Abstract
Hepatocellular carcinoma (HCC) is the most common primary liver cancer and one of the leading causes of cancer-related death worldwide. HCC is highly heterogeneous, both within the tumor and among individuals, which is closely related to the HCC surveillance, diagnosis, prognosis, and treatment response. With the advances of next-generation sequencing, the genomic landscape of HCC has been identified which vastly improves our understanding of genetic and epigenetic changes and their interaction during HCC development. In particular, gene mutations, epigenetic modifications, aberrant expression of coding and non-coding RNAs have been extensively explored and many of them are considered as biomarkers for HCC. Most recently, the gut microbiome has been proposed as potential non-invasive biomarkers for HCC diagnosis. In this review, we summarize the current development of HCC biomarkers studies and provide insights on further steps towards precision medicine of HCC.
Keywords: HCC, biomarker, diagnosis, prognosis
1. Introduction
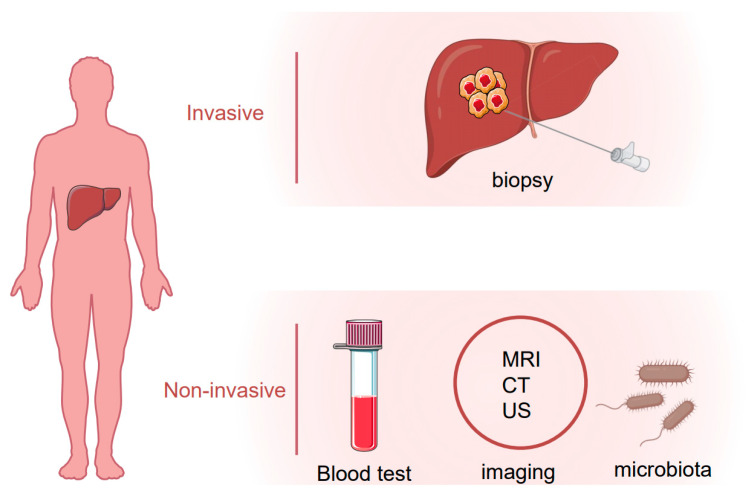
Hepatocellular carcinoma (HCC) is the most common primary liver tumor and the fourth-leading cause of cancer death worldwide [1]. Several risk factors are known to contribute to HCC development including the hepatitis B or C virus (HBV or HCV) infection, alcohol abuse, obesity and non-alcoholic fatty liver disease (NAFLD) [2]. For HCC patients at an early stage, surgical resection or percutaneous ablation is recommended as a first-line treatment option, and the recurrence rate five years after surgery is around 50% [3,4,5]. On the other hand, more than half of HCC patients were diagnosed with advanced or unresectable disease with a very poor prognosis due to extremely limited therapeutic options [6]. Early detection of HCC using imaging and tumor markers could dramatically improve patient outcomes. For patients with cirrhosis, surveillance of HCC is recommended which endorses significant benefits [7]. Several biomarkers in body fluid samples, e.g., plasma, serum, urine or stool, have been uncovered that could be objectively measured for HCC surveillance and diagnosis. Alpha-fetoprotein (AFP), AFP-L3 and des-γ-carboxy prothrombin (DCP) are the most well-studied and widely used non-invasive biomarkers in HCC. Apart from them, many other molecules such as Glypican 3 (GPC-3), Alpha-l fucosidase (AFU), Golgi protein-73 (GP73) and Squamous cell carcinoma antigen (SCCA), or tumor-associated signatures such as DNA mutation, DNA methylation, micro-RNAs (miRNAs) and long non-coding RNAs (lncRNAs) are under investigation that could be taken into consideration for future clinical practice. In this review, we summarize current HCC biomarker studies, highlighting novel biomarkers and imaging tests that may improve surveillance and diagnosis of HCC in the future (Figure 1).
Figure 1.
Invasive and noninvasive assessment of hepatocellular carcinoma (HCC).
2. Etiologic Factors of HCC
Etiologic agents, e.g., HBV, HCV, alcohol and NAFLD, could lead to chronic liver injury or liver cirrhosis and ultimately HCC, and thus are regarded as the risk factors for HCC. The risk factors of HCC vary in different geographic areas. In China, HBV is accountable for around 54% of HCC cases while 31% of liver cancer cases in Egypt are attributed to HCV infection [8]. As for western countries, NAFLD has emerged as an important cause of HCC in recent years [9]. The development of HCC in NAFLD patients may be associated with excessive body weight, hepatic iron-overload and insulin resistance which could contribute to advanced fibrosis and cirrhosis. Asides from these, gender and age are also thought to be risk factors of HCC. Intriguingly, the prevalence of HCC in males is two to four times more common than in females, a situation called gender disparity [10]. The reasons are complex and could be partially explained by the opposite effects of androgens and estrogen. Estradiol, an estrogen steroid hormone, has been reported to upregulate p53 expression thus suppress HCC [11]. On the other hand, testosterone, the predominant androgen, could promote the hepatocyte cell cycle via cyclin E [11]. In combination with other factors such as HBV and/or HCV infections, age is considered as another risk factor of HCC. A multi-center study across six South American countries involving 1336 patients revealed that nearly 40% of HCC patients with HBV infection at diagnosis were before age 50, while most cases with HCV infection were over the age of 60 [12]. Other environmental factors, such as dietary habits, alcohol consumption and exposure to aflatoxin, are also associated with HCC development.
3. Approaches to Identify Potential HCC Biomarkers
Biomarkers are defined as measurable indicators of physiological or pathological processes, or in response to various diagnostic or therapeutic procedures. The development of HCC is characterized by multiple genetic and epigenetic events alterations that run through cancer initiation, promotion and progression. During this process, liver cells are likely to present different molecular signatures, and release certain tumor-associated molecules into body fluid, e.g., blood, urine or stool, that could be monitored for the onset or progression of HCC. The development of detection technology has vastly advanced the development of HCC biomarkers. At present, many biotechnologies have been applied, such as chemiluminescence immunoassay, enzyme-linked immunosorbent assay, immunosensor, proteomics, liquid biopsy, and so on. The advent of Next-Generation Sequencing (NGS) has significantly increased our ability to look into the molecular pathogenesis and heterogeneity of HCC as well as a range of HCC biomarkers, including gene mutations, epigenetic modifications, aberrant expression of coding and non-coding RNAs, and gut microbiome [13,14,15,16,17,18]. An accurate landscape of HCC genetic and epigenetic alterations has been built up with high-throughput analyses of different cohorts which unravels potential biomarkers for monitoring the HCC imitation and progression [15,17]. Meanwhile, a recent study applied genome-wide 5-hydroxymethylcytosines detection using circulating cell-free DNA samples, providing a non-invasive tool in the early detection of HCC [19]. Another new technology, proteome, measuring global protein abundance and post-translational modifications, provides additional biological insights in HCC [14,20]. This method reveals a multi-omics profile of key signaling and metabolic pathways in HCC [20]. The proteomic profiles of tumor-derived extracellular vesicles and particles in human tissues and blood have been well characterized and can serve as reliable biomarkers [21]. Identification of novel non-invasive biomarkers with reliable analytical techniques will shed light on early diagnosis and management of HCC. In the following sections, we will discuss several HCC biomarkers.
4. Biomarkers for HCC
4.1. Protein Biomarkers
4.1.1. AFP and AFP-L3
Alpha-fetoprotein (AFP) is the most well-studied and commonly used biomarker for the diagnosis and prognosis of HCC [22,23]. AFP is primarily produced by the fetus’s liver and its expression declines rapidly to very a low level by the age of one. However, liver damage or liver cancer can dramatically increase AFP levels in the blood. In a nested case-control study, elevated AFP level could be observed 6 months before the diagnosis of HCC [24], implying that detection of AFP is useful for HCC diagnosis. Current criticisms on the use of AFP mainly focus on its insufficient sensitivity and specificity for early HCC detection if used alone. In addition, increased AFP levels can be found in the setting of cirrhosis patients with active hepatitis, elevated serum alanine aminotransferase (ALT), or non-HCC malignancies [25,26]. To date, AFP detection alone is not recommended for HCC screening. The European Association for the Study of the Liver recommends using liver ultrasound for the surveillance of HCC rather than AFP detection [27]. Nevertheless, the use of AFP is an effective auxiliary diagnostic tool for the detection and surveillance of HCC. In a meta-analysis study comparing the efficacy of ultrasound with or without AFP for early HCC detection (n = 2770), Kristina Tzartzeva et al. showed that the use of AFP in combination with abdominal ultrasound can significantly increases the sensitivity of early HCC detection as compared to ultrasound alone (63% vs. 45%) [28]. Moreover, AFP could be used for monitoring HCC progression considering that it promotes tumor proliferation and metastasis [29,30,31]. A meta-analysis consisting of 29 studies and 4726 HCC patients highlighted that AFP level was a potential noninvasive prognosis marker for HCC patients, and AFP Slope > 7.5 ng/mL per month was associated with HCC recurrence post-liver transplantation [32].
AFP-L3, an isoform of AFP, is specific to malignant tumors. The presence of AFP-L3 can serve to identify patients with a high risk of HCC who require increased monitoring. AFP-L3 has been approved by the US Food and Drug Administration (FDA) for assessing the risk of liver cancer. With a cutoff of 1.7%, the use of AFP-L3 demonstrates a better specificity but lower sensitivity for early HCC detection as compared to AFP [33]. Consistently, in a retrospective study recruiting 104 HCC patients with 104 matched non-HCC individuals, the elevation of AFP-L3 was present before the tumor became visible by imaging even though very low AFP levels could be detected, suggesting that AFP-L3 may serve as an early predictive HCC marker [34]. In the future, whether a combination of AFP-L3 and AFP could achieve better diagnostic efficacy for HCC warrants large population-based cohort studies.
4.1.2. DCP
Des-gamma-carboxy prothrombin (DCP), also known as the protein induced by vitamin K absence or antagonist II (PIVKA-II), is a nonfunctional prothrombin [35]. DCP was described as both an autologous growth factor that promotes HCC growth, and a paracrine factor that participates in the crosstalk between HCC and vascular endothelial cells. The biological malignant potential of DCP and its abnormal expression in HCC tissues pinpoints its potential for HCC prediction. In a study involving 1377 HCC patients and 355 patients with chronic hepatitis or cirrhosis, Shinichiro Nakamura et al. compared the diagnostic efficacy of DCP and AFP in discriminating HCC from chronic liver diseases [36]. The results demonstrated that DCP was superior to AFP in detecting large tumors (greater than 5 cm in diameter) [36]. In addition, DCP is a potential prognostic factor for patients with HCC after treatment. In a single-centre retrospective study comprising 412 patients with HBV-related HCC who were treated with radiofrequency ablation, DCP, but not AFP, was found to be an independent prognostic factor for both recurrence-free and overall survival in these patients [37]. The FDA has approved DCP for use in predicting liver cancer. Notably, DCP, AFP and AFP-L3 have been recommended for clinical practice according to Chinese and Japanese guideline [38,39]. However, a recent study carried out in Korea showed that a combination of DCP, AFP and AFP-L3 did not improve the performance for early HCC detection as compared to either AFP or AFP-L3 alone [24]. Further studies are required to evaluate the contribution of DCP for early HCC detection.
4.1.3. GPC-3
Glypican 3 (GPC-3) is a heparan sulfate proteoglycan that plays an important role in cell proliferation and differentiation, and is found to be highly associated with tumor development [40].
GPC-3 has emerged as a potential target for the diagnosis and treatment of HCC recently. GPC3 is rarely expressed in normal hepatocytes or pathological liver cells of hepatitis and cirrhosis. In contrast, GPC-3 is specifically overexpressed in HCC tissues [41]. Consistent results were reported that both GPC-3 mRNA and protein expressions were upregulated in HCC tissues [40,42]. However, the detection of GPC-3 in blood was not as effective as that in tissue biopsies for the diagnosis of HCC [43,44]. By examining serum GPC3 levels in HCC patients using enzyme-linked immunosorbent assay (ELISA), 36.1% to 95% of positive cases could be identified as reported by different studies [45]. Furthermore, serum GPC3 levels were comparable between patients without HCC and those with early HCC [45]. Additional investigations should be carried out to assess the potential of serum GPC3 as non-invasive diagnostic marker for HCC.
4.1.4. AFU
Alpha-l fucosidase (AFU) is a lysosomal enzyme and is reported to participate in the degradation of various fucose-containing fucoglycoconjugates. AFU has been proposed as a potential tumor marker in the diagnosis of HCC. At the cut-off value of 24 U/I, the area under the receiver operating characteristic curve (AUROC) for AFU was 0.83, with sensitivity and specificity of 56.1% and 69.2%, respectively [46]. The diagnostic efficiency of AFU was lower than AFP (cut-off value of 20 ng/mL for AFP) in this study [46]. In contrast, another study involving 1053 HCC patients showed that AFU exerted the same diagnostic power as AFP in both sensitivities (73.52% for AFU vs. 75.01% for AFP) and specificities (76.81% for AFU vs. 82.08% for AFP) [47]. It is worth noting that overexpression of AFP was also observed in other non-HCC diseases such as esophageal squamous cell carcinomas [48] and preeclampsia [49] which could markedly reduce the specificity of AFU for HCC diagnosis.
4.1.5. Other Protein Biomarkers
Proteins that are highly expressed in HCC compared with normal tissues could be promising candidates for HCC detection (Table 1). Golgi protein-73 (GP73, also called Golph2) is a transmembrane glycoprotein primarily expressed in epithelial cells. GP73 has been found upregulated in patients with diverse liver diseases, especially in HCC. In a large cohort study involving more than 4200 serum samples derived from healthy individuals and patients with benign or malignant liver disease, the sensitivity (74.6% for GP73 vs. 58.25% for AFP) and specificity (97.4% for GP73 vs. 85.3% for AFP) of GP73 for detection of HCC were higher than AFP [50]. A consistent result was observed in another study that GP73 had higher diagnostic performance than AFP [51]. Notably, a combination of these two markers could increase the sensitivity for HCC detection to 89.2%, with the specificity of 85.2% [50]. GP73 may also serve as an indicator for the recurrence of HCC given that serum GP73 levels diminished after surgical resection of HCC and rebound after tumor reappeared [50]. Furthermore, serum GP73 level was positively correlated with serum HBV DNA copies and the Child-Pugh score in cirrhotic patients [51]. GP73 is of importance for monitoring the patients with HBV infection who may eventually develop cirrhosis and HCC [51]. GP73 could be used for prediction of HCC in a cirrhotic population. However, in another study, the level of GP73 did not differ among patients with different types of liver disease [52]. Further large-scale and multi-centered studies are needed to evaluate the diagnostic accuracy and surveillance potential of GP73.
Table 1.
Biomarkers for HCC diagnosis.
| Biomarker | Samples | Type of Cohort | Sample Size | AUROC or Positive Rate (%) | Sensitivity (%) (95%CI) | Specificity (%) (95%CI) | Cutoff Value | Limitation | Refs |
|---|---|---|---|---|---|---|---|---|---|
| AFP | serum | prospective | 689 | 0.77 | 62 (48–76) | 87 (82–92) | 5 ng/mL | Modest accuracy | [24] |
| AFP-L3 | serum | prospective | 689 | 0.73 | 55 (40–69) | 90 (85–94) | 4.0% | Modest accuracy | [24] |
| GPC-3 | tissue | Variation among tests | |||||||
| mRNA | retrospective | 52–105 | 55.7–100 | NA | NA | NA | [45] | ||
| protein | 107–757 | 63.6–91 | NA | NA | NA | [51] | |||
| GPC-3 | serum | retrospective | 60–625 | 31.6–95 | NA | NA | [40,45] | ||
| DCP | serum | retrospective | 689 | 0.71 | 48 (33–64) | 86 (80–91) | NA | Modest accuracy | [24] |
| AFU | serum | retrospective | 512 | 0.68 | 56.1 (NA) | 69.2 (NA) | 24 U/I | Low accuracy | [46] |
| GP73 | serum | retrospective | 60–4217 | 0.73–0.94 | 72.4–74.6 | 61.5–97.4 | different cutoff | Modest accuracy | [50,51,52] |
| SCCA | serum | meta-analysis | 12 studies | 0.53–0.9 | 12–84 | 48–100 | different cutoff | Low accuracy | [53,54] |
| SCCA-IgM | serum | meta-analysis | 12 studies | 0.66–0.86 | 51–89 | 48–78 | different cutoff | Low accuracy | [53,54,55] |
NA: not available.
Squamous cell carcinoma antigen (SCCA) is composed of two highly homologous proteins SCCA1 and SCCA2 and belongs to the serine protease inhibitor family. SCCA is reported to participate in multiple biological processes such as cell proliferation, resistance to apoptosis, and epithelial-mesenchymal transition. Overexpression of SSCA was identified in HCC tissues at an early stage, indicating that it could be a potential candidate for HCC diagnosis [56]. Following studies were carried out to evaluate the diagnostic value of SCCA [53,55], showing that SCCA complexed with IgM (SCCA-IgM) was useful for assessment of HCC in cirrhotic patients with high sensitivity but poor specificity. A meta-analysis involving 11 studies concluded that both SCCA and SCCA-IgM presented diagnostic value for HCC, with AUROC of 0.8 and 0.77, respectively [57]. Moreover, SCCA can be used to predict the prognosis of HCC patients, thus is recommended to be included in clinical practice in some studies [53].
Others candidates include Apelin [58], β2 microglobulin [59], dickkopf-1 [60], GATA Zinc Finger Domain Containing 1 [61], osteopontin [62] and squalene epoxidase [63] that are reported to have abnormal expressions in HCC as compared to normal control. Although these markers are reported as sensitive biomarkers for HCC prediction, they have not yet been applied in clinical or recommended for use by major professional hepatology societies, probably because of limited sample size, lack of external validation, or sample accessibility, implying the complexity and challenges of biomarker development. Large prospective studies are needed to further validate their performance in HCC diagnosis and prognosis.
4.2. DNA Mutation and Methylation Related Biomarkers
The genomic landscape of HCC has been identified with the advances of next-generation sequencing. Over the past decades, a range of single-nucleotide polymorphisms (SNP) has been identified that is correlated with the presence of HCC [64,65]. Take the EGF gene as an example. The EGF gene polymorphism genotype significantly correlated with EGF levels and conferred high risk of HCC development in patients with liver cirrhosis [65]. EGF genotype G/G was found to be associated with increased risk of HCC, which may account for the difference in HCC incidence between black and white populations [64]. Besides SNP, telomerase reverse-trancriptase (TERT) promoter mutations appeared as an early event of HCC based on the exome sequencing analysis of 243 liver tumors [66]. TERT promoter mutations could induce TERT transcription or telomerase activation, and promote tumor initiation and progression. In HCC, TERT is the most frequent genetic alteration [67]. However, the occurrence of high GC contents in the TERT promoter region hinders the development of clinically relevant assays for the detection of TERT promoter mutations in patients’ biopsies. In the future, it will be of importance to explore the potential of plasmatic cell-free and tumor DNA (cfDNA and ctDNA) detection of TERT promoter mutations for diagnosing early HCC.
Epigenetic alterations such as DNA hypermethylation or hypomethylation are also thought to be early events in hepatocarcinogenesis, thus detection of DNA methylation biomarkers are suitable for detection of HCC. In a large cohort study comprising 1098 patients with HCC and 835 healthy controls, an effective blood-based diagnostic prediction model combining 10-methylation markers (cg10428836, cg26668608, cg25754195, cg05205842, cg11606215, cg24067911, cg18196829, cg2321194, cg17213048 and cg25459300) was established, showing potential for HCC diagnosis with high sensitivity and specificity [68]. Furthermore, the utility of this model demonstrated superior sensitivity and specificity than AFP for HCC diagnosis [68]. Another study comprised of patients harboring different cancer diseases reported that detection of six HCC-specific hypermethylated sites (cg23565942, cg21908638, cg11223367, cg03509671, cg05569109, and cg11481534) could distinguish HCC from other tumor types at very high sensitivity and specificity (92% and 98%, respectively) [69]. Taken together, circulating tumor DNA methylation markers are thought to be reliable for use in the screening, diagnosis, and prognosis of HCC.
4.3. miRNA and lncRNAs Related Biomarkers
Noncoding RNAs (ncRNAs) refer to transcripts without protein-coding regions, including microRNAs (miRNAs) and long noncoding RNAs (lncRNAs) (Table 2). miRNAs have been implicated in various biological processes during HCC pathogenesis. Accumulating evidence demonstrated that miRNA can serve as biomarkers for diagnosis, prognosis as well as prediction of therapeutic response of HCC. Detection of miR-221 and miR-101-1 could be used as non-invasive testing for the early diagnosis of HCC among patients with HCV infection [70]. Moreover, miR-939, miR-595 and miR-519 could be used to distinguish HCC from non-HCC among cirrhotic patients, and a combination of these microRNAs was reported to achieve higher AUROC than AFP [71]. Upon combining the AFP, a miRNA panel (miR-122, miR-885-5p, miR-221, and miR-22) was reported capable of distinguishing early HCC from liver cirrhosis, chronic hepatitis C, and healthy subjects, and therefore was recommended for clinical use in early detection of HCC by this study [72]. Moreover, a combination of miR-16, AFP, AFP-L3, and DCP hold great promise in predicting HCC with sensitivity and specificity of 92.4% and 78.5%, respectively [73].
Table 2.
Some biomarkers published in the past five years for HCC diagnosis.
| Biomarkers | Testing Method | Type of Cohort | Sample Size | AUROC | Finding | Ref |
|---|---|---|---|---|---|---|
| CTNNB1, TERT, CDKN2A, SMARCA2 and HGF | tissue | retrospective | 243 | NA | recurrently mutated in alcohol-related HCCs | [66] |
| TP53 | tissue | retrospective | 243 | NA | frequent mutation in HBV-related HCCs | [66] |
| TERT | tissue | retrospective | 243 | NA | frequent mutation at early stages of HCCs | [66] |
| Six HCC-specific methylation biomarkers | tissue | TCGA dataset | 4389 | NA | 92% sensitivity and 98% specificity in predicting HCCs | [69] |
| miR-221 | blood | retrospective | 115 | 0.673 | 56.8% sensitivity and 73.9% specificity for early prediction of HBV-related HCCs | [70] |
| miR-101-1 | blood | retrospective | 115 | 0.763 | 73% sensitivity and 71% specificity in predicting HCCs | [70] |
| PVT1 | blood and tissue | prospective | 272 | NA | upregulated in HCCs | [78] |
| SEPT9 | blood | prospective | 334 | initial study: 0.944; replication study: 0.930 | mSEPT9 test is promising for HCC diagnosis in patients with cirrhosis | [81] |
| miR-3126-5p | blood | retrospective | 155 | 0.881 | downregulated in HCCs | [82] |
| miR-92a-3p | blood | retrospective | 155 | 0.705 | upregulated in HCCs | [82] |
| miR-107 | blood | retrospective | 155 | 0.730 | upregulated in HCCs | [82] |
| FGF19 | blood | retrospective | 304 | 0.795 | cutoff value of 200.0 pg/mL | [83] |
NA: Not available.
Recently, lncRNAs have also been found to play important roles during HCC development and progression. Several HCC-related lncRNAs have been identified that are dysregulated in HCC tissues, including HULC [74], MALAT1 [75], HOTAIR [76], MVIH [77], and PVT1 [78]. MALAT1 was reported to present a high sensitivity for human HCC prediction, implying that the MALAT1 test could be a potential diagnostic technique [75]. On the other hand, circulating HULC and Linc00152 levels determined by real-time quantitative PCR (qRT-PCR) were found to be higher in the plasma of HCC patients as compared to control in both discovery and validation cohort, with AUROC of 0.78 and 0.85, respectively [79]. Combining HULC and Linc00152 could discriminate HCC from control with AUROC of 0.87 [79]. Thus, serum HULC and Linc00152 may act as novel biomarkers for HCC. Moreover, in combination with AFP and PIVKAII, plasma MALAT1 test could more accurately diagnose HCC as compared to individual parameters, with sensitivity and specificity of 88.6% and 75%, respectively [80]. Nevertheless, larger prospective studies are needed to evaluate the performance of the abovementioned ncRNAs for use in clinical practice.
4.4. Gut Microbiome Biomarkers
Gut microbial alteration is likely to contribute to the progression of liver disease and the development of liver cancer through the microbiota-liver axis, implying that detection of HCC-related bacterial could be used as potential non-invasive tools for the prediction of liver cancer (Table 3). In a large clinical cohort study comprising 419 fecal samples from China, 16S rRNA Miseq sequencing was performed and the data analysis using a random forest model identified 30 microbial markers as potential biomarkers for early HCC with AUROC of 0.806 (95% CI, 0.745 to 0.868) and 0.768 (95% CI, 0.679 to 0.857) in discovery and validation cohort, respectively [84]. Compared with the controls, lipopolysaccharide (LPS)—producing bacterial, Klebsiella and Haemophilus, were enriched in patients with HCC; in contrast, Ruminococcus, Oscillibacter, Faecalibacterium, Clostridium IV and Coprococcus were depleted in HCC patients [84]. In another study comparing the gut microbiome between patients with HCC and those with NAFLD-related cirrhosis, the HCC group presented higher enrichment of Bacteroides and Ruminococcaceae but lower abundance of Bifidobacterium compared to the cirrhosis group [5]. Bacteroides and Ruminococcaceae have been reported to associate with immune modulation by inducing proinflammatory cytokines IL18 and IL13 and recruiting activated monocytes and mMDSCs; while deficiency of Bifidobacterium may enhance intestinal and liver inflammation, and subsequently damage the intestinal barrier [85,86]. Apart from gut microbiota, the oral microbiome may also be used as diagnostic biomarkers for HCC [87]. In the future, studies of large-scale are required to further evaluate the role of the gut microbiome as predictors of HCC risk.
Table 3.
Microbiome biomarkers for the diagnosis of HCC.
| Biomarkers | Samples | Sample Size | Method | Finding | Diagnosis Potential | Ref |
|---|---|---|---|---|---|---|
| Gut microbiome | faecal | 190 (discovery) 131 (validation) | 16S rRNA sequencing | Butyrate-producing bacterial genera ↓ lipopolysaccharide-producing bacterial ↑ | optimal 30 microbial markers achieved AUROC of 80.64% among 75 early HCC and 105 non-HCC samples | [84] |
| faecal | 61 | 16S rRNA sequencing | Bifidobacterium↓ Bacteroides and Ruminococcaceae↑ | correlated with systemic inflammation | [5] | |
| faecal | 223 | 16s rRNA sequencing |
Bacteroides↑ Lachnospiracea incertae sedis↑ Clostridium XIVa ↑ |
correlated with HBV-related HCC | [18] | |
| Oral microbiome | tongue coat | 60 | 16S rRNA sequencing | Gammaproteobacteria ↓ Bacteroidetes↓ Fusobacteria↑ Epsilonproteobacteria↑ Actinobacteria↑ | Oribacterium and Fusobacterium could distinguish HCC patients from healthy subjects | [87] |
↑: upregulated in HCC. ↓: downregulated in HCC.
4.5. Imaging Biomarkers
Unlike other solid cancers, the diagnosis of HCC has relied on the assessment of noninvasive imaging without a regular biopsy confirmation. Meanwhile, chronic liver disease history and biomarkers detections sometimes are taken into consideration for HCC diagnosis. When the noninvasive criteria are not satisfied, needle biopsy may be performed for further confirmation. A systematic review of 47 studies comprising a total of 15,158 patients concluded that patients could benefit from HCC surveillance which has been proved to increase both the detection rate of early-stage tumor and curative treatment rates [88]. Imaging analysis, including computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography (US) or digital subtraction angiography (DSA), plays a critical role in the diagnosis and management of HCC. Currently, patients with cirrhosis or at high-risk of HCC are recommended to take the test of AFP and US every 6 months. US examination is a simple, real-time, non-invasive and sensitive method that can identify the location, size and shape of the liver, thus favors the diagnosis of HCC [89]. In addition, the contrast-enhanced ultrasound (CEUS) has proved itself as a valuable diagnostic tool for HCC prediction with the AUROC of 0.9432 [54]. Due to the limited sample size and potential selection bias in this meta-analysis, further validation is needed to verify the potential of CEUS for HCC diagnosis. MRI is another useful imaging-based biomarker that allows the mapping of the entire liver. In a prospective surveillance study recruiting a total of 407 patients with cirrhosis, the detection rate of HCC by MRI was significantly higher than in the US (86% vs. 27.9%) [90]. About 74.4% of patients with very early stage HCC (a single lesion < 2 cm) were diagnosed and got the chance to receive curable treatment [90]. Taken together, abdominal US is the most commonly method for monitoring patients at high risk of HCC because of its widely availability and low cost. Multiphase CT or multiphases MRI are recommended by the American Association for the Study of Liver Diseases for the diagnosis of HCC.
4.6. Biomarker Panels
Because of the limited accuracy for individual marker detection, their combinations have been thoroughly investigated to provide a more precise risk prediction of HCC (Table 4). The GALAD model is a commonly used panel consisting of gender, age, AFP-L3, AFP and DCP [91]. The AUROC of the GALAD in training and validation cohorts that were comprised of 6834 patients was between 0.85 and 0.95. More recently, Shen and colleagues established an online calculator based on serum biomarkers including age, sex, AFP and PIVKA-II, to detect HCC in patients with chronic hepatitis. Their program performed quite well which could accurately predict the presence of HCC in chronic hepatitis patients [92]. Another study developed a logistic regression algorithm, named as Doylestown algorithm, which combined AFP, sex, age, alkaline phosphatase (ALK) and alanine aminotransferase (ALT) and was capable to increase the AUROC of AFP detection for HCC diagnosis [93,94]. In addition, this algorithm could identify high-risk patients 9 months prior to the diagnosis of HCC. Nevertheless, there is a lack of independent validations, and HCC patients of different etiologic agents or ethnic groups should be taken into consideration in future studies.
Table 4.
Biomarker panels for the diagnosis of HCC.
| Biomarkers | Samples | Type of Cohort | Sample Size | AUROC | Finding | Ref |
|---|---|---|---|---|---|---|
| 10 DNA methylation markers | blood | retrospective | 1933 | 0.944 in training set 0.966 in validation set |
high sensitivity and specificity | [68] |
| miR-122+miR885-5p+miR-29b+AFP | blood | retrospective | 192 | 1 | early detection of HCC | [72] |
| miR-122+miR-885-5p+miR-221+miR-22+AFP | blood | retrospective | 96 | 0.982 | predict HCC in liver cirrhosis patients | [72] |
| miR+miR-199a-3p+AFP | blood | retrospective | 96 | 0.988 | predict HCC in hepatitis C patients | [72] |
| miR-3126-5p+miR-92a-3p+miR-107+AFP | blood | retrospective | 155 | 0.994 | useful for diagnosis of HCC | [82] |
| gender, age, AFP-L3, AFP and DCP | blood | retrospective | 6834 | ranging from 0.85 to 0.95 in five international cohorts | useful for diagnosis of HCC | [91] |
| age, sex, AFP and PIVKA-II | blood | retrospective | 2925 | 0.941 in training set 0.931 in validation set | predict HCC in hepatitis B patients | [92] |
5. Conclusions and Perspectives
Detection of tumor-associated molecular signatures is feasible for monitoring the development and progression of HCC. To date, there are several candidate biomarkers identified for early diagnosis and prognosis prediction of HCC. However, most of them cannot be used in a clinical setting at present, because of the reliability and validity of measurement. The challenges to biomarkers studies remain including incomplete cohort data, selection bias during sample collection and limited sample size for discovery and validation studies. Therefore, larger prospective cohorts with appropriate controls are required for proper validation of identified biomarkers which can be further translated into clinical applications. Moreover, detection technologies and patients’ characteristics should be taken into consideration for clinical biomarker research.
With the advancement of genomics and proteomics, more new biomarkers will be available for early diagnosis and surveillance of HCC. However, HCC is known as a complex disease caused by a variety of risk factors. Thus, it is difficult to use a single biomarker for HCC patients. The development and optimization of biomarkers combination will be more valuable for the early diagnosis and prognosis prediction of HCC. Moreover, demographic characteristics and genetic risks should be considered for the precision screening of HCC. With improved detection technologies and optimization of biomarkers combination, the promise of early detection and treatment of HCC should be realized in the near future.
Author Contributions
Conceptualization, H.C. and J.Y.; data curation, Y.P. and H.C.; writing—original draft preparation, Y.P. and H.C.; writing—review and editing, H.C. and J.Y.; funding acquisition, J.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by RGC-CRF Hong Kong (C4041-17GF; C7026-18G; C7065-18G); RGC Theme-based Res Scheme Hong Kong (T12-703/19-R), and Guangdong Natural Science Foundation (2018B030312009).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. Nov. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Villanueva A. Hepatocellular Carcinoma. N. Engl. J. Med. 2019;380:1450–1462. doi: 10.1056/NEJMra1713263. [DOI] [PubMed] [Google Scholar]
- 3.Liu P.H., Hsu C.Y., Hsia C.Y., Lee Y.H., Huang Y.H., Chiou Y.Y., Lin H.C., Huo T.I. Surgical Resection Versus Radiofrequency Ablation for Single Hepatocellular Carcinoma </= 2 cm in a Propensity Score Model. Ann. Surg. 2016;263:538–545. doi: 10.1097/SLA.0000000000001178. [DOI] [PubMed] [Google Scholar]
- 4.Kao W.Y., Chao Y., Chang C.C., Li C.P., Su C.W., Huo T.I., Huang Y.H., Chang Y.J., Lin H.C., Wu J.C. Prognosis of Early-Stage Hepatocellular Carcinoma: The Clinical Implications of Substages of Barcelona Clinic Liver Cancer System Based on a Cohort of 1265 Patients. Medicine. 2015;94:e1929. doi: 10.1097/MD.0000000000001929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ponziani F.R., Bhoori S., Castelli C., Putignani L., Rivoltini L., Del Chierico F., Sanguinetti M., Morelli D., Sterbini F.P., Petito V., et al. Hepatocellular Carcinoma Is Associated with Gut Microbiota Profile and Inflammation in Nonalcoholic Fatty Liver Disease. Hepatology. 2019;69:107–120. doi: 10.1002/hep.30036. [DOI] [PubMed] [Google Scholar]
- 6.Colagrande S., Inghilesi A.L., Aburas S., Taliani G.G., Nardi C., Marra F. Challenges of advanced hepatocellular carcinoma. World J. Gastroenterol. 2016;22:7645–7659. doi: 10.3748/wjg.v22.i34.7645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J.D., Mannalithara A., Piscitello A.J., Kisiel J.B., Gores G.J., Roberts L.R., Kim W.R. Impact of surveillance for hepatocellular carcinoma on survival in patients with compensated cirrhosis. Hepatology. 2018;68:78–88. doi: 10.1002/hep.29594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Llovet J.M., Zucman-Rossi J., Pikarsky E., Sangro B., Schwartz M., Sherman M., Gores G. Hepatocellular carcinoma. Nat. Rev. Dis. Primers. 2016;2:16018. doi: 10.1038/nrdp.2016.18. [DOI] [PubMed] [Google Scholar]
- 9.Seydel G.S., Kucukoglu O., Altinbasv A., Demir O.O., Yilmaz S., Akkız H., Otan E., Sowa J.-P., Canbay A. Economic growth leads to increase of obesity and associated hepatocellular carcinoma in developing countries. Ann. Hepatol. 2016;15:662–672. doi: 10.5604/16652681.1212316. [DOI] [PubMed] [Google Scholar]
- 10.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 11.Pok S., Wong H.J., Board P., Barn V.A., Blackburn A.C., Farrell G.C., Teoh N.C. Testosterone regulation of cyclin E kinase: A key factor in determining gender differences in hepatocarcinogenesis. J. Gastroenterol. Hepatol. 2016;31:1210–1219. doi: 10.1111/jgh.13232. [DOI] [PubMed] [Google Scholar]
- 12.Chan A.J., Balderramo D., Kikuchi L., Ballerga E.G., Prieto J.E., Tapias M., Idrovo V., Davalos M.B., Cairo F., Barreyro F.J., et al. Early Age Hepatocellular Carcinoma Associated with Hepatitis B Infection in South America. Clin. Gastroenterol. Hepatol. 2017;15:1631–1632. doi: 10.1016/j.cgh.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 13.Wu Z.-H., Yang D.-L. Identification of a protein signature for predicting overall survival of hepatocellular carcinoma: A study based on data mining. BMC Cancer. 2020;20:1–9. doi: 10.1186/s12885-020-07229-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang Y., Sun A., Zhao Y., Ying W., Sun H., Yang X., Xing B., Sun W., Ren L., Hu B., et al. Proteomics identifies new therapeutic targets of early-stage hepatocellular carcinoma. Nat. Cell Biol. 2019;567:257–261. doi: 10.1038/s41586-019-0987-8. [DOI] [PubMed] [Google Scholar]
- 15.Schulze K., Nault J.-C., Villanueva A. Genetic profiling of hepatocellular carcinoma using next-generation sequencing. J. Hepatol. 2016;65:1031–1042. doi: 10.1016/j.jhep.2016.05.035. [DOI] [PubMed] [Google Scholar]
- 16.Duan J., Wu Y., Liu J., Zhang J., Fu Z., Feng T., Liu M., Han J., Li Z., Chen S. Genetic Biomarkers for Hepatocellular Carcinoma in the Era of Precision Medicine. J. Hepatocell. Carcinoma. 2019;6:151–166. doi: 10.2147/JHC.S224849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zucman-Rossi J., Villanueva A., Nault J.-C., Llovet J.M. Genetic Landscape and Biomarkers of Hepatocellular Carcinoma. Gastroenterology. 2015;149:1226–1239.e4. doi: 10.1053/j.gastro.2015.05.061. [DOI] [PubMed] [Google Scholar]
- 18.Huang H., Ren Z., Gao X., Hu X., Zhou Y., Jiang J., Lu H., Yin S., Ji J., Zhou L., et al. Integrated analysis of microbiome and host transcriptome reveals correlations between gut microbiota and clinical outcomes in HBV-related hepatocellular carcinoma. Genome Med. 2020;12:1–14. doi: 10.1186/s13073-020-00796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cai J., Chen L., Zhang Z., Zhang X., Lu X., Liu W., Shi G., Ge Y., Gao P., Yang Y., et al. Genome-wide mapping of 5-hydroxymethylcytosines in circulating cell-free DNA as a non-invasive approach for early detection of hepatocellular carcinoma. Gut. 2019;68:2195–2205. doi: 10.1136/gutjnl-2019-318882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gao Q., Zhu H., Dong L., Shi W., Chen R., Song Z., Huang C., Li J., Dong X., Zhou Y., et al. Integrated Proteogenomic Characterization of HBV-Related Hepatocellular Carcinoma. Cell. 2019;179:561–577.e22. doi: 10.1016/j.cell.2019.08.052. [DOI] [PubMed] [Google Scholar]
- 21.Hoshino A., Kim H.S., Bojmar L., Gyan K.E., Cioffi M., Hernandez J., Zambirinis C.P., Rodrigues G., Molina H., Heissel S., et al. Extracellular Vesicle and Particle Biomarkers Define Multiple Human Cancers. Cell. 2020;182:1044–1061.e18. doi: 10.1016/j.cell.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Omata M., Cheng A.-L., Kokudo N., Kudo M., Lee J.M., Jia J., Tateishi R., Han K.-H., Chawla Y.K., Shiina S., et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: A 2017 update. Hepatol. Int. 2017;11:317–370. doi: 10.1007/s12072-017-9799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marrero J.A., Kulik L.M., Sirlin C.B., Zhu A.X., Finn R.S., Abecassis M., Roberts L.R., Heimbach J.K. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723–750. doi: 10.1002/hep.29913. [DOI] [PubMed] [Google Scholar]
- 24.Choi J., Kim G., Han S., Lee W., Chun S., Lim Y. Longitudinal Assessment of Three Serum Biomarkers to Detect Very Early-Stage Hepatocellular Carcinoma. Hepatology. 2019;69:1983–1994. doi: 10.1002/hep.30233. [DOI] [PubMed] [Google Scholar]
- 25.Yang J.D., Dai J., Singal A.G., Gopal P., Addissie B.D., Nguyen M.H., Befeler A.S., Reddy K.R., Schwartz M., Harnois D.M., et al. Improved Performance of Serum Alpha-Fetoprotein for Hepatocellular Carcinoma Diagnosis in HCV Cirrhosis with Normal Alanine Transaminase. Cancer Epidemiol. Biomark. Prev. 2017;26:1085–1092. doi: 10.1158/1055-9965.EPI-16-0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Di Bisceglie A.M., Sterling R.K., Chung R.T., Everhart J.E., Dienstag J.L., Bonkovsky H.L., Wright E.C., Everson G.T., Lindsay K.L., Lok A.S., et al. Serum alpha-fetoprotein levels in patients with advanced hepatitis C: Results from the HALT-C Trial. J. Hepatol. 2005;43:434–441. doi: 10.1016/j.jhep.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 27.European Association for the Study of the Liver EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 28.Tzartzeva K., Obi J., Rich N.E., Parikh N.D., Marrero J.A., Yopp A., Waljee A.K., Singal A.G. Surveillance Imaging and Alpha Fetoprotein for Early Detection of Hepatocellular Carcinoma in Patients with Cirrhosis: A Meta-analysis. Gastroenterology. 2018;154:1706–1718.e1. doi: 10.1053/j.gastro.2018.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li M.-S., Li P.-F., He S.-P., Du G.-G., Li G. The promoting molecular mechanism of alpha-fetoprotein on the growth of human hepatoma Bel7402 cell line. World J. Gastroenterol. 2002;8:469–475. doi: 10.3748/wjg.v8.i3.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li M., Li P.-F., Chen Q., Du G.-G., Li G. Alpha-fetoprotein stimulated the expression of some oncogenes in human hepatocellular carcinoma Bel 7402 cells. World J. Gastroenterol. 2004;10:819–824. doi: 10.3748/wjg.v10.i6.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu Y., Zhu M., Li W., Lin B., Dong X., Chen Y., Xie X., Guo J., Li M. Alpha fetoprotein plays a critical role in promoting metastasis of hepatocellular carcinoma cells. J. Cell. Mol. Med. 2016;20:549–558. doi: 10.1111/jcmm.12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giard J.-M., Mehta N., Dodge J.L., Roberts J.P., Yao F.Y. α-Fetoprotein Slope >7.5 ng/mL per Month Predicts Microvascular Invasion and Tumor Recurrence after Liver Transplantation for Hepatocellular Carcinoma. Transplantation. 2018;102:816–822. doi: 10.1097/TP.0000000000002094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marrero J.A., Feng Z., Wang Y., Nguyen M.H., Befeler A.S., Roberts L.R., Reddy K.R., Harnois D., Llovet J.M., Normolle D., et al. α-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137:110–118. doi: 10.1053/j.gastro.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumada T., Toyoda H., Tada T., Kiriyama S., Tanikawa M., Hisanaga Y., Kanamori A., Tanaka J., Kagebayashi C., Satomura S. High-sensitivity Lens culinaris agglutinin-reactive alpha-fetoprotein assay predicts early detection of hepatocellular carcinoma. J. Gastroenterol. 2014;49:555–563. doi: 10.1007/s00535-013-0883-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim T.S., Rhee H., Kim G.M., Kim S.U., Kim B.K., Park J.Y., Ahn S.H., Han K.-H., Choi J.-Y., Kim D.Y. Alpha-Fetoprotein, Des-Gamma-Carboxy Prothrombin, and Modified RECIST Response as Predictors of Survival after Transarterial Radioembolization for Hepatocellular Carcinoma. J. Vasc. Interv. Radiol. 2019;30:1194–1200.e1. doi: 10.1016/j.jvir.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 36.Nakamura S., Nouso K., Sakaguchi K., Ito Y.M., Ohashi Y., Kobayashi Y., Toshikuni N., Tanaka H., Miyake Y., Matsumoto E., et al. Sensitivity and Specificity of Des-Gamma-Carboxy Prothrombin for Diagnosis of Patients with Hepatocellular Carcinomas Varies According to Tumor Size. Am. J. Gastroenterol. 2006;101:2038–2043. doi: 10.1111/j.1572-0241.2006.00681.x. [DOI] [PubMed] [Google Scholar]
- 37.Lee S., Rhim H., Kim Y.-S., Kang T., Song K.D. Post-ablation des-gamma-carboxy prothrombin level predicts prognosis in hepatitis B-related hepatocellular carcinoma. Liver Int. 2015;36:580–587. doi: 10.1111/liv.12991. [DOI] [PubMed] [Google Scholar]
- 38.Kokudo N., Hasegawa K., Akahane M., Igaki H., Izumi N., Ichida T., Uemoto S., Kaneko S., Kawasaki S., Ku Y., et al. Evidence-based Clinical Practice Guidelines for Hepatocellular Carcinoma: The Japan Society of Hepatology 2013 update (3rd JSH-HCC Guidelines) Hepatol. Res. 2015;45 doi: 10.1111/hepr.12464. [DOI] [PubMed] [Google Scholar]
- 39.Xie D.-Y., Ren Z.-G., Zhou J., Fan J., Gao Q. Critical appraisal of Chinese 2017 guideline on the management of hepatocellular carcinoma. HepatoBiliary Surg. Nutr. 2017;6:387–396. doi: 10.21037/hbsn.2017.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Capurro M., Wanless I.R., Sherman M., DeBoer G., Shi W., Miyoshi E., Filmus J. Glypican-3: A novel serum and histochemical marker for hepatocellular carcinoma. Gastroenterology. 2003;125:89–97. doi: 10.1016/S0016-5085(03)00689-9. [DOI] [PubMed] [Google Scholar]
- 41.Hsu H.C., Cheng W., Lai P.L. Cloning and expression of a developmentally regulated transcript MXR7 in hepatocellular carcinoma: Biological significance and temporospatial distribution. Cancer Res. 1997;57:5179–5184. [PubMed] [Google Scholar]
- 42.Zhu Z.-W., Friess H., Wang L., Abou-Shady M., Zimmermann A., Lander A.D., Korc M., Kleeff J., Büchler M.W. Enhanced glypican-3 expression differentiates the majority of hepatocellular carcinomas from benign hepatic disorders. Gut. 2001;48:558–564. doi: 10.1136/gut.48.4.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nault J.-C., Guyot E., Laguillier C., Chevret S., Ganne-Carrie N., N’Kontchou G., Beaugrand M., Seror O., Trinchet J.-C., Coelho J., et al. Serum Proteoglycans as Prognostic Biomarkers of Hepatocellular Carcinoma in Patients with Alcoholic Cirrhosis. Cancer Epidemiol. Biomark. Prev. 2013;22:1343–1352. doi: 10.1158/1055-9965.EPI-13-0179. [DOI] [PubMed] [Google Scholar]
- 44.Shafizadeh N., Ferrell L.D., Kakar S. Utility and limitations of glypican-3 expression for the diagnosis of hepatocellular carcinoma at both ends of the differentiation spectrum. Mod. Pathol. 2008;21:1011–1018. doi: 10.1038/modpathol.2008.85. [DOI] [PubMed] [Google Scholar]
- 45.Zhou F., Shang W., Yu X., Tian J. Glypican-3: A promising biomarker for hepatocellular carcinoma diagnosis and treatment. Med. Res. Rev. 2018;38:741–767. doi: 10.1002/med.21455. [DOI] [PubMed] [Google Scholar]
- 46.Xing H., Qiu H., Ding X., Han J., Li Z., Wu H., Yan C., Li H., Han R., Zhang H., et al. Clinical performance of α-L-fucosidase for early detection of hepatocellular carcinoma. Biomark. Med. 2019;13:545–555. doi: 10.2217/bmm-2018-0414. [DOI] [PubMed] [Google Scholar]
- 47.Xi L., Yang C. Evaluation of alpha-l-fucosidase for the diagnosis of hepatocellular carcinoma based on meta-analysis. J. Lab. Med. 2020;44:183–189. doi: 10.1515/labmed-2019-0152. [DOI] [Google Scholar]
- 48.Yu X., Zhang R., Yang T., Zhang M., Xi K., Lin Y., Wen Y., Wang G., Huang Z., Zhang X., et al. Alpha-l-fucosidase: A novel serum biomarker to predict prognosis in early stage esophageal squamous cell carcinoma. J. Thorac. Dis. 2019;11:3980–3990. doi: 10.21037/jtd.2019.08.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang M., Wang L., Zhang H., Cong J., Zhang L. Serum α-l-fucosidase activities are significantly increased in patients with preeclampsia. Prog. Mol. Biol. Transl. Sci. 2019;162:349–362. doi: 10.1016/bs.pmbts.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 50.Mao Y., Yang H., Xu H., Lu X., Sang X., Du S., Zhao H., Chen W., Xu Y., Chi T., et al. Golgi protein 73 (GOLPH2) is a valuable serum marker for hepatocellular carcinoma. Gut. 2010;59:1687–1693. doi: 10.1136/gut.2010.214916. [DOI] [PubMed] [Google Scholar]
- 51.Ali O.M., El Amin H.A., Sharkawy Y.L., Ali A.A.M., Kholef E.F.M., Elsewify W.A.E. Golgi Protein 73 versus Alpha-Fetoprotein as a New Biomarker in Early Diagnosis of Hepatocellular Carcinoma. Int. J. Gen. Med. 2020;13:193–200. doi: 10.2147/IJGM.S253622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gu Y., Chen W., Zhao Y., Chen L., Peng T. Quantitative analysis of elevated serum Golgi protein-73 expression in patients with liver diseases. Pt 1Ann. Clin. Biochem. Int. J. Lab. Med. 2009;46:38–43. doi: 10.1258/acb.2008.008088. [DOI] [PubMed] [Google Scholar]
- 53.Pozzan C., Cardin R., Piciocchi M., Cazzagon N., Maddalo G., Vanin V., Giacomin A., Pontisso P., Cillo U., Farinati F. Diagnostic and prognostic role of SCCA-IgM serum levels in hepatocellular carcinoma (HCC) J. Gastroenterol. Hepatol. 2014;29:1637–1644. doi: 10.1111/jgh.12576. [DOI] [PubMed] [Google Scholar]
- 54.Zhang J., Yu Y., Li Y., Wei L. Diagnostic value of contrast-enhanced ultrasound in hepatocellular carcinoma: A meta-analysis with evidence from 1998 to 2016. Oncotarget. 2017;8:75418–75426. doi: 10.18632/oncotarget.20049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beneduce L., Castaldi F., Marino M., Quarta S., Ruvoletto M., Benvegnù L., Calabrese F., Gatta A., Pontisso P., Fassina G. Squamous cell carcinoma antigen-immunoglobulin M complexes as novel biomarkers for hepatocellular carcinoma. Cancer. 2005;103:2558–2565. doi: 10.1002/cncr.21106. [DOI] [PubMed] [Google Scholar]
- 56.Pontisso P., Calabrese F., Benvegnù L., Lise M., Belluco C., Ruvoletto M.G., De Falco S., Marino M., Valente M., Nitti D., et al. Overexpression of squamous cell carcinoma antigen variants in hepatocellular carcinoma. Br. J. Cancer. 2004;90:833–837. doi: 10.1038/sj.bjc.6601543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu J., Wang Z.-J., Chen L.-H., Dong W.-Z. Diagnostic value of serum squamous cell carcinoma antigen for hepatocellular carcinoma: A systematic review and meta-analysis. Scand. J. Clin. Lab. Investig. 2016;77:8–14. doi: 10.1080/00365513.2016.1238504. [DOI] [PubMed] [Google Scholar]
- 58.Chen H., Wong C.-C., Liu D., Go M.Y., Wu B., Peng S., Kuang M., Wong N., Yu J. APLN promotes hepatocellular carcinoma through activating PI3K/Akt pathway and is a druggable target. Theranostics. 2019;9:5246–5260. doi: 10.7150/thno.34713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Okoror L.E., Ajayi A.O., Ijalana O.B. Elevated serum beta2-microglobulin in individuals coinfected with hepatitis B and hepatitis D virus in a rural settings in Southwest Nigeria. BMC Res. Notes. 2017;10:719. doi: 10.1186/s13104-017-3015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang R., Lin H.M., Broering R., Yu X.H., Xu L.B., Wu W.R., Liu C. Dickkopf-1 contributes to hepatocellular carcinoma tumorigenesis by activating the Wnt/beta-catenin signaling pathway. Signal Transduct. Target. Ther. 2019;4:1–10. doi: 10.1038/s41392-019-0082-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 61.Sun W., Zhang Y., Wong K.C., Liu K., Yang Y., Wu B., Tong J.H., Chan A.W.H., Chan H.L.-Y., Yu J. Increased expression of GATA zinc finger domain containing 1 through gene amplification promotes liver cancer by directly inducing phosphatase of regenerating liver 3. Hepatology. 2018;67:2302–2319. doi: 10.1002/hep.29750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Da Costa A.N., Plymoth A., Santos-Silva D., Ortiz-Cuaran S., Camey S., Guilloreau P., Sangrajrang S., Khuhaprema T., Mendy M., Lesi O.A., et al. Osteopontin and latent-TGF beta binding-protein 2 as potential diagnostic markers for HBV-related hepatocellular carcinoma. Int. J. Cancer. 2015;136:172–181. doi: 10.1002/ijc.28953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu D., Wong C.C., Fu L., Chen H., Zhao L., Li C., Zhou Y., Zhang Y., Xu W., Yang Y., et al. Squalene epoxidase drives NAFLD-induced hepatocellular carcinoma and is a pharmaceutical target. Sci. Transl. Med. 2018;10:eaap9840. doi: 10.1126/scitranslmed.aap9840. [DOI] [PubMed] [Google Scholar]
- 64.Abu Dayyeh B.K., Yang M., Fuchs B.C., Karl D.L., Yamada S., Sninsky J.J., O’Brien T.R., Dienstag J.L., Tanabe K.K., Chung R.T. A Functional Polymorphism in the Epidermal Growth Factor Gene Is Associated with Risk for Hepatocellular Carcinoma. Gastroenterology. 2011;141:141–149. doi: 10.1053/j.gastro.2011.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tanabe K.K., Lemoine A., Finkelstein D.M., Kawasaki H., Fujii T., Chung R.T., Lauwers G.Y., Kulu Y., Muzikansky A., Kuruppu D., et al. Epidermal Growth Factor Gene Functional Polymorphism and the Risk of Hepatocellular Carcinoma in Patients with Cirrhosis. JAMA. 2008;299:53–60. doi: 10.1001/jama.2007.65. [DOI] [PubMed] [Google Scholar]
- 66.Schulze K., Imbeaud S., Letouzé E., Alexandrov L.B., Calderaro J., Rebouissou S., Couchy G., Meiller C., Shinde J., Soysouvanh F., et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 2015;47:505–511. doi: 10.1038/ng.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nault J.C., Mallet M., Pilati C., Calderaro J., Bioulac-Sage P., Laurent C., Laurent A., Cherqui D., Balabaud C., Zucman-Rossi J. High frequency of telomerase reverse-transcriptase promoter somatic mutations in hepatocellular carcinoma and preneoplastic lesions. Nat. Commun. 2013;4:2218. doi: 10.1038/ncomms3218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xu R.-H., Wei W., Krawczyk M., Wang W., Luo H., Flagg K., Yi S., Shi W., Quan Q., Li K., et al. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat. Mater. 2017;16:1155–1161. doi: 10.1038/nmat4997. [DOI] [PubMed] [Google Scholar]
- 69.Cheng J., Wei D., Ji Y., Chen L., Yang L., Li G., Wu L., Hou T., Xie L., Ding G., et al. Integrative analysis of DNA methylation and gene expression reveals hepatocellular carcinoma-specific diagnostic biomarkers. Genome Med. 2018;10:1–11. doi: 10.1186/s13073-018-0548-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shaker O., Alhelf M., Morcos G., Elsharkawy A. miRNA-101-1 and miRNA-221 expressions and their polymorphisms as biomarkers for early diagnosis of hepatocellular carcinoma. Infect. Genet. Evol. 2017;51:173–181. doi: 10.1016/j.meegid.2017.03.030. [DOI] [PubMed] [Google Scholar]
- 71.Fornari F., Ferracin M., Trerè D., Milazzo M., Marinelli S., Galassi M., Venerandi L., Pollutri D., Patrizi C., Borghi A., et al. Circulating microRNAs, miR-939, miR-595, miR-519d and miR-494, Identify Cirrhotic Patients with HCC. PLoS ONE. 2015;10:e0141448. doi: 10.1371/journal.pone.0141448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zekri A.-R.N., Youssef A.S.E.-D., El-Desouky E.D., Ahmed O.S., Lotfy M.M., Nassar A.A.-M., Bahnassey A.A. Serum microRNA panels as potential biomarkers for early detection of hepatocellular carcinoma on top of HCV infection. Tumor Biol. 2016;37:12273–12286. doi: 10.1007/s13277-016-5097-8. [DOI] [PubMed] [Google Scholar]
- 73.Qu K., Zhang K., Li H., Afdhal N.H., Albitar M. Circulating MicroRNAs as Biomarkers for Hepatocellular Carcinoma. J. Clin. Gastroenterol. 2011;45:355–360. doi: 10.1097/MCG.0b013e3181f18ac2. [DOI] [PubMed] [Google Scholar]
- 74.Panzitt K., Tschernatsch M.M., Guelly C., Moustafa T., Stradner M., Strohmaier H.M., Buck C.R., Denk H., Schroeder R., Trauner M., et al. Characterization of HULC, a Novel Gene with Striking Up-Regulation in Hepatocellular Carcinoma, as Noncoding RNA. Gastroenterology. 2007;132:330–342. doi: 10.1053/j.gastro.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 75.Lin R., Maeda S., Liu C., Karin M., Edgington T.S. A large noncoding RNA is a marker for murine hepatocellular carcinomas and a spectrum of human carcinomas. Oncogene. 2006;26:851–858. doi: 10.1038/sj.onc.1209846. [DOI] [PubMed] [Google Scholar]
- 76.Yang Z., Zhou L., Wu L.-M., Lai M.-C., Xie H.-Y., Zhang F., Zheng S. Overexpression of Long Non-coding RNA HOTAIR Predicts Tumor Recurrence in Hepatocellular Carcinoma Patients Following Liver Transplantation. Ann. Surg. Oncol. 2011;18:1243–1250. doi: 10.1245/s10434-011-1581-y. [DOI] [PubMed] [Google Scholar]
- 77.Yuan S.-X., Yang F., Yang Y., Tao Q.-F., Zhang J., Huang G., Wang R.-Y., Yang S., Huo X.-S., Zhang L., et al. Long noncoding RNA associated with microvascular invasion in hepatocellular carcinoma promotes angiogenesis and serves as a predictor for hepatocellular carcinoma patients’ poor recurrence-free survival after hepatectomy. Hepatology. 2012;56:2231–2241. doi: 10.1002/hep.25895. [DOI] [PubMed] [Google Scholar]
- 78.Ding C., Haiyang X., Lv Z., Du C., Xiao H., Peng C., Cheng S., Xie H., Zhou L., Wu J., et al. Long non-coding RNA PVT1 is associated with tumor progression and predicts recurrence in hepatocellular carcinoma patients. Oncol. Lett. 2015;9:955–963. doi: 10.3892/ol.2014.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li J., Wang X., Tang J., Jiang R., Zhang W., Ji J., Sun B. HULC and Linc00152 Act as Novel Biomarkers in Predicting Diagnosis of Hepatocellular Carcinoma. Cell. Physiol. Biochem. 2015;37:687–696. doi: 10.1159/000430387. [DOI] [PubMed] [Google Scholar]
- 80.Konishi H., Ichikawa D., Yamamoto Y., Arita T., Shoda K., Hiramoto H., Hamada J., Itoh H., Fujita Y., Komatsu S., et al. Plasma level of metastasis-associated lung adenocarcinoma transcript 1 is associated with liver damage and predicts development of hepatocellular carcinoma. Cancer Sci. 2016;107:149–154. doi: 10.1111/cas.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Oussalah A., Rischer S., Bensenane M., Conroy G., Filhine-Tresarrieu P., Debard R., Forest-Tramoy D., Josse T., Reinicke D., Garcia M., et al. Plasma mSEPT9: A Novel Circulating Cell-free DNA-Based Epigenetic Biomarker to Diagnose Hepatocellular Carcinoma. EBioMedicine. 2018;30:138–147. doi: 10.1016/j.ebiom.2018.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang Y., Li T., Qiu Y., Zhang T., Guo P., Ma X., Wei Q., Han L. Serum microRNA panel for early diagnosis of the onset of hepatocellular carcinoma. Medicine. 2017;96:e5642. doi: 10.1097/MD.0000000000005642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Maeda T., Kanzaki H., Chiba T., Ao J., Kanayama K., Maruta S., Kusakabe Y., Saito T., Kobayashi K., Kiyono S., et al. Serum fibroblast growth factor 19 serves as a potential novel biomarker for hepatocellular carcinoma. BMC Cancer. 2019;19:1088. doi: 10.1186/s12885-019-6322-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ren Z., Li A., Jiang J., Zhou L., Yu Z., Lu H., Xie H., Chen X., Shao L., Zhang R., et al. Gut microbiome analysis as a tool towards targeted non-invasive biomarkers for early hepatocellular carcinoma. Gut. 2019;68:1014–1023. doi: 10.1136/gutjnl-2017-315084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fang D., Shi D., Lv L., Gu S., Wu W., Chen Y., Guo J., Li A., Hu X., Guo F., et al. Bifidobacterium pseudocatenulatum LI09 and Bifidobacterium catenulatum LI10 attenuate D-galactosamine-induced liver injury by modifying the gut microbiota. Sci. Rep. 2017;7:1–13. doi: 10.1038/s41598-017-09395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sivan A., Corrales L., Hubert N., Williams J.B., Aquino-Michaels K., Earley Z.M., Benyamin F.W., Lei Y.M., Jabri B., Alegre M.L., et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 2015;350:1084–1089. doi: 10.1126/science.aac4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lu H., Ren Z., Li A., Zhang H., Jiang J., Xu S., Luo Q., Zhou K., Sun X., Zheng S., et al. Deep sequencing reveals microbiota dysbiosis of tongue coat in patients with liver carcinoma. Sci. Rep. 2016;6:33142. doi: 10.1038/srep33142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Singal A.G., Pillai A., Tiro J. Early Detection, Curative Treatment, and Survival Rates for Hepatocellular Carcinoma Surveillance in Patients with Cirrhosis: A Meta-analysis. PLoS Med. 2014;11:e1001624. doi: 10.1371/journal.pmed.1001624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pocha C., Dieperink E., McMaken K.A., Knott A., Thuras P., Ho S.B. Surveillance for hepatocellular cancer with ultrasonography vs. computed tomography—A randomised study. Aliment. Pharmacol. Ther. 2013;38:303–312. doi: 10.1111/apt.12370. [DOI] [PubMed] [Google Scholar]
- 90.Kim S.Y., Sang L.Y., Lim Y.-S., Han S., Lee J.-Y., Byun J.H., Won H.J., Lee S.J., Lee H.C., Lee Y.S. MRI with Liver-Specific Contrast for Surveillance of Patients with Cirrhosis at High Risk of Hepatocellular Carcinoma. JAMA Oncol. 2017;3:456–463. doi: 10.1001/jamaoncol.2016.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Berhane S., Toyoda H., Tada T., Kumada T., Kagebayashi C., Satomura S., Schweitzer N., Vogel A., Manns M.P., Benckert J., et al. Role of the GALAD and BALAD-2 Serologic Models in Diagnosis of Hepatocellular Carcinoma and Prediction of Survival in Patients. Clin. Gastroenterol. Hepatol. 2016;14:875–886.e6. doi: 10.1016/j.cgh.2015.12.042. [DOI] [PubMed] [Google Scholar]
- 92.Yang T., Xing H., Wang G., Wang N., Liu M., Yan C., Li H., Wei L., Li S., Fan Z., et al. A Novel Online Calculator Based on Serum Biomarkers to Detect Hepatocellular Carcinoma among Patients with Hepatitis B. Clin. Chem. 2019;65:1543–1553. doi: 10.1373/clinchem.2019.308965. [DOI] [PubMed] [Google Scholar]
- 93.Wang M., Devarajan K., Singal A.G., Marrero J.A., Dai J., Feng Z., Rinaudo J.A.S., Srivastava S., Evans A., Hann H.-W., et al. The Doylestown Algorithm: A Test to Improve the Performance of AFP in the Detection of Hepatocellular Carcinoma. Cancer Prev. Res. 2015;9:172–179. doi: 10.1158/1940-6207.CAPR-15-0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mehta A.S., Lau D.T., Wang M., Islam A., Nasir B., Javaid A., Poongkunran M., Block T.M. Application of the Doylestown algorithm for the early detection of hepatocellular carcinoma. PLoS ONE. 2018;13:e0203149. doi: 10.1371/journal.pone.0203149. [DOI] [PMC free article] [PubMed] [Google Scholar]