Abstract
Background
Despite investments to improve quality of emergency care for patients with acute myocardial infarction (AMI), few studies have described national, real‐world trends in AMI care in the emergency department (ED). We aimed to describe trends in the epidemiology and quality of AMI care in US EDs over a recent 11‐year period, from 2005 to 2015.
Methods and Results
We conducted an observational study of ED visits for AMI using the National Hospital Ambulatory Medical Care Survey, a nationally representative probability sample of US EDs. AMI visits were classified as ST‐segment–elevation myocardial infarction (STEMI) and non‐STEMI. Outcomes included annual incidence of AMI, median ED length of stay, ED disposition type, and ED administration of evidence‐based medications. Annual ED visits for AMI decreased from 1 493 145 in 2005 to 581 924 in 2015. Estimated yearly incidence of ED visits for STEMI decreased from 1 402 768 to 315 813. The proportion of STEMI sent for immediate, same‐hospital catheterization increased from 12% to 37%. Among patients with STEMI sent directly for catheterization, median ED length of stay decreased from 62 to 37 minutes. ED administration of antithrombotic and nonaspirin antiplatelet agents rose for STEMI (23%–31% and 10%–27%, respectively).
Conclusions
National, real‐world trends in the epidemiology of AMI in the ED parallel those of clinical registries, with decreases in AMI incidence and STEMI proportion. ED care processes for STEMI mirror evolving guidelines that favor high‐intensity antiplatelet therapy, early invasive strategies, and regionalization of care.
Keywords: acute myocardial infarction, emergency department, healthcare quality, temporal trends
Subject Categories: Health Services, Quality and Outcomes
Nonstandard Abbreviations and Acronyms
- CMS
Centers for Medicare and Medicaid Services
- NHAMCS
National Hospital Ambulatory Medical Care Survey
Clinical Perspective
What Is New?
The incidence of ST‐segment–elevation myocardial infarction in US emergency departments has continued to decrease, suggesting the overall success of systems‐level efforts to enhance care for ST‐segment–elevation myocardial infarction and outpatient coronary heart disease.
Quality of care of ST‐segment–elevation myocardial infarction in the emergency department setting has improved as well, though gaps likely remain.
What Are the Clinical Implications?
Especially given known associations between emergency department crowding and adverse outcomes among patients with acute myocardial infarction, our results indicate that the emergency department may benefit from further resource allocation to streamline acute myocardial infarction care processes.
Cardiovascular health services researchers should expand their focus beyond registries to examine the full spectrum of patients receiving care for acute myocardial infarction, to better understand real‐world care delivery for this population.
Care for acute myocardial infarction (AMI) has advanced considerably over the past 2 decades. 1 In particular, improvements in timeliness and efficiency of care 2 , 3 have likely contributed to decreasing AMI‐related morbidity and mortality in the United States. 4 Undergirding these improvements are efforts aimed at expediting emergency AMI care, including activation of the catheterization laboratory by emergency physicians, data monitoring, and feedback to emergency department (ED) staff, 5 as well as investments in regional systems of care. 6 Prior studies have demonstrated positive trends in the quality of AMI care and associated outcomes, but many of these studies are based on restrictive samples or older data. 7 , 8
Treatment for AMI, which includes ST‐segment–elevation myocardial infarction (STEMI) and non–ST‐segment–elevation myocardial infarction (NSTEMI), is often initiated in the ED. Over 90% of people with AMI receive emergency care. 9 While 60% of patients undergo same‐hospital admission, a substantial portion are transferred between hospitals via the ED. 10 But despite the ED's role as a critical entry point to acute care in the US healthcare system, the most contemporary available data regarding the epidemiology of AMI in US EDs are, by now, nearly a decade old. 11 Beyond epidemiology, few studies have specifically examined quality of AMI care delivered in the ED. 12 , 13 , 14 These gaps in knowledge, coupled with the fact that national quality measurement programs assessing the quality of emergency AMI care may exclude as many as 60% of patients, 15 reflect the need for a contemporary, real‐world assessment of AMI care in US EDs.
Accordingly, we examined trends in the epidemiology and quality of care for the entire spectrum of STEMI and NSTEMI visits evaluated in the ED between 2005 and 2015. Specifically, we assessed trends in the timeliness and effectiveness of ED care for AMI based on existing quality measures and evidence‐based practices, including ED length of stay, ED disposition, and ED administration of guideline‐directed pharmacotherapies. Rather than assessing the performance of specific metrics that may often be limited to narrow populations, the purpose of our study was to observe, in a holistic fashion, directional trends in ED AMI care based on a real‐world population.
Methods
Design
We conducted an observational analysis of the National Hospital Ambulatory Medical Care Survey (NHAMCS) between 2005 and 2015. We selected this period because it encompasses recent advances in AMI care, including the implementation of national quality measures assessing rapidity of diagnosis, ED management, and reperfusion. 2
Source of Data
We utilized 11 annual data files of the NHAMCS, an annual survey of ambulatory and ED visits to US hospitals excluding federal, military, and Veterans Administration facilities. The data that support the findings of this study are available from the corresponding author upon reasonable request. The NHAMCS is administered by the National Center for Health Statistics of the Centers for Disease Control and Prevention. Designed to be nationally representative of hospital ambulatory and ED care delivery and use, the NHAMCS uses a 4‐stage probability sampling design to enable weighted national estimates. The survey narrows from 112 primary geographic sampling units (selected from among those used in the National Health Interview Survey) to hospitals within these primary sampling units to EDs within these hospitals to specific patient encounters. The survey instrument is a patient record form, completed by trained staff for a random sample of ED visits during a randomly assigned reporting period. The patient record form includes patient demographic information, payor, chief complaint, ED diagnosis, medications prescribed and procedures performed, and disposition. Each individual patient encounter is weighted using the product of the corresponding sampling fractions at each of the 4 stages. To address survey nonresponses, the National Center for Health Statistics adjusts sampling weights. Detailed descriptions of the survey sample design and sampling methods have been previously well described by the Centers for Disease Control and Prevention. 16 The institutional review board of Yale University exempted the study.
Study Population
The overall study population included all patients aged ≥18 years diagnosed with AMI by an ED provider.
The NHAMCS records include ED diagnoses (International Classification of Disease, Ninth Revision [ICD‐9]) for each visit. We classified each AMI visit as STEMI or NSTEMI on the basis of prior work. We defined STEMI as 410.00, 410.01, 410.10, 410.11, 410.20, 410.21, 410.30, 410.31, 410.40, 410.41, 410.50, 410.51, 410.60, 410.61, 410.80, 410.81, 410.90, and 410.91. We defined NSTEMI as 410.70 and 410.71. These definitions have been previously validated and used in prior studies, 17 , 18 , 19 , 20 , 21 , 22 as well as supported by billing guidance to coders from the Centers for Medicare and Medicaid Services (CMS). 23 The ICD‐9 codes we used to define STEMI have previously been demonstrated to have a specificity of 93.4% after chart and ECG adjudication among ED patients. 22 Moreover, among patients presenting with ECG evidence of STEMI, <10% are misclassified under code 410.7x (NSTEMI). 18
For each included visit, we also obtained patient‐level data elements including age, sex, self‐reported race/ethnicity, and mode of ED arrival (ie, arrival via emergency medical services [EMS] or not). We excluded patients who were transferred from the ED to a psychiatric hospital. We also excluded those patients who died in the ED and left the ED without completing treatment.
Outcomes
We examined several primary epidemiologic and quality outcomes. Epidemiologic outcomes included estimated annual incidence of AMI, NSTEMI, and STEMI. Quality outcomes included timeliness and effectiveness of ED AMI care.
Outcomes relating to timeliness of ED AMI care included median ED length of stay and ED disposition (admit/transfer). Consistent with definitions published by the Emergency Department Benchmarking Alliance and incorporated into national CMS quality measures, 24 we defined ED length of stay as the time from ED arrival to the time of ED departure for procedure, admission, or interhospital transfer. We categorized ED disposition into general (overall) admission to the same hospital, admission to a critical care unit of the same hospital, direct admission to the cardiac catheterization laboratory, or transfer to another hospital. In 2005 and 2006, admission to the cardiac catheterization laboratory and admission to the operating room were grouped as a single variable in the NHAMCS. From 2007 onward, admission to the cardiac catheterization laboratory was captured as a distinct variable.
Outcomes relating to effectiveness of ED AMI care included ED administration of guideline‐based pharmacologic therapy for AMI. We grouped medications administered in the ED into the following major drug classes: nonaspirin oral antiplatelet agents (clopidogrel, ticagrelor, ticlopidine, and prasugrel), intravenous antithrombotic agents (heparin, bivalirudin, and argatroban), fibrinolytic agents (tenecteplase, alteplase, reteplase, streptokinase, urokinase, anistreplase, and tissue plasminogen activator), and glycoprotein IIb/IIIa inhibitors (eptifibatide, abciximab, and tirofiban). We specifically chose these drug classes because of their inclusion within current professional society guidelines for the treatment of STEMI and NSTEMI. 25 , 26 Drugs were coded in terms of their generic components and therapeutic classes using Lexicon Plus (Cerner Multum). 16 We calculated each outcome as the proportion of patients with AMI, STEMI, and NSTEMI receiving each class of pharmacotherapy.
Statistical Analysis
To characterize changes in AMI incidence over time, we calculated the yearly proportion of ED visits with an ED discharge diagnosis of AMI (STEMI and NSTEMI). To improve the stability of estimates and meet Centers for Disease Control and Prevention reliability criteria, we grouped data into 3‐year increments and a final 2‐year increment, as other authors have done and as recommended by the National Center for Health Statistics. 27 , 28 , 29 , 30
For each outcome measure, we report proportions for categorical variables and means (SEs) for continuous variables. Outcomes are reported with 95% CIs where appropriate. Race/ethnicity was defined by the providers completing the survey. We divided race into 4 categories: White, Black, Hispanic, and other, which included individuals of Asian, Native Hawaiian, Pacific Islander, American Indian, or multiple races. Analyses were performed using R version 3.3.3 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Trends in the Epidemiology of AMI Across US EDs
Incidence of AMI, STEMI, and NSTEMI over time are displayed in Figure 1. From 2005 to 2015, there were an estimated 4 398 762 ED visits for AMI, 3 605 165 ED visits for STEMI, and 793 597 ED visits for NSTEMI in the United States. These represent 0.33%, 0.27%, and 0.06% of all ED visits, respectively. Estimated yearly incidence of ED visits for AMI decreased from 1 493 145 in 2005 to 2007 to 581 924 in 2014 to 2015 (Table S1). Estimated yearly incidence of ED visits for STEMI decreased from 1 402 768 in 2005 to 2007 (95% CI, 1 101 967–1 703 569) to 315 813 in 2014 to 2015 (95% CI, 194 655–436 971) (Table). Among patients with STEMI who arrived by EMS, estimated yearly incidence decreased from 552 971 in 2005 to 2007 to 165 960 in 2014 to 2015 (Table S2). Estimated yearly incidence of ED visits for NSTEMI increased from 90 377 in 2005 to 2007 (95% CI, 43 107–137 647) to 266 111 in 2014 to 2015 (95% CI, 142 184–390 038) (Table S3). Over this 11‐year period, the proportion of all ED visits for AMI declined from 0.05% to 0.02%. Concurrently, the proportion of ED AMI visits for STEMI decreased from 94% to 54%.
Figure 1. Estimated yearly incidence of acute myocardial infarction (AMI), non–ST‐segment–elevation myocardial infarction (NSTEMI), and ST‐segment–elevation myocardial infarction (STEMI).
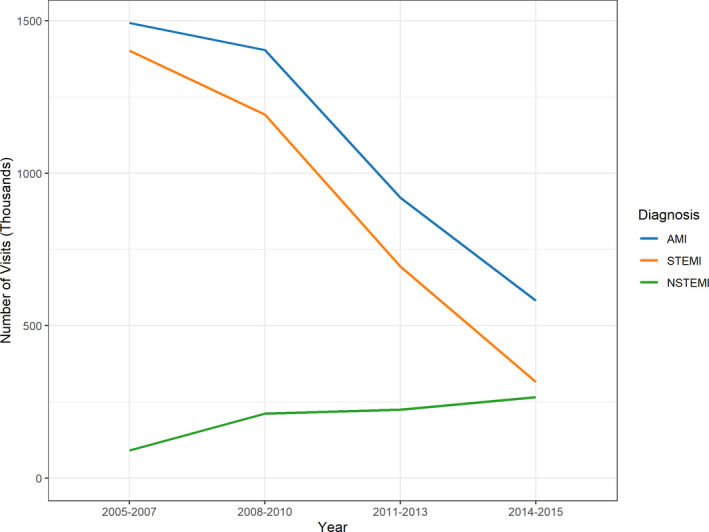
Our findings corroborate those of prior epidemiologic studies, demonstrating that the overall incidence of emergency department (ED) visits for AMI and STEMI have declined, while ED NSTEMI diagnoses have increased, albeit to a lesser degree.
Table 1.
Patient Characteristics and Outcomes, STEMI
| 2005–2007 | 2008–2010 | 2011–2013 | 2014–2015 | |
|---|---|---|---|---|
| Estimated number of visits | 1 402 768 | 1 192 090 | 694 494 | 315 813 |
| Demographic characteristics, N (%) | ||||
| Age, y, mean (SE) | 64.9 (1.2) | 63.5 (1.1) | 65.1 (1.7) | 68.2 (2.4) |
| Male | 797 965 (56.9) | 681 363 (57.2) | 436 145 (62.8) | 149 949 (47.5) |
| White | 1 121 066 (79.9) | 890 081 (74.7) | 523 509 (75.4) | 279 486 (88.5) |
| Black | 164 334 (11.7) | 116 696 (9.8) | 99 578 (14.3) | 20 819 (6.6) |
| Hispanic | 84 801 (6.1) | 135 981 (11.4) | 61 149 (8.8) | 15 508 (4.9) |
| Other race | 32 567 (2.3) | 49 332 (4.1) | 10 258 (1.5) | 0 (0.0) |
| Outcomes, % (SE) | ||||
| ED LOS, median (IQR), min | 195 (121, 315) | 211 (83, 325) | 158 (70, 296) | 148 (59, 220) |
| Admitted | 66.3 (3.3) | 72.2 (3.9) | 68.9 (4.9) | 57.6 (8.1) |
| Admission to critical care unit | 34.0 (4.1) | 33.6 (4.5) | 31.9 (5.9) | 39.6 (9.8) |
| Admission to cardiac catheterization lab | 11.8 (2.7) | 23.4 (4.5) | 36.7 (7.1) | 37.3 (8.5) |
| Transferred | 19.7 (3.0) | 14.9 (3.1) | 20.9 (4.4) | 24.4 (6.8) |
| Nonaspirin antiplatelet agents | 10.5 (2.0) | 13.6 (2.7) | 13.1 (2.9) | 26.6 (8.3) |
| Intravenous antithrombotic agents | 23.0 (2.5) | 28.7 (3.8) | 30.2 (4.8) | 30.7 (7.6) |
| Fibrinolytic agents | 2.2 (1.1) | 1.8 (1.4) | 3.8 (1.7) | 5.0 (3.0) |
| Glycoprotein IIb/IIIa inhibitors | 5.0 (1.2) | 3.6 (1.5) | 3.3 (1.9) | 5.8 (3.4) |
ED indicates emergency department; IQR, interquartile range; LOS, length of stay; and STEMI, ST‐segment–elevation myocardial infarction.
Trends in Timeliness of ED AMI Care
For patients with STEMI sent for cardiac catheterization directly from the ED, median ED length of stay decreased from 62 to 37 minutes (Figure 2). Among patients with STEMI who arrived by EMS, median ED length of stay decreased from 195 to 94 minutes. Within this EMS cohort, the proportion of patients sent for cardiac catheterization directly from the ED increased from 12% to 56%, and median ED length of stay for patients sent for cardiac catheterization directly from the ED decreased from 47 to 37 minutes.
Figure 2. Median ED length of stay for ST‐elevation myocardial infarction (STEMI), by disposition type, presented with 95% CIs.
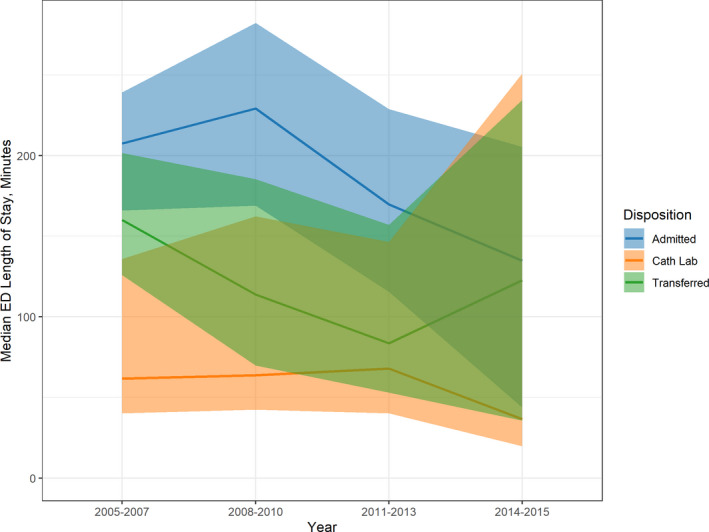
For patients with STEMI sent for cardiac catheterization directly from the emergency department (ED), median ED length of stay decreased from 62 to 37 minutes over the study period, likely attributable to ongoing efforts to streamline ED STEMI care processes.
Overall, median ED length of stay decreased from 195 to 148 minutes for STEMI and increased from 174 to 235 minutes for NSTEMI. The proportion of STEMI sent for cardiac catheterization directly from the ED increased from 12% to 37%. Interhospital transfer rates increased from 20% to 24% for STEMI. Interhospital transfer rates decreased from 17% to 12% for EMS‐arrival patients with STEMI.
Trends in Effectiveness of ED AMI Care
Trends in ED administration of pharmacotherapies for STEMI are shown in Figure 3. ED administration of nonaspirin antiplatelet agents for patients with STEMI increased from 10% to 27%. ED administration of nonaspirin antiplatelet agents for patients with NSTEMI increased from 0% to 9%. ED administration of antithrombotic agents increased for STEMI (23%–31%) and remained stable for NSTEMI (22% to 20%). ED administration of fibrinolytic agents for STEMI ranged from 2% to 5%. ED administration of glycoprotein IIb/IIIa inhibitors ranged from 5% to 6% for STEMI and from 3% to 0% for NSTEMI.
Figure 3. Trends in evidence‐based pharmacotherapies for ST‐segment–elevation myocardial infarction (STEMI), presented with 95% CIs.
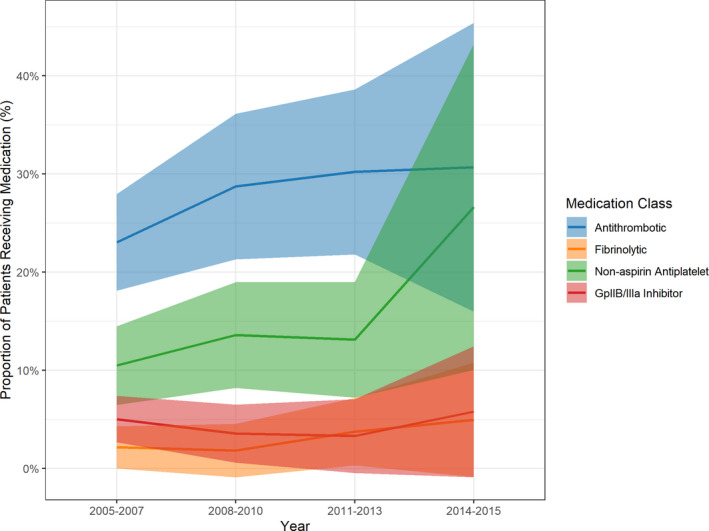
During the study period, several landmark clinical trials of traditional and novel pharmacotherapies were published, along with major clinical practice guidelines and performance measures for the treatment of STEMI. We demonstrate steady increases in the administration of nonaspirin antiplatelet agents and antithrombotic agents in the emergency department.
Discussion
We found several notable trends in the epidemiology and quality of ED care for AMI over the past decade. Specifically, we observed a decline in the incidence of STEMI and improvements in the timeliness and effectiveness of STEMI care. To our knowledge, this work represents the most contemporary assessment of real‐world patterns of emergency care for AMI in a nationally representative sample.
Our work encompasses the timeline of national initiatives aimed at improving the care of AMI, STEMI in particular: 2005, when the CMS began to report publicly the proportion of patients with STEMI receiving timely treatment; 2006, when the American College of Cardiology launched the D2B Alliance 5 ; 2007, when the American Heart Association launched Mission: Lifeline and the CMS began publicly reporting hospital‐specific mortality rates for AMI 6 , 31 ; and 2012, when the CMS began to include certain outcomes related to emergency AMI care in its Value‐Based Purchasing Program. 32
Similar to prior epidemiologic studies, we found that the overall incidence of ED visits for AMI and STEMI have declined, while ED NSTEMI diagnoses have increased, albeit to a lesser degree. The observed decline in STEMI incidence in US EDs, especially, builds on prior studies reporting declining rates of STEMI hospitalizations in two different regions of the United States. 33 , 34 A host of interrelated factors may be responsible for this continued decline, including improvements in preventive care and outpatient management of chronic coronary heart disease, 35 as well as successful system‐wide efforts to enhance regional STEMI care.
There are several possible explanations for the high initial proportion of ED AMI visits for STEMI that we observe. The NHAMCS captures ED diagnoses as opposed to hospital discharge diagnoses, which may inflate the observed STEMI proportion. As other authors have noted, nearly one‐third of patients who are admitted to the hospital with a diagnosis of an acute coronary syndrome carry a different diagnosis at hospital discharge. 36 This, coupled with ambiguous clinical documentation in the ED and deficiencies in the coding system itself, may have contributed to an observed high proportion of patients with STEMI who, in reality, likely contained a mix of AMI scenarios. In 2005, the beginning of our study period, the ICD‐9 coding system was changed to recognize NSTEMI as a separate pathologic entity, distinct from STEMI. Before 2005, the ICD‐9 coding system, despite its widespread use in the evaluation of healthcare outcomes, did not draw this distinction. Previous work has demonstrated that even after the aforementioned change to the ICD‐9 coding schema, patients with NSTEMI are more likely to be misclassified as having STEMI than vice versa. 18
An increase in the incidence of ED visits for NSTEMI may be explained by a number of factors as well. The study period saw widespread adoption of rapid troponin testing in the ED, in keeping with evolving definitions of AMI relying on ischemic symptoms, ECG findings, and troponin measurement. 37 , 38 Increasing use of troponin testing may have led to an increase in the number of cases qualifying as an NSTEMI diagnosis, even though elevations in serum troponin may arise from a variety of clinical conditions other than AMI. Indeed, prior work prospectively evaluating definitions of AMI that rely on troponin measurement demonstrated that the application of these criteria results in large increases in observed rates of myocardial infarction. 39 The observed increase in incidence of ED visits for NSTEMI could also reflect a true epidemiologic trend, as recent data has indicated a shift toward AMI occurring among younger demographic groups. 40 Finally, from a clinical diagnosis perspective, the diagnosis of NSTEMI often relies on serial biomarker measurements conducted during hospitalization—data that the NHAMCS, which only addresses ED care delivery, does not contain, and which may actually have led to undercounting of NSTEMI cases.
Our study also provides real‐world insights into the timeliness of ED AMI care. Recent work in a clinical registry has demonstrated that efforts aimed at regionalizing STEMI care—efforts that involve EMS, ED providers, and hospital systems—have resulted in a nationwide decrease in median first medical contact‐to‐device time. 7 In focusing on a longer and more recent time period, our study expands upon these findings, demonstrating decreases in ED length of stay for patients with STEMI as well. Among the subset of patients with STEMI sent for cardiac catheterization directly from the ED, median ED length of stay decreased dramatically, likely indicating the success of efforts to streamline ED STEMI care processes. Importantly, we observe these trends among the cohort of patients with STEMI who arrived by EMS as well those who did not.
We also note an increase in ED length of stay for patients with NSTEMI. Whereas improvements in the timeliness of STEMI care may reflect the implementation of STEMI protocols and enhanced systemwide performance, increases in ED length of stay for patients with NSTEMI may relate to the growing and linked problems of hospital bed shortages and ED boarding and crowding. 41 Moreover, owing to their lack of uniform ECG findings and heterogeneity in clinical presentation, patients with NSTEMI may be triaged to lower‐acuity ED beds, facing longer ED lengths of stay. This carries important clinical ramifications, as patients with NSTEMI experiencing longer ED lengths of stay are less likely to receive guideline‐concordant care, 42 and ED crowding has been linked to adverse outcomes among patients with AMI. 43
We identified trends in ED administration of pharmacotherapies for AMI consistent with evolving clinical practice guidelines. During the study period, several landmark clinical trials of traditional and novel pharmacotherapies were published, including TRITON‐TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel–Thrombolysis in Myocardial Infarction 38), ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy), HORIZONS‐AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction), and EARLY‐ACS (Early Glycoprotein IIb/IIIa Inhibition in Non–ST‐Segment Elevation Acute Coronary Syndrome), 44 , 45 , 46 , 47 as well as major clinical practice guidelines and performance measures for the treatment of STEMI and NSTEMI.
Particularly in the case of STEMI, our results mirror the results of these trials and guidelines, as demonstrated by steady increases in the administration of nonaspirin antiplatelet agents and antithrombotic agents. These trends suggest the ongoing adoption by ED providers of clinical practice guidelines emphasizing dual antiplatelet therapy and antithrombotic therapy as cornerstones of STEMI management. Rates of administration of glycoprotein IIb/IIIa inhibitors for STEMI remained low and decreased for most of the study period. This trend may also reflect an evolution in evidence. Trial results initially favored early upstream administration of these agents, but their routine use has been declining in favor of newer antiplatelet agents, which demonstrate similar ischemic end points and lower bleeding rates. 48
Consistently low rates of fibrinolytic use may also be explained by several trends. First, given the established superiority of timely primary percutaneous coronary intervention (PCI) over fibrinolysis, increases in the proportion of patients with STEMI transferred or directly admitted from the ED for PCI may reflect reduced motivation on the part of emergency physicians to administer on‐site fibrinolysis. Second, as other authors have noted, both fibrinolysis and PCI remain underused nationwide, 49 with use of fibrinolysis for STEMI decreasing and concurrent worsening of door‐to‐needle times. 50 Only one‐third of acute care hospitals in the United States have full‐time PCI capability, 51 and long transfer times often result in patients with STEMI failing to achieve timely PCI. 52 Though we observe reductions in ED length of stay in the subset of patients with STEMI who underwent transfer (among both EMS‐ and non–EMS‐arrival patients), overall, lengths of stay in this group far exceeded the recommended 30‐minute door‐in–door‐out time frame specified in current guidelines. 26 Our findings thus echo renewed calls to examine the role that early on‐site fibrinolysis may play in the treatment of STEMI among patients unable to undergo timely primary PCI. 53
Though rates of guideline‐directed pharmacotherapies for STEMI increased over our study period, we observe that overall, use of these medications remains low. This is likely attributable to clinical contraindications to certain therapies or undercounting, as the NHAMCS, similar to many data sets, lacks the ability to capture upstream (eg, via EMS) or downstream (eg, in the cardiac catheterization laboratory) medication administration. Low rates of pharmacotherapy administration may also be attributable to the fact that many ED STEMI protocols limit the number of medications given in the ED to ensure timely reperfusion. Indeed, bypassing traditional ED processes has been shown to reduce door‐to‐balloon time in STEMI. 54 Our findings do suggest, however, an opportunity for further research into real‐world practice patterns in the ED setting, specifically as they relate to evidence‐based pharmacotherapies given in the hyperacute phase of AMI.
Prior studies examining trends in the epidemiology and quality of AMI care have been conducted in clinical cardiovascular disease registries. The limitations of such registries have been documented previously. 55 Perhaps most notably, such data sets may exclude large swaths of patients with AMI from publicly reported measures of timely reperfusion, 56 thereby limiting the conclusions one can draw regarding broader trends in timeliness of emergency AMI care. Other data sources, such as the Nationwide Inpatient Sample (NIS), have also yielded similar observations regarding longitudinal trends in NSTEMI and STEMI. 57 , 58 As an inpatient care database, however, the Nationwide Inpatient Sample cannot differentiate between diagnoses that were present on admission versus those that arose during hospitalization 59 and thus is not well suited to investigate contemporary patterns of emergency AMI care, such as those we describe here. Similar to recent work in a cohort of Medicare beneficiaries showing reductions in hospitalization rates for AMI and improvements in short‐term mortality, 1 our findings underscore the fact that system‐wide efforts to enhance STEMI care represent one of the major public health achievements of the past few decades. Our study is unique in that we demonstrate similar trends in an expansive, heterogeneous, and real‐world data set of ED patients with AMI, one that is substantially different from the narrower cohorts included in clinical cardiovascular registries and quality measurement programs.
Our study has certain limitations. Because we focus exclusively on ED patients, our study cannot describe overall patterns of NSTEMI and STEMI treated outside the emergency setting. Other studies documenting longitudinal trends in AMI care in US EDs also possess this same limitation. 11 Second, our study relies on administrative diagnosis codes to distinguish NSTEMI from STEMI. We base our coding schema on prior literature and billing guidance, but not an adjudicated case definition. The NHAMCS does not contain variables that might capture additional types of emergency care (eg, aspirin administered via EMS or at other presenting EDs, or in the cardiac catheterization laboratory), nor does it distinguish between primary versus nonprimary PCI hospitals. Finally, because of the method in which admission destination is coded in the NHAMCS, it is possible that patients with noncardiac catheterization laboratory destinations (eg, critical care unit, stepdown unit) also underwent urgent catheterization, depending on ED coding practices.
Despite these limitations, however, and unlike many data sets, the NHAMCS does provide richer insight into care administered in the ED, which is unavailable in traditional claims‐based data sets that lack clinical data.
Conclusions
In a national, real‐world sample of US EDs, trends in the epidemiology of AMI demonstrate substantial reductions in the annual incidence of STEMI, with commensurate increases in NSTEMI. Across a range of measures, the timeliness and effectiveness of emergency care for AMI has improved, likely reflecting the ongoing adoption of evidence‐based processes for AMI care. Nevertheless, gaps remain between guidelines and management of patients with AMI in the ED setting.
Sources of Funding
This work was supported by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science, a component of the National Institutes of Health.
Disclosures
Dr Krumholz reported personal fees from UnitedHealth, IBM Watson Health, Element Science, Aetna, Facebook, Arnold & Porter, and the Ben C. Martin Law Firm; grants from the Centers for Medicare & Medicaid Services, Medtronic, Johnson & Johnson, and the Food and Drug Administration; and serving as founder of the personal health information platform Hugo outside the submitted work. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S3
(J. Am. Heart Assoc. 2020;9:e017208 DOI: 10.1161/JAHA.120.017208.)
For Sources of Funding and Disclosures, see page 8 and 9.
References
- 1. Krumholz HM, Normand S‐LT, Wang Y. Twenty‐year trends in outcomes for older adults with acute myocardial infarction in the United States. JAMA Netw Open. 2019;9:e191938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, et al. Improvements in door‐to-balloon time in the United States, 2005 to 2010. Circulation. 2011;1038–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nuti SV, Wang Y, Masoudi FA, Bratzler DW, Bernheim SM, Murugiah K, Krumholz HM. Improvements in the distribution of hospital performance for the care of patients with acute myocardial infarction, heart failure, and pneumonia, 2006–2011. Med Care. 2015;485–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, et al. Heart disease and stroke statistics‐2018 update: a report from the American Heart Association. Circulation. 2018;e67–e492. [DOI] [PubMed] [Google Scholar]
- 5. Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline‐Rogers E, Stern AF, Byrd JR, Brush JE. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door‐to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;97–104. [DOI] [PubMed] [Google Scholar]
- 6. Jacobs AK, Antman EM, Ellrodt G, Faxon DP, Gregory T, Mensah GA, Moyer P, Ornato J, Peterson ED, Sadwin L. Recommendation to develop strategies to increase the number of ST‐segment‐elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006;2152–2163. [DOI] [PubMed] [Google Scholar]
- 7. Granger CB, Bates ER, Jollis JG, Antman EM, Nichol G, O'Connor RE, Gregory T, Roettig ML, Peng SA, Ellrodt G, et al. Improving care of STEMI in the United States 2008 to 2012. J Am Heart Assoc. 2019;9:e008096 DOI: 10.1161/JAHA.118.008096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, Smith SC, Pollack CV, Newby LK, Harrington RA, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;1912–1920. [DOI] [PubMed] [Google Scholar]
- 9. Kocher KE, Dimick JB, Nallamothu BK. Changes in the source of unscheduled hospitalizations in the United States. Med Care. 2013;689–698. [DOI] [PubMed] [Google Scholar]
- 10. Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;391–393. [DOI] [PubMed] [Google Scholar]
- 11. Ward MJ, Kripalani S, Zhu Y, Storrow AB, Dittus RS, Harrell FE Jr, Self WH. Incidence of emergency department visits for ST‐elevation myocardial infarction in a recent six‐year period in the United States. Am J Cardiol. 2015;167–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tsai CL, Magid DJ, Sullivan AF, Gordon JA, Kaushal R, Ho MP, Peterson PN, Blumenthal D, Camargo CA Jr. Quality of care for acute myocardial infarction in 58 U.S. emergency departments. Acad Emerg Med. 2010;940–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pham JC, Kelen GD, Pronovost PJ. National study on the quality of emergency department care in the treatment of acute myocardial infarction and pneumonia. Acad Emerg Med. 2007;856–863. [DOI] [PubMed] [Google Scholar]
- 14. Vinson DR, Magid DJ, Brand DW, Masoudi FA, Ho PM, Lyons EE, Crounse L, van der Vlugt TM, Padgett TG, Tricomi AJ, et al. Patient sex and quality of ED care for patients with myocardial infarction. Am J Emerg Med. 2007;996–1003. [DOI] [PubMed] [Google Scholar]
- 15. Bernheim SM, Wang Y, Bradley EH, Masoudi FA, Rathore SS, Ross JS, Drye E, Krumholz HM. Who is missing from the measures? Trends in the proportion and treatment of patients potentially excluded from publicly reported quality measures. Am Heart J. 2010;943–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention, National Center for Health Statistics . Available at: https://www.cdc.gov/nchs/ahcd/index.htm. Accessed May 8, 2019.
- 17. Elbadawi A, Elgendy IY, Ha LD, Mahmoud K, Lenka J, Olorunfemi O, Reyes A, Ogunbayo GO, Saad M, Abbott JD. National trends and outcomes of percutaneous coronary intervention in patients >/=70 years of age with acute coronary syndrome (from the National Inpatient Sample Database). Am J Cardiol. 2019;25–32. [DOI] [PubMed] [Google Scholar]
- 18. Steinberg BA, French WJ, Peterson E, Frederick PD, Cannon CP; National Registry of Myocardial Infarction Investigators . Is coding for myocardial infarction more accurate now that coding descriptions have been clarified to distinguish ST‐elevation myocardial infarction from non‐ST elevation myocardial infarction? Am J Cardiol. 2008;513–517. [DOI] [PubMed] [Google Scholar]
- 19. Agarwal M, Agrawal S, Garg L, Garg A, Bhatia N, Kadaria D, Reed G. Effect of chronic obstructive pulmonary disease on in‐hospital mortality and clinical outcomes after ST‐segment elevation myocardial infarction. Am J Cardiol. 2017;1555–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel B, Carson P, Shah M, Garg L, Agarwal M, Agrawal S, Arora S, Steigerwalt S, Bavry A, Dusaj R, et al. Acute kidney injury requiring dialysis and in‐hospital mortality in patients with chronic kidney disease and non‐ST-segment elevation acute coronary syndrome undergoing early vs delayed percutaneous coronary intervention: a nationwide analysis. Clin Cardiol. 2017;1303–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Khera S, Kolte D, Gupta T, Mujib M, Aronow WS, Agarwal P, Palaniswamy C, Jain D, Ahmed A, Fonarow GC, et al. Management and outcomes of ST‐elevation myocardial infarction in nursing home versus community‐dwelling older patients: a propensity matched study. J Am Med Dir Assoc. 2014;593–599. [DOI] [PubMed] [Google Scholar]
- 22. Glickman SW, Shofer FS, Wu MC, Scholer MJ, Ndubuizu A, Peterson ED, Granger CB, Cairns CB, Glickman LT. Development and validation of a prioritization rule for obtaining an immediate 12‐lead electrocardiogram in the emergency department to identify ST‐elevation myocardial infarction. Am Heart J. 2012;372–382. [DOI] [PubMed] [Google Scholar]
- 23. Centers for Medicare and Medicaid Services . Available at: https://www.cms.gov/Medicare/Coding/ICD10/2015-ICD-10-CM-and-GEMs.html. Accessed May 8, 2019.
- 24. Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone‐Griffith S. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med. 2015;542–553. [DOI] [PubMed] [Google Scholar]
- 25. Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, Jaffe AS, Jneid H, Kelly RF, Kontos MC, et al. 2014 AHA/ACC guideline for the management of patients with non‐ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;2354–2394.25249586 [Google Scholar]
- 26. O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, De Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, et al. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;e362–e425. [DOI] [PubMed] [Google Scholar]
- 27. Schissler AJ, Rozenshtein A, Schluger NW, Einstein AJ. National trends in emergency room diagnosis of pulmonary embolism, 2001–2010: a cross‐sectional study. Respir Res. 2015;44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mafi JN, Edwards ST, Pedersen NP, Davis RB, McCarthy EP, Landon BE. Trends in the ambulatory management of headache: analysis of NAMCS and NHAMCS data 1999–2010. J Gen Intern Med. 2015;548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mazer‐Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001–2010. Acad Emerg Med. 2014;236–243. [DOI] [PubMed] [Google Scholar]
- 30. Centers for Disease Control and Prevention, National Center for Health Statistics . Understanding and using NAMCS and NHAMCS data. 2010. Available at: https://www.cdc.gov/nchs/ppt/nchs2010/03_Hsiao.pdf. Accessed June 21, 2019.
- 31. Ross JS, Bernheim SM, Drye ED. Expanding the Frontier of outcomes measurement for public reporting. Circ Cardiovasc Qual Outcomes. 2011;11–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chee TT, Ryan AM, Wasfy JH, Borden WB. Current state of value‐based purchasing programs. Circulation. 2016;2197–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;2155–2165. [DOI] [PubMed] [Google Scholar]
- 34. McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Go AS, Iribarren C, Chandra M, Lathon PV, Fortmann SP, Quertermous T, Hlatky MA. Statin and beta‐blocker therapy and the initial presentation of coronary heart disease. Ann Intern Med. 2006;229–238. [DOI] [PubMed] [Google Scholar]
- 36. Handrinos A, Braitberg G, Mosley IT. Comparison of emergency department and hospital discharge diagnosis of acute coronary syndrome. Emerg Med Australas. 2014;153–157. [DOI] [PubMed] [Google Scholar]
- 37. Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined: a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;959–969. [DOI] [PubMed] [Google Scholar]
- 38. Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D, Goldberg RJ, Hand MM, Jaffe AS, Julian DG, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;2543–2549. [DOI] [PubMed] [Google Scholar]
- 39. Roger VL, Killian JM, Weston SA, Jaffe AS, Kors J, Santrach PJ, Tunstall‐Pedoe H, Jacobsen SJ. Redefinition of myocardial infarction: prospective evaluation in the community. Circulation. 2006;790–797. [DOI] [PubMed] [Google Scholar]
- 40. Andersson C, Vasan R. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol. 2018;230–240. [DOI] [PubMed] [Google Scholar]
- 41. Warden G, Griffin RB, Erickson SM, Mchugh M, Wheatley B, Dharshi AS, Trenum C. Hospital‐Based Emergency Care: at the Breaking Point. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 42. Diercks DB, Roe MT, Chen AY, Peacock WF, Kirk JD, Pollack CV Jr, Gibler WB, Smith SC Jr, Ohman M, Peterson ED. Prolonged emergency department stays of non-ST‐segment‐elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann Emerg Med. 2007;489–496. [DOI] [PubMed] [Google Scholar]
- 43. Pines JM, Pollack CV Jr, Diercks DB, Chang AM, Shofer FS, Hollander JE. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med. 2009;617–625. [DOI] [PubMed] [Google Scholar]
- 44. Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;2001–2015. [DOI] [PubMed] [Google Scholar]
- 45. Stone GW, McLaurin BT, Cox DA, Bertrand ME, Lincoff AM, Moses JW, White HD, Pocock SJ, Ware JH, Feit F, et al. Bivalirudin for patients with acute coronary syndromes. N Engl J Med. 2006;2203–2216. [DOI] [PubMed] [Google Scholar]
- 46. Stone GW, Witzenbichler B, Guagliumi G, Peruga JZ, Brodie BR, Dudek D, Kornowski R, Hartmann F, Gersh BJ, Pocock SJ, et al. Bivalirudin during primary PCI in acute myocardial infarction. N Engl J Med. 2008;2218–2230. [DOI] [PubMed] [Google Scholar]
- 47. Giugliano RP, White JA, Bode C, Armstrong PW, Montalescot G, Lewis BS, van `t Hof A, Berdan LG, Lee KL, Strony JT, et al. Early versus delayed, provisional eptifibatide in acute coronary syndromes. N Engl J Med. 2009;2176–2190. [DOI] [PubMed] [Google Scholar]
- 48. Di Mario C. Rise and fall of glycoprotein IIb–IIIa inhibitors in ST‐segment elevation myocardial infarction. Heart. 2014;823–824. [DOI] [PubMed] [Google Scholar]
- 49. Vora AN, Holmes DN, Rokos I, Roe MT, Granger CB, French WJ, Antman E, Henry TD, Thomas L, Bates ER, et al. Fibrinolysis use among patients requiring interhospital transfer for ST‐segment elevation myocardial infarction care: a report from the US National Cardiovascular Data Registry. JAMA Intern Med. 2015;207–215. [DOI] [PubMed] [Google Scholar]
- 50. Hira RS, Bhatt DL, Fonarow GC, Heidenreich PA, Ju C, Virani SS, Bozkurt B, Petersen LA, Hernandez AF, Schwamm LH, et al. Temporal trends in care and outcomes of patients receiving fibrinolytic therapy compared to primary percutaneous coronary intervention: insights from the Get With The Guidelines Coronary Artery Disease (GWTG‐CAD) Registry. J Am Heart Assoc. 2016;9:e004113 DOI: 10.1161/JAHA.116.004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Concannon TW, Nelson J, Goetz J, Griffith JL. A percutaneous coronary intervention lab in every hospital? Circ Cardiovasc Qual Outcomes. 2012;14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McMullan JT, Hinckley W, Bentley J, Davis T, Fermann GJ, Gunderman M, Hart KW, Knight WA, Lindsell CJ, Miller C, et al. Ground emergency medical services requests for helicopter transfer of ST‐segment elevation myocardial infarction patients decrease medical contact to balloon times in rural and suburban settings. Acad Emerg Med. 2012;153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Redberg RF. Reconsidering transfer for percutaneous coronary intervention strategy: time is of the essence. Arch Intern Med. 2012;98–99. [DOI] [PubMed] [Google Scholar]
- 54. Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, et al. Strategies for reducing the door‐to-balloon time in acute myocardial infarction. N Engl J Med. 2006;2308–2320. [DOI] [PubMed] [Google Scholar]
- 55. Messenger JC, Ho KK, Young CH, Slattery LE, Draoui JC, Curtis JP, Dehmer GJ, Grover FL, Mirro MJ, Reynolds MR, et al. The National Cardiovascular Data Registry (NCDR) data quality brief: the NCDR data quality program in 2012. J Am Coll Cardiol. 2012;1484–1488. [DOI] [PubMed] [Google Scholar]
- 56. Cotoni DA, Roe MT, Li S, Kontos MC. Frequency of nonsystem delays in ST‐elevation myocardial infarction patients undergoing primary percutaneous coronary intervention and implications for door‐to-balloon time reporting (from the American Heart Association Mission: Lifeline program). Am J Cardiol. 2014;24–28. [DOI] [PubMed] [Google Scholar]
- 57. Agarwal M, Agrawal S, Garg L, Mohananey D, Garg A, Bhatia N, Lavie CJ. National trends in the incidence, management, and outcomes of heart failure complications in patients hospitalized for ST‐segment elevation myocardial infarction. Mayo Clin Proc Innov Qual Outcomes. 2017;26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Khera S, Kolte D, Aronow WS, Palaniswamy C, Subramanian KS, Hashim T, Mujib M, Jain D, Paudel R, Ahmed A, et al. Non-ST‐elevation myocardial infarction in the United States: contemporary trends in incidence, utilization of the early invasive strategy, and in‐hospital outcomes. J Am Heart Assoc. 2014;9:e000995 DOI: 10.1161/JAHA.114.000995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, Chan PS, Krumholz HM. Adherence to methodological standards in research using the National Inpatient Sample. JAMA. 2017;2011–2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3


