Abstract
Background
Needlestick and sharp injuries are a big risk to the health of nurses. Every day, nurses face the likelihood that they will injure themselves. Although many injuries will have no adverse effect, the possibility of acquiring infections like hepatitis C virus, hepatitis B virus, and human immunodeficiency virus can cause untold psychological harm. Nurses are in danger of injuries caused by needlestick and sharp instruments in hospitals.
Objective
The objective of this study was to assess the magnitude and determinants of needlestick and/or sharp injuries among nurses working at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia, 2018.
Methods
An institution-based cross-sectional study was conducted among 268 nurses working at Tikur Anbessa Specialized Hospital from February to March 2018. A stratified random sampling technique was used to select the study participants. Data were collected using a self-administered questionnaire. A bivariate and multivariate logistic regression model was fitted to spot factors associated with needlestick and/or sharp injury. An adjusted odds ratio with a 95% confidence interval was computed to determine the level of significance.
Result
The prevalence of needlestick and/or sharp injuries among nurses was 36.2% (95% CI 30.2%, 42.3%). Presence of contaminated needles and/or sharp materials in the working area (AOR = 2.052 (95% CI 1.110, 3.791)), needle recapping after use (AOR = 1.780 (95% CI 1.025, 3.091)), working in the pediatric ward (AOR = 0.323 (95% CI 0.112, 0.930)), and being female (AOR = 0.461 (95% CI 0.252, 0.845)) were significantly associated with needlestick and/or sharp injury at p value of ≤0.05. Conclusion and Recommendation. The proportion of needlestick and/or sharp injury was high among nurses. The safety of nurses depends directly on the degree to which nurses can identify and control the numerous occupational hazards specific to jobs. Thus, working unit specific safety precautions, a safe working environment, and appropriate needle and sharp disposal improve nurses' safety practices and thereby decrease the injuries.
1. Introduction
Needlestick and sharp injuries are wounds that are caused by sharps that accidentally puncture the skin. Sharps include hypodermic needles, blood collection needles, and IV (intravenous) cannulas or needles as well as items such as scalpels, razor blades, lancets, retractors, scissors, pins, clamps, cutters, staples, and glass items [1]. These preventable injuries expose health care workers to over 20 different bloodborne pathogens, which resulted in 1000 infections per year [2]. It is estimated that through occupational exposure, 2.6% of health care workers are exposed to hepatitis C virus (HCV), 5.9% to hepatitis B virus (HBV), and 0.5% to HIV annually. This equates to approximately 16,000 HCV infections, 66,000 HBV infections, and 200-600 HIV (human immunodeficiency virus) infections worldwide [3]. According to the World Health Organization (WHO), needlestick and sharp injuries cause about 40% of hepatitis C and B infections and 2.5% of HIV infections among health care providers worldwide [4]. The World Health Organization has also estimated that in developing regions, 40%–65% of HBV and HCV infections in HCWs are attributable to percutaneous occupational exposure [5]. Health care workers (HCWs) in Africa suffer two to four needlestick injuries per year on average [6], with Nigeria, Tanzania, and South Africa reporting 2.1% injuries per year on average [7]. The Centers for Disease Control and Prevention (CDC) estimates that about 236,000 to 384,000 hospital workers sustain needlestick and sharp injuries, and nurses share 40% of it [8]. In the United States of America (USA), it was estimated that the reported incidence of NSI among nurses is currently 16.3% [9]. 48% of nurses in Ireland [10], 39% of registered nurses in the USA [11], 39.4% of nurses in Iran [12] reported an incident in their careers by a needle or sharp injury in the last 12 months.
Globally, it is estimated that 3 million health care workers worldwide experience NSI every year; of those, up to 50% of all NSI are being sustained by nurses [13]. Previous works of literature conducted in South Korea (70.4%) [14], Pakistan (67%) [15], Thailand (55.5%) [16], India (33.3%) [17], Nepal (74%) [18], Iran (41%, 54%) [19, The World Health Organization (WHO) reports that the number of needlestick injuries per person among health care staff is 4 per year in Africa, Western Mediterranean, and Asia [23]. Developing countries, especially those in sub-Saharan Africa, account for the highest prevalence of HIV-infected patients, and more than 90% of occupational exposure occurs in these countries [24–27]. The burden of the problem is not only on individual health but also on human resources and economic and social destruction [28]. Bloodborne pathogens are generally considered endemic in sub-Saharan Africa [29]. For instance, 62% of nurses in Nigeria [30], 18.8% in South Africa [31], 74.57% in Egypt [1], and 40.2% in Nigeria had sustained a needlestick injury in 12 months [30].
Moreover, health care workers practicing in developing countries such as Ethiopia are more exposed to human immunodeficiency virus (HIV) and hepatitis B virus (HBV) following occupational exposure and are less likely to use postexposure prophylaxis (PEP) than those working in developed countries [32, 33]. Even though there is no national data regarding the magnitude of NSSI among HCWs, particularly among nurses, the prevalence of sharp injuries among HCPs was 32.8% [34]. In studies conducted in Southwest Ethiopia (58.8%) [35]; Jimma University Hospital, Ethiopia (39.3%) [36]; and Bahir Dar, Ethiopia (66.6%) [37], nurses sustained sharp and or needlestick injuries in the past 12 months. Needlestick and sharp injuries represent a serious hazard within the health care industry, with professional nurses incurring an outsized proportion of the entire burden particularly with items that have been previously used on patients [38–40].
These injuries occur in different types of procedures such as needle recapping, operative procedures, blood collection, intravenous line administration, suturing, checking blood sugar, and poor sharp disposal [41]. The causes include various factors: type and elegance of needles, recapping activity, handling/transferring specimens, collision between HCWs and sharps, during cleanups, manipulating needles in patient line-related work, passing/handling devices, or failure to dispose of the needle in puncture-proof containers [42]. Therefore, needlestick and sharp injuries are a serious concern to all health care personnel and pose a significant risk of transmission of occupational bloodborne pathogens [43]. There is a paucity of information in Ethiopia particularly in Tikur Anbessa Specialized Hospital describing the magnitude and determinants of needlestick and sharp injuries. In Ethiopia, where primary health care services are covered by nurses, the risk of contracting infections following needlestick and sharp injuries is high in their day-to-day activities. Since the researchers have seen different kinds of literature, there is no single study on nurses other than overall health professionals in the study area, and the devastating effect of NSSI in the economic and psychological terms and health of nurses and their families needs more attention in the daily life of health care professionals. The reason why Tikur Anbessa Specialized Hospital was selected was that this hospital is the largest referral hospital in the country. It is also an establishment where specialized clinical services that are not available in other public or private institutions are rendered to the entire nation. Hence, the objective of this study is to determine the magnitude and determinants of needlestick and/or sharp injuries among nurses at Tikur Anbessa Specialized Hospital.
1.1. Conceptual Framework
The factors associated with needlestick and sharp injuries are classified as sociodemographic factors like sex, age, service year or experiences, and marital status; work-related environmental factors like injection practice, disposal of used sharps, department, and favorability of workplace; and behavioral factors like education and training. The three factors are interrelated to affect one another. Figure 1 shows the interrelation between the sharp and needlestick injury (independent) variables in detail [32, 33, 44].
Figure 1.
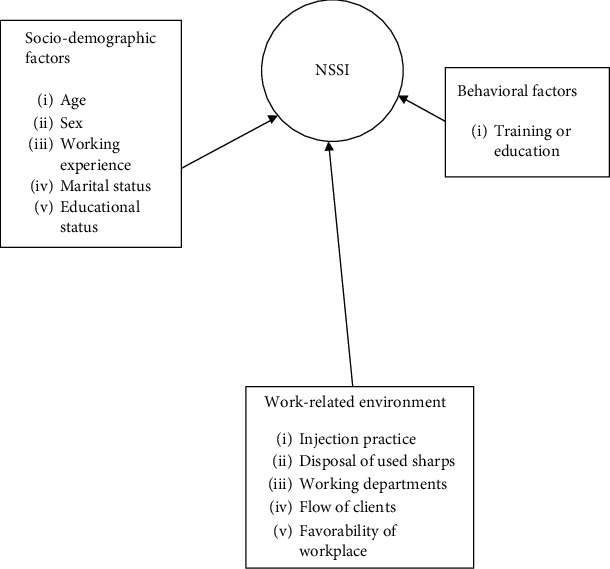
Conceptual framework literature review, TASH, Addis Ababa, Ethiopia, June 2018.
2. Methods
2.1. Study Setting
The study was conducted in Tikur Anbessa Specialized Hospital which is found in Addis Ababa (the capital city of Ethiopia) in the Lideta subcity. According to the Central Statistical Agency (CSA) of Ethiopia, as of 2013, the town of Addis Ababa has a total population of 3,130,673, of which 1,478,890 are men and 1,624,783 are women. It is the nation's largest and highest referral hospital. This hospital sees approximately 370,000–400,000 patients a year, but the exact number is not known. It has 700 beds. This is the largest teaching hospital in Ethiopia. There are a total of 789 nurses with different qualifications. The hospital is planned and accommodated and facilitated with the outpatient department (OPD), which has seven X-ray, nine surgical, and two diagnostic laboratory rooms. The hospital provides medical services in internal medicine, gynecologic and obstetric, surgical, pediatric, and emergency departments. The hospital also has special units (referral clinics), which include chest, renal, neurology, cardiology, dermatology, orthopedic, general surgical, gynecologic and obstetric, diabetic, hematology, and medical intensive care units and units for sexually transmitted diseases, gastrointestinal diseases, and infectious diseases.
2.2. Study Design and Populations
An institution-based cross-sectional study was conducted to assess the prevalence and associated factors of needlestick and/or sharp injuries (NSSI) from February 19 to March 31, 2018. The source population for this study was all nurses who were working in Tikur Anbessa Specialized Hospital. The sample populations of the study were all selected nurses working in Tikur Anbessa Specialized Hospital at the time of data collection. Nurses either males or females who were working in the same department or unit for at least one year and all those registered nurses who were working in Tikur Anbessa Specialized Hospital of Addis Ababa during the study period involved in clinical work were included in the study, whereas the nursing personnel not involved in the direct management of the patients (e.g., nursing managers, tutorial staff) and those nurses who were students, retired, and on sick or maternity leave and with less than six months of working experience were excluded from the study.
2.3. Sample Size and Sampling Procedure
The actual sample size for the study was determined using the formula for a single population proportion. To determine the initial sample size, the following assumption has been made: ni is the initial sample size from a finite population, nfis the final sample size from a finite population, Z is the standard score (critical value) corresponding to the 95% confidence level, and p is the proportion of nurses experiencing needlestick and sharp injuries, which was 39.3%, taken from a study done in Jimma University Specialized Hospital taking the prevalence of NSSI among nurses [45]. So sample size can be calculated as follows: ni = (Za/2)2 × P(1 − P)/d2 = (1.96)2 × 0.393(1 − 0.393)/(0.05)2 = 367. Because of the total population size of the study area (N = 789) which is less than 10,000, we shall apply the population correction formula: nf = ni/1 + ni/N = 367/1 + 367/789 = 250, and by adding a 10% nonresponse rate, the total sample size of this study was 275. A stratified random sampling technique was used to select the nurses. Hospital departments are classified into 5 main strata that had nearly the same working conditions: (1) internal medicine, (2) pediatric, (3) surgical, (4) outpatient clinic, and (5) emergency and intensive care departments. The proportional allocation was taken from each stratum. Data were collected in Tikur Anbessa Specialized Hospital by introducing themselves (researchers), explaining the aim of the study, and acquiring consent. Data assurance was applied from the very beginning by review prior to the study and pretested by taking 5% of the study sample and by closely monitoring the activity of data collectors and supervisors by the principal investigator. The collected data were checked for completeness, accuracy, and clarity. Codes were given to the questionnaire, and any identified errors could get traced back using the codes. Each filled questionnaire was checked and reviewed for completeness by the supervisor and principal investigator; the necessary feedback was given to the data collectors the next morning (Figure 2).
Figure 2.
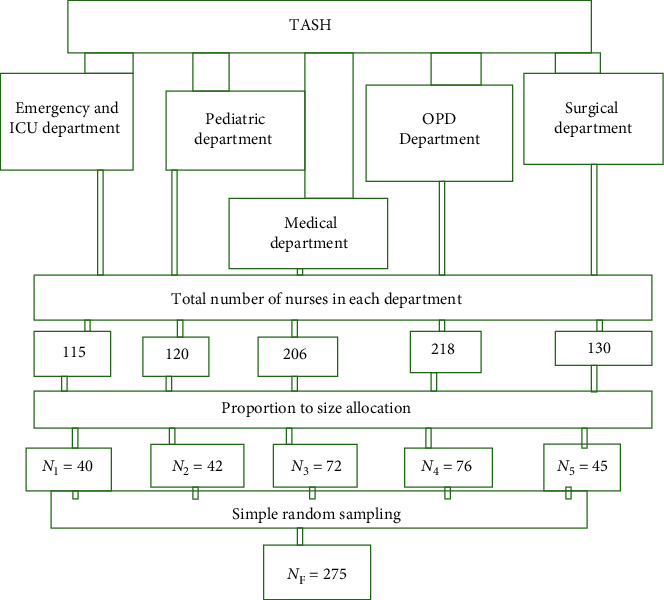
Schematic presentation of the sampling procedure to select the study participants, TASH, Addis Ababa, Ethiopia, June 2018.
2.4. Data Collection Tool and Procedure
Data were collected using a structured self-administered questionnaire. The questionnaire was adapted by reviewing the literature of similar studies on needlestick and sharp injuries [46–48] and adapted from the WHO/ICN (World Health Organization and International Council of Nurses) tool kit injection safety and the experience of the research done by the Ethiopian Nurse Association [49]. The questionnaire had 3 parts:
Part one: sociodemographic characteristics and work-related aspects (years of experience, department, hepatitis B vaccine status, etc.)
Part two: information on needlestick injury and sharp injury
Part three: circumstances or procedures that contribute to NSSI
For a binary outcome variable indicating “have you had any sharp and needlestick injury since last year?”, the response was coded as “yes” and “no” and it was used as the dependent variable. Data were collected by four trained data collectors (BSC nurse professionals) using the Amharic version of the questionnaire. The questionnaire was designed in English and was translated to Amharic, the official language of Ethiopia, and back to English (forward and backward translation for its consistency). The training was on introduction to NSSI, research methods, sampling and recruitment, and ethical aspects of research.
2.5. Data Processing and Analysis
The data cleanup and cross-checking were done before analysis. Data were checked and coded, and completed questionnaires were given identification numbers and entered into Epi Info version 7.2.2; then, they were exported to SPSS version 23 for analysis. Both the descriptive and analytical statistical procedures were utilized. Descriptive statistics like percentage, mean, and standard deviation were used for the presentation of sociodemographic data and prevalence of needlestick and/or sharp injury. Tables were also used for data presentation. Binary logistic regression was used to identify associated factors of needlestick and sharp injuries among nurses working at Tikur Anbessa Specialized Hospital. All explanatory variables with a p value of ≤0.2 from the bivariate logistic regression model were fitted into the multivariate logistic regression model to control the possible effect of confounders, and finally, the variables which had an independent association with needlestick and/or sharp injury were identified based on OR with 95% CI, and p values less than 0.05 were significant. The total model was significant (p ≤ 0.001). Multicollinearity was detected by tolerance, variance inflation factor (VIF), and correlation matrix. In this study, the values of tolerance, variance inflation factor (VIF), and correlation matrix were 0.498-0.964, 1.037-2.009, and ≤0.66, respectively.
The value of the standard error in the model (0.127) was below 5 which indicated no multicollinearity among variables. The result of the Hosmer and Lemeshow test (p = 0.791) indicated the goodness of fit of the model. Nagelkerke's R2 shows that about 50% of the variation in the outcome variable (NSSI) is explained by this binary logistic regression model.
3. Result
3.1. Sociodemographic Characteristics of Participants
A total of 268 hospital nurses responded fully to the self-administered questionnaire providing a response rate of 97.5%. Of the total, 191 (71.3%) respondents were female nurses. 115 (42.9%) of respondents were between the ages of 25-30 with a mean age of 29.97 years (SD ± 5.68 years). One hundred eighty-seven (69.8%) of participants were Orthodox Christians. More than half (158 (58.9%)) of participants were single. One hundred ninety-eight (73.9%) of nurses have work experience of fewer than five years with a mean work experience of 5.08 years (SD ± 5.883 years). The majority (202 (75.4%)) of the study participants were BSC nurses. Regarding the injection environment, 187 (69.8%) staff responded that their injection environments were unsafe. From the total respondents, one hundred forty-six (54.5%) had offsite and onsite training on infection prevention before the study (Table 1).
Table 1.
Distribution of sociodemographic, working environment, and behavioral characteristics of nurses, TASH, Addis Ababa, Ethiopia, June 2018.
| Variables | Characteristics | Frequency (N = 268) | Percentage (%) |
|---|---|---|---|
| Age | <25 | 59 | 22.0 |
| 25-30 | 115 | 42.9 | |
| >30 | 94 | 35.1 | |
| Total | 268 | 100 | |
|
| |||
| Sex | Male | 77 | 28.7 |
| Female | 191 | 71.3 | |
| Total | 268 | 100 | |
|
| |||
| Religion | Orthodox | 187 | 69.8 |
| Protestant | 40 | 14.9 | |
| Muslim | 35 | 13.1 | |
| Catholic | 6 | 2.2 | |
| Total | 268 | 100 | |
|
| |||
| Marital status | Single | 158 | 59.0 |
| Married | 89 | 33.2 | |
| Divorced | 9 | 3.4 | |
| Widowed | 12 | 4.5 | |
| Total | 268 | 100 | |
|
| |||
| Educational status | Diploma | 31 | 11.6 |
| BSC | 202 | 75.4 | |
| MSC | 35 | 13.1 | |
| Total | 268 | 100 | |
|
| |||
| Work experiences | <5 | 198 | 73.9 |
| 5-10 | 41 | 15.3 | |
| >10 | 29 | 10.8 | |
| Total | 268 | 100 | |
|
| |||
| Working departments | Emergency & ICU | 38 | 14.2 |
| Medical | 72 | 26.9 | |
| Surgical | 45 | 16.8 | |
| OPD | 73 | 27.2 | |
| Pediatric | 40 | 14.9 | |
| Total | 268 | 100 | |
|
| |||
| Training | Yes | 146 | 54.5 |
| No | 122 | 45.5 | |
| Total | 268 | 100 | |
|
| |||
| IP committee | Yes | 197 | 73.5 |
| No | 71 | 26.5 | |
| Total | 268 | 100 | |
|
| |||
| PEP | Yes | 150 | 56 |
| No | 118 | 44 | |
| Total | 268 | 100 | |
|
| |||
| HBV vaccination | Yes | 174 | 64.9 |
| No | 94 | 35.1 | |
| Total | 268 | 100 | |
|
| |||
| Department report when NSSI occurs | Yes | 173 | 64.6 |
| No | 95 | 35.4 | |
| Total | 268 | 100 | |
|
| |||
| Recapping of a needle after use | Yes | 118 | 44.0 |
| No | 150 | 56.0 | |
| Total | 268 | 100 | |
|
| |||
| Observe any NSSI on nurses | Yes | 193 | 72 |
| No | 75 | 28 | |
| Total | 268 | 100 | |
|
| |||
| Sharp collection box | Yes | 180 | 67.2 |
| No | 88 | 32.8 | |
| Total | 268 | 100 | |
|
| |||
| Injection equipment | Sterilized and reused | 21 | 7.8 |
| Single-use | 233 | 86.9 | |
| Autodisposable | 14 | 5.2 | |
| Total | 268 | 100 | |
|
| |||
| Recommended practice to prevent NSSI | Yes | 192 | 71.6 |
| No | 76 | 28.4 | |
| Total | 268 | 100 | |
|
| |||
| Dirty sharps in working places | Yes | 184 | 68.7 |
| No | 84 | 31.3 | |
| Total | 268 | 100 | |
|
| |||
| Injection environment | Safe | 81 | 30.2 |
| Unsafe | 187 | 69.8 | |
| Total | 268 | 100 | |
∗OPD = outpatient department; ICU = intensive care units; NSSI = needlestick and/or sharp injuries; TASH = Tikur Anbessa Specialized Hospital; IP = infection prevention; HBV = hepatitis B virus; PEP = postexposure practice.
3.2. Magnitude and Circumstances of Needlestick and/or Sharp Injuries
The prevalence (occurrence) of needlestick and sharp injuries to nurses in TASH was 97 (36.2%) (95% CI 30.2%, 42.3%). From the total of respondents who had experienced NSSI in the last 12 months before the study, 49.5% were exposed once, while 27.8%, 14.4%, and 8.2% were exposed two, three, and four times per year, respectively. But out of the total respondents who had experienced NSSI in the last year, 58.8% of nurses were exposed one month before the study, while 6.2% were exposed two times and none of the respondents were exposed three, four, and more times per month. Nearly one-half of (46.2%) injuries occurred in the ICU. Other injuries occurred in the surgical (44.4%), medical (39.9%), emergency (36%), OPD (35.6%), and pediatric (20%) departments. Regarding parts of the body injured, the finger accounted for 72.2% followed by the hand (15.5%), and 7.2%, 7.2%, and 6.2% were the arm, thigh, and palm, respectively.
The degree or severity of injury accounted for by slight skin penetration was 53.6%, followed by superficial and deep injuries which were 33% and 18.6%, respectively. On the other hand, injuries of 77.3% of nurses were self-inflicted and injuries of 14.4% and 12.4% of nurses were inflicted by another staff and a noncompliant patient, respectively. Regarding the practice of nurses on the job, 44% of the respondents had recapped needles after use at least once during their work time. Of those, 69.5% of the needles were recapped using one-handed recapping, whereas nearly one-third (30.5%) of needles were recapped using two-handed recapping. Among those nurses exposed to NSSI, workload (61.9%), fatigue (7.2%), and lack of proper equipment disposal (35.1%) were perceived as causes of NSSI. 64.5% of nurses know in which department or room they report, and 71.3% of nurses responded that safety boxes were available at the right working places. The study result revealed that the most frequent causative tools of needlestick and sharp injuries among exposed nurses were needles (87.6%) followed by blades (9.3%) and then lancets (5.2%) (Figure 3).
Figure 3.
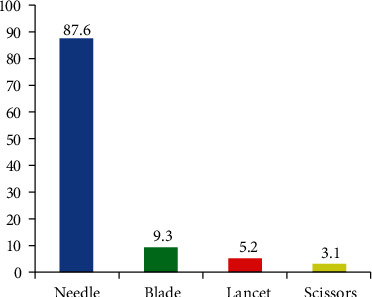
Frequency distribution of causative tools of needlestick and sharp injuries among exposed nurses during the last year working at TASH, Addis Ababa, Ethiopia, June 2018.
This study result represented that the most frequent procedures at which exposure happens were injection, sample drawing, and operation (38.1%, 24.7%, and 16.5%), respectively. In this study, 51.5% of nurses used antiseptic after NSSI exposure while 45.4% let blood flow. Regarding vaccination, only 2.1% took the vaccine while no one reported the incident after exposure (Table 2).
Table 2.
Frequency distribution of procedures at which exposure happened and actions taken after exposure happened among the exposed nurses during the last year working at TASH, Addis Ababa, Ethiopia, June 2018.
| Procedures at which exposure happened among exposed nurses | N = 97 | Percent (%)∗ |
|---|---|---|
| Injection | 37 | 38.1 |
| Suturing wound | 12 | 12.4 |
| Sample drawing | 24 | 24.7 |
| Operation | 16 | 16.5 |
| Needle recapping | 10 | 10.3 |
| Sharp disposal | 6 | 6.2 |
| Cleaning and sterilization of instruments | 12 | 12.4 |
| Failing of tools | 2 | 2.1 |
| Actions taken after exposure happened | ||
| Let blood flow | 11 | 11.3 |
| Wash with water | 50 | 51.5 |
| Use antiseptic | 44 | 45.4 |
| Lab investigation | 2 | 2.1 |
| Vaccination | 2 | 2.1 |
| Seroprophylaxis | 9 | 9.3 |
∗Each of the percentages does not add up to 100% because respondents could choose several responses which could be more than one reason.
In this study, among exposed nurses during the last year, the most likely cause of needlestick and/or sharp injuries was the syringe (74.2%) (Figure 4).
Figure 4.
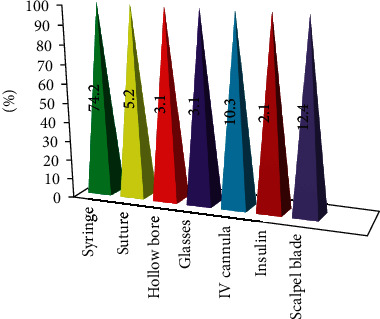
Frequency distribution of the type of items that causes NSSI among exposed nurses during the last year working at TASH, Addis Ababa, Ethiopia, June 2018.
In this study result, the factors that contributed to NSSI were excess clients (35.7%) followed by shortage of gloves (29.6%), and the rest were suturing (17.35%), shortage of sharp collection boxes (13.3%), emergencies (5.1%), recapping of used needles (8.2%), and removing of used needles (12.2%). In another way from the total respondents, 193 (72%) of nurses observe needlestick and sharp injuries on nurses. From this, in 101 (52.3%) nurses, NSSI occurs by the abrupt movement of patients during clinical practice, followed by unsafe sharp collection (51 (26.4%)), and the rest were two-handed recapping (37 (19.2%)) and carelessness (negligence) (18 (9.3%)) of nurses, respectively. In this study, from 268 participants, 180 (67.2%) of nurses say that there was a sharp collection box in the clinical area (Figure 5).
Figure 5.
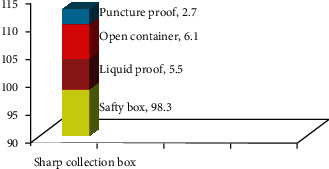
Distribution of the sharp collection box in the clinical area of TASH, Addis Ababa, Ethiopia, June 2018.
In this study, from 268 study participants, 188 (70.1%) of nurses had seen overfilled sharp collection containers in the clinical area, whereas 50 (18.7%) and 30 (11.2%) had seen torn needles and seen dirty syringes inside, respectively (Figure 6).
Figure 6.
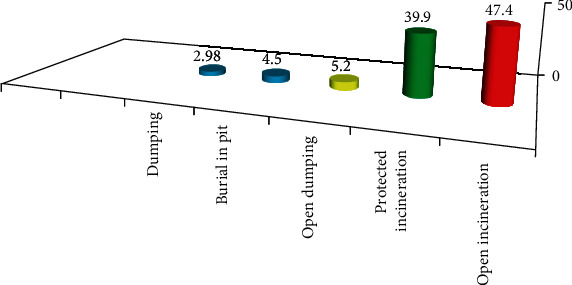
Percentage distribution of the needle, syringe, and sharp disposal system in TASH, Addis Ababa, Ethiopia, June 2018.
3.3. Determinants of Needlestick and/or Sharp Injuries within the Past 12 Months
3.3.1. Bivariate Logistic Regression Model Analysis of Factors Associated with NSSI
As shown in Table 3, the regression analysis of sociodemographic and NSSI circumstances on bivariate logistic regression showed that sex (COR = 0.425 (95% CI 0.247, 0.731)), educational status (COR = 0.227 (95% CI 0.075, 0.688)), current working department (COR = 0.313 (95% CI 0.118, 0.8270)), dirty sharps in working places (COR = 1.939 (95% CI 1.098, 3.423)), and needle recapping (COR = 1.964 (95% CI 1.185, 3.255)) had a significant association with NSSI. On bivariate logistic regression analysis, respondents being diploma holders in educational status were 77% less likely to risk experiencing injury compared to their counterparts (Table 3).
Table 3.
Bivariate logistic regression model analysis of factors associated with NSSI, TASH, Addis Ababa, Ethiopia, June 2018.
| Variables | Category | NSSI | COR (95% CI) | p value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age | <25 | 21 | 38 | 0.932 (0.473, 1.834) | 0.838 |
| 25-30 | 41 | 74 | 0.934 (0.530, 1.645) | 0.813 | |
| >30 | 35 | 59 | 1 | ||
|
| |||||
| Sex | Male | 39 | 38 | 1 | |
| Female | 58 | 133 | 0.425 (0.247, 0.731) | 0.002∗∗ | |
|
| |||||
| Marital status | Single | 53 | 105 | 0.707 (0.214, 2.3330) | 0.569 |
| Married | 35 | 54 | 0.907 (0.267, 3.7086) | 0.876 | |
| Divorced | 4 | 5 | 1.120 (0.196, 6.414) | 0.899 | |
| Widowed | 5 | 7 | 1 | ||
|
| |||||
| Educational status | BSC | 73 | 129 | 0.5349 (0.260, 1.101) | 0.089∗ |
| Diploma | 6 | 25 | 0.227 (0.075, 0.688) | 0.009∗∗ | |
| MSC | 18 | 17 | 1 | ||
|
| |||||
| Working departments | Emergency | 9 | 16 | 0.703 (0.257, 1.923) | 0.493 |
| ICU | 6 | 7 | 1.071 (0.310, 3.6980) | 0.913 | |
| Medical | 28 | 44 | 0.795 (0.374, 1.6930) | 0.553 | |
| Surgical | 20 | 5 | 1 | ||
| OPD | 26 | 47 | 0.691 (0.324, 1.476) | 0.340 | |
| Pediatric | 8 | 32 | 0.313 (0.118, 0.827) | 0.019∗∗ | |
|
| |||||
| Training | Yes | 60 | 86 | 1.603 (0.965, 2.663) | 0.069∗ |
| No | 37 | 85 | 1 | ||
|
| |||||
| Working experiences | <5 | 71 | 127 | 0.599 (0.273, 1.312) | 0.200∗ |
| 5-10 | 12 | 29 | 0.4439 (0.164, 1.195) | 0.108∗ | |
| >10 | 14 | 15 | 1 | ||
|
| |||||
| Dirty sharps in working places | Yes | 75 | 109 | 1.939 (1.098, 3.423) | 0.022∗∗ |
| No | 22 | 62 | 1 | ||
|
| |||||
| IP committee | Yes | 76 | 21 | 1.495 (0.833, 2.684) | 0.1778∗ |
| No | 121 | 50 | 1 | ||
|
| |||||
| Safety box at right places | Yes | 70 | 121 | 1.071 (0.616, 1.862) | 0.808 |
| No | 27 | 50 | 1 | ||
|
| |||||
| Universal precaution | Yes | 72 | 120 | 1.224 (0.699, 2.144) | 0.480 |
| No | 25 | 51 | 1 | ||
|
| |||||
| Sharp collection box | Yes | 66 | 114 | 1.065 (0.625, 1.812) | 0.818 |
| No | 31 | 57 | 1 | ||
|
| |||||
| Needle recapping | Yes | 53 | 65 | 1.964 (1.185, 3.255) | 0.009∗∗ |
| No | 44 | 106 | 1 | ||
|
| |||||
| Injection environments | Safe | 32 | 49 | 1 | |
| Unsafe | 65 | 122 | 1.226 (0.716, 2.098) | 0.458 | |
∗Significant at p ≤ 0.2. ∗∗Significant at p ≤ 0.05. COR = crude odds ratio; OPD = outpatient department; ICU = intensive care units; NSSI = needlestick and/or sharp injuries; TASH = Tikur Anbessa Specialized Hospital; IP = infection prevention; HBV = hepatitis B virus; PEP = postexposure practice.
3.3.2. Multivariate Logistic Regression Model Analysis of Factors Associated with NSSI
In the multivariate logistic regression analysis, sex, current working department, dirty sharps in working places, and needle recapping are statistically significant with the occurrence of needlestick and/or sharp injury. But working experiences, educational status, and status of the infection prevention committee had not shown any significant association. Those variables were not significant after controlling other variables in multivariate logistic regression analysis. In multivariate logistic regression analysis, the odds of needlestick or sharp injury was 54% less likely in female nurses than male nurses (AOR = 0.461 (95% CI 0.252, 0.845)). Those who worked in the pediatric ward were 68% less likely to get injured by needlestick and sharp objects than those who worked in the surgical ward (AOR = 0.323 (95% CI 0.112, 0.930)). The risk of NSSI was 1.78 times higher in nurses who recapped needles after use than those nurses who had not recapped needles after use (AOR = 1.780 (95% CI 1.025, 3.091)) (Table 4).
Table 4.
Logistic regression model analysis of factors associated with NSSI, TASH, Addis Ababa, Ethiopia, June 2018 (N = 268).
| Variables | Category | NSSI | AOR (95% CI) | p value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Sex | Male | 39 | 38 | 1 | |
| Female | 58 | 133 | 0.461 (0.252, 0.845) | 0.012∗ | |
|
| |||||
| Working departments | Emergency | 9 | 16 | 0.670 (0.226, 1.984) | 0.469 |
| ICU | 6 | 7 | 0.8464 (0.214, 3.487) | 0.838 | |
| Medical | 28 | 44 | 0.666 (0.288, 1.542) | 0.343 | |
| OPD | 26 | 47 | 0.711 (0.299, 1.692) | 0.441 | |
| Pediatric | 8 | 32 | 0.323 (0.112, 0.930) | 0.036∗ | |
| Surgical | 20 | 25 | 1 | ||
|
| |||||
| Educational status | BSC | 73 | 129 | 0.460 (0.172, 1.234) | 0.123 |
| Diploma | 6 | 25 | 0.256 (0.063, 1.048) | 0.058 | |
| MSC | 18 | 17 | 1 | ||
|
| |||||
| Dirty sharps in working places | Yes | 75 | 109 | 2.052 (1.110, 3.791) | 0.022∗ |
| No | 22 | 62 | 1 | ||
|
| |||||
| Work experiences | <5 | 71 | 127 | 1.413 (0.520, 3.839) | 0.498 |
| 5-10 | 12 | 29 | 0.602 (0.202, 1.795) | 0.363 | |
| >10 | 14 | 15 | 1 | ||
|
| |||||
| IP committee | Yes | 76 | 121 | 1.702 (0.878, 3.299) | 0.116 |
| No | 21 | 50 | 1 | ||
|
| |||||
| Needle recapping | Yes | 53 | 65 | 1.780 (1.025, 3.091) | 0.041∗ |
| No | 44 | 106 | 1 | ||
|
| |||||
| Training | Yes | 60 | 86 | 0.753 (0.429, 1.323) | 0.324 |
| No | 37 | 85 | 1 | ||
∗Significant at p ≤ 0.05. AOR = adjusted odds ratio; OPD = outpatient department; ICU = intensive care units; NSSI = needlestick and/or sharp injuries; TASH = Tikur Anbessa Specialized Hospital.
4. Discussion
In this study, the prevalence of nurses who sustains NSSI in the last 12 months was found to be 36.2% (95% CI 30.2%, 42.3%). This is in line with the studies done in Jimma University Hospital, Ethiopia (39.3%) [50]; India (33.3%) [17]; Tehran (41%) [19]; Southern Ethiopia (42.1%) [51]; Malaysia (31.6) [52]; Iran (39.4%) [53]; and Bahir Dar, Northwest Ethiopia (31.0%) [54]. The current study demonstrated that the magnitude of NSSI was higher than studies done in South Africa (18.8%, 23.5%) [31, 55]; Awi zone, Ethiopia (18.7%) [56]; Nigeria (23.1%) [57]; Tigray, Northern Ethiopia (25.9%) [58]; Bahir Dar (29%) [59]; Malaysia (23.5%, 24.6%, and 9.8%) [60–62]; Kenya (19%) [27]; United Arab Emirates (19%) [63]; East Gojjam, Ethiopia (22.2%) [64]; and Switzerland (9.7%) [65]. It could be due to the difference in the study health facility setups so that the number of screening, diagnostic, follow-up, and other intervention procedures that use needles and medical sharp materials was less in health centers and even the year of the study. But whatever is the difference in the proportion of needlestick and sharp injuries, nurses are at much higher risk to acquire bloodborne pathogens such as HIV and other infectious diseases through needlestick and sharp injuries.
The prevalence in this study is lower than the figure from earlier studies in Southwest Ethiopia (58.8%) [44]; Sri Lanka (43%) [22]; Thailand Regional Hospital (55.5%) [16]; Iran Shiraz University Hospital (54%) [20]; Nigeria (55.8%) [57]; Dessie, Ethiopia (43%) [66]; Saudi Arabia (50.9%) [67]; Egypt (62.3%, 67.9%) [68]; Sarajevo, Bosnia and Herzegovina (61.1%) [69]; Jimma, Ethiopia (44.12) [70]; Hawassa, Ethiopia (46%) [47]; Pakistan (66%) [71]; and Jordan (67.6%) [21]. However, this result is much lower when compared with a study done in Bahir Dar, Ethiopia (66.6%) [37]; South Korea (74.4%) [14]; Pakistan (67%) [15]; and Nepal (74%) [18]. This difference might be related to the fact that the above studies were conducted by mixing all types of health professionals from hospitals, health centers, and clinics, including sociodemographic/economic status, cultural characteristics of the study participants, sampling method, and sample size. The other possible reason might be related to workload and the availability of resources, as well as the work environment, and related to a different time of recall periods.
In this study, the majority of injuries were slight skin penetration (53.1%) while 32.7% were superficial. Regarding causative tools, the most frequent causative tools were needles (86.3%). The present study revealed that 51% of exposed nurses wash with water after exposure while 44.9% with an antiseptic solution. This was lower than the study conducted in Zagazig University, Egypt, which reported that the severity of penetration of needlestick and sharp injuries during the last year among nurses was superficial (74.24%), and the procedures which mostly exposed nurses were injection and withdrawal of blood (56.06% and 43.18%), respectively, and the procedure taken after exposure showed that all exposed nurses used antiseptic after exposure while half of them let blood flow [1]. But this result is higher than the study done by Jimma University for nurses which showed 25.6% for needles and 23.2% for surgical blades [50]. This variation might be due to different times of the recall period. The current study revealed that the syringe needle was a major cause of the injuries (74.2%). It is much higher as compared to the study done in Tehran (Iran) (46.3%) [19] and Southwest Ethiopia (58.8%) [35]. However, it is consistent with a study done in South Africa (78.3%) [31]. This implies that nurses who had been injured by NSSI might be due to inappropriate needle handling practices. It might also be because the majority of the procedures done for the patients require syringe needles that may put nurses at risk of injuries.
Regarding the frequency of injury, 49.5% of the respondents had experienced injuries at least once in a year. This is a little bit higher than the study done in India (33.3%) [17]. But whatever the difference of the proportions of NSSI, nurses might practice needle recapping after use which may put them at risk of injury. For instance, the prevalence of needle recapping after use in this study was 44%, and of these, nearly one-third (30.5%) was recapping using two hands. The practice of recapping is higher in the studies in Nigeria (35.3%) [72]. In this study, injection (37.7%) and blood withdrawal (24.5%) were the major clinical activities that lead to NSSI in this study. A study conducted in Saudi Arabia showed that most of the injuries occur during injections (31.8%) and drawing of venous blood samples (17.2%) [73], and a study conducted in India showed that the commonest clinical activities to cause NSSIS in that study were blood withdrawal (55%), suturing (20.3%), vaccination (11.7%), and recapping needles after use (66.3%), and according to a study done on Malaysian hospital nurses, 27.2% of NSSI causes were recapping of syringes after use [60]. In this study, 64.9% of nurses were vaccinated against hepatitis B. This result is higher than a study done in Jimma University Hospital which showed that 1.76% of the study subjects were vaccinated for hepatitis B vaccine [50], and a study conducted in Egypt showed that only 6.81% were vaccinated for hepatitis B [1]. This variation may be due to the presence of the vaccine in TASH.
Regarding factors found to be associated with the high prevalence of NSSI. From those factors, being female was significantly associated with NSSI; the odds of needlestick or sharp injury was 54% less likely in female nurses than male nurses (AOR = 0.461 (95% CI 0.252, 0.845)). This is consistent with the report from Southwest Ethiopia [35]. The possible explanations might be because men are less likely to use universal precautions, but further studies are warranted to identify exposure differences. Those who worked in the pediatric ward were 68% less likely to get injured by needlestick and sharp objects than those who worked in the surgical ward: AOR = 0.323 (95% CI 0.112, 0.930). This may be because more advanced procedures and manipulation of the syringe and sharp materials were done in the surgical ward. Respondents who practiced needle recapping were 1.78 times more likely to experience an injury than those who did not recap needles after use: AOR = 1.780 (95% CI 1.025, 3.091). This is supported by previous studies [36].
According to this study, there was also a statistically significant difference of NSSI among nurses working in the presence of contaminated needles and sharp materials in the working places (AOR = 2.052 (95% CI 1.110, 3.791)) than their counterparts. Neither age nor marital status was significant, but training and work experience had a significant effect on the magnitude of NSSI among nurses. This is inconsistent with a study conducted in Malaysia [60]. The possible justification might be due to the setup and working environment safety. A safe working environment reduces the probability of sustained needlestick and sharp injuries.
Current working unit/department (AOR = 0.323 (95% CI 0.112, 0.930)), sex (AOR = 0.461 (95% CI 0.252, 0.845)), presence of contaminated needles and sharp materials in the working area (AOR = 2.052 (95% CI 1.110, 3.791)), and needle recapping (AOR = 1.780 (95% CI 1.025, 3.091)) had a significant association with the occurrence of sharp and needlestick injuries in nurses at p < 0.05. This result is almost different with the study conducted in East Gojjam Zone Health Institutions health care workers which showed the following results: infection prevention and safety information access and getting training on infection prevention showed a significant association with the occurrence of needlestick and sharp injuries in health care workers [64]. This difference may be related to the difference of the setups they used (standard precaution guidelines) and the mixing of all types of health professionals from health centers. Taking training on infection prevention was not found to be statistically significant in multivariable analysis in this study. Similarly, this finding goes in line with previous findings in a study in Bahir Dar [59], in which training for workers did not necessarily bring about protection from injury exposure. The reason for this may be because the knowledge gained may not necessarily be transferred into the practice of preventive measures and those who participated in the infection prevention training may be other workers who are working as nursing managers and are not involved in clinical practice. Lastly, the sample size might not be sufficient enough to detect the differences. Besides, the result of this study indicates that the infection prevention committee was not a significant determinant of needlestick and sharp injuries. This study was inconsistent with other previous studies [74]. On the opposite side, a study carried out in Debre Berhan, Ethiopia, revealed that the absence of onsite training on IP and safety practice was the main contributor to occupational exposure [75]. According to a study done in Kenya, previous training on IP was protective [27]. The reason for this difference could be the methodological differences and variation in study recall periods, the difference of the setups they used (standard precaution guidelines), and the mixing of all types of health professionals from health centers. The current study found out that educational status was not significantly associated with needlestick and sharp injuries. However, in a study conducted in Egypt, low education levels were the most significant predictors of needlestick and sharp injuries among nurses [1]. Moreover, the result of this study indicates that work experience was not a significant predictor of needlestick and sharp injuries. This study was inconsistent with other previous studies [21, 76]. Generally, needlestick or sharp injury is significantly different among current working unit/department, sex, presence of contaminated needles and sharp materials in the working area, and needle recapping. For the health care provider, complete surveillance of exposure is necessary for the identification of high-risk activities and environments to define new targets for preventive measures and monitoring of the success and failure of the measure taken.
5. Strength and Limitation of the Study
Since the study was conducted among randomly selected nurses, it might be generalized to all nurses who had direct contact with patients or equipment used on patients when working in the study hospital. Some staff could not remember if they sustained needlestick and sharp injuries within the past 12 months, some respondents were not sure if their information was kept secret, and nurses were recruited during their lunchtime and were not comfortable to answer freely. Since participants have been asked a one-year exposure experience, there might be recall bias. Since the study was based on self-reported data in estimating the prevalence of NSSI exposure, a common threat to the validity of the self-report can lead to information bias such as social desirability and recall bias. Besides, a cross-sectional study by its nature cannot establish a definitive cause-and-effect relationship to identify the risk factors.
6. Conclusion
This study revealed that more than one-third of the study participants had needlestick and/or sharp injury at least once in the previous 12 months. The proportion of needlestick and sharp injuries in the last year was found to be high. In general, this study revealed that no single factor accounted for the occurrence of NSSI. The presence of contaminated needles and/or sharp materials in the working area and needle recapping after use were positively associated with needlestick/sharp injury, while working in the pediatric ward and being female showed a negative association.
7. Recommendation
Based on the findings of this study, the following recommendations are forwarded to MOH Ethiopia, Addis Ababa City Administration Health Bureau, TASH managers, and TASH nursing professionals to reduce the occurrence of NSSI and the consequences of NSSI among nurses working in TASH:
TASH Hospital Administrates and Nursing Service Directors. Strengthened regular provision of information on infection prevention and safety to nurses at all levels to create a safe working environment for nurses. Continuous monitoring of workplace safety and an appropriate sharp disposal system
TASH Nurse Professionals. Practice proper use of safety boxes and personal protective equipment when handling needles and sharps. Nurses involved in safe segregation and disposal of all sharp items immediately in marked containers
Health Policymakers. Formulate strategies to improve the working condition for nursing professionals and increase their adherence to universal precautions
MOH. Continuous monitoring of workplace safety should be ensured by MOH
Addis Ababa City Administration Health Bureau. Regular reporting, follow-up, and evaluation of occupational injury exposure among nurses need to be introduced
NGO. Creating awareness for nursing professionals on safety practices of injection
Acknowledgments
We would like to thank Addis Ababa University and the hospital directors and the head of each working unit of TASH for their kind assistance during data collection. The authors also would like to thank all of the study participants who participated in this study.
Abbreviations
- AAU:
Addis Ababa University
- AIDS:
Acquired immunodeficiency syndrome
- AOR:
Adjusted odds ratio
- BSC:
Bachelor of Science
- CHS:
College of Health Sciences
- CI:
Confidence interval
- COR:
Crude odds ratio
- GC:
Gregorian calendar
- HBV:
Hepatitis B virus
- HCV:
Hepatitis C virus
- ICN:
International Council of Nurses
- HIV:
Human immunodeficiency virus
- NSI:
Needlestick injury
- NSSI:
Needlestick and sharp injury
- TASH:
Tikur Anbessa Specialized Hospital
- USA:
United States of America
- WHO:
World Health Organization.
Data Availability
All data about this study are contained and presented in this document.
Ethical Approval
Ethical clearance was obtained from the Institutional Review Board of Addis Ababa University, College of Medicine and Health Science, Department of Emergency Medicine and Critical Care (Ref No. EM/533/2018). An official letter of permission was obtained from the administration of Tikur Anbessa Specialized Hospital. A letter of cooperation was written by TASH to conduct this research in the hospital.
Consent
Informed consent was obtained from participants who signed or gave verbal consent to fill the questionnaires. Nurses who refused to participate in the survey were not forced to participate in the study. Each study subject was informed about the objective of the study and the confidentiality of the information they gave. Besides, they were told that they have the full right to withdraw from the study at any time if they feel uncomfortable.
Conflicts of Interest
The authors declare no competing interest.
Authors' Contributions
BL conceived and designed the study, analyzed the data, and wrote the manuscript. MS, MM, ADT, and TK advised about the whole research paper and also were involved in the interpretation of the data and contributed to manuscript preparation. All authors read and approved the final manuscript.
References
- 1.Ahmed A. S. Needle stick and sharp injuries among nurses at Zagazig University Hospitals, Sharkia Governorate, Egypt. Middle East Journal of Applied Sciences. 2014;4(4):1205–1211. [Google Scholar]
- 2.Singru S. A., Banerjee A. Occupational exposure to blood and body fluids among health care workers in a teaching hospital in Mumbai, India. Indian Journal of Community Medicine. 2008;33(1):26–30. doi: 10.4103/0970-0218.39239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elliott S., Keeton A., Holt A. Medical students' knowledge of sharps injuries. Journal of Hospital Infection. 2005;60(4):374–377. doi: 10.1016/j.jhin.2005.01.033. [DOI] [PubMed] [Google Scholar]
- 4.Organization WH. The world health report. Box 4.4. 2002. Geneva, Switzerland: World Health Organization; 2002. https://www.who.int/whr/2002/en/ [Google Scholar]
- 5.Organization WH. The world health report 2002: reducing risks, promoting healthy life. World Health Organization; 2002. [DOI] [PubMed] [Google Scholar]
- 6.Prüss-Üstün A., Rapiti E., Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. American Journal of Industrial Medicine. 2005;48(6):482–490. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 7.Rapiti E., Prüss-Üstün A., Hutin Y. J. Sharps Injuries: Assessing the Burden of Disease from Sharps Injuries to Health-Care Workers at National and Local Levels. Geneva: Environmental Burden of Disease Series; 2005. [Google Scholar]
- 8.Clarke S. P., Sloane D. M., Aiken L. H. Needlestick injuries to nurses, in context. LDI Issue Brief. 2002;8(1):1–4. [PubMed] [Google Scholar]
- 9.Trinkoff A. M., Le R., Geiger-Brown J., Lipscomb J. Work schedule, needle use, and needlestick injuries among registered nurses. Infection Control & Hospital Epidemiology. 2007;28(2):156–164. doi: 10.1086/510785. [DOI] [PubMed] [Google Scholar]
- 10.Abdulmahdi L. Implementation of online reporting form for needle stick injury in the accident and emergency department. Royal College of Surgeons in Ireland; 2014. [Google Scholar]
- 11.Doebbeling B. N., Vaughn T. E., McCoy K. D., et al. Percutaneous injury, blood exposure, and adherence to standard precautions: are hospital-based health care providers still at risk? Clinical Infectious Diseases. 2003;37(8):1006–1013. doi: 10.1086/377535. [DOI] [PubMed] [Google Scholar]
- 12.Ghofranipour F., Asadpour M., Ardebili H. E., Niknami S., Hajizadeh E. Needle sticks/sharps injuries and determinants in nursing care workers. European Journal of Social Sciences. 2009;11(2):191–197. [Google Scholar]
- 13.Risks R. Promoting healthy life. Vol. 58. The world health report; 2002. [Google Scholar]
- 14.Cho E., Lee H., Choi M., Park S. H., Yoo I. Y., Aiken L. H. Factors associated with needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire survey. International Journal of Nursing Studies. 2013;50(8):1025–1032. doi: 10.1016/j.ijnurstu.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Habib H., Khan E. A., Aziz A. Prevalence and factors associated with needle stick injuries among registered nurses in public sector tertiary care hospitals of Pakistan. 2011.
- 16.Honda M., Chompikul J., Chompikul J., Rattanapan C., Ratanapan C. Sharps injuries among nurses in a Thai regional hospital: prevalence and risk factors. 2011. [PubMed]
- 17.Kaushik A., Sarin J. Prevalence of needlestick injuries and its related factors among nurses. Surgery. 2016;4:10–17. [Google Scholar]
- 18.Gurubacharya D. L., Mathura K. C., Karki D. B. Knowledge, attitude, and practices among health care workers on needle-stick injuries. Kathmandu University medical journal (KUMJ) 2003;1(2):91–94. [PubMed] [Google Scholar]
- 19.Mahmodi N., Sepandi M., Mohammadi A. S., Masoumbeigi H. Epidemiological aspects of occupational exposure to sharp tools among nurses in a military hospital in Tehran, Iran. Iranian Journal of Health, Safety, and Environment. 2015;2(4):374–379. [Google Scholar]
- 20.Jahangiri M., Rostamabadi A., Hoboubi N., Tadayon N., Soleimani A. Needle stick injuries and their related safety measures among nurses in a university hospital, Shiraz, Iran. Safety and health at work. 2016;7(1):72–77. doi: 10.1016/j.shaw.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khraisat F. S., Juni M. H., Salmiah M., Rahman A. A., Hamdan-Mansour A. Needlestick injuries prevalence among nurses in Jordanian hospitals. International Journal of Public Health and Clinical Sciences. 2015;2(4):7–16. [Google Scholar]
- 22.Priyangani Y. M., Dharmaratne G. S., Sridharan S. Factors associated and response to needle stick injuries among nursing officers in district general hospitals of Sri Lanka. Global Journal of Health Science. 2017;9(8) doi: 10.5539/gjhs.v9n8p107. [DOI] [Google Scholar]
- 23.İlhan M. N., Durukan E., Aras E., Türkçüoğlu S., Aygün R. Long working hours increase the risk of sharp and needlestick injury in nurses: the need for new policy implication. Journal of advanced nursing. 2006;56(5):563–568. doi: 10.1111/j.1365-2648.2006.04041.x. [DOI] [PubMed] [Google Scholar]
- 24.Girmaye E. Assessment of percutaneous exposure incidents and associated factors among health care personnel at Gandhi Memorial Hospital. Addis Ababa: Addis Ababa University; 2015. [Google Scholar]
- 25.Reda A. A., Fisseha S., Mengistie B., Vandeweerd J.-M. Standard precautions: occupational exposure and behavior of health care workers in Ethiopia. PLoS One. 2010;5(12, article e14420) doi: 10.1371/journal.pone.0014420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Esin I., Ojo E., Alabi S., Ajape A. Knowledge of human immunodeficiency virus post-exposure prophylaxis among doctors in a Nigerian tertiary hospital. Nigerian Journal of clinical practice. 2011;14(4, article 91757):464–466. doi: 10.4103/1119-3077.91757. [DOI] [PubMed] [Google Scholar]
- 27.Mbaisi E. M., Ng'ang'a Z., Wanzala P., Omolo J. Prevalence and factors associated with percutaneous injuries and splash exposures among health-care workers in a provincial hospital, Kenya, 2010. Pan African Medical Journal. 2013;14(1) doi: 10.11604/pamj.2013.14.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henderson D. K. Management of needlestick injuries: a house officer who has a needlestick. Journal of the American Medical Association. 2012;307(1):75–84. doi: 10.1001/jama.2011.1828. [DOI] [PubMed] [Google Scholar]
- 29.Afridi A. A. K., Kumar A., Sayani R. Needle Stick Injuries – Risk and preventive factors: a study among health care workers in tertiary care hospitals in Pakistan. Global journal of health science. 2013;5(4):85–92. doi: 10.5539/gjhs.v5n4p85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mokuolu O., Olawumi H. Needlestick injuries among nurses in a Nigerian tertiary hospital. International journal of current research. 2011;3(7):12–14. [Google Scholar]
- 31.Kruger W. H., Joubert G., Jimoh S. O. Needlestick injuries among nurses in a regional hospital in South Africa. Occupational Health Southern Africa. 2012;18(3):4–10. [Google Scholar]
- 32.Alemayehu T. Assessment of health care workers occupational exposure to HIV and post- exposure prophylaxis (PEP) in health centers and hospitals of Addis Ababa, Ethiopia. International Journal of Infectious Diseases. 2010;14, article e249 doi: 10.1016/j.ijid.2010.02.2043. [DOI] [Google Scholar]
- 33.Tadesse M., Tadesse T. Epidemiology of needlestick injuries among health-care workers in Awassa City, Southern Ethiopia. Tropical doctor. 2010;40(2):111–113. doi: 10.1258/td.2009.090191. [DOI] [PubMed] [Google Scholar]
- 34.Wolde G. Y. Assessment of the safety of injections and related medical practices in health institutions in Sidamo Zone, SNNPR [MPH Thesis] Department of Community Health, Addis Ababa University; 2004. [Google Scholar]
- 35.Atlaw W. D. Patterns of occupational exposure to patients' body fluids among health care workers in Tikuranbesa University Hospital, Addis Ababa, Ethiopia. 2013.
- 36.Bidira K., Woldie M., Nemera G. Prevalence and predictor of needlestick injury among nurses in public hospitals of Jimma zone, Southwest Ethiopia. International Journal of Nursing and Midwifery. 2014;6(7):90–96. [Google Scholar]
- 37.Walle L., Abebe E., Tsegaye M., Franco H., Birhanu D., Azage M. Factors associated with needle stick and sharp injuries among healthcare workers in Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia: facility based cross-sectional survey. International Journal of Infection Control. 2013;9(4) doi: 10.3396/IJIC.v9i4.030.13. [DOI] [Google Scholar]
- 38.Smith D. R., Choe M.-A., Jeong J. S., Jeon M.-Y., Chae Y. R., An G. J. Epidemiology of needlestick and sharps injuries among professional Korean nurses. Journal of professional nursing. 2006;22(6):359–366. doi: 10.1016/j.profnurs.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 39.Ng L. N., Lim H. L., Chan Y. H., Bin Bachok D. Analysis of sharps injury occurrences at a hospital in Singapore. International journal of nursing practice. 2002;8(5):274–281. doi: 10.1046/j.1440-172X.2002.00377.x. [DOI] [PubMed] [Google Scholar]
- 40.Ayranci U., Kosgeroglu N. Needlestick and sharps injuries among nurses in the healthcare sector in a city of western Turkey. Journal of Hospital Infection. 2004;58(3):216–223. doi: 10.1016/j.jhin.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 41.Rodrigues C. Needlestick injuries & the health care worker--the time to act is now. Indian Journal of Medical Research. 2010;131(3):384–387. [PubMed] [Google Scholar]
- 42.Wilburn S. Q. Needlestick and sharps injury prevention. An online journal of issues in nursing. 2004;9(3) [PubMed] [Google Scholar]
- 43.Clarke S. P., Rockett J. L., Sloane D. M., Aiken L. H. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. American journal of infection control. 2002;30(4):207–216. doi: 10.1067/mic.2002.123392. [DOI] [PubMed] [Google Scholar]
- 44.Bidira K., Woldie M., Nemera G. Prevalence and predictors of needle stick injury among nurses in public hospitals of Jimma Zone, South West Ethiopia. International Journal of Nursing and Midwifery. 2014;6(7):90–96. [Google Scholar]
- 45.Bidira K., Woldie M., Nemera G. Prevalence and predictors of needlestick injury among nurses in public hospitals of Jimma Zone, South West Ethiopia. International Journal of Nursing and midwifery. 2014;6:90–96. [Google Scholar]
- 46.Beyene H., Yirsaw B. Occupational risk factors associated with needle-stick injury among healthcare workers in Hawassa City, Southern Ethiopia. Occupational Medicine & Health Affairs. 2014;2(156) [Google Scholar]
- 47.Kaweti G., Abegaz T. Prevalence of percutaneous injuries and associated factors among health care workers in Hawassa Referral and Adare District hospitals, Hawassa, Ethiopia, January 2014. BMC Public Health. 2015;16(1) doi: 10.1186/s12889-015-2642-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aynalem Tesfay F., Dejenie Habtewold T. Assessment of prevalence and determinants of occupational exposure to HIV infection among healthcare workers in selected health institutions in Debre Berhan town, North Shoa Zone, Amhara Region, Ethiopia, 2014. AIDS research and treatment. 2014;2014:11. doi: 10.1155/2014/731848.731848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Foley M., Leyden T. Needlestick prevention guide. Washington, DC: American Nurses Association‟ s; 2002. [Google Scholar]
- 50.Tesafa Bamlie J. B., Bamlie T. Needle Stick and sharp injuries and associated factors among nurses working in Jimma University Specialized Hospital, South West Ethiopia. Journal of Nursing & Care. 2015;4(5):1–8. doi: 10.4172/2167-1168.1000291. [DOI] [Google Scholar]
- 51.Kelebore W. G. Assessment of factors affecting needle stick and sharp injuries among health professionals and cleaners in Arba Minch General Hospital, Gamo Gofa Zone, Southern Ethiopia, 2015 G. C. Science Journal of Public Health. 2016;4(6, article 2511380) doi: 10.11648/j.sjph.20160406.18. [DOI] [Google Scholar]
- 52.Ng Y., Hassim I. N. Needlestick injury among medical personnel in accident and emergency department of two teaching hospital. Medical Journal of Malaysia. 2007;62(1) [PubMed] [Google Scholar]
- 53.Hofranipour F., Asadpour M., Ardebili H., Niknami S., Hajizadeh E. Needlestick/sharp injuries and determinants in nursing care. European Journal of Social Sciences. 2009;2(2):191–197. [Google Scholar]
- 54.Walle L., Abebe E., Tsegaye M., Franco H., Birhanu D., Azage M. Factors associated with needlestick and sharp injuries among healthcare workers in Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia: facility-based cross-sectional survey. International Journal of Infection Control. 2013;9(4):1–9. [Google Scholar]
- 55.Lachowicz R., Matthews P. The pattern of sharps injury to health care workers at Witbank Hospital. South African Family Practice. 2009;51(2):148–151. doi: 10.1080/20786204.2009.10873831. [DOI] [Google Scholar]
- 56.Dilie A., Amare D., Gualu T. Occupational exposure to needle stick and sharp injuries and associated factors among health care workers in Awi Zone, Amhara Regional State, Northwest Ethiopia, 2016. Journal of environmental and public health. 2017;2017:6. doi: 10.1155/2017/2438713.2438713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oluwatosin O. A., Oladapo M. M., Asuzu M. C. Needlestick injuries among health care workers in Ondo State, Nigeria. International Journal of Medicine and Public Health. 2016;6(1) doi: 10.4103/2230-8598.179757. [DOI] [Google Scholar]
- 58.Weldesamuel E., Gebreyesus H., Beyene B., Teweldemedhin M., Welegebriel Z., Tetemke D. Assessment of needle stick and sharp injuries among health care workers in central zone of Tigray, northern Ethiopia. BMC research notes. 2019;12(1, article 4683):1–6. doi: 10.1186/s13104-019-4683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yenesew M. A., Fekadu G. A. Occupational exposure to blood and body fluids among health care professionals in Bahir Dar town, Northwest Ethiopia. Safety and health at work. 2014;5(1):17–22. doi: 10.1016/j.shaw.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rampal L., Zakaria R., Sook L. W., Zain A. M. Needlestick and sharps injuries and factors associated among health care workers in a Malaysian hospital. European Journal of Social Sciences. 2010;13(3):354–362. [Google Scholar]
- 61.Lee L. K., Hassim I. N. Implication of the prevalence of needlestick injuries in a general hospital in Malaysia and its risk in clinical practice. Environmental health and preventive medicine. 2005;10(1):33–41. doi: 10.1265/ehpm.10.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nagandla K., Kumar K., Bhardwaj A., et al. Prevalence of needle stick injuries and their underreporting among healthcare workers in the department of obstetrics and gynaecology. International Archives of Medicine. 2015;8 doi: 10.3823/1780. [DOI] [Google Scholar]
- 63.Jacob A., Newson-Smith M., Murphy E., Steiner M., Dick F. Sharps injuries among health care workers in the United Arab Emirates. Occupational medicine. 2010;60(5):395–397. doi: 10.1093/occmed/kqq039. [DOI] [PubMed] [Google Scholar]
- 64.Aderaw Z. Assessment on the magnitude of needle stick and sharp injuries and associated factors among health care workers in East Gojjam Zone Health Institutions, Amahara Regional State, Ethiopia. Global journal of medical research. 2013;13(3):41–49. [Google Scholar]
- 65.Voide C., Darling K. E., Kenfak-Foguena A., Erard V., Cavassini M., Lazor-Blanchet C. Underreporting of needlestick and sharps injuries among healthcare workers in a Swiss University Hospital. Swiss medical weekly. 2012;142(w13523):1–7. doi: 10.4414/smw.2012.13523. [DOI] [PubMed] [Google Scholar]
- 66.Abebe A. M., Kassaw M. W., Shewangashaw N. E. Prevalence of needle-stick and sharp object injuries and its associated factors among staff nurses in Dessie referral hospital Amhara region, Ethiopia, 2018. BMC research notes. 2018;11(1):1–6. doi: 10.1186/s13104-018-3930-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Halwani M. A., Khyat I. I., Sallam T. A. Needle pricks among health care workers in a tertiary care general hospital, Saudi Arabia: a nine-year survey. Dent Stud. 2015;1:p. 9. [Google Scholar]
- 68.Hanafi M., Mohamed A., Kassem M., Shawki M. Needlestick injuries among health care workers of University of Alexandria Hospitals. Eastern Mediterranean Health Journal. 2011;17(1):26–35. doi: 10.26719/2011.17.1.26. [DOI] [PubMed] [Google Scholar]
- 69.Musa S., Peek-Asa C., Young T., Jovanovic N. Needle stick injuries, sharp injuries and other occupational exposures to blood and body fluids among health care workers in a general hospital in Sarajevo, Bosnia and Herzegovina. International journal of occupational safety and health. 2015;4(1):31–37. doi: 10.3126/ijosh.v4i1.9847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tesafa Bamlie J. B. Needle Stick and sharp injuries and associated factors among nurses working in Jimma University Specialized Hospital, South West Ethiopia. The Journal of Nursing Care. 2015;4(5) doi: 10.4172/2167-1168.1000291. [DOI] [Google Scholar]
- 71.Aslam M., Taj T., Ali A., et al. Needle stick injuries among health care workers of public sector tertiary care hospitals of Karachi. Journal of the College of Physicians and Surgeons Pakistan. 2010;20(3):150–153. [PubMed] [Google Scholar]
- 72.Adejumo P. O., Olatunji B. T. Exposure to work-related sharp injuries among nurses in Nigeria. Journal of Nursing Education and Practice. 2013;4(1) doi: 10.5430/jnep.v4n1p229. [DOI] [Google Scholar]
- 73.Alam M. Knowledge, attitude, and practices among health care workers on needle-stick injuries. Annals of Saudi Medicine. 2002;22(5-6):396–399. doi: 10.5144/0256-4947.2002.396. [DOI] [PubMed] [Google Scholar]
- 74.Feleke B. E. Prevalence and determinant factors for sharp injuries among Addis Ababa hospitals health professionals. Science Journal of Public Health. 2013;1(5, article 2510136):189–193. doi: 10.11648/j.sjph.20130105.11. [DOI] [Google Scholar]
- 75.Sharew N. T., Mulu G. B., Habtewold T. D., Gizachew K. D. Occupational exposure to sharps injury among healthcare providers in Ethiopia regional hospitals. Annals of occupational and environmental medicine. 2017;29(1) doi: 10.1186/s40557-017-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Honda M., Chompikul J., Rattanapan C., Wood G., Klungboonkrong S. Sharps injuries among nurses in a Thai regional hospital: prevalence and risk factors. International Journal of Occupational and Environmental Medicine. 2011;2(4) [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data about this study are contained and presented in this document.


