 2016;14:892–900. doi: 10.2174/1570159X14666160404124127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burke KE, Boumitri C, Ananthakrishnan AN. Modifiable environmental factors in inflammatory bowel disease. Curr Gastroenterol Rep. 2017;19:21. doi: 10.1007/s11894-017-0562-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lerma A, Perez-Grovas H, Bermudez L, et al. Brief cognitive behavioural intervention for depression and anxiety symptoms improves quality of life in chronic haemodialysis patients. Psychol Psychother. 2017;90:105–23. doi: 10.1111/papt.12098. [DOI] [PubMed] [Google Scholar]
- 8.Couppé C, Comins J, Beyer N, et al. Health-related quality of life in patients with chronic rheumatic disease after a multidisciplinary rehabilitation regimen. Qual Life Res. 2016;26:381–91. doi: 10.1007/s11136-016-1402-7. [DOI] [PubMed] [Google Scholar]
- 9.Meijer A, Roseman M, Delisle VC, et al. Effects of screening for psychological distress on patient outcomes in cancer: a systematic review. J Psychosom Res. 2013;75:10. doi: 10.1016/j.jpsychores.2013.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valery PC, Powell E, Moses N, et al. Systematic review: unmet supportive care needs in people diagnosed with chronic liver disease. BMJ Open. 2015;5:e007451. doi: 10.1136/bmjopen-2014-007451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huppertz-Hauss G, Høivik ML, Langholz E, et al. Health-related quality of life in inflammatory bowel disease in a European-wide population-based cohort 10 years after diagnosis. Inflamm Bowel Dis. 2015;21:337–44. doi: 10.1097/MIB.0000000000000272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bennebroek Evertsz’ F, Thijssens NA, Stokkers PC, et al. Do inflammatory bowel disease patients with anxiety and depressive symptoms receive the care they need? J Crohns Colitis. 2012;6:68–76. doi: 10.1016/j.crohns.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Verissimo R. Quality of life in inflammatory bowel disease: psychometric evaluation of an IBDQ cross-culturally adapted version. J Gastrointestin Liver Dis. 2008;17:439–44. [PubMed] [Google Scholar]
- 14.John OP, Srivastava S. The Big Five trait taxonomy: history, measurement, and theoretical perspectives. In: John OP, Pervin LA, editors. Handbook of personality: Theory and research. Vol. 2. The Guilford Press; New York: 1999. pp. 102–38. [Google Scholar]
- 15.Knowles SR, Graff LA, Wilding H. Quality of life in inflammatory bowel disease: a systematic review and meta-analyses - Part I. Inflamm Bowel Dis. 2018;24:742–51. doi: 10.1093/ibd/izy015. [DOI] [PubMed] [Google Scholar]
- 16.Habibi F, Habibi ME, Gharavinia A, et al. Quality of life in inflammatory bowel disease patients: a cross-sectional study. J Res Med Sci. 2017;22:104. doi: 10.4103/jrms.JRMS_975_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bjarnason I. The use of fecal calprotectin in inflammatory bowel disease. Gastroenterol Hepatol. 2017;13:53–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Mikocka-Walus A, Bampton P, Hetzel D, Hughes P, Esterman A, Andrews JM. Cognitive-behavioural therapy for inflammatory bowel disease: 24-month data from a randomised controlled trial. Int J Behav Med. 2017;24:127–35. doi: 10.1007/s12529-016-9580-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Timmer A, Preiss JC, Motschall E, et al. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2011;16:CD006913. doi: 10.1002/14651858.CD006913.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Hisamatsu T, Inoue N, Yajima T, et al. Psychological aspects of inflammatory bowel disease. J Gastroenterol. 2007;42:34–40. doi: 10.1007/s00535-006-1937-4. [DOI] [PubMed] [Google Scholar]
- 21.Knowles SR, Monshat K, Castle DJ. The efficacy and methodological challenges of psychotherapy for adults with inflammatory bowel disease: a review. Inflamm Bowel Dis. 2013;19:2704–15. doi: 10.1097/MIB.0b013e318296ae5a. [DOI] [PubMed] [Google Scholar]
- 22.Mikocka-Walus A, Bampton P, Hetzel D, Hughes P, Esterman A, Andrews JM. Cognitive-behavioural therapy for inflammatory bowel disease: 24-month data from a randomised controlled trial. Int J Behav Med. 2017;24:127–35. doi: 10.1007/s12529-016-9580-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Timmer A, Preiss JC, Motschall E, et al. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2011;16:CD006913. doi: 10.1002/14651858.CD006913.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Eccleston C, Fisher E, Law E, et al. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2012;4:CD009660. doi: 10.1002/14651858.CD009660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Farmer RF, Chapman AL American Psychological Association. Behavioral Interventions in Cognitive Behavior Therapy: Practical Guidance for Putting Theory into Action. Washington, DC: American Psychological Association; 2008. [Google Scholar]
- 26.Schoultz M, Atherton I, Watson A. Mindfulness-based cognitive therapy for inflammatory bowel disease patients: findings from an exploratory pilot randomised controlled trial. Trials. 2015;16:379. doi: 10.1186/s13063-015-0909-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennebroek Evertsz’ F, Bockting CL, Stokkers PC, et al. The effectiveness of cognitive behavioral therapy on the quality of life of patients with inflammatory bowel disease: multicenter design and study protocol (KL!C-study) BMC Psychiatry. 2012;12:227. doi: 10.1186/1471-244X-12-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Royal College of Physicians. National Audit Report of Inflammatory Bowel Disease Service Provision: Adult National Report. London: Royal College of Physicians; 2014. [Google Scholar]
- 29.Goodhand JR, Wahed M, Rampton DS. Management of stress in inflammatory bowel disease: a therapeutic option? Expert Rev Gastroenterol Hepatol. 2009;3:661–79. doi: 10.1586/egh.09.55. [DOI] [PubMed] [Google Scholar]
- 30.McCombie AM, Mulder RT, Gearry RB. Psychotherapy for inflammatory bowel disease: a review and update. J Crohns Colitis. 2013;7:935–49. doi: 10.1016/j.crohns.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Riehl ME, Kinnucan JA, Chey WD, Stidham RW. Nuances of the psychogastroenterology patient: a predictive model for gastrointestinal quality of life improvement. Neurogastroenterol Motil. 2019;201:e13663. doi: 10.1111/nmo.13663. [DOI] [PubMed] [Google Scholar]
- 32.Kinsinger SW, Ballou S, Keefer L. Snapshot of an integrated psychosocial gastroenterology service. World J Gastroenterol. 2015;21:1893–9. doi: 10.3748/wjg.v21.i6.1893. [DOI] [PMC free article] [PubMed] [Google Scholar]