Abstract
Aim
The aim of the study was to determine levels of depression, anxiety, and stress symptoms and factors associated with psychological burden amongst critical care healthcare workers in the early stages of the coronavirus disease 2019 pandemic.
Methods
An anonymous Web-based survey distributed in April 2020. All healthcare workers employed in a critical care setting were eligible to participate. Invitations to the survey were distributed through Australian and New Zealand critical care societies and social media platforms. The primary outcome was the proportion of healthcare workers who reported moderate to extremely severe scores on the Depression, Anxiety, and Stress Scale-21 (DASS-21).
Results
Of the 3770 complete responses, 3039 (80.6%) were from Australia. A total of 2871 respondents (76.2%) were women; the median age was 41 years. Nurses made up 2269 (60.2%) of respondents, with most (2029 [53.8%]) working in intensive care units. Overall, 813 (21.6%) respondents reported moderate to extremely severe depression, 1078 (28.6%) reported moderate to extremely severe anxiety, and 1057 (28.0%) reported moderate to extremely severe stress scores. Mean ± standard deviation values of DASS-21 depression, anxiety, and stress scores amongst woman vs men was as follows: 8.0 ± 8.2 vs 7.1 ± 8.2 (p = 0.003), 7.2 ± 7.5 vs 5.0 ± 6.7 (p < 0.001), and 14.4 ± 9.6 vs 12.5 ± 9.4 (p < 0.001), respectively. After adjusting for significant confounders, clinical concerns associated with higher DASS-21 scores included not being clinically prepared (β = 4.2, p < 0.001), an inadequate workforce (β = 2.4, p = 0.001), having to triage patients owing to lack of beds and/or equipment (β = 2.6, p = 0.001), virus transmission to friends and family (β = 2.1, p = 0.009), contracting coronavirus disease 2019 (β = 2.8, p = 0.011), being responsible for other staff members (β = 3.1, p < 0.001), and being asked to work in an area that was not in the respondents' expertise (β = 5.7, p < 0.001).
Conclusion
In this survey of critical care healthcare workers, between 22 and 29% of respondents reported moderate to extremely severe depression, anxiety, and stress symptoms, with women reporting higher scores than men. Although female gender appears to play a role, modifiable factors also contribute to psychological burden and should be studied further.
Keywords: Critical care, Wellbeing, DASS-21, COVID-19, Depression, Anxiety, Stress
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2, emerged in Wuhan, China, late in 2019 and rapidly spread globally, currently with more than 100 million confirmed infections and more than two million deaths (as of January 27, 2021).1 Healthcare workers (HCWs) responding to pandemics serve the needs of the community and place themselves at risk of physical and psychological harm.[2], [3], [4] They are directly and indirectly exposed to death, grief, injury, loss, significant stressors, lack of appropriate equipment, difficult ethical decisions, moral injury, long hours, physical hardship, extended separation from family and friends, and the risk of becoming infected themselves.2 The previously reported emotional impacts of pandemics (Middle Eastern Respiratory Syndrome [MERS], severe acute respiratory syndrome [SARS], H1N1 influenza) can be significant and include feelings of fear, stigmatisation, isolation, and post-traumatic stress symptoms[5], [6], [7], [8], [9], [10] which have been reported to impact HCWs out to 2 years.11
There is limited information about how to best ameliorate these emotional impacts and support the wellbeing of staff during a pandemic as most research occurs after the event. It has been suggested that the emotional response of HCWs can be influenced by the level of exposure, perceived social support, level of supervision in the disaster, and individual factors such as personal coping style, underlying psychopathology, and socio-economic factors.[12], [13], [14] Implementing structured wellbeing programs before, during, and after a disaster can reduce negative psychological reactions and promote growth, mastery, and self-efficacy after the experience.[15], [16], [17]
To inform guidelines for structured psychological and wellbeing supports for frontline critical care HCWs, we aimed to measure the psychological burden in the early stages of the COVID-19 pandemic using the Depression, Anxiety, and Stress Scale-21 (DASS-21) and understand the factors that are associated with higher and lower scores.
2. Methods
2.1. Study design and participants
The survey was approved as a quality assurance project and exempt from full review by Human Research Ethics Committee, Children's Health Queensland, Australia. An invitation to complete an online survey was distributed via five Australian and New Zealand critical care networks, social media, and investigator contacts with a request to forward to their respective networks. The online survey using SurveyMonkey (SurveyMonkey Inc., San Mateo, California) was open for 1 month (April 1−30, 2020). We did not capture a denominator as a snowball distribution method was used. The survey was aimed at all HCWs in critical care settings including medical, nursing, and allied health staff. This included educators, researchers, and students redeployed to work outside their normal clinical areas such as in emergency departments, intensive care, high-dependency units, anaesthetic departments, and operating theatres. Completion of the survey was voluntary and considered implied consent from the respondents. All data collected were anonymous.
2.2. Pandemic incidence during the survey
During the survey period, the global incidence of confirmed cases of COVID-19 increased from just more than 930,000 on the 1st of April 2020 to more than 3.25 million by the 30th of April 2020. The highest burden globally was in China, Italy, the United Kingdom (UK), and the United States of America. At the time of the survey, Australia's case numbers increased from 4862 to 6766, China's case numbers increased from 82,361 to 83,596, Italy's case numbers increased from 110,574 to 205,463, the UK's case numbers increased from 29,865 to 172,481, and the United States of America's case numbers increased from 214,194 to 1.073 million between the 1st and 30th of April 2020.1
2.3. Outcomes and data collected
The primary outcome was the proportion of critical care HCWs who reported moderate to extremely severe symptom scores on the DASS-21. Secondary outcomes were to determine the factors associated with increased or reduced DASS-21 scores. Both primary and secondary outcomes were analysed by gender to understand if any gendered impacts of the COVID-19 pandemic exist.18
The DASS-21 is an abbreviated version of the empirically developed DASS.19 It was chosen for its validity for use on multiple populations.20 This validated instrument comprises three subsections of seven questions that evaluate states of depression, anxiety, and stress with an individual scale range of 0–21 and a total score range of 0–63. Respondents were asked to read each statement and rate on a scale of 0 to 3 the degree to which the statements applied to themselves over the past week, with 0 meaning did not apply, 1 meaning applied some degree or some of the time, 2 meaning applied a considerable degree or good part of the time, and 3 meaning applied very much or most of the time. These constructs are interrelated, and the combined score can be used to screen for general psychological distress.19 , 20
For the purposes of this survey, the respondents were self-reporting the degree to which the statements applied to them during the past week. The resultant score within each subsection highlights the severity of symptoms the respondent had at the time of the survey. The DASS-21 was not being used as a diagnostic tool for depression, anxiety, and/or stress, and the reported levels within this article refer to symptom severity.
A 13-item pandemic specific questionnaire was developed by the multidisciplinary authors, with an understanding of possible concerns and wellbeing of potential respondents (Survey provided in eSupp). These items included the phase of the pandemic, prior disaster preparedness training, the main source of COVID-19 information, how much information on COVID-19 was being received, support in the workplace, main concerns about caring for patients with COVID-19, if they were expected to perform duties outside of their usual scope of practice, essential training requirement, impact on sleep, personal growth, and commitment to working during a pandemic. Demographic items (gender, age, living arrangements, highest education level), country, workplace (area of work, role), employment status (full-time, part-time, or casual), years of clinical and critical care experience, and hospital type were also collected. One open-ended question was asked regarding what could assist the respondent's wellbeing. Owing to the numbers responding and the richness and depth of comments, these data will be reported in a separate article.
2.4. Statistical analysis
Means ± standard deviations (SDs) were reported for continuous data, and numbers and proportions were reported for categorical data. DASS-21 scores were doubled for analysis for comparability with the full DASS scores, according to the developer's recommendations.20 Scores were categorised for each metric as follows: (i) for depression: normal, scores 0–9; mild, 10–13; moderate, 14–20; severe, 21–27; and extremely severe, 28 and above; (ii) for anxiety: normal, 0–7; mild, 8–9; moderate, 10–14; severe, 15–19; and extremely severe, 20 and above; and (iii) for stress: normal, 0–14; mild, 15–18; moderate, 19–25; severe, 26–3; and extremely severe, 34 and above. The results were further dichotomised into normal/mild or moderate to extremely severe. The DASS-21 was reported as a mean ± SD score and numbers and proportions for all respondents and by gender. DASS-21 scores were also matched to Australian population norms by age and gender using the means described by Crawford et al.21 to determine individual percentile ranks (interquartile range [IQR]) within the general population.
The reliability of the three scales was assessed by examination of internal consistency (Cronbach's alpha coefficient). A value of 0.75 or higher was considered indicative of good reliability.22
To estimate the relative association between respondent and workplace characteristics and the DASS-21 score, univariate linear regression was performed and presented as a beta (β) coefficient with 95% confidence intervals (presented in the figures). These factors included gender, age, home arrangement, level of education, area of practice in the hospital (emergency, intensive care, operating theatre, or other), professional role (nursing, medical, allied health, or other), provision of care to adults and/or paediatrics, clinical experience, critical care experience, rurality of practice, current COVID status, prior disaster preparedness training, amount of information received, and amount of support received (etable 2). Characteristics associated with the DASS-21 with a p-value <0.2 were entered into a predictive multivariable linear regression model using forward and backward elimination to achieve the optimal Akaike information criterion. The final characteristics were evaluated with the respondents' concerns to determine the impact of each concern on psychological outcomes.
All statistical analyses were conducted using R (version 4.0.2; R Foundation for Statistical Computing, Vienna, Austria). Two-tailed P values <0.01 were deemed significant.
3. Results
Over the month of April 2020, a total of 3992 responses were received. Of these, 222 did not complete the survey and were excluded from the analysis. (etable 1 reports respondent characteristics by completions vs noncompletions.) Table 1 outlines all respondent demographics and clinical information. Of the 3770 completed surveys, 80.6% (3039) were from Australia. Most had a graduate diploma and/or certificate (1277 [33.9%]) and bachelor's degree (1232 [32.7%]). The majority were women (2871 [76.2%]), the median (IQR) age was 41 (33–50) years, 1814 (48.1%) particpants lived at home with a partner and children/dependants, and 1373 (36.4%) particpants lived with a partner and/or housemates. Nurses accounted for 2269 (60.2%) of the respondents. Most respondents treated adult patients (2479 [67.3%]) in tertiary hospitals (2148 [57.7%]), in intensive care units (2029 [53.8%]), and in emergency departments (1104 [29.6%]).
Table 1.
Clinical demographics of the respondents.
| Demographics | All (N = 3770) | Women (N = 2871) | Men (N = 846) |
|---|---|---|---|
| Country | |||
| Australia | 3039 (81) | 2438 (85) | 582 (69) |
| New Zealand | 270 (7) | 217 (8) | 50 (6) |
| Europe | 195 (5) | 109 (4) | 85 (10) |
| North America | 172 (5) | 80 (3) | 90 (11) |
| Asia/South America/Africa/Middle East | 55 (1) | 19 (1) | 36 (4) |
| Gender | |||
| Female | 2871 (77) | 2871 (100) | 0 (0) |
| Male | 846 (23) | 0 (0) | 846 (100) |
| Not specified | 12 (0) | 0 (0) | 0 (0) |
| Age (median, interquartile range) | 41 (33–50) | 40 (33–50) | 43 (35–51) |
| 20–29 years | 558 (15) | 476 (17) | 78 (9) |
| 30–39 years | 1173 (31) | 924 (32) | 243 (29) |
| 40–49 years | 1114 (30) | 799 (28) | 307 (36) |
| 50–59 years | 688 (18) | 520 (18) | 165 (20) |
| 60–65 years | 171 (5) | 129 (4) | 38 (4) |
| >65 years | 36 (1) | 22 (1) | 14 (2) |
| Home arrangement | |||
| Sole occupant | 485 (13) | 399 (14) | 84 (10) |
| With partner/housemate | 1373 (37) | 1093 (38) | 272 (32) |
| With partner and/or children | 1814 (49) | 1326 (46) | 477 (57) |
| Other | 60 (2) | 50 (2) | 10 (1) |
| Highest level of education | |||
| Graduate diploma/certificate | 1277 (34) | 1082 (38) | 186 (22) |
| Bachelor's degree | 1232 (33) | 968 (34) | 255 (30) |
| Master's degree | 771 (21) | 568 (20) | 201 (24) |
| Doctorate/PhD | 321 (9) | 153 (5) | 167 (20) |
| Other | 129 (3) | 93 (3) | 36 (4) |
| Area of practice | |||
| Adult | 2479 (67) | 1901 (67) | 564 (68) |
| Adult and paediatric/neonate | 805 (22) | 596 (21) | 204 (24) |
| Paediatric/neonate | 394 (11) | 328 (12) | 64 (8) |
| Nonclinical | 8 (0) | 5 (0) | 3 (0) |
| Location of practice | |||
| Emergency | 1104 (30) | 817 (29) | 280 (33) |
| Intensive care/HDU | 2029 (54) | 1580 (55) | 438 (52) |
| Anaesthetic departments/operating theatres | 256 (7) | 187 (7) | 69 (8) |
| Hospital ward | 130 (3) | 116 (4) | 13 (2) |
| Cardiac catheterisation laboratory | 48 (1) | 42 (1) | 6 (1) |
| Outpatient/GP/community | 46 (1) | 37 (1) | 9 (1) |
| Prehospital | 23 (1) | 12 (0) | 10 (1) |
| Other | 91 (2) | 72 (3) | 18 (2) |
| Nurse | |||
| Nurse practitioner/consultant | 131 (4) | 105 (4) | 26 (3) |
| Clinical registered nurse | 1802 (48) | 1598 (56) | 192 (23) |
| Clinical enrolled nurse | 32 (1) | 31 (1) | 1 (0) |
| Nurse (other) | 304 (8) | 276 (10) | 28 (3) |
| Doctor | |||
| Consultant | 763 (20) | 367 (13) | 392 (47) |
| Fellow/registrar | 266 (7) | 164 (6) | 100 (12) |
| Resident/student | 59 (2) | 31 (1) | 28 (3) |
| Allied health | 208 (6) | 176 (6) | 31 (4) |
| Other | 159 (4) | 113 (4) | 44 (5) |
| Employment status | |||
| Full-time | 2187 (59) | 1485 (52) | 689 (82) |
| Part-time | 1437 (39) | 1292 (45) | 139 (16) |
| Casual | 98 (3) | 81 (3) | 16 (2) |
| Clinical experience | |||
| <1 year | 50 (1) | 37 (1) | 13 (2) |
| 1–2 years | 123 (3) | 104 (4) | 17 (2) |
| 3–5 years | 425 (11) | 340 (12) | 83 (10) |
| 6–10 years | 784 (21) | 621 (22) | 159 (19) |
| 11–15 years | 675 (18) | 516 (18) | 156 (18) |
| 16–20 years | 477 (13) | 339 (12) | 137 (16) |
| >20 years | 1192 (32) | 902 (32) | 280 (33) |
| Critical care experience | |||
| Nil | 182 (5) | 141 (5) | 40 (5) |
| <1 year | 216 (6) | 166 (6) | 49 (6) |
| 1–2 years | 336 (9) | 268 (9) | 66 (8) |
| 3–5 years | 571 (15) | 454 (16) | 114 (14) |
| 6–10 years | 763 (20) | 596 (21) | 163 (19) |
| 11–15 years | 621 (17) | 458 (16) | 159 (19) |
| 16–20 years | 382 (10) | 282 (10) | 99 (12) |
| >20 years | 652 (18) | 495 (17) | 153 (18) |
| Hospital site | |||
| Tertiary | 2148 (58) | 1652 (58) | 486 (58) |
| Metropolitan | 774 (21) | 567 (20) | 202 (24) |
| Rural | 348 (9) | 273 (10) | 72 (9) |
| Private | 270 (7) | 227 (8) | 41 (5) |
| Other | 185 (5) | 141 (5) | 42 (5) |
Data are presented as n (%) or median (interquartile range).
HDU, high-dependency unit; GP, General Practice.
Responses specific to COVID-19 are shown in Table 2 . Most respondents were identified as being in the prephase or early phase of the COVID-19 pandemic (3435 [91.1%]). The primary source of COVID-19 information was from local health management (1017 [28.4%]), health authorities (863 [24.1%]), and social media/websites (812 [22.6%]), with 1205 (33.6%) respondents reporting that the amount of information received was comprehensive and 1149 (32.1%) reporting that it was too much. The most common primary concern for respondents was virus transmission to family (1060 [29.6%]). Despite this concern, the respondents were strongly committed to working in the hospital during the pandemic (3137 [83.0%]) and strongly agreed they could grow professionally and personally as a result of the COVID-19 pandemic (2663 [70.6%]).
Table 2.
COVID-19 specific responses.
| All (N = 3770) | Women (N = 2871) | Men (N = 847) | |
|---|---|---|---|
| Current COVID status | |||
| Pre (no COVID-19 patients) | 614 (17) | 499 (18) | 111 (14) |
| Early phase (some/handful of COVID-19 patients) | 2821 (79) | 2172 (79) | 633 (78) |
| Peak (overwhelmed/large numbers of COVID-19 patients) | 79 (2) | 45 (2) | 34 (4) |
| Post (reducing burden of COVID-19 patients) | 71 (2) | 39 (1) | 31 (4) |
| Prior disaster preparedness training | |||
| Yes | 1652 (46) | 1203 (44) | 439 (54) |
| No | 1934 (54) | 1554 (56) | 370 (46) |
| Primary source of information | |||
| Health authorities | 863 (24) | 702 (25) | 157 (19) |
| Local hospital management | 1017 (28) | 868 (31) | 143 (18) |
| Medical literature | 398 (11) | 215 (8) | 181 (22) |
| Traditional media | 395 (11) | 305 (11) | 88 (11) |
| Social media/websites | 812 (23) | 584 (21) | 223 (28) |
| Other | 102 (3) | 82 (3) | 18 (2) |
| Amount of information received | |||
| None | 3 (0) | 2 (0) | 1 (0) |
| Too little | 242 (7) | 196 (7) | 44 (5) |
| Adequate | 985 (27) | 777 (28) | 201 (25) |
| Comprehensive | 1205 (34) | 950 (34) | 248 (31) |
| Too much | 1149 (32) | 829 (30) | 316 (39) |
| Support received | |||
| Not at all | 139 (4) | 109 (4) | 28 (3) |
| Not really | 723 (20) | 563 (20) | 157 (19) |
| Adequate | 1598 (45) | 1204 (44) | 386 (48) |
| More than adequate | 638 (18) | 489 (18) | 143 (18) |
| Very well | 486 (14) | 389 (14) | 95 (12) |
| Primary concern | |||
| Transmission to friends/family/children | 1060 (30) | 850 (31) | 203 (25) |
| Adequate/appropriate PPE | 751 (21) | 552 (20) | 196 (24) |
| Contracting COVID-19 | 430 (12) | 340 (12) | 86 (11) |
| Responsibility for staff | 245 (7) | 191 (7) | 54 (7) |
| Inadequate workforce | 225 (6) | 160 (6) | 64 (8) |
| Scarce resources | 191 (5) | 132 (5) | 57 (7) |
| Not clinically prepared | 165 (5) | 140 (5) | 24 (3) |
| Patient triage due to lack of beds and/or equipment | 148 (4) | 105 (4) | 42 (5) |
| Being asked to work in an area that is not my expertise | 84 (2) | 75 (3) | 9 (1) |
| Being required to self-isolate | 78 (2) | 55 (2) | 23 (3) |
| Other | 207 (6) | 154 (6) | 51 (6) |
| Secondary concerna | |||
| Contracting COVID-19 | 1648 (43.7) | 1264 (44.0) | 372 (44.0) |
| Adequate/appropriate PPE | 1789 (47.5) | 1372 (47.8) | 407 (48.1) |
| Transmission to friends/family/children | 1784 (47.3) | 1385 (48.2) | 392 (46.3) |
| Inadequate workforce | 1270 (33.7) | 961 (33.5) | 303 (35.8) |
| Scarce resources | 1241 (32.9) | 920 (32.0) | 315 (37.2) |
| Responsibility for staff | 1097 (29.1) | 831 (28.9) | 259 (30.6) |
| Patient triage due to lack of beds and/or equipment | 906 (24.0) | 666 (23.2) | 235 (27.8) |
| Being required to self-isolate | 809 (21.5) | 597 (20.8) | 205 (24.2) |
| Not clinically prepared | 656 (17.4) | 536 (18.7) | 118 (13.9) |
| Being asked to work in an area that is not my expertise | 456 (12.1) | 391 (13.6) | 62 (7.3) |
| Are you required to work outside your usual practicea | |||
| No | 1992 (52.8) | 1494 (52.0) | 485 (57.3) |
| Yes, scope of practice different, e.g., manage ventilated patients? | 343 (9.1) | 262 (9.1) | 80 (9.5) |
| Yes, requirement to manage a higher ratio of patients? | 675 (17.9) | 527 (18.4) | 144 (17.0) |
| Yes, supervise non-ICU staff redeployed to the ICU? | 763 (20.2) | 602 (21.0) | 157 (18.6) |
| Yes, take on a different role in the ICU? | 366 (9.7) | 272 (9.5) | 93 (11.0) |
| Essential training requireda | |||
| Donning/doffing PPE | 3432 (91.0) | 2644 (92.1) | 768 (90.8) |
| Simulated rehearsal | 3024 (80.2) | 2364 (82.3) | 644 (76.1) |
| Coping strategies and well-being | 2931 (77.7) | 2306 (80.3) | 608 (71.9) |
| ICU bed and staff surge plan | 2897 (76.8) | 2232 (77.7) | 648 (76.6) |
| Hospital disaster plan | 2852 (75.6) | 2230 (77.7) | 606 (71.6) |
| Managing the patients’ and families’ expectations | 2554 (67.7) | 2022 (70.4) | 515 (60.9) |
| Managing home/family obligations | 2467 (65.4) | 1928 (67.2) | 522 (61.7) |
| Triage | 2444 (64.8) | 1889 (65.8) | 539 (63.7) |
| Clinical supervision | 2350 (62.3) | 1845 (64.3) | 489 (57.8) |
| My sleep has been negatively impacted during COVID-19 | |||
| Strongly agree | 536 (15) | 409 (15) | 125 (15) |
| Agree | 1367 (38) | 1097 (40) | 260 (32) |
| Neutral | 783 (22) | 613 (22) | 165 (20) |
| Disagree | 595 (17) | 434 (16) | 157 (19) |
| Strongly disagree | 299 (8) | 197 (7) | 102 (13) |
| I am committed to work in the hospital during COVID-19 | |||
| Strongly agree | 1778 (50) | 1306 (47) | 464 (57) |
| Agree | 1352 (38) | 1078 (39) | 264 (33) |
| Neutral | 286 (8) | 242 (9) | 44 (5) |
| Disagree | 77 (2) | 60 (2) | 16 (2) |
| Strongly disagree | 91 (3) | 69 (3) | 20 (2) |
| I can grow personally and professional as a result of COVID-19 | |||
| Strongly agree | 1034 (29) | 764 (28) | 265 (33) |
| Agree | 1628 (45) | 1278 (46) | 339 (42) |
| Neutral | 679 (19) | 529 (19) | 145 (18) |
| Disagree | 152 (4) | 120 (4) | 31 (4) |
| Strongly disagree | 89 (2) | 61 (2) | 28 (3) |
COVID-19, coronavirus disease 2019; ICU, intensive care unit; PPE, personal protective equipment.
Multichoice selection allowed.
3.1. Depression, anxiety, and stress
The DASS-21 subscales had high internal consistency, with Cronbach's alpha for depression, anxiety, and stress subscales to be 0.88, 0.89, and 0.90, respectively.
Overall, the mean of each subscale was within the normal range (Table 3 ). Prevalence of any severity of symptoms of depression, anxiety, and stress in the sample was 33.0% (1244/3770), 36.6% (1380/3770), and 41.2% (1552/3770), respectively. The number of respondents reporting moderate to extremely severe depression symptoms was 813 (21.6%), 1078 (28.6%) reported moderate to extremely severe anxiety, and 1057 (28.0%) reported moderate to extremely severe stress. Mean ± SD values of DASS-21 depression, anxiety, and stress scores amongst women vs men were 8.0 ± 8.2 vs 7.1 ± 8.2 (p = 0.003), 7.2 ± 7.5 vs 5.0 ± 6.7 (p < 0.001), and 14.4 ± 9.6 vs 12.5 ± 9.4 (p < 0.001), respectively (Table 3).
Table 3.
Levels of depression, anxiety, and stress amongst all respondents, based on the DASS-21.
| DASS level | All (N = 3770) | Women (N = 2871) | Men (N = 846) | P-value (M vs F) |
|---|---|---|---|---|
| Depression, n (%) | ||||
| Normal | 2526 (67) | 1890 (66) | 607 (72) | |
| Mild | 431 (11) | 355 (12) | 75 (9) | |
| Moderate | 504 (13) | 383 (13) | 108 (13) | |
| Severe | 157 (4) | 129 (4) | 24 (3) | |
| Extremely severe | 152 (4) | 114 (4) | 32 (4) | |
| Mean (± SD) score | 7.8 ± 8.3 | 8.0 ± 8.2 | 7.1 ± 8.2 | 0.003 |
| Anxiety, n (%) | ||||
| Normal | 2390 (63) | 1737 (61) | 624 (74) | |
| Mild | 302 (8) | 248 (9) | 53 (6) | |
| Moderate | 577 (15) | 466 (16) | 101 (12) | |
| Severe | 203 (5) | 179 (6) | 23 (3) | |
| Extremely severe | 298 (8) | 241 (8) | 45 (5) | |
| Mean (± SD) score | 6.8 ± 7.5 | 7.2 ± 7.5 | 5.0 ± 6.7 | <0.001 |
| Stress n (%) | ||||
| Normal | 2218 (59) | 1633 (57) | 555 (66) | |
| Mild | 495 (13) | 398 (14) | 90 (11) | |
| Moderate | 507 (13) | 388 (14) | 110 (13) | |
| Severe | 387 (10) | 318 (11) | 65 (8) | |
| Extremely severe | 163 (4) | 134 (5) | 26 (3) | |
| Mean (± SD) score | 14.0 ± 9.6 | 14.4 ± 9.6 | 12.5 ± 9.4 | <0.001 |
| DASS-21 total mean (± SD) score | 28.6 ± 22.6 | 29.7 ± 22.5 | 24.5 ± 21.4 | <0.001 |
SD, standard deviation; DASS-21, Depression, Anxiety, and Stress Scale-21.
For the age- and gender-matched Australian population percentile analysis, the depression median percentile rank was 74 (IQR = 55–89), the median anxiety percentile rank was 75 (IQR = 53–92), and the median stress percentile rank was 76 (IQR = 54–91). Overall reported psychological symptoms of distress amongst respondents revealed a percentile rank of 78 (IQR = 60–92), suggesting that more than half of all respondents had similar psychological distress as the top (i.e., worst) quartile of the Australian population.
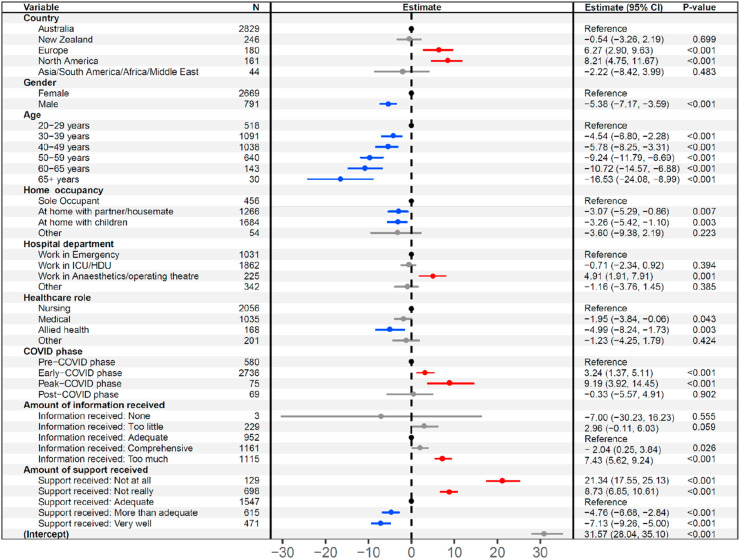
Factors that were associated with reduced DASS-21 scores and symptoms of distress on multivariable regression included male gender (β = −5.4, p < 0.001), older age (>65 years, β = −16.5, p < 0.001) compared with younger age (20–29 years), living at home with children (β = −3.3, p = 0.003) compared with living alone, and being an allied health professional (β = −5.0, p = 0.003) (Fig. 1 ).
Fig. 1.
Factors associated with lower or higher DASS-21 scores. Blue represents factors that significantly reduced DASS-21 scores, whereas red represents factors that significantly increased DASS-21 scores. Grey represents factors that did not achieve statistical significance. Estimate represents change in the DASS-21 score. Significance is established at p < 0.01. CI, confidence interval; HDU, high-dependency unit; ICU, intensive care unit; DASS-21, Depression, Anxiety, and Stress Scale-21; COVID, coronavirus disease.
Factors that increased DASS-21 scores included living in Europe or North America compared with Australia (β = 6.3, p < 0.001; β = 8.2, p < 0.001, respectively), working in anaesthetic departments/operating theatres (β = 4.9; p = 0.001), being in the early phase (β = 3.24, p = 0.001) or peak of the pandemic (β = 9.2, p = 0.001), receiving too much information (β = 7.4, p < 0.001) compared with an adequate level, and not feeling well supported in the work environment (β = 21.3, p < 0.001) compared with adequate support (Fig. 1).
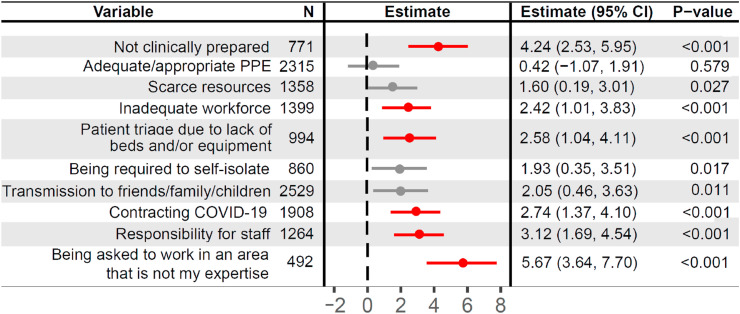
After adjusting for significant confounders, the clinical concerns associated with higher DASS-21 scores included not being clinically prepared (β = 4.2, p < 0.001), an inadequate workforce (β = 2.4; p < 0.001), having to triage patients owing to lack of beds and/or equipment (β = 2.6, p < 0.001), contracting COVID-19 (β = 2.7, p < 0.001), being responsible for other staff members (β = 3.1, p < 0.001), and being asked to work in an area that was not in the respondents' expertise (β = 5.7, p < 0.001) (Fig. 2 ).
Fig. 2.
Clinical concerns and association with the DASS-21 score. Clinical concerns adjusted for country, age, gender, home arrangement, location of practice, professional role, COVID status, amount of information, and support received. Red represents factors that significantly increased DASS-21 scores. Grey represents factors that did not achieve statistical significance. Estimate represents change in the DASS-score. Significance is established at p < 0.01. CI, confidence interval; N, number of respondents; DASS-21, Depression, Anxiety, and Stress Scale-21; COVID, coronavirus disease.
4. Discussion
4.1. Statement of principle findings
This survey of critically care HCWs in the early phases of the COVID-19 pandemic found that between one-fifth and one-third of respondents reported moderate to extremely severe depression, anxiety, and stress symptoms, with higher mean scores reported for women than for men. Modifiable factors associated with higher DASS-21 scores including receiving too much information and not feeling well supported in the work environment. The primary concerns for respondents were work related (not being clinically prepared, having to triage patients and equipment, being responsible for other staff members, working outside their area of expertise) and virus related (being infected by the virus and the risk of transmitting the infection to family and friends).
4.2. Comparison with other studies
In this study, one-fifth to one-third of the respondents reported moderate to extremely severe symptom levels of depression, anxiety, and stress. In a recent study of HCWs working in three provinces of China during the acute outbreak of COVID-19, 14.8% and 12.3% of respondents reported moderate to severe depression and anxiety, respectively.23 Our reported numbers for moderate to severe anxiety and depression are higher (21.6% and 28.6%, respectively). This could possibly be related to the different validated instruments used to assess anxiety and depression, cultural differences, or to the type of HCW, given our sample was critical care health professionals as opposed to HCWs working in other departments. The difference could also be attributed to this survey being conducted in April and receiving mostly Australian respondents, whereas the survey was performed in Wuhan, China, the location of the source of COVID-19, and two other Chinese provinces and was conducted in January/February. It is possible the high proportion of respondents experiencing moderate to severe physiological symptoms seen in our sample was related to anticipatory anxiety resulting from media reports, societal lockdown, reported rates of death in the public and in HCWs globally, and the speed of the spread of COVID-19 from China to other countries. The reports of overwhelmed healthcare systems, particularly intensive care units, may explain the higher levels of depression, anxiety, and stress symptoms reported in our survey than in the study conducted in China.
Lai et al.23 also reported more adverse psychological symptoms in women than in men, and this finding concurs with our study findings. Reports from the UK24 and Australia25 identify that women have a higher prevalence of diagnosed mental illness than men. Our findings may be related to general population prevalence of psychological symptoms or report that women are more likely to self-report psychological problems than men. Interventions to support HCWs need to address these gender differences to ensure that all HCWs are adequately supported.
More than half of the women responding to our survey were nurses (n = 2269; 60.2%). In a survey of psychosocial effects of the 2003 SARS outbreak in hospital staff in Toronto, the authors found that being a nurse was significantly associated with emotional distress.26 Similarly, in a study on HCWs working in an emergency department in Hong Kong during the SARS outbreak, nurses scored higher for psychological distress than other healthcare professionals.27 These findings may not be isolated to working during pandemics. A small study (n = 102) of Australian nurses working across multiple areas measured depression, anxiety, and stress using the DASS-42, with similar scores seen in our study.28 Nonetheless, the findings in our cohort are still important as nurses consistently reported higher DASS-21 scores. Concerns related to not being clinically prepared, working outside of one's area of expertise, and being responsible for other staff members were major components of pandemic surge planning.29 , 30 Nurses comprise the majority of the healthcare workforce, particularly during the management of pandemics. Managers and administrators should be cognisant that the decisions to redeploy HCWs to new areas, be responsible for junior or inexperienced staff members, or be expected to work out of their trained scope of practice may have major psychological impacts. Strategies, such as those outlined in COVID-19 guidelines,29 , 30 should be instigated to ensure HCWs are optimally prepared and supported to mitigate potential negative impacts.
4.3. Limitations
The key limitation of this survey was the convenience sampling method and uncontrolled distribution strategy; therefore, a denominator could not be captured to provide a response rate, and generalisability is limited. The rationale for using snowball sampling was to distribute the survey to as many frontline critical care workers as possible and be able to report results in a timely fashion to enable institutions and guideline developers to use the results to assist in recommendations and interventions for critical care HCWs. We recognise that without a response rate, it is difficult to determine the representativeness of the sample to critical care HCWs. Response bias is likely to be in a survey of this nature, with those experiencing no emotional distress and similarly with those experiencing high levels of emotional distress less likely to respond. The results of higher levels of depression, anxiety, and stress may not be unexpected, given the unique global situation and the impact and exposure of media coverage of this pandemic. The methods used in this study are also a potential limitation in that we have only captured a snapshot of each respondent's experience. Repeated surveys and longitudinal and qualitative studies would enable a complete understanding of the long-term impact of the COVID-19 pandemic on critical care HCWs. The pandemic-specific questions were not tested for content validity, but the multidisciplinary authors were able to draw on their current experiences, strengthening the appropriateness of the questions. The strengths of this study include the large number of responses from the critical care community, which has enabled useful analysis and insights into the concerns, preparedness, and wellbeing of critical care HCWs globally. We used a valid and reliable instrument to determine levels of depression, anxiety, and stress among the respondents. We also prespecified a gender-disaggregated analysis, which is considered best practice,18 and in the case of our study, we highlighted the gender-associated impacts of the early phase of the pandemic on women and men working as health professionals in critical care areas.
4.4. Future direction
Further work on the potential benefits of preparing for the pandemic and external disasters and conducting wellbeing programs for HCWs, particularly women and nurses, is important. High levels of stress has been associated with poor performance, absenteeism, and burnout, which may lead to additional strain on an already stressed healthcare system during a pandemic.29 , 30 Managers and administrators should be cognisant of how they deliver information to HCWs and develop appropriate support and training, particularly for less experienced HCWs and those expected to work out of their usual scope of practice. Institutions should emphasise simulation and disaster preparedness training along with provision of equipment to simplify and enable HCWs to perform their work with as little addition stress as possible. Strategies to enhance resilience and work engagement may secure the longevity of HCWs and maintain and improve patient safety and outcomes.31 , 32
5. Conclusion
In this survey of critical care HCWs in the early phase of the COVID-19 pandemic, between 22% and 29% of respondents reported moderate to extremely severe depression, anxiety, and stress symptoms, with women experiencing higher scores for all three subdomains than men. Modifiable factors associated with higher DASS-21 scores included receiving too much information and not feeling well supported in the work environment. The primary concerns for the respondents were related to the working environment and risk of infection to themselves or family and friends. Although female gender appears to play a role, modifiable factors also contributed to psychological burden and should be studied further.
Funding
The research team acknowledges support of the UNSW Covid-19 Rapid Research Fund in undertaking this project.
CRediT authorship contribution statement
N.E. Hammond: Conceptualisation, survey design, completed regulatory and survey build, distributed the survey, checked data quality, analysis, interpretation, Writing - original draft, Writing - review & editing. L. Crowe: Conceptualisation, survey design, completed regulatory and survey build, distributed the survey, Writing - review & editing. B. Abbenbroek: survey design, completed regulatory and survey build, distributed the survey, checked data quality, analysis, interpretation, Writing - review & editing. R. Elliott: survey design, distributed the survey, Writing - review & editing. D.H. Tian: survey design, distributed the survey, checked data quality, analysis, interpretation, Writing - review & editing. L.H. Donaldson: survey design, distributed the survey, Writing - review & editing. E. Fitzgerald: survey design, distributed the survey, Writing - review & editing. O. Flower: survey design, distributed the survey, Writing - review & editing. S. Grattan: survey design, completed regulatory and survey build, distributed the survey, Writing - review & editing. R. Harris: survey design, distributed the survey, Writing - review & editing. L. Sayers: survey design, distributed the survey, Writing - review & editing. A. Delaney: Conceptualisation, survey design, distributed the survey, checked data quality, analysis, interpretation, Writing - review & editing.
Acknowledgements
The authors would like to thank all the respondents for taking the time to complete this survey, which has enabled insights into the critical care workforce's psychological wellbeing during the coronavirus disease 2019 pandemic.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.aucc.2020.12.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Johns Hopkins University. https://coronavirus.jhu.edu/map.html. Accessed 17th June, 2020.
- 2.Quevillon R.P., Gray B.L., Erickson S.E., Gonzalez E.D., Jacobs G.A. Helping the helpers: assisting staff and volunteer workers before, during, and after disaster relief operations. J Clin Psychol. 2016;72(12):1348–1363. doi: 10.1002/jclp.22336. [DOI] [PubMed] [Google Scholar]
- 3.Pfefferbaum B., North C.S. Mental health and the covid-19 pandemic. N Engl J Med. 2020 Aug 6;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 4.Williamson V., Murphy D., Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occup Med (Lond). 2020 Jul 17;70(5):317–319. doi: 10.1093/occmed/kqaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corley A., Hammond N.E., Fraser J.F. The experiences of health care workers employed in an Australian intensive care unit during the H1N1 Influenza pandemic of 2009: a phenomenological study. Int J Nurs Stud. 2010;47(5):577–585. doi: 10.1016/j.ijnurstu.2009.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan A.O., Huak C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond). 2004;54(3):190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sim K., Chong P.N., Chan Y.H., Soon W.S. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. J Clin Psychiatr. 2004;65(8):1120–1127. doi: 10.4088/jcp.v65n0815. [DOI] [PubMed] [Google Scholar]
- 8.Kang H.S., Son Y.D., Chae S.M., Corte C. Working experiences of nurses during the Middle East respiratory syndrome outbreak. Int J Nurs Pract. 2018;24(5) doi: 10.1111/ijn.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goulia P., Mantas C., Dimitroula D., Mantis D., Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010;10:322. doi: 10.1186/1471-2334-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Styra R., Hawryluck L., Robinson S., Kasapinovic S., Fones C., Gold W.L. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J Psychosom Res. 2008;64(2):177–183. doi: 10.1016/j.jpsychores.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Declercq F., Palmans V. Two subjective factors as moderators between critical incidents and the occurrence of post traumatic stress disorders: 'Adult attachment' and 'perception of social support'. Psychol Psychother. 2006;79:323–337. doi: 10.1348/147608305X53684. [DOI] [PubMed] [Google Scholar]
- 13.Littleton H., Horsley S., John S., Nelson D. Trauma coping strategies and psychological distress: a meta-analysis. J Trauma Stress. 2007;20:977–988. doi: 10.1002/jts.20276. [DOI] [PubMed] [Google Scholar]
- 14.Brooks S., Dunn R., Sage C., Amlôt R., Greenberg N., Rubin G. Risk and resilience factors affecting the psychological wellbeing of individuals deployed in humanitarian relief roles after a disaster. J Ment Health (Abingdon, England) 2015;24:1–29. doi: 10.3109/09638237.2015.1057334. [DOI] [PubMed] [Google Scholar]
- 15.Wise E., Hersh M., Gibson C. Ethics, self-care and well-being for psychologists: reenvisioning the stress-distress continuum. Prof Psychol Res Pract. 2012;43:487. [Google Scholar]
- 16.Measuring compassion satisfaction as well as fatigue: Developmental history of the Compassion Satisfaction and Fatigue Test [computer program] Brunner-Routledge; New York, NY, US: 2002. [Google Scholar]
- 17.Tedeschi R.G., Calhoun L.G. Lawrence Erlbaum; 2004. Target article: "posttraumatic growth: conceptual foundations and empirical evidence"; pp. 1–18. [Google Scholar]
- 18.Heidari S., Babor T.F., De Castro P., Tort S., Curno M. Sex and Gender Equity in Research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2016;1 doi: 10.1186/s41073-016-0007-6. 2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lovibond S.H., Lovibond P.F. 2nd ed. Psychology Foundation; Sydney: 1995. Manual for the depression anxiety stress scales. [Google Scholar]
- 20.Depression anxiety stress scale (DASS). http://www2.psy.unsw.edu.au/dass//. Accessed 23rd June, 2020.
- 21.Crawford J., Cayley C., Lovibond P.F., Wilson P.H., Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS) Aust Psychol. 2011;46(1):3–14. [Google Scholar]
- 22.Thorndike R.M. vol. 19. McGraw-Hill; New York: 1994. pp. 303–305. (Book review: psychometric theory (3rd ed.) by Jum Nunnally and Ira Bernstein). xxiv + 752 pp. Applied Psychological Measurement. 1995 (3) [Google Scholar]
- 23.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. e203976-e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gulland A. Women have higher rates of mental disorders than men, NHS survey finds. BMJ. 2016;354:i5320. doi: 10.1136/bmj.i5320. [DOI] [PubMed] [Google Scholar]
- 25.Australian Government: Department of Health 2020. https://www1.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-m-mhaust2-toc∼mental-pubs-m-mhaust2-hig∼mental-pubs-m-mhaust2-hig-pre
- 26.Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Can Med Assoc J. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong T.W., Yau J.K.Y., Chan C.L.W., Kwong R.S.Y., Ho S.M.Y., Lau C.C. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. 2005;12(1):13–18. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Maharaj S., Lees T., Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int J Environ Res Publ Health. 2019;16(1):61. doi: 10.3390/ijerph16010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Australian and New Zealand Intensive Care Society . ANZICS; Melbourne: 2020. ANZICS COVID-19 guidelines. [Google Scholar]
- 30.Aziz S. Managing ICU surge during the COVID-19 crisis: Rapid guidelines. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo Y.F., Luo Y.H., Lam L., Cross W., Plummer V., Zhang J.P. Burnout and its association with resilience in nurses: a cross-sectional study. J Clin Nurs. 2018;27(1–2):441–449. doi: 10.1111/jocn.13952. [DOI] [PubMed] [Google Scholar]
- 32.Galletta M., Portoghese I., D’Aloja E., Mereu A., Contu P., Coppola R.C. Relationship between job burnout, psychosocial factors and health care-associated infections in critical care units. Intensive Crit Care Nurs. 2016;34:51–58. doi: 10.1016/j.iccn.2015.11.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.