Abstract
Background
Outcomes of patients from out‐of‐hospital cardiac arrest (OHCA) vary widely globally because of differences in prehospital systems of emergency care. National efforts had gone into improving OHCA outcomes in Singapore in recent years including community and prehospital initiatives. We aimed to document the impact of implementation of a national 5‐year Plan for prehospital emergency care in Singapore on OHCA outcomes from 2011 to 2016.
Methods and Results
Prospective, population‐based data of OHCA brought to Emergency Departments were obtained from the Pan‐Asian Resuscitation Outcomes Study cohort. The primary outcome was Utstein (bystander witnessed, shockable rhythm) survival‐to‐discharge or 30‐day postarrest. Mid‐year population estimates were used to calculate age‐standardized incidence. Multivariable logistic regression was performed to identify prehospital characteristics associated with survival‐to‐discharge across time. A total of 11 465 cases qualified for analysis. Age‐standardized incidence increased from 26.1 per 100 000 in 2011 to 39.2 per 100 000 in 2016. From 2011 to 2016, Utstein survival rates nearly doubled from 11.6% to 23.1% (P=0.006). Overall survival rates improved from 3.6% to 6.5% (P<0.001). Bystander cardiopulmonary resuscitation rates more than doubled from 21.9% to 56.3% and bystander automated external defibrillation rates also increased from 1.8% to 4.6%. Age ≤65 years, nonresidential location, witnessed arrest, shockable rhythm, bystander automated external defibrillation, and year 2016 were independently associated with improved survival.
Conclusions
Implementation of a national prehospital strategy doubled OHCA survival in Singapore from 2011 to 2016, along with corresponding increases in bystander cardiopulmonary resuscitation and bystander automated external defibrillation. This can be an implementation model for other systems trying to improve OHCA outcomes.
Keywords: bystander CPR, emergency medical services, interventions, outcomes, out‐of‐hospital‐cardiac arrest, prehospital, resuscitation
Subject Categories: Cardiopulmonary Arrest, Cardiopulmonary Resuscitation and Emergency Cardiac Care, Epidemiology
Nonstandard Abbreviations and Acronyms
- CARES
Cardiac Arrest Registry to Enhance Survival
- OHCA
out‐of‐hospital cardiac arrest
- OPALS
Ontario Prehospital Advanced Life Support
- PAROS
Pan‐Asian Resuscitation Outcomes Study
Clinical Perspective
What Is New?
Outcomes of patients from out‐of‐hospital cardiac arrest vary widely globally because of differences in prehospital systems of emergency care.
Data from the Pan‐Asian Resuscitation Outcomes Study, a prospective, population‐based study of out‐of‐hospital cardiac arrest presenting to Emergency Departments, showed that between 2011 and 2016, national Utstein (bystander witnessed, shockable rhythm) survival‐to‐discharge or 30‐days postarrest nearly doubled from 11.6% to 23.1% in Singapore (P=0.006).
What Are the Clinical Implications?
This was associated with the implementation of a 5‐year national plan of prehospital emergency care consisting of both policy and implementation measures in community and prehospital areas.
Increases in both bystander cardiopulmonary resuscitation and bystander automated external defibrillation were independently associated with the rapidly improved survival.
This can be an implementation model for other systems trying to improve out‐of‐hospital cardiac arrest outcomes.
Out‐of‐hospital cardiac arrest (OHCA) is a global disease, being a leading cause of death in Singapore, paralleling worldwide trends. 1 Outcomes from OHCA vary widely between communities, relating to differences in patient demographics and emergency care systems. 2 , 3 Survival rates in the Asia‐Pacific region showed great variation, ranging from no reported survivors to 31.2% (Japan), 3 and this was associated with systemic differences in emergency care delivery. 3 , 4 , 5 In Singapore, the Utstein (bystander witnessed, shockable rhythm) survival‐to‐hospital discharge rate in Singapore was 11.0% between 2010 and 2012. 6 While this was a marked improvement from the 2.5% found between 2001 and 2004, 7 when benchmarked against sites such as Seattle, Washington, there was significant room for improvement.
Effective treatment of OHCA hinges on the “Chain of Survival” concept, which describes the rapid commencement and seamless provision of rescuer actions. 8 More recently, there is increased recognition of the important role of fundamental elements not confined to the traditional sphere of influence of the Emergency Medical Services (EMS) in enabling optimal OHCA care. These were encapsulated under the Modified Frame of Survival framework by the Global Resuscitation Alliance, and included cultural views, political commitment, and legislative environment. 9 , 10
Despite advancement in resuscitation science, OHCA outcomes have not consistently improved. 1 , 11 A 2010 systematic review of 79 studies concluded that from 1980 to 2008, aggregate survival remained unchanged at 6.7% to 8.4%. 12 Since this systematic review, steady improvements in survival over time have been subsequently reported in Denmark, 13 Sweden, 14 the Netherlands, 15 Canada, 16 and the United States. 17 It has been recognized, such as through the work of the Global Resuscitation Alliance, that OHCA care (OHCA being a prototypical time‐critical emergency condition) benefits from medical science only if there is educational efficiency and local implementation. This requires strategic policy, multi‐agency coordination, and systematic implementation measures.
Extensive national efforts have gone into improving OHCA outcomes in Singapore 6 , 18 through community and prehospital interventions. A period of exceptionally intense reorganization, policy restructuring, and organized implementation to improve the prehospital emergency care system occurred between 2009 and 2014, codified as the National Pre‐hospital Emergency Care System 5‐year Plan (henceforth, “5‐year Plan” or “Plan”).
This study investigated the epidemiology, treatment, and outcomes trends for OHCA in Singapore over a 6‐year period (2011–2016). It was hypothesized that Utstein survival from OHCA has improved over the period, and that the improvement is related to patient, bystander, and system factors. These findings would allow Singapore to “take stock” of the returns from a 5‐year Plan consisting of both policy and implementation measures, as well as to benchmark the Singapore emergency care system. In addition, an examination of the effectiveness of these strategies would provide useful lessons for other communities in comparable circumstances.
Methods
Data and Research Materials Transparency
The data that support the findings of this study may be available from the corresponding author upon reasonable request, subject to approval by the local institution.
Setting
Singapore is an urbanized island city‐state situated in Southeast Asia with a population of 5.5 million over a land area of 719.1 km2. 19 A population‐based survey in 2010 showed that 31.4% of responders had ever been trained in cardiopulmonary resuscitation (CPR), 10.7% had ever been trained in automated external defibrillation (AED), while 9.6% and 3.7% possessed valid certificates for these skills, respectively. 20
EMS are provided by the Singapore Civil Defence Force, which operates a fire‐based system activated by a centralized “995” dispatch system. This is provided free of charge. Singapore Civil Defence Force handled 131 806 ambulance calls in 2011 and this had increased to 178 154 in 2016. 21 Singapore Civil Defence Force utilized computer‐aided dispatch protocols, global positioning satellite vehicle location systems, and road traffic monitoring systems. During the study period, there was a single tier of paramedics (equivalent to North American emergency medical technician‐intermediate) who were trained in basic life support, AED, and specific interventions including intravenous adrenaline administration. Sixty‐nine percent of OHCA in Singapore occur at home in high‐rise apartments 22 with substantial vertical travel time. 23
Community and Prehospital Interventions and the National Pre‐Hospital Emergency Care System 5‐Year Plan (2009–2014)
The Plan was ratified as a response to a lack of multiagency coordination, planning, and oversight of prehospital emergency care. It was proposed that a national blueprint focusing on the strategic imperatives of leadership, community responsiveness, ambulance responsiveness, emergency department responsiveness, skills development, and technology be implemented in phases, over the next 5 years. The major interventions during this period were the following: mechanical CPR devices on ambulances (May 2011), Fire Bikers Scheme (April 2012, fire/rescue specialists on motorcycle dispatched ahead of ambulance arrival), dispatcher‐assisted CPR (July 2012), Dispatcher‐Assisted First Responder community training (April 2014), intraosseous devices on ambulances (April 2014), large‐scale deployment of AED in residential areas (April 2015), and crowdsourced community rescuer app (April 2015). Details of these interventions are given in the Appendix.
Study Population—the Pan‐Asian Resuscitation Outcomes Study
PAROS (Pan‐Asian Resuscitation Outcomes Study) is an ongoing clinical research network for OHCA. 3 It is a prospective, multicenter registry designed to provide baseline information on OHCA epidemiology, describe variations among EMS systems, and compare systemic and structural interventions in the Asia‐Pacific area. 3 , 4 , 5 The network was established in 2010 with aims to improve outcomes by informing on cost‐effective strategies. 3 For the current study, only data from Singapore were used.
PAROS methodology had been previously detailed. 3 Data definitions follow the Utstein recommendations, 24 and collaboration with the CARES (Cardiac Arrest Registry to Enhance Survival) in the United States enabled a unified taxonomy and data dictionary to allow valid global comparisons. 25 Data were extracted from emergency dispatch records, ambulance case notes, and emergency department and in‐hospital records. Quality assurance data checks were built into the data entry system, and data verification checks were implemented to ensure data integrity. 3
The registry included OHCA from 2011 to 2016 of all causes including traumatic arrests brought in by EMS or presenting to EDs via private or public transport, as confirmed by the absence of pulse, unresponsiveness, and apnea. Both adult and pediatric cases were included. All cases were prospectively collected in compliance with Utstein Style. Patients for whom resuscitation was not attempted and were immediately pronounced dead (because of decapitation, rigor mortis, dependent lividity, and “do not attempt resuscitation” orders) were excluded from the study.
Mid‐year population estimates from the Singapore Department of Statistics were used to calculate crude and age‐standardized incidence and survival rates. Population estimates pertain to resident population (Singapore citizens and permanent residents). Incidence rates were calculated by dividing the number of OHCA cases by the mid‐year population. Age‐standardized incidence rates were derived by applying the category‐specific incidence rates of each population to the Segi World Standard population. 26 Age‐standardized survival rates were calculated by the direct method using the Singapore population as the standard population in the corresponding year. 19
Outcomes were summarized in a 3‐tier cascade manner: (1) Utstein (bystander‐witnessed arrest, ventricular fibrillation), (2) cases where resuscitation was attempted, and (3) cases where resuscitation was attempted and who experienced nontraumatic cardiac arrest (not caused by blunt or penetrating trauma, and includes presumed cardiac cause, respiratory cause, drowning, and other causes). The following outcomes were reported: (1) EMS return of spontaneous circulation, (2) emergency department return of spontaneous circulation, (3) survival to admission, (4) survival rate to discharge, (5) postarrest cerebral performance category score 1 or 2, and (6) postarrest overall performance category score 1 or 2.
Study Variables, Definitions, and Outcomes
The primary exposure was calendar year as a continuous variable. The primary outcome was Utstein survival‐to‐hospital discharge or 30‐day postarrest. Utstein survival rates were calculated by dividing the number of those achieving the primary outcome by the total number of cases that are nontraumatic in origin, bystander witnessed, and had shockable initial rhythms (ventricular fibrillation or pulseless ventricular tachycardia). 24 Utstein survival was chosen to be the primary outcome because in these cases there were opportunities to intervene, and therefore reflects the efficiency and efficacy of the emergency care system. Furthermore, it is an agreed‐upon convention of measuring OHCA outcomes. 24 This enables comparison with data from other communities.
Secondary outcomes included return of spontaneous circulation, survival to hospital admission, and neurological status on discharge. Neurological status was assessed using Glasgow–Pittsburgh Outcome Scores (cerebral performance category and overall performance category). Neurologic status was evaluated by abstraction from clinical records, telephone, and face‐to‐face interviews by the attending physician either upon discharge or at 30 days postarrest.
Response time refers to the interval between time call was received by the dispatch center and time of arrival at scene (location street address) of either the ambulance, or a rapid responder dispatched via the same dispatch center.
Ethics Approval
The Centralised Institutional Review Board (2013/604/C) and Domain Specific Review Board (2013/00929) granted approval for this study with a waiver of patient informed consent.
Statistical Analysis
Data analysis was performed using Stata version 14 (StataCorp LLC, TX). Patient demographics and OHCA characteristics for all cases were summarized as frequency and percentage for categorical data and median and interquartile range for continuous data. Pearson χ2 test was used for categorical variables and nonparametric t test was used for continuous variables. Univariate logistic regression was performed to identify potential predictors of survival retrieved from existing literature. These potential predictors and calendar year were adjusted for in a multivariable logistic regression model. α was set at P<0.05.
Results
Study Population
Table 1 shows the summary of patient demographics and characteristics. A total of 11 465 cases were included for analysis between 2011 and 2016. Median age was 67 years (interquartile range, 55–79) and 64.8% were males. Seventy‐one percent of the cases occurred in residential locations.
Table 1.
Patient Characteristics
| All (n=11 465) | 2011 (n=1377) | 2012 (n=1440) | 2013 (n=1736) | 2014 (n=2037) | 2015 (n=2372) | 2016 (n=2503) | |
|---|---|---|---|---|---|---|---|
| Age, y, median (IQR) | 67 (55–79) | 65 (53–77) | 66 (54–78) | 67 (55–79) | 68 (55–80) | 67 (56–79) | 67 (55–79) |
| Sex (%) | |||||||
| Male | 7431 (64.8) | 935 (67.9) | 912 (63.3) | 1131 (65.2) | 1316 (64.6) | 1546 (65.2) | 1591 (63.6) |
| Female | 4034 (35.2) | 442 (32.1) | 528 (36.7) | 605 (34.9) | 721 (35.4) | 826 (34.8) | 912 (36.4) |
| Race (%) | |||||||
| Chinese | 7750 (67.6) | 893 (64.9) | 984 (68.3) | 1225 (70.6) | 1349 (66.2) | 1587 (66.9) | 1712 (68.4) |
| Indian | 1259 (11.0) | 185 (13.4) | 146 (10.1) | 161 (9.3) | 209 (10.3) | 277 (11.7) | 281 (11.2) |
| Malay | 1796 (15.7) | 201 (14.6) | 222 (15.4) | 265 (15.3) | 362 (17.8) | 363 (15.3) | 383 (15.3) |
| Other | 660 (5.8) | 90 (7.1) | 88 (6.1) | 85 (4.9) | 117 (5.7) | 145 (6.1) | 127 (5.1) |
| Location type (%) | |||||||
| Residential | 8196 (71.5) | 985 (71.5) | 990 (68.8) | 1246 (71.8) | 1480 (72.7) | 1658 (69.9) | 1837 (73.4) |
| Nonresidential | 3269 (28.5) | 392 (28.5) | 450 (31.2) | 490 (28.2) | 557 (27.3) | 714 (30.1) | 666 (26.6) |
| Medical history (%) | |||||||
| Unknown | 803 (7.0) | 144 (10.5) | 111 (7.7) | 139 (8.0) | 110 (5.4) | 145 (6.1) | 154 (6.2) |
| Heart disease | 4163 (36.3) | 511 (37.1) | 512 (35.6) | 624 (35.9) | 761 (37.4) | 816 (34.4) | 939 (37.5) |
| Diabetes mellitus | 3693 (32.2) | 382 (27.7) | 443 (30.8) | 592 (34.1) | 679 (33.3) | 785 (33.1) | 812 (32.4) |
| Hypertension | 6188 (53.9) | 653 (47.4) | 739 (51.3) | 961 (55.4) | 1118 (54.9) | 1314 (55.4) | 1403 (56.0) |
| Cause of arrest (%) | |||||||
| Nontrauma | 11 073 (96.6) | 1330 (96.6) | 1403 (97.4) | 1681 (96.8) | 1979 (97.2) | 2275 (95.9) | 2405 (96.1) |
| Presumed cardiac | 7848 (68.5) | 1064 (77.3) | 1003 (69.7) | 1166 (67.2) | 1386 (68.0) | 1552 (65.4) | 1677 (67.0) |
| Respiratory | 594 (5.2) | 82 (6.0) | 129 (9.0) | 93 (5.4) | 86 (4.2) | 104 (4.4) | 100 (4.0) |
| Drowning | 82 (0.7) | 11 (0.8) | 10 (0.7) | 10 (0.6) | 16 (0.8) | 14 (0.6) | 21 (0.8) |
| Electrocution | 13 (0.1) | 2 (0.1) | 2 (0.1) | 3 (0.2) | 2 (0.1) | 1 (0.0) | 3 (0.1) |
| Other | 2536 (22.1) | 171 (12.4) | 259 (18.0) | 409 (23.6) | 489 (24.0) | 604 (25.5) | 604 (24.1) |
| Trauma | 391 (3.4) | 47 (3.4) | 37 (2.6) | 55 (3.2) | 58 (2.8) | 97 (4.1) | 97 (3.9) |
| Missing | 1 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) |
IQR indicates interquartile range.
Prehospital and Hospital Characteristics
Considering prehospital and hospital resuscitation characteristics (Table 2), bystander CPR rates increased from 21.9% in 2011 to 56.3% in 2016. Bystander AED rates increased from 1.8% to 4.6%. Prehospital advanced airway and prehospital adrenaline administration increased from 82.6% to 85.3% and 46.2% to 60.1%, respectively. The average EMS response time improved slightly from 8:22 minutes in 2011 to 8:13 minutes in 2016. Age‐adjusted incidence rates for all EMS‐treated OHCA increased from 25.6 in 2011 to 38.2 per 100 000 population in 2016. Similarly, age adjusted for OHCA cases with initial shockable rhythm also increased from 4.8 in 2011 to 7.0 per 100 000 population in 2016. Postarrest resuscitation care in the hospital such as initiation of therapeutic hypothermia increased from 1.2% in 2011 to 5.3% in 2016.
Table 2.
Prehospital and Hospital Characteristics
| Variables, n (%) | All (n=11 465) | 2011 (n=1377) | 2012 (n=1440) | 2013 (n=1736) | 2014 (n=2037) | 2015 (n=2372) | 2016 (n=2503) |
|---|---|---|---|---|---|---|---|
| Bystander CPR | 5244 (45.7) | 302 (21.9) | 472 (32.8) | 744 (42.9) | 1031 (50.6) | 1284 (54.1) | 1411 (56.3) |
| Bystander AED applied | 378 (3.3) | 24 (1.8) | 27 (1.9) | 43 (2.5) | 73 (3.6) | 96 (4.1) | 115 (4.6) |
| Bystander defibrillation | 157 (1.4) | 11 (0.8) | 16 (1.1) | 22 (1.3) | 25 (1.2) | 37 (1.6) | 46 (1.8) |
| Arrest witnessed by | |||||||
| EMS/private ambulance | 994 (8.7) | 112 (8.1) | 121 (8.4) | 138 (7.9) | 155 (7.61) | 216 (9.1) | 252 (10.1) |
| Bystander | 5991 (52.3) | 775 (56.3) | 716 (49.7) | 881 (50.8) | 1082 (53.1) | 1271 (53.6) | 1266 (50.6) |
| Not witnessed | 4480 (39.1) | 490 (35.6) | 603 (41.9) | 717 (41.3) | 800 (39.3) | 885 (37.3) | 985 (39.4) |
| Initial arrest rhythm | |||||||
| Nonshockable rhythm | 9276 (80.9) | 1114 (80.9) | 1144 (79.4) | 1405 (80.9) | 1651 (81.1) | 1941 (81.8) | 2021 (80.7) |
| Shockable rhythm | 1995 (17.4) | 251 (18.2) | 280 (19.4) | 304 (17.5) | 347 (17.0) | 378 (15.9) | 435 (17.4) |
| Missing | 194 (1.7) | 12 (0.9) | 16 (1.1) | 27 (1.6) | 39 (1.9) | 53 (2.2) | 47 (1.9) |
| Prehospital advanced airway | 9764 (85.3) | 1132 (82.6) | 1201 (83.7) | 1515 (87.3) | 1751 (85.9) | 2031 (85.6) | 2134 (85.3) |
| Prehospital drug administration | 6108 (53.3) | 634 (46.2) | 696 (48.5) | 871 (50.2) | 1056 (51.8) | 1347 (56.8) | 1504 (60.1) |
| Response time in min, median (IQR) | 08:22 (06:29–10:44) | 07:42 (05:51–10:15) | 08:09 (06:15–10:36) | 08:05 (06:08–10:50) | 09:05 (07:08–11:28) | 08:32 (06:47–10:44) | 08:13 (06:26–10:23) |
| Response time | |||||||
| ≤8 min | 5105 (45.2) | 729 (52.9) | 705 (49.0) | 849 (48.9) | 712 (35.0) | 1019 (43.0) | 1091 (46.8) |
| >8 min | 6186 (54.8) | 648 (47.1) | 735 (51.0) | 887 (51.1) | 1325 (65.0) | 1353 (57.0) | 1238 (53.2) |
| Age‐adjusted incidence rates (per 100 000 pop.) | |||||||
| All EMS treated (resuscitation attempted) | 25.6 (n=1363) | 26.0 (n=1421 | 29.4 (n=1714) | 32.8 (n=2002) | 36.9 (n=2321) | 38.2 (n=2470) | |
| Initial shockable rhythm | 4.8 (n=251) | 5.1 (n=280) | 5.3 (n=304) | 5.8 (n=347) | 6.2 (n=378) | 7.0 (n=435) | |
| Hospital interventions | |||||||
| ECMO therapy | 31 (0.3) | 1 (0.1) | 0 (0) | 1 (0.1) | 11 (0.5) | 9 (0.4) | 9 (0.4) |
| Hypothermia therapy | 485 (4.2) | 17 (1.2) | 23 (1.6) | 61 (3.5) | 117 (5.7) | 135 (5.7) | 132 (5.3) |
AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenation; EMS, emergency medical services; and IQR, interquartile range.
Clinical Outcomes
EMS and hospital outcomes are presented in Table 3. Prehospital return of spontaneous circulation improved from 4.6% in 2011 to 12.5% in 2016 (P<0.001). Overall survival rates improved over the years from 3.5% in 2011 to 6.5% in 2016 (P<0.001). Of those who survived to discharge, 67.7% had good neurological function upon discharge in 2016 compared with 52.1% in 2011 (P=0.007). Survival outcomes stratified by sex and initial arrest rhythm did not show statistical significance during the study period (P=0.636 and P=0.621, respectively). Utstein survival rates nearly doubled from 11.6% in 2011 to 23.1% (P=0.006). However, good neurological function upon discharge for this group was not statistically significant (P=0.591).
Table 3.
Clinical Outcomes (All and by Year)
| Characteristic, n (%) | All (n=11 465) | 2011 (n=1377) | 2012 (n=1440) | 2013 (n=1736) | 2014 (n=2037) | 2015 (n=2372) | 2016 (n=2503) | P Value |
|---|---|---|---|---|---|---|---|---|
| Outcomes (overall) | ||||||||
| ROSC at scene | 391 (8.1) | 63 (4.6) | 86 (6.0) | 113 (6.5) | 148 (7.3) | 208 (8.8) | 312 (12.5) | <0.001 |
| ROSC at ED | 3210 (28.0) | 374 (27.2) | 400 (27.8) | 509 (29.3) | 593 (29.1) | 684 (28.8) | 650 (26.0) | <0.001 |
| Survival to admission | 2111 (18.4) | 251 (18.2) | 249 (17.3) | 303 (17.5) | 358 (17.6) | 453 (19.1) | 497 (19.9) | 0.175 |
| Survival to discharge | 545 (4.8) | 48 (3.5) | 53 (3.7) | 73 (4.2) | 83 (4.1) | 125 (5.3) | 163 (6.5) | <0.001 |
| Good‐to‐moderate neurological function (of those discharged alive) | 343 (63.4) | 25 (52.1) | 33 (63.5) | 36 (49.3) | 63 (75.9) | 77 (62.1) | 109 (67.7) | 0.007 |
| Outcomes (Utstein) | n=1315 | n=173 | n=172 | n=210 | n=229 | n=241 | n=290 | |
| Utstein survival | 228 (17.3) | 20 (11.6) | 23 (13.4) | 32 (15.2) | 35 (15.3) | 51 (21.2) | 67 (23.1) | 0.006 |
| Good‐to‐moderate neurological function (of those discharged alive) | 152 (66.7) | 12 (60.0) | 14 (60.9) | 18 (56.3) | 24 (68.6) | 35 (68.6) | 49 (73.1) | 0.591 |
| Survival to discharge—sex | n=545 | n=48 | n=53 | n=73 | n=83 | n=125 | n=163 | 0.636 |
| Male | 422 (77.4) | 36 (75.0) | 38 (71.7) | 53 (72.6) | 64 (77.1) | 100 (80.0) | 131 (80.4) | |
| Female | 123 (22.6) | 12 (25.0) | 15 (28.3) | 20 (27.4) | 19 (22.9) | 25 (20.0) | 32 (19.6) | |
| Survival to discharge—initial arrest rhythm | 0.621 | |||||||
| Nonshockable rhythm | 174 (31.9) | 12 (25.0) | 15 (28.3) | 25 (34.2) | 21 (25.3) | 48 (38.4) | 53 (32.5) | |
| Shockable rhythm | 357 (65.5) | 35 (72.9) | 37 (69.8) | 47 (64.4) | 58 (69.9) | 75 (60.0) | 105 (64.4) | |
| Missing | 14 (2.6) | 1 (2.1) | 1 (1.9) | 1 (1.4) | 4 (4.8) | 2 (1.6) | 5 (3.1) | |
ED indicates emergency department; and ROSC, return of spontaneous circulation.
Factors Associated With Overall Survival
On logistic regression (Table 4), the factors significantly associated with survival‐to‐discharge or 30‐day postarrest were age ≤65 years old (adjusted odds ratio [aOR] 0.64 for >65 years old, 95% CI, [95% CI, 0.52–0.80]), nonresidential location (aOR 0.61 for residential location, 95% CI, 0.49–0.75), EMS witnessed (aOR 7.23; 95% CI, 4.98–10.49), bystander witnessed (aOR 2.14; 95% CI, 1.61–2.85), shockable rhythm (aOR 10.18; 95% CI, 8.17–12.69), bystander AED (aOR 1.99; 95% CI, 1.40–2.85), and year 2016 (aOR 1.63; 95% CI, 1.13–2.36).
Table 4.
Logistic Regression for Overall Survival to Discharge
| Characteristic (N=11 465) | Crude OR (95% CI) | Global P Value | P Value | Adjusted OR (95% CI) | Global P Value | P Value |
|---|---|---|---|---|---|---|
| Age | ||||||
| ≤65 y | Ref | Ref | ||||
| >65 y | 0.39 (0.33– 0.47) | <0.001 | 0.64 (0.52– 0.80) | <0.001 | ||
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 0.52 (0.43– 0.64) | <0.001 | 1.06 (0.83– 1.35) | 0.661 | ||
| Location type | ||||||
| Nonresidential | Ref | Ref | ||||
| Residential | 0.28 (0.24, 0.34) | <0.001 | 0.61 (0.49– 0.75) | <0.001 | ||
| Arrest witnessed | <0.001 | <0.001 | ||||
| Not witnessed | Ref | Ref | ||||
| EMS/private ambulance | 6.05 (4.50– 8.14) | <0.001 | 7.23 (4.98–10.49) | <0.001 | ||
| Bystander | 3.33 (2.61– 4.23) | <0.001 | 2.14 (1.61– 2.85) | <0.001 | ||
| Initial arrest rhythm | ||||||
| Nonshockable rhythm | Ref | Ref | ||||
| Shockable rhythm | 13.82 (11.31– 16.89) | <0.001 | 10.18 (8.17– 12.69) | <0.001 | ||
| Bystander CPR | ||||||
| No | Ref | Ref | ||||
| Yes | 1.53 (1.28– 1.81) | <0.001 | 1.27 (0.99– 1.62) | 0.058 | ||
| Bystander AED | ||||||
| No | Ref | Ref | ||||
| Yes | 4.49 (3.37– 5.97) | <0.001 | 1.99 (1.40– 2.85) | <0.001 | ||
| Response time ≤8 min | ||||||
| No | Ref | Ref | ||||
| Yes | 1.10 (0.92– 1.31) | 0.281 | 1.05 (0.86–1.28) | 0.623 | ||
| Year | <0.01 | 0.01 | ||||
| 2011 | Ref | Ref | ||||
| 2012 | 1.06 (0.71– 1.57) | 0.781 | 1.01 (0.66– 1.55) | 0.956 | ||
| 2013 | 1.22 (0.84– 1.76) | 0.303 | 1.21 (0.81– 1.80) | 0.354 | ||
| 2014 | 1.18 (0.82– 1.69) | 0.380 | 1.03 (0.69– 1.54) | 0.888 | ||
| 2015 | 1.54 (1.10– 2.16) | 0.013 | 1.39 (0.95– 2.01) | 0.094 | ||
| 2016 | 1.93 (1.39– 2.68) | <0.001 | 1.63 (1.13–2.36) | 0.009 | ||
Global P value=Wald test. Missing variables: initial arrest rhythm—194 (1.69); bystander AED—96 (0.84); response time—174 (1.52). AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; and OR, odds ratio.
Age‐Standardized Incidence and Survival Rates
Figure 1 shows the yearly crude and age‐standardized incidence rate. In 2016, the age‐standardized incidence rate for OHCA was 39.2 per 100 000 populations. Stratified by age, while incidence rate among people aged <65 years remained relatively low (2.0 per 10 000 population in 2011; 3.0 in 2016), there was a greater increase among people aged >65 years (19.6 cases per 10 000 population in 2011; 29.9 in 2016). Males overall had a much higher age‐standardized incidence rate in 2016 (54.9 per 100 000) compared with females (23.6 per 100 000).
Figure 1. Yearly crude and age‐standardized incidence rates.
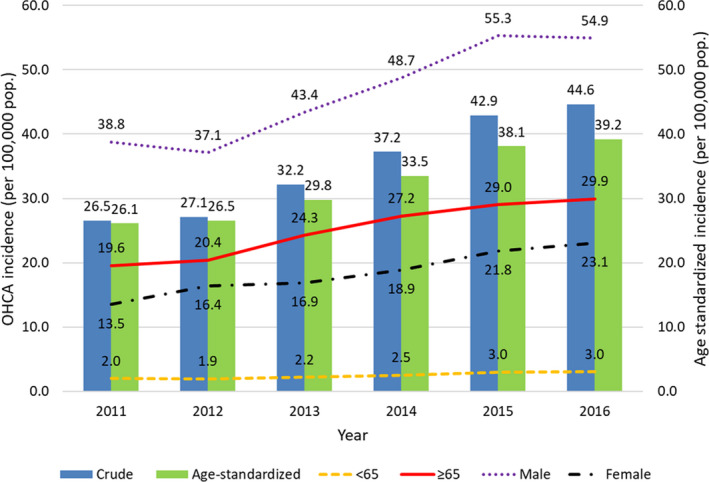
OHCA indicates out‐of‐hospital cardiac arrest.
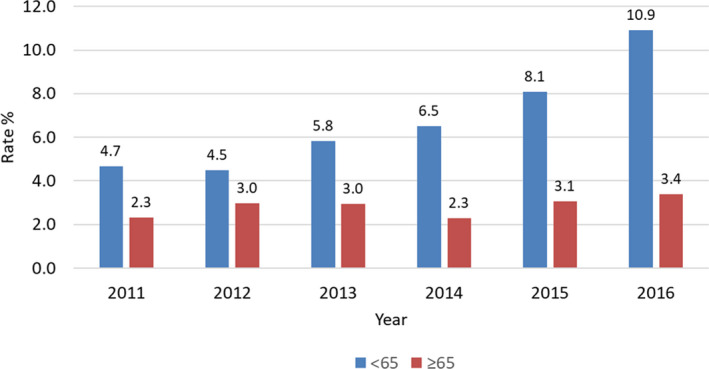
Figure 2 shows the trend of age‐standardized survival rates between age groups. Among younger OHCA (age ≤65 years) the survival rate increased from 4.7% to 10.9%. Survival rates among older OHCA (age >65 years) remained consistently low: 2.3% in 2011 to 3.4% in 2016. Over the same period, age‐standardized survival rates significantly increased from 2.9% in 2011 to 12.0% in 2016.
Figure 2. Age‐standardized survival rates by age groups.
Discussion
This prospective, observational, national registry study of OHCA in Singapore showed a doubling in national Utstein survival from 2011 to 2016. This was associated with increased rates of bystander CPR and bystander AED, and temporally associated with a series of community and prehospital interventions to improve OHCA survival under a national strategic 5‐year Plan.
The pace of improvement in outcomes observed in our cohort is significant, and outpaced the majority of published reports. For example, the Swedish Cardiac Arrest Register showed an increase in 30‐day survival from 4.8% to 10.7% (and for shockable rhythms, 12.7%–31.6%), and achieved this over a 10‐year period from 1992 to 2011. 14 A similar study of 9 cities in Oregon showed an increase in 30‐day survival from 6.7% to 18.2% (and for Utstein survival, from 14.3% to 31.3%), and achieved this over 15 years from 1998 to 2013. 27 Other communities have also reported rapid improvement in Utstein survival such as Toronto, Canada (16%–31% from 2006 to 2013), 16 Chicago, Illinois (16.3%–35.4% from 2013 to 2016), 28 and Detroit, Michigan (12.5%–18.2% from 2014 to 2016). 28 The focus on community training and EMS (particularly dispatcher) interventions appear to have been a common factor.
Increased rates of bystander CPR and public access defibrillation improve survival. 27 , 29 The role of the community and emergency medical dispatch in coordination of bystander CPR and early defibrillation is increasingly recognized. 27 In a landmark study, the OPALS (Ontario Prehospital Advanced Life Support) study investigators found bystander CPR to be the most important modifiable factor for survival. 30 In our study, bystander CPR rates more than doubled after implementation of dispatcher assistance‐CPR. Dispatcher assistance‐CPR recruits the dispatch center in the crucial tasks of early identification of OHCA, and giving just‐in‐time education and persuasion to callers to facilitate bystander CPR. Studies suggest advantages over large‐scale community training, which often have not achieved large increases in CPR rates because of high costs to the system, difficulty in identifying OHCA, fear of causing harm, and reluctance to perform mouth‐to‐mouth ventilation. 29 , 31 , 32 In our cohort, response times improved slightly with survival. Indeed, reduction of ambulance response time is challenging for most EMS systems and might not be a cost‐effective target. Our results suggest that a focus on proven and cost‐effective strategies to strengthen the chain of survival, particularly in the community, ambulances, and dispatch, is essential for developing EMS systems.
Singapore has a fairly recently developed EMS system. 33 , 34 Having a single national EMS provider in a compact, highly urbanized setting is ostensibly advantageous in terms of policy implementation, monitoring, and enforcement. At the same time, there are unique challenges such as those resulting from high‐rise buildings where there is the need to navigate tight corridors and administer CPR in elevators. 35 , 36 Certainly, every EMS system has unique circumstances and challenges that need to be considered in planning interventions.
The large increase (73%) in OHCA incidence over 5 years observed in this study is likely multifactorial: the population is still growing (5.18 million in 2011 to 5.6 in 2017), there is an aging population, an increased awareness of the population resulting in more EMS calls and resuscitation attempted, and better reporting. The proportion of ethnic groups appears comparable with the total population in Singapore.
This study has several limitations. First, we did not have data on some possible postresuscitation care practice changes such as coronary angiography, percutaneous coronary intervention, or intensive care unit bundles that have been suggested to affect survival. 37 These may be potential confounders in the logistic regression for survival. The presence of unmeasured confounders is suggested by how “year of resuscitation” remained independently associated with outcome despite correction for major prognostic factors.
Secondly, there were missing prehospital timings in cases conveyed by private transportation or private ambulances. However, these comprised only ≈2% of cases.
Thirdly, we used survival‐to‐discharge instead of functional outcomes as the end point. This is because cerebral performance score at discharge and whether the survivors were discharged to care facilities were not consistently available. Also, because of the small population size and low proportion of neurologically intact survivors, there was insufficient power to meaningfully test these outcomes in the Utstein cohort.
Lastly, given the observational design, while there was strong temporal association and plausibility, findings are ecological and do not prove causality between interventional programs and survival benefit. Multiple initiatives that overlapped in timeline made it difficult to make clear inferences on the effect on survival.
Conclusions
Utstein survival for OHCA in Singapore doubled from 2011 to 2016, along with corresponding increases in bystander CPR and bystander AED. These improvements occurred during a period when a series of national community and EMS initiatives were implemented to improve OHCA outcomes under a national 5‐year Plan.
Appendix
Singapore PAROS Investigators
Dr Ling Tiah, Accident & Emergency, Changi General Hospital, Singapore; Dr Wei Ming Ng, Emergency Medicine Department, Ng Teng Fong General Hospital, Singapore; Dr Wei Ling Tay, Emergency Medicine Department, Ng Teng Fong General Hospital, Singapore; Dr Shir Lynn Lim, Department of Cardiology, National University Heart Centre Singapore, Singapore.
Details of Interventions
In May 2011, mechanical CPR devices were deployed in SCDF ambulances, initially as a pragmatic cluster‐randomized prehospital trial comparing LUCAS 2 (Physio‐Control, Redmond, WA) with manual CPR. Subsequently, LUCAS 2 was rolled out to all ambulances as standard procedure for all eligible OHCA cases. In April 2012, the Fire Bikers Scheme was implemented where in times of traffic congestion, fire/rescue specialists on a motorcycle trained in CPR/AED were dispatched ahead of an ambulance. In July 2012, Singapore implemented a comprehensive dispatcher‐assisted CPR (DA‐CPR) protocol comprising of dispatcher training focused on communication and persuasion, review of audio recordings of all OHCA calls, feedback to dispatchers, and public education. After a planned six‐month “run‐in” program, all dispatchers were able to provide DA‐CPR.
In April 2014, a community‐based Dispatcher‐Assisted first REsponder (DARE) training initiative, which simulates a rescuer‐dispatcher sequence that is initiated by a call to ‘995’ was implemented. This was developed to be an abbreviated (45 minutes) course including a video and instructor‐led hands‐on manikin session with hands‐only CPR, and was administered to groups of school‐children or other laypersons. DARE program has since trained over 50,000 providers.
In August 2014, intraosseous (IO) access was introduced to ambulances as part of a cluster‐randomized prehospital trial. This was used in OHCA cases for administration of adrenaline when intravenous access (IV) attempts had failed. Unpublished data (under review) showed that IO use when IV failed led to a higher rate of vascular access and faster adrenaline administration.
In April 2015, Save‐A‐Life (SAL) initiative was developed by SCDF, in collaboration with Singapore Heart Foundation and Ministry of Health Singapore to improve community first response to cardiac arrest cases in residential areas. SAL initiative involves installation of an AED in the lift lobby of every two public housing apartment block in Singapore. Installation of AEDs were done in phases and first phase began in July 2015. By end of 2016, total number of AEDs installed were 360. In the same month, a mobile phone application known as myResponder app was implemented to allow community responders to register and receive alerts from SCDF’s dispatch center if a potential cardiac arrest case occurs within 400 meters of their vicinity.
Sources of Funding
This study was supported by grants from National Medical Research Council, Clinician Scientist Awards, Singapore (NMRC/CSA/024/2010 and NMRC/CSA/0049/2013), National Medical Research Council (NMRC/CS_Seedfd/012/2018), Ministry of Health, Health Services Research Grant, Singapore (HSRG/0021/2012), and Khoo Clinical Scholars Programme, Khoo Pilot Award (KP/2019/0034), Duke‐NUS Medical School.
Disclosures
Ong reports funding from the Zoll Medical Corporation for a study involving mechanical cardiopulmonary resuscitation devices; grants from the Laerdal Foundation, Laerdal Medical, and Ramsey Social Justice Foundation for funding of the Pan‐Asian Resuscitation Outcomes Study; an advisory relationship with Global Healthcare SG, a commercial entity that manufactures cooling devices; and funding from Laerdal Medical on an observation program to their Community CPR Training Centre Research Program in Norway. Ong has a licensing agreement and patent filed (Application no: 13/047,348) with ZOLL Medical Corporation for a study titled “Method of predicting acute cardiopulmonary events and survivability of a patient.” The remaining authors have no disclosures to report.
Supporting information
Supplementary Material
Acknowledgments
The authors would like to thank the late Susan Yap and Pek Pin Pin from Department of Emergency Medicine, Singapore General Hospital; Nurul Asyikin and Joann Poh from Unit for Prehospital Emergency Care, Singapore General Hospital and SingHealth Emergency Medicine Academic Clinical Programme for their support and contributions to the study.
(J. Am. Heart Assoc. 2020;9:e015368 DOI: 10.1161/JAHA.119.015368.)
This work was presented as an oral presentation at the International Conference on Emergency Medicine, June 12 to 15, 2019, in Seoul, South Korea.
For Sources of Funding and Disclosures, see page 10.
Contributor Information
Andrew Fu Wah Ho, Email: sophronesis@gmail.com.
for the Singapore Pan‐Asian Resuscitation Outcomes Study (PAROS) investigators:
REFERENCES
- 1. Ong MEH, Perkins GD, Cariou A. Out‐of‐hospital cardiac arrest: prehospital management. Lancet. 2018;391:980–988. [DOI] [PubMed] [Google Scholar]
- 2. Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, et al. Regional variation in out‐of‐hospital cardiac arrest incidence and outcome. J Am Med Assoc. 2008;300:1423–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ong ME, Shin SD, De Souza NN, Tanaka H, Nishiuchi T, Song KJ, Ko PC, Leong BS, Khunkhlai N, Naroo GY, et al. Outcomes for out‐of‐hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation. 2015;96:100–108. [DOI] [PubMed] [Google Scholar]
- 4. Ong ME, Cho J, Ma MH, Tanaka H, Nishiuchi T, Al Sakaf O, Abdul Karim S, Khunkhlai N, Atilla R, Lin CH, et al. Comparison of emergency medical services systems in the Pan‐Asian resuscitation outcomes study countries: report from a literature review and survey. Emerg Med Australas. 2013;25:55–63. [DOI] [PubMed] [Google Scholar]
- 5. Shin SD, Ong ME, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, Karim SA, Khunkhlai N, Lin CH, Song KJ, et al. Comparison of emergency medical services systems across Pan‐Asian countries: a Web‐based survey. Prehosp Emerg Care. 2012;16:477–496. [DOI] [PubMed] [Google Scholar]
- 6. Lai H, Choong CV, Fook‐Chong S, Ng YY, Finkelstein EA, Haaland B, Goh ES, Leong BS, Gan HN, Foo D, et al. Interventional strategies associated with improvements in survival for out‐of‐hospital cardiac arrests in Singapore over 10 years. Resuscitation. 2015;89:155–161. [DOI] [PubMed] [Google Scholar]
- 7. Eng Hock Ong M, Chan YH, Anantharaman V, Lau ST, Lim SH, Seldrup J. Cardiac arrest and resuscitation epidemiology in Singapore (CARE I study). Prehosp Emerg Care. 2003;7:427–433. [DOI] [PubMed] [Google Scholar]
- 8. Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the "chain of survival" concept. A statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation. 1991;83:1832–1847. [DOI] [PubMed] [Google Scholar]
- 9. Chong SL, Laerdal T, Cordero J, Khursheed M, Haedar A, Cai W, Nadarajan GD, Ho AFW, Pek PP, Chan SKT, et al. Global resuscitation alliance consensus recommendations for developing emergency care systems: reducing perinatal mortality. Resuscitation. 2018;133:71–74. [DOI] [PubMed] [Google Scholar]
- 10. Nadarajan GD, Tiah L, Ho AFW, Azazh A, Castren MK, Chong SL, El Sayed MJ, Hara T, Leong BS, Lippert FK, et al. Global resuscitation alliance utstein recommendations for developing emergency care systems to improve cardiac arrest survival. Resuscitation. 2018;132:85–89. [DOI] [PubMed] [Google Scholar]
- 11. Hassager C, Nagao K, Hildick‐Smith D. Out‐of‐hospital cardiac arrest: in‐hospital intervention strategies. Lancet. 2018;391:989–998. [DOI] [PubMed] [Google Scholar]
- 12. Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- 13. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang‐Jensen T, Olesen JB, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA. 2013;310:1377–1384. [DOI] [PubMed] [Google Scholar]
- 14. Strömsöe A, Svensson L, Axelsson ÅB, Claesson A, Göransson KE, Nordberg P, Herlitz J. Improved outcome in Sweden after out‐of‐hospital cardiac arrest and possible association with improvements in every link in the chain of survival. Eur Heart J. 2015;36:863–871. [DOI] [PubMed] [Google Scholar]
- 15. Blom MT, Beesems SG, Homma PC, Zijlstra JA, Hulleman M, van Hoeijen DA, Bardai A, Tijssen JG, Tan HL, Koster RW. Improved survival after out‐of‐hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868–1875. [DOI] [PubMed] [Google Scholar]
- 16. Buick JE, Drennan IR, Scales DC, Brooks SC, Byers A, Cheskes S, Dainty KN, Feldman M, Verbeek PR, Zhan C, et al. Improving temporal trends in survival and neurological outcomes after out‐of‐hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2018;11:e003561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chan PS, McNally B, Tang F, Kellermann A; CARES Surveillance Group . Recent trends in survival from out‐of‐hospital cardiac arrest in the United States. Circulation. 2014;130:1876–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Anantharaman V. Developing resuscitation programmes in the community: the tasks ahead for the National Resuscitation Council. Singapore Med J. 2011;52:634–641. [PubMed] [Google Scholar]
- 19. Department of Statistics Singapore . Available at: http://www.singstat.gov.sg/statistics/latest_data.html#14. Accessed June 11, 2018.
- 20. Ong ME, Quah JL, Ho AF, Yap S, Edwin N, Ng YY, Goh ES, Leong BS, Gan HN, Foo DC. National population‐based survey on the prevalence of first aid, cardiopulmonary resuscitation and automated external defibrillator skills in Singapore. Resuscitation. 2013;84:1633–1636. [DOI] [PubMed] [Google Scholar]
- 21. Singapore Civil Defence Force . Annual report. Available at: https://www.scdf.gov.sg/home/about‐us/media‐room/publications/annual‐reports. Accessed June 8, 2020.
- 22. Goh ES, Liang B, Fook‐Chong S, Shahidah N, Soon SS, Yap S, Leong B, Gan HN, Foo D, Tham LP, et al. Effect of location of out‐of‐hospital cardiac arrest on survival outcomes. Ann Acad Med Singapore. 2013;42:437–444. [PubMed] [Google Scholar]
- 23. Lian TW, Allen JC, Ho AFW, Lim SH, Shahidah N, Ng YY, Doctor N, Leong BSH, Gan HN, Mao DR, et al. Effect of vertical location on survival outcomes for out‐of‐hospital cardiac arrests in Singapore. Resuscitation. 2019;139:24–32. [DOI] [PubMed] [Google Scholar]
- 24. Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, Bossaert L, Delooz HH, Dick WF, Eisenberg MS, et al. Recommended guidelines for uniform reporting of data from out‐of‐hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–975. [DOI] [PubMed] [Google Scholar]
- 25. McNally B, Stokes A, Crouch A, Kellermann AL. CARES: cardiac arrest registry to enhance survival. Ann Emerg Med. 2009;54:674–683.e2. [DOI] [PubMed] [Google Scholar]
- 26. World Health Organization . Age standardization of rates: a new WHO standard. Available at: www.who.int/healthinfo/paper31.pdf. Accessed June 11, 2018.
- 27. Tanaka H, Ong MEH, Siddiqui FJ, Ma MHM, Kaneko H, Lee KW, Kajino K, Lin CH, Gan HN, Khruekarnchana P, et al. Modifiable factors associated with survival after out‐of‐hospital cardiac arrest in the Pan‐Asian resuscitation outcomes study. Ann Emerg Med. 2018;71:608–617.e15. [DOI] [PubMed] [Google Scholar]
- 28. May S, Zhang L, Foley D, Brennan E, O'Neil B, Bork E, Levy P, Dunne R. Improvement in non‐traumatic, out‐of‐hospital cardiac arrest survival in Detroit from 2014 to 2016. J Am Heart Assoc. 2018;7:e009831 DOI: 10.1161/JAHA.118.009831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kragholm K, Wissenberg M, Mortensen RN, Hansen SM, Malta Hansen C, Thorsteinsson K, Rajan S, Lippert F, Folke F, Gislason G, et al. Bystander efforts and 1‐year outcomes in out‐of‐hospital cardiac arrest. N Engl J Med. 2017;376:1737–1747. [DOI] [PubMed] [Google Scholar]
- 30. Stiell IG, Wells GA, DeMaio VJ, Spaite DW, Field BJ III, Munkley DP, Lyver MB, Luinstra LG, Ward R. Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario Prehospital Advanced Life Support. Ann Emerg Med. 1999;33:44–50. [DOI] [PubMed] [Google Scholar]
- 31. Nichol G, Laupacis A, Stiell IG, O'Rourke K, Anis A, Bolley H, Detsky AS. Cost‐effectiveness analysis of potential improvements to emergency medical services for victims of out‐of‐hospital cardiac arrest. Ann Emerg Med. 1996;27:711–720. [DOI] [PubMed] [Google Scholar]
- 32. Dami F, Carron PN, Praz L, Fuchs V, Yersin B. Why bystanders decline telephone cardiac resuscitation advice. Acad Emerg Med. 2010;17:1012–1115. [DOI] [PubMed] [Google Scholar]
- 33. Lim SH, Anantharaman V. Emergency medicine in Singapore: past, present, and future. Ann Emerg Med. 1999;33:338–343. [DOI] [PubMed] [Google Scholar]
- 34. Ho AF, Chew D, Wong TH, Ng YY, Pek PP, Lim SH, Anantharaman V, Hock Ong ME. Prehospital trauma care in Singapore. Prehosp Emerg Care. 2015;19:409–415. [DOI] [PubMed] [Google Scholar]
- 35. Lateef F, Anantharaman V. Delays in the EMS response to and the evacuation of patients in high‐rise buildings in Singapore. Prehosp Emerg Care. 2000;4:327–332. [DOI] [PubMed] [Google Scholar]
- 36. Drennan IR, Strum RP, Byers A, Buick JE, Lin S, Cheskes S, Hu S, Morrison LJ; Rescu Investigators . Out‐of‐hospital cardiac arrest in high‐rise buildings: delays to patient care and effect on survival. Can Med Assoc J. 2016;188:413–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Spaite DW, Bobrow BJ, Stolz U, Berg RA, Sanders AB, Kern KB, Chikani V, Humble W, Mullins T, Stapczynski JS, et al. Statewide regionalization of postarrest care for out‐of‐hospital cardiac arrest: association with survival and neurologic outcome. Ann Emerg Med. 2014;64:496–506.e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


