Abstract
Simple Summary
This revision is about the problem of Escherichia coli as a commensal and pathogenic bacterium among food-producing animals and health implications. Escherichia coli may play an important ecological role and can be used as a bioindicator of antimicrobial resistance. All animal species used for food production, as well as humans, carry E. coli in their intestinal tract; plus, the genetic flexibility and adaptability of this bacteria to constantly changing environments allows it to acquire a great number of antimicrobial resistance mechanisms. The majority of E. coli strains are commensals inhabiting the intestinal tract of humans and warm-blooded animals and rarely causes diseases. However, E. coli also remains as one of the most frequent causes of several common bacterial infections in humans and animals. All over the word, antibiotic resistance is commonly detected among commensal bacteria from food-producing animals, raising important questions on the potential impact of antibiotic use in animals and the possible transmission of these resistant bacteria to humans through the food chain. The use, in food-producing animals, of antibiotics that are critically important in human medicine has been implicated in the emergence of new forms of resistant bacteria, including new strains of multidrug-resistant foodborne bacteria, such as extended spectrum β-lactamase (ESBL)-producing E. coli.
Abstract
Escherichia coli are facultative, anaerobic Gram-negative rods with many facets. Within resistant bacterial populations, they play an important ecological role and can be used as a bioindicator of antimicrobial resistance. All animal species used for food production, as well as humans, carry E. coli in their intestinal tracts; plus, the genetic flexibility and adaptability of this bacteria to constantly changing environments allows it to acquire a great number of antimicrobial resistance mechanisms. Thus, the prevalence of antimicrobial resistance in these commensal bacteria (or others, such as enterococci) can be a good indicator for the selective pressure caused by the use of antimicrobial agents, providing an early warning of the emergence of antimicrobial resistance in pathogens. As many as 90% of E. coli strains are commensals inhabiting the intestinal tracts of humans and warm-blooded animals. As a commensal, it lives in a mutually beneficial association with its hosts and rarely causes diseases. However, E. coli also remains as one of the most frequent causes of several common bacterial infections in humans and animals. In humans, it is the prominent cause of enteritis, community- and hospital-acquired urinary tract infection (UTI), septicemia, postsurgical peritonitis, and other clinical infections, such as neonatal meningitis, while, in farm animals, it is more prominently associated with diarrhea. On a global scale, E. coli can be considered the most important human pathogen, causing severe infection along with other major bacterial foodborne agents, such as Salmonella spp. and Campylobacter. Thus, the importance of resistance in E. coli, typically considered a benign commensal, should not be underestimated.
Keywords: Escherichia coli, ESBL, food-producing animals, antimicrobial resistance
1. Pathogenicity of Escherichia coli
E. coli is a ubiquitous commensal of food-producing animals and humans. Most strains of this enterobacterial species are harmless commensals that live in a mutually beneficial association with their hosts and seldom cause disease. E. coli is, however, a particularly complex species, having diversified into pathogenic strains. Based on the type of virulence factor present, and the host’s clinical symptoms, E. coli strains are classified into pathotypes of zoonotic intestinal pathogenic E. coli (IPEC) or extraintestinal pathogenic E. coli (ExPEC) [1].
Within the IPEC, the diarrheagenic E. coli (DEC) groups include enteropathogenic E. coli (EPEC), enterotoxigenic E. coli (ETEC), enteroinvasive E. coli (EIEC), enteroaggregative E. coli (EAggEC), diffusely adherent E. coli (DAEC), enterohemorrhagic E. coli (EHEC) and Vero cytotoxin-producing E. coli (VTEC) or Shiga toxin-producing E. coli (STEC) [2]. Food poisoning outbreaks have been particularly associated with VTEC and, to a lesser extent, EPEC, ETEC and EAggEC strains [3]. The E. coli O157:H7 VTEC strain has become widely recognized as a very important cause of foodborne illness [4]. Since 1982, outbreaks have been recorded in the U.S. and throughout Europe. The source most often found to be contaminated was beef meat, often minced, but today, the organism is widespread in the guts of asymptomatic cattle, and their feces can potentially contaminate other products (like vegetables, sprouts, fruits, meat products, drinking water, juices and milk) [5,6].
The ExPEC group brings together the uropathogenic E. coli (UPEC), the neonatal meningitis E. coli (NMEC) and the avian pathogenic E. coli (APEC), which are frequently associated with nosocomial and community-associated infections [7]. Poultry meat is the food of the animal source most closely linked to human ExPEC. In addition to the overall highest levels of E. coli contamination found in poultry meat, virulence genes similar to those of human ExPEC are often found in poultry-associated E. coli strains [8]. Moreover, extensive genetic similarity has been documented between APEC and ExPEC strains, causing disease in poultry and humans, respectively [8,9]. Although beef and pork meats were also evaluated as potential reservoirs of ExPEC causing urinary tract infections (UTIs) in humans, the recovered ExPEC isolates were significantly less likely to be genetically related to isolates from humans with UTIs than those from poultry [10]. Some of the emerging ExPEC lineages associated with human outbreaks are known to be linked with food-producing animals. For example, E. coli O25:H4-B2-ST131 has a globally emerging lineage with an extensive antimicrobial resistance profile, including the CTX-M-15 enzyme, and fluoroquinolone resistance [10]. In addition, wild, companion and food-producing animals have been reported as carriers of this group [11]. Furthermore, E. coli (various serotypes)-A-ST10, a commonly encountered, antimicrobial susceptible, low-virulence, human intestinal colonizer has been associated with some human infections and extended spectrum β-lactamase (ESBL) production [11,12]. Moreover, the ESBL-producing E. coli ST10 has been recovered from chicken meat, other meat types, rectal swab samples from healthy humans and human blood cultures [13,14].
The presence of several putative virulence genes enables pathogenic ExPEC bacteria to cause infections. According to their phylogenetic classification, ExPECs typically belong to group B2 and, less commonly, to group D, whereas commensal intestinal strains belong to group A or B1 [15]. However, virulence-associated genes, in and of themselves, rarely make an organism virulent. Their levels of expression, which can vary between pathogenic and nonpathogenic isolates, can also be a determining factor [16]. Moreover, it seems that these putative virulence factors, rather than being directly involved in infection, also contribute to ExPEC fitness, increasing their adaptability, competitiveness and ability to colonize the human body [16]. ExPEC strains are characterized by virulence factors that may be present in various combinations, including adhesins (papC, F10papA, sfaDE, afaBC III, iha, fimH, clpG, tsh and hra); invasin (ibe10); iron-sequestering systems (iucD, irp2 and chuA); toxins (ompT, ehxA, espP, hlyA, hlyD, vat, sat and cnf1); capsules (K1, K5, kpsMT II and kpsMT III); siderophores (iroN, fyuA and ireA) and various other factors (iss, usp, traT, malX, cvaC and H7 fliC) [17].
2. Antimicrobial Resistance Trends in E. coli
The presence of mobile genetic elements such as plasmids, insertion sequences and transposons contributes to the plasticity of E. coli’s genome. Horizontal gene transfer has promoted the diffusion of antibiotic resistance genes among this species and other commensals [18], particularly in environments such as the intestinal tract, where the species diversity and bacterial population density are large. Therefore, E. coli has been used as a sentinel microorganism for antimicrobial resistance surveillance, especially in the case of the β-lactams [19].
Antimicrobial-resistant E. coli strains are broadly distributed in Europe, both in humans and in food-producing animals. As reported in the 2018 Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net), more than half of the E. coli isolates in Europe were resistant to at least one class of antimicrobials. Aminopenicillin resistance, followed by a resistance to fluoroquinolones, third-generation cephalosporins and aminoglycosides, were the most prevalent [20]. Furthermore, the reduction of antimicrobial-resistant E. coli in Europe was very low or nonexistent between 2015 and 2018, with E. coli being the major burden of antimicrobial resistance both in the number of cases and number of deaths [20]. Meanwhile, among food-producing animals, the European Food Safety Authority (EFSA) reported that the high proportions of Salmonella, Campylobacter and indicator E. coli isolates exhibiting reduced susceptibility to fluoroquinolones remain of concern [21]. However, co-resistance to “clinically important antimicrobials”, such as a resistance to third-generation cephalosporins or fluoroquinolones, are generally reported at very low to low levels in commensal E. coli isolates from animals [21].
These trends among food-producing animals are also evidenced by several other reports. Resistance to third-generation cephalosporins and quinolones was found among clinical E. coli, already resistant to most antimicrobials available for poultry, in a study conducted in 200 industrial poultry farms in Italy [22]. Likewise, in Germany, animals from 60 beef cattle and 52 dairy cattle production units were sampled; third-generation cephalosporin-resistant E. coli were isolated from at least one sample in 70% of the beef cattle farms and 85% of the dairy farms [23]. Besides resistances to antimicrobial classes that have been extensively used for a long time (e.g., sulphonamides and tetracyclines), high resistance rates to ciprofloxacin were also found among isolates from food-producing animals, more often in broilers, chicken meat and turkey meat than in the cattle and pig production chains [24,25,26]. These reports notwithstanding, E. coli with resistance to “critically important” antibiotics (especially to quinolones but, also, to colistin) in food-producing animals has been increasingly reported by others, as well as multidrug resistance (MDR) in commensal E. coli [27,28,29,30,31,32,33,34]. Moreover, the worldwide dissemination of MDR E. coli strains is mainly due to the spread of genes located on mobilizable genetic elements, including integrons, plasmids and transposons [35,36,37,38,39]. Since quinolones, colistin and third-generation cephalosporins are priority antimicrobials in human antimicrobial therapy, the emergence of this resistance warrants special concern and requires close monitoring.
3. The Major Threat from ESBL-Producing E. coli
3.1. Contextualizing the Issue
ESBL production is of importance not only in the nosocomial and long-term care perspectives but, also, for community-onset infections, with increasing reports of the latter. The transmission of ESBL-producing bacteria may occur from human to human, or from animal sources to humans via the food chain [40]. The clinical impact of infections by ESBL-producing E. coli strains has mainly been studied in hospitalized patients. These infections present a higher mortality rate associated with a delay in implementing an appropriate antimicrobial therapy, since empirically prescribed antibiotics may not be effective in this case [40]. In a study in Europe [41], ESBL-producing E. coli infections were estimated to be in the order of 300,000 and to have caused 9000 attributable deaths. Besides, infections with ESBL-producing bacteria have been associated with longer hospital stays and with an increased burden on the health services [42]. An overall global burden of the infections by ESBL-producing E. coli in farm animals is yet to be estimated, but their potential role as a reservoir of these microorganisms for humans necessitates a One Health, interdisciplinary approach to keep this threat under control [43].
Organisms producing ESBLs have been increasingly reported worldwide since their first description in Europe in the early 1980s [44]. A recent study reported a cumulative global pooled prevalence of ESBL-producing E. coli intestinal carriage, in the community, of 16.5% for the 2013–2018 period, with an eight-fold increase during the past two decades, indicating that preventing the dissemination of such strains may require new therapeutic and public health strategies [45].
The presence of ESBLs and their combined resistance is a serious public health concern. In addition to the resistance conferred by the ESBL enzymes, co-resistance to other antibiotic classes is frequently observed, drastically limiting therapeutic options available and putting human health in peril [46]. Moreover, this phenomenon may lead to the increased use of carbapenems, favoring further dissemination of carbapenemase-producing Enterobacteriaceae [47].
ESBLs are, mostly, plasmid-encoded enzymes that confer extended resistance to β-lactams (penicillins, first-, second- and third-generation cephalosporins and aztreonam) but not to cephamycins or carbapenems [48]. They are inhibited by β-lactamase inhibitors such as clavulanic acid and belong to Ambler’s classes A and D [49]. ESBLs are found in Bush-Jacoby-Medeiros classes 2be and 2d [50]. ESBL production is common in E. coli and Klebsiella pneumoniae, but it also occurs in other Enterobacteriaceae and in Pseudomonas aeruginosa. ESBL have been classified in three major subtypes: TEM, SHV and CTX-M β-lactamases. ESBLs derived from Bush-Jacoby-Medeiros type 2b enzymes—the TEM- and SHV-type ESBLs—are a large, widespread group and differ from their parental enzymes by as few as one or two amino acids [51]. These minor differences in their amino acid sequences are, nevertheless, enough to extend the spectrum of their enzymatic activity, making them able to hydrolyze cephalosporins that have an oxyimino side chain (third-generation cephalosporins and aztreonam) [50]. Contrarily to other ESBLs, the CTX-M family is a heterogenous, complex group of enzymes that possibly derived from the relocation of chromosomal Kluyvera genes to mobile genetic elements, conferring resistance to cefotaxime and ceftazidime [52].
For a long time, TEM and SHV types were the dominant ESBL enzymes all over the world. However, this situation changed dramatically in the present century. Nowadays, CTX-M enzymes have become the most widespread type of ESBLs [53]. Worryingly, most ESBL-producing isolates are now E. coli-expressing CTX-M β-lactamases that, in the modern landscape, “crossed the border” from hospital settings to the community [42]. We are now witnessing a worldwide epidemic of E. coli strains harboring CTX-M enzymes that require serious attention. The CTX-M-15 enzymes are, by far, the most globally spread—virtually present in all human and animal compartments, as well as in the environment—all over the world [54,55,56,57].
3.2. CTX-M β-Lactamases and Their Relevance
The CTX-M enzymes constitute a distinct phylogenetic lineage of molecular class A β-lactamases. The first blaCTX-M was described in 1990, from a clinical E. coli isolate, in Germany [58]. Nowadays, at least 170 members of the CTX-M family have been identified, in at least 26 bacterial species, but the majority are from E. coli, K. pneumoniae and Proteus mirabilis [59]. Based upon their amino acid homology, the CTX-Ms can be divided into five main groups: Group 1 (CTX-M-1, 3, 10, 11, 12, 15, 22, 23, 28, 29, 30 and UOE- 1), Group 2 (CTX-M-2, 4, 5, 6, 7 and 20), Group 3 (CTX-M-8), Group 4 (CTX-M-9, 13, 14, 16, 17, 19, 21 and 27) and Group 5 (CTX-M-25 and 26) [60].
The CTX-M genes can be traced back to the chromosome-encoded genes of Kluyvera spp., strongly indicating that these chromosomal β-lactamase genes were the probable progenitors of all groups of plasmid-mediated CTXMs [58]. The original Kluyvera blaCTX-M genes conferred hydrolytic activity against cefotaxime to a higher degree than against ceftazidime. Later on, similarly to other ESBLs, divergence by point mutations led to increased activity against the latter antimicrobial as well [61].
3.3. Dissemination of CTX-M and Its Implications
In Enterobacteriaceae, the great adaptive success of blaCTX-M genes has been associated with a few surrounding genetic structures and a few plasmids [62,63]. The spread of CTX-M is dependent upon its mobility. The mobilization of blaCTX-M genes from their original chromosomal position in Kluyvera species has been facilitated by mobile genetic elements, such as ISEcp1 or ISCR1, and their later incorporation in mobilizable genetic platforms, including class 1 integrons, plasmids and/or transposons [64]. The insertion sequence ISEcp1 provides a high-level expression promoter for the blaCTX-M gene and is positioned upstream of blaCTX-M genes from group CTX-M-1, -2, -9 and -25 enzymes [58,65]. Furthermore, the ISEcp1 element has been linked to other multiple resistance determinants (blaCMY, aph(2′), rmtC and qnr) in various members of the Enterobacteriaceae family, underlining their ability to facilitate the expression and spread of different antimicrobial resistance determinants [58]. More intriguingly, the ISCR can mobilize the blaCTX-M gene via rolling circle transposition and insertion into a class 1 integron, providing a putative promoter for high-level expression [58,66].
It is acknowledged that, once transferred on plasmid(s) and/or integron(s), the blaCTX-M genes have broader opportunities for horizontal spread among different Gram-negative organisms, and these mobile elements became one important factor in the epidemiology of this bacterial ecosystem [67]. Epidemiological studies based on molecular techniques have revealed a close and significant linkage of blaCTX-M genes to plasmids, mainly of the IncF, IncI, IncN, IncHI2, IncL/M and IncK groups [65,68]. The gene blaCTX-M-15 has been often identified in IncF group plasmids (FIA, FIB and FII), while IncF, IncK and IncI1 are closely related to the wide spread of blaCTX-M-14 genes [58,65]. In addition, CTX-Ms, such as blaCTX-M-1 and blaCTX-M-3, have frequently been reported on broad host-range replicon plasmids IncN, IncI1 and IncL/M [62]. Moreover, the presence of IncN plasmids carrying blaCTX-M-1 in farm animals, as well as their spread between humans and animals, have been documented, with the IncN and IncI1 plasmids found to be highly prevalent among E. coli from pig fecal microbiota [69]. Furthermore, genes encoding a resistance to quinolones, aminoglycosides, macrolides, tetracyclines, sulfonamides, trimethoprim and chloramphenicol have all been associated with blaCTX-M-containing plasmids [58]. The successful associations of these units, and the coexistence of blaCTX-M genes with other resistance determinants, might have contributed to the extraordinary spread of CTX-M enzymes and to the present uncontrolled pandemic scenario. On the other hand, the coexistence of two or more β-lactamases in the same strain is frequently found [52]. Moreover, there is little doubt that the use of cephalosporins and related compounds has been one of the driving forces in the persistence and dissemination of ESBL-producing bacteria, with the use of other antimicrobial compounds also exerting the same selective force [68].
One of the most interesting issues in the dispersion of CTX-M enzymes is the dissemination of specific clones. The application of Multi-Locus Sequence Typing (MLST) technologies to the study of CTX-M-15-producing ESBL isolates led to the recognition of the internationally disseminated clone B2,O25:H4-ST131 [66,70]. There is great concern about the pandemic spread of the CTX-M-15-producing E. coli of Sequence Type (ST) 131 [66]. This clone belongs to the phylogenetic group B2, a highly virulent group of ExPEC, which is responsible for urinary tract infections, bacteremia, urinary sepsis and neonatal sepsis [71,72]. Further, ST131 is the most studied phylogenetic lineage in terms of antimicrobial resistance in E. coli, and blaCTX-M-15-carrying strains of ST131 are often associated with other resistance determinants, such as trimethoprim-sulfamethoxazole, aminoglycosides, fosfomycin and fluoroquinolones [58]. In addition, they have been associated with 100% of ciprofloxacin resistance rates, close to those of the aminoglycosides [73]. The combination of virulence and antimicrobial resistance may give E. coli ST131 a fitness advantage over other E. coli strains. Furthermore, the spread of ST131 occurred among human isolates, but it is also disseminated to various animal species, including poultry, cattle, pigs, wildlife and pets [71]. Other E. coli lineages of the “virulent” phylogroup D, also associated with multi-resistance, include ST69, ST405 and O15:K52:H1 [11,74]. In addition, E. coli clones belonging STs 10 and 23, and to phylogroup A, are increasingly reported in association with ESBL production [75].
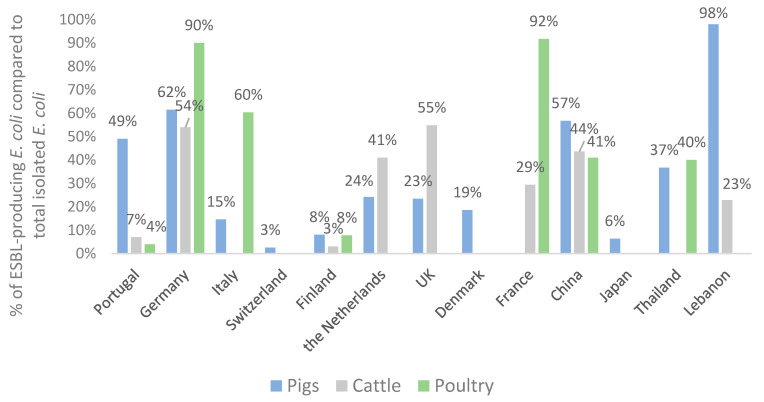
It is worrisome that commensal E. coli bacteria from food-producing animals may contribute to the dissemination of ESBL resistance and to the transference of resistance genes to human pathogenic bacteria, such as Salmonella spp. [76]. Figure 1 compares the percentages of ESBL-producing E. coli strains reported in food-producing animals by different European and non-European countries. For comparison purposes, we selected studies where samples were collected from healthy animals at the farm or slaughter level. Apart from Lebanon, Germany, China, Portugal and Thailand, where high percentages (>25%) of ESBL-producing E. coli were found among pig isolates, only low-to-moderate percentages (>1% to <25%) were detected in the other countries. Concerning cattle isolates, the overall results pointed towards lower percentages than in swine, but percentages were still high (>25%) in Germany, the Netherlands, the UK and China. Regarding the presence of ESBL-producing E. coli isolated from poultry, there was a very high percentage in Germany, France and Italy.
Figure 1.
Percentage of extended spectrum β-lactamase (ESBL)-producing Escherichia coli strains reported in healthy food-producing animals in different countries [23,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98].
The variability across data can be explained by differences in husbandry practices, antibiotic usage or, even, in experimental methodologies. However, in most reports, the data from antibiotic use were not included, making it impossible to draw practical conclusions concerning this aspect. Furthermore, isolation methods (e.g., the use of different enrichment broths and/or selective media) and sample sizes vary greatly between countries, which may have resulted in different screening sensitivities. Hence, comparing prevalence data should, in some instances, be performed cautiously; for example, in the recent report by the EFSA, the overall levels of resistance to cefotaxime and ceftazidime in the reporting countries were generally low (<4%), both in pigs and in cattle [21]. It is of note that differences in the type of cattle (dairy cattle, veal calves or beef cattle) sampled should also be taken in consideration when comparing data. Therefore, the higher percentages of ESBL-producing E. coli obtained among cattle isolates in Germany can be explained by the type of cattle included in that study, in which samples were collected from mixed farms and beef cattle farms [23]. This fact can also be explained by farming differences, like housing and exposure to antibiotics. Conversely, in France, the study by Haenni et al. (2014), in which 29% of ESBL-producing E. coli were found, was performed at the slaughterhouse [83].
The globalization of CTX-M enzymes is illustrated by their presence not only in humans but, also, in food, food-producing, companion and wild animals, as well as in the environment [71]. Nowadays, the prevalence of food-producing animals carrying E. coli producing CTX-M-type ESBLs has reached worryingly high levels, raising questions about the possible role of animals and food, as related reservoirs, in this phenomenon. The high proportions of resistance to third-generation cephalosporins and fluoroquinolones reported for E. coli in humans are concerning; meaning that, in many settings, the treatment must rely on carbapenems, a more expensive drug, that may not be available in resource-constrained settings and which is also likely to further accelerate the development of resistance [99]. The rapid, global dissemination of the plasmid-borne, colistin resistance-encoding mcr-1 gene, since its discovery in 2016 and its presence in environmental sources, in animals and in food [100], as well as its co-occurrence with genes that encode ESBLs [92] and New Delhi Metallo-β-lactamase (NDM-1) [101], has also raised concerns about colistin resistance in E. coli.
3.4. Distribution of ESBL Enzymes in E. coli Isolates from Food-Producing Animals
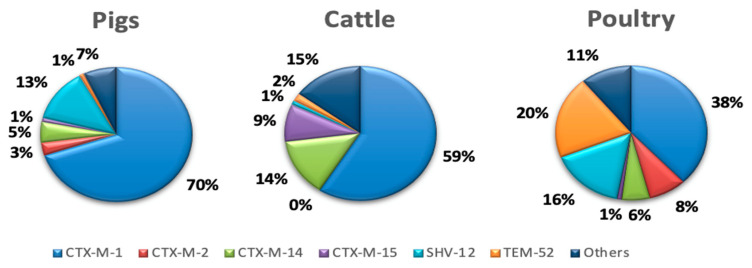
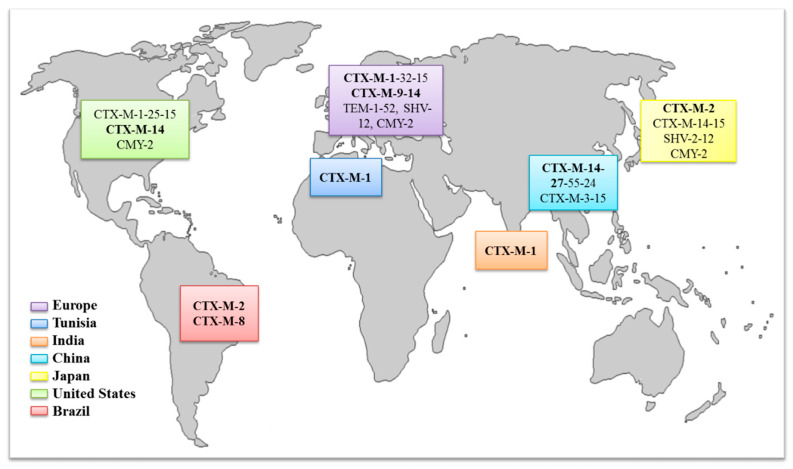
There are several different types of β-lactamase that can confer resistance to third-generation cephalosporins. These are conveniently subdivided into four classes, designated A to D; ESBL enzymes of the TEM, SHV and CTX-M families belong to class A, while class C includes the AmpC β-lactamases [52]. In animals, the most common genes associated with this resistance are blaCTX-M-1, blaCTX-M-2, blaCTX-M-14, blaCTX-M-15, blaTEM-52 and blaSHV-12 [102]. Figure 2 and Figure 3 show the distribution of ESBL enzymes detected in pigs, cattle and poultry in Europe and the global distribution of the ESBL enzymes most frequently detected in E. coli isolates from food-producing animals, respectively.
Figure 2.
Distribution of ESBL enzymes in isolates from food-producing animals in Europe [102].
Figure 3.
Global distribution of ESBL enzymes frequently (bold) detected in E. coli isolates from food-producing animals [71,103,104,105].
Looking at the world distribution of genes responsible for resistance to extended-spectrum cephalosporins, the CTX-M-1 group (CTX-M-1 and -15) is predominant in European countries. Additionally, the CTX-M-9 group (CTX-M-9 and -14) has been frequently identified in animals from Spain, Portugal and the United Kingdom. The CTX-M-2 group has been mainly described in South America and Japan, whereas, in China, enzymes of the CTX-M-9 group are prevalent, and in the United States or North Africa, the enzymes of the CTX-M-1 group are frequently identified. Apart from this general overview, CTX-M-15 and CTX-M-14 are, by far, the most important ones, since they are broadly distributed in food-producing animals and humans and are commonly detected in clinically important pathogens [105].
Nowadays, the global spread, and high prevalence, of CTX-M enzymes in E. coli is a matter of concern in both human and veterinary medicines. Although the dominant variants of CTX-Ms can be geographically different, in humans, CTX-M-15 and CTX-M-14 are among the most common variants detected worldwide in clinically important pathogens [71,105], whereas, overall, in food-producing animals, the most commonly reported genes encode for CTXM-type enzymes (e.g., CTX-M-1, -2, -9, -14, -15, -32 and -55), followed by SHV-12 and TEM-52 ESBLs [71,102]. In particular, the CTX-M-1 is broadly disseminated among food-producing animals in Europe. However, it is rarely reported in other regions and settings [102]. On the other hand, although CTX-M-15 has spread in a pandemic fashion in humans, they were only detected incidentally in poultry in European countries, whereas pets (15%) and cattle/pigs (8%) are frequently associated with this enzyme type [71]. Furthermore, the zoonotic potential of ESBL-producing bacteria and the fact that CTX-M expression is often associated with a co-resistance to other “critical important antibiotics” can have direct implications in human health by reducing treatment options. This underlines the need to consider carefully the use of fluoroquinolones, colistin or third- and fourth-generation cephalosporins as treatment options in animals in view of their critical importance in the treatment of systemic or invasive Gram-negative bacterial infections in humans.
4. Conclusions
All over the world, antibiotic resistance is commonly detected among commensal bacteria from food-producing animals, raising important questions on the potential impact of antibiotic use in animals and the possible transmission of these resistant bacteria to humans through the food chain. The use, in food-producing animals, of antibiotics that are critically important in human medicine has been implicated in the emergence of new forms of resistant bacteria, including new strains of multidrug-resistant foodborne bacteria, such as ESBL-producing E. coli. The ample, rapid dissemination of ESBLs among commensal and pathogenic E. coli strains, in humans, domestic animals and environmental sources, during the last two decades makes them an important threat in terms of public health. Addressing this challenge requires a continued research effort towards a better understanding of the nature and dissemination pathways of ESBLs and of the bacterial strains that bear them. A relentless vigilance of the evolution of the ESBL situation and the application of a One Health interdisciplinary approach is necessary to keep this problem under control.
Author Contributions
Conceptualization, S.R., M.T.T.-J., G.I. and P.P.; data curation, S.R., V.S., M.C. and M.d.L.E.D.; writing—original draft preparation, S.R. and V.S.; and supervision, G.I. and P.P. All authors have read and agreed to the published version of the manuscript.
Funding
Vanessa Silva is grateful to FCT (Fundação para a Ciência e a Tecnologia) for financial support through PhD grant SFRH/BD/137947/2018. This work was supported by the Associate Laboratory for Green Chemistry—LAQV, which is financed by national funds from FCT/MCTES (UIDB/50006/2020). The authors express their gratitude to the Regional Government of the Azores for funding the Open Access publication of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lindstedt B.-A., Finton M.D., Porcellato D., Brandal L.T. High frequency of hybrid Escherichia coli strains with combined Intestinal Pathogenic Escherichia coli (IPEC) and Extraintestinal Pathogenic Escherichia coli (ExPEC) virulence factors isolated from human faecal samples. BMC Infect. Dis. 2018;18:544. doi: 10.1186/s12879-018-3449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alizade H., Hosseini Teshnizi S., Azad M., Shojae S., Gouklani H., Davoodian P., Ghanbarpour R. An overview of diarrheagenic Escherichia coli in Iran: A systematic review and meta-analysis. J. Res. Med. Sci. 2019;24:23. doi: 10.4103/jrms.JRMS_256_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basak Unver K., Ahmet K. Vero-Toxigenic Escherichia coli (VTEC): To sum up all we know. J. Gastroenterol. Res. 2017;1:14–23. doi: 10.36959/621/583. [DOI] [Google Scholar]
- 4.Nileshkumar V., Hati S., Gawai K., Sreeja V. Food borne pathogens: A threat to dairy industry. Res. Rev. J. Dairy Sci. Technol. 2015;4:28–36. [Google Scholar]
- 5.Nobili G., Franconieri I., La Bella G., Basanisi M.G., La Salandra G. Prevalence of Verocytotoxigenic Escherichia coli strains isolated from raw beef in southern Italy. Int. J. Food Microbiol. 2017;257:201–205. doi: 10.1016/j.ijfoodmicro.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 6.Newell D.G., Koopmans M., Verhoef L., Duizer E., Aidara-Kane A., Sprong H., Opsteegh M., Langelaar M., Threfall J., Scheutz F., et al. Food-borne diseases—The challenges of 20 years ago still persist while new ones continue to emerge. Int. J. Food Microbiol. 2010;139:S3–S15. doi: 10.1016/j.ijfoodmicro.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nielsen D.W., Ricker N., Barbieri N.L., Allen H.K., Nolan L.K., Logue C.M. Outer membrane protein A (OmpA) of extraintestinal pathogenic Escherichia coli. BMC Res. Notes. 2020;13:51. doi: 10.1186/s13104-020-4917-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stromberg Z.R., Johnson J.R., Fairbrother J.M., Kilbourne J., Van Goor A., Curtiss Rd R., Mellata M. Evaluation of Escherichia coli isolates from healthy chickens to determine their potential risk to poultry and human health. PLoS ONE. 2017;12:e0180599. doi: 10.1371/journal.pone.0180599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manges A.R., Johnson J.R. Food-borne origins of Escherichia coli causing extraintestinal infections. Clin. Infect. Dis. 2012;55:712–719. doi: 10.1093/cid/cis502. [DOI] [PubMed] [Google Scholar]
- 10.Manges A.R. Escherichia coli and urinary tract infections: The role of poultry-meat. Clin. Microbiol. Infect. 2016;22:122–129. doi: 10.1016/j.cmi.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Manges A.R., Johnson J.R. Reservoirs of extraintestinal pathogenic Escherichia coli. Microbiol. Spectr. 2015;3 doi: 10.1128/microbiolspec.UTI-0006-2012. [DOI] [PubMed] [Google Scholar]
- 12.García-Meniño I., García V., Mora A., Díaz-Jiménez D., Flament-Simon S.C., Alonso M.P., Blanco J.E., Blanco M., Blanco J. Swine enteric colibacillosis in Spain: Pathogenic potential of mcr-1 ST10 and ST131 E. coli isolates. Front. Microbiol. 2018;9:2659. doi: 10.3389/fmicb.2018.02659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Müller A., Stephan R., Nüesch-Inderbinen M. Distribution of virulence factors in ESBL-producing Escherichia coli isolated from the environment, livestock, food and humans. Sci. Total Environ. 2016;541:667–672. doi: 10.1016/j.scitotenv.2015.09.135. [DOI] [PubMed] [Google Scholar]
- 14.Eibach D., Dekker D., Gyau Boahen K., Wiafe Akenten C., Sarpong N., Belmar Campos C., Berneking L., Aepfelbacher M., Krumkamp R., Owusu-Dabo E., et al. Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in local and imported poultry meat in Ghana. Vet. Microbiol. 2018;217:7–12. doi: 10.1016/j.vetmic.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 15.Chakraborty A., Saralaya V., Adhikari P., Shenoy S., Baliga S., Hegde A. Characterization of Escherichia coli phylogenetic groups associated with extraintestinal infections in South Indian population. Ann. Med. Health Sci. Res. 2015;5:241–246. doi: 10.4103/2141-9248.160192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koga V.L., Tomazetto G., Cyoia P.S., Neves M.S., Vidotto M.C., Nakazato G., Kobayashi R.K.T. Molecular screening of virulence genes in extraintestinal pathogenic Escherichia coli isolated from human blood culture in Brazil. Biomed. Res. Int. 2014;2014:465054. doi: 10.1155/2014/465054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarowska J., Futoma-Koloch B., Jama-Kmiecik A., Frej-Madrzak M., Ksiazczyk M., Bugla-Ploskonska G., Choroszy-Krol I. Virulence factors, prevalence and potential transmission of extraintestinal pathogenic Escherichia coli isolated from different sources: Recent reports. Gut Pathog. 2019;11:10. doi: 10.1186/s13099-019-0290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raimondi S., Righini L., Candeliere F., Musmeci E., Bonvicini F., Gentilomi G., Erjavec M.S., Amaretti A., Rossi M. Antibiotic resistance, virulence factors, phenotyping, and genotyping of E. coli isolated from the feces of healthy subjects. Microorganisms. 2019;7:251. doi: 10.3390/microorganisms7080251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nyirabahizi E., Tyson G.H., Dessai U., Zhao S., Kabera C., Crarey E., Womack N., Crews M.K., Strain E., Tate H. Evaluation of Escherichia coli as an indicator for antimicrobial resistance in Salmonella recovered from the same food or animal ceca samples. Food Control. 2020;115:107280. doi: 10.1016/j.foodcont.2020.107280. [DOI] [Google Scholar]
- 20.ECDC . Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2017. ECDC; Stockholm, Sweden: 2018. [Google Scholar]
- 21.EFSA The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2017. EFSA J. 2019;17:5598. doi: 10.2903/j.efsa.2019.5598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niero G., Bortolaia V., Vanni M., Intorre L., Guardabassi L., Piccirillo A. High diversity of genes and plasmids encoding resistance to third-generation cephalosporins and quinolones in clinical Escherichia coli from commercial poultry flocks in Italy. Vet. Microbiol. 2018;216:93–98. doi: 10.1016/j.vetmic.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 23.Hille K., Ruddat I., Schmid A., Hering J., Hartmann M., von Münchhausen C., Schneider B., Messelhäusser U., Friese A., Mansfeld R., et al. Cefotaxime-resistant E. coli in dairy and beef cattle farms—Joint analyses of two cross-sectional investigations in Germany. Prev. Vet. Med. 2017;142:39–45. doi: 10.1016/j.prevetmed.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen D.P., Nguyen T.A.D., Le T.H., Tran N.M.D., Ngo T.P., Dang V.C., Kawai T., Kanki M., Kawahara R., Jinnai M., et al. Dissemination of extended-spectrum β-lactamase- and AmpC β-Lactamase-producing Escherichia coli within the food distribution system of Ho Chi Minh City, Vietnam. Biomed. Res. Int. 2016;2016:8182096. doi: 10.1155/2016/8182096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seo K.W., Lee Y.J. Characterization of plasmid mediated quinolone resistance determinants in ciprofloxacin resistant-Escherichia coli from chicken meat produced by integrated broiler operations in Korea. Int. J. Food Microbiol. 2019;307:108274. doi: 10.1016/j.ijfoodmicro.2019.108274. [DOI] [PubMed] [Google Scholar]
- 26.Lambrecht E., Van Meervenne E., Boon N., Van de Wiele T., Wattiau P., Herman L., Heyndrickx M., Van Coillie E. Characterization of cefotaxime- and ciprofloxacin-resistant commensal Escherichia coli originating from Belgian farm animals indicates high antibiotic resistance transfer rates. Microb. Drug Resist. 2017;24:707–717. doi: 10.1089/mdr.2017.0226. [DOI] [PubMed] [Google Scholar]
- 27.Wasyl D., Hoszowski A., Zając M., Szulowski K. Antimicrobial resistance in commensal Escherichia coli isolated from animals at slaughter. Front. Microbiol. 2013;4:221. doi: 10.3389/fmicb.2013.00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cummings K.J., Aprea V.A., Altier C. Antimicrobial resistance trends among Escherichia coli isolates obtained from dairy cattle in the Northeastern United States, 2004–2011. Foodborne Pathog. Dis. 2013;11:61–67. doi: 10.1089/fpd.2013.1605. [DOI] [PubMed] [Google Scholar]
- 29.Myrenås M., Slettemeås J.S., Thorsteinsdottir T.R., Bengtsson B., Börjesson S., Nilsson O., Landén A., Sunde M. Clonal spread of Escherichia coli resistant to cephalosporins and quinolones in the Nordic broiler production. Vet. Microbiol. 2018;213:123–128. doi: 10.1016/j.vetmic.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Hang B.P.T., Wredle E., Börjesson S., Sjaunja K.S., Dicksved J., Duse A. High level of multidrug-resistant Escherichia coli in young dairy calves in southern Vietnam. Trop. Anim. Health Prod. 2019;51:1405–1411. doi: 10.1007/s11250-019-01820-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Callens B., Cargnel M., Sarrazin S., Dewulf J., Hoet B., Vermeersch K., Wattiau P., Welby S. Associations between a decreased veterinary antimicrobial use and resistance in commensal Escherichia coli from Belgian livestock species (2011–2015) Prev. Vet. Med. 2018;157:50–58. doi: 10.1016/j.prevetmed.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 32.Belaynehe K.M., Shin S.W., Hong-Tae P., Yoo H.S. Occurrence of aminoglycoside-modifying enzymes among isolates of Escherichia coli exhibiting high levels of aminoglycoside resistance isolated from Korean cattle farms. FEMS Microbiol. Lett. 2017;364 doi: 10.1093/femsle/fnx129. [DOI] [PubMed] [Google Scholar]
- 33.Slettemeås J.S., Sunde M., Ulstad C.R., Norström M., Wester A.L., Urdahl A.M. Occurrence and characterization of quinolone resistant Escherichia coli from Norwegian turkey meat and complete sequence of an IncX1 plasmid encoding qnrS1. PLoS ONE. 2019;14:e0212936. doi: 10.1371/journal.pone.0212936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahmed M.A.E.E., Zhong L.-L., Shen C., Yang Y., Doi Y., Tian G.-B. Colistin and its role in the era of antibiotic resistance: An extended review (2000–2019) Emerg. Microbes Infect. 2020;9:868–885. doi: 10.1080/22221751.2020.1754133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schrijver R., Stijntjes M., Rodríguez-Baño J., Tacconelli E., Babu Rajendran N., Voss A. Review of antimicrobial resistance surveillance programmes in livestock and meat in EU with focus on humans. Clin. Microbiol. Infect. 2018;24:577–590. doi: 10.1016/j.cmi.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Azam H., Ghezeljeh S.M., Mahmoud S. Prevalence of class 1 and 2 integrons among the multidrug resistant uropathogenic strains of Escherichia coli. Asian Biomed. 2017;9:49–54. doi: 10.5372/1905-7415.0901.367. [DOI] [Google Scholar]
- 37.Wyrsch E.R., Reid C.J., DeMaere M.Z., Liu M.Y., Chapman T.A., Roy Chowdhury P., Djordjevic S.P. Complete sequences of multiple-drug resistant IncHI2 ST3 plasmids in Escherichia coli of porcine origin in Australia. Front. Sustain. Food Syst. 2019;3:18. doi: 10.3389/fsufs.2019.00018. [DOI] [Google Scholar]
- 38.Mbelle N.M., Feldman C., Osei Sekyere J., Maningi N.E., Modipane L., Essack S.Y. The resistome, mobilome, virulome and phylogenomics of multidrug-resistant Escherichia coli clinical isolates from Pretoria, South Africa. Sci. Rep. 2019;9:16457. doi: 10.1038/s41598-019-52859-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reid C.J., Wyrsch E.R., Roy Chowdhury P., Zingali T., Liu M., Darling A.E., Chapman T.A., Djordjevic S.P. Porcine commensal Escherichia coli: A reservoir for class 1 integrons associated with IS26. Microb. Genom. 2017;3:e000143. doi: 10.1099/mgen.0.000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Falagas M.E., Karageorgopoulos D.E. Extended-spectrum beta-lactamase-producing organisms. J. Hosp. Infect. 2009;73:345–354. doi: 10.1016/j.jhin.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 41.Cassini A., Högberg L.D., Plachouras D., Quattrocchi A., Hoxha A., Simonsen G.S., Colomb-Cotinat M., Kretzshcmar M.E., Devlesschauwer B., Cecchini M., et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwaber M.J., Carmeli Y. Mortality and delay in effective therapy associated with extended-spectrum beta-lactamase production in Enterobacteriaceae bacteraemia: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2007;60:913–920. doi: 10.1093/jac/dkm318. [DOI] [PubMed] [Google Scholar]
- 43.Mughini-Gras L., Dorado-García A., van Duijkeren E., van den Bunt G., Dierikx C.M., Bonten M.J.M., Bootsma M.C.J., Schmitt H., Hald T., Evers E.G., et al. Attributable sources of community-acquired carriage of Escherichia coli containing β-lactam antibiotic resistance genes: A population-based modelling study. Lancet Planet Health. 2019;3:e357–e369. doi: 10.1016/S2542-5196(19)30130-5. [DOI] [PubMed] [Google Scholar]
- 44.Cantón R., Novais A., Valverde A., Machado E., Peixe L., Baquero F., Coque T.M. Prevalence and spread of extended-spectrum β-lactamase-producing Enterobacteriaceae in Europe. Clin. Microbiol. Infect. 2008;14:144–153. doi: 10.1111/j.1469-0691.2007.01850.x. [DOI] [PubMed] [Google Scholar]
- 45.Bezabih Y.M., Sabiiti W., Alamneh E., Bezabih A., Peterson G.M., Bezabhe W.M., Roujeinikova A. The global prevalence and trend of human intestinal carriage of ESBL-producing Escherichia coli in the community. J. Antimicrob. Chemother. 2020:dkaa399. doi: 10.1093/jac/dkaa399. [DOI] [PubMed] [Google Scholar]
- 46.Mueller L., Cimen C., Poirel L., Descombes M.-C., Nordmann P. Prevalence of fosfomycin resistance among ESBL-producing Escherichia coli isolates in the community, Switzerland. Eur. J. Clin. Microbiol. Infect. Dis. 2019;38:945–949. doi: 10.1007/s10096-019-03531-0. [DOI] [PubMed] [Google Scholar]
- 47.Adler M., Anjum M., Andersson D.I., Sandegren L. Combinations of mutations in envZ, ftsI, mrdA, acrB and acrR can cause high-level carbapenem resistance in Escherichia coli. J. Antimicrob. Chemother. 2016;71:1188–1198. doi: 10.1093/jac/dkv475. [DOI] [PubMed] [Google Scholar]
- 48.Patterson D.L., Bonomo R.A. Extended-spectrum β-lactamases: A clinical update. Clin. Microbiol. Rev. 2005;18:657–686. doi: 10.1128/CMR.18.4.657-686.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sawa T., Kooguchi K., Moriyama K. Molecular diversity of extended-spectrum β-lactamases and carbapenemases, and antimicrobial resistance. J. Intensive Care. 2020;8:13. doi: 10.1186/s40560-020-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rawat D., Nair D. Extended-spectrum β-lactamases in Gram negative bacteria. J. Glob. Infect. Dis. 2010;2:263–274. doi: 10.4103/0974-777X.68531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smet A., Martel A., Persoons D., Dewulf J., Heyndrickx M., Herman L., Haesebrouck F., Butaye P. Broad-spectrum β-lactamases among Enterobacteriaceae of animal origin: Molecular aspects, mobility and impact on public health. FEMS Microbiol. Rev. 2010;34:295–316. doi: 10.1111/j.1574-6976.2009.00198.x. [DOI] [PubMed] [Google Scholar]
- 52.Cantón R., González-Alba J.M., Galán J.C. CTX-M enzymes: Origin and diffusion. Front. Microbiol. 2012;3:110. doi: 10.3389/fmicb.2012.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jena J., Sahoo R.K., Debata N.K., Subudhi E. Prevalence of TEM, SHV, and CTX-M genes of extended-spectrum β-lactamase-producing Escherichia coli strains isolated from urinary tract infections in adults. 3 Biotech. 2017;7:244. doi: 10.1007/s13205-017-0879-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Manyahi J., Moyo S.J., Tellevik M.G., Ndugulile F., Urassa W., Blomberg B., Langeland N. Detection of CTX-M-15 beta-lactamases in Enterobacteriaceae causing hospital- and community-acquired urinary tract infections as early as 2004, in Dar es Salaam, Tanzania. BMC Infect. Dis. 2017;17:282. doi: 10.1186/s12879-017-2395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barrios H., Garza-Ramos U., Mejia-Miranda I., Reyna-Flores F., Sánchez-Pérez A., Mosqueda-García D., Silva-Sanchez J. ESBL-producing Escherichia coli and Klebsiella pneumoniae: The most prevalent clinical isolates obtained between 2005 and 2012 in Mexico. J. Glob. Antimicrob. Resist. 2017;10:243–246. doi: 10.1016/j.jgar.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 56.Falgenhauer L., Imirzalioglu C., Ghosh H., Gwozdzinski K., Schmiedel J., Gentil K., Bauerfeind R., Kämpfer P., Seifert H., Michael G.B., et al. Circulation of clonal populations of fluoroquinolone-resistant CTX-M-15-producing Escherichia coli ST410 in humans and animals in Germany. Int. J. Antimicrob. Agents. 2016;47:457–465. doi: 10.1016/j.ijantimicag.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 57.Nascimento T., Cantamessa R., Melo L., Fernandes M.R., Fraga E., Dropa M., Sato M.I.Z., Cerdeira L., Lincopan N. International high-risk clones of Klebsiella pneumoniae KPC-2/CC258 and Escherichia coli CTX-M-15/CC10 in urban lake waters. Sci. Total Environ. 2017;598:910–915. doi: 10.1016/j.scitotenv.2017.03.207. [DOI] [PubMed] [Google Scholar]
- 58.Naseer U., Sundsfjord A. The CTX-M Conundrum: Dissemination of plasmids and Escherichia coli clones. Microb. Drug Resist. 2011;17:83–97. doi: 10.1089/mdr.2010.0132. [DOI] [PubMed] [Google Scholar]
- 59.Lee K., Yong D., Jeong S.H., Tulgaa K., Docquier J.-D., Rossolini G.M., Chong Y. Genetic and biochemical characterisation of CTX-M-37 extended-spectrum β-lactamase from an Enterobacter cloacae clinical isolate from Mongolia. J. Glob. Antimicrob. Resist. 2017;10:3–7. doi: 10.1016/j.jgar.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 60.Akya A., Ahmadi M., Khodamoradi S., Rezaei M.R., Karani N., Elahi A., Lorestani R.C., Rezaei M. Prevalence of blaCTX-M, blaCTX-M-2, blaCTX-M-8, blaCTX-M-25 and blaCTX-M-3 genes in Escherichia coli isolated from urinary tract infection in Kermanshah City, Iran. J. Clin. Diagnostic Res. 2019;13:DC04–DC07. doi: 10.7860/JCDR/2019/40684.13055. [DOI] [Google Scholar]
- 61.Poirel L., Naas T., Nordmann P. Genetic support of extended-spectrum β-lactamases. Clin. Microbiol. Infect. 2008;14:75–81. doi: 10.1111/j.1469-0691.2007.01865.x. [DOI] [PubMed] [Google Scholar]
- 62.Hamamoto K., Hirai I. Characterisation of chromosomally-located blaCTX-M and its surrounding sequence in CTX-M-type extended-spectrum β-lactamase-producing Escherichia coli isolates. J. Glob. Antimicrob. Resist. 2019;17:53–57. doi: 10.1016/j.jgar.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 63.Stohr J.J.J.M., Kluytmans-van den Bergh M.F.Q., Wedema R., Friedrich A.W., Kluytmans J.A.J.W., Rossen J.W.A. Detection of extended-spectrum beta-lactamase (ESBL) genes and plasmid replicons in Enterobacteriaceae using PlasmidSPAdes assembly of short-read sequence data. bioRxiv. 2019:863316. doi: 10.1101/863316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li P., Shen K., Zhang Y., Ying J., Zhu T., Liu Y., Xu L., Lin C., Zhang K., Li P., et al. Characterization of a Novel blaKLUC variant with reduced β-lactam resistance from an IncA/C group plasmid in a clinical Klebsiella pneumoniae isolate. Front. Microbiol. 2018;9:1908. doi: 10.3389/fmicb.2018.01908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhao W.-H., Hu Z.-Q. Epidemiology and genetics of CTX-M extended-spectrum β-lactamases in Gram-negative bacteria. Crit. Rev. Microbiol. 2013;39:79–101. doi: 10.3109/1040841X.2012.691460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seiffert S.N., Hilty M., Perreten V., Endimiani A. Extended-spectrum cephalosporin-resistant gram-negative organisms in livestock: An emerging problem for human health? Drug Resist. Updat. 2013;16:22–45. doi: 10.1016/j.drup.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 67.Singh N.S., Singhal N., Virdi J.S. Genetic environment of blaTEM-1, blaCTX-M-15, blaCMY-42 and characterization of integrons of Escherichia coli isolated from an Indian urban aquatic environment. Front. Microbiol. 2018;9:382. doi: 10.3389/fmicb.2018.00382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liebana E., Carattoli A., Coque T.M., Hasman H., Magiorakos A.-P., Mevius D., Peixe L., Poirel L., Schuepbach-Regula G., Torneke K., et al. Public health risks of enterobacterial isolates producing extended-epectrum β-lactamases or AmpC β-lactamases in food and food-producing animals: An EU perspective of epidemiology, analytical methods, risk factors, and control options. Clin. Infect. Dis. 2012;56:1030–1037. doi: 10.1093/cid/cis1043. [DOI] [PubMed] [Google Scholar]
- 69.Shafiq M., Huang J., Ur Rahman S., Shah J.M., Chen L., Gao Y., Wang M., Wang L. High incidence of multidrug-resistant Escherichia coli coharboring mcr-1 and bla (CTX-M-15) recovered from pigs. Infect. Drug Resist. 2019;12:2135–2149. doi: 10.2147/IDR.S209473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Woodford N., Turton J.F., Livermore D.M. Multiresistant Gram-negative bacteria: The role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiol. Rev. 2011;35:736–755. doi: 10.1111/j.1574-6976.2011.00268.x. [DOI] [PubMed] [Google Scholar]
- 71.Ewers C., Bethe A., Semmler T., Guenther S., Wieler L.H. Extended-spectrum β-lactamase-producing and AmpC-producing Escherichia coli from livestock and companion animals, and their putative impact on public health: A global perspective. Clin. Microbiol. Infect. 2012;18:646–655. doi: 10.1111/j.1469-0691.2012.03850.x. [DOI] [PubMed] [Google Scholar]
- 72.Flament-Simon S.-C., Nicolas-Chanoine M.-H., García V., Duprilot M., Mayer N., Alonso M.P., García-Meniño I., Blanco J.E., Blanco M., Blanco J. Clonal structure, virulence factor-encoding genes and antibiotic resistance of Escherichia coli causing urinary tract infections and other extraintestinal infections in humans in Spain and France during 2016. Antibiotics. 2020;9:161. doi: 10.3390/antibiotics9040161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Harris P.N.A., Ben Zakour N.L., Roberts L.W., Wailan A.M., Zowawi H.M., Tambyah P.A., Lye D.C., Jureen R., Lee T.H., Yin M., et al. Whole genome analysis of cephalosporin-resistant Escherichia coli from bloodstream infections in Australia, New Zealand and Singapore: High prevalence of CMY-2 producers and ST131 carrying blaCTX-M-15 and blaCTX-M-27. J Antimicrob. Chemother. 2018;73:634–642. doi: 10.1093/jac/dkx466. [DOI] [PubMed] [Google Scholar]
- 74.Mostafavi S.K.S., Najar-Peerayeh S., Mobarez A.M., Parizi M.K. Characterization of uropathogenic E. coli O25b-B2-ST131, O15:K52:H1, and CGA: Neutrophils apoptosis, serum bactericidal assay, biofilm formation, and virulence typing. J. Cell. Physiol. 2019;234:18272–18282. doi: 10.1002/jcp.28459. [DOI] [PubMed] [Google Scholar]
- 75.Usein C.-R., Papagheorghe R., Oprea M., Condei M., Strãuţ M. Molecular characterization of bacteremic Escherichia coli isolates in Romania. Folia Microbiol. (Praha) 2016;61:221–226. doi: 10.1007/s12223-015-0427-6. [DOI] [PubMed] [Google Scholar]
- 76.Dominguez J.E., Redondo L.M., Figueroa Espinosa R.A., Cejas D., Gutkind G.O., Chacana P.A., Di Conza J.A., Fernández Miyakawa M.E. Simultaneous carriage of mcr-1 and other antimicrobial resistance determinants in Escherichia coli from poultry. Front. Microbiol. 2018;9:1679. doi: 10.3389/fmicb.2018.01679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barilli E., Vismarra A., Villa Z., Bonilauri P., Bacci C. ESβL E. coli isolated in pig’s chain: Genetic analysis associated to the phenotype and biofilm synthesis evaluation. Int. J. Food Microbiol. 2019;289:162–167. doi: 10.1016/j.ijfoodmicro.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 78.Dohmen W., Dorado-García A., Bonten M.J.M., Wagenaar J.A., Mevius D., Heederik D.J.J. Risk factors for ESBL-producing Escherichia coli on pig farms: A longitudinal study in the context of reduced use of antimicrobials. PLoS ONE. 2017;12:e0174094. doi: 10.1371/journal.pone.0174094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ramos S., Silva N., Dias D., Sousa M., Capelo-Martinez J.L., Brito F., Caniça M., Igrejas G., Poeta P. Clonal diversity of ESBL-producing Escherichia coli in pigs at slaughter level in Portugal. Foodborne Pathog. Dis. 2012;10:74–79. doi: 10.1089/fpd.2012.1173. [DOI] [PubMed] [Google Scholar]
- 80.Randall L.P., Lemma F., Rogers J.P., Cheney T.E.A., Powell L.F., Teale C.J. Prevalence of extended-spectrum-β-lactamase-producing Escherichia coli from pigs at slaughter in the UK in 2013. J. Antimicrob. Chemother. 2014;69:2947–2950. doi: 10.1093/jac/dku258. [DOI] [PubMed] [Google Scholar]
- 81.Hering J., Hille K., Frömke C., von Münchhausen C., Hartmann M., Schneider B., Friese A., Roesler U., Merle R., Kreienbrock L. Prevalence and potential risk factors for the occurrence of cefotaxime resistant Escherichia coli in German fattening pig farms—A cross-sectional study. Prev. Vet. Med. 2014;116:129–137. doi: 10.1016/j.prevetmed.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 82.Ramos S., Igrejas G., Silva N., Jones-Dias D., Capelo-Martinez J.-L., Caniça M., Poeta P. First report of CTX-M producing Escherichia coli, including the new ST2526, isolated from beef cattle and sheep in Portugal. Food Control. 2013;31:208–210. doi: 10.1016/j.foodcont.2012.10.011. [DOI] [Google Scholar]
- 83.Haenni M., Châtre P., Métayer V., Bour M., Signol E., Madec J.-Y., Gay E. Comparative prevalence and characterization of ESBL-producing Enterobacteriaceae in dominant versus subdominant enteric flora in veal calves at slaughterhouse, France. Vet. Microbiol. 2014;171:321–327. doi: 10.1016/j.vetmic.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 84.Velasova M., Smith R.P., Lemma F., Horton R.A., Duggett N.A., Evans J., Tongue S.C., Anjum M.F., Randall L.P. Detection of extended-spectrum β-lactam, AmpC and carbapenem resistance in Enterobacteriaceae in beef cattle in Great Britain in 2015. J. Appl. Microbiol. 2019;126:1081–1095. doi: 10.1111/jam.14211. [DOI] [PubMed] [Google Scholar]
- 85.Zheng B., Feng C., Xu H., Yu X., Guo L., Jiang X., Song X. Detection and characterization of ESBL-producing Escherichia coli expressing mcr-1 from dairy cows in China. J. Antimicrob. Chemother. 2018;74:321–325. doi: 10.1093/jac/dky446. [DOI] [PubMed] [Google Scholar]
- 86.Gonggrijp M.A., Santman-Berends I.M.G.A., Heuvelink A.E., Buter G.J., van Schaik G., Hage J.J., Lam T.J.G.M. Prevalence and risk factors for extended-spectrum β-lactamase- and AmpC-producing Escherichia coli in dairy farms. J. Dairy Sci. 2016;99:9001–9013. doi: 10.3168/jds.2016-11134. [DOI] [PubMed] [Google Scholar]
- 87.Boonyasiri A., Tangkoskul T., Seenama C., Saiyarin J., Tiengrim S., Thamlikitkul V. Prevalence of antibiotic resistant bacteria in healthy adults, foods, food animals, and the environment in selected areas in Thailand. Pathog. Glob. Health. 2014;108:235–245. doi: 10.1179/2047773214Y.0000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nuangmek A., Rojanasthien S., Chotinun S., Yamsakul P., Tadee P., Thamlikitkul V., Tansakul N., Patchanee P. Antimicrobial resistance in ESBL-producing Escherichia coli isolated from layer and pig farms in Thailand. Acta Sci. Vet. 2018;46:1538. doi: 10.22456/1679-9216.81823. [DOI] [Google Scholar]
- 89.Reich F., Schill F., Atanassova V., Klein G. Quantification of ESBL-Escherichia coli on broiler carcasses after slaughtering in Germany. Food Microbiol. 2016;54:1–5. doi: 10.1016/j.fm.2015.10.020. [DOI] [Google Scholar]
- 90.Casella T., Nogueira M.C.L., Saras E., Haenni M., Madec J.-Y. High prevalence of ESBLs in retail chicken meat despite reduced use of antimicrobials in chicken production, France. Int. J. Food Microbiol. 2017;257:271–275. doi: 10.1016/j.ijfoodmicro.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 91.Wu C., Wang Y., Shi X., Wang S., Ren H., Shen Z., Wang Y., Lin J., Wang S. Rapid rise of the ESBL and mcr-1 genes in Escherichia coli of chicken origin in China, 2008–2014. Emerg. Microbes Infect. 2018;7:1–10. doi: 10.1038/s41426-018-0033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang H., Zhai Z., Li Q., Liu L., Guo S., Li Q., Yang L., Ye C., Chang W., Zhai J. Characterization of extended-spectrum β-lactamase-producing Escherichia coli isolates from pigs and farm workers. J. Food Prot. 2016;79:1630–1634. doi: 10.4315/0362-028X.JFP-16-093. [DOI] [PubMed] [Google Scholar]
- 93.Norizuki C., Kawamura K., Wachino J., Suzuki M., Nagano N., Kondo T., Arakawa Y. Detection of Escherichia coli producing CTX-M-1-group extended-spectrum β-lactamases from pigs in Aichi prefecture, Japan, between 2015 and 2016. Jpn. J. Infect. Dis. 2017;71:33–38. doi: 10.7883/yoken.JJID.2017.206. [DOI] [PubMed] [Google Scholar]
- 94.Diab M., Hamze M., Madec J.-Y., Haenni M. High Prevalence of non-ST131 CTX-M-15-producing Escherichia coli in healthy cattle in Lebanon. Microb. Drug Resist. 2016;23:261–266. doi: 10.1089/mdr.2016.0019. [DOI] [PubMed] [Google Scholar]
- 95.Manageiro V., Clemente L., Graça R., Correia I., Albuquerque T., Ferreira E., Caniça M. New insights into resistance to colistin and third-generation cephalosporins of Escherichia coli in poultry, Portugal: Novel blaCTX-M-166 and blaESAC genes. Int. J. Food Microbiol. 2017;263:67–73. doi: 10.1016/j.ijfoodmicro.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 96.Päivärinta M., Pohjola L., Fredriksson-Ahomaa M., Heikinheimo A. Low occurrence of extended-spectrum β-lactamase-producing Escherichia coli in Finnish food-producing animals. Zoonoses Public Health. 2016;63:624–631. doi: 10.1111/zph.12277. [DOI] [PubMed] [Google Scholar]
- 97.Apostolakos I., Mughini-Gras L., Fasolato L., Piccirillo A. Assessing the occurrence and transfer dynamics of ESBL/pAmpC-producing Escherichia coli across the broiler production pyramid. PLoS ONE. 2019;14:e0217174. doi: 10.1371/journal.pone.0217174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kraemer J.G., Pires J., Kueffer M., Semaani E., Endimiani A., Hilty M., Oppliger A. Prevalence of extended-spectrum β-lactamase-producing Enterobacteriaceae and methicillin-resistant Staphylococcus aureus in pig farms in Switzerland. Sci. Total Environ. 2017;603–604:401–405. doi: 10.1016/j.scitotenv.2017.06.110. [DOI] [PubMed] [Google Scholar]
- 99.WHO . Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early Implementation 2017–2018. WHO; Geneva, Switzerland: 2018. [Google Scholar]
- 100.Poirel L., Madec J.-Y., Lupo A., Schink A.-K., Kieffer N., Nordmann P., Schwarz S. Antimicrobial Resistance in Escherichia coli. Microbiol. Spectr. 2018;6 doi: 10.1128/microbiolspec.ARBA-0026-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Liu B.-T., Song F.-J., Zou M., Zhang Q.-D., Shan H. High incidence of Escherichia coli strains coharboring mcr-1 and blaNDM from chickens. Antimicrob. Agents Chemother. 2017;61 doi: 10.1128/AAC.02347-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Silva N., Carvalho I., Currie C., Sousa M., Igrejas G., Poeta P. Extended-spectrum-β-lactamase and carbapenemase-producing Enterobacteriaceae in food-producing animals in Europe. Antibiot. Drug Resist. 2019;12:261–273. [Google Scholar]
- 103.Carattoli A. Animal reservoirs for extended spectrum β-lactamase producers. Clin. Microbiol. Infect. 2008;14:117–123. doi: 10.1111/j.1469-0691.2007.01851.x. [DOI] [PubMed] [Google Scholar]
- 104.Clemente L., Manageiro V., Correia I., Amaro A., Albuquerque T., Themudo P., Ferreira E., Caniça M. Revealing mcr-1-positive ESBL-producing Escherichia coli strains among Enterobacteriaceae from food-producing animals (bovine, swine and poultry) and meat (bovine and swine), Portugal, 2010–2015. Int. J. Food Microbiol. 2019;296:37–42. doi: 10.1016/j.ijfoodmicro.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 105.Day M.J., Hopkins K.L., Wareham D.W., Toleman M.A., Elviss N., Randall L., Teale C., Cleary P., Wiuff C., Doumith M., et al. Extended-spectrum β-lactamase-producing Escherichia coli in human-derived and food chain-derived samples from England, Wales, and Scotland: An epidemiological surveillance and typing study. Lancet Infect. Dis. 2019;19:1325–1335. doi: 10.1016/S1473-3099(19)30273-7. [DOI] [PubMed] [Google Scholar]