Abstract
Leukemia is one of the most common cancers. We conducted this study to comprehensively analyze the temporal trends of leukemia mortality during 2003–2017 and project the trends until 2030. We extracted national-level data on annual leukemia mortality from China Health Statistics Yearbooks (2003–2017). We applied the Joinpoint regression model to assess leukemia mortality trends in urban and rural China by sex during 2003–2017. We also produced sex-specific leukemia mortality using the adjusted Global Burden Disease (GBD) 2016 projection model. In urban areas, age-standardized leukemia mortality decreased significantly among females during 2003–2017 (APC = −0.9%; 95% CI: −1.7, −0.1%). In rural areas, significant decreases of age-standardized leukemia mortality were both found among males (APC = −1.7%; 95% CI: −2.9, −0.5%) and females (APC = −1.6%; 95% CI: −2.6, −0.7%) from 2008 to 2017. Rural-urban and sex disparities of leukemia mortality will continue to exist until the year 2030. According to projection, the leukemia mortality rates of males and rural populations are higher than that of females and urban populations. In 2030, leukemia mortality is projected to decrease to 3.03/100,000 and 3.33/100,000 among the males in urban and rural areas, respectively. In females, leukemia mortality will decrease to 1.87/100,000 and 2.26/100,000 among urban and rural areas, respectively. Our study suggests that more precautionary measures to reduce leukemia mortality are need, and more attention should be paid to rural residents and males in primary prevention of leukemia in China.
Keywords: leukemia, mortality, joinpoint analysis, projection, SDGs
Introduction
Leukemia, also known as leukemia, is a group of blood cancers that start in blood-forming tissues and result in large numbers of abnormal blood cells in the bloodstream. The main types of leukemia include acute myeloid leukemia, acute lymphoblastic leukemia, chronic lymphocytic leukemia, chronic myelogenous leukemia, and hairy cell leukemia (1, 2). Leukemia ranks as the tenth most common cause of death from cancer worldwide with an estimated 309,006 deaths in 2018 (3). According to the Global Burden Disease (GBD) 2017 report, an estimated 141,317 new cases and 60,010 deaths of leukemia occurred in 2017 in China, accounting for 27.3% of 518,485 new cases and 17.3% of 347,583 deaths worldwide, respectively (4–6).
In the socioeconomic context of economic growth and urbanization, China has long been characterized by large rural-urban disparities in health care. Leukemia is closely related to ionizing radiation, benzene, formaldehyde, pesticides and infectious agents (7), and rural residents are more likely to expose to these risk factors, which could lead to the rise of leukemia mortality in rural areas and the enlarging rural-urban disparities for leukemia mortality. Besides, sex disparities are also observed in leukemia mortality. More men than women are diagnosed with leukemia and die from the disease. About 30% more men have developed leukemia than women (8). Thus, it is necessary to examine the trends of leukemia mortality by sex and area in China to provide positive implications for policy-makers in their attempt to reduce health inequities related to leukemia.
Literature analyzing the mortality trends of leukemia in China is scarce. Although previous studies have reported leukemia mortality trends in China, they either covered a small proportion of the Chinese population in some certain cities such as Tianjin (9) and Kunshan (10), or no updated data were provided (11). Large-scale nationwide epidemiological study of leukemia mortality trends with the latest data in China is needed. Therefore, we comprehensively examined the temporal trends of leukemia mortality during 2003–2017 and project the trends until the year 2030 using the most valid and updated data available in China. In addition, we examined rural-urban and sex disparities in leukemia mortality. Key findings reported in this paper will be critically important for policy-makers in China to develop appropriate and effective prevention and treatment of leukemia, which will further contribute to achieving “leaving no one behind” (a key SDGs pledge) (12).
Materials and Methods
Data Source
We extracted age-specific crude mortality rates of leukemia by year from China Health Statistics Yearbooks (2003–2017), which cover disease-specific mortality stratified by age and sex in urban and rural populations. The age-standardized mortality rates were calculated by way of the world standard population, and age-specific rates were calculated for age groups of 0–14, 15–34, 35–54, 55–74, and ≥75-years, respectively. According to the China Health Statistics Yearbooks, the urban areas include municipalities under the direct administration of central government and prefecture-level cities. The rural areas include counties and county-level cities, and township health centers and village clinics are included as well. China Health Statistics Yearbooks are annual informative publications that reflect the development of health care and residents' health status in China. The data are collected by the Center for Health Information and Statistics (CHIS) of China through national routine death reporting system and have been recognized as representative of common cancers in China (13, 14). The data from China Health Statistics Yearbooks is of high quality. Compared with data from China Health Statistics Yearbooks, the quality of cancer registry data in China needs to be improved. At present, the number of cancer registries in China is insufficient, and the coverage of the population is not wide (15).
Joinpoint Regression Analysis
We applied the Joinpoint regression model to analyze the leukemia mortality trends during 2003–2017 in urban populations and rural populations by sex, respectively. Several straight-line segments were connected at the Joinpoints, where the slope of leukemia mortality trend significantly changed. We assessed the annual percent changes (APCs) and the average annual percent changes (AAPCs) in leukemia mortality to describe the temporal trends. Joinpoint Regression Program 4.8.0.1(https://surveillance.cancer.gov/joinpoint/) was downloaded from the website of the US National Cancer Institute. The software takes trend data (e.g., cancer mortality rates) and fits the simplest joinpoint model that the data allow. The user supplies the minimum and maximum number of joinpoints. The program starts with the minimum number of joinpoint (e.g., 0 joinpoints, which is a straight line) and tests whether more joinpoints are statistically significant and must be added to the model (up to two points). This enables the user to test that an apparent change in trend is statistically significant. The tests of significance use a Monte Carlo Permutation method. The models may incorporate estimated variation for each point or use a Poisson model of variation. In addition, the models may also be linear on the log of the response (e.g., for calculating annual percentage rate change). The software also allows viewing one graph for each joinpoint model, from the model with the minimum number of joinpoints to the model with maximum number of joinpoints and the user could choose to present the software recommended model (16). All tests were 2-sided and the statistical significance was set at p < 0.05.
Projection of Leukemia Mortality
We explored adjusted GBD method to project leukemia mortality. The GBD methodology considers the historical trend and weights more on recent changes, and was designed to use different methods to produce reasonable outcomes according to different types of data, which shows comparative reliability in projecting results. For instance, it will not produce a percentage below 0 or above 100% (17). We further adjusted the GBD methods (details below) and a calculation tool was designed to do the projections.
The adjusted GBD methods following the original GBD methodology to first convert data into logit-space (for percentage data) or natural-log space (for other data) and calculate the annual rate of change. Afterwards, a time-based weight matrix is established to add more weight to rate of change in recent years. The weight of rate of change in year t is:
| (1) |
Where T is the last year with available data. The parameter ω was determined with a validity test: we selected the ω that used the first half of available data to predict the second half most accurately.
Results
Joinpoint Regression Analysis
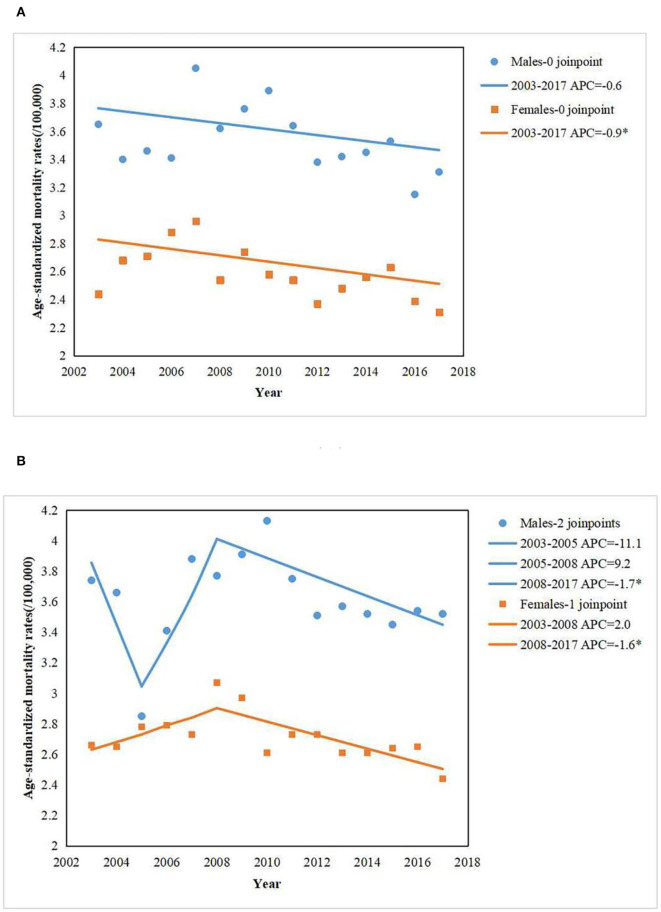
Figure 1A showed the trends of age-standardized leukemia mortality rates in urban areas, by sex from 2003 to 2017. In males, there was a non-significant decrease in age-standardized leukemia mortality rates from 2003 to 2017 (APC = −0.6%; 95% CI: −1.4, 0.2%). In females, a statistically significant decrease was presented from 2003 to 2017 (APC = −0.9%, 95% CI: −1.7, −0.1%). Figure 1B showed the trends of age-standardized leukemia mortality rates in rural areas, by sex from 2003 to 2017. In males, a statistically significant decrease was presented from 2008 to 2017 (APC = −1.7%; 95% CI: −2.9, −0.5%). In females, these was a non-significant increase in age-standardized leukemia mortality rates from 2003 to 2008 (APC = 2.0%; 95% CI: −0.4, 4.4%), followed by a statistically significant decrease from 2008 to 2017 (APC = −1.6%; 95% CI: −2.6, −0.7%). Sex disparities were substantial for leukemia mortality among urban and rural areas. Higher leukemia mortality rates were observed among men than among women during 2003–2017 (Figures 1A,B).
Figure 1.
Age-standardized leukemia mortality (/100,000) in Chinese populations among urban (A) and rural areas (B) from 2003 to 2017. The scattered data points represent the leukemia mortality. The trend lines were estimate d by modeling leukemia mortality from Joinpoint analysis.
Table 1 presented the APCs and AAPCs of age-specific leukemia mortality (2003–2017). During 2003–2017, a significant decrease of age-specific leukemia mortality rates was presented in urban populations aged 15–34 years. However, an upward trend of age-specific leukemia mortality was presented in rural populations aged over 75 years during 2003–2009. In addition, leukemia mortality has a statistically significant increase in rural males aged 55–74 years during 2003–2017.
Table 1.
Joinpoint regression analysis of age-specific and age-standardized leukemia mortality rates by sex and area during 2003–2017.
| Age | Urban areas | Rural areas | ||||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | |||||
| Period | APC (95% CI) | Period | APC (95% CI) | Period | APC (95% CI) | Period | APC (95% CI) | |
| 0–14 | 2003–2017 | −0.9 (−2.8, 0.9) | 2003–2017 | −0.8 (−2.4, 0.9) | 2003–2017 | −2.3 (−4.5, −0.1)* | 2003–2017 | −1.0 (−2.4, 0.5) |
| 15–34 | 2003–2017 | −1.5 (−2.7, −0.4) * | 2003–2017 | −1.8 (−3.4, −0.1)* | 2003–2017 | −0.6 (−2.1, 0.9) | 2003–2017 | −2.1 (−3.6, −0.5)* |
| 35–54 | 2003–2017 | −2.9 (−3.9, −1.8) * | 2003–2005 | 16.1 (4.6, 29.0)* | 2003–2017 | −0.8 (−2.5, 0.8) | 2003–2017 | −2.0 (−3.8, −0.2)* |
| 2005–2017 | −3.9 (−4.5, −3.3)* | |||||||
| AAPC | −1.3 (−2.6,0.1) | |||||||
| 55–74 | 2003–2017 | 0.6 (−0.8, 2.0) | 2003–2017 | −0.0 (−1.3, 1.3) | 2003–2017 | 2.0 (0.3, 3.7)* | 2003–2017 | 1.5 (−0.1, 3.1) |
| ≥75 | 2003–2017 | 1.7 (−0.8, 4.3) | 2003–2017 | 1.1 (−1.3, 3.5) | 2003–2009 | 8.0 (3.6, 12.6)* | 2003–2009 | 15.1 (6.7, 24.2)* |
| 2009–2017 | −0.3 (−3.0, 2.4) | 2009–2017 | −3.3 (−8.0, 1.5) | |||||
| AAPC | 3.2 (1.1, 5.3)* | AAPC | 4.2 (0.3, 8.2)* | |||||
| Age standardized Overall | 2003–2017 | −0.6 (−1.4, 0.2) | 2003–2017 | −0.9 (−1.7, −0.1)* | 2003–2005 | −11.1 (−22.2, 1.4) | 2003–2008 | 2.0 (−0.4, 4.4) |
| 2005–2008 | 9.2 (−4.3, 24.7) | 2008–2017 | −1.6 (−2.6, −0.7)* | |||||
| 2008–2017 | −1.7 (−2.9, −0.5)* | AAPC | −0.4 (−1.3, 0.6) | |||||
| AAPC | −0.9 (−3.7, 2.0) | |||||||
AAPC (average annual percent change) presented for full period.
APC, annual percent change; CI, confidence interval.
Statistically significant trend (p < 0.05).
Projection of Leukemia Mortality
Sex and rural-urban disparities will still exist in leukemia mortality until the year 2030. Based on the projections of the leukemia mortality, it is estimated that among the males and females, leukemia mortality will decrease in both urban and rural areas (Figures 2A,B). In 2030, leukemia mortality is projected to drop to 3.03/100,000 in urban areas and 3.33/100,000 in rural areas among the males (Table 2). Among the females, leukemia mortality will continue to decrease in both urban and rural areas (Figures 2A,B), which will decrease to 1.87/100,000 and 2.26/100,000 among urban and rural areas in 2030, respectively (Table 2). It is also projected that the male population will continue to have higher leukemia mortality rates than the female population in both urban and rural areas (Figures 2A,B).
Figure 2.
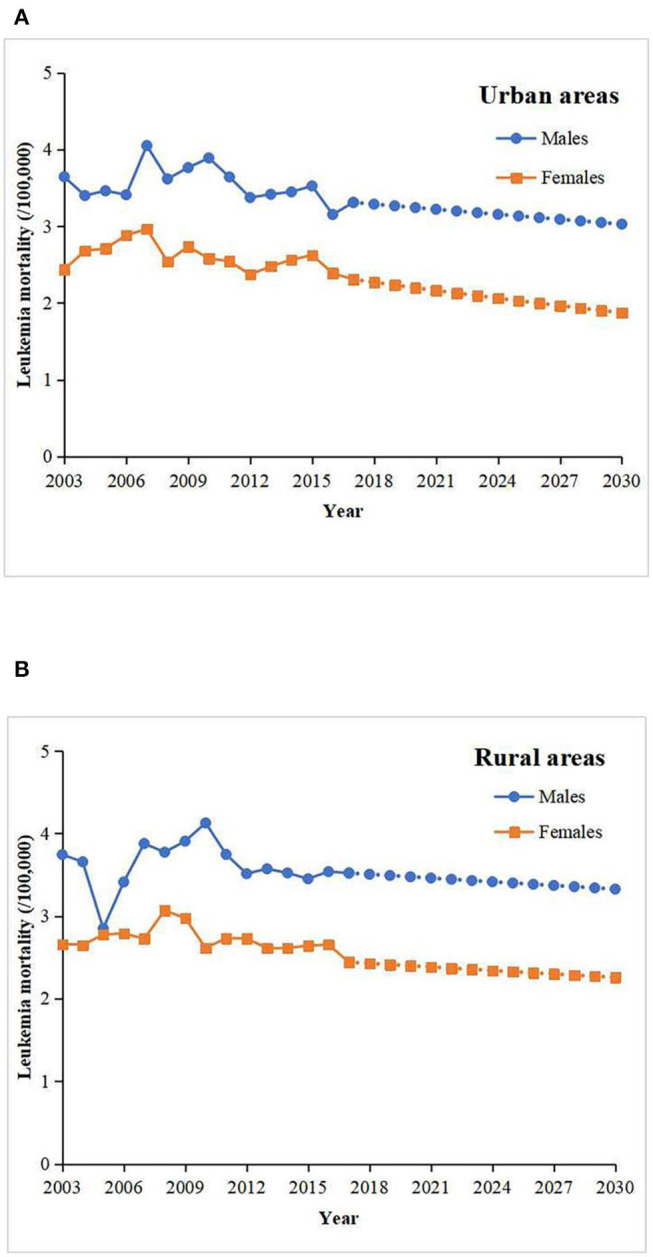
The projected leukemia mortality (/100,000) in the males and females among urban (A) and rural areas (B) from 2017 to 2030.
Table 2.
Predicted number of leukemia mortality (/100,000) in males and females among urban and rural areas in 2020, 2025, and 2030.
| Population | Leukemia mortality (/100,000) | ||
|---|---|---|---|
| 2020 | 2025 | 2030 | |
| Males | |||
| Urban areas | 3.24 | 3.13 | 3.03 |
| Rural areas | 3.47 | 3.40 | 3.33 |
| Females | |||
| Urban areas | 2.20 | 2.03 | 1.87 |
| Rural areas | 2.40 | 2.33 | 2.26 |
Discussion
This study is an updated systematic analysis and projection of nationwide leukemia mortality rates in urban and rural China by using the latest representative data. From 2008 to 2017, leukemia mortality decreased among the males and females in urban and rural areas. In rural areas, leukemia mortality significantly decreased by 1.7 and 1.6% among the males and females, respectively, from 2008 to 2017. In urban areas, leukemia mortality significantly decreased by 0.9% in the females during 2003–2017. Rural-urban disparities and sex disparities were substantial for leukemia mortality, which will still exist until 2030. In 2030, leukemia mortality is projected to drop to 3.03/100,000 in urban areas and 3.33/100,000 in rural areas among the males. Among the females, leukemia mortality will decrease to 1.87/100,000 and 2.26/100,000 among urban and rural areas in 2030, respectively.
The findings on leukemia mortality trends are consistent with a previous study (9) in Tianjin, China from 1999 to 2015, which reported that the age-adjusted leukemia mortality among urban residents showed a decreasing trend with the APC of −1.12% (p = 0.026). Besides, significant drops in the mortality of adult patients diagnosed with myeloid leukemia were observed from 1994 to 2001 with the APC of −21.22% and from 1994 to 2003 with the APC of −12.86% for males and females, respectively, in southeastern Brazil (18). Mortality from leukemia steadily declined in the European Union with the APC of −3.7% in males and −3.8% in females at age 0–14, −2% in both sexes at age 15–44, and −0.6% in males and −1% in females at middle-age and overall from 1970 to 2009 (19). In Croatia, mortality rates were stable for myeloid leukemia in both sexes during 1988–2009 (20). These differences in trends were attributable to data source, research period, population composition, different types of leukemia involved in research, and different socioeconomic statuses of different countries.
Rural-urban disparities and sex disparities were substantial for leukemia mortality. An investigation in Gansu province of China found that the leukemia mortality in rural areas was 5.07 times higher than urban areas, with the mortality rates of 4.57/100,000 in rural areas and 0.90/100,000 in urban areas, respectively (21). A study conducted in the USA showed that the age-adjusted mortality rates per 100,000 population was 7.90 for metropolitan and 8.25 for nonmetropolitan areas during 1990–1992, and was 7.01 for metropolitan and 7.47 for nonmetropolitan areas during 2005–2009, respectively. This presented widening rural-urban disparities in leukemia mortality in the USA over time, which was contributed by the larger mortality reductions in metropolitan residents than non-metropolitan residents (22). Besides, another study in the USA depicted the estimated leukemia deaths by sex in 2019, which was 13,150 in men and 9,690 in women, respectively (23). A study in the European Union reported the age-standardized mortality rates of leukemia was 4.57/100,000 in males and 2.78/100,000 in females in 2011 (24). A study in Korea showed the crude leukemia mortality rates was 3.9 in men and 2.8 in women per 100,000 people in 2015 (25). All above studies suggested rural-urban and/or sex disparities existed in leukemia mortality in either high-income countries or low and middle-income countries.
There are several risk factors related to leukemia incidence, especially in rural male residents, and reductions in incidence can largely contribute to reductions in mortality. Ionizing radiation can be closely linked to the increase of leukemia mortality (26, 27). Several systematic reviews have presented a significant correlation between exposure to benzene and the incidence of acute myeloid leukemia (28, 29). Benzene is widely used as a solvent in industrial processes such as production of chemicals and plastics as well as oil processing. Tobacco smoke was also identified as one of the main potential sources of benzene exposure (30, 31). Use of tobacco is associated with a small increase in the risk of developing acute myeloid leukemia in adults (32). In addition, a statistically significant excess risk of leukemia has been observed among those occupationally exposed to formaldehyde in a meta-analysis (33). Besides, a few studies have recorded statistically significant excess risk of leukemia among agricultural workers exposed to pesticides (34–36). Moreover, there is an association of the increase of leukemia risk with exposure to infectious agents, which could be highly exposed to specific populations working on agriculture, animal husbandry and food processing (37–39). Rural residents, especially men, earn a living in farms and factories, where they may get exposed to ionizing radiation, benzene, formaldehyde, pesticides and/or infectious agents, and male population accounts for a large proportion of tobacco consumption. On the other hand, the improvement of early diagnosis technology for leukemia has provided effective help for the early detection of leukemia patients, which may lead to a decline in leukemia mortality to a certain extent. Chen et al. conducted a metabolomics study on the serum of new-onset Acute Myeloid Leukemia patients and healthy volunteers and found that six significantly different metabolites can be used for early diagnosis and prognostic analysis of Acute Myeloid Leukemia (40). Wang et al. found that the small molecule metabolites detected by the metabolomics method based on hydrogen spectrum nuclear magnetic resonance (1H-NMR) can be used for the early diagnosis of leukemia and the judgment of the severity of leukemia (41). In China, progress in the treatment of leukemia also contributed to the decline in leukemia mortality. Wang et al. systematically reviewed the new developments in clinical treatment of leukemia in China (42). In addition to conventional surgical treatment, the use of treatments with Chinese characteristics have also significantly improved the survival rate of leukemia patients. A meta-analysis of Chinese studies showed that the treatment of Acute Myeloid Leukemia with Homoharringtonine has a higher total complete response (CR) rate (43). Furthermore, new successful therapies will first be introduced in university hospitals or research institutes in urban areas and it will take some time until they are also applied in more peripheral hospitals in rural areas. So, their effect on mortality rates will take some time causing downward trends in rural areas. Consequently, the rural-urban disparities and sex disparities for leukemia mortality become substantial.
Rural-urban disparities and sex disparities will still exist in leukemia mortality until the year 2030. According to projection, the leukemia mortality rates of males and rural populations are higher than that of females and urban populations. In general, primary prevention is of particular relevance for cancer, where reductions in mortality are largely achieved through reductions in incidence (44). Thus, precautionary measures through health promotion and education are of paramount importance (45, 46). Primary prevention of leukemia can be accomplished in two ways: (i) avoiding or reducing the introduction of carcinogenic agents into the environment. For example, there is an urgent need to focus on health policies and systems, including pricing of tobacco (47), setting permissible exposure limits of ionizing radiation, benzene and formaldehyde in the workplace. What is more important is to earnestly ensure the implementation of the relevant policies and constantly improve the health systems (48). (ii) eliminating or reducing the exposure to carcinogenic agents that are already in our environment. Health education of high-risk individuals and populations, particularly in the early stages, should be taken into consideration. For instance, pesticides safety education and pesticide applicator regulation should be well designed to protect the public from pesticide misuse. In the long-run, accelerating economic growth in rural areas and improving living standards of rural residents could reduce their exposure to the risk factors, which is the fundamental solution to reduce rural-urban disparities in leukemia mortality. In the future, more attention should be paid to epidemiological evidence that is suggestive of an exposure-leukemia association, and experimental evidence of carcinogenicity supported by mechanistic considerations (44). Follow-up studies designed to determine whether leukemia mortality rates declined as the result of preventive measures (“before-after” effect) are in need.
There are several limitations in this study. First, leukemia is one of the most common cancers (49), and there are five main types of leukemia (2). Thus, further epidemiological studies of leukemia focusing on only one type of leukemia are needed. Second, the projection methodology, though carefully selected through comprehensive comparisons, can only reflect future changes based on historical trajectories. It fails to capture other possible changes such as stronger political commitment, new and effective technology advances and interventions, and does not consider the possibility of a ceiling effect. Moreover, we only roughly projected the leukemia mortality trends on the basis of past trends and do not model demographic, socioeconomic and other related factors into the model. Therefore, our results in the present study on temporal trends and projections of leukemia should be treated carefully.
Conclusions
From 2008 to 2017, leukemia mortality decreased among the males and females in urban and rural areas. Rural-urban disparities and sex disparities were substantial for leukemia mortality, which will still exist until 2030. Precautionary measures should be taken, especially for rural residents and males. Studies focusing on epidemiological evidence, experimental evidence and “before-after” effect are needed to further explore the risk factors and prevention measures of leukemia.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: http://www.cnki.net/.
Author Contributions
HX: conceptualization, funding acquisition, project administration, writing—review, and editing. ZC and YZ: data curation and visualization. BL and HT: formal analysis, investigation, methodology, resources, software, validation, and writing—original draft. YZ and HX: supervision. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We acknowledge Bill and Melinda Gates Foundation for supporting this work, and appreciate Duke Global Health Institute and partnership of several Chinese universities and organizations.
Footnotes
Funding. This research was funded by Bill & Melinda Gates Foundation (Grant No. OOP1148464) and Natural Science Fund of Hubei Province (Grant No. 2018CFB634).
References
- 1.McGuire S. World cancer report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv Nutr. (2016) 7:418–9. 10.3945/an.116.012211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Cancer Institute Leukemia Patient Version. Available online at: https://www.cancer.gov/types/leukemia (accessed September 10, 2020).
- 3.International Agency for Research on Cancer Cancer Today (powered by GLOBOCAN 2018). Available online at: http://gco.iarc.fr/ (accessed September 10, 2020).
- 4.Collaborators GDaIIaP. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collaborators GCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GHDx GBD Results Tool. Available online at: http://ghdx.healthdata.org/gbd-results-tool (accessed September 10, 2020).
- 7.Polychronakis I, Dounias G, Makropoulos V, Riza E, Linos A. Work-related leukemia: a systematic review. J Occup Med Toxicol. (2013) 8:14. 10.1186/1745-6673-8-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson N, Menon BS, Zarina W, Zawawi N, Naing NN. Why is acute leukemia more common in males? A possible sex-determined risk linked to the ABO blood group genes. Ann Hematol. (1999) 78:233–6. 10.1007/s002770050507 [DOI] [PubMed] [Google Scholar]
- 9.Wang DZ, Zhang S, Zhang H. Analysis on trend of leukemia mortality from 1999 to 2015 in Tianjin, China. Chin J Prev Med. (2019) 53:319–22. 10.1097/CM9.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 10.Zhang T, Qin W, Hu WB. Trends of leukemia mortality in Kunshan City, Jiangsu Province from 1993 to 2014. Cancer Res Prev Treat. (2016) 43:1072–5. 10.3971/j.issn.1000-8578.2016.12.013 [DOI] [Google Scholar]
- 11.Chen WQ, Shan BE, Zheng RS. Analysis of incidence and mortality of leukemia in registration areas of China from 2003 to 2007. Tumor. (2012) 32:251–5. 10.3781/j.issn.1109-0721.2012.04.005 [DOI] [Google Scholar]
- 12.Watkins K. Leaving no one behind: an agenda for equity. Lancet. (2014) 384:2248–55. 10.1016/S0140-6736(13)62421-6 [DOI] [PubMed] [Google Scholar]
- 13.China Health Statistics Yearbook Statistical Database of China's Economic and Social Development. Available online at: https://tongji.oversea.cnki.net/chn/navi/HomePage.aspx?id=N2019030282&name=YSIFE&floor=1 (accessed November 30, 2020).
- 14.Gao K, Wu J. National trend of gastric cancer mortality in China (2003-2015): a population-based study. Cancer Commun. (2019) 39:24. 10.1186/s40880-019-0372-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen WQ, Liang ZH, Cen HS, Wei KR. Current status and development of cancer registration in China. Chin J Med Front. (2016) 8:1–6. 10.3969/j.issn.1674-7372.2016.07.001 [DOI] [Google Scholar]
- 16.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. (2000) 19:335–51. [DOI] [PubMed] [Google Scholar]
- 17.Collaborators GS. Measuring progress and projecting attainment on the basis of past trends of the health-related sustainable development goals in 188 countries: an analysis from the global burden of disease study 2016. Lancet. (2017) 390:1423–59. 10.1016/S0140-6736(17)32336-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callera F, Callera AF, Rosa ES. Trends in mortality of adult patients diagnosed with myeloid leukemia from 1994 to 2011 in southeastern Brazil. Rev Bras Hematol Hemoter. (2015) 37:7–11. 10.1016/j.bjhh.2014.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bertuccio P, Bosetti C, Malvezzi M, Levi F, Chatenoud L, Negri E, et al. Trends in mortality from leukemia in Europe: an update to 2009 and a projection to 2012. Int J Cancer. (2013) 132:427–36. 10.1002/ijc.27624 [DOI] [PubMed] [Google Scholar]
- 20.Novak I, Jaksić O, Kulis T, Batinjan K, Znaor A. Incidence and mortality trends of leukemia and lymphoma in Croatia, 1988-2009. Croat Med J. (2012) 53:115–23. 10.3325/cmj.2012.53.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Si YX, Qian H, Liu YQ. An analysis of the incidence and mortality of leukemia in Gansu, 2010. China Cancer. (2015) 2:81–8. 10.11735/j.issn.1004-0242.2015.02.A001 [DOI] [Google Scholar]
- 22.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. J Urban Health. (2014) 91:272–92. 10.1007/s11524-013-9847-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. (2019) 69:7–34. 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- 24.Malvezzi M, Carioli G, Bertuccio P, Rosso T, Boffetta P, Levi F, et al. European cancer mortality predictions for the year 2016 with focus on leukaemias. Ann Oncol. (2016) 27:725–31. 10.1093/annonc/mdw022 [DOI] [PubMed] [Google Scholar]
- 25.Jung KW, Won YJ, Kong HJ, Lee ES, Registries CoP-BRC. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. (2018) 50:303–16. 10.4143/crt.2018.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson D, Sugiyama H, Nishi N, Sakata R, Shimizu Y, Grant EJ, et al. Ionizing radiation and leukemia mortality among Japanese Atomic Bomb Survivors, 1950-2000. Radiat Res. (2009) 172:368–82. 10.1667/RR1801.1 [DOI] [PubMed] [Google Scholar]
- 27.Noshchenko AG, Zamostyan PV, Bondar OY, Drozdova VD. Radiation-induced leukemia risk among those aged 0-20 at the time of the Chernobyl accident: a case-control study in the Ukraine. Int J Cancer. (2002) 99:609–18. 10.1002/ijc.10406 [DOI] [PubMed] [Google Scholar]
- 28.Khalade A, Jaakkola MS, Pukkala E, Jaakkola JJ. Exposure to benzene at work and the risk of leukemia: a systematic review and meta-analysis. Environ Health. (2010) 9:31. 10.1186/1476-069X-9-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lamm SH, Engel A, Joshi KP, Byrd DM, Chen R. Chronic myelogenous leukemia and benzene exposure: a systematic review and meta-analysis of the case-control literature. Chem Biol Interact. (2009) 182:93–7. 10.1016/j.cbi.2009.08.010 [DOI] [PubMed] [Google Scholar]
- 30.Fiebelkorn S, Meredith C. Estimation of the leukemia risk in human populations exposed to benzene from tobacco smoke using epidemiological data. Risk Anal. (2018) 38:1490–501. 10.1111/risa.12956 [DOI] [PubMed] [Google Scholar]
- 31.Burns DM, Dybing E, Gray N, Hecht S, Anderson C, Sanner T, et al. Mandated lowering of toxicants in cigarette smoke: a description of the World Health Organization TobReg proposal. Tob Control. (2008) 17:132–41. 10.1136/tc.2007.024158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiernik PH. Adult Leukemias. Hamilton, London: BC Decker Inc; (2001). p. 3–15. [Google Scholar]
- 33.Schwilk E, Zhang L, Smith MT, Smith AH, Steinmaus C. Formaldehyde and leukemia: an updated meta-analysis and evaluation of bias. J Occup Environ Med. (2010) 52:878–86. 10.1097/JOM.0b013e3181ef7e31 [DOI] [PubMed] [Google Scholar]
- 34.Chrisman JeR, Koifman S, de Novaes Sarcinelli P, Moreira JC, Koifman RJ, Meyer A. Pesticide sales and adult male cancer mortality in Brazil. Int J Hyg Environ Health. (2009) 212:310–21. 10.1016/j.ijheh.2008.07.006 [DOI] [PubMed] [Google Scholar]
- 35.Orsi L, Delabre L, Monnereau A, Delval P, Berthou C, Fenaux P, et al. Occupational exposure to pesticides and lymphoid neoplasms among men: results of a French case-control study. Occup Environ Med. (2009) 66:291–8. 10.1136/oem.2008.040972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rusiecki JA, Patel R, Koutros S, Beane-Freeman L, Landgren O, Bonner MR, et al. Cancer incidence among pesticide applicators exposed to permethrin in the agricultural health study. Environ Health Perspect. (2009) 117:581–6. 10.1289/ehp.11318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wong O, Harris F, Armstrong TW, Hua F. A hospital-based case-control study of acute myeloid leukemia in Shanghai: analysis of environmental and occupational risk factors by subtypes of the WHO classification. Chem Biol Interact. (2010) 184:112–28. 10.1016/j.cbi.2009.10.017 [DOI] [PubMed] [Google Scholar]
- 38.Johnson ES, Ndetan H, Lo KM. Cancer mortality in poultry slaughtering/processing plant workers belonging to a union pension fund. Environ Res. (2010) 110:588–94. 10.1016/j.envres.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 39.Johnson ES, Zhou Y, Lillian Yau C, Prabhakar D, Ndetan H, Singh K, et al. Mortality from malignant diseases-update of the Baltimore union poultry cohort. Cancer Causes Control. (2010) 21:215–21. 10.1007/s10552-009-9452-6 [DOI] [PubMed] [Google Scholar]
- 40.Chen WL, Wang JH, Zhao AH, Xu X, Wang YH, Chen TL, et al. A distinct glucose metabolism signature of acute myeloid leukemia with prognostic value. Blood. (2014) 124:1645–54. 10.1182/blood-2014-02-554204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang YH, Zhang LM, Chen WL, Wang JH, Li N, Li JM, et al. Rapid diagnosis and prognosis of de novo acute myeloid leukemia by serum metabonomic analysis. J Proteome Res. (2013) 12:4393–401. 10.1021/pr400403p [DOI] [PubMed] [Google Scholar]
- 42.Wang Y, Wei H. Progress of the diagnosis and treatment of acute leukemia in China: work review of Institute of Hematology & Blood Disease Hospital, Chinese Academy of Medical Science. J Leuk Lymphoma. (2019) 28:611–4. 10.3760/cma.j.issn.1009-9921.2019.10.007 [DOI] [Google Scholar]
- 43.Kantarjian H, O'Brien S, Jabbour E, Barnes G, Pathak A, Cortes J. Effectiveness of homoharringtonine (omacetaxine mepesuccinate) for treatment of acute myeloid leukemia: a meta-analysis of Chinese studies. Clin Lymphoma Myeloma Leuk. (2015) 15:13–21. 10.1016/j.clml.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 44.Tomatis L, Huff J, Hertz-Picciotto I, Sandler DP, Bucher J, et al. Avoided and avoidable risks of cancer. Carcinogenesis. (1997) 18:97–105. 10.1093/carcin/18.1.97 [DOI] [PubMed] [Google Scholar]
- 45.Carneiro-Proietti AB, Catalan-Soares BC, Castro-Costa CM, Murphy EL, Sabino EC, Hisada M, et al. HTLV in the Americas: challenges and perspectives. Rev Panam Salud Publica. (2006) 19:44–53. 10.1590/S1020-49892006000100007 [DOI] [PubMed] [Google Scholar]
- 46.Atun R, Jaffar S, Nishtar S, Knaul FM, Barreto ML, Nyirenda M, et al. Improving responsiveness of health systems to non-communicable diseases. Lancet. (2013) 381:690–7. 10.1016/S0140-6736(13)60063-X [DOI] [PubMed] [Google Scholar]
- 47.Driezen P, Abdullah AS, Quah ACK, Nargis N, Fong GT. Determinants of intentions to quit smoking among adult smokers in Bangladesh: findings from the International Tobacco Control (ITC) Bangladesh wave 2 survey. Glob Health Res Policy. (2016) 1:11. 10.1186/s41256-016-0012-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Witter S, Chirwa Y, Chandiwana P, Munyati S, Pepukai M, Bertone MP. The political economy of results-based financing: the experience of the health system in Zimbabwe. Glob Health Res Policy. (2019) 4:20. 10.1186/s41256-019-0111-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mohseni M, Uludag H, Brandwein JM. Advances in biology of acute lymphoblastic leukemia (ALL) and therapeutic implications. Am J Blood Res. (2018) 8:29–56. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: http://www.cnki.net/.