Abstract
Background and Objectives: The aims of this systematic review were to identify additional infection control measures implemented in dental practice globally to prevent cross-infection and evaluate the psychological impacts of the pandemic among dental professionals. Materials and Methods: A sequential systematic literature search was conducted from December 2019 to 30 April 2020 through PubMed, CINAHL, Scopus, Google Scholar, Embase, and Web of Science databases. The search yielded the following results: “COVID-19” (n = 12,137), “Novel corona virus” (n = 63), “COVID-19 and dentistry” (n = 46), “COVID-19 and oral health” (n = 41), “Novel Corona virus and Dentistry” (n = 0), “dental health and Novel Coronavirus” (n = 26), and “dental practice and Novel Coronavirus” (n = 6). Results: After a careful review and eliminating articles based on inclusion and exclusion criteria, the final review included 13 articles. Management of infection control is discussed extensively in the literature and remains the main theme of many Coronavirus Disease 2019 (COVID-19) articles on dentistry. Telephone triage using a questionnaire, hand hygiene, personal protective equipment (PPE) for clinical and nonclinical staff, a preprocedural mouth rinse, and aerosol management have been discussed and implemented in few countries. Three studies recommended that elective treatments for patients with a temperature of >100.4 F or 38 °C should be postponed or performed in an airborne infection isolation room (AIIR) or negative-pressure room. Limiting the number of patients in the waiting area, the removal of shared objects, proper ventilation, and physical distancing were highly recommended. Psychological distress among dental professionals in relation to existing medical conditions and self-efficacy has been discussed. Conclusions: Although the COVID-19 pandemic has had a substantial impact on the dental profession worldwide, our review highlights many practice management approaches to adopt the new norm. More research highlighting evidence-based safety practices and multisectoral collaboration is required to help dental professionals make informed decisions and make the profession safe, both for the patient and dental professionals.
Keywords: COVID-19, pandemic, simulation, dentistry, oral health, infection control, dental practice, management
1. Introduction
Coronavirus Disease 2019 (COVID-19), a pneumonia of unknown origin, was reported in Wuhan, a town in Eastern China. The World Health Organization office in China provided the first reports of a new virus of unknown origin. A surveillance system was implemented, and patients’ throat swabs were sent to laboratories for etiological analysis [1]. The causative agent was identified by the Chinese Center for Disease Control and Prevention, and the causative Wuhan seafood market was shut down immediately [2]. Initially, the virus was named the 2019 novel coronavirus; later, it was named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), as suggested by the Coronavirus Study Group (CSG) of the International Committee on the Taxonomy of Viruses [3]. On 30 January 2020, the World Health Organization (WHO) declared the rapid spread of SARS-CoV-2 and its associated Coronavirus Disease 2019 (COVID-19) as a public health emergency of international concern with an overall case-fatality rate of 3.4% [4,5]. Precisely 34,838,209 confirmed COVID-19 cases and 1,033,356 deaths have been reported globally (as of 3 October 2020) [6].
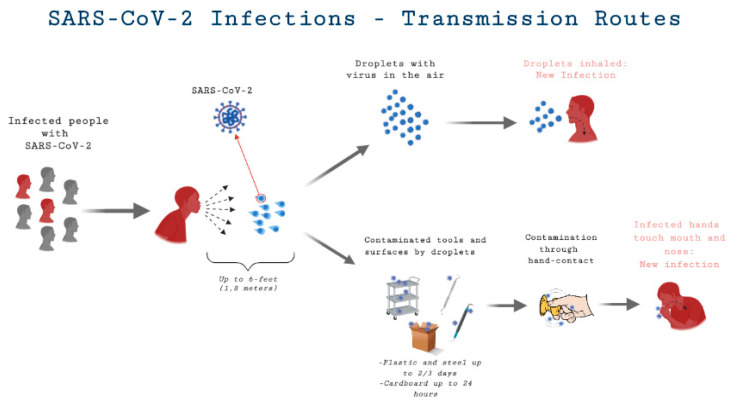
Scientific studies have shown that there are two main routes of transmission of COVID-19: direct (person-to-person touch or inhalation of short-range respiratory droplets) and indirect (airborne and fomite-mediated) [7,8,9]. Individuals may acquire indirect infection by getting into contact with contaminated surfaces and touching their oral, nasal, or ocular mucosal surfaces [10,11]. The infection is spread by large droplets formed by symptomatic patients while coughing and sneezing, which may also occur in infected, asymptomatic individuals [9,11,12,13]. Many symptoms have been reported, but the most commonly cited clinical symptoms are raised body temperature, dry cough, malaise, and dyspnea [12]. Computerized Tomography (CT) scan findings included pneumonia with anomalous findings in all cases. Although all demographics of the global population are at risk for COVID-19 infection, healthcare workers and patients hospitalized for other reasons are at a higher risk for COVID-19 due to the possibility of frequent close contact with symptomatic and/or asymptomatic individuals infected with COVID-19 [14].
The dental fraternity is experiencing a drastic transition and will continue to do so over the coming weeks and months due to the SARS-CoV-2 outbreak [15]. The consequences are far-reaching and unpredictable, particularly for the dental community and patients seeking dental care. A study from the National Institute of Health (NIH) found that aerosols containing SARS-CoV-2 remain infectious for up to 3 h in confined spaces, 4 h on copper, 24 h on cardboard, and up to 3 days on stainless steel and plastic [16]. Figure 1 demonstrates the possible route of transmission for SARS-Cov-2 in dental practice. The use of an ultrasonic scaler, a triple syringe, dental handpiece, and other high-speed-driven instruments during dental treatment can generate significant amounts of aerosols, putting dental professionals, dental teams, and their patients at high risk for contracting COVID-19 [16,17,18,19]. In the initial phases of the pandemic, there were many recommendations in the United States and elsewhere to cease nonessential dental procedures and restrict treatment to emergency care. However, with additional measures and protocols in place, many dental practices have been able to provide routine healthcare delivery during the pandemic [20,21,22,23].
Figure 1.
Coronavirus Disease 2019 (COVID-19) transmission routes.
Dental practitioners are facing uncertainty and being forced to rely on general information of COVID-19 transmission routes and other recommendations being followed by general frontline health staff to protect themselves and their patients [21]. With its outbreak, COVID-19 has raised the bar for taking additional measures along with universal infection control standard precautions.
Therefore, the aims of this systematic review were (i) to identify additional infection control measures implemented in dental practice globally to prevent cross-infection, and (ii) evaluate the psychological impact of the pandemic among dental professionals.
2. Materials and Methods
Two independent reviewers (S.S.M. and Z.A.) screened the titles and abstracts of all the identified studies to determine their relevance and whether they met the predetermined inclusion criteria (Table 1). The authors screened PubMed, Scopus, Web of Science, Embase, CINAHL, and Google Scholar databases from December 2019 to 30 April 2020 for appropriate articles addressing the question under review. The researchers carefully reviewed all the articles based on the desired outcome(s) by reading the abstracts of the relevant publications. Full texts were screened if there was insufficient detail to make a clear decision based on the inclusion criteria. A structured and logical approach to the literature search was used to identify the relevant papers that investigated COVID-19 and dental practice implications. Reference lists of original studies were manually searched to identify any articles that could have been missed during the initial search, keeping the inclusion criteria in mind. Any disagreements regarding study selection were resolved via discussion (Table 1 of inclusion and exclusion criteria).
Table 1.
Inclusion and exclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Articles published after the COVID-19 outbreak (Dec 2019 onwards) | Studies published prior to COVID-19 |
| English language only | Articles not in the English language |
| Original articles and reviews | Editorials, opinions, perspective, correspondences, case reports, case series |
| Only articles published in peer-review and indexed journals | Non-peer-reviewed/nonindexed journals |
| Databases examined (PubMed, CINAHL, Scopus, Embase, Google Scholar) | Little or no focus on dental aspects |
2.1. Outcome and Review Question
The primary outcome was “dental practice management”, particularly the management of infection control procedures through additional measures during the COVID-19 pandemic. The secondary outcome was psychological distress among dental professionals during the COVID-19 pandemic.
Based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines, a specific question was constructed [24]. The addressed question in focus was “What additional measures have been taken around the globe for the management of potentially infectious persons visiting a dental practice?”
2.2. Data Sources and Study Selection
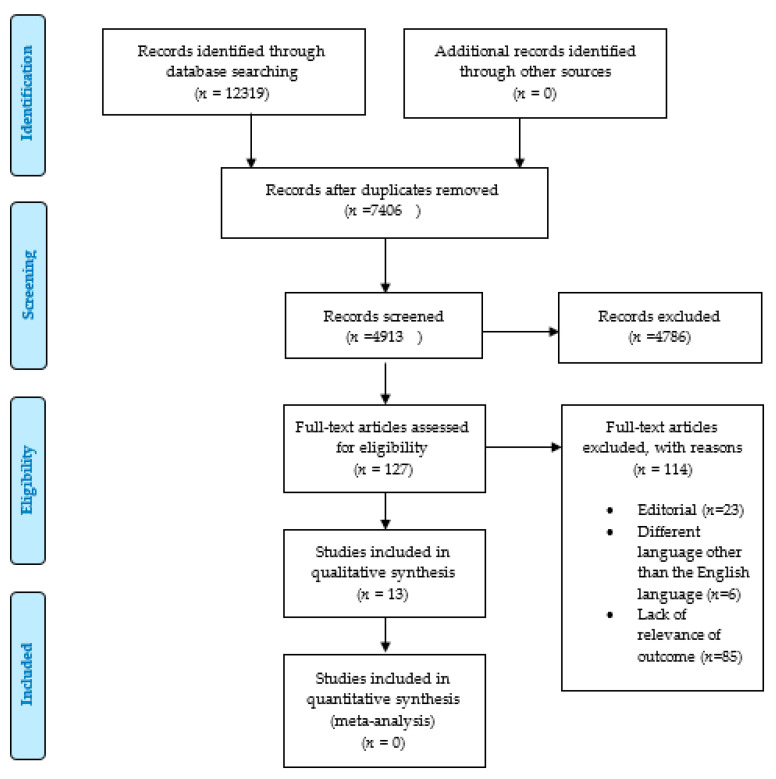
A sequential systematic literature search was conducted on the above-mentioned databases using the following keywords: “COVID-19” (n = 12,137), “Novel corona virus” (n = 63), “COVID-19 and dentistry” (n = 46), “COVID-19 and oral health” (n = 41), “Novel Corona virus and Dentistry” (n = 0), “dental health and Novel Coronavirus” (n = 26), and “dental practice and Novel Coronavirus” (n = 6) (Table 2). A Medical Subjects heading (MeSH) search strategy did not return any articles, probably due to the novelty and scarcity of articles for the topic under review. MeSH terms “Coronavirus and Dentistry,” “Corona virus and oral health,” “COVID-19 and dentistry,” and “COVID-19 and oral health” were used, which gave zero results (PRISMA flow chart, Figure 2). The search parameters used for the inclusion criteria were articles written in the English language, with at least one keyword corresponding to the above entries in the title/abstract, and studies based on the evaluation of research articles (Table 3). Original articles and systematic reviews addressing COVID-19 and dentistry were entitled to inclusion. Correspondences and editorials were not included. All keyword searches, title and abstract screenings, as well as the selection of studies, were carried out independently by two investigators (Drs. S.S.M./R.A.). Articles published before December 2019 were not included, as the subject of novel coronavirus only emerged into the scientific conscience and mainstream after December 2019. Furthermore, online outpatient department (OPD) reports/patient–physician testimonials and other online materials were skimmed for other relevant material (PRISMA flowchart, Figure 2). Given the heterogeneous and emerging sources relevant to dental aspects of COVID-19, only articles published in peer-reviewed journals were selected for final review to provide dental professionals with the highest level of evidence. We were able to gather a considerable number of studies that could serve as the initial groundwork for providing strategies to successfully manage safety in dental practice. Endnote 8.0 was used to organize the extracted references. The majority of the studies we used in the final sample are original studies and discussions based mainly on original studies; however, we included some reviews due to the dearth of articles on the topic and that, for reviewing on a scientific basis, one may evaluate other secondary or systematic review papers. Review articles were used to identify original articles on the topic of interest, and some of the conclusions of the various studies were used in the discussion. COVID-19 in dentistry has frequently been the topic of reviews in the last few months, and our project required a few review articles to build a complete scientific picture. As such, there was a crossover of some parallel review studies. This is obviously a very novel topic and an ongoing event; therefore, only original articles were evaluated for quality assessment through the Newcastle–Ottawa Scale.
Table 2.
Keywords and search strings.
| Keywords/Search Strings | Number of Entries Found |
|---|---|
| COVID-19 | 12,137 |
| COVID-19 and dentistry | 46 |
| Novel corona virus | 63 |
| COVID-19 and oral health | 41 |
| Dental practice and novel corona virus | 6 |
| Dental health and novel corona virus | 26 |
| Novel corona virus and dentistry | 0 |
Figure 2.
Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow chart.
Table 3.
Newcastle–Ottawa scale quality assessment form for nonrandomized studies included in the review.
| Selection | Comparability | Outcome | Overall | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study & Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Score (*) |
| Kamate S.T et al., 2020 [26] | * | * | * | * | * | * | 6 | ||||
| Schacham et al., 2020 [27] | * | * | * | * | * | * | * | 7 | |||
| Ahmed M.A et al., 2020 [28] | * | * | * | * | * | * | * | 7 | |||
| Khader Y et al., 2020 [29] | * | * | * | * | * | * | 6 | ||||
| Yang Y et al., 2020 [30] | * | * | * | * | * | * | * | * | 8 | ||
| Al Harbi et al., 2020 [31] | * | * | * | * | * | * | 6 | ||||
(*) = poor (0–4 *), fair (5–6 *), or good (7–9 *).
Exclusion Criteria: Studies or other materials published before December 2019 were not included in our analysis. Therefore, the selected articles were published between January 2020 and April 2020. Papers not published in peer-reviewed journals were excluded, as well as studies not matching the inclusion criteria and desired outcomes. Case reports and case series were also excluded along with editorials. Articles published in any language other than English were discarded as none of the authors were fluent in other languages.
2.3. Risk of Bias Assessment
Assessment of the risk of bias of the reviewed studies is a fundamental aspect of conducting a systematic review. Bias risk assessment in the reviewed studies was examined using the Newcastle–Ottawa scale (NOS) [25]. The NOS scale can only be applied to original studies; therefore, only original articles were graded using the NOS scale. The Newcastle–Ottawa scale is a tool for quality assessment and ranking studies by assigning them stars (*), and a modified version was used in the study, which used a 10-star rating system instead of the usual nine. The stars are ranked by 3 key domains of the study being assessed (selection, comparability, and outcome). The NOS can be interchanged with the commonly used Agency for Healthcare Research and Quality Standard Assessment (ARHQ). The more stars, the lesser the risk of bias in the studies included. Each study is rated as poor (0–4 *), fair (5–6 *), or good (7–9 *). The results of the assessment are displayed in this article (Table 3).
2.4. Statistical Analysis
For the evaluation of reliability, inter and intra observer reproducibility were evaluated using the weighted Kappa (κw) statistic using IBM SPSS for Windows version 22.0 (IBM Corp., Armonk, NY, USA).
3. Results
A total of 12,319 articles were extracted for screening (Figure 2). The removal of duplicates resulted in 4913 articles. An additional 4786 articles were excluded based on title and abstract, leaving 127 for full-text assessments. The final systematic review included 13 publications after excluding 114 articles, which comprised editorial letters, lacked relevance to our desired outcomes, or used languages other than English.
Another search was done following the same keywords from May to 30 September. It produced 1066 articles, out of which only six articles demonstrated our objective question. Out of six articles, three assessed knowledge, attitude, and awareness of dentists towards the COVID-19 pandemic [32,33,34,35]. One study assessed the risk of aerosol transmission in a dental setup [19], and another demonstrated the psychological impact of dentists towards COVID-19 [36]. Moreover, the findings were consistent with the articles published between December 2019 and 30 April 2020.
To this date (30 April 2020), six original articles and seven review articles were identified and extracted. Of 13 studies, nine addressed the primary outcome of practice management, particularly infection control management [30,31,37,38,39,40,41,42,43]. The remaining four discussed psychological distress, phobia, awareness, and self-efficacy during the COVID-19 pandemic among dental professionals [26,27,28,29]. With the majority of shortlisted publications from China [30,37,38,39,43] discussing additional infection control measures along with standard precautions, one each was conducted in Austria [40], the USA [41], and Italy [42]. A telephone triage to screen out suspected COVID-19 cases using a questionnaire was implemented in several studies [31,38,39,41,42]. Three studies recommended that elective treatments for patients coming with a temperature >100.4 F or 38 °C should be postponed if possible or performed in an airborne infection isolation room (AIIR) or negative-pressure room [31,39,41]. Minimal invasive procedures as an alternative to aerosol-generating procedures are recommended, such as the use of CariSolv for caries removal [37], extraoral radiographs [41], which are preferred over intraoral radiographs to prevent gag, and the use of a hand scaler where a rubber dam is unavailable [31]. Likewise, a two-before-and-three-after hand hygiene guideline recommended by the CDC (Centre for Disease Control) and WHO has been suggested [26,37,39,41,42]. An extraoral high-volume suction for aerosol-generating procedures [37,39], a pre-procedural mouth rinse [31,37,38,39,41,42], limiting the number of patients and displaying cough etiquette in the waiting area [39] with proper ventilation, and physical distancing were extra measures implemented to safely manage dental practice during the pandemic [30,33,36,41,43]. The theme of protective masks was recurrent in the literature, and differing views were observed. Some authors suggested wearing an FFP1/standard surgical mask for non-aerosol-generating procedures and FFP2/N95 or higher for aerosol-generating procedures [37,39]. Several others suggested using FFP2/N95 for all procedures for both clinical and nonclinical staff (clinicians and assistants) [41,42,43]. Waste management and the psychological impact of COVID-19 on the global dental workforce was another theme explored extensively in the literature [26,28,29,37,42,43].
Among four studies evaluating the psychological impact of the COVID-19 pandemic using cross-sectional surveys among dental professionals [26,27,28,29], it was observed that the majority of dental providers across the globe were nervous and frightened by the disastrous consequences of the pandemic. One of the studies highlighted the possible interaction between psychological distress in relation to self-efficacy and a pre-existing medical condition among dental professionals [27]. Dental professionals with a lower score for self-efficacy and any pre-existing medical conditions had elevated psychological distress, and vice versa [27]. A summary of the characteristics of the reviewed articles is presented in Table 4. The weighted Kappa for intraobserver reproducibility exceeded the 0.70 cut off, with a mean of 0.86, indicating almost a perfect reproducibility, while the mean weighted Kappa (κw) for interobserver reproducibility was 0.80, showing substantial reproducibility.
Table 4.
Descriptive characteristics of articles reviewed.
| First Author (Date) | Type of Article | Population/Setting | Article Key Points | Recommendations/Outcomes | Limitations |
|---|---|---|---|---|---|
| Peng, et al., 2020 [31] | Review Article | Setup: Routes of 2019-nCoV transmission and control in dental practice. Context: China | Dental care environments typically bear the possibility of contamination with 2019-nCoV owing to the complexity of its practice, which requires face-to-face contact with patients. Patients and dentists can be exposed via inhalation of suspended airborne particles, indirect contact from contaminated surfaces, and direct contact with bodily fluids of infected individuals. |
|
Lack of evidence for the effectiveness of chlorhexidine mouth rinse against 2019-nCoV |
| |||||
| |||||
| |||||
| |||||
| |||||
| |||||
| |||||
| Meng, L. et al., 2020 [32] | Review Article | Setup: Risk of cross-infection in dental settings. Context: China. | This study offers critical information regarding COVID-19 and nosocomial infections in dental settings. Management and guidelines for dental practitioners and students in (potentially) infected areas. |
|
None |
| |||||
| |||||
| Ge, Z. et al., 2020 [33] | Review Article | Setup: Transmission and control of COVID-19 infection in dental settings via aerosol. Context: China | The article emphasizes the importance of aerosol transmission of COVID-19 in dental settings and the implementation of precautionary measures to limit its spread. |
|
Distinguishing symptoms of fever and fatigue caused by dental infections from COVID-19 is merely dependent on the practitioner’s expertise. Effect of preprocedural mouth rinse against SARS-Cov-2 with oxidative agents and chlorhexidine is still unknown. |
| |||||
| |||||
| |||||
| Kamate, S.K. et al., 2020 [40] | KAP Study | Setup: 860 dental practitioners from different continents. Context: Global | The present research was conducted with the intention of evaluating the awareness, behaviors, and activities (KAP) of dental practitioners in light of the COVID-2019 pandemic. |
|
A bias in social desirability. |
|
Owing to the cross-sectional aspect of the sample and the sampling method used, the effect of self-selection of the part of the respondents may have arisen. Questionnaire bias. | ||||
| Yang, Y. et al., 2020 [34] | Original Article | Setup: 48 public tertiary dental hospitals. Context: China | The state of nonemergency dental care, emergency dental facilities, online consultation, and regional spread of hospitals were evaluated during the COVID-19 pandemic. |
|
Within the limitation of this report, we observed significant changes in the health service provision of Chinese public tertiary hospitals during the COVID-19 epidemic. Nonetheless, more research should concentrate on the possible long-term effects that the outbreak may contribute on dental treatment. |
| |||||
| Zimerman et al., 2020 [35] | Review Article | Setup: Risk of COVID 19 risk in Oral and Maxillofacial Surgery Department. Context: Vienna | The purpose of the study is therefore to compile and address facets of the treatment of patients in oral and maxillofacial surgery during the COVID-19 pandemic. |
|
Necessary investments should be made for dreadful future situations. |
| |||||
| |||||
| |||||
| Ather, A. et al., 2020 [36] | Review Article | Setup: Recommendations for clinical dental practice in COVID-19. Context: USA | The purpose of this article is to provide a summary of the epidemiology, symptoms, and mechanisms of transmission of this novel infection. Implications for clinical dental practice in response to COVID-19 have been highlighted. |
|
Likelihood of treating an asymptomatic COVID-19 patient in a dental setting is high due to the large incubation period from 0 to 24 days and mild presentation of disease in some individuals. |
| |||||
| |||||
| |||||
| |||||
| |||||
| AlHarbi, A. et al., 2020 [37] | Original Article | Setup: Recommended provisions for dental care during the COVID-19 pandemic. Context: Global | This research sought to establish recommendations for the treatment of dental patients before and after the COVID-19 pandemic. |
|
The recommendations established in this research are general guidance and the final decision will always be made at the discretion of the practitioner. |
| |||||
| |||||
| Khader, Y. et al., 2020 [41] | Cross-sectional study | Setup: 368 Jordanian dentists from private clinics, hospitals, and health centers. Context: Jordan | The study assessed the degree of understanding, interpretation, and attitude of COVID-19 and infection management among Jordanian dentists. |
|
Low response rate, Selection bias, and sampling error limits the generalizability of the findings |
| Izzeti, R. et al., 2020 [38] | Review Article | Setup: Risk of transmission of COVID-19 in dental practice and preventive measures. Context: Italy. | There is a substantial risk of direct and indirect transmission of COVID-19 among dental practitioners and between patients when performing dental procedures with handpiece under irrigation due to generation of aerosol and surface/environmental contamination. |
|
There is a lack of systemic data on the use of chlorhexidine against SARS-CoV-2. Lack of evidence, data, and unpredictable nature of this disease is affecting the adequate delivery of clinical dental care. |
| Xu, R. et al., 2020 [39] | Review Article | Setup: Role of Saliva in transmission and diagnostic tool for 2019-nCoV. Context: China | The article discusses saliva being a potential noninvasive diagnostic tool for 2019-nCoV detection and a potential transient medium for the spread of infection via short-distance droplets or sustained airborne aerosols. |
|
None |
| Ahmed, et al., 2020 [42] | Cross-sectional Study | Setup: 669 dentists from 30 different countries. Context: Global | The present research measured distress and fear of infection among dentists operating during the current viral epidemic. In addition, the dentist’s information on various practice modifications in the battle against a novel coronavirus disease epidemic has been analyzed. |
|
Information gathered over a concise span of time, keeping in mind the sudden effect this epidemic had on the mindset and dental professionals. Responses from all countries impacted by the outbreak were not received. Owing to the cross-sectional design of the research, we were unable to establish a cause-and-effect connection. |
| |||||
| Shacham, M. et al., 2020 [43] | Cross-sectional study | Setup: 338 Israeli dentists. Context: Israel. | The analysis examined the correlation of COVID-19 variables and psychological factors with psychological distress in dental workers during the outbreak of the COVID-19 pandemic. |
|
Cross-section model, which precludes causal inferences. Low response rate. Selection bias and sampling error. |
|
4. Discussion
According to local and regional health authorities’ recommendations during the COVID-19 pandemic, the protective measures that should be undertaken in a dental setting can be categorized into four phases: (a) patient triage, (b) patient evaluation upon arrival (c) during dental treatment, and (d) after dental treatment.
4.1. (a) Patient Triage Prior to Patient Arrival
Patient triage for the detection of suspected/confirmed cases of COVID-19 and determining the need for emergency and urgent dental care are among the policies and procedures that can be considered prior to the patient’s arrival at the dental clinic. Six out of the thirteen articles from different geographical locations (including China, USA, Italy) and practice settings implemented telephone triage using a questionnaire to evaluate the potential risk of SARS-Cov-2 transmission and type of dental care needed [31,37,38,39,41,42]. Telephone triage using a screening questionnaire was implemented. Emergency dental care for patients who reported symptoms of COVID-19, had contact with COVID-19-infected individuals, or traveled to regions with a high number of COVID-19 cases in the past 14 days was postponed for two weeks, and pharmacologic management of pain or infection was considered [36,41,44]. More recently, a new protocol was adopted to delay any treatment for patients with confirmed cases of COVID-19 until two consecutive negative swab tests were established taken 24 h apart [44]. A few articles mentioned that the same questionnaire should be repeated, and body temperature should be documented using a noncontact thermometer upon the patient’s arrival at the clinic [37,41,42].
4.2. (b) Patient Evaluation and Screening Upon Arrival
Screening of patients, maintaining a 1 m physical distance in the dental office, use of face masks for those accessing the dental office, patient education, and use of personal protective equipment (PPE) by dental staff are among the activities to be carried out in the dental office. The patient must be unaccompanied in the treatment room and any caregiver should remain in the waiting area [22,44]. Dental professionals should also consider reducing the number of patients in the waiting area and increasing the amount of time for each visit to complete the maximum possible treatment in one visit to reduce repeated exposure [19,33,36]. Upon arrival, the patient should be asked to disinfect their hands with an alcohol-based sanitizer [36,45]. Patients with a temperature of >100.4 F or 38 °C requiring urgent dental care should have their appointments postponed if possible or performed in an airborne infection isolation room (AIIR) or negative-pressure room [31,39,41]. These are single-patient isolated rooms with a minimum of six air changes per hour [39,46]. Air from these rooms is exhausted outside, away from areas of human traffic or gatherings. It is filtered through a high-efficiency particulate air (HEPA) filter with a negative-pressure monitoring system held in place [39,46,47]. More recent recommendations provided by healthcare authorities emphasize that patients in the waiting area must wear a mask, gloves, and eye protection [36,41,44,48]. Ge et al. suggested displaying cough etiquette instructions at the entrance and in the waiting area to promote respiratory hygiene, which should also include reminders for physical distancing and wearing a mask all the time [39].
4.3. (c) Infection Control during Dental Treatment
Ensuring hand hygiene, providing preoperative antimicrobial mouth rinse to patients, utilizing rubber dams and high-volume saliva ejectors, minimizing aerosol-generating procedures and extraoral radiographs, a one visit treatment, and disinfection operations should be carried out throughout dental procedures. Before starting the dental procedure, a preprocedural mouth rinse for 60 s with an oxidizing agent such as 1% hydrogen peroxide or 0.2% povidone–iodine to reduce the viral load in aerosols has been suggested [11,37,41,42,49]. Several studies reported that chlorhexidine might not be effective against SARS-Cov-2 because there is a lack of evidence and systemic data, and the virus is primarily susceptible to oxidation [37,39,42,44]. The use of a rubber dam and high-volume evacuation/suction (HVE) during aerosol-generating restorative procedures has been suggested to reduce both airborne and surface contamination [11,18,31,37,41,42,50,51,52]. A rubber dam could potentially provide a 70% reduction in aerosols and eliminate all sources of aerosol contamination from blood or saliva by blocking the throat and soft tissue area, except the tooth/teeth undergoing treatment [50,51,52]. High-volume evacuator (HVE) or expensive high-efficiency particulate arrestor (HEPA) filters, if held within 6–15 mm of the aerosol-generating tip, can clean up to 90% and 99.99% of contaminated air, respectively [39]. Peng et al. also recommended a minimally invasive chemomechanical agent, CariSolv, for the removal of carious dentine, in addition to a hand scaler for periodontal procedures where a rubber dam is not feasible [19,37]. Although there is emerging evidence on the effectiveness of an antiretraction valve for eliminating the risk of cross-infection, its use has been suggested as an additional preventive measure to reduce cross-contamination and the dispersion of droplets or aerosols [11,37,53].
There has been much debate about the choice of a filtering face-piece (FFP), level 1 vs. level 2 vs. level 3, for aerosol- and non-aerosol-generating dental procedures. Some authors suggested wearing an FFP1/standard surgical mask for non-aerosol-generating procedures and FFP2/N95 or higher for aerosol-generating procedures [37,39]. Others suggested FFP2/N95 for all procedures for clinicians, dental surgery assistants, and front desk staff [41,42,43]. A systematic review of clinical trials assessing the effectiveness of N95 respirators in comparison to a standard surgical mask found no additional protection in preventing influenza [52]. Evidence from SARS-CoV research suggests that small infectious particles of up to 3 μm remain airborne indefinitely in an isolated room [54]. Patients and dental professionals can be exposed via inhalation of sustained small airborne infectious particles upon entering a room that was used to perform aerosol-generating procedures when wearing minimal airborne protection and using a standard surgical mask [18,37,43]. Therefore, considering the highly infectious nature of SARS-Cov-2 compared to influenza, we recommend the use of FFP2/N95 for both clinical and nonclinical staff for all dental procedures. Due to the risk of transmission from asymptomatic individuals and those in an incubation period, every patient should be considered potentially contagious [13,18].
Hand hygiene using a two-before-and-three-after technique recommended by the CDC and WHO has been extensively emphasized as a key factor in preventing cross-contamination [26,37,39,41,42]. In China, dental professionals were advised to disinfect their hands with soap or 70–90% alcohol before examination, before procedure, after touching the patient, patient-contaminated surroundings or instruments, and exposure to bodily fluids [37,39]. Reusable eye protection with safety glasses and a face shield were implemented in Italy and China [37,42]. Alharbi et al. recommended the use of extraoral radiographs such as orthopantomogram and cone-beam computer tomography over intraoral radiographs to prevent gagging and excessive salivation [31]. Overall, a layering approach, including head covers, long-sleeved water-resistant gowns, shoe covers, level 2 FFP, and eye protection for both clinical and nonclinical staff, has been suggested [37,39,41,42].
4.4. (d) Disinfection after Treatment
Disinfection of the treatment room and waiting area, including doorknobs, chairs, floor, desks, restrooms, and elevators between patients, has been suggested [39,41,42]. Hospital-grade disinfectants, including quaternary ammonium-based, phenol-based, and alcohol-based products such as 0.1% sodium hypochlorite or 70% isopropyl alcohol, have proven to be effective against coronaviruses [11,55,56]. The literature suggests the use of UVC light, a HEPA filter air purifier, or room ventilation for 30 min prior to surface disinfection after treatment may reduce the risk of infection [57,58]. However, we only found few articles from Italy and China where treatment/waiting area ventilation was implemented between patients [33,36,39,42].
Cleaning and disinfection of reusable facial protective devices and the handling of surgical waste after normal procedures should be considered after dental care. Waste management was another theme explored extensively in the literature. The treatment and disposal of medical waste pose indirect health risks due to environmental contamination; therefore, medical waste should be disposed of in accordance with the protocols provided by local health authorities. Peng et al. suggested that a temporary storage area should be assigned in the clinic for the storage of medical waste [37]. Reusable instruments should be adequately pretreated using an oxidizing disinfectant, cleaned, sterilized, and stored in accordance with the local health authorities’ protocol [11,37]. Additionally, double-layered packing, appropriate labeling, and gooseneck ligation have been suggested for medical waste generated from suspected/confirmed cases of COVID-19 [11,37]. Contaminated disposable PPE, including gloves, gowns, and head covers, should be safely disposed of in a bag within the clinical area before entering nonclinical areas.
4.5. Psychological Impact of COVID-19 among Dental Professionals
Four articles examined awareness, perception, attitudes, and behavior among dental professionals regarding the COVID-19 pandemic [26,27,28,29]. Dental healthcare professionals are at high risk for acquiring and transmitting the infection to their peers, families, and other patients due to the possibility of exposure to suspected/confirmed COVID-19 patients [18,28]. This is especially important as emotional instability due to fear and anxiety can foster irrational behavior and inadequate infection control practices [28]. Khader et al. conducted a cross-sectional study among 368 Jordanian dentists from different clinical settings to assess awareness, perception, and attitude regarding COVID-19 and infection control practices [29]. Jordanian dentists were found to have limited knowledge about the incubation period for the viral infection, physical distancing, masks for patients in the waiting area, hand hygiene practices, and protective clothing for clinical and nonclinical staff. Over 80% reported avoiding treatment for suspected/confirmed COVID-19 cases amid fear of contracting the disease [29]. Another study conducted by Ahmed et al. surveying 669 dentists from 30 different countries reported that almost 80% feared contracting COVID-19 and indicated avoiding treating suspected cases [28]. This is further backed by scientific evidence available from previous research showing an unwillingness of dental providers to treat patients with infectious diseases such as SARS, HIV, tuberculosis, and MERS [27,28]. The use of a rubber dam and preprocedural mouth rinse with an oxidizing agent were ignored by the majority of dental providers [28]. A high level of anxiety was reported among dental professionals related to practice closure and subsequent economic implications [28]. A study evaluating psychological stress experienced by Israeli dentists and dental hygienists during the COVID-19 pandemic identified that elevated psychological distress was significantly associated with having an existing chronic medical condition, a low self-efficacy score, and contracting COVID-19 from patients [27]. The study further highlights that psychological distress among dental professionals may have long-term effects and recommends mental health education or workshops to enhance self-efficacy [27].
Other studies assessing knowledge, awareness, and the psychological impact of COVID-19 among dental professionals from India [32], Italy [33,36], and Poland [34] have reported high perceived risk and a low level of awareness concerning infection management. A cross-sectional survey assessing hygiene practices among Indian dental professionals found that 33% were unaware of adequate use of PPE and only 60% were aware of guidelines recommended by the WHO [32]. One-third of the participants did not disinfect the lab work area, and almost 40% had a low knowledge score measured on a Likert scale [32]. Dental professionals with postgraduate education had a significantly high level of knowledge compared to graduates [32]. Another study from Italy assessing the psychological impact of COVID-19 among dental professionals using the General Anxiety Disorder-7 (GAD-7) test found an overall mild level of anxiety in 33% of the participants due to the pandemic [36]. The anxiety level was significantly positively correlated with concerns about the professional future, contracting the COVID-19 disease, and the risk of infection transmission among patients [36]. Using a self-reported questionnaire, the study also identified that 1% of dental practitioners contracted COVID-19 and 70% knew at least one person (friend/patient/colleague) who tested positive [36]. Continuing educational (CE) courses can benefit dental providers by providing them with infection control protocols in dental settings during the COVID-19 pandemic. However, a survey from Northern Italy found that only 30% of dental providers completed a CE course on COVID-19, where only 2% claimed to be confident in avoiding infection [36]. Other factors affecting dental professionals’ attitudes include adequate access to PPE, continuity of clinical practice, and type of practice (public compared to private) [34]. Another survey of Italian dental practitioners assessing the perceived risk of aerosol contamination during the COVID-19 pandemic found that the majority (70%) of dentists believed fine-aerosol-producing treatments to be of increased risk [19]. A more recent study related to disinfection knowledge, attitude, and practices among dental professionals during the COVID-19 pandemic globally found that almost 50% failed to correctly indicate surface disinfectant as an effective measure against COVID-19 [35]. The study also found inconsistent knowledge regarding the stability of SARS-CoV-2 on different surfaces, and the majority of dental providers believed chlorhexidine to be an effective preprocedural mouth rinse against SARS-CoV-2 [35].
The role of local authorities in providing procedural guidelines in the face of the pandemic is vital to help healthcare providers in making informed decisions. As identified in this review, adequate knowledge of the incubation period, routes of transmission, adequate use of PPE, and disinfection protocols are essential to curb the chain of transmission and safely treat suspected/confirmed COVID-19 patients [19,29,32,33,34,35,36].
4.6. Limitations
This review has few limitations pertaining to ongoing emergency due to the COVID-19 pandemic and substantial heterogeneity in the selection of sources addressing infection control management in the dental practice. Additionally, cross-sectional surveys addressing psychological distress among dental professionals are subjective/self-reported and may present reporting.
5. Conclusions
The COVID-19 pandemic presents a substantial risk for dental professionals and the community. Hence, only strict adherence to protocols can protect dental teams and patients from contracting COVID-19. The future trajectory of COVID-19, strength of individual healthcare systems, availability of rapid testing kits, vaccines, and successful therapeutic options for COVID-19 are factors that could possibly influence dental practice and additional precautionary measures that dental practitioners should adopt in the coming weeks and months. More research is required on aerosol’s specific risk assessment and measures that can protect the dental workforce and patients from aerosol and droplet infection. The economic and psychological aspect of the COVID-19 pandemic also needs special attention as the pandemic is taking a toll on the mental health of large segments of the population in these unprecedented and stressful times. It is important to fill in the gaps in knowledge regarding the complex nature of COVID-19′s impact on dental practice.
Author Contributions
Conception and research design, S.S.M., R.A., U.D., and Z.A.; designed search strategies and laid down inclusion/exclusion criteria for review of literature on the topic, S.S.M., F.A., U.D., Z.A., and A.P.; prepared figures and charts, A.P. and S.S.M.; drafted the manuscript, S.S.M., Z.A., and R.A.; approved final version of the manuscript, M.N.B., F.A., L.L.S., U.D., and S.S.M.; analyzed the results and wrote the discussion section, Z.A., S.S.M., and R.A.; edited and revised manuscript, L.L.S., U.D., M.N.B., S.S.M., Z.A., and F.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lake M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. 2020;20:124–127. doi: 10.7861/clinmed.2019-coron. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J., Tan K.-S., Wang D.-Y., Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020;7:1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) Coronavirus Disease (COVID-19) Dashboard. [(accessed on 22 August 2020)]; Available online: https://covid19.who.int/?gclid=Cj0KCQjwhIP6BRCMARIsALu9LfnBrJCWM-3csCkflq1Ni0GKcv-W0z7_mRrqt7ZKBvxWY2zG1NBx3GMaAsZ-EALw_wcB.
- 5.Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coronavirus Update (Live): 34,838,209 Cases and 1,033,356 Deaths from COVID-19 Virus Pandemic—Worldometer. [(accessed on 3 October 2020)]; Available online: https://www.worldometers.info/coronavirus/
- 7.Duda-Chodak A., Lukasiewicz M., Zięć G., Florkiewicz A., Filipiak-Florkiewicz A. Covid-19 pandemic and food: Present knowledge, risks, consumers fears and safety. Trends Food Sci. Technol. 2020;105:145–160. doi: 10.1016/j.tifs.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roy S. COVID-19 pandemic: Impact of lockdown, contact and non-contact transmissions on infection dynamics. medRxiv. 2020 doi: 10.1101/2020.04.04.20050328. [DOI] [Google Scholar]
- 9.Cai J., Sun W., Huang J., Gamber M., Wu J., He G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China. Emerg. Infect. Dis. 2020;26:1343–1345. doi: 10.3201/eid2606.200412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu C.-W., Liu X.-F., Jia Z.-F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fallahi H.R., Keyhan S.O., Zandian D., Kim S.-G., Cheshmi B. Being a front-line dentist during the Covid-19 pandemic: A literature review. Maxillofac. Plast. Reconstr. Surg. 2020;42:1–9. doi: 10.1186/s40902-020-00256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Guggemos W., et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N. Engl. J. Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kowalski L.P., Sanabria A., Ridge J.A., Ng W.T., De Bree R., Rinaldo A., Takes R., Mäkitie A.A., Carvalho A.L., Bradford C.R., et al. COVID -19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42:1259–1267. doi: 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicola M., O’Neill N., Sohrabi C., Khan M., Agha M., Agha R. Evidence based management guideline for the COVID-19 pandemic—Review article. Int. J. Surg. 2020;77:206–216. doi: 10.1016/j.ijsu.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evans K.L., Ewen J.G., Guillera-Arroita G., Johnson J.A., Penteriani V., Ryan S.J., Sollmann R., Gordon I.J. Conservation in the maelstrom of Covid-19—A call to action to solve the challenges, exploit opportunities and prepare for the next pandemic. Anim. Conserv. 2020;23:235–238. doi: 10.1111/acv.12601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li G., Chang B., Li H., Wang R., Li G. Precautions in dentistry against the outbreak of corona virus disease. J. Infect. Public Health. 2020 doi: 10.1016/j.jiph.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramos-Gomez F., Folayan M., Campus G. Global Impact of COVID-19 on Service Delivery and Vulnerable Populations’ Access to Dental Care. CAD J. 2020;48:507–516. [Google Scholar]
- 19.Patil S., Bhandi S., Gambarini G., Seracchiani M., Testarelli L., Miccoli G., Di Nardo D., Obino F.V., Galli M., Gambarini E. Fine Aerosols and Perceived Risk of COVID-19 among Italian Dental Practitioners: An Experimental Survey. J. Contemp. Dent. Pr. 2020;21:599–603. doi: 10.5005/jp-journals-10024-2850. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J., Wu W., Zhao X., Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precis. Clin. Med. 2020;3:3–8. doi: 10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gurzawska-Comis K., Becker K., Giulia B., Agata G., Schwarz F. Recommendations for dentists during COVID-19. Clin. Oral Implant. Res. 2020;31:158. doi: 10.1111/clr.100_13644. [DOI] [Google Scholar]
- 23.Simon L. How Will Dentistry Respond to the Coronavirus Disease 2019 (COVID-19) Pandemic? JAMA Health Forum. 2020;1:e200625. doi: 10.1001/jamahealthforum.2020.0625. [DOI] [PubMed] [Google Scholar]
- 24.Shamseer L., Moher D., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peterson J., Welch V., Losos M., Tugwell P.J. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa Hospital Research Institute; Ottawa, ON, Canada: 2011. [Google Scholar]
- 26.Kamate S.K., Sharma S., Thakar S., Srivastava D., Sengupta K., Hadi A.J., Chaudhary A., Joshi R., Dhanker K. Assessing Knowledge, Attitudes and Practices of dental practitioners regarding the COVID-19 pandemic: A multinational study. Dent. Med. Probl. 2020;57:11–17. doi: 10.17219/dmp/119743. [DOI] [PubMed] [Google Scholar]
- 27.Shacham M., Hamama-Raz Y., Kolerman R., Mijiritsky O., Ben-Ezra M., Mijiritsky E. COVID-19 Factors and Psychological Factors Associated with Elevated Psychological Distress among Dentists and Dental Hygienists in Israel. Int. J. Environ. Res. Public Health. 2020;17:2900. doi: 10.3390/ijerph17082900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmed M.A., Jouhar R., Ahmed N., Adnan S., Aftab M., Zafar M.S., Khurshid Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health. 2020;17:2821. doi: 10.3390/ijerph17082821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khader Y., Al Nsour M., Al-Batayneh O.B., Saadeh R., Bashier H., Alfaqih M., Al-Azzam S., Alshurman B.A. Dentists’ Awareness, Perception, and Attitude Regarding COVID-19 and Infection Control: Cross-Sectional Study Among Jordanian Dentists. JMIR Public Health Surveill. 2020;6:e18798. doi: 10.2196/18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang Y., Zhou Y., Liu X., Tan J. Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin. Oral Investig. 2020;24:1861–1864. doi: 10.1007/s00784-020-03267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alharbi A., Alharbi S., Alqaidi S. Guidelines for dental care provision during the COVID-19 pandemic. Saudi Dent. J. 2020;32:181–186. doi: 10.1016/j.sdentj.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gambhir R.S., Dhaliwal J.S., Aggarwal A., Anand S., Anand V., Bhangu A.K. Covid-19: A survey on knowledge, awareness and hygiene practices among dental health professionals in an Indian scenario. Rocz. Państw. Zakł. Hig. 2020;71:223–229. doi: 10.32394/rpzh.2020.0115. [DOI] [PubMed] [Google Scholar]
- 33.Cagetti M.G., Cairoli J.L., Senna A., Guglielmo Campus COVID-19 Outbreak in North Italy: An Overview on Dentistry A Questionnaire Survey. Int. J. Environ. Res. Public Health. 2020;17:3835. doi: 10.3390/ijerph17113835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tysiąc-Miśta M., Dziedzic A. The Attitudes and Professional Approaches of Dental Practitioners during the COVID-19 Outbreak in Poland: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health. 2020;17:4703. doi: 10.3390/ijerph17134703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sarfaraz S., Shabbir J., Mudasser M.A., Khurshid Z., Al-Quraini A.A.A., Abbasi M.S., Ratnayake J., Zafar M.S. Knowledge and Attitude of Dental Practitioners Related to Disinfection during the COVID-19 Pandemic. Healthcare. 2020;8:232. doi: 10.3390/healthcare8030232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Consolo U., Bellini P., Bencivenni D., Iani C., Checchi V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int. J. Environ. Res. Public Health. 2020;17:3459. doi: 10.3390/ijerph17103459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meng L., Hua F., Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ge Z.-Y., Yang L.-M., Xia J.-J., Fu X.-H., Zhang Y.-Z. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J. Zhejiang Univ. Sci. B. 2020;21:361–368. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J. Cranio Maxillofac. Surg. 2020;48:521–526. doi: 10.1016/j.jcms.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ather A., Patel B., Ruparel N.B., Diogenes A., Hargreaves K.M. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. J. Endodont. 2020;46 doi: 10.1016/j.joen.2020.03.008. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Izzetti R., Nisi M., Gabriele M., Graziani F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020;99:1030–1038. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 43.Xu R., Cui B., Duan X., Zhang P., Zhou X., Yuan Q. Saliva: Potential diagnostic value and transmission of 2019-nCoV. Int. J. Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Amato A., Caggiano M., Amato M., Moccia G., Capunzo M., De Caro F. Infection Control in Dental Practice During the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2020;17:4769. doi: 10.3390/ijerph17134769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Horzov L., Goncharuk-Khomyn M., Kostenko Y., Melnyk V. Dental Patient Management in the Context of the COVID-19 Pandemic: Current Literature Mini-Review. Open Public Health J. 2020;13:459–463. doi: 10.2174/1874944502013010459. [DOI] [Google Scholar]
- 46.Chandy P.E., Nasir M.U., Srinivasan S., Klass D., Nicolaou S., Babu S.B. Interventional radiology and COVID-19: Evidence-based measures to limit transmission. Diagn. Interv. Radiol. 2020;26:236–240. doi: 10.5152/dir.2020.20166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mousavi E., Kananizadeh N., Martinello R.A., Sherman J.D. COVID-19 Outbreak and Hospital Air Quality: A Systematic Review of Evidence on Air Filtration and Recirculation. Environ. Sci. Technol. 2020 doi: 10.1021/acs.est.0c03247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Diaz K.T., Smaldone G.C. Quantifying exposure risk: Surgical masks and respirators. Am. J. Infect. Control. 2010;38:501–508. doi: 10.1016/j.ajic.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 49.Fine D.H., Mendieta C., Barnett M.L., Furgang D., Meyers R., Olshan A., Vincent J. Efficacy of Preprocedural Rinsing with an Antiseptic in Reducing Viable Bacteria in Dental Aerosols. J. Periodontol. 1992;63:821–824. doi: 10.1902/jop.1992.63.10.821. [DOI] [PubMed] [Google Scholar]
- 50.Harrel S.K., Molinari J. Aerosols and splatter in dentistry. J. Am. Dent. Assoc. 2004;135:429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Samaranayake L.P., Reid J., Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J. Dent. Child. 1989;56:442–444. [PubMed] [Google Scholar]
- 52.Al-Amad S.H., Awad M.A., Edher F.M., Shahramian K., Omran T.A. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. J. Infect. Public Health. 2017;10:195–200. doi: 10.1016/j.jiph.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 53.Hu T., Li G., Zuo Y., Zhou X. Risk of Hepatitis B Virus Transmission via Dental Handpieces and Evaluation of an Antisuction Device for Prevention of Transmission. Infect. Control. Hosp. Epidemiol. 2007;28:80–82. doi: 10.1086/510808. [DOI] [PubMed] [Google Scholar]
- 54.Tellier R., Li Y., Cowling B.J., Tang J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019;19:1–9. doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wenzel R.P., Edmond M.B. Managing SARS amidst Uncertainty. N. Engl. J. Med. 2003;348:1947–1948. doi: 10.1056/NEJMp030072. [DOI] [PubMed] [Google Scholar]
- 56.Dexter F., Parra M.C., Brown J.R., Loftus R.W. Perioperative COVID-19 defense: An evidence-based approach for optimization of infection control and operating room management. Anesth. Analg. 2020 doi: 10.1213/ANE.0000000000004829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen C., Zhao B., Cui W., Dong L., An N., Ouyang X. The effectiveness of an air cleaner in controlling droplet/aerosol particle dispersion emitted from a patient’s mouth in the indoor environment of dental clinics. J. R. Soc. Interface. 2010;7:1105–1118. doi: 10.1098/rsif.2009.0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hallier C., Williams D.W., Potts A.J.C., Lewis M.A.O. A pilot study of bioaerosol reduction using an air cleaning system during dental procedures. Br. Dent. J. 2010;209:E14. doi: 10.1038/sj.bdj.2010.975. [DOI] [PMC free article] [PubMed] [Google Scholar]