Abstract
Herpes simplex viruses (HSVs) are neurotropic viruses with broad host range whose infections cause considerable health problems in both animals and humans. In fact, 67% of the global population under the age of 50 are infected with HSV-1 and 13% have clinically recurrent HSV-2 infections. The most prescribed antiherpetics are nucleoside analogues such as acyclovir, but the emergence of mutants resistant to these drugs and the lack of available vaccines against human HSVs has led to an imminent need for new antivirals. Valproic acid (VPA) is a branched short-chain fatty acid clinically used as a broad-spectrum antiepileptic drug in the treatment of neurological disorders, which has shown promising antiviral activity against some herpesviruses. Moreover, its amidic derivatives valpromide and valnoctamide also share this antiherpetic activity. This review summarizes the current research on the use of VPA and its amidic derivatives as alternatives to traditional antiherpetics in the fight against HSV infections.
Keywords: alphaherpesvirus, valproic acid, valpromide, valnoctamide
1. Introduction
The Alphaherpesvirinae are a large subfamily of neurotropic DNA viruses that cause epithelial lesions and may subsequently establish latency in sensory ganglia or neurons of the peripheral nervous system, potentially reactivating in the future [1,2]. Members of this group present a broad host range, short replication cycles and the capacity to rapidly spread and destroy the infected cell [3,4]. This subfamily includes a variety of species whose infections cause global health problems in both humans and animals. The alphaherpesviruses that can infect humans are herpes simplex virus type 1 (HSV-1 or HHV-1), herpes simplex virus type 2 (HSV-2 or HHV-2) and varicella-zoster virus (VZV or HVV-3) [5]. HSV-1 is characterized by orofacial (cold sores) and ocular lesions, encephalitis and genital lesions in various age groups [6,7]. However, the most common cause of genital herpes is HSV-2, which is sexually transmitted and also causes recurrent aseptic meningitis [8,9]. On the other hand, VZV causes chickenpox as a primary infection usually in children and then establishes latency, but its reactivation in adults or immunosuppressed individuals can lead to herpes zoster (shingles), which may derive postherpetic neuralgia [10] or lead to aseptic meningitis [9].
In terms of animal health, more than 30 alphaherpesviruses infecting different species (mammals, birds, reptiles, amphibians, and even invertebrates) have been reported [1]. Pseudorabies virus (suid herpesvirus 1, SuHV-1), equid alphaherpesvirus 1 (EHV-1) and bovine herpesvirus 1 and 5 (BoHV-1 and BoHV-5) should be highlighted for causing respiratory problems, neurological disorders and abortions mainly in swine, horses and cattle, respectively, causing significant economic losses in the affected herds. [3,11,12].
According to the WHO, 67% of the global population under the age of 50 are infected with HSV-1 and 13% have clinically recurrent HSV-2. In the case of VZV, its seroprevalence among European children under the age of 5 years reaches 70% or more [13]. Moreover, BoHV-1 affects cattle from many developed and developing countries; the prevalence of the virus in the UK has risen to 83% among unvaccinated herds [12].
Three classes of antivirals are approved for treatment of alphaherpesvirus infections, all of which target viral genome replication: acyclic guanosine analogues; acyclic nucleotide analogues; and pyrophosphate analogues [14]. The most frequently used antiherpetic is acyclovir (ACV), a guanosine analogue which is selectively phosphorylated by the viral enzyme thymidine kinase (TK), and subsequently by other kinases of the infected cell. ACV triphosphate is incorporated by the viral DNA polymerase into the replicating DNA chain, where it inhibits elongation due to the lack of a second hydroxyl group in its structure, thus avoiding the addition of another residue [15,16]. Many nucleoside analogues have been developed which have activity similar to ACV but with enhanced characteristics that improve their pharmacokinetics and pharmacodynamics. Examples of these are oral prodrugs valacyclovir (prodrug of ACV), famciclovir (prodrug of penciclovir) and valgancyclovir (prodrug of ganciclovir), which are effective at lower doses and have greater oral bioavailability compared to ACV [16,17,18].
Unfortunately, the emergence of mutant viruses that are resistant to traditional antiherpetics (especially in immunocompromised patients) and the lack of available vaccines against human HSVs [19] has led to an imminent need for new antivirals. In one study, 4–7% of patients coinfected with HIV and HSV-1 had virus strains which were resistant to approved antiherpetic drugs [20]. In 95% of cases, ACV resistance is acquired via mutations in the TK gene; thus, an alternative treatment strategy is to stop viral replication by targeting the viral DNA polymerase (for example by using the pyrophosphate analogue foscarnet) [21]. Nonetheless, resistance mutations can also occur in the viral DNA polymerase (5% of cases), decreasing its affinity for the nucleoside analogue [22,23,24]. Additionally, none of the antivirals discovered so far protect against the reactivation of herpesvirus in the event that the virus has established latency [2]. Thus, the therapeutic potential of several new drugs is being evaluated, which may be added to potential multi-drug treatment regimens against HSV infections. The current search for new antiherpetics is looking for selective compounds with improved efficacy and minimal adverse reactions, which prevent emergence of resistant mutants by targeting different steps in the viral cycle (adhesion and entry, replication, protein synthesis, assembly or exit). Novel nucleoside analogues as well as specific inhibitors of viral DNA polymerase, viral helicase-primase or ribonucleotide reductase are currently being tested [23,25].
2. Valproic Acid
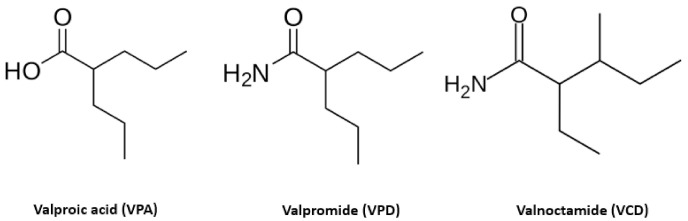
An interesting proposal to reduce the appearance of resistance mutants is to search for compounds which target cellular processes that are essential for the viral life cycle. Valproic acid (VPA; 2-n-propylpentanoic acid or n-dipropylacetic acid) is a branched short-chain fatty acid (Figure 1) clinically used as a broad-spectrum antiepileptic drug in the treatment of neurological disorders including epilepsy, bipolar disorders, neuropathic pain, migraine, and absence, myoclonic, generalized and partial seizures [26,27]. It is also prescribed in the treatment of attention deficit hyperactivity disorder in children, diskynesia, and other disorders that affect learning, thinking and understanding [28]. VPA belongs to the first generation of antiepileptic drugs (AED), which also includes carbamazepine, ethosuximide, phenobarbital, phenytoin and primidone [29,30]. The origin of VPA dates from a hundred years ago, when it was synthesized as a derivate of valeric acid [31], and despite its old age, in 2010 it was the most highly prescribed AED when considering mono- or polytherapeutic uses [28].
Figure 1.
Molecular structure of valproic acid (VPA) and its amidic derivatives valpromide (VPD) and valnoctamide (VCD). VPD and VCD differ from VPA in structure as they contain an amide group instead of a carboxylic group.
The precise mechanism of action of VPA at a molecular level is not fully understood, though it acts at different levels. VPA potentiates the inhibitory activity of the neurotransmitter gamma amino butyrate (GABA) in the central nervous system, by inhibition of GABA degradation and turnover, and by stimulation of its synthesis [32]. VPA also inhibits NDMA receptor-mediated excitatory transmission [33] and reduces the rapid firing of neurons by destabilizing voltage-gated sensitive Na+ channels [34,35] as well as T-type Ca2+ channels and K+ channels. It alters lipid metabolism, downregulates the expression of proteins involved in chromatin maintenance [32], inhibits glycogen synthase kinase 3 (GSK3) and protein kinase A (PKA) [36]. Inhibition of histone deacetylase (HDAC) by VPA makes it an interesting candidate for cancer and HIV treatments [37]. In fact, VPA plays an important role in new virotherapies for cancer, based on the administration of oncolytic herpesvirus vectors combined with drug therapy to enhance tumor eradication [38].
Previous studies have positioned VPA as a potential broad-spectrum antiviral, since it inhibited in vitro infection by enveloped viruses from various viral families, though it showed no effect against non-enveloped viruses [39]. VPA caused a drastic reduction of the yield of the flaviviruses West Nile virus (WNV) and Usutu virus (USUV), the arenavirus lymphocytic choriomeningitis virus (LCMV), the rhabdovirus vesicular stomatitis virus (VSV), the togaviruses Semliki forest virus (SFV) and Sindbis virus (SINV), the asfivirus African swine fever virus (ASFV) and the poxvirus vaccinia virus (VACV). On the contrary, VPA had no effect on the nonenveloped viruses tested, including foot-and-mouth disease virus (FMDV), encephalomyocarditis virus (EMCV), bovine enterovirus (BEV), and equine rhinitis A virus (ERAV) (picornaviruses). The results suggested that VPA can act at different steps of enveloped virus infection; although WNV RNA and protein synthesis were drastically abolished, VSV RNA and protein synthesis remained unaltered [39]. Considering that alphaherpesviruses present a lipid bilayer membrane, it was hypothesized that VPA would also have an antiviral effect against this viral subfamily.
In fact, the antiviral activity of VPA against HSV-1 has been demonstrated, in our group, in the human oligodendrocyte cell line HOG [40]. This cell line is a suitable cell model for the investigation of demyelinating disorders such as multiple sclerosis, an autoimmune disease whose etiology may involve some herpesviruses [41,42,43,44]. In that study, the half maximal inhibitory concentration (IC50) for VPA inhibition of HSV-1 infection was 0.55 mM [40], comparable to the regular dosage recommended for treatment of epilepsy which ranges between 0.3 to 0.6 mM in the plasma [45]. Moreover, cytotoxicity assays showed that HOG cells incubated with 4 mM of VPA for 48 h maintained more than 80% of viability [40]. Although clinical trials in humans have not yet been carried out, its AED dosage may be sufficient for antiviral activity against HSV-1. This is supported by the results of a nested case-control study, in which patients on VPA therapy lasting longer than 90 days were associated with a downward trend in risk of herpesvirus infection [26].
Nowadays, the use of VPA is limited and under surveillance due to its teratogenic and hepatotoxic effects. Indeed, as VPA can alter the gene expression of approximately 20% of the transcriptome in a tissue-dependent manner [32], predicting the effects of this drug can be a real challenge. The most important described teratogenic effects for VPA are major congenital malformations and neural tube defects in embryo and fetus, and thus is not recommended for women of childbearing age [46,47]. This teratogenicity is achieved through its structural characteristics: having a carboxylic acid, branching in carbon atom 2 (C-2) with two side chains, each containing at least three carbon atoms, and presenting a hydrogen atom at C-2 [48] Regarding hepatotoxicity, it is suggested that VPA metabolism leads to two hepatotoxic metabolites (4-ene-VPA and 2,4-diene-VPA), which may form an intermediate thioester with the free form of the mitochondrial coenzyme A in the liver [49,50]. Another hypothesis proposed that the hepatotoxicity associated with VPA originates from the inhibition of pyruvate transport, ATP- and GTP-dependent succinate-CoA ligases, hepatic N-acetylglutamate synthase and α-lipoamide dehydrogenase [51].
3. Amidic Derivatives of Valproic Acid
With the intention of reducing the toxic effects associated with VPA, some of its amidic derivatives have been tested as potential antivirals against alphaherpesviruses, the so-called “second-generation” VPAs. Valpromide (VPD; dipropylacetamide or 2-propylvaleramide) and valnoctamide (VCD, valmethamide or 2-etyhl-3-methyl-pentanamide) are aliphatic amide derivatives of VPA that barely differ in structure, containing an amide group (see Figure 1). This slight difference in the acidic core molecule (absence of a free carboxylic group) might be responsible for the lack of hepatotoxic and teratogenic effects [52,53,54]. Both drugs have been commercialized in various European countries for more than 50 years [54].
3.1. Valpromide
VPD is the primary amide of VPA and is currently used as an anticonvulsant and antipsychotic drug authorized in all EU Member States. It is indicated for treatment of primary generalized epilepsies and bipolar disorder in cases when lithium therapy is not tolerated [55,56]. VPD acts as a prodrug which, after oral or intravenous administration, is rapidly biotransformed through metabolic hydrolysis into its corresponding acid (90% of the total VPD dose) [54,57]. VPD easily crosses the blood-brain barrier and seems to have an anticonvulsive effect 3 to 5 times more potent than that of VPA [48,58]. In terms of teratogenicity, VPD does not show any such effect in pregnant rats, mice, or dogs [59,60]. Nevertheless, since VPD is transformed into VPA in humans, this drug is still contraindicated in women of childbearing age or pregnant women, since it may exhibit the same teratogenic effects [54,61].
The antiviral effect of VPD against HSV-1 was tested in our laboratory in human and murine cell lines and primary cultures based on rat oligodendrocyte precursor cells (OPCs), revealing an antiherpetic effect comparable to ACV. VPD was tested at 0.5 mM, a concentration compatible with the therapeutic doses already approved in humans. Indeed, OPCs viability in the presence of 0.5 mM VPD during 24 h was close to 100% [49]. These promising results encourage testing VPD antiviral activity in animal models and possibly in human clinical trials. Although VPD in humans is biotransformed into teratogenic VPA and therefore would not be an ideal drug in the treatment of infections in pregnant women, it could be used in the treatment of animal species where VPD does not carry such metabolization.
3.2. Valnoctamide
VCD is the primary amide of valnoctic acid and a constitutional isomer of VPD. Actually, it is a racemic compound which encompasses four stereoisomers, all of them showing a higher anticonvulsant efficacy in rodent models of epilepsy in comparison to VPA (about 3 to 10 times higher) [62,63]. In particular, the stereoisomer (2S,3R)-VCD stands out for having a greater oral clearance and a shorter half-life [52,64]. VCD is used as an anxiolytic and it has been involved in various clinical trials for acute mania and bipolar disorder [65,66]. Unlike VPD, VCD does not biotransform into VPA, so its pharmacological activity is different and its half-life is ten times longer than that of VPD [55]. Moreover, VCD has shown no teratogenic effects in murine models [67,68].
VCD’s antiviral effect against HSV-1 was also tested in HOG cells at the concentration 0.1 mM (VCD shows no cytotoxicity in this cells at this concentration), and it significantly inhibited the infection at accepted human dosage, similar to the effect achieved with ACV [49].
3.3. Antiviral Mechanism of VPA and Related Derivatives
Little is still known about the antiviral mechanism of VPA and its amidic derivatives. The fact that VPA acts at different molecular levels gives this compound the characteristic of broad-spectrum antiherpetic. This may be explained by an interference with different cellular and viral processes. Some studies have revealed that VPA and VPD may interfere with the initial steps of the viral cycle, specifically during virus entry [49]. As mentioned previously, VPA affects lipid metabolism (including the synthesis of phosphatidylinositols) and formation of cell membranes, so it may alter the viral acquisition of lipid envelope, resulting in mature viral particles with low stability [45]. Furthermore, some studies have reported antiviral activity of VPA, VCD and VPD against cytomegalovirus (CMV), a virus belonging to the Herpesviridae family that causes brain defects in neonates, not only outside the central nervous system but also in the developing brain of rodents [65,69]. CMV attaches to the cell through interaction of its glycoprotein gB with cellular heparan sulfate proteoglycans, and both VCD and VPD appear to affect the recognition of gB [49,69]. This mechanism may also explain the antiviral activity of these drugs against HSV-1. Moreover, some studies demonstrated that VPA inhibits the reactivation of Epstein-Barr virus (EBV) lytic cycle in vitro due to VPA’s HDAC inhibitory activity. However, despite the fact that VPD does not have this HDAC inhibitory property, it still inhibits reactivation of the EBV lytic cycle [70,71]. Furthermore, a recent study has shown that VPA could also have a potential antiviral effect against RNA virus SARS-CoV-2, as it reduces the number of angiotensin-converting enzyme 2 (ACE-2) in endothelial cells, the main cellular receptor that this coronavirus uses to enter the cell [72]. Thus, further research needs to be performed to unravel the antiviral mechanism of VPA and related derivatives.
4. Conclusions
There is proof that VPA and its amidic derivatives have shown antiviral activity against various members from the Herpesviridae family, specifically against alphaherpesviruses that can infect humans. Nowadays, the high incidence of alphaherpesvirus infection, especially HSVs, must be taken as a major concern, and the need for effective therapies also in animals should not be forgotten. The fact that VPA acts at different molecular levels gives this compound the characteristics of a broad-spectrum antiherpetic. Hence, it would be very interesting to test the potential inhibitory activity of VPA and its amidic derivatives against animal infections due to the importance of some alphaherpesviruses such as SuHV-1, BoHV-1 or EHV. Considering that VPA, VPD and VCD are already licensed for clinical use by the EMA (European Medicines Agency), the time required to approve their brand-new use for the treatment of alphaherpesvirus infections should be shorter than for novel drugs. In this way, VPA and its amidic derivatives VPD and VCD may be part of the solution to the growing problem of viral resistance against traditional antiherpetics.
Acknowledgments
The professional editing service NB Revisions was used for technical preparation of the 434 text prior to submission.
Author Contributions
Conceptualization, S.A. and R.B.-M.; writing—original draft preparation, S.A.; writing—review and editing, S.A., R.B.-M., I.R. and J.A.L.-G.; project administration, J.A.L.-G.; funding acquisition, R.B.-M. and J.A.L.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Fundación Severo Ochoa-Aeromédica Canaria and Ministerio de Ciencia e Innovación, Spain. Grant number PID2019 110570GB-I00.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Davison A.J., Eberle R., Ehlers B., Hayward G.S., McGeoch D.J., Minson A.C., Pellett P.E., Roizman B., Studdert M.J., Thiry E. The order Herpesvirales. Arch. Virol. 2009;154:171–177. doi: 10.1007/s00705-008-0278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kukhanova M.K., Korovina A.N., Kochetkov S.N. Human herpes simplex virus: Life cycle and development of inhibitors. Biochemistry. 2014;79:1635–1652. doi: 10.1134/S0006297914130124. [DOI] [PubMed] [Google Scholar]
- 3.Carrasco L., Almendral J.M. Virus Patógenos. Editorial Hélice, Fundación BBVA; Madrid, Spain: 2006. [Google Scholar]
- 4.Smith T.T., Whitley R.J. Infectious Diseases. Elsevier; Amsterdam, The Netherlands: 2017. Herpesviruses; pp. 1426–1438.e1. [DOI] [Google Scholar]
- 5.Cassady K.A., Whitley R.J. New therapeutic approaches to the alphaherpesvirus infections. J. Antimicrob. Chemother. 1997;39:119–128. doi: 10.1093/jac/39.2.119. [DOI] [PubMed] [Google Scholar]
- 6.De Mello C.P.P., Bloom D.C., Paixão I.C.N.P. Herpes simplex virus type-1: Replication, latency, reactivation and its antiviral targets. Antivir. Ther. 2016;21:277–286. doi: 10.3851/IMP3018. [DOI] [PubMed] [Google Scholar]
- 7.Widener R.W., Whitley R.J. Handbook of Clinical Neurology. Volume 123. Elsevier B.V.; Amsterdam, The Netherlands: 2014. Herpes simplex virus; pp. 251–263. [DOI] [PubMed] [Google Scholar]
- 8.Groves M.J. Genital Herpes: A Review. Am. Fam. Physician. 2016;93:928–934. [PubMed] [Google Scholar]
- 9.Rosenberg J., Galen B.T. Recurrent Meningitis. Curr. Pain Headache Rep. 2017;21:33. doi: 10.1007/s11916-017-0635-7. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy P.G.E., Gershon A.A. Clinical features of varicella-zoster virus infection. Viruses. 2018;10:609. doi: 10.3390/v10110609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mettenleiter T.C., Keil G.M., Fuchs W. Animal viruses: Molecular Biology. Volume 12. Caister Academic Press; Norfolk, UK: 2008. Molecular biology of animal herpesviruses; p. 531. [Google Scholar]
- 12.Biswas S., Bandyopadhyay S., Dimri U., Patra P.H. Bovine herpesvirus-1 (BHV-1) a re-emerging concern in livestock: A revisit to its biology, epidemiology, diagnosis, and prophylaxis. Vet. Q. 2013;33:68–81. doi: 10.1080/01652176.2013.799301. [DOI] [PubMed] [Google Scholar]
- 13.Bollaerts K., Riera-Montes M., Heininger U., Hens N., Souverain A., Verstraeten T., Hartwig S. A systematic review of varicella seroprevalence in European countries before universal childhood immunization: Deriving incidence from seroprevalence data. Epidemiol. Infect. 2017;145:2666–2677. doi: 10.1017/S0950268817001546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang Y.C., Feng H., Lin Y.C., Guo X.R. New strategies against drug resistance to herpes simplex virus. Int. J. Oral Sci. 2016;8:1–6. doi: 10.1038/ijos.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King D.H. History, pharmacokinetics, and pharmacology of acyclovir. J. Am. Acad. Dermatol. 1988;18:176–179. doi: 10.1016/S0190-9622(88)70022-5. [DOI] [PubMed] [Google Scholar]
- 16.Shiraki K. Antiviral drugs against alphaherpesvirus. In: Kawaguchi Y., Mori Y., editors. Human Herpesviruses. Advances in Experimental Medicine and Biology. Volume 1045. Springer; Singapore: 2018. pp. 103–122. [DOI] [PubMed] [Google Scholar]
- 17.Lebrun-Vignes B. Valaciclovir. Ann. Dermatol. Venereol. 2002;129:708–715. doi: 10.2165/00128415-201113810-00106. [DOI] [PubMed] [Google Scholar]
- 18.Al-Badr A.A., Ajarim T.D.S. Profiles of Drug Substances, Excipients and Related Methodology. Volume 43. Elsevier; Amsterdam, The Netherlands: 2018. Ganciclovir; pp. 1–208. [DOI] [PubMed] [Google Scholar]
- 19.Johnston C., Gottlieb S.L., Wald A. Status of vaccine research and development of vaccines for herpes simplex virus. Vaccine. 2016;34:2948–2952. doi: 10.1016/j.vaccine.2015.12.076. [DOI] [PubMed] [Google Scholar]
- 20.Levin M.J., Bacon T.H., Leary J.J. Resistance of herpes simplex virus infections to nucleoside analogues in HIV-infected patients. Clin. Infect. Dis. 2004;39 doi: 10.1086/422364. [DOI] [PubMed] [Google Scholar]
- 21.Garikapati S., Nguyen M. Foscarnet. StatPearls Publishing; Treasure Island, FL, USA: 2020. [PubMed] [Google Scholar]
- 22.Piret J., Boivin G. Antiviral resistance in herpes simplex virus and varicella-zoster virus infections: Diagnosis and management. Curr. Opin. Infect. Dis. 2016;29:654–662. doi: 10.1097/QCO.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 23.Vissani M.A., Thiry E., Dal Pozzo F., Barrandeguy M. Antiviral agents against equid alphaherpesviruses: Current status and perspectives. Vet. J. 2016;207:38–44. doi: 10.1016/j.tvjl.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 24.Vere Hodge R.A., Field H.J. Advances in Pharmacology. Volume 67. Elsevier; Amsterdam, The Netherlands: 2013. Antiviral agents for herpes simplex virus; pp. 1–38. [DOI] [PubMed] [Google Scholar]
- 25.De S.K., Hart J.C.L., Breuer J. Herpes simplex virus and varicella zoster virus: Recent advances in therapy. Curr. Opin. Infect. Dis. 2015;28:589–595. doi: 10.1097/QCO.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 26.Gil M., González-González R., Vázquez-Calvo A., Álvarez-Gutiérrez A., Martín-Acebes M.A., Praena B., Bello-Morales R., Saiz J.C., López-Guerrero J.A., Tabarés E., et al. Clinical Infections by Herpesviruses in Patients Treated with Valproic Acid: A Nested Case-Control Study in the Spanish Primary Care Database, BIFAP. J. Clin. Med. 2019;8:1442. doi: 10.3390/jcm8091442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu M.M., Li H.L., Shi L.H., Chen X.P., Luo J., Zhang Z.L. The pharmacogenomics of valproic acid. J. Hum. Genet. 2017;62:1009–1014. doi: 10.1038/jhg.2017.91. [DOI] [PubMed] [Google Scholar]
- 28.Nanau R.M., Neuman M.G. Adverse drug reactions induced by valproic acid. Clin. Biochem. 2013;46:1323–1338. doi: 10.1016/j.clinbiochem.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 29.Linde M., Mulleners W.M., Chronicle E.P., Mccrory D.C. Valproate (valproic acid or sodium valproate or a combination of the two) for the prophylaxis of episodic migraine in adults. Cochrane Database Syst. Rev. 2013;24:CD010611. doi: 10.1002/14651858.CD010611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patsalos P.N., Spencer E.P., Berry D.J. Therapeutic drug monitoring of antiepileptic drugs in epilepsy: A 2018 update. Ther. Drug Monit. 2018;40:526–548. doi: 10.1097/FTD.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 31.Tomson T., Battino D., Perucca E. Valproic acid after five decades of use in epilepsy: Time to reconsider the indications of a time-honoured drug. Lancet Neurol. 2016;15:210–218. doi: 10.1016/S1474-4422(15)00314-2. [DOI] [PubMed] [Google Scholar]
- 32.Diederich M., Chateauvieux S., Morceau F., Dicato M. Molecular and therapeutic potential and toxicity of valproic acid. J. Biomed. Biotechnol. 2010 doi: 10.1155/2010/479364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gean P.W., Huang C.C., Hung C.R., Tsai J.J. Valproic acid suppresses the synaptic response mediated by the NMDA receptors in rat amygdalar slices. Brain Res. Bull. 1994;33:333–336. doi: 10.1016/0361-9230(94)90202-X. [DOI] [PubMed] [Google Scholar]
- 34.Zanatta G., Sula A., Miles A.J., Ng L.C.T., Torella R., Pryde D.C., DeCaen P.G., Wallace B.A. Valproic acid interactions with the NavMs voltage-gated sodium channel. Proc. Natl. Acad. Sci. USA. 2019;116:26549–26554. doi: 10.1073/pnas.1909696116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farber N.B., Jiang X.P., Heinkel C., Nemmers B. Antiepileptic drugs and agents that inhibit voltage-gated sodium channels prevent NMDA antagonist neurotoxicity. Mol. Psychiatry. 2002;7:726–733. doi: 10.1038/sj.mp.4001087. [DOI] [PubMed] [Google Scholar]
- 36.Silva M.R., Correia A.O., dos Santos G.C.A., Parente L.L.T., de Siqueira K.P., Lima D.G.S., Moura J.A., da Silva Ribeiro A.E., Costa R.O., Lucetti D.L., et al. Neuroprotective effects of valproic acid on brain ischemia are related to its HDAC and GSK3 inhibitions. Pharmacol. Biochem. Behav. 2018;167:17–28. doi: 10.1016/j.pbb.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Ghodke-Puranik Y., Thorn C.F., Lamba J.K., Leeder J.S., Song W., Birnbaum A.K., Altman R.B., Klein T.E. Valproic acid pathway: Pharmacokinetics and pharmacodynamics. Pharm. Genom. 2013 doi: 10.1097/FPC.0b013e32835ea0b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watanabe D., Goshima F. Advances in Experimental Medicine and Biology. Volume 1045. Springer; New York, YA, USA: 2018. Oncolytic virotherapy by HSV; pp. 63–84. [DOI] [PubMed] [Google Scholar]
- 39.Vazquez-Calvo A., Saiz J.-C., Sobrino F., Martin-Acebes M.A. Inhibition of Enveloped Virus Infection of Cultured Cells by Valproic Acid. J. Virol. 2011;85:1267–1274. doi: 10.1128/JVI.01717-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crespillo A.J., Praena B., Bello-Morales R., Lerma L., Vázquez-Calvo A., Martín-Acebes M.A., Tabarés E., Sobrino F., López-Guerrero J.A. Inhibition of herpes virus infection in oligodendrocyte cultured cells by valproic acid. Virus Res. 2016;214:71–79. doi: 10.1016/j.virusres.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 41.Bello-Morales R., Andreu S., López-Guerrero J.A. The role of herpes simplex virus type 1 infection in demyelination of the central nervous system. Int. J. Mol. Sci. 2020;21:5026. doi: 10.3390/ijms21145026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bello-Morales R., Fedetz M., Alcina A., Tabarés E., López-Guerrero J.A. High susceptibility of a human oligodendroglial cell line to herpes simplex type 1 infection. J. Neurovirol. 2005;11:190–198. doi: 10.1080/13550280590924179. [DOI] [PubMed] [Google Scholar]
- 43.Hogestyn J.M., Mock D.J., Mayer-Proschel M. Contributions of neurotropic human herpesviruses herpes simplex virus 1 and human herpesvirus 6 to neurodegenerative disease pathology. Neural Regen. Res. 2018;13:211–221. doi: 10.4103/1673-5374.226380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bello-Morales R., Crespillo A.J., García B., Dorado L.Á., Martín B., Tabarés E., Krummenacher C., De Castro F., López-Guerrero J.A. The effect of cellular differentiation on HSV-1 infection of oligodendrocytic cells. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0089141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vázquez-Calvo Á., Martín-Acebes M.A., Sáiz J.C., Ngo N., Sobrino F., de la Torre J.C. Inhibition of multiplication of the prototypic arenavirus LCMV by valproic acid. Antiviral Res. 2013;99:172–179. doi: 10.1016/j.antiviral.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hanold K.C. Teratogenic Potential of Valproic Acid. J. Obstet. Gynecol. Neonatal Nurs. 1986;15:111–116. doi: 10.1111/j.1552-6909.1986.tb01376.x. [DOI] [PubMed] [Google Scholar]
- 47.Ornoy A. Valproic acid in pregnancy: How much are we endangering the embryo and fetus? Reprod. Toxicol. 2009;28:1–10. doi: 10.1016/j.reprotox.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 48.Isoherranen N., Yagen B., Bialer M. New CNS-active drugs which are second-generation valproic acid: Can they lead to the development of a magic bullet? Curr. Opin. Neurol. 2003;16:203–211. doi: 10.1097/00019052-200304000-00014. [DOI] [PubMed] [Google Scholar]
- 49.Praena B., Bello-Morales R., de Castro F., López-Guerrero J.A. Amidic derivatives of valproic acid, valpromide and valnoctamide, inhibit HSV-1 infection in oligodendrocytes. Antiviral Res. 2019;168:91–99. doi: 10.1016/j.antiviral.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 50.Winkler I., Blotnik S., Shimshoni J., Yagen B., Devor M., Bialer M. Efficacy of antiepileptic isomers of valproic acid and valpromide in a rat model of neuropathic pain. Br. J. Pharmacol. 2005;146:198–208. doi: 10.1038/sj.bjp.0706310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kudin A.P., Mawasi H., Eisenkraft A., Elger C.E., Bialer M., Kunz W.S. Mitochondrial liver toxicity of valproic acid and its acid derivatives is related to inhibition of α-lipoamide dehydrogenase. Int. J. Mol. Sci. 2017;18:1912. doi: 10.3390/ijms18091912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaufmann D., Yagen B., Minert A., Wlodarczyk B., Finnell R.H., Schurig V., Devor M., Bialer M. Evaluation of the antiallodynic, teratogenic and pharmacokinetic profile of stereoisomers of valnoctamide, an amide derivative of a chiral isomer of valproic acid. Neuropharmacology. 2010;58:1228–1236. doi: 10.1016/j.neuropharm.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 53.Bialer M. Chemical properties of antiepileptic drugs (AEDs) Adv. Drug Deliv. Rev. 2012;64:887–895. doi: 10.1016/j.addr.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 54.Bialer M., Yagen B. Valproic Acid: Second Generation. Neurotherapeutics. 2007;4:130–137. doi: 10.1016/j.nurt.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bialer M., Haj-Yehia A., Barzaghi N., Pisani F., Perucca E. Pharmacokinetics of a valpromide isomer, valnoctamide, in healthy subjects. Eur. J. Clin. Pharmacol. 1990;38:289–291. doi: 10.1007/BF00315032. [DOI] [PubMed] [Google Scholar]
- 56.European Medicines Agency (EMA) Valproate and Related Substances. [(accessed on 28 October 2020)]; Available online: https://www.ema.europa.eu/en/medicines/human/referrals/valproate-related-substances-0#overview-section.
- 57.Vademecum 2020 Valpromida 2020. [(accessed on 28 October 2020)]; Available online: https://www.vademecum.es/principios-activos-valpromida-N03AG02.
- 58.Bialer M. Clinical Pharmacology of Valpromide. Clin. Pharmacokinet. 1991;20:114–122. doi: 10.2165/00003088-199120020-00003. [DOI] [PubMed] [Google Scholar]
- 59.Okada A., Kurihara H., Aoki Y., Bialer M., Fujiwara M. Amidic Modification of Valproic Acid Reduces Skeletal Teratogenicity in Mice. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2004;71:47–53. doi: 10.1002/bdrb.10057. [DOI] [PubMed] [Google Scholar]
- 60.Bialer M. Pharmacokinetic considerations in the design of better and safer new antiepileptic drugs. J. Control. Release. 1999;62:187–192. doi: 10.1016/S0168-3659(99)00037-1. [DOI] [PubMed] [Google Scholar]
- 61.Bialer M., Haj-Yehia A., Badir K., Hadad S. Can we develop improved derivatives of valproic acid? Pharm. World Sci. 1994;16:2–6. doi: 10.1007/BF01870931. [DOI] [PubMed] [Google Scholar]
- 62.Isoherranen N., White H.S., Klein B.D., Roeder M., Woodhead J.H., Schurig V., Yagen B., Bialer M. Pharmacokinetic-pharmacodynamic relationships of (2S,3S)-valnoctamide and its stereoisomer (2R,3S)-valnoctamide in rodent models of epilepsy. Pharm. Res. 2003;20:1293–1301. doi: 10.1023/A:1025069519218. [DOI] [PubMed] [Google Scholar]
- 63.Modi H.R., Ma K., Chang L., Chen M., Rapoport S.I. Valnoctamide, which reduces rat brain arachidonic acid turnover, is a potential non-teratogenic valproate substitute to treat bipolar disorder. Psychiatry Res. 2017;254:279–283. doi: 10.1016/j.psychres.2017.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shekh-Ahmad T., Mawasi H., McDonough J.H., Yagen B., Bialer M. The potential of sec-butylpropylacetamide (SPD) and valnoctamide and their individual stereoisomers in status epilepticus. Epilepsy Behav. 2015;49:298–302. doi: 10.1016/j.yebeh.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 65.Ornaghi S., Hsieh L.S., Bordey A., Vergani P., Paidas M.J., Van Den Pol A.N. Valnoctamide inhibits cytomegalovirus infection in developing brain and attenuates neurobehavioral dysfunctions and brain abnormalities. J. Neurosci. 2017;37:6877–6893. doi: 10.1523/JNEUROSCI.0970-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bersudsky Y., Applebaum J., Gaiduk Y., Sharony L., Mishory A., Podberezsky A., Agam G., Belmaker R.H. Valnoctamide as a valproate substitute with low teratogenic potential in mania: A double-blind, controlled, add-on clinical trial. Bipolar Disord. 2010;12:376–382. doi: 10.1111/j.1399-5618.2010.00828.x. [DOI] [PubMed] [Google Scholar]
- 67.Bialer M., Johannessen S.I., Levy R.H., Perucca E., Tomson T., White H.S. Progress report on new antiepileptic drugs: A summary of the Thirteenth Eilat Conference on New Antiepileptic Drugs and Devices (EILAT XIII) Epilepsia. 2017;58:181–221. doi: 10.1111/epi.13634. [DOI] [PubMed] [Google Scholar]
- 68.Lin Y.L., Bialer M., Cabrera R.M., Finnell R.H., Wlodarczyk B.J. Teratogenicity of valproic acid and its constitutional isomer, amide derivative valnoctamide in mice. Birth Defects Res. 2019;111:1013–1023. doi: 10.1002/bdr2.1406. [DOI] [PubMed] [Google Scholar]
- 69.Ornaghi S., Davis J.N., Gorres K.L., Miller G., Paidas M.J., van den Pol A.N. Mood stabilizers inhibit cytomegalovirus infection. Virology. 2016;499:121–135. doi: 10.1016/j.virol.2016.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gorres K.L., Daigle D., Mohanram S., McInerney G.E., Lyons D.E., Miller G. Valpromide inhibits Lytic cycle reactivation of epstein-Barr virus. MBio. 2016;7 doi: 10.1128/mBio.00113-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Anderson A.G., Gaffy C.B., Weseli J.R., Gorres K.L. Inhibition of epstein-barr virus lytic reactivation by the atypical antipsychotic drug clozapine. Viruses. 2019;11:450. doi: 10.3390/v11050450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Singh S., Singh K. Valproic Acid in Prevention and Treatment of COVID-19. Authorea Prepr. 2020 doi: 10.22541/AU.158931086.64128149. [DOI] [Google Scholar]