Abstract
Hepatocellular carcinoma (HCC) is a leading cause of cancer-associated mortality globally. Given the limited therapeutic efficacy in advanced HCC, prevention of HCC carcinogenesis could serve as an effective strategy. Patients with chronic fibrosis due to viral or metabolic etiologies are at a high risk of developing HCC. Primary prevention seeks to eliminate cancer predisposing risk factors while tertiary prevention aims to prevent HCC recurrence. Secondary prevention targets patients with baseline chronic liver disease. Various epidemiological and experimental studies have identified candidates for secondary prevention—both etiology-specific and generic prevention strategies—including statins, aspirin, and anti-diabetic drugs. The introduction of multi-cell based omics analysis along with better characterization of the hepatic microenvironment will further facilitate the identification of targets for prevention. In this review, we will summarize HCC risk factors, pathogenesis, and discuss strategies of HCC prevention. We will focus on secondary prevention and also discuss current challenges in translating experimental work into clinical practice.
Keywords: hepatocellular carcinoma, hepatitis, NASH, chemoprevention
1. Introduction
Hepatocellular carcinoma (HCC) is the fifth most common malignancy and the fourth leading cause of cancer-associated mortality worldwide [1,2]. In 2015, there were 854,000 cases of HCC globally, with a male-to-female ratio of 2.4:1 [3]. Sub-Saharan Africa and East Asia have the highest incidence rate of HCC (more than 20 per 100,000 individuals), while North America and Europe have lower incidence levels (less than 5 per 100,000 individuals) [4,5,6]. Between 1996 and 2006, the HCC incidence rate in the US surveillance, epidemiology and end results (SEER) registries increased from 3.1 to 5.1 per 100,000 individuals, while the US liver cancer mortality rose from 3.3 to 4.0 per 100,000 individuals [7]. From 2006 to 2017, the rate of HCC has increased by 2–3% annually, largely due to the high prevalence of hepatitis C virus (HCV) cirrhosis and nonalcoholic steatohepatitis (NASH) [8,9].
Early HCC diagnosis occurs in 30–60% of cases, enabling curative treatments such as surgical resection and liver transplantation. Even with curative approaches, HCC recurrence is observed in up to 80% of patients within 5 years [10]. In advanced disease, surgical and systemic therapies have largely failed to yield survival benefits [11]. Until recently, Sorafenib was the only FDA-approved agent for advanced HCC. Since 2017, other multi-kinase inhibitors have been approved for second-line treatments, such as Cabozantinib and Ramucirumab [12,13,14]. Checkpoint inhibitors such as Nivolumab [15] and Pembrolizumab [16] have been either FDA approved or under investigation. Importantly, systemic therapies have substantial adverse effects that are difficult to manage in cirrhotic patients [17]. Finally, the high costs of approved therapies limit their use in low-resource countries [18]. Given the potential to identify high risk individuals and low survival rate once diagnosed, HCC prevention in at-risk patients can be a successful and alternative approach for HCC management. Here, we will review HCC risk factors, pathogenesis and current strategies for prevention, specifically secondary prevention and its clinical challenges.
2. Risk Factors and Carcinogenesis
2.1. Hepatitis B Virus (HBV)
Globally, 2 billion people have been exposed to HBV along with 250–350 million chronic carriers [19]. In high endemic areas, the HBV carrier rate is nearly 8% [20]. In areas of high incidence, 80% of patients with HCC are seropositive for the hepatitis B surface antigen (HBsAg) [21]. In East Asia, the HCC incidence rate in chronic HBV carriers ranges from 0.6 per 100 individuals without cirrhosis to 3.7 per 100 individuals with compensated cirrhosis. In Europe and the United states, the incidence rate ranges from 0.3 per 100 individuals without cirrhosis to 2.2 per 100 individuals in subjects with cirrhosis [22,23]. In addition, 10–20% of patients with HBV can develop HCC in the absence of cirrhosis [24]. Other factors that have been reported to increase the risk of HCC include duration of infection, viral load, environmental exposures (aflatoxin, alcohol, or tobacco), demographic features such as male sex, older age, family history of HCC, and co-infections with HCV, HDV, and HIV [25,26].
Two major mechanisms of HBV-induced HCC carcinogenesis have been proposed. First, chronic HBV can induce cirrhosis through the activation of HBV-specific T-cells, chemokine-mediated neutrophils, macrophages, and natural-killers [27,28]. These inflammatory cells promote carcinogenesis by stimulating hepatocyte regeneration, reactive oxygen species (ROSs) production, and DNA damage. Second, HBV DNA can be integrated into the host genome, prompting insertional activation of proto-oncogenes [29], induction of chromosomal instability [30], and the transcription of pro-carcinogenic HBV genes such as truncated envelope proteins [31], hepatitis B X gene (HBx) [32], and hepatitis B spliced proteins [33].
2.2. Hepatitis C Virus (HCV)
HCC induced by HCV has the highest HCC mortality rates per 100,000 individuals in the United States [34,35]. Chronic HCV is most prevalent in the “baby boomer” generation, defined as adults born between 1945 and 1965 who were exposed to blood transfusions, clotting factors, and hemodialysis prior to 1992 [36]. Moreover, the current opioid epidemic further contributes to the spread of HCV [37]. Between 2010 and 2017, a three-fold increase in acute HCV infections was reported by the CDC resulting from the opioid epidemic [38]. The annual incidence of HCV related HCC in patients with cirrhosis is extremely high, ranging from 1 to 12% per year [39,40]. In a large cohort of US patients with HCV, patients with genotype 3 are more likely to develop cirrhosis and HCC than other HCV genotypes [41].
HCC development in HCV is primarily associated with fibrosis and the viral copy number [42]. HCV associated HCC development occurs in a stepwise fashion, typically spanning over decades. All cases of HCV HCC arise from mutations in hepatocytes within a cirrhotic background. HCV proteins have also been shown to promote cellular proliferation, transformation, and tumor growth. Over-expression of HCV core proteins, NS3 and NS5A, inhibit tumor suppressor genes TP53, TP73, and RB1, as well as negative cell cycle regulators such as CDKN1A. E2 and NS5B activate the RAF/mitogen-activated protein kinase (MAPK)/ERK kinase pathways [43]. NS5A activates the PI3K/AKT and beta-catenin/WNT pathways, and evades apoptosis by caspase-3 inhibition [44]. It is important to note that the interaction between nonstructural protein NS5A and HCV is dependent on Rab18-positive lipid droplets [45].
2.3. Nonalcoholic Fatty Liver Disease (NAFLD)/Nonalcoholic Steatohepatitis (NASH)
NAFLD/NASH has emerged as a leading cause of end-stage liver disease as well as HCC. Studies have demonstrated that the incidence of HCC in patients with NASH ranges from 2.4% over 7 years to 12.8% over 3 years [46]. Recent studies in the US have shown that NAFLD/NASH-related mortality has dramatically increased in the last 10 years together with NAFLD/NASH-related liver cirrhosis [47]. HCC in NAFLD/NASH is often diagnosed in patients without cirrhosis and is associated with late onset diagnosis and a higher tumor burden [48]. Moreover, patients with NASH receive sub-optimal HCC surveillance in comparison to patients with HCV cirrhosis [49].
The mechanism of HCC carcinogenesis as a result of NAFLD is not completely clear. Steatosis alone is not a driver of HCC as chronic inflammation is necessary for carcinogenesis [50]. Fat- tissue-derived free fatty acids (FFAs) lead to steatosis and lobular inflammation through the activation of intrahepatic lymphocytes and infiltrating macrophages. Hepatocyte cell death and compensatory proliferation together with increasing levels of tissue necrosis factor (TNF) superfamily members, transforming growth factor β (TGF-β), activation of hepatic stellate/liver sinusoidal endothelial cells, and hepatocyte chromosomal aberrations all contribute to HCC development [51]. The increased hepatocyte metabolism and oxidation of fatty acid induce overproduction of ROSs [52]. The excess of triglycerides and FFAs impair the initiation of autophagy through the activation of mammalian target of rapamycin (mTOR). When the antioxidant capacity of the hepatocytes is exceeded, DNA damage and oxidation occurs, eventually resulting in cell death [53,54].
It has also been suggested that the inflammatory responses seen in patients with NASH might be caused by an increase in gut permeability. Even though it is unclear whether a leaky gut is the consequence or the cause of NASH, it is evident that the translocation of lipopolysaccharide from gram-negative bacteria is an important aggravating factor for liver inflammation and fibrosis [55].
2.4. Lifestyle Risk Factors
Alcoholic liver disease (ALD) alters hepatic metabolism, causing progressive steatosis, fibrosis/cirrhosis, and HCC [56,57]. The risk of HCC increases with alcohol consumption as low as 10 g/day [58]. Perrsen et al. found that consuming more than three drinks daily was associated with an increase in HCC incidence and liver disease-related mortality [59]. There is a synergistic relationship between alcohol use of >60 g per day and viral hepatitis, with an approximately two-fold increase in the odds-ratio of developing HCC [60]. Alcohol use at least four times per week annually along with obesity (BMI > 30) increases the incidence of HCC [61]. Kimura et al. found that mild alcohol use (<20 g/day) in patients with NASH and advanced fibrosis was associated with a significant increase in the risk of HCC [62], while Ochiai et al. showed that ethanol intake ≥ 40 g was associated with a significant increase in multinodular HCCs [63].
The mechanism of ALD induced HCC is partially understood. Alcohol consumption can alter metabolic pathways including fatty acid oxidation and lipogenesis. Chronic alcohol consumption leads to an abnormal accumulation of acetaldehyde, which can exert carcinogenic effects through the formation of DNA-protein adduct [64]. Acetaldehyde has been shown in vitro to interfere with the transcriptional activities of peroxisome proliferator activated receptors (PPARs) and sterol regulatory element binding protein 1 (SREBP-1) [65,66]. Alcohol consumption can also reduce the level of 5′ AMP-activated protein kinase (AMPK), an important regulator of lipogenesis [67]. It is important to note that the severity of ALD is associated with genetic susceptibility. Genome-wide association studies (GWASs) have identified genetic risk loci for ALD, including PNPLA3 [68] and MBOAT7/TMC4 being related to a higher risk of cirrhosis in alcohol abusers [69].
Smoking is another important lifestyle risk factor for HCC. Tobacco smoking contributes to 13% of all HCC cases globally [70]. Current smokers have higher risks of HCC (hazard ratio 1.86, 95% CI: 1.57–2.20) [71], while those who quit for over 30 years have similar risks to non-smokers [72]. Tobacco contains multiple carcinogenic agents, including aromatic hydrocarbons [73], diethylnitrosamine (DEN) [74], and 4-aminobiphenyl [75]. Tobacco use is associated with an increase in inflammatory cytokines and ROS [76]. Tobacco also has been shown in rodent models to exacerbate the severity of NAFLD through the increasing of oxidative stress and hepatocellular apoptosis [77].
2.5. Environmental Carcinogens
A number of environmental chemicals have been implicated in HCC carcinogenesis. The best documented are aflatoxins. Other factors include vinyl chloride, arsenic compounds, polychlorinated biphenyls, and radioactive compounds [78]. Aflatoxins, mycotoxins produced by Aspergillus flavus and Aspergillus parasiticus, are frequently found in contaminated grain products such as maize and ground nuts in farming communities in sub-Saharan Africa, South America, and parts of Eastern Asia [79,80]. Aflatoxin B1 has been shown to form DNA adducts with hepatic DNA, leading to carcinogenesis in both humans and animal models [81]. In regions with high aflatoxin exposure, a 70-fold increase in the risk of HCC development has been observed [82].
2.6. Genetic Predisposition
Alpha 1-antitrypsin (AAT) deficiency is an autosomal recessive disease that results from mutations in the SERPINA1 gene. This gene encodes a serine protease inhibitor, which functions to inhibit neutrophil elastase. A retrospective study in Sweden found an odds ratio of 20 for the development of HCC in patients with AAT deficiency [83]. Glycogen storage disease I, or Von Gierke’s disease, leads to the impairment of glucose-6-phosphatase activity with excess glycogen storage in the liver [84]. Patients with glycogen storage disease I can develop hepatocellular adenomas by their second or third decade of life. A number of these patients go on to develop HCC [85]. The risk of HCC in patients with hemochromatosis is approximately 20 times higher than the general population [86]. Lastly, hereditary tyrosinemia type I is an autosomal recessive disease caused by an enzymatic deficiency in the catabolic pathway of tyrosine [87]. This disease can lead to acute hepatic failure or cirrhosis in infancy. In addition, 40% of patients who survive beyond the age of 2 develop HCCs [88].
GWAS have identified single-nucleotide polymorphisms (SNPs) that are associated with HCC carcinogenesis. A SNP in the epidermal growth factor (EGF) gene (rs4444903) was associated with an elevated risk of HCC in patients with cirrhosis [89]. A SNP (rs17401966) in Kinesin family member 1B (KIF1B) was associated with HBV-related HCC. Other SNPs in the Ubiquitination factor E4B (UBE4B) and Phosphogluconate dehydrogenase (PDG) genes were also shown to be associated with HCC amongst HBV positive patients [90]. Two SNPs (rs2596542 and rs1012068) discovered in a GWAS conducted in two large Japanese cohorts were significantly related with HCV-induced HCC [91,92].
2.7. Endocrine Risk Factors
Thyroid hormones are essential for lipid metabolism and have been shown to play a role in the pathogenesis of NAFLD/NASH [93]. Hypothyroidism has been demonstrated to be more common in patients with HCV, with a higher prevalence in those with cirrhosis [94]. Studies have also shown that patients with hypothyroidism have a two-fold higher risk of HCC than those with no prior history of thyroid cancer [95,96]. High thyroid stimulating hormone levels in HCC patients were found to be associated with larger tumor sizes [97]. Huang et al. demonstrated that 3,3′5-tri-iodo-l-thyronine (T3) suppressed HCC cell proliferation through the inhibition of serine/threonine-protein kinase, PIM-1, via miRNA (miR-214-3p) [98]. T3 supplementation in rats resulted in fewer tumor nodules as well as a shift in global transcriptomic expression profile. T3 was shown to exert anti-carcinogenic effects through the maintaining of genes responsible for hepatocyte differentiation, such as KLF9 and HNF4a [99].
Epidemiologically, HCC predominately occurs in males, with a male-to-female ratio ranging from 1.5:1 to 11:1. HCC prognosis, survival, and disease free survival after surgery are significantly better in females than males [100]. The predominance of HCC in males has been thought to be related to the effects of androgen/androgen receptors (ARs). ARs have been shown to promote HBV viral replication and HBV induced HCC [101], while AR knockout mice have fewer tumor nodules [102]. AR signaling has been demonstrated to promote key regulators of HCC carcinogenesis, including the MAPK/STAT/AKT pathway [103].
Estrogen/estrogen receptors (ERs) have been found to have protective effects against HCC while postmenopausal females have higher incidences of HCC [104,105]. Estrogen administration has been shown to reduce proinflammatory cytokines such as IL-6, a critical cytokine in HCC carcinogenesis [106]. Naugler et al. reported that estrogen treatment could reduce HCC carcinogenesis in DEN-injured rats by attenuating MyD88-dependent NF- κB signaling and inhibiting IL-6 signaling [107]. ER activation has also been shown to reduce STAT3 activation [108], a key regulator of the inflammatory tumor microenvironment [109].
3. Pathogenesis of HCC
A large body of research has been performed to address HCC pathogenesis. Large-scale genomic quantitative comparisons of HCC tumors have revealed the occurrence of chromosomal and microsatellite instability [110]. Loss of heterozygosity and SNP arrays have shown loss or mutations in tumor suppressor genes such as TP53 (P53) [111], retinoblastoma RB1 (RB1) [112], CDKN2A (P16INK4A) [113], and insulin-like growth factor-2 receptor (IGF-2R) [114]. Gain of function mutations such as CTNNBI (β-catenin) can upregulate the transcription of MYC, cyclin D1, and COX2 [115]. There is a strong association between HBV encoded viral protein HBx and the suppression of P53 induced apoptosis [116]. HCV core protein can also have direct carcinogenic effects by inducing ROSs [117].
Dysregulations of miRNAs, a class of small non-coding RNAs, can lead to HCC carcinogenesis [118]. Gene expression profiling has revealed that miR-181 upregulation is associated with the Wnt/B-catenin pathway [119]. MiR-26 downregulation has been shown to be associated with poor prognosis and a higher risk for metastasis [120]. Silencing of miR-122 was associated with increased cancer invasion, elevated alpha-fetoprotein expression, as well as higher HCC grades [121].
Genome-wide gene expression profiling has been used to capture dysregulated gene-expression signatures [122]. Numerous genome-wide expression studies have identified molecular sub-classes of HCC [123,124]. Aggressive HCC tumors are characterized by increased genetic instability, cellular proliferation, and impairment of tumor suppressor genes [125]. Hoshida et al. categorized HCC into three classes. S1 tumors are the most aggressive and are characterized by higher activation of TGF-β. S2 tumors overexpress EPCAM, AFP, and IGF-2 [126], while S3 tumors have matured hepatocyte-like phenotypes [127]. Zucman-Rossi et al. characterized proliferative vs. non-proliferative sub-classes of HCC. The main traits of the proliferative subclass are related to tumor proliferation and survival, while non-proliferative HCCs resemble normal hepatocytes [128].
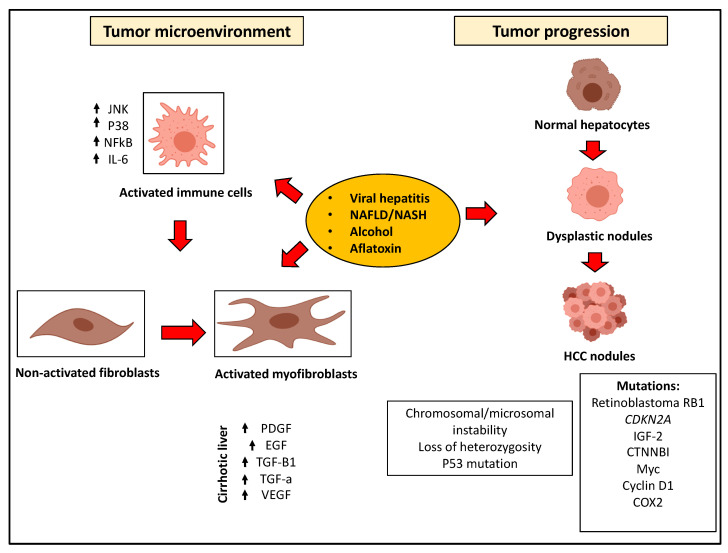
It is also important to recognize that the hepatic microenvironment significantly promotes tumor progression [129] and concomitantly limits therapeutic interventions [130]. The normal liver stroma maintains tissue integrity and acts as a barrier against tumor formation [131]. During chronic inflammation, a modified stroma is formed, enriched in carcinoma-associated fibroblasts [132,133] and tumor-associated immune cells [134,135]. In such a pro-carcinogenic environment, cancer cells are potentiated to grow and proliferate such that responses to conventional treatments are altered (Figure 1).
Figure 1.
Mechanisms of hepatocellular carcinoma. Molecular pathways of HCC carcinogenesis are summarized. Risk factors include viral hepatitis, NAFLD, alcohol and toxins. HCC tumors develop as dysplastic nodules through the gaining of molecular aberrations and mutations. The cirrhotic microenvironment in the liver promotes HCC carcinogenesis through the activation of hepatic stellate cells into myofibroblasts. The cirrhotic background also promotes inflammation leading to the upregulation of pro-carcinogenic genes and pathways (text for details).
4. Molecular Biomarkers of HCC—The Prognostic Liver Signature
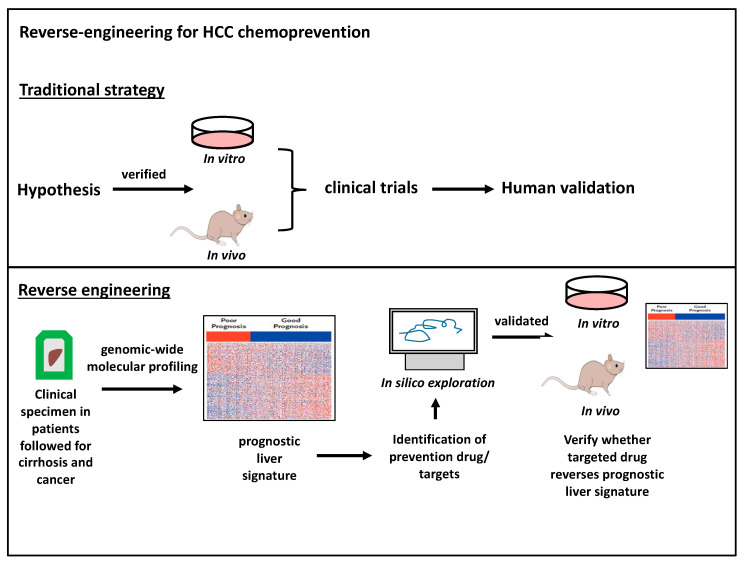
The major challenge in managing HCC is the complex and elusive mechanism of HCC carcinogenesis, leading to a scarcity of cancer biomarkers for targeted prevention trials. To circumvent this obstacle, a reverse engineering approach was developed to identify carcinogenic targets using long-term clinical follow-up patient cohorts, subsequently verified using in silico, in vitro, and in vivo models (Figure 2). It is hypothesized that cirrhosis leads to field cancerization, whereby cirrhotic liver tissue can harbor gene-expression signatures associated with carcinogenesis or recurrence after resection [136].
Figure 2.
Reverse engineering for HCC chemoprevention. Traditionally, chemoprevention targets are verified in both in vitro and experimental animal models and then introduced into clinical trials (top panel). The reverse-engineering identifies targets for chemoprevention in human cohorts already followed for decades. Samples are genetically profiled into molecular signatures and then experimentally evaluated for mechanisms and therapeutic strategies (bottom panel).
To verify this hypothesis, Hoshida et al. analyzed liver tissues surrounding resected HCV HCC tumors in 106 formalin-fixed, paraffin embedded blocks and identified a prognostic liver signature (PLS) containing 186 genes [137]. The poor-prognosis signature was found to be associated with an increase in liver-related deaths, progression of the Child–Pugh class, as well as HCC development. The 10-year HCC development rates were 42% and 18% for patients with poor and good prognostic signatures, respectively [138]. Though initially verified in HCV patients, the PLS also demonstrated significant concordance in liver tissues from HBV, alcohol, and NAFLD/NASH patients followed for 23 years [139]. This prognostic signature successfully verified the chemopreventive effect of erlotinib, a small molecule EGF pathway inhibitor, in multiple rodent models [140], and also led to the initiation of a cancer chemoprevention clinical trial (NCT02273362).
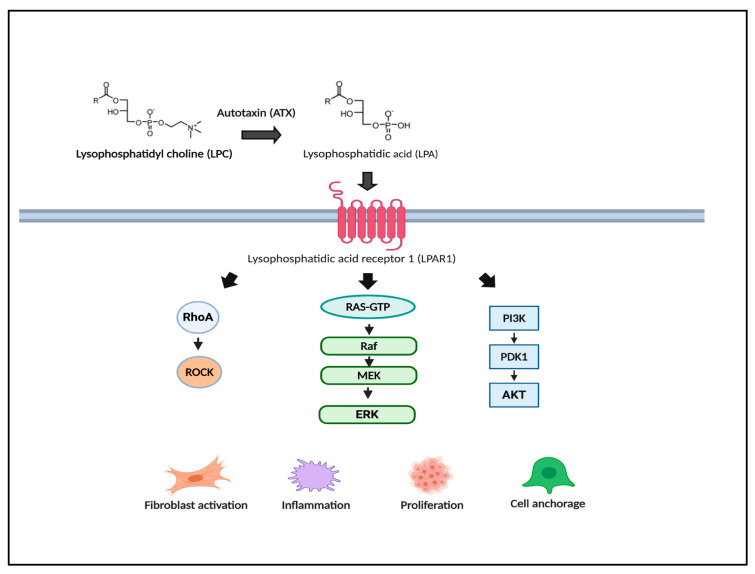
Besides the EGF pathway, other inflammatory and fibrotic pathways have been identified as valuable cancer targets for prevention. Top enriched regulator genes were AKT1, SLC35A1, DDX42, ILK, and LPAR1. AKT-activated mTOR inhibitors, including everolimus and sirolimus, are currently being investigated for chemoprevention after transplantation [141]. Lysophosphatidic acid receptor 1 (LPAR1) is the receptor for the bioactive lipid lysophosphatidic acid (LPA) produced from lysophosphatidyl choline (LPC) through the actions of a secrete lysophospholipase D named autotaxin (ATX). LPAR1 overexpression has been shown to promote fibrosis [142], inflammation and HCC carcinogenesis via upregulation of its downstream effectors, including RhoA/ROCK, RAS/MAPK/ERK, and AKT/PI3K (Figure 3) [143]. In a DEN model of cirrhosis, LPAR1 upregulation coincided with the development of cirrhosis. Furthermore, LPAR1 inhibition with ATX inhibitors attenuated liver fibrosis, reduced the number of HCC nodules, and reversed the PLS risk gene signature [137,144].
Figure 3.
Lysophosphatidic acid (LPA) pathway as a novel chemoprevention target. Reverse engineering transcriptome analysis revealed the LPA pathway as a target for HCC prevention. LPA and its G protein-coupled receptors, lysophosphatidic acid receptors (LPARs), promote fibrosis, inflammation, and carcinogenesis through the activation of down-stream RhoA, Ras/mitogen-activated protein kinase (MAPK)/extracellular-signal-regulated kinase (ERK), and Akt/PI3K. LPA activation has been observed in human and rodent cirrhotic livers at risk for HCC.
The reverse-engineering technique along with the transcriptomic analysis of cancer-prone markers can be used to not only unearth key biomarkers of cancer prevention, but also be used for the proof-of-concept of other experimental compounds. Inhibition of chromatin reader Bromodomain 4—a target identified by reverse-engineering—by use of a small molecule, JQ1, reduced HCC carcinogenesis in experimental rodent models by reverting the epigenetic as well as the poor prognostic signature [145]. Villa et al. found a five-gene signature that predicted tumor doubling time as well as overall survival. In this study, ultrasound surveillance was used to identify newly diagnosed HCCs in cirrhotic patients. Patients then underwent two CT scans 6 weeks apart in order to determine tumor doubling time. In this study, five genes (ANGPT2, NETO2, ESM1, NR4A1, and DLL4) that regulated angiogenesis and endothelial cell migration were significantly upregulated and predicted tumor doubling time and survival [146].
5. Prevention Strategies
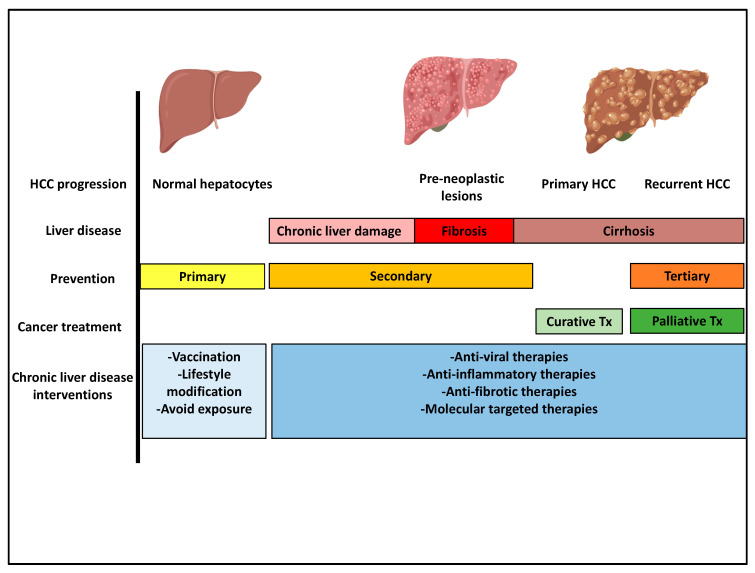
Understanding the risk factors and pathogenesis of HCC provides an opportunity for prevention strategies. Prevention can be sub-divided into primary, secondary, and tertiary prevention. Primary prevention focuses on eliminating cancer-predisposing factors through early vaccination, lifestyle modifications, as well as environmental interventions. Globally, a significant reduction in the incidence of HCC was observed after the implementation of hepatitis B vaccination [147,148,149]. Preventive actions against HCV can be taken through changes in social/cultural/medical practices such as the prevention of IV drug use and efficient screening of blood products and medical instruments [150]. In Australia, a substantial decline in the estimated intravenous drug use resulted in a decline in the number of new HCV infections from 14,000 per year in 2000 to 10,000 per year in 2005 [151]. Regulations of environmental carcinogens, such as Aflatoxin through information dissemination, have significantly reduced the Aflatoxin level in endemic areas [152].
Secondary prevention aims to delay the progression of chronic liver disease. This approach strives to eradicate the etiological agents (HBV and HCV) or inhibit the various steps in the carcinogenic progression. In general, chemoprevention agents should be inexpensive, well tolerated for long-term treatment, and available to the general population.
Tertiary prevention targets cancer recurrence or de-novo carcinogenesis within 1–2 years after curative treatment [153]. Ikeda et al. demonstrated in a randomized control trial that interferon-based immunotherapy after HCC resection resulted in a significant reduction in HCC recurrence [154]. Mazzaferro et al. demonstrated that adjuvant interferon therapy may reduce late recurrence of HCC [155]. Post-operative interferon-alpha is currently being investigated in patients with low miR-26 expression after HCC resection (NCT01681446). Immunosuppression with mTOR inhibitors has also been shown to reduce HCC recurrence [156,157] (Figure 4).
Figure 4.
HCC-prevention strategies through the progression of HCC development. HCC prevention strategies, primary, secondary, and tertiary prevention, target various stages of liver disease progression (text for details).
6. Early Diagnosis and Surveillance
Compliance to HCC surveillance is associated with early diagnosis, allocation of curative treatment, and longer adjusted overall survival [158]. Practice guidelines from The American Association for the Study of Liver Diseases (AASLD) and The European Association for the Study of the Liver (EASL) recommend HCC surveillance for high risk patients by abdominal ultrasound performed by experienced personnel every 6 months [159,160]. Surveillance is indicated for all patients with cirrhosis. For patients with less advanced liver diseases, risk stratification using regression analysis is used to determine surveillance interval.
Models predicting the need for HCC surveillance in HCV patients use factors such as age, alcohol intake, platelet count, gamma-glutamyltransferase, and non-sustained virological response [161,162]. The ADRESS-HCC study, performed in 34,932 patients with decompensated cirrhosis from the US national liver transplant waiting list, identified six predictors of HCC (age, diabetes, race, etiology, sex, and severity of disease according to the Child–Turcotte–Pugh score) [163]. A retrospective analysis of the HALT-C trial demonstrated that the addition of the EGF SNP to clinical parameters (age, gender, smoking status, ALK-p level, and platelet count) could improve HCC risk stratification [164]. Furthermore, Ioannou et al. developed a risk stratification model for both NAFLD and ALD cirrhosis using seven predictors (age, gender, diabetes, BMI, platelet count, serum albumin, and AST/ALT ratio) [165].
HCC surveillance is often underutilized. Real-life worldwide retrospective cohorts reported screening adherence ranging from 5.7% to 78.8%, with higher rates occurring in countries with national screening programs [166]. A study from the US including 13,002 patients showed that only 42% of patients with HCV-cirrhosis received one or two surveillance tests during the first year and only 12% of them received surveillance two to four years after the diagnosis of cirrhosis [167].
Although ultrasound surveillance is currently the gold standard for HCC surveillance, there are downsides including sensitivities ranging from 47% to 84% depending on the operator’s experience [168]. Magnetic resonance imaging (MRI) has high sensitivity and specificity for diagnosis of HCC and has the potential to improve HCC surveillance outcomes. In high-risk patients with cirrhosis, surveillance by MRI using liver-specific contrast increased early HCC detection compared to ultrasound but survival benefits and cost-effectiveness have not been demonstrated [169].
7. Etiology-Specific Secondary Chemoprevention
7.1. Hepatitis B
Antiviral treatments for HBV consist mainly of interferon therapies and nucleoside/nucleotide analogs [170]. Interferon alpha (IFN-α) therapy has shown inconsistent effects on HCC prevention due to its moderate effects on HBV viral replication [171]. The beneficial effects of nucleoside/nucleotide analogs are well established. In a randomized control trial, Liaw et al. demonstrated that continuous treatment with lamivudine significantly reduced the incidence of hepatic decompensation and the risk of HCC (3.9 percent vs. 7.4 percent) in patients with advanced liver disease [172]. In a retrospective study of 872 patients versus 699 historical controls, the annual incidence of HCC was reduced from 4.1% to 0.95% in patients with sustained response to lamivudine [173]. In one systemic review of 21 studies, the incidence of HCC was significantly lowered in HBV positive patients treated with lamivudine (2.8% vs. 6.4%; p < 0.01) [174].
7.2. Hepatitis C
Direct-acting anti-virals (DAAs) targeting viral protease, polymerase, and non-structural proteins have enabled improved sustained viral response compared to interferon-based therapies [175]. DAAs are better tolerated in cirrhotic patients in comparison to interferon-based therapies [176]. HCV-related cirrhosis mortality reached a plateau in 2014 and markedly declined from 2014 to 2016 after the introduction of DAAs [177]. After treatment, the sustained virologic response (SVR) is the best indication for successful HCV treatment [178]. Janjua et al. demonstrated that among DAA-treated patients, the HCC incidence rate was 6.9% in the SVR group vs. 38.2% in the non-SVR group [179]. Ioannou et al. found that DAA-induced SVR was associated with a 71% HCC risk reduction [180]. However, patients with pre-SVR fibrosis scores ≥ 3.25 have a higher annual incidence of HCC (3.66%/year) than those with <3.25 (1.16%/year) [181]. The persistence of HCC risk after HCV treatment can be partially explained by HCV-induced epigenetic modifications [182].
HCC surveillance should be continued in high-risk patients after DAA therapy. Despite the ongoing developments in HCV treatment options, the increasing rate of infection in young adults (age < 30) and the lack of screening are significant obstacles [183]. Barriers to HCV screening include lack of awareness, mental illness, lack of access to health care, and substance misuse [184]. The US Preventive Services Task Force recommends screening for adults at high risk, as well as one-time hepatitis C screening to all individuals born between 1945 and 1965. In high risk communities, the use of non-invasive fibroscanning can potentially identify individuals with chronic HCV [185].
Lifestyle intervention can be effective in patients with NAFLD and NASH. Weight loss > 10% has been shown to induce complete regression of NASH and partial regression of fibrosis [186]. Obese, sedentary individuals have increased risks of NAFLD in comparison to weight-matched physically active individuals [187]. EASL guidelines recommend moderate-intense aerobic physical activities in 3–5 sessions for a total of 150 min per week [188]. AASLD guidelines suggest the beneficial effects of physical activity but does not specify the exercise regimen [189]. There are currently no longitudinal studies demonstrating the effects of exercise on HCC risk reduction. Various pre-clinical rodent studies have demonstrated the efficacy of exercise in delaying HCC. In a hepatocyte-specific PTEN-deficient mouse model that developed steatohepatitis and spontaneous HCC, animals randomized to exercising developed fewer HCC nodules compared to sedentary animals (71% vs. 100%, respectively) [190].
Bariatric surgery is an effective option for weight loss in patients who are refractory to conservative treatment options. It has also been shown that bariatric surgery is a potential therapy for NASH. Lassailly et al. demonstrated that NASH resolved in 85% of patients after bariatric surgery while fibrosis was reduced in 33.8% of patients [191]. A meta-analysis demonstrated that bariatric surgery was associated with improvements in steatosis (91.6%), NASH (81.3%), as well as fibrosis (65.5%) [192]. Kwak et al. found that bariatric surgery was associated with a lower risk of HCC among matched cohorts of morbidly obese patients [193].
Diabetes mellitus (DM) has been shown to be an independent risk factor for HCC development [194]. Hyperinsulinemia can stimulate liver cell proliferation via the upregulation of IGF-1 [195] as well as hepatic stellate cell activation [196]. Insulin resistance is also an independent risk factor for liver fibrosis [197]. Given that NAFLD/NASH and DM commonly exist together, it is a reasonable hypothesis that anti-diabetic drugs have potential chemopreventive effects against NAFLD/NASH induced HCC. Metformin has been shown in several non-randomized studies to have HCC preventative effects in type-2 diabetic males [198]. In pre-clinical studies, the anti-carcinogenic effects of metformin have been shown to be mediated through the upregulation of AMPK, and the subsequent inactivation of mTOR via the upstream regulator of AMPK, LKB1 [199,200]. When exposed to DEN, male rats treated with metformin developed less fibrosis, cirrhosis, and overall fewer tumor nodules [201]. Metformin has been shown to improve liver histology and ALT levels in 30% of patients with NASH (NCT00063232). However, there are no completed clinical trials to date examining the effects of metformin administration on HCC prevention. The only trial to date (NCT02319200) was terminated early due to the lack of participants.
Long-term pioglitazone treatment can improve hepatic triglyceride content and fibrosis in patients with diabetes and NASH [202]. In a standard model, mice receiving a single injection of DEN, followed by the administration of a choline deficient L-amino acid diet, developed hepatic fibrosis and HCC nodules. In this model, pioglitazone administration at the initial onset of fibrosis resulted in a reduction in fibrosis and tumor nodules [203]. Pioglitazone targets downstream nuclear hormone PPARγ by binding to retinoid X receptor and subsequently regulating insulin sensitivity, glucose metabolism, and hepatic inflammation [204]. However, there are non-negligible side effects associated with pioglitazione, such as heart failure, weight gain, and bone loss.
Vitamin E is a lipid-soluble nutrient that acts as an antioxidant to prevent free radical damage in membranes and plasma lipoproteins [205]. Treatment with vitamin E has been shown to improve liver functions and fibrosis [206,207]. However, the effects of vitamin E on inflammation are controversial. A number of studies demonstrated no improvement in inflammation, while other studies concluded that vitamin E was associated with a significant improvement in steatosis, fibrosis, and inflammation [208,209,210]. No clinical data is available on vitamin E’s HCC prevention effects.
7.3. Alcohol
Alcohol abstinence remains to be the most important treatment for alcohol-related hepatic disease. Alcohol cessation has been shown to decrease the risk of HCC by 6–10% per year. After two decades, the risk becomes equal to the general population [211]. Among former versus current drinkers, the odds-ratio of men developing HCC was significantly higher in those who stopped drinking for less than 10 years [212].
However, targeting sobriety is both complex and difficult to maintain. The current gold standard for alcohol use disorder is achieving total abstinence and preventing relapse [213]. Both inpatient and outpatient rehabilitation programs have shown efficacy in helping patients maintain abstinence [214]. It has also been shown that participation and communication with an alcohol addiction specialist in Alcoholic Anonymous can help to maintain abstinence [215]. Cognitive-behavioral coping skills therapy (CBT) is a psychotherapeutic approach that helps patients recognize risks for relapse and develop strategies to mitigate the risks. Patients are also encouraged to keep a diary to document the risk events [216].
Disulfiram, the most common and oldest pharmaceutical intervention for alcohol use disorder, works by inhibiting aldehyde dehydrogenase, resulting in an accumulation of aldehyde that usually results in a disulfiram–alcohol reaction, consisting primarily of tachycardia, flushing, nausea, and vomiting [217]. Studies have shown that disulfiram is effective in promoting short-term abstinence [218]. Naltrexone is an agent that blocks opioid receptors, which in turn leads to a reduction in dopamine levels and a reduction in alcohol intake [219]. The Combined Pharmacotherapies and Behavioral Interventions (COMBINE) study (NCT00006206) demonstrated that naltrexone, when given with medical counseling, resulted in an increase in the days of abstinence [220].
8. Etiology-Independent Secondary Chemoprevention Strategies
8.1. Statins
Statins, 3-hydroxy-3-methylgutaryl coenzyme A reductase inhibitors, are cholesterol-lowering agents that have cardiovascular protective effects [221]. Several randomized-controlled trials have demonstrated that statins have preventative effects in colorectal [222], breast [223], and prostate cancer [224]. Atorvastatin (10 mg/day) use in biopsy proven NASH patients demonstrated a 74% improvement in liver function tests as well as a rise in serum protein and adiponectin, a key regulator of lipid metabolism [225,226]. Statin use has been shown to correlate with a decreased risk of HCC carcinogenesis and recurrence after resection [227,228,229].
The anti-neoplastic effects of statins have been attributed to the inhibition of MYC [230], AKT [231,232], NF-κB, and IL6 production [233]. Statin use also reduces hepatic stellate cell activation via the induction of sterol regulatory element-binding protein 1 and PPAR [234], as well as reduction in portal hypertension via non-canonical hedgehog signaling [235]. Secondary prevention effects of simvastatin in patients with cirrhosis are being tested in a phase II clinical trial (NCT02968810). Currently, a multi-center double-blinded randomized clinical trial of tertiary prevention is being conducted with atorvastatin vs. placebo for HCC recurrence after completion ablation or hepatic resection (SHOT trial; NCT03024684).
8.2. Aspirin, COX2 Inhibitors and Anti-Platelet Agents
The major risk factor for HCC carcinogenesis is the non-resolving inflammation resulting in dysregulated production of cytokines, chemokines, growth factors, prostaglandins, and ROSs [236]. It is well established that TNF-α activated NF-κB is a critical mediator for HCC carcinogenesis [237]. In a large prospective study, the use of nonsteroidal anti-inflammatory drugs (NSAIDs) among men and women between the ages of 50 and 71 years was associated with a 37% reduced risk of HCC as well as a 51% reduced risk of mortality from chronic liver disease [238]. Cyclooxygenease-2 (COX2) controlled prostaglandins are upregulated in chronic liver disease [239]. Leng et al. demonstrated that COX2 overexpression in vitro resulted in cell growth and overexpression of AKT, while treatment with COX-2 inhibitor, celecoxib, resulted in a significant reduction in AKT activation and upregulation of apoptosis [240].
In two prospective cohorts of U.S. men and women, regular use of aspirin was associated with a significant reduction in the risk of developing HCC compared to non-regular use (2.1 vs. 5.2 cases per 100,000 person-years). However, prevention effects were not observed with other NSAIDs [241]. Aspirin has also been shown to inhibit platelet thromboxane, subsequently leading to the inhibition of spingosine-1-phosphate S1P, a lipid molecule that has been shown to promote HCC proliferation [242]. A study demonstrated that the combination of aspirin and clopidogrel reduced intrahepatic immune cell infiltration, NASH, and HCC [243]. However, increased risk of bleeding may limit the use of these drugs for long-term prevention, particularly in cirrhotic patients. Besides its anti-inflammatory properties, aspirin has also been shown to have anti-fibrotic properties. Wang et al. showed that aspirin targets P4HA2, an enzyme involved in collagen synthesis [244]. Aspirin administration to mice that were subcutaneously engrafted with HepG2 cells resulted in a reduction in collagen deposition and tumor growth [245]. Daily aspirin use was also shown to significantly lower the odds-ratio of NASH and fibrosis in 361 adults with biopsy-proven NAFLD [246].
8.3. Anti-Fibrosis Therapy
Fibrosis has been shown to be a key risk factor for HCC [247]. However, anti-fibrotic therapies for HCC prevention have not been established. Most clinical trials are designed to study the anti-fibrosis or anti-cancer effects of drugs, but rarely both. Though promising, therapies such as ASK-1 inhibitor, selonsertib (NCT02466516) and dual PPARα/δ agonist, elafibranor (NCT02704403), have demonstrated efficacy in reducing fibrosis but have not been tested for HCC prevention [248,249].
8.4. Nutritional Agents
Food-derived agents, nutritional supplements, and certain phytochemicals, plant-derived bioactive chemicals, have been recognized as potential prevention options for HCC. Glycyrrhizin, an extract of licorice root, has been shown to lower serum aminotransferases, improve liver histology, and delay HCC carcinogenesis in humans and animal models [250,251,252,253]. Sho-saiko-to, a Chinese herbal medicine that contains glycyrrhizin, was shown to increase survival in cirrhotic HBV patients as well as decrease the incidence of HCC [254]. Beta-carotene derived from fruits and vegetables reduced the number and size of hepatic nodules in rats injured by DEN and phenobarbital [255]. Epigallocatechin gallate (EGCG), the most abundant green tea catechin polyphenol, has been shown to inhibit tumor growth and induce apoptosis in vitro [256]. In a rodent HCC model of DEN and aflatoxin, EGCG treatment reduced the number of placental glutathione S-transferase positive pre-neoplastic nodules [257]. In a phase 2 clinical trial, consumption of green tea polyphenols led to a significant reduction in oxidative DNA damage in HBV positive patients exposed to aflatoxin [258]. EGCG was also shown to reverse the poor prognostic gene signature described by Hoshida et al. [137,259]. The mechanisms of HCC risk reduction with coffee consumption have yet to be determined. However, coffee has been shown to contain numerous anti-carcinogenic chemical compounds. Diterpenes have been shown to upregulate detoxifying enzymes and reduce the formation of aflatoxin–DNA adducts [260].
Higher vitamin D, 25(OH)D, levels have been associated with a reduced risk of HCC, while low levels are associated with increased risk of HBV-related HCC [261,262]. In DEN-injured mice, vitamin D3 up-regulated protein 1 (VDUP1) has been shown to suppress TNF and NF-κB activation [263]. Oral vitamin D3 is currently under investigation for the prevention of HCC in HBV patients (NCT02779465). Branched-chain amino acids (BCAA) have been shown to reduce hepatic fibrosis and HCC carcinogenesis in DEN-injured rats [264]. In an observational study of cirrhotic patients in Japan, BCAA supplementation was associated with a lower incidence of HCC development [265].
Fish is a rich source for n-3 polyunsaturated fatty acids and has been shown to reduce the risk of HCC by 35% [266] irrespective of the viral hepatitis status [267]. In a NAFLD HCC rodent model, mice fed with an n-3 polyunsaturated fatty acid supplemented diet have significant reductions in fibrosis and tumor nodules [268]. However, processed red meat has been shown to actually increase the risk of HCC [269] (Figure 5).
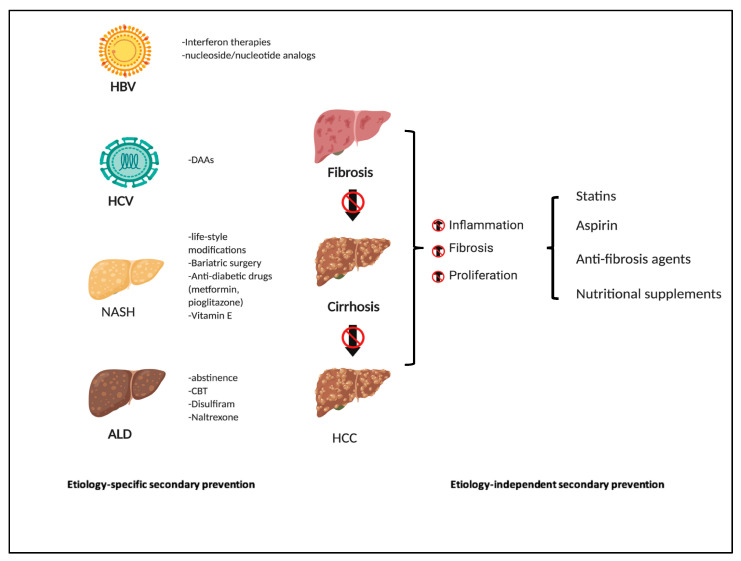
Figure 5.
Etiology-specific and independent secondary HCC prevention. Etiology-specific secondary prevention targets the various risk factors of HCC development, including HBV, HCV, NAFLD/NASH, and ALD. Etiology independent prevention strategies include agents that have anti-fibrosis or anti-inflammatory activities.
9. Challenges and Obstacles in Prevention
A major obstacle in HCC chemoprevention is the lack of accurate pre-clinical models that closely mimic HCC carcinogenesis in humans. Many drugs that enter phase I clinical trials are able to progress to phase II [270]. However, 95% of drugs that enter clinical trials do not enter the market [271]. Many drugs are initially tested in the pre-clinical setting using in vitro systems. Cancer cell lines are invaluable in vitro models that are widely used for cancer research and novel drug discovery. The major concern is that they do not accurately reflect their tissues of origin due to genetic mutations and passage cycle-derived transcriptomic alterations. Many human HCC cell lines are strikingly different to their tumors of origin [272]. This is likely why compounds that show promise in in vitro models are ineffective clinically [273]. There lacks an in vitro system in cancer prevention research that captures cancer initiation, promotion, and progression. Most commonly established human HCC cell lines such as HepG3 and HuH7 can be used to investigate cancer treatment, but not prevention.
An ideal in vivo animal model should capture the key biological features of HCC and recapitulate the tumor microenvironment. Major etiologies for failure include the complex molecular heterogeneity as well as the limited understanding of HCC carcinogenesis. HCC genetically engineered mouse models (GEEMs) activate oncogenes such as HRAS or MYC [274] or disrupt tumor suppressor genes such as PTEN or TP53 [275]. However, most GEMMs have failed in addressing the complex interaction between HCC and the representative microenvironment.
Chemical carcinogens such as carbon tetrachloride [276], DEN [277] and thioacetamide [278] induce fibrosis, cirrhosis and HCC sequentially. The repeated, low dose DEN cirrhosis-driven rat model [279] demonstrated an induction of the HCC prognostic gene signature similar to that of the human signature [139]. Chemical carcinogens such as DEN are an excellent model for chemoprevention research given the accurate recapitulation of all steps in the HCC carcinogenesis pathway.
Prior to the omics era, there were limited HCC prevention targets. Transcriptomic analysis of clinical specimens and reverse-engineering prevention targets may ultimately overcome this challenge. Cirrhotic patients expressing the poor prognostic signature would benefit the most from chemoprevention. HCC chemoprevention clinical trials are difficult to conduct and expensive given the requirement for a large sample size and long observation periods. Even if an agent demonstrates efficacy with a low toxicity profile, it still takes 5–10 years for a drug to move through phase III clinical trial [280]. Prevention trials focused on lifestyle modification, such as weight control, diet, and physical activity, can be challenging because these activities are typically clustered, thus identifying the change of a single behavior can be difficult if not impossible [281].
Another major challenge in HCC prevention is the lack of understanding of the long term tolerability and impact on quality of life of many drugs. To be acceptable for HCC prevention, a drug needs to be well tolerated for an extended period of time with minimal—if any—side effects. It is also important for physicians to be comfortable in prescribing these medications. Even minor side effects can be enough to affect quality of life and compliance with a cancer prevention medication, thus limiting its efficacy. This is especially of importance in HCC prevention, where a majority of this patient population have some form of chronic cirrhosis. Metformin is generally well tolerated with a good safety profile. However, lactic acidosis, one of its most notorious side effects, is more likely to occur in patients with hepatic insufficiency [282]. Aspirin is also commonly prescribed and well tolerated, but physicians may not be comfortable prescribing aspirin to cirrhotic patients who are at high risk of gastrointestinal bleeds.
10. Conclusions
Integration of HCC prevention research to the clinical setting is an extremely important strategy. Prevention clinical trials are very challenging to conduct because of the need for large sample sizes and long observation times. In addition, establishing the optimal dose and duration for chemopreventive drugs remains a challenge. Although there has been notable success in primary and secondary prevention for viral hepatitis such as the HBV vaccine or HCV cure by DAAs, similar successes for prevention of metabolic HCC are largely absent given the challenges associated with strategies of improved diet and regular exercise. Furthermore, there is no approved strategy to prevent HCC in advanced fibrosis or post HCC resection. Advances in the field of HCC chemoprevention will be aided by a more complete characterization of HCC carcinogenesis as well as a better understanding of the liver microenvironment. The main challenge in HCC prevention research will always be translating pre-clinical research into successful clinical trials but there is a promise for success as we develop more individualized therapies.
Abbreviations
| AR | Androgen receptor |
| ALD | Alcoholic liver disease |
| AMPK | AMP-activated protein kinase |
| COX2 | Cyclooxygenease-2 |
| DAA | Direct-acting antivirals |
| DEN | N-diethylnitrosamine |
| DM | Diabetes mellitus |
| EGF | Epidermal growth factor |
| EGFR | Epidermal growth factor receptor |
| GWAS | Genome wide associated studies |
| HBV | Hepatitis B virus |
| HCV | Hepatitis C virus |
| HCC | Hepatocellular carcinoma |
| IFN-α | Interferon alpha |
| LAR | Lysophosphatidic acid receptor |
| LPAR1 | Lysophosphatidic Acid Receptor 1 |
| mTOR | Mammalian target of rapamycin |
| NAFLD | Nonalcoholic fatty liver disease |
| NF-κB | Nuclear factor κB |
| NASH | Nonalcoholic steatohepatitis |
| NSAIDS | Nonsteroidal anti-inflammatory drugs |
| PPAR | Peroxisome proliferator activated receptors |
| PLS | Prognostic liver signature |
| ROS | Reactive oxygen species |
| SNP | Single nucleotide polymorphism |
| SVR | Sustained virologic response |
| TNF-a | Tumor-Necrosis-Factor alpha |
Author Contributions
S.L., A.S., B.C.F., T.B., and K.K.T. contributed to conceptualization; S.L., A.S., D.J.E. contributed to original draft preparation. S.L., A.S., D.J.E., Y.H., B.C.F., T.B., and K.K.T. contributed to reviewing and editing. S.L. contributed to visualization. K.K.T. contributed to supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Institutes of Health (grant numbers T32 CA071345 to S.L.) and the Massachusetts General Hospital Department of Surgery (K.K.T.).
Conflicts of Interest
The authors have no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yang J.D., Hainaut P., Gores G.J., Amadou A., Plymoth A., Roberts L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019;16:589–604. doi: 10.1038/s41575-019-0186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray F., Me J.F., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Asrani S.K., Devarbhavi H., Eaton J., Kamath P.S. Burden of liver diseases in the world. J. Hepatol. 2019;70:151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Siegel R.L., Miller K.D., Jemal A. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 5.Beste L.A., Leipertz S.L., Green P.K., Dominitz J.A., Ross D., Ioannou G.N. Trends in Burden of Cirrhosis and Hepatocellular Carcinoma by Underlying Liver Disease in US Veterans, 2001–2013. Gastroenterology. 2015;149:1471–1482.e5. doi: 10.1053/j.gastro.2015.07.056. [DOI] [PubMed] [Google Scholar]
- 6.Mokdad A.H., Forouzanfar M.H., Daoud F., Mokdad A.A., El Bcheraoui C., Moradi-Lakeh M., Kyu H.H., Barber R.M., Wagner J., Cercy K., et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:2383–2401. doi: 10.1016/S0140-6736(16)00648-6. [DOI] [PubMed] [Google Scholar]
- 7.Kanwal F., Hoang T., Kramer J.R., Asch S.M., Goetz M.B., Zeringue A., Richardson P., El–Serag H.B. Increasing Prevalence of HCC and Cirrhosis in Patients with Chronic Hepatitis C Virus Infection. Gastroenterology. 2011;140:1182–1188.e1. doi: 10.1053/j.gastro.2010.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howlader N., Noone A.M., Krapcho M., Miller D., Brest A., Yu M., Ruhl J., Tatalovich Z., Mariotto A., Lewis D.R., et al. SEER Cancer Statistics Review, 1975-2016. National Cancer Institute; Bethesda, MD, USA: 2019. Based on November 2018 SEER Data Submission, Posted to the SEER Web Site. [Google Scholar]
- 9.Altekruse S.F., McGlynn K.A., Reichman M.E. Hepatocellular Carcinoma Incidence, Mortality, and Survival Trends in the United States From 1975 to 2005. J. Clin. Oncol. 2009;27:1485–1491. doi: 10.1200/JCO.2008.20.7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez P.M., Villanueva A., Llovet J.M. Systematic review: Evidence-based management of hepatocellular carcinoma—An updated analysis of randomized controlled trials. Aliment. Pharmacol. Ther. 2006;23:1535–1547. doi: 10.1111/j.1365-2036.2006.02932.x. [DOI] [PubMed] [Google Scholar]
- 11.Pompili M., Saviano A., De Matthaeis N., Cucchetti A., Ardito F., Federico B., Brunello F., Pinna A.D., Giorgio A., Giulini S.M., et al. Long-term effectiveness of resection and radiofrequency ablation for single hepatocellular carcinoma ≤ 3 cm. Results of a multicenter Italian survey. J. Hepatol. 2013;59:89–97. doi: 10.1016/j.jhep.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Llovet J.M., Ricci S., Mazzaferro V., Hilgard P., Gane E., Blanc J.-F., De Oliveira A.C., Santoro A., Raoul J.-L., Forner A., et al. Sorafenib in Advanced Hepatocellular Carcinoma. N. Engl. J. Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 13.Abou-Alfa G.K., Meyer T., Cheng A.-L., El-Khoueiry A.B., Rimassa L., Ryoo B.-Y., Cicin I., Merle P., Chen Y., Park J.-W., et al. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N. Engl. J. Med. 2018;379:54–63. doi: 10.1056/NEJMoa1717002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu A.X., Galle P.R., Kudo M., Finn R.S., Qin S., Xu Y., Abada P., Llovet J. A study of ramucirumab (LY3009806) versus placebo in patients with hepatocellular carcinoma and elevated baseline alpha-fetoprotein (REACH-2) J. Clin. Oncol. 2018;36:TPS538. doi: 10.1200/JCO.2018.36.4_suppl.TPS538. [DOI] [Google Scholar]
- 15.El-Khoueiry A.B., Sangro B., Yau T., Crocenzi T.S., Kudo M., Hsu C., Kim T.-Y., Choo S.-P., Trojan J., Welling T.H., et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): An open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finn R.S., Ryoo B.-Y., Merle P., Kudo M., Bouattour M., Lim H.-Y., Breder V.V., Edeline J., Chao Y., Ogasawara S., et al. Results of KEYNOTE-240: Phase 3 study of pembrolizumab (Pembro) vs. best supportive care (BSC) for second line therapy in advanced hepatocellular carcinoma (HCC) J. Clin. Oncol. 2019;37:4004. doi: 10.1200/JCO.2019.37.15_suppl.4004. [DOI] [Google Scholar]
- 17.Pinter M., Jain R.K., Duda D.G. The Current Landscape of Immune Checkpoint Blockade in Hepatocellular Carcinoma. JAMA Oncol. 2020;22 doi: 10.1001/jamaoncol.2020.3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang P., Yang Y., Wen F., He X., Tang R., Du Z., Zhou J., Zhang J., Li Q. Cost-effectiveness of sorafenib as a first-line treatment for advanced hepatocellular carcinoma. Eur. J. Gastroenterol. Hepatol. 2015;27:853–859. doi: 10.1097/MEG.0000000000000373. [DOI] [PubMed] [Google Scholar]
- 19.El-Serag H.B., Rudolph K.L. Hepatocellular Carcinoma: Epidemiology and Molecular Carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 20.Franco E. Hepatitis B: Epidemiology and prevention in developing countries. World J. Hepatol. 2012;4:74–80. doi: 10.4254/wjh.v4.i3.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsu Y.-S., Chien R.-N., Yeh C.-T., Sheen I.-S., Chiou H.-Y., Chu C.-M., Liaw Y.-F. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002;35:1522–1527. doi: 10.1053/jhep.2002.33638. [DOI] [PubMed] [Google Scholar]
- 22.Fattovich G., Olivari N., Pasino M., D’Onofrio M., Martone E., Donato F. Long-term outcome of chronic hepatitis B in Caucasian patients: Mortality after 25 years. Gut. 2007;57:84–90. doi: 10.1136/gut.2007.128496. [DOI] [PubMed] [Google Scholar]
- 23.Fattovich G. Natural History and Prognosis of Hepatitis B. Semin. Liver Dis. 2003;23:047–058. doi: 10.1055/s-2003-37590. [DOI] [PubMed] [Google Scholar]
- 24.Yang J.D., Kim W.R., Coelho R., Mettler T.A., Benson J.T., Sanderson S.O., Therneau T.M., Kim B., Roberts L.R. Cirrhosis Is Present in Most Patients with Hepatitis B and Hepatocellular Carcinoma. Clin. Gastroenterol. Hepatol. 2011;9:64–70. doi: 10.1016/j.cgh.2010.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osawa M., Akuta N., Suzuki F., Fujiyama S., Kawamura Y., Sezaki H., Hosaka T., Kobayashi M., Kobayashi M., Saitoh S., et al. Prognosis and predictors of hepatocellular carcinoma in elderly patients infected with hepatitis B virus. J. Med. Virol. 2017;89:2144–2148. doi: 10.1002/jmv.24890. [DOI] [PubMed] [Google Scholar]
- 26.El-Serag H.B. Epidemiology of Viral Hepatitis and Hepatocellular Carcinoma. Gastroenterology. 2012;142:1264–1273.e1. doi: 10.1053/j.gastro.2011.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soussan P., Garreau F., Zylberberg H., Ferray C., Brechot C., Kremsdorf D. In vivo expression of a new hepatitis B virus protein encoded by a spliced RNA. J. Clin. Investig. 2000;105:55–60. doi: 10.1172/JCI8098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edmunds W.J., Medley G.F., Nokes D.J., Hall A.J., Whittle H.C. The influence of age on the development of the hepatitis B carrier state. Proc. R. Soc. B Boil. Sci. 1993;253:197–201. doi: 10.1098/rspb.1993.0102. [DOI] [PubMed] [Google Scholar]
- 29.Sung W.-K., Zheng H., Li S., Chen R., Liu X., Li Y., Lee N.P., Lee W.H., Ariyaratne P.N., Tennakoon C., et al. Genome-wide survey of recurrent HBV integration in hepatocellular carcinoma. Nat. Genet. 2012;44:765–769. doi: 10.1038/ng.2295. [DOI] [PubMed] [Google Scholar]
- 30.Yan H., Yang Y., Zhang L., Tang G., Wang Y., Xue G., Zhou W., Sun S. Characterization of the genotype and integration patterns of hepatitis B virus in early- and late-onset hepatocellular carcinoma. Hepatology. 2015;61:1821–1831. doi: 10.1002/hep.27722. [DOI] [PubMed] [Google Scholar]
- 31.Chemin I., Zoulim F. Hepatitis B virus induced hepatocellular carcinoma. Cancer Lett. 2009;286:52–59. doi: 10.1016/j.canlet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 32.Lucifora J., Arzberger S., Durantel D., Belloni L., Strubin M., Levrero M., Zoulim F., Hantz O., Protzer U. Hepatitis B virus X protein is essential to initiate and maintain virus replication after infection. J. Hepatol. 2011;55:996–1003. doi: 10.1016/j.jhep.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 33.Bayliss J., Lim L., Thompson A.J., Desmond P., Angus P., Locarnini S., Revill P.A. Hepatitis B virus splicing is enhanced prior to development of hepatocellular carcinoma. J. Hepatol. 2013;59:1022–1028. doi: 10.1016/j.jhep.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 34.Wong R.J., Cheung R., Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59:2188–2195. doi: 10.1002/hep.26986. [DOI] [PubMed] [Google Scholar]
- 35.Galbraith J.W., Franco R.A., Donnelly J.P., Rodgers J.B., Morgan J.M., Viles A.F., Overton E.T., Saag M.S., Wang H.E. Unrecognized chronic hepatitis C virus infection among baby boomers in the emergency department. Hepatology. 2015;61:776–782. doi: 10.1002/hep.27410. [DOI] [PubMed] [Google Scholar]
- 36.Jacobson I.M., Davis G.L., El–Serag H., Negro F., Trepo C. Prevalence and Challenges of Liver Diseases in Patients with Chronic Hepatitis C Virus Infection. Clin. Gastroenterol. Hepatol. 2010;8:924–933. doi: 10.1016/j.cgh.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 37.Liang T.J., Ward J.W. Hepatitis C in Injection-Drug Users—A Hidden Danger of the Opioid Epidemic. New Engl. J. Med. 2018;378:1169–1171. doi: 10.1056/NEJMp1716871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khan A.D., Magee E., Grant G. National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Volume 62. CDC; Atlanta, GA, USA: 2013. p. 149. CDC Health Disparities Inequalities Report—United States. [Google Scholar]
- 39.Galbraith J.W., Donnelly J.P., Franco R.A., Overton E.T., Rodgers J.B., Wang H.E. National Estimates of Healthcare Utilization by Individuals with Hepatitis C Virus Infection in the United States. Clin. Infect. Dis. 2014;59:755–764. doi: 10.1093/cid/ciu427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yoshida H., Shiratori Y., Moriyama M., Arakawa Y., Ide T., Sata M., Inoue O., Yano M., Tanaka M., Fujiyama S., et al. Interferon Therapy Reduces the Risk for Hepatocellular Carcinoma: National Surveillance Program of Cirrhotic and Noncirrhotic Patients with Chronic Hepatitis C in Japan. Ann. Intern. Med. 1999;131:174–181. doi: 10.7326/0003-4819-131-3-199908030-00003. [DOI] [PubMed] [Google Scholar]
- 41.Kanwal F., Kramer J.R., Ilyas J., Duan Z., El-Serag H.B. HCV genotype 3 is associated with an increased risk of cirrhosis and hepatocellular cancer in a national sample of U.S. Veterans with HCV. Hepatology. 2014;60:98–105. doi: 10.1002/hep.27095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoshida Y., Fuchs B.C., Bardeesy N., Baumert T.F., Chung R.T. Pathogenesis and prevention of hepatitis C virus-induced hepatocellular carcinoma. J. Hepatol. 2014;61:S79–S90. doi: 10.1016/j.jhep.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vescovo T., Refolo G., Vitagliano G., Fimia G., Piacentini M. Molecular mechanisms of hepatitis C virus–induced hepatocellular carcinoma. Clin. Microbiol. Infect. 2016;22:853–861. doi: 10.1016/j.cmi.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 44.Street A., Macdonald A., McCormick C.J., Harris M. Hepatitis C Virus NS5A-Mediated Activation of Phosphoinositide 3-Kinase Results in Stabilization of Cellular β-Catenin and Stimulation of β-Catenin-Responsive Transcription. J. Virol. 2005;79:5006–5016. doi: 10.1128/JVI.79.8.5006-5016.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Salloum S., Wang H., Ferguson C., Parton R.G., Tai A.W. Rab18 Binds to Hepatitis C Virus NS5A and Promotes Interaction between Sites of Viral Replication and Lipid Droplets. PLoS Pathog. 2013;9:e1003513. doi: 10.1371/journal.ppat.1003513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang J.D., Roberts L.R. Hepatocellular carcinoma: A global view. Nat. Rev. Gastroenterol. Hepatol. 2010;7:448–458. doi: 10.1038/nrgastro.2010.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim D., Li A.A., Gadiparthi C., Khan M.A., Cholankeril G., Glenn J.S., Ahmed A. Changing Trends in Etiology-Based Annual Mortality From Chronic Liver Disease, From 2007 through 2016. Gastroenterology. 2018;155:1154–1163.e3. doi: 10.1053/j.gastro.2018.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Piscaglia F., Svegliati-Baroni G., Barchetti A., Pecorelli A., Marinelli S., Tiribelli C., Bellentani S., HCC-NAFLD Italian Study Group Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology. 2016;63:827–838. doi: 10.1002/hep.28368. [DOI] [PubMed] [Google Scholar]
- 49.White D.L., Kanwal F., El–Serag H.B. Association Between Nonalcoholic Fatty Liver Disease and Risk for Hepatocellular Cancer, Based on Systematic Review. Clin. Gastroenterol. Hepatol. 2012;10:1342–1359.e2. doi: 10.1016/j.cgh.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McKeating J.A., Pfister D., O’Connor T., Pikarsky E., Heikenwalder M. The immunology of hepatocellular carcinoma. Nat. Immunol. 2018;19:222–232. doi: 10.1038/s41590-018-0044-z. [DOI] [PubMed] [Google Scholar]
- 51.Younossi Z., Anstee Q.M., Marietti M., Hardy T., Henry L., Eslam M., George J., Bugianesi E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018;15:11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 52.Yuan Y., Liu L., Chen H., Wang Y., Xu Y., Mao H., Li J., Mills G.B., Shu Y., Li L., et al. Comprehensive Characterization of Molecular Differences in Cancer between Male and Female Patients. Cancer Cell. 2016;29:711–722. doi: 10.1016/j.ccell.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Singh R., Kaushik S., Wang Y., Xiang Y., Novak I., Komatsu M., Tanaka K., Cuervo A.M., Czaja M.J. Autophagy regulates lipid metabolism. Nature. 2009;458:1131–1135. doi: 10.1038/nature07976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tanaka S., Hikita H., Tatsumi T., Sakamori R., Nozaki Y., Sakane S., Shiode Y., Nakabori T., Saito Y., Hiramatsu N., et al. Rubicon inhibits autophagy and accelerates hepatocyte apoptosis and lipid accumulation in nonalcoholic fatty liver disease in mice. Hepatology. 2016;64:1994–2014. doi: 10.1002/hep.28820. [DOI] [PubMed] [Google Scholar]
- 55.Gäbele E., Dostert K., Hofmann C., Wiest R., Schölmerich J., Hellerbrand C., Obermeier F. DSS induced colitis increases portal LPS levels and enhances hepatic inflammation and fibrogenesis in experimental NASH. J. Hepatol. 2011;55:1391–1399. doi: 10.1016/j.jhep.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 56.European Association for the Study of the Liver (EASL) Liver Int. 2001;21:71. doi: 10.1034/j.1600-0676.2001.210111.x. [DOI] [Google Scholar]
- 57.Ganne-Carrié N., Nahon P. Hepatocellular carcinoma in the setting of alcohol-related liver disease. J. Hepatol. 2019;70:284–293. doi: 10.1016/j.jhep.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 58.Meadows G.G., Zhang H. Effects of Alcohol on Tumor Growth, Metastasis, Immune Response, and Host Survival. Alcohol Res. Curr. Rev. 2015;37:311–322. doi: 10.35946/arcr.v37.2.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Persson E.C., Schwartz L.M., Park Y., Trabert B., Hollenbeck A.R., Graubard B.I., Freedman N.D., McGlynn K.A. Alcohol consumption, folate intake, hepatocellular carcinoma, and liver disease mortality. Cancer Epidemiol. Biomark. Prev. 2013;22:415–421. doi: 10.1158/1055-9965.EPI-12-1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Donato F., Tagger A., Gelatti U., Parrinello G., Boffetta P., Albertini A., DeCarli A., Trevisi P., Ribero M.L., Martelli C., et al. Alcohol and hepatocellular carcinoma: The effect of lifetime intake and hepatitis virus infections in men and women. Am. J. Epidemiol. 2002;155:323–331. doi: 10.1093/aje/155.4.323. [DOI] [PubMed] [Google Scholar]
- 61.Loomba R., Yang H.-I., Su J., Brenner D.A., Iloeje U., Chen C.-J. Obesity and Alcohol Synergize to Increase the Risk of Incident Hepatocellular Carcinoma in Men. Clin. Gastroenterol. Hepatol. 2010;8:891–898.e2. doi: 10.1016/j.cgh.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 62.Kimura T., Tanaka N., Fujimori N., Sugiura A., Yamazaki T., Joshita S., Komatsu M., Umemura T., Matsumoto A., Tanaka E. Mild drinking habit is a risk factor for hepatocarcinogenesis in non-alcoholic fatty liver disease with advanced fibrosis. World J. Gastroenterol. 2018;24:1440–1450. doi: 10.3748/wjg.v24.i13.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ochiai Y., Kawamura Y., Kobayashi M., Shindoh J., Kobayashi Y., Okubo S., Muraishi N., Kajiwara A., Iritani S., Fujiyama S., et al. Effects of alcohol consumption on multiple hepatocarcinogenesis in patients with fatty liver disease. Hepatol. Res. 2020 doi: 10.1111/hepr.13572. [DOI] [PubMed] [Google Scholar]
- 64.Setshedi M., Wands J.R., De La Monte S.M. Acetaldehyde Adducts in Alcoholic Liver Disease. Oxidative Med. Cell. Longev. 2010;3:178–185. doi: 10.4161/oxim.3.3.12288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fischer M., You M., Matsumoto M., Crabb D.W. Peroxisome Proliferator-activated Receptor α (PPARα) Agonist Treatment Reverses PPARα Dysfunction and Abnormalities in Hepatic Lipid Metabolism in Ethanol-fed Mice. J. Biol. Chem. 2003;278:27997–28004. doi: 10.1074/jbc.M302140200. [DOI] [PubMed] [Google Scholar]
- 66.Li C., Yang W., Zhang J., Zheng X., Yao Y., Tu K., Liu Q. SREBP-1 Has a Prognostic Role and Contributes to Invasion and Metastasis in Human Hepatocellular Carcinoma. Int. J. Mol. Sci. 2014;15:7124–7138. doi: 10.3390/ijms15057124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hu M., Wang F., Li X., Rogers C.Q., Liang X., Finck B.N., Mitra M.S., Zhang R., Mitchell D.A., You M. Regulation of hepatic lipin-1 by ethanol: Role of AMP-activated protein kinase/sterol regulatory element-binding protein 1 signaling in mice. Hepatology. 2011;55:437–446. doi: 10.1002/hep.24708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.He S., McPhaul C., Li J.Z., Garuti R., Kinch L., Grishin N.V., Cohen J.C., Hobbs H.H. A Sequence Variation (I148M) in PNPLA3 Associated with Nonalcoholic Fatty Liver Disease Disrupts Triglyceride Hydrolysis. J. Biol. Chem. 2010;285:6706–6715. doi: 10.1074/jbc.M109.064501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bucher S.S., Stickel F., Trépo E., Way M.M., Herrmann A., Nischalke H.D., Brosch M.M., Rosendahl J.J., Berg T., Ridinger M.M., et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat. Genet. 2015;47:1443–1448. doi: 10.1038/ng.3417. [DOI] [PubMed] [Google Scholar]
- 70.Baecker A., Liu X., La Vecchia C., Zhang Z.-F. Worldwide incidence of hepatocellular carcinoma cases attributable to major risk factors. Eur. J. Cancer Prev. 2018;27:205–212. doi: 10.1097/CEJ.0000000000000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Petrick J.L., Campbell P.T., Koshiol J., Thistle J.E., Andreotti G., Freeman L.E.B., Buring J.E., Chan A.T., Chong D.Q., Doody M.M., et al. Tobacco, alcohol use and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: The Liver Cancer Pooling Project. Br. J. Cancer. 2018;118:1005–1012. doi: 10.1038/s41416-018-0007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kolly P., Knöpfli M., Dufour J.-F.F. Effect of smoking on survival of patients with hepatocellular carcinoma. Liver Int. 2017;37:1682–1687. doi: 10.1111/liv.13466. [DOI] [PubMed] [Google Scholar]
- 73.Staretz M.E., Murphy S.E., Patten C.J., Nunes M.G., Koehl W., Amin S., Koenig L.A., Guengerich F.P., Hecht S.S. Comparative metabolism of the tobacco-related carcinogens benzo[a]pyrene, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol, and N’- nitrosonornicotine in human hepatic microsomes. Drug Metab. Dispos. 1997;25:154–162. [PubMed] [Google Scholar]
- 74.Barbieri S.S., Zacchi E., Amadio P., Gianellini S., Mussoni L., Weksler B.B., Tremoli E. Cytokines present in smokers’ serum interact with smoke components to enhance endothelial dysfunction. Cardiovasc. Res. 2011;90:475–483. doi: 10.1093/cvr/cvr032. [DOI] [PubMed] [Google Scholar]
- 75.JM D.P., MJ F.A., MJ L.A., Álvarez A. Tumor necrosis factor as an early marker of inflammation in healthy smokers. Med. Clin. 2012;139:47–53. doi: 10.1016/j.medcli.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 76.Dooley K., Von Tungeln L., Bucci T., Fu P., Kadlubar F. Comparative carcinogenicity of 4-aminobiphenyl and the food pyrolysates, Glu-P-1, IQ, PhIP, and MeIQx in the neonatal B6C3F1 male mouse. Cancer Lett. 1992;62:205–209. doi: 10.1016/0304-3835(92)90097-F. [DOI] [PubMed] [Google Scholar]
- 77.Azzalini L., Ferrer E., Ramalho L.N., Moreno M., Domínguez M., Colmenero J., Peinado V.I., Barberà J.A., Arroyo V., Ginès P., et al. Cigarette smoking exacerbates nonalcoholic fatty liver disease in obese rats. Hepatology. 2009;51:1567–1576. doi: 10.1002/hep.23516. [DOI] [PubMed] [Google Scholar]
- 78.Kew M. Aflatoxins as a cause of hepatocellular carcinoma. J. Gastrointest. Liver Dis. 2013;22:305–310. [PubMed] [Google Scholar]
- 79.Wu H.-C., Santella R. The Role of Aflatoxins in Hepatocellular Carcinoma. Zahedan J. Res. Med Sci. 2012;12 doi: 10.5812/hepatmon.7238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Woo L.L., Egner P.A., Belanger C.L., Wattanawaraporn R., Trudel L.J., Croy R.G., Groopman J.D., Essigmann J.M., Wogan G.N., Bouhenguel J.T. Aflatoxin B1-DNA Adduct Formation and Mutagenicity in Livers of Neonatal Male and Female B6C3F1 Mice. Toxicol. Sci. 2011;122:38–44. doi: 10.1093/toxsci/kfr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yu M.-W., Lien J.-P., Chiu Y.-H., Santella R.M., Liaw Y.-F., Chen C.-J. Effect of aflatoxin metabolism and DNA adduct formation on hepatocellular carcinoma among chronic hepatitis B carriers in Taiwan. J. Hepatol. 1997;27:320–330. doi: 10.1016/S0168-8278(97)80178-X. [DOI] [PubMed] [Google Scholar]
- 82.Yang J.D., A Mohamed E., Aziz A.O.A., I Shousha H., Hashem M.B., Nabeel M.M., Abdelmaksoud A.H., Elbaz T.M., Afihene M.Y., Duduyemi B.M., et al. Characteristics, management, and outcomes of patients with hepatocellular carcinoma in Africa: A multicountry observational study from the Africa Liver Cancer Consortium. Lancet Gastroenterol. Hepatol. 2017;2:103–111. doi: 10.1016/S2468-1253(16)30161-3. [DOI] [PubMed] [Google Scholar]
- 83.Eriksson S.G. Liver Disease in α 1 -Antitrypsin Deficiency: Aspects of Incidence and Prognosis. Scand. J. Gastroenterol. 1985;20:907–911. doi: 10.3109/00365528509088844. [DOI] [PubMed] [Google Scholar]
- 84.Janecke A.R., Mayatepek E., Utermann G. Molecular Genetics of Type 1 Glycogen Storage Disease. Mol. Genet. Metab. 2001;73:117–125. doi: 10.1006/mgme.2001.3179. [DOI] [PubMed] [Google Scholar]
- 85.Bianchi L. Glycogen storage disease I and hepatocellular tumours. Eur. J. Nucl. Med. Mol. Imaging. 1993;152:63–70. doi: 10.1007/BF02072092. [DOI] [PubMed] [Google Scholar]
- 86.Elmberg M., Hultcrantz R., Ekbom A., Brandt L., Olsson S., Olsson R., Lindgren S., Lööf L., Stål P., Wallerstedt S., et al. Cancer risk in patients with hereditary hemochromatosis and in their first-degree relatives. Gastroenterology. 2003;125:1733–1741. doi: 10.1053/j.gastro.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 87.Scott C.R. The genetic tyrosinemias. Am. J. Med. Genet. Part C Semin. Med. Genet. 2006;142:121–126. doi: 10.1002/ajmg.c.30092. [DOI] [PubMed] [Google Scholar]
- 88.Weinberg A.G., Mize C.E., Worthen H.G. The occurrence of hepatoma in the chronic form of hereditary tyrosinemia. J. Pediatr. 1976;88:434–438. doi: 10.1016/S0022-3476(76)80259-4. [DOI] [PubMed] [Google Scholar]
- 89.Tanabe K.K., Lemoine A., Finkelstein D.M., Kawasaki H., Fujii T., Chung R.T., Lauwers G.Y., Kulu Y., Muzikansky A., Kuruppu D., et al. Epidermal Growth Factor Gene Functional Polymorphism and the Risk of Hepatocellular Carcinoma in Patients with Cirrhosis. JAMA. 2008;299:53–60. doi: 10.1001/jama.2007.65. [DOI] [PubMed] [Google Scholar]
- 90.Zhang H., Zhai Y., Hu Z., Wu C., Qian J., Jia W., Ma F., Huang W., Yu L., Yue W., et al. Genome-wide association study identifies 1p36.22 as a new susceptibility locus for hepatocellular carcinoma in chronic hepatitis B virus carriers. Nat. Genet. 2010;42:755–758. doi: 10.1038/ng.638. [DOI] [PubMed] [Google Scholar]
- 91.Kumar V., Kato N., Urabe Y., Takahashi A., Muroyama R., Hosono N., Otsuka M., Tateishi R., Omata M., Nakagawa H., et al. Genome-wide association study identifies a susceptibility locus for HCV-induced hepatocellular carcinoma. Nat. Genet. 2011;43:455–458. doi: 10.1038/ng.809. [DOI] [PubMed] [Google Scholar]
- 92.Miki D., Ochi H., Hayes C.N., Abe H., Yoshima T., Aikata H., Ikeda K., Kumada H., Toyota J., Morizono T., et al. Variation in the DEPDC5 locus is associated with progression to hepatocellular carcinoma in chronic hepatitis C virus carriers. Nat. Genet. 2011;43:797–800. doi: 10.1038/ng.876. [DOI] [PubMed] [Google Scholar]
- 93.Lonardo A., Mantovani A., Lugari S., Targher G. NAFLD in Some Common Endocrine Diseases: Prevalence, Pathophysiology, and Principles of Diagnosis and Management. Int. J. Mol. Sci. 2019;20:2841. doi: 10.3390/ijms20112841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Antonelli A., Ferri C., Pampana A., Fallahi P., Nesti C., Pasquini M., Marchi S., Ferrannini E. Thyroid disorders in chronic hepatitis C. Am. J. Med. 2004;117:10–13. doi: 10.1016/j.amjmed.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 95.Hassan M.M., Kaseb A., Li D., Patt Y.Z., Vauthey J.-N., Thomas M.B., Curley S.A., Spitz M.R., Sherman S.I., Abdalla E.K., et al. Association between hypothyroidism and hepatocellular carcinoma: A case-control study in the United States. Hepatology. 2009;49:1563–1570. doi: 10.1002/hep.22793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lonardo A., Ballestri S., Mantovani A., Nascimbeni F., Lugari S., Targher G. Pathogenesis of hypothyroidism-induced NAFLD: Evidence for a distinct disease entity? Dig. Liver Dis. 2019;51:462–470. doi: 10.1016/j.dld.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 97.Pinter M., Haupt L., Hucke F., Bota S., Bucsics T., Trauner M., Peck-Radosavljevic M., Sieghart W. The impact of thyroid hormones on patients with hepatocellular carcinoma. PLoS ONE. 2017;12:e0181878. doi: 10.1371/journal.pone.0181878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Huang P.-S., Lin Y.-H., Chi H.-C., Hsiang-Cheng C., Huang Y.-H., Yeh C.-T., Kwang-Huei L., Lin K.-H. Thyroid hormone inhibits growth of hepatoma cells through induction of miR-214. Sci. Rep. 2017;7:1–11. doi: 10.1038/s41598-017-14864-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Laurent–Puig P., Legoix P., Bluteau O., Belghiti J., Franco D., Binot F., Monges G., Thomas G., Bioulac–Sage P., Zucman-Rossi J. Genetic alterations associated with hepatocellular carcinomas define distinct pathways of hepatocarcinogenesis. Gastroenterology. 2001;120:1763–1773. doi: 10.1053/gast.2001.24798. [DOI] [PubMed] [Google Scholar]
- 100.Yeh S.-H., Chen P.-J. Gender Disparity of Hepatocellular Carcinoma: The Roles of Sex Hormones. Oncology. 2010;78:172–179. doi: 10.1159/000315247. [DOI] [PubMed] [Google Scholar]
- 101.Wu M.-H., Ma W.-L., Hsu C.-L., Chen Y.-L., Ou J.-H.J., Ryan C.K., Hung Y.-C., Yeh S., Chang C. Androgen Receptor Promotes Hepatitis B Virus-Induced Hepatocarcinogenesis Through Modulation of Hepatitis B Virus RNA Transcription. Sci. Transl. Med. 2010;2:32ra35. doi: 10.1126/scitranslmed.3001143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ma C.-L., Hsu C., Wu M., Wu C., Wu C., Lai J., Jou Y., Cheng-Lung H., Yeh S., Chang C. Androgen Receptor Is a New Potential Therapeutic Target for the Treatment of Hepatocellular Carcinoma. Gastroenterology. 2008;135:947–955.e5. doi: 10.1053/j.gastro.2008.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kanda T., Yokosuka O. The androgen receptor as an emerging target in hepatocellular carcinoma. J. Hepatocell. Carcinoma. 2015;2:91–99. doi: 10.2147/JHC.S48956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Shimizu I. Impact of oestrogens on the progression of liver disease. Liver Int. 2003;23:63–69. doi: 10.1034/j.1600-0676.2003.00811.x. [DOI] [PubMed] [Google Scholar]
- 105.McGlynn K.A., Sahasrabuddhe V.V., Campbell P.T., Graubard B.I., Chen J., Schwartz L.M., Petrick J.L., Alavanja M.C., Andreotti G., Boggs D.A., et al. Reproductive factors, exogenous hormone use and risk of hepatocellular carcinoma among US women: Results from the Liver Cancer Pooling Project. Br. J. Cancer. 2015;112:1266–1272. doi: 10.1038/bjc.2015.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hsia C.-Y., Huo T.-I., Chiang S.-Y., Lu M.-F., Sun C.-L., Wu J.-C., Lee P.-C., Chi C.-W., Lui W.-Y., Lee S.-D. Evaluation of interleukin-6, interleukin-10 and human hepatocyte growth factor as tumor markers for hepatocellular carcinoma. Eur. J. Surg. Oncol. 2007;33:208–212. doi: 10.1016/j.ejso.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 107.Naugler W.E., Sakurai T., Kim S., Maeda S., Kim K., Elsharkawy A.M., Karin M. Gender Disparity in Liver Cancer Due to Sex Differences in MyD88-Dependent IL-6 Production. Science. 2007;317:121–124. doi: 10.1126/science.1140485. [DOI] [PubMed] [Google Scholar]
- 108.He G., Yu G.-Y., Temkin V., Ogata H., Kuntzen C., Sakurai T., Sieghart W., Peck-Radosavljevic M., Leffert H.L., Karin M. Hepatocyte IKKβ/NF-κB Inhibits Tumor Promotion and Progression by Preventing Oxidative Stress-Driven STAT3 Activation. Cancer Cell. 2010;17:286–297. doi: 10.1016/j.ccr.2009.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Calvisi D.F. Dr. Jekyll and Mr. Hyde: A paradoxical oncogenic and tumor suppressive role of signal transducer and activator of transcription 3 in liver cancer. Hepatology. 2011;54:9–12. doi: 10.1002/hep.24435. [DOI] [PubMed] [Google Scholar]
- 110.Edamoto Y., Hara A., Biernat W., Terracciano L., Cathomas G., Riehle H.-M., Matsuda M., Fujii H., Scoazec J.-Y., Ohgaki H. Alterations of RB1, p53 and Wnt pathways in hepatocellular carcinomas associated with hepatitis C, hepatitis B and alcoholic liver cirrhosis. Int. J. Cancer. 2003;106:334–341. doi: 10.1002/ijc.11254. [DOI] [PubMed] [Google Scholar]
- 111.Murakami Y., Hayashi K., Hirohashi S., Sekiya T. Aberrations of the tumor suppressor p53 and retinoblastoma genes in human hepatocellular carcinomas. Cancer Res. 1991;51:5520–5525. [PubMed] [Google Scholar]
- 112.Liew C.T., Li H.-M., Lo K.-W., Leow C.K., Chan J.Y., Hin L.Y., Lau W.Y., Lai P.B.S., Lim B.K., Huang J., et al. High frequency of p16INK4A gene alterations in hepatocellular carcinoma. Oncogene. 1999;18:789–795. doi: 10.1038/sj.onc.1202359. [DOI] [PubMed] [Google Scholar]
- 113.De Souza A.T., Hankins G.R., Washington M.K., Orton T.C., Jirtle R.L. M6P/IGF2R gene is mutated in human hepatocellular carcinomas with loss of heterozygosity. Nat. Genet. 1995;11:447–449. doi: 10.1038/ng1295-447. [DOI] [PubMed] [Google Scholar]
- 114.Shang S., Hua F., Hu Z.-W. The regulation of β-catenin activity and function in cancer: Therapeutic opportunities. Oncotarget. 2017;8:33972–33989. doi: 10.18632/oncotarget.15687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wong C.M., Fan S.T., Ng I.O.L. β-catenin mutation and overexpression in hepatocellular carcinoma. Cancer. 2001;92:136–145. doi: 10.1002/1097-0142(20010701)92:1<136::AID-CNCR1301>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 116.Wang X.W., Forrester K., Yeh H., Feitelson M.A., Gu J.R., Harris C.C. Hepatitis B virus X protein inhibits p53 sequence-specific DNA binding, transcriptional activity, and association with transcription factor ERCC3. Proc. Natl. Acad. Sci. USA. 1994;91:2230–2234. doi: 10.1073/pnas.91.6.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ji J., Wang X.W. New kids on the block: Diagnostic and prognostic microRNAs in hepatocellular carcinoma. Cancer Biol. Ther. 2009;8:1683–1690. doi: 10.4161/cbt.8.18.8898. [DOI] [PubMed] [Google Scholar]
- 118.Ji J., Yamashita T., Budhu A., Forgues M., Jia H.-L., Li C., Deng C., Wauthier E., Reid L.M., Ye Q.-H., et al. Identification of microRNA-181 by genome-wide screening as a critical player in EpCAM-positive hepatic cancer stem cells. Hepatology. 2009;50:472–480. doi: 10.1002/hep.22989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gong J., He X.-X., Tian D.-A. Emerging role of microRNA in hepatocellular carcinoma (Review) Oncol. Lett. 2015;9:1027–1033. doi: 10.3892/ol.2014.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kojima K., Takata A., Vadnais C., Otsuka M., Yoshikawa T., Akanuma M., Kondo Y., Kang Y.J., Kishikawa T., Kato N., et al. MicroRNA122 is a key regulator of α-fetoprotein expression and influences the aggressiveness of hepatocellular carcinoma. Nat. Commun. 2011;2:338. doi: 10.1038/ncomms1345. [DOI] [PubMed] [Google Scholar]
- 121.Lee J.-S., Chu I.-S., Heo J., Calvisi D.F., Sun Z., Roskams T., Durnez A., Demetris A.J., Thorgeirsson S.S. Classification and prediction of survival in hepatocellular carcinoma by gene expression profiling. Hepatology. 2004;40:667–676. doi: 10.1002/hep.20375. [DOI] [PubMed] [Google Scholar]
- 122.Coulouarn C., Factor V.M., Thorgeirsson S.S. Transforming growth factor-β gene expression signature in mouse hepatocytes predicts clinical outcome in human cancer. Hepatology. 2008;47:2059–2067. doi: 10.1002/hep.22283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kaposi-Novak P., Lee J.-S., Gòmez-Quiroz L., Coulouarn C., Factor V.M., Thorgeirsson S.S. Met-regulated expression signature defines a subset of human hepatocellular carcinomas with poor prognosis and aggressive phenotype. J. Clin. Investig. 2006;116:1582–1595. doi: 10.1172/JCI27236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Goossens N., Sun X., Hoshida Y. Molecular classification of hepatocellular carcinoma: Potential therapeutic implications. Hepatic Oncol. 2015;2:371–379. doi: 10.2217/hep.15.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu M., Jiang L., Guan X.-Y. The genetic and epigenetic alterations in human hepatocellular carcinoma: A recent update. Protein Cell. 2014;5:673–691. doi: 10.1007/s13238-014-0065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hoshida Y., Nijman S.M., Kobayashi M., Chan J.A., Brunet J.-P., Chiang D.Y., Villanueva A., Newell P., Ikeda K., Hashimoto M., et al. Integrative Transcriptome Analysis Reveals Common Molecular Subclasses of Human Hepatocellular Carcinoma. Cancer Res. 2009;69:7385–7392. doi: 10.1158/0008-5472.CAN-09-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lachenmayer A., Alsinet C., Savic R., Cabellos L., Toffanin S., Hoshida Y., Villanueva A., Minguez B., Newell P., Tsai H.W., et al. Wnt-pathway activation in two molecular classes of hepatocellular carcinoma and experimental modulation by sorafenib. Clin. Cancer Res. 2012;18:4997–5007. doi: 10.1158/1078-0432.CCR-11-2322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zucman-Rossi J., Villanueva A., Nault J.-C., Llovet J.M. Genetic Landscape and Biomarkers of Hepatocellular Carcinoma. Gastroenterology. 2015;149:1226–1239.e4. doi: 10.1053/j.gastro.2015.05.061. [DOI] [PubMed] [Google Scholar]
- 129.Castven D., Fischer M., Becker D., Heinrich S., Andersen J.B., Strand D., Sprinzl M.F., Strand S., Czauderna C., Heilmann-Heimbach S., et al. Adverse genomic alterations and stemness features are induced by field cancerization in the microenvironment of hepatocellular carcinomas. Oncotarget. 2017;8:48688–48700. doi: 10.18632/oncotarget.16231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Elsharkawy A.M., Mann D.A. Nuclear factor-κB and the hepatic inflammation-fibrosis-cancer axis. Hepatology. 2007;46:590–597. doi: 10.1002/hep.21802. [DOI] [PubMed] [Google Scholar]
- 131.Shimoda M., Mellody K.T., Orimo A. Carcinoma-associated fibroblasts are a rate-limiting determinant for tumour progression. Semin. Cell Dev. Biol. 2010;21:19–25. doi: 10.1016/j.semcdb.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lau E.Y.T., Lo J., Cheng B.Y.L., Ma M.K.F., Lee J.M.F., Ng J.K.Y., Chai S., Lin C.H., Tsang S.Y., Ma S., et al. Cancer-associated fibroblasts regulate tumor-initiating cell plasticity in hepatocellular carcinoma through c-Met/FRA1/HEY1 signaling. Cell Rep. 2016;15:1175–1189. doi: 10.1016/j.celrep.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 133.Faouzi S., Lepreux S., Bedin C., Dubuisson L., Balabaud C., Bioulac-Sage P., Desmoulière A., Rosenbaum J. Activation of cultured rat hepatic stellate cells by tumoral hepatocytes. Lab. Investig. 1999;79:485–493. [PubMed] [Google Scholar]
- 134.Noy R., Pollard J.W. Tumor-associated macrophages: From mechanisms to therapy. Immunity. 2014;41:49–61. doi: 10.1016/j.immuni.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mantovani A., Bottazzi B., Colotta F., Sozzani S., Ruco L.P. The origin and function of tumor-associated macrophages. Immunol. Today. 1992;13:265–270. doi: 10.1016/0167-5699(92)90008-U. [DOI] [PubMed] [Google Scholar]
- 136.Llovet J.M., Schwartz M., Mazzaferro V. Resection and Liver Transplantation for Hepatocellular Carcinoma. Semin. Liver Dis. 2005;25:181–200. doi: 10.1055/s-2005-871198. [DOI] [PubMed] [Google Scholar]
- 137.Hoshida Y., Villanueva A., Kobayashi M., Peix J., Chiang D.Y., Camargo A., Gupta S., Moore J., Wrobel M.J., Lerner J., et al. Gene Expression in Fixed Tissues and Outcome in Hepatocellular Carcinoma. N. Engl. J. Med. 2008;359:1995–2004. doi: 10.1056/NEJMoa0804525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hoshida Y., Villanueva A., SanGiovanni A., Sole M., Hur C., Andersson K.L., Chung R.T., Gould J., Kojima K., Gupta S., et al. Prognostic Gene Expression Signature for Patients with Hepatitis C–Related Early-Stage Cirrhosis. Gastroenterology. 2013;144:1024–1030. doi: 10.1053/j.gastro.2013.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nakagawa S., Wei L., Song W.M., Higashi T., Ghoshal S., Kim R.S., Bian C.B., Yamada S., Sun X., Venkatesh A., et al. Molecular Liver Cancer Prevention in Cirrhosis by Organ Transcriptome Analysis and Lysophosphatidic Acid Pathway Inhibition. Cancer Cell. 2016;30:879–890. doi: 10.1016/j.ccell.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Fuchs B.C., Hoshida Y., Fujii T., Wei L., Yamada S., Lauwers G.Y., McGinn C.M., Deperalta D.K., Chen X., Kuroda T., et al. Epidermal growth factor receptor inhibition attenuates liver fibrosis and development of hepatocellular carcinoma. Hepatology. 2014;59:1577–1590. doi: 10.1002/hep.26898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Burra P., Rodriguez-Castro K.I. Neoplastic disease after liver transplantation: Focus onde novoneoplasms. World J. Gastroenterol. 2015;21:8753. doi: 10.3748/wjg.v21.i29.8753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kihara Y., Mizuno H., Chun J. Lysophospholipid receptors in drug discovery. Exp. Cell Res. 2015;333:171–177. doi: 10.1016/j.yexcr.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sakai N., Chun J., Duffield J.S., Wada T., Luster A.D., Tager A.M. LPA 1 -induced cytoskeleton reorganization drives fibrosis through CTGF-dependent fibroblast proliferation. FASEB J. 2013;27:1830–1846. doi: 10.1096/fj.12-219378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hoshida Y., Toffanin S., Lachenmayer A., Villanueva A., Minguez B., Llovet J.M. Molecular Classification and Novel Targets in Hepatocellular Carcinoma: Recent Advancements. Semin. Liver Dis. 2010;30:35–51. doi: 10.1055/s-0030-1247131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jühling F., Hamdane N., Crouchet E., Li S., El Saghire H., Mukherji A., Fujiwara N., Oudot M.A., Thumann C., Saviano A., et al. Targeting clinical epigenetic reprogramming for chemoprevention of metabolic and viral hepatocellular carcinoma. Gut. 2020 doi: 10.1136/gutjnl-2019-318918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Villa E., Critelli R., Lei B., Marzocchi G., Cammà C., Giannelli G., Pontisso P., Cabibbo G., Enea M., Colopi S., et al. Neoangiogenesis-related genes are hallmarks of fast-growing hepatocellular carcinomas and worst survival. Results from a prospective study. Gut. 2015;65:861–869. doi: 10.1136/gutjnl-2014-308483. [DOI] [PubMed] [Google Scholar]
- 147.Zanetti A.R., Van Damme P., Shouval D. The global impact of vaccination against hepatitis B: A historical overview. Vaccine. 2008;26:6266–6273. doi: 10.1016/j.vaccine.2008.09.056. [DOI] [PubMed] [Google Scholar]
- 148.Ni Y.-H., Chang M.-H., Huang L.-M., Chen H.-L., Hsu H.-Y., Chiu T.-Y., Tsai K.-S., Chen D.-S. Hepatitis B Virus Infection in Children and Adolescents in a Hyperendemic Area: 15 Years after Mass Hepatitis B Vaccination. Ann. Intern. Med. 2001;135:796–800. doi: 10.7326/0003-4819-135-9-200111060-00009. [DOI] [PubMed] [Google Scholar]
- 149.Chen C.-H., Yang P.-M., Huang G.-T., Lee H.-S., Sung J.-L., Sheu J.-C. Estimation of Seroprevalence of Hepatitis B Virus and Hepatitis C Virus in Taiwan from a Large-scale Survey of Free Hepatitis Screening Participants. J. Formos. Med. Assoc. 2007;106:148–155. doi: 10.1016/S0929-6646(09)60231-X. [DOI] [PubMed] [Google Scholar]
- 150.Aitken C., Lewis J., Hocking J., Bowden D., Hellard M. Does information about IDUs’ injecting networks predict exposure to the hepatitis C virus? Hepat Monthly. 2009;9:17–23. [Google Scholar]
- 151.Razali K., Thein H.-H., Bell J., Cooper-Stanbury M., Dolan K., Dore G., George J., Kaldor J., Karvelas M., Li J., et al. Modelling the hepatitis C virus epidemic in Australia. Drug Alcohol Depend. 2007;91:228–235. doi: 10.1016/j.drugalcdep.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 152.Azziz-Baumgartner E., Lindblade K., Gieseker K., Rogers H.S., Kieszak S., Njapau H., Schleicher R., McCoy L.F., Misore A., Decock K., et al. Case–Control Study of an Acute Aflatoxicosis Outbreak, Kenya, 2004. Environ. Heal. Perspect. 2005;113:1779–1783. doi: 10.1289/ehp.8384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Luedde T., Schwabe R.F. NF-κB in the liver—Linking injury, fibrosis and hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2011;8:108–118. doi: 10.1038/nrgastro.2010.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ikeda K., Arase Y., Saitoh S., Kobayashi M., Suzuki Y., Suzuki F., Tsubota A., Chayama K., Murashima N., Kumada H. Interferon beta prevents recurrence of hepatocellular carcinoma after complete resection or ablation of the primary tumor—A prospective randomized study of hepatitis C virus–related liver cancer. Hepatology. 2000;32:228–232. doi: 10.1053/jhep.2000.9409. [DOI] [PubMed] [Google Scholar]
- 155.Mazzaferro V., Romito R., Schiavo M., Mariani L., Camerini T., Bhoori S., Capussotti L., Calise F., Pellicci R., Belli G., et al. Prevention of hepatocellular carcinoma recurrence with alpha-interferon after liver resection in HCV cirrhosis. Hepatology. 2006;44:1543–1554. doi: 10.1002/hep.21415. [DOI] [PubMed] [Google Scholar]
- 156.Chinnakotla S., Davis G.L., Vasani S., Kim P., Tomiyama K., Sanchez E., Onaca N., Goldstein R., Levy M., Klintmalm G.B. Impact of sirolimus on the recurrence of hepatocellular carcinoma after liver transplantation. Liver Transplant. 2009;15:1834–1842. doi: 10.1002/lt.21953. [DOI] [PubMed] [Google Scholar]
- 157.Toso C., Merani S., Bigam D.L., Shapiro A.J., Kneteman N.M. Sirolimus-based immunosuppression is associated with increased survival after liver transplantation for hepatocellular carcinoma. Hepatology. 2010;51:1237–1243. doi: 10.1002/hep.23437. [DOI] [PubMed] [Google Scholar]
- 158.Costentin C., Layese R., Bourcier V., Cagnot C., Marcellin P., Guyader D., Pol S., Larrey D., De Lédinghen V., Ouzan D., et al. Compliance with Hepatocellular Carcinoma Surveillance Guidelines Associated With Increased Lead-Time Adjusted Survival of Patients With Compensated Viral Cirrhosis: A Multi-Center Cohort Study. Gastroenterology. 2018;155:431–442.e10. doi: 10.1053/j.gastro.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 159.Galle P.R., Forner A., Llovet J.M., Mazzaferro V., Piscaglia F., Raoul J.-L., Schirmacher P., Vilgrain V. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 160.Heimbach J.K., Kulik L.M., Finn R.S., Sirlin C.B., Abecassis M.M., Roberts L.R., Zhu A.X., Murad M.H., Marrero J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358–380. doi: 10.1002/hep.29086. [DOI] [PubMed] [Google Scholar]
- 161.Ganne-Carrié N., Layese R., Bourcier V., Cagnot C., Marcellin P., Guyader D., Pol S., Larrey D., De Lédinghen V., Ouzan D., et al. Nomogram for individualized prediction of hepatocellular carcinoma occurrence in hepatitis C virus cirrhosis (ANRS CO12 CirVir) Hepatology. 2016;64:1136–1147. doi: 10.1002/hep.28702. [DOI] [PubMed] [Google Scholar]
- 162.Lok A.S., Seeff L.B., Morgan T.R., Di Bisceglie A.M., Sterling R.K., Curto T.M., Everson G.T., Lindsay K.L., Lee W.M., Bonkovsky H.L., et al. Incidence of Hepatocellular Carcinoma and Associated Risk Factors in Hepatitis C-Related Advanced Liver Disease. Gastroenterology. 2009;136:138–148. doi: 10.1053/j.gastro.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Flemming J.A., Yang J.D., Vittinghoff E., Kim W.R., Terrault N.A. Risk prediction of hepatocellular carcinoma in patients with cirrhosis: The ADRESS-HCC risk model. Cancer. 2014;120:3485–3493. doi: 10.1002/cncr.28832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Abu Dayyeh B.K., Yang M., Fuchs B.C., Karl D.L., Yamada S., Sninsky J.J., O’Brien T.R., Dienstag J.L., Tanabe K.K., Chung R.T. A Functional Polymorphism in the Epidermal Growth Factor Gene Is Associated with Risk for Hepatocellular Carcinoma. Gastroenterology. 2011;141:141–149. doi: 10.1053/j.gastro.2011.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ioannou G.N., Green P., Kerr K.F., Berry K. Models estimating risk of hepatocellular carcinoma in patients with alcohol or NAFLD-related cirrhosis for risk stratification. J. Hepatol. 2019;71:523–533. doi: 10.1016/j.jhep.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mancebo A., González-Diéguez M.L., Navascués C.A., Cadahía V., Varela M., Pérez R., Rodrigo L., Rodríguez M. Adherence to a Semiannual Surveillance Program for Hepatocellular Carcinoma in Patients With Liver Cirrhosis. J. Clin. Gastroenterol. 2017;51:557–563. doi: 10.1097/MCG.0000000000000734. [DOI] [PubMed] [Google Scholar]
- 167.Davila J.A., Henderson L., Kramer J.R., Kanwal F., Richardson P.A., Duan Z., El-Serag H.B. Utilization of Surveillance for Hepatocellular Carcinoma Among Hepatitis C Virus–Infected Veterans in the United States. Ann. Intern. Med. 2011;154:85–93. doi: 10.7326/0003-4819-154-2-201101180-00006. [DOI] [PubMed] [Google Scholar]
- 168.Harris P.S., Hansen R.M., Gray M.E., Massoud O.I., McGuire B.M., Shoreibah M.G. Hepatocellular carcinoma surveillance: An evidence-based approach. World J. Gastroenterol. 2019;25:1550–1559. doi: 10.3748/wjg.v25.i13.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Kim S.Y., Sang L.Y., Lim Y.-S., Han S., Lee J.-Y., Byun J.H., Won H.J., Lee S.J., Lee H.C., Lee Y.S. MRI With Liver-Specific Contrast for Surveillance of Patients with Cirrhosis at High Risk of Hepatocellular Carcinoma. JAMA Oncol. 2017;3:456–463. doi: 10.1001/jamaoncol.2016.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lin S.-M., Sheen I.-S., Chien R.-N., Chu C.-M., Liaw Y.-F. Long-term beneficial effect of interferon therapy in patients with chronic hepatitis B virus infection. Hepatology. 1999;29:971–975. doi: 10.1002/hep.510290312. [DOI] [PubMed] [Google Scholar]
- 171.Lin S.-M., Yu M.-L., Lee C.-M., Chien R.-N., Sheen I.-S., Chu C.-M., Liaw Y.-F. Interferon therapy in HBeAg positive chronic hepatitis reduces progression to cirrhosis and hepatocellular carcinoma. J. Hepatol. 2007;46:45–52. doi: 10.1016/j.jhep.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 172.Liaw Y.-F., Sung J.J., Chow W.C., Farrell G., Lee C.-Z., Yuen H., Tanwandee T., Tao Q.-M., Shue K., Keene O.N., et al. Lamivudine for Patients with Chronic Hepatitis B and Advanced Liver Disease. N. Engl. J. Med. 2004;351:1521–1531. doi: 10.1056/NEJMoa033364. [DOI] [PubMed] [Google Scholar]
- 173.Eun J.R., Lee H.J., Kim T.N., Lee K.S. Risk assessment for the development of hepatocellular carcinoma: According to on-treatment viral response during long-term lamivudine therapy in hepatitis B virus-related liver disease. J. Hepatol. 2010;53:118–125. doi: 10.1016/j.jhep.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 174.Papatheodoridis G.V., Lampertico P., Manolakopoulos S., Lok A. Incidence of hepatocellular carcinoma in chronic hepatitis B patients receiving nucleos(t)ide therapy: A systematic review. J. Hepatol. 2010;53:348–356. doi: 10.1016/j.jhep.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 175.Webster D.P., Klenerman P., Dusheiko G.M. Hepatitis C. Lancet. 2015;385:1124–1135. doi: 10.1016/S0140-6736(14)62401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Morgan R.L., Baack B., Smith B.D., Yartel A., Pitasi M., Falck-Ytter Y. Eradication of Hepatitis C Virus Infection and the Development of Hepatocellular Carcinoma. Ann. Intern. Med. 2013;158:329–337. doi: 10.7326/0003-4819-158-5-201303050-00005. [DOI] [PubMed] [Google Scholar]
- 177.Guarino M., Sessa A., Cossiga V., Morando F., Caporaso N., Morisco F. Direct-acting antivirals and hepatocellular carcinoma in chronic hepatitis C: A few lights and many shadows. World J. Gastroenterol. 2018;24:2582–2595. doi: 10.3748/wjg.v24.i24.2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Pearlman B.L., Traub N. Sustained Virologic Response to Antiviral Therapy for Chronic Hepatitis C Virus Infection: A Cure and So Much More. Clin. Infect. Dis. 2011;52:889–900. doi: 10.1093/cid/cir076. [DOI] [PubMed] [Google Scholar]
- 179.Janjua N.Z., Wong S., Darvishian M., Butt Z.A., Yu A., Binka M., Alvarez M., Woods R., Yoshida E.M., Ramji A., et al. The impact of SVR from direct-acting antiviral- and interferon-based treatments for HCV on hepatocellular carcinoma risk. J. Viral Hepat. 2020;27:781–793. doi: 10.1111/jvh.13295. [DOI] [PubMed] [Google Scholar]
- 180.Ioannou G.N., Green P.K., Berry K. HCV eradication induced by direct-acting antiviral agents reduces the risk of hepatocellular carcinoma. J. Hepatol. 2018;68:25–32. doi: 10.1016/j.jhep.2017.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ioannou G.N., Beste L.A., Green P.K., Singal A.G., Tapper E.B., Waljee A.K., Sterling R.K., Feld J.J., Kaplan D.E., Taddei T.H., et al. Increased Risk for Hepatocellular Carcinoma Persists Up to 10 Years after HCV Eradication in Patients with Baseline Cirrhosis or High FIB-4 Scores. Gastroenterology. 2019;157:1264–1278.e4. doi: 10.1053/j.gastro.2019.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hamdane N., Jühling F., Crouchet E., El Saghire H., Thumann C., Oudot M.A., Bandiera S., Saviano A., Ponsolles C., Suarez A.A.R., et al. HCV-Induced Epigenetic Changes Associated with Liver Cancer Risk Persist After Sustained Virologic Response. Gastroenterology. 2019;156:2313–2329.e7. doi: 10.1053/j.gastro.2019.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Volk M.L., Tocco R., Saini S., Lok A.S.-F. Public health impact of antiviral therapy for hepatitis C in the United States. Hepatology. 2009;50:1750–1755. doi: 10.1002/hep.23220. [DOI] [PubMed] [Google Scholar]
- 184.McGowan C.E., Fried M.W. Barriers to hepatitis C treatment. Liver Int. 2012;32:151–156. doi: 10.1111/j.1478-3231.2011.02706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Crowley D., Cullen W., Laird E., Lambert J.S., Mc Hugh T., Murphy C., Van Hout M.C. Exploring patient characteristics and barriers to Hepatitis C treatment in patients on opioid substitution treatment attending a community based fibro-scanning clinic. J. Transl. Intern. Med. 2017;5:112–119. doi: 10.1515/jtim-2017-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Romero-Gómez M., Zelber-Sagi S., Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J. Hepatol. 2017;67:829–846. doi: 10.1016/j.jhep.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 187.Pälve K., Pahkala K., Suomela E., Aatola H., Hulkkonen J., Juonala M., Lehtimäki T., Rönnemaa T., Viikari J.S.A., Kähönen M., et al. Cardiorespiratory Fitness and Risk of Fatty Liver. Med. Sci. Sports Exerc. 2017;49:1834–1841. doi: 10.1249/MSS.0000000000001288. [DOI] [PubMed] [Google Scholar]
- 188.Byrne C.D., Targher G. EASL–EASD–EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease: Is universal screening appropriate? Diabetologia. 2016;59:1141–1144. doi: 10.1007/s00125-016-3910-y. [DOI] [PubMed] [Google Scholar]
- 189.Chalasani N., Younossi Z., LaVine J.E., Charlton M., Cusi K., Rinella M., Harrison S.A., Brunt E.M., Sanyal A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 190.Piguet A.-C., Saran U., Simillion C.A.M., Keller I., Terracciano L., Reeves H.L., Dufour J.-F.F. Regular exercise decreases liver tumors development in hepatocyte-specific PTEN-deficient mice independently of steatosis. J. Hepatol. 2015;62:1296–1303. doi: 10.1016/j.jhep.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 191.Lassailly G., Caiazzo R., Buob D., Pigeyre M., Verkindt H., Labreuche J., Raverdy V., Leteurtre E., Dharancy S., Louvet A., et al. Bariatric Surgery Reduces Features of Nonalcoholic Steatohepatitis in Morbidly Obese Patients. Gastroenterology. 2015;149:379–388. doi: 10.1053/j.gastro.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 192.Mummadi R.R., Kasturi K.S., Chennareddygari S., Sood G.K. Effect of Bariatric Surgery on Nonalcoholic Fatty Liver Disease: Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2008;6:1396–1402. doi: 10.1016/j.cgh.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 193.Kwak M., Mehaffey J.H., Hawkins R.B., Hsu A., Schirmer B., Hallowell P.T. Bariatric surgery is associated with reduction in non-alcoholic steatohepatitis and hepatocellular carcinoma: A propensity matched analysis. Am. J. Surg. 2020;219:504–507. doi: 10.1016/j.amjsurg.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 194.Singh M.K., Das B.K., Choudhary S., Gupta D., Patil U.K. Diabetes and hepatocellular carcinoma: A pathophysiological link and pharmacological management. Biomed. Pharmacother. 2018;106:991–1002. doi: 10.1016/j.biopha.2018.06.095. [DOI] [PubMed] [Google Scholar]
- 195.Chou C.K., Ho L.T., Ting L.P., Hu C.P., Su T.S., Chang W.C., Suen C.S., Huang M.Y., Chang C.M. Selective suppression of insulin-induced proliferation of cultured human hepatoma cells by somatostatin. J. Clin. Investig. 1987;79:175–178. doi: 10.1172/JCI112780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Paradis V., Perlemuter G., Bonvoust F., Dargere D., Parfait B., Vidaud M., Conti M., Huet S., Bâ N., Buffet C., et al. High glucose and hyperinsulinemia stimulate connective tissue growth factor expression: A potential mechanism involved in progression to fibrosis in nonalcoholic steatohepatitis. Hepatology. 2001;34:738–744. doi: 10.1053/jhep.2001.28055. [DOI] [PubMed] [Google Scholar]
- 197.Evans J.M., Donnelly L.A., Emslie-Smith A.M., Alessi D.R., Morris A.D. Metformin and reduced risk of cancer in diabetic patients. BMJ. 2005;330:1304–1305. doi: 10.1136/bmj.38415.708634.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Tseng C.-H. Metformin and risk of hepatocellular carcinoma in patients with type 2 diabetes. Liver Int. 2018;38:2018–2027. doi: 10.1111/liv.13872. [DOI] [PubMed] [Google Scholar]
- 199.Zhou G., Myers R., Li Y., Chen Y., Shen X., Fenyk-Melody J., Wu M., Ventre J., Doebber T., Fujii N., et al. Role of AMP-activated protein kinase in mechanism of metformin action. J. Clin. Investig. 2001;108:1167–1174. doi: 10.1172/JCI13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Zheng L., Yang W., Wu F., Wang C., Yu L., Tang L., Qiu B., Li Y., Guo L., Wu M., et al. Prognostic Significance of AMPK Activation and Therapeutic Effects of Metformin in Hepatocellular Carcinoma. Clin. Cancer Res. 2013;19:5372–5380. doi: 10.1158/1078-0432.CCR-13-0203. [DOI] [PubMed] [Google Scholar]
- 201.Deperalta D.K., Wei L., Ghoshal S., Schmidt B., Lauwers G.Y., Lanuti M., Chung R.T., Tanabe K.K., Fuchs B.C. Metformin prevents hepatocellular carcinoma development by suppressing hepatic progenitor cell activation in a rat model of cirrhosis. Cancer. 2016;122:1216–1227. doi: 10.1002/cncr.29912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cusi K., Orsak B., Bril F., Lomonaco R., Hecht J., Ortiz-Lopez C., Tio F., Hardies J., Darland C., Musi N., et al. Long-Term Pioglitazone Treatment for Patients with Nonalcoholic Steatohepatitis and Prediabetes or Type 2 Diabetes Mellitus. Ann. Intern. Med. 2016;165:305–315. doi: 10.7326/M15-1774. [DOI] [PubMed] [Google Scholar]
- 203.Li S., Ghoshal S., Sojoodi M., Arora G., Masia R., Erstad D.J., Lanuti M., Hoshida Y., Baumert T.F., Tanabe K.K., et al. Pioglitazone Reduces Hepatocellular Carcinoma Development in Two Rodent Models of Cirrhosis. J. Gastrointest. Surg. 2018;23:101–111. doi: 10.1007/s11605-018-4004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Huang M.-Y., Chung C.-H., Chang W.-K., Lin C.-S., Chen K.-W., Hsieh T.-Y., Chien W.-C., Lin H.-H. The role of thiazolidinediones in hepatocellular carcinoma risk reduction: A population-based cohort study in Taiwan. Am. J. Cancer Res. 2017;7:1606–1616. [PMC free article] [PubMed] [Google Scholar]
- 205.Hasegawa T., Yoneda M., Nakamura K., Makino I., Terano A. Plasma transforming growth factor-β1 level and efficacy of α-tocopherol in patients with non-alcoholic steatohepatitis: A pilot study. Aliment. Pharmacol. Ther. 2001;15:1667–1672. doi: 10.1046/j.1365-2036.2001.01083.x. [DOI] [PubMed] [Google Scholar]
- 206.Kugelmas M., Hill D.B., Vivian B., Marsano L., McClain C.J. Cytokines and NASH: A pilot study of the effects of lifestyle modification and vitamin E. Hepatology. 2003;38:413–419. doi: 10.1053/jhep.2003.50316. [DOI] [PubMed] [Google Scholar]
- 207.Vajro P., Mandato C., Franzese A., Ciccimarra E., Lucariello S., Savoia M., Capuano G., Migliaro F. Vitamin E Treatment in Pediatric Obesity-Related Liver Disease: A Randomized Study. J. Pediatr. Gastroenterol. Nutr. 2004;38:48–55. doi: 10.1097/00005176-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 208.Sanyal A.J., Chalasani N., Kowdley K.V., McCullough A., Diehl A.M., Bass N.M., Neuschwander-Tetri B.A., LaVine J.E., Tonascia J., Unalp A., et al. Pioglitazone, Vitamin E, or Placebo for Nonalcoholic Steatohepatitis. N. Engl. J. Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Miller E.R., Pastor-Barriuso R., Dalal D., Riemersma R.A., Appel L.J., Guallar E. Meta-analysis: High-dosage vitamin E supplementation may increase all-cause mortality. Ann. Intern. Med. 2005;142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 210.Klein E.A., Thompson I.M., Tangen C.M., Crowley J.J., Lucia M.S., Goodman P.J., Minasian L.M., Ford L.G., Parnes H.L., Gaziano J.M., et al. Vitamin E and the Risk of Prostate Cancer: The selenium and vitamin e cancer prevention trial (SELECT) JAMA. 2011;306:1549–1556. doi: 10.1001/jama.2011.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Testino G., Leone S., Borro P. Alcohol and hepatocellular carcinoma: A review and a point of view. World J. Gastroenterol. 2014;20:15943–15954. doi: 10.3748/wjg.v20.i43.15943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Addolorato G., Mirijello A., Barrio P., Gual A. Treatment of alcohol use disorders in patients with alcoholic liver disease. J. Hepatol. 2016;65:618–630. doi: 10.1016/j.jhep.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 213.Miller W.R., Walters S.T., Bennett M.E. How effective is alcoholism treatment in the United States? J. Stud. Alcohol. 2001;62:211–220. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- 214.Menon K.V.N., Gores G.J., Shah V.H. Pathogenesis, Diagnosis, and Treatment of Alcoholic Liver Disease. Mayo Clin. Proc. 2001;76:1021–1029. doi: 10.4065/76.10.1021. [DOI] [PubMed] [Google Scholar]
- 215.Humphreys K., Blodgett J.C., Wagner T.H. Estimating the Efficacy of Alcoholics Anonymous without Self-Selection Bias: An Instrumental Variables Re-Analysis of Randomized Clinical Trials. Alcohol. Clin. Exp. Res. 2014;38:2688–2694. doi: 10.1111/acer.12557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.McHugh R.K., Hearon B.A., Otto M.W. Cognitive Behavioral Therapy for Substance Use Disorders. Psychiatr. Clin. N. Am. 2010;33:511–525. doi: 10.1016/j.psc.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Harrison S.A., Torgerson S., Hayashi P., Ward J., Schenker S. Vitamin E and vitamin C treatment improves fibrosis in patients with nonalcoholic steatohepatitis. Am. J. Gastroenterol. 2003;98:2485–2490. doi: 10.1111/j.1572-0241.2003.08699.x. [DOI] [PubMed] [Google Scholar]
- 218.Jørgensen C.H., Pedersen B., Tønnesen H. The Efficacy of Disulfiram for the Treatment of Alcohol Use Disorder. Alcohol. Clin. Exp. Res. 2011;35:1749–1758. doi: 10.1111/j.1530-0277.2011.01523.x. [DOI] [PubMed] [Google Scholar]
- 219.Benjamin D., Grant E.R., Pohorecky L.A. Naltrexone reverses ethanol-induced dopamine release in the nucleus accumbens in awake, freely moving rats. Brain Res. 1993;621:137–140. doi: 10.1016/0006-8993(93)90309-B. [DOI] [PubMed] [Google Scholar]
- 220.Anton R.F., O’Malley S.S., Ciraulo D.A., Cisler R.A., Couper D., Donovan D.M., Gastfriend D.R., Hosking J.D., Johnson B.A., LoCastro J.S., et al. Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- 221.Cholesterol Treatment Trialists’ (CTT) Collaboration Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Poynter J.N., Gruber S.B., Higgins P.D., Almog R., Bonner J.D., Rennert H.S., Low M., Greenson J.K., Rennert G. Statins and the risk of colorectal cancer. N. Engl. J. Med. 2005;352:2184–2192. doi: 10.1056/NEJMoa043792. [DOI] [PubMed] [Google Scholar]
- 223.Campbell M.J., Esserman L.J., Zhou Y., Shoemaker M., Lobo M., Borman E., Baehner F., Kumar A.S., Adduci K., Marx C., et al. Breast Cancer Growth Prevention by Statins. Cancer Res. 2006;66:8707–8714. doi: 10.1158/0008-5472.CAN-05-4061. [DOI] [PubMed] [Google Scholar]
- 224.Shannon J., Tewoderos S., Garzotto M., Beer T.M., Derenick R., Palma A., Farris P.E. Statins and Prostate Cancer Risk: A Case-Control Study. Am. J. Epidemiol. 2005;162:318–325. doi: 10.1093/aje/kwi203. [DOI] [PubMed] [Google Scholar]
- 225.Hyogo H., Tazuma S., Arihiro K., Iwamoto K., Nabeshima Y., Inoue M., Ishitobi T., Nonaka M., Chayama K. Efficacy of atorvastatin for the treatment of nonalcoholic steatohepatitis with dyslipidemia. Metabolism. 2008;57:1711–1718. doi: 10.1016/j.metabol.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 226.Athyros V., Alexandrides T.K., Bilianou H., Cholongitas E., Doumas M., Ganotakis E., Goudevenos J., Elisaf M.S., Germanidis G., Giouleme O., et al. The use of statins alone, or in combination with pioglitazone and other drugs, for the treatment of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis and related cardiovascular risk. An Expert Panel Statement. Metabolism. 2017;71:17–32. doi: 10.1016/j.metabol.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 227.Tsan Y.-T., Lee C.-H., Wang J.-D., Chen P.-C. Statins and the Risk of Hepatocellular Carcinoma in Patients with Hepatitis B Virus Infection. J. Clin. Oncol. 2012;30:623–630. doi: 10.1200/JCO.2011.36.0917. [DOI] [PubMed] [Google Scholar]
- 228.Butt A.A., Yan P., Bonilla H., Abou-Samra A.B., Shaikh O.S., Simon T.G., Chung R.T., Rogal S.S., ERCHIVES (Electronically Retrieved Cohort of HCV Infected Veterans) Study Team Effect of addition of statins to antiviral therapy in hepatitis C virus-infected persons: Results from ERCHIVES. Hepatology. 2015;62:365–374. doi: 10.1002/hep.27835. [DOI] [PubMed] [Google Scholar]
- 229.Kawaguchi Y., Sakamoto Y., Ito D., Ito K., Arita J., Akamatsu N., Kaneko J., Hasegawa K., Moriya K., Kokudo N. Statin use is associated with a reduced risk of hepatocellular carcinoma recurrence after initial liver resection. Biosci. Trends. 2017;11:574–580. doi: 10.5582/bst.2017.01191. [DOI] [PubMed] [Google Scholar]
- 230.Cao Z., Fan-Minogue H., Bellovin D.I., Yevtodiyenko A., Arzeno J., Yang Q., Gambhir S.S., Felsher D.W. MYC phosphorylation, activation, and tumorigenic potential in hepatocellular carcinoma are regulated by HMG-CoA reductase. Cancer Res. 2011;71:2286–2297. doi: 10.1158/0008-5472.CAN-10-3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Roudier E., Mistafa O., Stenius U. Statins induce mammalian target of rapamycin (mTOR)-mediated inhibition of Akt signaling and sensitize p53-deficient cells to cytostatic drugs. Mol. Cancer Ther. 2006;5:2706–2715. doi: 10.1158/1535-7163.MCT-06-0352. [DOI] [PubMed] [Google Scholar]
- 232.Ghalali A., Martin-Renedo J., Högberg J., Stenius U. Atorvastatin Decreases HBx-Induced Phospho-Akt in Hepatocytes via P2X Receptors. Mol. Cancer Res. 2017;15:714–722. doi: 10.1158/1541-7786.MCR-16-0373. [DOI] [PubMed] [Google Scholar]
- 233.Wang J., Tokoro T., Higa S., Kitajima I. Anti-inflammatory Effect of Pitavastatin on NF-κB Activated by TNF-α in Hepatocellular Carcinoma Cells. Biol. Pharm. Bull. 2006;29:634–639. doi: 10.1248/bpb.29.634. [DOI] [PubMed] [Google Scholar]
- 234.Marinho T.D.S., Kawasaki A., Bryntesson M., Souza-Mello V., Barbosa-Da-Silva S., Aguila M.B., Mandarim-De-Lacerda C.A. Rosuvastatin limits the activation of hepatic stellate cells in diet-induced obese mice. Hepatol. Res. 2016;47:928–940. doi: 10.1111/hepr.12821. [DOI] [PubMed] [Google Scholar]
- 235.Uschner F.E., Ranabhat G., Choi S.S., Granzow M., Klein S., Schierwagen R., Raskopf E., Gautsch S., Van Der Ven P.F.M., Fürst D.O., et al. Statins activate the canonical hedgehog-signaling and aggravate non-cirrhotic portal hypertension, but inhibit the non-canonical hedgehog signaling and cirrhotic portal hypertension. Sci. Rep. 2015;5:14573. doi: 10.1038/srep14573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Pikarsky E., Porat R.M., Stein I., Abramovitch R., Amit S., Kasem S., Gutkovich-Pyest E., Urieli-Shoval S., Galun E., Ben-Neriah Y. NF-κB functions as a tumour promoter in inflammation-associated cancer. Nat. Cell Biol. 2004;431:461–466. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- 237.He G., Karin M. NF-κB and STAT3—Key players in liver inflammation and cancer. Cell Res. 2011;21:159–168. doi: 10.1038/cr.2010.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Sahasrabuddhe V.V., Gunja M.Z., Graubard B.I., Trabert B., Schwartz L.M., Park Y., Hollenbeck A.R., Freedman N.D., McGlynn K.A. Nonsteroidal Anti-inflammatory Drug Use, Chronic Liver Disease, and Hepatocellular Carcinoma. J. Natl. Cancer Inst. 2012;104:1808–1814. doi: 10.1093/jnci/djs452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Chen H., Cai W., Chu E.S.H., Tang J., Wong C.-C., Wong S.H., Sun W., Liang Q., Fang J., Sun Z., et al. Hepatic cyclooxygenase-2 overexpression induced spontaneous hepatocellular carcinoma formation in mice. Oncogene. 2017;36:4415–4426. doi: 10.1038/onc.2017.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Leng J., Han C., Demetris A.J., Michalopoulos G.K., Wu T. Cyclooxygenase-2 promotes hepatocellular carcinoma cell growth through Akt activation: Evidence for Akt inhibition in celecoxib-induced apoptosis. Hepatology. 2003;38:756–768. doi: 10.1053/jhep.2003.50380. [DOI] [PubMed] [Google Scholar]
- 241.Simon T.G., Ma Y., Ludvigsson J.F., Chong D.Q., Giovannucci E.L., Fuchs C.S., Meyerhardt J.A., Corey K.E., Chung R.T., Zhang X., et al. Association Between Aspirin Use and Risk of Hepatocellular Carcinoma. JAMA Oncol. 2018;4:1683–1690. doi: 10.1001/jamaoncol.2018.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Funaki M., Kitabayashi J., Shimakami T., Nagata N., Kai T., Takegoshi K., Okada H., Murai K., Shirasaki T., Oyama T., et al. Peretinoin, an acyclic retinoid, inhibits hepatocarcinogenesis by suppressing sphingosine kinase 1 expression in vitro and in vivo. Sci. Rep. 2017;7:16978. doi: 10.1038/s41598-017-17285-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Malehmir M., Pfister D., Gallage S., Szydlowska M., Inverso D., Kotsiliti E., Leone V., Peiseler M., Surewaard B.G.J., Rath D., et al. Platelet GPIbα is a mediator and potential interventional target for NASH and subsequent liver cancer. Nat. Med. 2019;25:641–655. doi: 10.1038/s41591-019-0379-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Wang T., Fu X., Jin T., Zhang L., Liu B., Wu Y., Xu F., Wang X., Ye K., Zhang W., et al. Aspirin targets P4HA2 through inhibiting NF-κB and LMCD1-AS1/let-7g to inhibit tumour growth and collagen deposition in hepatocellular carcinoma. EBioMedicine. 2019;45:168–180. doi: 10.1016/j.ebiom.2019.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Roehlen N., Baumert T.F. Uncovering the mechanism of action of aspirin in HCC chemoprevention. EBioMedicine. 2019;46:21–22. doi: 10.1016/j.ebiom.2019.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Simon T.G., Henson J., Osganian S., Masia R., Chan A.T., Chung R.T., Corey K.E. Daily Aspirin Use Associated with Reduced Risk For Fibrosis Progression In Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2019;17:2776–2784.e4. doi: 10.1016/j.cgh.2019.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Sakurai T., Kudo M. Molecular Link between Liver Fibrosis and Hepatocellular Carcinoma. Liver Cancer. 2013;2:365–366. doi: 10.1159/000343851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Loomba R., Lawitz E., Mantry P.S., Jayakumar S., Caldwell S.H., Arnold H., Diehl A.M., Djedjos C.S., Han L., Myers R.P., et al. The ASK1 inhibitor selonsertib in patients with nonalcoholic steatohepatitis: A randomized, phase 2 trial. Hepatology. 2018;67:549–559. doi: 10.1002/hep.29514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Ratziu V., Harrison S.A., Francque S., Bedossa P., Lehert P., Serfaty L., Romero-Gomez M., Boursier J., Abdelmalek M., Caldwell S., et al. Elafibranor, an Agonist of the Peroxisome Proliferator−Activated Receptor−α and −δ, Induces Resolution of Nonalcoholic Steatohepatitis without Fibrosis Worsening. Gastroenterol. 2016;150:1147–1159.e5. doi: 10.1053/j.gastro.2016.01.038. [DOI] [PubMed] [Google Scholar]
- 250.Kumada H. Long-term treatment of chronic hepatitis C with glycyrrhizin [stronger neo-minophagen C (SNMC)] for preventing liver cirrhosis and hepatocellular carcinoma. Oncology. 2002;62:94–100. doi: 10.1159/000048283. [DOI] [PubMed] [Google Scholar]
- 251.Arase Y., Ikeda K., Murashima N., Chayama K., Tsubota A., Koida I., Suzuki Y., Saitoh S., Kobayashi M., Kumada H. The long term efficacy of glycyrrhizin in chronic hepatitis C patients. Cancer. 1997;79:1494–1500. doi: 10.1002/(SICI)1097-0142(19970415)79:8<1494::AID-CNCR8>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 252.Van Rossum T.G.J., Vulto A.G., De Man R.A., Brouwer J.T., Schalm S.W. glycyrrhizin as a potential treatment for chronic hepatitis C. Aliment. Pharmacol. Ther. 1998;12:199–205. doi: 10.1046/j.1365-2036.1998.00309.x. [DOI] [PubMed] [Google Scholar]
- 253.Shiota G., Harada K.-I., Ishida M., Tomie Y., Okubo M., Katayama S., Ito H., Kawasaki H. Inhibition of hepatocellular carcinoma by glycyrrhizin in diethylnitrosamine-treated mice. Carcinogenesis. 1999;20:59–63. doi: 10.1093/carcin/20.1.59. [DOI] [PubMed] [Google Scholar]
- 254.Oka H., Yamamoto S., Kuroki T., Harihara S., Marumo T., Kim S.R., Monna T., Kobayashi K., Tango T. Prospective study of chemoprevention of hepatocellular carcinoma with sho-saiko-to (TJ-9) Cancer. 1995;76:743–749. doi: 10.1002/1097-0142(19950901)76:5<743::AID-CNCR2820760506>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 255.Bishayee A., Chatterjee M., Chatterjee M. Further Evidence for Chemopreventive Potential of β-Carotene Against Experimental Carcinogenesis: Diethylnitrosamine-Initiated and Phenobarbital-Promoted Hepatocarcinogenesis Is Prevented More Effectively by β-Carotene Than by Retinoic Acid. Nutr. Cancer. 2000;37:89–98. doi: 10.1207/S15327914NC3701_12. [DOI] [PubMed] [Google Scholar]
- 256.Mann C.D., Neal C.P., Garcea G., Manson M.M., Dennison A.R., Berry D.P. Phytochemicals as potential chemopreventive and chemotherapeutic agents in hepatocarcinogenesis. Eur. J. Cancer Prev. 2009;18:13–25. doi: 10.1097/CEJ.0b013e3282f0c090. [DOI] [PubMed] [Google Scholar]
- 257.Qin G., Ning Y., Lotlikar P.D. Chemoprevention of Aflatoxin B1-Initiated and Carbon Tetrachloride-Promoted Hepatocarcinogenesis in the Rat by Green Tea. Nutr. Cancer. 2000;38:215–222. doi: 10.1207/S15327914NC382_11. [DOI] [PubMed] [Google Scholar]
- 258.Luo H., Tang L., Tang M., Billam M., Huang T., Yu J., Wei Z., Liang Y., Wang K., Zhang Z.-Q., et al. Phase IIa chemoprevention trial of green tea polyphenols in high-risk individuals of liver cancer: Modulation of urinary excretion of green tea polyphenols and 8-hydroxydeoxyguanosine. Carcinogenesis. 2005;27:262–268. doi: 10.1093/carcin/bgi147. [DOI] [PubMed] [Google Scholar]
- 259.Sojoodi M., Wei L., Erstad D.J., Yamada S., Fujii T., Hirschfield H., Kim R.S., Lauwers G.Y., Lanuti M., Hoshida Y., et al. Epigallocatechin Gallate Induces Hepatic Stellate Cell Senescence and Attenuates Development of Hepatocellular Carcinoma. Cancer Prev. Res. 2020;13:497–508. doi: 10.1158/1940-6207.CAPR-19-0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Cavin C., Holzhäuser D., Constable A., Huggett A.C., Schilter B. The coffee-specific diterpenes cafestol and kahweol protect against aflatoxin B1-induced genotoxicity through a dual mechanism. Carcinogenesis. 1998;19:1369–1375. doi: 10.1093/carcin/19.8.1369. [DOI] [PubMed] [Google Scholar]
- 261.Wong G.L.H., Chan H.L.-Y., Chan H.-Y., Tse C.-H., Chim A.M.-L., Lo A.O.-S., Wong V.W.-S. Adverse Effects of Vitamin D Deficiency on Outcomes of Patients with Chronic Hepatitis B. Clin. Gastroenterol. Hepatol. 2015;13:783–790.e1. doi: 10.1016/j.cgh.2014.09.050. [DOI] [PubMed] [Google Scholar]
- 262.Fedirko V., Duarte-Salles T., Bamia C., Trichopoulou A., Aleksandrova K., Trichopoulos D., Trepo E., Tjønneland A., Olsen A., Overvad K., et al. Prediagnostic circulating vitamin D levels and risk of hepatocellular carcinoma in European populations: A nested case-control study. Hepatology. 2014;60:1222–1230. doi: 10.1002/hep.27079. [DOI] [PubMed] [Google Scholar]
- 263.Kwon H.-J., Won Y.-S., Suh H.-W., Jeon J.-H., Shao Y., Yoon S.-R., Chung J.-W., Kim T.-D., Kim H.-M., Nam K.-H., et al. Vitamin D3 Upregulated Protein 1 Suppresses TNF-α–Induced NF-κB Activation in Hepatocarcinogenesis. J. Immunol. 2010;185:3980–3989. doi: 10.4049/jimmunol.1000990. [DOI] [PubMed] [Google Scholar]
- 264.Cha J.H., Bae S.H., Kim H.L., Park N.R., Choi E.S., Jung E.S., Choi J.Y., Yoon S.K. Branched-Chain Amino Acids Ameliorate Fibrosis and Suppress Tumor Growth in a Rat Model of Hepatocellular Carcinoma with Liver Cirrhosis. PLoS ONE. 2013;8:e77899. doi: 10.1371/journal.pone.0077899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Kawaguchi T., Shiraishi K., Ito T., Suzuki K., Koreeda C., Ohtake T., Iwasa M., Tokumoto Y., Endo R., Kawamura N., et al. Branched-Chain Amino Acids Prevent Hepatocarcinogenesis and Prolong Survival of Patients with Cirrhosis. Clin. Gastroenterol. Hepatol. 2014;12:1012–1018.e1. doi: 10.1016/j.cgh.2013.08.050. [DOI] [PubMed] [Google Scholar]
- 266.Gao M., Sun K., Guo M., Gao H., Liu K., Yang C., Li S., Liu N. Fish consumption and n-3 polyunsaturated fatty acids, and risk of hepatocellular carcinoma: Systematic review and meta-analysis. Cancer Causes Control. 2014;26:367–376. doi: 10.1007/s10552-014-0512-1. [DOI] [PubMed] [Google Scholar]
- 267.Sawada N., Inoue M., Iwasaki M., Sasazuki S., Shimazu T., Yamaji T., Takachi R., Tanaka Y., Mizokami M., Tsugane S. Consumption of n-3 Fatty Acids and Fish Reduces Risk of Hepatocellular Carcinoma. Gastroenterology. 2012;142:1468–1475. doi: 10.1053/j.gastro.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 268.Liebig M., Dannenberger D., Vollmar B., Abshagen K. n-3 PUFAs reduce tumor load and improve survival in a NASH-tumor mouse model. Ther. Adv. Chronic Dis. 2019;10:2040622319872118. doi: 10.1177/2040622319872118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Ma Y., Yang W., Li T., Liu Y., Simon T.G., Sui J., Wu K., Giovannucci E.L., Chan A.T., Zhang X. Meat intake and risk of hepatocellular carcinoma in two large US prospective cohorts of women and men. Int. J. Epidemiol. 2019;48:1863–1871. doi: 10.1093/ije/dyz146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Briske-Anderson M.J., Finley J.W., Newman S.M. The Influence of Culture Time and Passage Number on the Morphological and Physiological Development of Caco-2 Cells. Exp. Biol. Med. 1997;214:248–257. doi: 10.3181/00379727-214-44093. [DOI] [PubMed] [Google Scholar]
- 271.Hartung T. Food for thought look back in anger–What clinical studies tell us about preclinical work. Altex. 2013;30:275. doi: 10.14573/altex.2013.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Chen B., Sirota M., Fan-Minogue H., Hadley D., Butte A.J. Relating hepatocellular carcinoma tumor samples and cell lines using gene expression data in translational research. BMC Med. Genom. 2015;8:S5. doi: 10.1186/1755-8794-8-S2-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Gillet J.-P., Calcagno A.M., Varma S., Marino M., Green L.J., Vora M.I., Patel C., Orina J.N., Eliseeva T.A., Singal V., et al. Redefining the relevance of established cancer cell lines to the study of mechanisms of clinical anti-cancer drug resistance. Proc. Natl. Acad. Sci. USA. 2011;108:18708–18713. doi: 10.1073/pnas.1111840108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Moon H., Ju H.-L., Chung S.I., Cho K.J., Eun J.W., Nam S.W., Han K.-H., Calvisi D.F., Ro S.W. Transforming Growth Factor-β Promotes Liver Tumorigenesis in Mice via Up-regulation of Snail. Gastroenterology. 2017;153:1378–1391.e6. doi: 10.1053/j.gastro.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 275.Liu Y., Qi X., Zeng Z., Wang L., Wang J., Zhang T., Xu Q., Shen C., Zhou G., Yang S., et al. CRISPR/Cas9-mediated p53 and Pten dual mutation accelerates hepatocarcinogenesis in adult hepatitis B virus transgenic mice. Sci. Rep. 2017;7:2796. doi: 10.1038/s41598-017-03070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Recknagel R.O., Glende E.A., Dolak J.A., Waller R.L. Mechanisms of carbon tetrachloride toxicity. Pharmacol. Ther. 1989;43:139–154. doi: 10.1016/0163-7258(89)90050-8. [DOI] [PubMed] [Google Scholar]
- 277.Hall C.N., Badawi A.F., O’Connor P.J., Saffhill R. The detection of alkylation damage in the DNA of human gastrointestinal tissues. Br. J. Cancer. 1991;64:59–63. doi: 10.1038/bjc.1991.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Wallace M., Hamesch K., Lunova M., Kim Y., Weiskirchen R., Strnad P., Friedman S.L. Standard Operating Procedures in Experimental Liver Research: Thioacetamide model in mice and rats. Lab. Anim. 2015;49:21–29. doi: 10.1177/0023677215573040. [DOI] [PubMed] [Google Scholar]
- 279.Kushida M., Kamendulis L.M., Peat T.J., Klaunig J.E. Dose-Related Induction of Hepatic Preneoplastic Lesions by Diethylnitrosamine in C57BL/6 Mice. Toxicol. Pathol. 2011;39:776–786. doi: 10.1177/0192623311409596. [DOI] [PubMed] [Google Scholar]
- 280.Van Norman G.A. Phase II Trials in Drug Development and Adaptive Trial Design. JACC Basic Transl. Sci. 2019;4:428–437. doi: 10.1016/j.jacbts.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Rebholz C.E., Swiss Paediatric Oncology Group (SPOG) Rueegg C.S., Michel G., Ammann R.A., Von Der Weid N.X., Kuehni C.E., Spycher B.D. Clustering of health behaviours in adult survivors of childhood cancer and the general population. Br. J. Cancer. 2012;107:234–242. doi: 10.1038/bjc.2012.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Perrone J., Phillips C., Gaieski D. Occult Metformin Toxicity in Three Patients with Profound Lactic Acidosis. J. Emerg. Med. 2011;40:271–275. doi: 10.1016/j.jemermed.2007.11.055. [DOI] [PubMed] [Google Scholar]