Abstract
The progressive accumulation of apoptosis-resistant and secretory active senescent cells (SCs) in animal and human aged tissues may limit lifespan and healthspan and lead to age-related diseases such as cancer, neurodegenerative disorders, and metabolic syndrome. Thus, SCs are suggested targets in anti-aging therapy. In the last two decades, a number of nanomaterials have gained much attention as innovative tools in theranostic applications due to their unique properties improving target visualization, drug and gene delivery, controlled drug release, effective diagnosis, and successful therapy. Although the healthcare industry has focused on a plethora of applications of nanomaterials, it remains elusive how nanomaterials may modulate cellular senescence, a hallmark of aging. In this review paper, we consider novel nanotechnology-based strategies for healthspan promotion and the prevention of age-related dysfunctions that are based on the delivery of therapeutic compounds capable to preferentially killing SCs (nano-senolytics) and/or modulating a proinflammatory secretome (nano-senomorphics/nano-senostatics). Recent examples of SC-targeted nanomaterials and the mechanisms underlying different aspects of the nanomaterial-mediated senolysis are presented and discussed.
Keywords: nanomaterials, cellular senescence, senotherapy, senolytics, nanotherapeutic-mediated senolysis
1. Cellular Senescence
Cellular senescence (CS) is characterized by a state of permanent cell growth arrest with altered metabolic features (e.g., affected glycolysis, mitochondrial function, and autophagic flux), modified protein secretion, and biomolecular damage that occurs in response to stressful stimuli [1,2]. CS was originally described in 1961 by Hayflick and colleagues, who observed that normal diploid embryonic fibroblasts had a limited ability to proliferate in an in vitro culture [3]. Based on these results, Hayflick coined the term replicative senescence to describe this phenomenon. Subsequently, progressive telomere shortening promoting DNA damage response (DDR) has been recognized as one of the major determinants of replicative senescence [4,5]. Later, the presence of senescent cells (SCs) in aging tissues that linked cellular senescence with organismal aging was documented [6]. Cells can also prematurely activate the senescence program upon treatment with stress stimuli such as UV radiation, oxidants, or DNA-damaging agents [7,8]. This process is known as stress-induced premature senescence (SIPS) [9]. Moreover, the expression of oncogenes could trigger senescence prematurely, in a process called oncogene-induced senescence (OIS) [10]. Cellular senescence may be considered as a tumor suppression mechanism by blocking the proliferation and division of cells with unrepaired DNA damage to prevent their stepwise malignant propagation [11]. However, it has also been demonstrated that cellular senescence may participate in other physiological processes such as specific tissue remodeling (so-called developmentally-programmed senescence) that acts in a damage-independent manner during embryonic development and wound healing in adulthood [12,13]. Despite the protective role of cellular senescence during stress-induced cellular responses, it is commonly accepted that CS may promote aging and contribute to the development of age-related diseases. Namely, it has been revealed that diverse pathological conditions associated with accelerated aging such as cancer, neurodegenerative diseases, cardiovascular disorders, and progeroid and metabolic syndromes are accompanied by the accumulation of SCs and cellular senescence may be a causative factor for the progression of age-related pathologies [14,15,16,17,18,19].
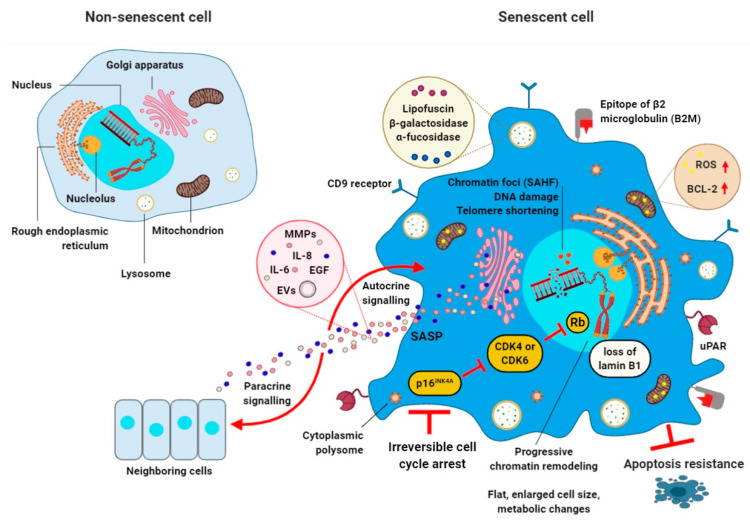
Many different molecular pathways have been proven to contribute to cellular senescence [20,21]. However, one of common features of all SCs is irreversible cell-cycle arrest regulated by p53/p21WAF1/Cip1 and p16INK4A/RB (retinoblastoma) tumor-suppressor pathways, which can interact with each other or act independently [2]. Unlike quiescent cells (the cells at the G0 phase) or terminally-differentiated cells, SCs do not respond to growth and mitogenic stimuli, thus they are irreversibly withdrawn from the cell cycle [17,22]. Two cell-cycle inhibitors that are often overexpressed in SCs, namely p21WAF1/Cip1 (encoded by CDKN1a gene) and p16INK4A (encoded by CDKN2a gene) are crucial mediators of senescence. Accumulation of these cyclin-dependent kinase inhibitors (CDKI) resulted in permanent activation of RB family proteins, inhibition of E2F family transcription factor activity, and finally cell-cycle arrest [20].
SCs display common features such as granularity, increased activity of lysosomal senescence-associated β-galactosidase (SA-β-gal), lipofuscin accumulation, exclusion of proliferative markers, formation of senescence-associated heterochromatin foci (SAHF), and persistent expression of proteins that participate in DDR (Figure 1) [23,24,25]. Moreover, SCs are characterized by senescence-associated secretory phenotype (SASP) [26,27]. The SASP entails secretion of numerous molecules, such as inflammatory chemokines (e.g., MCP-1, MIP 1α, and CCL-16) and cytokines (e.g., IL-6 and IL-8), growth factors (e.g., IGF-1 and EGF) and angiogenic factors/regulators, miRNAs, proteases, and damage-associated molecular patterns (DAMPs), which can induce changes in neighboring cells via both paracrine and autocrine mechanisms [28,29,30,31]. SASP may have both beneficial and pathological functions. First, these factors are suggested to regulate immune clearance of SCs to prevent fibrosis and promote tissue regeneration [1,32,33]. Contrariwise, SASP factors can induce the development of secondary senescence within non-senescent nearby cells [34]. In addition, the SASP is responsible for promotion of low-grade chronic inflammation. This malfunction can alter the tissue microenvironment, which can also stimulate neoplastic cell growth, tumor metastasis, and angiogenesis [35].
Figure 1.
Biomarkers of cellular senescence. Senescent cell (right) is characterized by irreversible cell cycle arrest induced by various stressors (e.g., DNA damage or telomere shortening). Classical features of senescent cells include flat and enlarged cell size, elevated expression of cell cycle inhibitors (such as p16INK4A or p21Cip1), increased nucleus size and multiple nucleoli, lysosomes overexpressing β-galactosidase, α-fucosidase, and lipofuscin, chromatin reorganization based on senescence-associated heterochromatic foci (SAHF) and loss of lamin B1, senescence-associated ribosome biogenesis defects (e.g., “free” cytoplasmic polysomes with ribosomes), the overexpression of anti-apoptotic Bcl-2 family members, reactive oxygen species (ROS) production in mitochondria, and expression of cell surface markers such as CD9 receptor, urokinase-type plasminogen activator receptor (uPAR), and epitope of β2 microglobulin (B2M). A characteristic key feature of cellular senescence is also the manifestation of the senescence-associated secretory phenotype (SASP) via the Golgi apparatus. SASP mediates the autocrine/paracrine activities of senescent cells by the secretion of matrix metalloproteinases (MMPs) such as MMP-3 and MMP-9, growth factors (e.g., epidermal growth factor (EGF)), cytokines and chemokines (e.g., IL-6 and IL-8), miRNAs, activins, and inhibins, lipids (e.g., ceramides), as well as exosome-like small extracellular vesicles (EVs). SASP can modify the microenvironment of senescent cells (SCs) and directly affects neighboring cells. A non-senescent cell is also presented (left).
A recently-proposed strategy to delay symptoms of aging is the suppression of SASP components [36]. Notably, compounds that interfere with the pathways involved in SASP regulation are the most effective. These include nuclear factor (NF)-κB, Janus kinase (JAK)/signal transducer and activator of transcription (STAT), mitogen-activated protein kinase (MAPK), and mammalian target of rapamycin (mTOR) pathways [37]. For example, various drugs have been shown to lower production or secretion of SASP factors. Simvastatin decreases production of interleukins IL-6 and IL-8 in vitro [38]. Natural compounds such as flavonoids have also been documented to impair the secretory phenotype in SCs [39]. Importantly, SASP is not the only mechanism by which SCs modulate their neighboring cells. For example, it has been shown that OIS is accompanied by a dynamic fluctuation of NOTCH1 activity [40], reactive oxygen species (ROS) production [41], or by release of exosomes [42]. Apart from irreversible withdrawal from the cell cycle and SASP, another feature of SCs is their resistance to apoptosis through the multilevel regulated pro-survival senescent cell anti-apoptotic pathways (SCAPs) such as p53/p21/serpins, BCL-2/Bcl-XL, PI3K/AKT/ceramide signaling, the hypoxia-inducible factor (HIF-1α) pathway, or HSP90-dependent networks [24,30,43].
2. Nano-Based Delivery Systems for Diagnostic and Therapeutic Purposes
The applications of nanotechnology to medicine provide an opportunity to improve the safety, efficiency, and sensitivity of conventional medical therapeutics [44]. A nano-based drug delivery system relies on the use of nanostructures and nanomaterials for targeted transport of a therapeutic or diagnostic molecule and for its release in controlled manner [45,46]. In addition, the use of large-size structures in drug delivery is challenging, because of their poor bioavailability and stability, undesirable effects, limited targeted drug delivery, and therapy efficiency [47]. Recently, several approaches to drug delivery have been proposed to minimize these limitations by the development and production of smart nanomaterials. Nanomaterials have attracted widespread attention due to their unique properties such as size (100 nanometers or smaller in at least one dimension), shape, surface area, permeability, and various mechanical, magnetic, optical, and electronic properties [48,49,50,51]. Nanomaterial properties are significant in determining their important pharmacokinetics criteria, such as adsorption, distribution, accumulation, cellular uptake, and excretion mechanisms [52]. Uptake of nano-sized materials by cellular systems may occur via four different basic endocytic mechanisms, namely phagocytosis, macropinocytosis, clathrin-mediated endocytosis, and caveolae-mediated endocytosis [53]. Among the most-often-used nano-sized materials are nanoparticles (NPs), polymers, dendrimers, micelles, liposomes, carbon nanotubes, and fullerenes [52,54]. Moreover, an interesting idea in nanomedical approaches may be the design of multifunctional nanomaterial complexes able to carry out intracellular delivery of one or several cargos, such as diagnostic, imaging, or therapeutic molecules to specific locations in the body (e.g., cells, tissues, or organs) (Figure 2). Such conjugates, upon synthesis, coating, and functionalization, can integrate various functionalities [52,55]. Of note, surface functionalization and coating of nanostructures with various substances such as polymers [56,57], antibodies [58], peptides [59], or surfactants [60] may improve their biocompatibility and limit their immunogenicity. Polyethylene glycol (PEG)-coating of nanostructures (PEGylation) is one of the commonly-used chemical modifications, which may also affect the bioavailability of nano-sized materials [61]. The combination of imaging and therapeutic compounds within a single nanostructure complex may yield a theranostic nanodevice for improved diagnosis and therapy of various diseases such as cancer [62,63]. In addition, nanoformulations for cancer theranostics have been used for targeted drug delivery to solid tumors at relatively high concentrations with minimal toxic effects on surrounding normal cells or tissues [64,65].
Figure 2.
Schematic illustration of nanostructure-based multifunctional complexes. Cargos such as diagnostic probes (e.g., fluorescent or chromogenic dyes, radiotracers, or contrast agents), therapeutic agents (e.g., drugs, siRNA, natural compounds, or chemotherapeutics), surface coating (e.g., PEG, Gal, or mesoporous silica) and targeting ligands (e.g., antibodies or aptamers) can be attached/encapsulated to nanostructures using chemistry and surface modification methods. PEG, polyethylene glycol; Gal, galacto-oligosaccharides.
The use of a nano-based drug delivery system is a rapidly-developing branch of nanomedicine where materials in the nanoscale range are employed to serve as diagnostic and therapeutic tools that may offer multiple benefits in treating human diseases [66]. One of the uses of nanocarriers as drug delivery systems is nano-encapsulation, conjugation, and site-specific transport of therapeutic agents or natural substances for therapeutic purposes [46]. For example, the nucleolin-targeting AS1411 aptamer-decorated niosomes can both effectively recognize cancer cells and deliver the nucleolipidic anticancer drugs that in turn promote antiproliferative effects against human cervical cancer cells [67]. Moreover, the efficiency of natural bioactive compounds, such as quercetin, curcumin, resveratrol, and berberine has been significantly improved by the use of nano-based drug delivery systems [46,68,69,70,71,72]. The properties of nanoscale-sized materials also often differ significantly from those of the same materials at large scales. Hence, nanotechnology has been used to improve the uptake of small agents [46,52]. Moreover, the small size of these agents may enable them to overcome various anatomical and physiological barriers which may improve nanodrug mobility and diffusivity to specific body parts [46,73]. For example, it has been shown that transferrin-containing gold nanoparticles have increased ability to cross the blood–brain barrier through transcytosis in vivo [74]. In addition, nanosized materials loaded with poorly-water-soluble and chemically-unstable compounds such as quercetin may improve their bioavailability and promote targeted delivery [75]. For example, a six-fold increase in bioavailability of thymoquinone (bioactive compound isolated from Nigella sativa) has been shown after its encapsulation in a lipid nanocarrier in comparison with the unmodified plant-derived compound. The combined use of lipid nanocarrier with thymoquinone increased the pharmacokinetic properties of the bioactive product resulting in better therapeutic effects [76]. Nanotechnology-based drug delivery systems may also protect drugs from the degradation in the gastrointestinal tract and bypass the liver first-pass metabolism, increasing lymphatic absorption and improving drug solubility. Moreover, drugs encapsulated in nano-structures have prolonged circulation time, reduced toxicity, decreased immunogenicity, and increased efficacy [46,77,78].
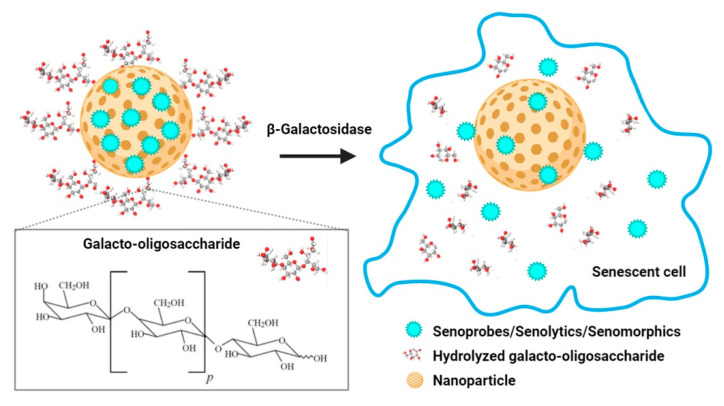
It is important to mention that stimuli-responsive nanocarriers (also called stimuli-triggered drug delivery) that provide a drug in a time-dependent and concentration-controlled manner can be sensitive to microenvironmental changes and various parameters, namely enzyme concentration, hypoxia, pH, heat, light or electronic pulses, magnetism, temperature and others [79]. For instance, stable at physiological pH, pH-responsive nanocarriers are promising agents for specific drug delivery to acidic diseased tissues, such as cancer [80]. pH-sensitive controlled release of doxorubicin from doxorubicin-encapsulated nanoparticles has been revealed to result in apoptosis in MCF-7 breast-cancer cells [81]. pH-sensitive nanoparticles loaded with the chemotherapeutic agent are also considered as non-toxic to normal tissues [82]. Recently, several nanocarriers have been proposed for efficient targeting of SCs in vitro and in vivo [83]. The most frequently-used method to detect SCs in vitro and in vivo is the evaluation of the senescence-associated β-galactosidase activity [84]. It was shown that nanoparticles coated with a substrate for SA-β-gal and encapsulated with cytotoxic drugs, small molecules, or probes were able to target cargo release mediated by increased SA-β-gal activity in SCs (Figure 3) [83,85]. Molecules that have been developed and designed to detect and visualize SCs are called senoprobes [55]. Importantly, the coated nanostructures are activated only in SCs, where the coating is digested and the cytotoxic drugs/senolytics can be released into the cytoplasm to induce apoptotic cell death that promotes healthspan and extends lifespan in mouse aging models [83,86].
Figure 3.
Nanoparticles capped with galacto-oligosaccharide and loaded with senoprobes, senolytics, and/or senomorphics. Cargos can be preferentially released and activated in senescent cells with high activity of SA-β-galactosidase that is based on SA-β-galactosidase-mediated hydrolysis of an oligosaccharide coat.
3. Senolytics and Senotherapy
As cellular senescence is an important contributor to aging and age-related disorders, new approaches are required to postpone/prevent detrimental effects mediated by dysfunctional SCs. It has been shown that the selective elimination of SCs is able to attenuate numerous aging-related disorders and extend mouse longevity [87,88]. For instance, in progeroid BubR1 (BubR1H/H) mouse model, the selective eradication of SCs reduces age-related disorders, in a process termed senolysis [88]. It has been shown that removing senescent cells from tissues might inhibit cancer formation in mice suggesting that senolysis in older patients may have healthspan benefits [87]. Senolytic drugs and novel galacto-oligosaccharide-coated nanomaterials with toxic cargos can be considered to target SCs. Senolytic compounds are able to selectively kill SCs, whereas senomorphic compounds are able to diminish SASP [15,43,88,89]. It should be pointed out that senolytics must be precisely targeted to eliminate SCs without affecting normal neighboring cells [30].
Bioinformatics approaches based on RNA and protein expression profiles of senescent versus non-senescent cells have been used for identification of SCAPs. Key pro-survival proteins were recognized as potential targets for senotherapy. It is important to note that inhibition of pro-survival pathways and a decrease in the expression of SCAPs may promote death of SCs [43,90,91,92]. Selected drugs and small molecules from chemical libraries were found to interfere with key components of pro-survival pathways in senescent cells and were considered as first-generation senolytics [24]. Until now, several classes of first-generation senolytics such as natural compounds (e.g., fisetin, quercetin, and piperlongumine), a pan-receptor tyrosine kinase inhibitor dasatinib, HSP90 inhibitors (e.g., geldanamycin, 17-AAG, and 17-DMAG), and Bcl-2 family inhibitors (e.g., navitoclax, ABT-737, A1331852, and UBX1967) have been described [24,43,86,90,91,92,93,94,95,96,97,98,99]. Targeting SCAPs in culture in vitro using senolytics may result in apoptosis of some SCs. For example, it has been documented that a combination of drugs with senolytic activity, namely dasatinib (a tyrosine kinase inhibitor) and quercetin (a flavonoid with estrogenic activity) eliminates SCs in human and murine cultured cells in vitro and in vivo [90,93]. In addition, this combined treatment significantly improves physiological function and increases lifespan in prematurely-aged mice [90,94,95,96]. Another agent having senotherapeutic activity is a naturally-occurring flavonoid with low toxicity, fisetin. It has been shown that treatment of old and progeroid mice with fisetin reduces some senescence markers in multiple tissues and extends animal lifespan [97,98]. Moreover, fisetin preferentially induces apoptosis in senescent human umbilical vein endothelial cells [97]. It has been shown that a natural product, piperlongumine is also a senolytic agent and preferentially induces apoptosis in oncogene-induced senescent human fibroblast cells [99]. In addition, the senolytic potential of curcumin analog EF24 (a synthetic analog of natural anti-aging compound) in vitro has been reported that was achieved by apoptosis induction in SCs in an ROS-independent manner, and enhanced proteasome mediated-degradation of the Bcl-2 anti-apoptotic protein [100]. Panobinostat, a histone deacetylase inhibitor, also has post-chemotherapy senolytic activity in senescent cancer cells [101]. It has been shown that panobinostat is able to increase caspase 3/7 activity and decrease the expression of anti-apoptotic proteins leading to clearance of SCs, which accumulate after anticancer drug treatment. Another approach to removing SCs from aged mice is targeting the pathways involved in senescence such as the FOXO–p53 axis. Activated FOXO4 transcription factor can induce cellular senescence by interacting with p53, which leads to upregulation of the transcription of a major regulator of senescence, p21. A novel FOXO4-interacting peptide disturbs the FOXO4 communication with p53 and also can induce apoptosis in both prematurely- and naturally-aging mice. Treatment with FOXO4-peptide can enhance health and lifespan in old mice [102]. Recently, several compounds targeting the chaperone protein HSP90, namely 17-AAG (tanespimycin), geldanamycin, and 17-DMAG (alvespimycin) have been demonstrated to be effective in inducing apoptosis in senescent murine and human cells [43,103]. Interestingly, the first in-human pilot study (14 patients) demonstrated that dasatinib and quercetin can eliminate SCs in patients with age-related chronic lung disease (idiopathic pulmonary fibrosis), reduce inflammation, and limit frailty [93]. More recently, senolytic chimeric antigen receptor (CAR) T cells were designed and their efficacy in eliminating of SCs expressing urokinase-type plasminogen activator receptor (uPAR) in vitro and in vivo systems was documented [104]. It has been shown that uPAR-specific CAR T cells may preferentially eradicate SCs in a number of experimental models of senescence [104]. Moreover, BET-family protein degrader (BETd) has been tested for a potential senolytic activity in obesity-induced hepatocellular carcinoma mouse model [105]. It has been reported that BETd may induce senolysis by targeting non-homologous end joining (NHEJ) and autophagy [105]. Autophagy is generally considered as a protective and adaptive stress response, but in some cellular settings, autophagy may also contribute to cell death [106]. Indeed, BETd provoked autophagy-induced apoptosis in senescent cells that was achieved, at least in part, by up-regulation of autophagic gene expression [105].
Several other strategies have been recently proposed to provide more accurate and targeted senolytic-based interventions. These include nanotechnology-based approaches for detection, site-specific delivery of senolytics and/or senoprobes, and successful elimination of SCs [83,107,108,109,110]. As cellular senescence may be implicated in the pathogenesis of age-related neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease [111,112], the use of nano-senolytics in the central nervous system (CNS) seems promising. One should remember that nano-based systems are able to overcome the blood–brain barrier and improve the delivery of encapsulated therapeutic agents and dietary polyphenols at lower systemic doses [68,74].
4. Nanomaterials for the Clearance of Senescent Cells
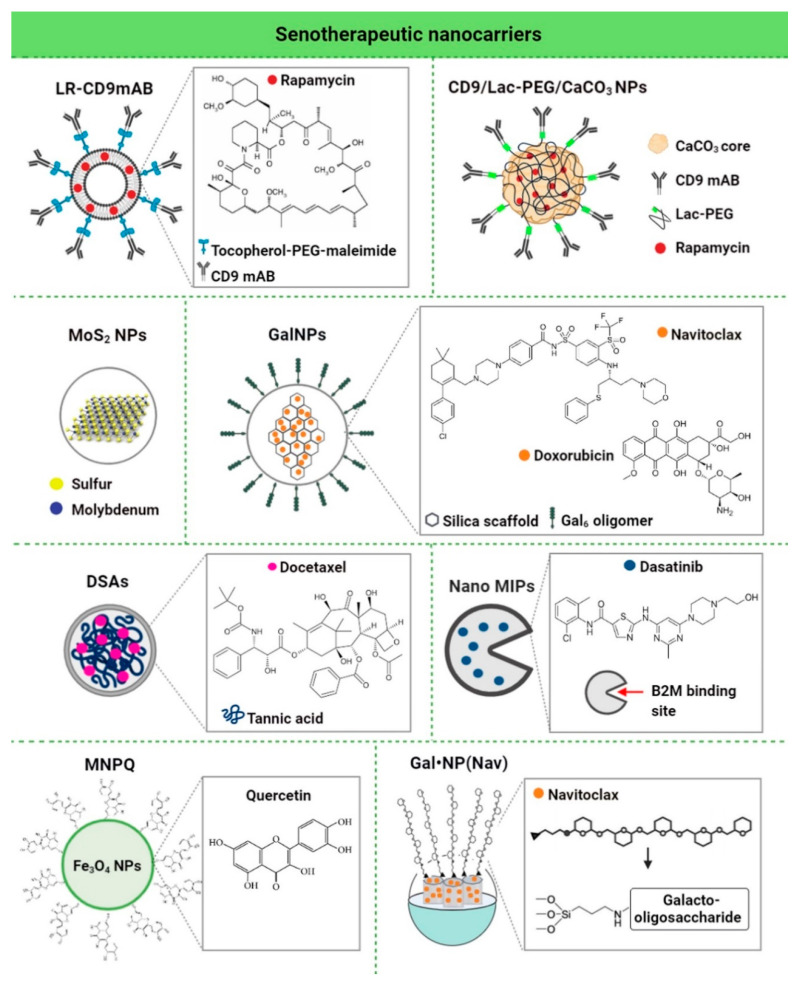
As the main purpose of senotherapy is to kill SCs, safe and effective detection and targeting of these cells is crucial to improving human health and prolonging lifespan [113]. Nano-based systems developed to identify and kill senescent cells can be considered as second-generation targeted and selective senolytics that are able to efficiently eliminate senescent cells upon systemic administration without causing adverse side effects. One of the best-explored groups of nano-senolytics is smart nanodevices that are based on porous calcium carbonate nanoparticles, mesoporous silica nanoparticles, carbon quantum dots, and molecularly-imprinted polymer nanoparticles (nanoMIPs) (Figure 4) [114]. Targeted delivery and detection/elimination of SCs can be achieved by encapsulation of senolytics/senomorphics/fluorophores using a number of nanomaterials. For example, cargo release in the presence of β-galactosidase (β-gal) was due to the hydrolysis of the capping galacto-oligosaccharide (Gal) polymer [109]. In vitro studies demonstrated that nanomaterials covered with Gal and loaded with fluorophores (e.g., rhodamine B, indocyanine green, coumarin-6, or Nile blue) were preferentially activated in β-galactosidase-overexpressing SCs, which were able to lyse the galacto-oligosaccharide coat (Figure 3) [85,114]. Moreover, β-galactosidase-instructed supramolecular assemblies can also lead to the formulation of hydrogels and nanofibers in SCs, which decreases the expression of senescence-driving proteins [115]. Apart from β-gal, increased expression of other lysosomal hydrolases (e.g., α-L-fucosidase) has been used for detection of senescent cells [116]. To date, a collection of senoprobes has been described [114]. Nano-based senoprobes could be utilized to monitor the response of tumors to the administration of senescence-inducing chemotherapeutic drugs. More recently, another method for the real-time in vivo detection of senescent cells based on mesoporous silica nanoparticles loaded with Nile blue and coated with a galacto-hexasaccharide was proposed [117]. Functionalized nanomaterials appear to have a promising potential as nanocarriers and can be used for improving SC clearance. Table 1 provides published examples of in vitro and in vivo senotherapeutic action of nano-based drug delivery systems [83,107,108,109,110,114,118,119,120,121].
Figure 4.
Different examples of nanocarriers used for targeted delivery of senolytics/senomorphics to senescent cells. Chemical structures of the loaded cargos are presented. LR, rapamycin-loaded PEGylated liposomes; NPs, nanoparticles; PEG, polyethylene glycol; Lac-PEG, lactose-polyethylene glycol; Gal, galacto-oligosaccharide; DSAs, docetaxel-tannic acid self-assemblies; NanoMIPs, molecularly imprinted nanoparticles; B2M, beta-2 microglobulin; Gal6, 6-mer galacto-oligosaccharide; Nav, navitoclax; MNPQ, quercetin surface-functionalized Fe3O4 nanoparticles.
Table 1.
Nanomaterials targeting senescent cells using cellular in vitro and in vivo models.
| Nanomaterial | Biologically- Active Component |
Concentration | Senescence Model | In Vitro/In Vivo Model | Senolytic Effects and Mechanism | Ref. |
|---|---|---|---|---|---|---|
| LR-CD9mAb CD9 monoclonal antibody conjugated to PEGylated liposomes | Rapa | 25 nM | Human dermal fibroblasts (HDF), doxorubicin-induced senescence | In vitro | Anti-senescence activity (increased proliferative potential, decreased β-galactosidase activity and p53/p21 expression, and increased cell migration) | [118] |
| CD9-Lac/CaCO3/Rapa NPs CD9 monoclonal antibody-conjugated lactose-wrapped calcium carbonate nanoparticles loaded with rapamycin | Rapa | 0.2 mg of rapamycin per mg of CaCO3 NPs | Human dermal fibroblasts (HDF), replicative and doxorubicin-induced senescence | In vitro | Anti-senescence activity (decreased β-galactosidase activity and p53/p21/CD9/cyclin D1 expression, increased cell proliferation and cell migration ability, decreased population doubling time, and prevention of G1 cell cycle arrest) | [107] |
| MoS2 NPs molybdenum disulfide mesoporous silica nanoparticles | - | 50 μg/mL | Human aortic endothelial cells (HAECs), stress-induced premature senescence | In vitro | Anti-senescence activity (decreased γ−H2AX phosphorylation, repressed upregulation of p16, p21 and p53, activation of autophagy, improved autophagic flux, and prevention of lysosomal and mitochondrial dysfunction) | [108] |
| GalNP(dox) 6-mer galacto-oligosaccharide encapsulated doxorubicin | Dox | 1 mg/kg | Mouse, bleomycin-induced lung fibrosis | In vivo | Anti-senescence activity (improved lung function) | [109] |
| GalNP(nav) 6-mer galacto-oligosaccharide encapsulated navitoclax | Nav | 0.06 mg/mL | Melanoma (SK-MEL-103), palbociclib-induced senescence | In vitro | Senolytic activity (apoptosis of senescent cells) | |
| GalNP(dox) 6-mer galacto-oligosaccharide encapsulated doxorubicin | Dox | 1 mg/kg | Mouse-bearing SK-MEL-103 tumor xenografts, palbociclib-induced tumor senescence | In vivo | Clearance of senescent cells and induced regression of tumor xenografts | |
| GalNP(nav) 6-mer galacto-oligosaccharide encapsulated navitoclax | Nav | |||||
| DSAs Docetaxel-tannic acid self-assemblies (DSAs)-based nanoparticles | Docetaxel | 2.5-5 nM | Prostate cancer cells (C4-2 and PC- 3) | In vitro | Senolytic activity (inhibition of senescence-related TGFβR1, FOXO1, and p21 proteins and activation of apoptosis) | [119] |
| 30 mg/kg | Mouse-bearing PC-3 tumor xenografts | In vivo | Clearance of senescent cells (induced regression of tumor xenografts by blockade of TGFβR1/p21-mediated senescence signaling and activation of apoptosis) | |||
| NanoMIPs molecularly-imprinted nanoparticles | Dasatinib | 10 μM dasatinib-conjugated B2M nanoMIPs | Bladder cancer cells with a tetracycline (tet)-regulatable p16 expression systems (EJp16) | In vitro | Senolytic activity (decreased number of senescent cancer cells) | [110] |
| MNPQ quercetin surface-functionalized Fe3O4 nanoparticles | Quercetin | 5 μg/mL | Human foreskin fibroblasts (BJ), hydrogen peroxide-induced senescence | In vitro | Senolytic and senostatic activity (AMPK activation, induction of non-apoptotic cell death, and inhibition of SASP components, namely IL-6 and IFN-β) | [120] |
| GalNP(nav) | Nav | 40 mg GalNP (Nav)/kg (≈2.5 mg/kg of free navitoclax) | Triple-negative breast cancer mouse model, palbociclib-induced senescence | In vivo | Senolytic activity (inhibited tumor growth, reduced metastasis, and limited systemic toxicity of navitoclax, and apoptosis of senescent cancer cells) | [121] |
Abbreviations: Rapa, rapamycin; Dox, doxorubicin; Nav, navitoclax.
The first-reported SC-targeted cargo delivery nano-system is a nano-structure based on mesoporous silica nanoparticles (MSN S1) coated with galacto-oligosaccharides and loaded with rhodamine B [85]. MSN S1 are engulfed by human SCs and activated by SA-β-gal. There are also studies showing that encapsulation of a senolytic agent, namely navitoclax with β(1,4)-galacto-oligosaccharides is effective in clearing SCs in models of damage-induced and chemotherapy-induced senescence [109]. Nanostructures conjugated with drugs may also exert a senomorphic effect by inhibiting the SASP [107,120]. A recent in vitro study demonstrated that nanoparticles functionalized with monoclonal antibody against CD9 receptor (overexpressed in old cells) and loaded with rapamycin (an mTOR inhibitor with well-recognized anti-aging activity) (CD9-Lac/CaCO3/Rapa NPs) have anti-senescence effect [107]. CD9-Lac/CaCO3/Rapa NPs significantly improved the proliferative capacity of SCs, which was accompanied by lower expression of IL-6 and IL-1β, the SASP components [107]. Moreover, CD9-targeted PEGylated liposomes have been documented as a promising drug delivery platform to target senescent cells [118]. The uptake of CD9-targeted liposomes by premature senescent human dermal fibroblasts (HDFs) was revealed to be higher than that by young HDFs [118]. Targeted delivery of rapamycin (LR-CD9mAb) to diminish senescence of CD9-receptor-overexpressing cells was also explored and rapamycin was found to promote cell proliferation and reduce the levels of SA-β-gal-positive cells [118]. Another study performed by Ke et al. [108] showed that MoS2 NPs suppressed hydrogen-peroxide-induced senescence in endothelial cells. In addition, MoS2 NP treatment leads to autophagy activation, which suppressed SIPS in vitro [108]. More recently, the docetaxel–tannic acid self-assembly (DSA)-based nanoparticle strategy has been developed and documented to be an efficient delivery system to provide docetaxel to prostate cancer cells and xenograft tumors and diminish cellular senescence [119]. DSAs-induced anti-senescence and anti-cancer effects were mediated by the inhibition of TGFβR1/FOXO1/p21-associated senescence and apoptosis induction in vitro and in vivo [119]. The authors concluded that DSAs can be considered as a useful nano-platform to deliver anticancer molecules (here docetaxel) to cancer cells that would result in improved therapeutic benefits and limited chemotherapy-induced senescence and drug resistance [119]. Targeted clearance of SCs using B2M (β2 microglobulin) nanoMIPs (molecularly imprinted nanoparticles) has been also described [110]. B2M nanoMIPs specifically recognize one of the previously-identified members of a cell membrane surface protein that is overexpressed in SCs, namely B2M [110]. In addition, it has been shown that B2M nanoMIPs loaded with a senolytic drug (dasatinib) can kill senescent bladder cancer cells [110]. Moreover, fluorescently-tagged nanoMIPs detected senescent cells in vivo and were not toxic when injected at single doses [110]. The authors concluded that nanoMIPs may have diagnostic, prognostic, and therapeutic potential when considering the pathological conditions mediated by the accumulation of senescent cells [110]. We have also documented a senolytic and senostatic activity of quercetin surface-functionalized magnetite nanoparticles (MNPQ) in prematurely-senescent human fibroblasts (hydrogen peroxide treatment in vitro) [120]. It has been shown that MNPQ are able to eliminate senescent human fibroblast cells in vitro [120]. MNPQ diminish senescence-mediated proinflammatory response as judged by decreased secretion of IL-8 and IFN-β that was accompanied by the activation of AMP-activated protein kinase (AMPK) [120].
5. Conclusions
The nano-based drug delivery system and its applications in the field of aging research have developed and evolved over the last several years. Because of their nano-sized nature and their ability to meet diverse functionalities, senescent-cell-targeted nanocarriers may have potential for elimination of senescent cells from the human body, which may improve the treatment of age-related disorders. However, many challenges restrain their successful clinical translation. Firstly, our current knowledge about molecular mechanisms underlying cellular senescence and modulating senescence-associated secretory phenotype in the context of age-associated disorders is not yet complete. In addition, successful application of senotherapeutic nanocarriers may depend on the development of best-suited methods for minimizing potential off-target effects and maximizing on-target effects. Next, for those who study senescent-cell-targeted nanocarriers, it may be challenging to find an optimal nanocarrier type for senolytic drug delivery as well as optimal biocompatible concentration(s), improved drug encapsulation, and ligand conjugation efficiency. The parameters of nanocarrier absorption, interactions with human biological fluids, distribution, metabolism, and excretion are also important for future anti-aging applications of senotherapeutic nanocarriers. In conclusion, a nano-based drug delivery system constitutes a novel strategy to target senescent cells for potential therapeutic interventions. While few initial studies are promising, additional further studies involving the development of second-generation targeted and selective senolytics, namely senescence-targeted nanocarriers and validation of nano-senolytics using preclinical aging model systems and clinical trials are needed to determine whether these nanodevices might be effective against age-related diseases.
Acknowledgments
Figures were created using Biorender, https://biorender.com/.
Abbreviations
| 17-AAG | tanespimycin |
| 17-DMAG | alvespimycin |
| AKT | protein kinase B |
| AMPK | AMP-activated protein kinase |
| B2M | Beta-2 microglobulin |
| Bcl-2 | B cell lymphoma 2 family |
| BETd | BET family protein degrader |
| CAR | Chimeric antigen receptor |
| CCL-16 | Monotactin-1 |
| CDKI | Cyclin-dependent kinase inhibitor |
| CS | Cellular senescence |
| DAMPs | Damage-associated molecular patterns |
| DDR | DNA damage response |
| DNA | Deoxyribonucleic acid |
| Dox | Doxorubicin |
| DSAs | Docetaxel-tannic acid self-assemblies |
| EGF | Endothelial growth factor |
| EGF | Epidermal growth factor |
| EVs | Extracellular vesicles |
| FOXO4 | Forkhead box protein O4 |
| Gal | Galacto-oligosaccharide |
| Gal6 | 6-mer galacto-oligosaccharide |
| HAECs | Human aortic endothelial cells |
| HDF | Human dermal fibroblasts |
| HIF-1α | Hypoxia inducible factor 1α |
| HSP90 | Chaperone heat shock protein 90 |
| IFN-β | Interferon beta |
| IGF-1 | Insulin-like growth factor 1 |
| IL-6 | Interleukin 6 |
| IL-8 | Interleukin 8 |
| IL-1β | Interleukin 1β |
| JAK | Janus kinase |
| Lac-PEG | Lactose-polyethylene glycol |
| LR | Rapamycin-loaded PEGylated liposomes |
| MAPK | Mitogen-activated protein kinase |
| MCP-1 | Monocyte chemoattractant protein 1 |
| MIP-1α | Macrophage inflammatory protein 1α |
| miRNA | MicroRNA |
| MMPs | Metalloproteinases |
| MoS2 | Molybdenum disulfide |
| MNPQ | Quercetin surface-functionalized Fe3O4 nanoparticles |
| MSN | Mesoporous silica nanoparticles |
| mTOR | Mammalian target of rapamycin |
| nanoMIPs | Molecularly-imprinted polymer nanoparticles |
| Nav | Navitoclax |
| NF | Nuclear factor |
| NHEJ | Non-homologous end joining |
| NPs | Nanoparticles |
| OIS | Oncogene-induced senescence |
| p16 | Cyclin-dependent kinase inhibitor 2A |
| p21 | Cyclin-dependent kinase inhibitor 1A |
| p53 | Tumor suppressor protein p53 |
| PEG | Polyethylene glycol |
| PI3K | Phosphatidylinositol-3-kinase |
| Rapa | Rapamycin |
| Rb | Retinoblastoma |
| RNA | Ribonucleic acid |
| ROS | Reactive oxygen species |
| SAHF | Senescence-associated heterochromatin foci |
| SASP | Senescence-associated secretory phenotype |
| SA-β-gal | Senescence associated β-galactosidase |
| SCAPs | Senescent cell anti-apoptotic pathways |
| SCs | Senescent cells |
| SIPS | Stress-induced premature senescence |
| siRNA | Small interfering RNA |
| STAT | Signal transducer and activator of transcription |
| uPAR | Urokinase-type plasminogen activator receptor |
Author Contributions
Conceptualization, J.A.-G. and A.L.; writing—original draft preparation, J.A.-G. and A.L.; writing—review and editing, J.A.-G. and A.L.; visualization, J.A.-G.; supervision, J.A.-G. and A.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rodier F., Campisi J. Four faces of cellular senescence. J. Cell Biol. 2011;192:547–556. doi: 10.1083/jcb.201009094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herranz N., Gil J. Mechanisms and functions of cellular senescence. J. Clin. Investig. 2018;128:1238–1246. doi: 10.1172/JCI95148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayflick L., Moorhead P.S. The serial cultivation of human diploid cell strains. Exp. Cell Res. 1961;25:585–621. doi: 10.1016/0014-4827(61)90192-6. [DOI] [PubMed] [Google Scholar]
- 4.Shay J.W., Wright W.E. Telomeres and telomerase: Three decades of progress. Nat. Rev. Genet. 2019;20:299–309. doi: 10.1038/s41576-019-0099-1. [DOI] [PubMed] [Google Scholar]
- 5.Bodnar A.G. Extension of Life-Span by Introduction of Telomerase into Normal Human Cells. Science. 1998;279:349–352. doi: 10.1126/science.279.5349.349. [DOI] [PubMed] [Google Scholar]
- 6.Dimri G.P., Lee X., Basile G., Acosta M., Scott G., Roskelley C., Medrano E.E., Linskens M., Rubelj I., Pereira-Smith O. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc. Natl. Acad. Sci. USA. 1995;92:9363–9367. doi: 10.1073/pnas.92.20.9363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Q., Fischer A., Reagan J.D., Yan L.J., Ames B.N. Oxidative DNA damage and senescence of human diploid fibroblast cells. Proc. Natl. Acad. Sci. USA. 1995;92:4337–4341. doi: 10.1073/pnas.92.10.4337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuilman T., Michaloglou C., Mooi W.J., Peeper D.S. The essence of senescence. Genes Dev. 2010;24:2463–2479. doi: 10.1101/gad.1971610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toussaint O., Medrano E.E., von Zglinicki T. Cellular and molecular mechanisms of stress-induced premature senescence (SIPS) of human diploid fibroblasts and melanocytes. Exp. Gerontol. 2000;35:927–945. doi: 10.1016/S0531-5565(00)00180-7. [DOI] [PubMed] [Google Scholar]
- 10.Serrano M., Lin A.W., McCurrach M.E., Beach D., Lowe S.W. Oncogenic ras Provokes Premature Cell Senescence Associated with Accumulation of p53 and p16INK4a. Cell. 1997;88:593–602. doi: 10.1016/S0092-8674(00)81902-9. [DOI] [PubMed] [Google Scholar]
- 11.Collado M., Serrano M. Senescence in tumours: Evidence from mice and humans. Nat. Rev. Cancer. 2010;10:51–57. doi: 10.1038/nrc2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Storer M., Mas A., Robert-Moreno A., Pecoraro M., Ortells M.C., Di Giacomo V., Yosef R., Pilpel N., Krizhanovsky V., Sharpe J., et al. Senescence Is a Developmental Mechanism that Contributes to Embryonic Growth and Patterning. Cell. 2013;155:1119–1130. doi: 10.1016/j.cell.2013.10.041. [DOI] [PubMed] [Google Scholar]
- 13.Muñoz-Espín D., Serrano M. Cellular senescence: From physiology to pathology. Nat. Rev. Mol. Cell Biol. 2014;15:482–496. doi: 10.1038/nrm3823. [DOI] [PubMed] [Google Scholar]
- 14.Tchkonia T., Morbeck D.E., Von Zglinicki T., Van Deursen J., Lustgarten J., Scrable H., Khosla S., Jensen M.D., Kirkland J.L. Fat tissue, aging, and cellular senescence: Fat tissue and aging. Aging Cell. 2010;9:667–684. doi: 10.1111/j.1474-9726.2010.00608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naylor R.M., Baker D.J., van Deursen J.M. Senescent cells: A novel therapeutic target for aging and age-related diseases. Clin. Pharmacol. Ther. 2013;93:105–116. doi: 10.1038/clpt.2012.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Deursen J.M. The role of senescent cells in ageing. Nature. 2014;509:439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He S., Sharpless N.E. Senescence in Health and Disease. Cell. 2017;169:1000–1011. doi: 10.1016/j.cell.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kritsilis M., Rizou V.S., Koutsoudaki P.N., Evangelou K., Gorgoulis V.G., Papadopoulos D. Ageing, Cellular Senescence and Neurodegenerative Disease. Int. J. Mol. Sci. 2018;19:2937. doi: 10.3390/ijms19102937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmer A.K., Gustafson B., Kirkland J.L., Smith U. Cellular senescence: At the nexus between ageing and diabetes. Diabetologia. 2019;62:1835–1841. doi: 10.1007/s00125-019-4934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wei W., Ji S. Cellular senescence: Molecular mechanisms and pathogenicity. J. Cell. Physiol. 2018;233:9121–9135. doi: 10.1002/jcp.26956. [DOI] [PubMed] [Google Scholar]
- 21.Sikora E., Bielak-Zmijewska A., Mosieniak G. Targeting normal and cancer senescent cells as a strategy of senotherapy. Ageing Res. Rev. 2019;55:100941. doi: 10.1016/j.arr.2019.100941. [DOI] [PubMed] [Google Scholar]
- 22.Terzi M.Y., Izmirli M., Gogebakan B. The cell fate: Senescence or quiescence. Mol. Biol. Rep. 2016;43:1213–1220. doi: 10.1007/s11033-016-4065-0. [DOI] [PubMed] [Google Scholar]
- 23.Sharpless N.E., Sherr C.J. Forging a signature of in vivo senescence. Nat. Rev. Cancer. 2015;15:397–408. doi: 10.1038/nrc3960. [DOI] [PubMed] [Google Scholar]
- 24.Childs B.G., Gluscevic M., Baker D.J., Laberge R.M., Marquess D., Dananberg J., van Deursen J.M. Senescent cells: An emerging target for diseases of ageing. Nat Rev Drug Discov. 2017;16:718–735. doi: 10.1038/nrd.2017.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.von Kobbe C. Targeting senescent cells: Approaches, opportunities, challenges. Aging. 2019;11:12844–12861. doi: 10.18632/aging.102557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coppé J.-P., Patil C.K., Rodier F., Sun Y., Muñoz D.P., Goldstein J., Nelson P.S., Desprez P.-Y., Campisi J. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol. 2008;6:2853–2868. doi: 10.1371/journal.pbio.0060301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuilman T., Peeper D.S. Senescence-messaging secretome: SMS-ing cellular stress. Nat. Rev. Cancer. 2009;9:81–94. doi: 10.1038/nrc2560. [DOI] [PubMed] [Google Scholar]
- 28.Rodier F., Coppé J.-P., Patil C.K., Hoeijmakers W.A.M., Muñoz D.P., Raza S.R., Freund A., Campeau E., Davalos A.R., Campisi J. Persistent DNA damage signalling triggers senescence-associated inflammatory cytokine secretion. Nat. Cell Biol. 2009;11:973–979. doi: 10.1038/ncb1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coppé J.-P., Desprez P.-Y., Krtolica A., Campisi J. The senescence-associated secretory phenotype: The dark side of tumor suppression. Annu. Rev. Pathol. 2010;5:99–118. doi: 10.1146/annurev-pathol-121808-102144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kirkland J.L., Tchkonia T. Cellular Senescence: A Translational Perspective. EBioMedicine. 2017;21:21–28. doi: 10.1016/j.ebiom.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Panda A.C., Abdelmohsen K., Gorospe M. SASP regulation by noncoding RNA. Mech. Ageing Dev. 2017;168:37–43. doi: 10.1016/j.mad.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang T.-W., Yevsa T., Woller N., Hoenicke L., Wuestefeld T., Dauch D., Hohmeyer A., Gereke M., Rudalska R., Potapova A., et al. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature. 2011;479:547–551. doi: 10.1038/nature10599. [DOI] [PubMed] [Google Scholar]
- 33.Yun M.H. Cellular senescence in tissue repair: Every cloud has a silver lining. Int. J. Dev. Biol. 2018;62:591–604. doi: 10.1387/ijdb.180081my. [DOI] [PubMed] [Google Scholar]
- 34.Acosta J.C., O’Loghlen A., Banito A., Guijarro M.V., Augert A., Raguz S., Fumagalli M., Da Costa M., Brown C., Popov N., et al. Chemokine Signaling via the CXCR2 Receptor Reinforces Senescence. Cell. 2008;133:1006–1018. doi: 10.1016/j.cell.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 35.Krtolica A., Parrinello S., Lockett S., Desprez P.-Y., Campisi J. Senescent fibroblasts promote epithelial cell growth and tumorigenesis: A link between cancer and aging. Proc. Natl. Acad. Sci. USA. 2001;98:12072. doi: 10.1073/pnas.211053698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vizioli M.G., Adams P.D. Senescence Can Be BETter without the SASP? Cancer Discov. 2016;6:576–578. doi: 10.1158/2159-8290.CD-16-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soto-Gamez A., Demaria M. Therapeutic interventions for aging: The case of cellular senescence. Drug Discov. Today. 2017;22:786–795. doi: 10.1016/j.drudis.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Sakoda K., Yamamoto M., Negishi Y., Liao J.K., Node K., Izumi Y. Simvastatin Decreases IL-6 and IL-8 Production in Epithelial Cells. J. Dent. Res. 2006;85:520–523. doi: 10.1177/154405910608500608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lim H., Park H., Kim H.P. Effects of flavonoids on senescence-associated secretory phenotype formation from bleomycin-induced senescence in BJ fibroblasts. Biochem. Pharmacol. 2015;96:337–348. doi: 10.1016/j.bcp.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 40.Hoare M., Ito Y., Kang T.-W., Weekes M.P., Matheson N.J., Patten D.A., Shetty S., Parry A.J., Menon S., Salama R., et al. NOTCH1 mediates a switch between two distinct secretomes during senescence. Nat. Cell Biol. 2016;18:979–992. doi: 10.1038/ncb3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson G., Wordsworth J., Wang C., Jurk D., Lawless C., Martin-Ruiz C., von Zglinicki T. A senescent cell bystander effect: Senescence-induced senescence. Aging Cell. 2012;11:345–349. doi: 10.1111/j.1474-9726.2012.00795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lehmann B.D., Paine M.S., Brooks A.M., McCubrey J.A., Renegar R.H., Wang R., Terrian D.M. Senescence-Associated Exosome Release from Human Prostate Cancer Cells. Cancer Res. 2008;68:7864–7871. doi: 10.1158/0008-5472.CAN-07-6538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fuhrmann-Stroissnigg H., Niedernhofer L.J., Robbins P.D. Hsp90 inhibitors as senolytic drugs to extend healthy aging. Cell Cycle Georget. Tex. 2018;17:1048–1055. doi: 10.1080/15384101.2018.1475828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sajja H., East M., Mao H., Wang Y., Nie S., Yang L. Development of Multifunctional Nanoparticles for Targeted Drug Delivery and Noninvasive Imaging of Therapeutic Effect. Curr. Drug Discov. Technol. 2009;6:43–51. doi: 10.2174/157016309787581066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Obeid M.A., Al Qaraghuli M.M., Alsaadi M., Alzahrani A.R., Niwasabutra K., Ferro V.A. Delivering natural products and biotherapeutics to improve drug efficacy. Ther. Deliv. 2017;8:947–956. doi: 10.4155/tde-2017-0060. [DOI] [PubMed] [Google Scholar]
- 46.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., Rodriguez-Torres M.P., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S., et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chenthamara D., Subramaniam S., Ramakrishnan S.G., Krishnaswamy S., Essa M.M., Lin F.-H., Qoronfleh M.W. Therapeutic efficacy of nanoparticles and routes of administration. Biomater. Res. 2019;23:20. doi: 10.1186/s40824-019-0166-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farokhzad O., Langer R. Nanomedicine: Developing smarter therapeutic and diagnostic modalities. Adv. Drug Deliv. Rev. 2006;58:1456–1459. doi: 10.1016/j.addr.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 49.Nie S., Xing Y., Kim G.J., Simons J.W. Nanotechnology Applications in Cancer. Annu. Rev. Biomed. Eng. 2007;9:257–288. doi: 10.1146/annurev.bioeng.9.060906.152025. [DOI] [PubMed] [Google Scholar]
- 50.Seigneuric R., Markey L., Nuyten S.A.D., Dubernet C., Evelo T.A.C., Finot E., Garrido C. From Nanotechnology to Nanomedicine: Applications to Cancer Research. Curr. Mol. Med. 2010;10:640–652. doi: 10.2174/156652410792630634. [DOI] [PubMed] [Google Scholar]
- 51.Kolahalam L.A., Kasi Viswanath I.V., Diwakar B.S., Govindh B., Reddy V., Murthy Y.L.N. Review on nanomaterials: Synthesis and applications. Mater. Today Proc. 2019;18:2182–2190. doi: 10.1016/j.matpr.2019.07.371. [DOI] [Google Scholar]
- 52.Ventola C.L. The nanomedicine revolution: Part 1: Emerging concepts. P T Peer-Rev. J. Formul. Manag. 2012;37:512–525. [PMC free article] [PubMed] [Google Scholar]
- 53.Salatin S., Yari Khosroushahi A. Overviews on the cellular uptake mechanism of polysaccharide colloidal nanoparticles. J. Cell. Mol. Med. 2017;21:1668–1686. doi: 10.1111/jcmm.13110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kargozar S., Mozafari M. Nanotechnology and Nanomedicine: Start small, think big. Mater. Today Proc. 2018;5:15492–15500. doi: 10.1016/j.matpr.2018.04.155. [DOI] [Google Scholar]
- 55.Paez-Ribes M., González-Gualda E., Doherty G.J., Muñoz-Espín D. Targeting senescent cells in translational medicine. EMBO Mol. Med. 2019;11 doi: 10.15252/emmm.201810234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pelaz B., del Pino P., Maffre P., Hartmann R., Gallego M., Rivera-Fernández S., de la Fuente J.M., Nienhaus G.U., Parak W.J. Surface Functionalization of Nanoparticles with Polyethylene Glycol: Effects on Protein Adsorption and Cellular Uptake. ACS Nano. 2015;9:6996–7008. doi: 10.1021/acsnano.5b01326. [DOI] [PubMed] [Google Scholar]
- 57.Schöttler S., Becker G., Winzen S., Steinbach T., Mohr K., Landfester K., Mailänder V., Wurm F.R. Protein adsorption is required for stealth effect of poly(ethylene glycol)- and poly(phosphoester)-coated nanocarriers. Nat. Nanotechnol. 2016;11:372–377. doi: 10.1038/nnano.2015.330. [DOI] [PubMed] [Google Scholar]
- 58.Kolhar P., Anselmo A.C., Gupta V., Pant K., Prabhakarpandian B., Ruoslahti E., Mitragotri S. Using shape effects to target antibody-coated nanoparticles to lung and brain endothelium. Proc. Natl. Acad. Sci. USA. 2013;110:10753–10758. doi: 10.1073/pnas.1308345110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gao H., Yang Z., Zhang S., Cao S., Shen S., Pang Z., Jiang X. Ligand modified nanoparticles increases cell uptake, alters endocytosis and elevates glioma distribution and internalization. Sci. Rep. 2013;3:2534. doi: 10.1038/srep02534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gao W., Zhang L. Coating nanoparticles with cell membranes for targeted drug delivery. J. Drug Target. 2015;23:619–626. doi: 10.3109/1061186X.2015.1052074. [DOI] [PubMed] [Google Scholar]
- 61.Suk J.S., Xu Q., Kim N., Hanes J., Ensign L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016;99:28–51. doi: 10.1016/j.addr.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zavaleta C., Ho D., Chung E.J. Theranostic Nanoparticles for Tracking and Monitoring Disease State. SLAS Technol. Transl. Life Sci. Innov. 2018;23:281–293. doi: 10.1177/2472630317738699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramanathan S., Archunan G., Sivakumar M., Tamil Selvan S., Fred A.L., Kumar S., Gulyás B., Padmanabhan P. Theranostic applications of nanoparticles in neurodegenerative disorders. Int. J. Nanomed. 2018;13:5561–5576. doi: 10.2147/IJN.S149022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Haley B., Frenkel E. Nanoparticles for drug delivery in cancer treatment. Urol. Oncol. Semin. Orig. Investig. 2008;26:57–64. doi: 10.1016/j.urolonc.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 65.Chen F., Ehlerding E.B., Cai W. Theranostic nanoparticles. J. Nucl. Med. 2014;55:1919–1922. doi: 10.2967/jnumed.114.146019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen G., Roy I., Yang C., Prasad P.N. Nanochemistry and Nanomedicine for Nanoparticle-based Diagnostics and Therapy. Chem. Rev. 2016;116:2826–2885. doi: 10.1021/acs.chemrev.5b00148. [DOI] [PubMed] [Google Scholar]
- 67.Riccardi C., Fàbrega C., Grijalvo S., Vitiello G., D’Errico G., Eritja R., Montesarchio D. AS1411-decorated niosomes as effective nanocarriers for Ru(iii)-based drugs in anticancer strategies. J. Mater. Chem. B. 2018;6:5368–5384. doi: 10.1039/C8TB01563E. [DOI] [PubMed] [Google Scholar]
- 68.Squillaro T., Cimini A., Peluso G., Giordano A., Melone M.A.B. Nano-delivery systems for encapsulation of dietary polyphenols: An experimental approach for neurodegenerative diseases and brain tumors. Biochem. Pharmacol. 2018;154:303–317. doi: 10.1016/j.bcp.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 69.Di Martino P., Censi R., Gigliobianco M.R., Zerrillo L., Magnoni F., Agas D., Quaglia W., Lupidi G. Nano-medicine Improving the Bioavailability of Small Molecules for the Prevention of Neurodegenerative Diseases. Curr. Pharm. Des. 2017;23:1897–1908. doi: 10.2174/1381612822666161227154447. [DOI] [PubMed] [Google Scholar]
- 70.McClements D.J., Xiao H. Designing food structure and composition to enhance nutraceutical bioactivity to support cancer inhibition. Semin. Cancer Biol. 2017;46:215–226. doi: 10.1016/j.semcancer.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 71.Squillaro T., Peluso G., Melone M.A.B. Nanotechnology-Based Polyphenol Delivery: A Novel Therapeutic Strategy for the Treatment of Age-Related Neurodegenerative Disorder. Austin Aging Res. 2017;1:1004. [Google Scholar]
- 72.Li C., Zhang J., Zu Y.J., Nie S.F., Cao J., Wang Q., Nie S.P., Deng Z.Y., Xie M.Y., Wang S. Biocompatible and biodegradable nanoparticles for enhancement of anti-cancer activities of phytochemicals. Chin. J. Nat. Med. 2015;13:641–652. doi: 10.1016/S1875-5364(15)30061-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thomas O.S., Weber W. Overcoming Physiological Barriers to Nanoparticle Delivery-Are We There Yet? Front. Bioeng. Biotechnol. 2019;7:415. doi: 10.3389/fbioe.2019.00415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Clark A.J., Davis M.E. Increased brain uptake of targeted nanoparticles by adding an acid-cleavable linkage between transferrin and the nanoparticle core. Proc. Natl. Acad. Sci. USA. 2015;112:12486–12491. doi: 10.1073/pnas.1517048112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang W., Sun C., Mao L., Ma P., Liu F., Yang J., Gao Y. The biological activities, chemical stability, metabolism and delivery systems of quercetin: A review. Trends Food Sci. Technol. 2016;56:21–38. doi: 10.1016/j.tifs.2016.07.004. [DOI] [Google Scholar]
- 76.Abdelwahab S.I., Sheikh B.Y., Taha M.M.E., How C.W., Abdullah R., Yagoub U., El-Sunousi R., Eid E.E.M. Thymoquinone-loaded nanostructured lipid carriers: Preparation, gastroprotection, in vitro toxicity, and pharmacokinetic properties after extravascular administration. Int. J. Nanomed. 2013;8:2163–2172. doi: 10.2147/IJN.S44108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sharma M., Sharma R., Jain D.K. Nanotechnology Based Approaches for Enhancing Oral Bioavailability of Poorly Water Soluble Antihypertensive Drugs. Scientifica. 2016;2016:8525679. doi: 10.1155/2016/8525679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Caster J.M., Patel A.N., Zhang T., Wang A. Investigational nanomedicines in 2016: A review of nanotherapeutics currently undergoing clinical trials: Investigational nanomedicines in 2016. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2017;9:e1416. doi: 10.1002/wnan.1416. [DOI] [PubMed] [Google Scholar]
- 79.Mura S., Nicolas J., Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013;12:991–1003. doi: 10.1038/nmat3776. [DOI] [PubMed] [Google Scholar]
- 80.Liu J., Huang Y., Kumar A., Tan A., Jin S., Mozhi A., Liang X.-J. pH-Sensitive nano-systems for drug delivery in cancer therapy. Biotechnol. Adv. 2014;32:693–710. doi: 10.1016/j.biotechadv.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 81.Wang X., Teng Z., Wang H., Wang C., Liu Y., Tang Y., Wu J., Sun J., Wang H., Wang J., et al. Increasing the cytotoxicity of doxorubicin in breast cancer MCF-7 cells with multidrug resistance using a mesoporous silica nanoparticle drug delivery system. Int. J. Clin. Exp. Pathol. 2014;7:1337–1347. [PMC free article] [PubMed] [Google Scholar]
- 82.Hamidu A., Mokrish A., Mansor R., Razak I.S.A., Danmaigoro A., Jaji A.Z., Bakar Z.A. Modified methods of nanoparticles synthesis in pH-sensitive nano-carriers production for doxorubicin delivery on MCF-7 breast cancer cell line. Int. J. Nanomed. 2019;14:3615–3627. doi: 10.2147/IJN.S190830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Muñoz-Espín D. Nanocarriers targeting senescent cells. Transl. Med. Aging. 2019;3:1–5. doi: 10.1016/j.tma.2019.01.001. [DOI] [Google Scholar]
- 84.Lee B.Y., Han J.A., Im J.S., Morrone A., Johung K., Goodwin E.C., Kleijer W.J., DiMaio D., Hwang E.S. Senescence-associated β-galactosidase is lysosomal β-galactosidase. Aging Cell. 2006;5:187–195. doi: 10.1111/j.1474-9726.2006.00199.x. [DOI] [PubMed] [Google Scholar]
- 85.Agostini A., Mondragón L., Bernardos A., Martínez-Máñez R., Marcos M.D., Sancenón F., Soto J., Costero A., Manguan-García C., Perona R., et al. Targeted Cargo Delivery in Senescent Cells Using Capped Mesoporous Silica Nanoparticles. Angew. Chem. Int. Ed. 2012;51:10556–10560. doi: 10.1002/anie.201204663. [DOI] [PubMed] [Google Scholar]
- 86.Ovadya Y., Krizhanovsky V. Strategies targeting cellular senescence. J. Clin. Investig. 2018;128:1247–1254. doi: 10.1172/JCI95149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Baker D.J., Childs B.G., Durik M., Wijers M.E., Sieben C.J., Zhong J., Saltness R.A., Jeganathan K.B., Verzosa G.C., Pezeshki A., et al. Naturally occurring p16(Ink4a)-positive cells shorten healthy lifespan. Nature. 2016;530:184–189. doi: 10.1038/nature16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baker D.J., Wijshake T., Tchkonia T., LeBrasseur N.K., Childs B.G., van de Sluis B., Kirkland J.L., van Deursen J.M. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature. 2011;479:232–236. doi: 10.1038/nature10600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kirkland J.L., Tchkonia T. Clinical strategies and animal models for developing senolytic agents. Exp. Gerontol. 2015;68:19–25. doi: 10.1016/j.exger.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu Y., Tchkonia T., Pirtskhalava T., Gower A.C., Ding H., Giorgadze N., Palmer A.K., Ikeno Y., Hubbard G.B., Lenburg M., et al. The Achilles’ heel of senescent cells: From transcriptome to senolytic drugs. Aging Cell. 2015;14:644–658. doi: 10.1111/acel.12344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhu Y., Tchkonia T., Fuhrmann-Stroissnigg H., Dai H.M., Ling Y.Y., Stout M.B., Pirtskhalava T., Giorgadze N., Johnson K.O., Giles C.B., et al. Identification of a novel senolytic agent, navitoclax, targeting the Bcl-2 family of anti-apoptotic factors. Aging Cell. 2016;15:428–435. doi: 10.1111/acel.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.González-Gualda E., Pàez-Ribes M., Lozano-Torres B., Macias D., Wilson J.R., González-López C., Ou H.-L., Mirón-Barroso S., Zhang Z., Lérida-Viso A., et al. Galacto-conjugation of Navitoclax as an efficient strategy to increase senolytic specificity and reduce platelet toxicity. Aging Cell. 2020:e13142. doi: 10.1111/acel.13142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Justice J.N., Nambiar A.M., Tchkonia T., LeBrasseur N.K., Pascual R., Hashmi S.K., Prata L., Masternak M.M., Kritchevsky S.B., Musi N., et al. Senolytics in idiopathic pulmonary fibrosis: Results from a first-in-human, open-label, pilot study. EBioMedicine. 2019;40:554–563. doi: 10.1016/j.ebiom.2018.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schafer M.J., White T.A., Iijima K., Haak A.J., Ligresti G., Atkinson E.J., Oberg A.L., Birch J., Salmonowicz H., Zhu Y., et al. Cellular senescence mediates fibrotic pulmonary disease. Nat. Commun. 2017;8:14532. doi: 10.1038/ncomms14532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ogrodnik M., Miwa S., Tchkonia T., Tiniakos D., Wilson C.L., Lahat A., Day C.P., Burt A., Palmer A., Anstee Q.M., et al. Cellular senescence drives age-dependent hepatic steatosis. Nat. Commun. 2017;8:15691. doi: 10.1038/ncomms15691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Farr J.N., Xu M., Weivoda M.M., Monroe D.G., Fraser D.G., Onken J.L., Negley B.A., Sfeir J.G., Ogrodnik M.B., Hachfeld C.M., et al. Targeting cellular senescence prevents age-related bone loss in mice. Nat. Med. 2017;23:1072–1079. doi: 10.1038/nm.4385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhu Y., Doornebal E.J., Pirtskhalava T., Giorgadze N., Wentworth M., Fuhrmann-Stroissnigg H., Niedernhofer L.J., Robbins P.D., Tchkonia T., Kirkland J.L. New agents that target senescent cells: The flavone, fisetin, and the BCL-XL inhibitors, A1331852 and A1155463. Aging. 2017;9:955–963. doi: 10.18632/aging.101202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yousefzadeh M.J., Zhu Y., McGowan S.J., Angelini L., Fuhrmann-Stroissnigg H., Xu M., Ling Y.Y., Melos K.I., Pirtskhalava T., Inman C.L., et al. Fisetin is a senotherapeutic that extends health and lifespan. EBioMedicine. 2018;36:18–28. doi: 10.1016/j.ebiom.2018.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wang Y., Chang J., Liu X., Zhang X., Zhang S., Zhang X., Zhou D., Zheng G. Discovery of piperlongumine as a potential novel lead for the development of senolytic agents. Aging. 2016;8:2915–2926. doi: 10.18632/aging.101100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Li W., He Y., Zhang R., Zheng G., Zhou D. The curcumin analog EF24 is a novel senolytic agent. Aging. 2019;11:771–782. doi: 10.18632/aging.101787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Samaraweera L., Adomako A., Rodriguez-Gabin A., McDaid H.M. A Novel Indication for Panobinostat as a Senolytic Drug in NSCLC and HNSCC. Sci. Rep. 2017;7:1900. doi: 10.1038/s41598-017-01964-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Baar M.P., Brandt R.M.C., Putavet D.A., Klein J.D.D., Derks K.W.J., Bourgeois B.R.M., Stryeck S., Rijksen Y., van Willigenburg H., Feijtel D.A., et al. Targeted Apoptosis of Senescent Cells Restores Tissue Homeostasis in Response to Chemotoxicity and Aging. Cell. 2017;169:132–147.e16. doi: 10.1016/j.cell.2017.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kirkland J.L., Tchkonia T., Zhu Y., Niedernhofer L.J., Robbins P.D. The Clinical Potential of Senolytic Drugs. J. Am. Geriatr. Soc. 2017;65:2297–2301. doi: 10.1111/jgs.14969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Amor C., Feucht J., Leibold J., Ho Y.-J., Zhu C., Alonso-Curbelo D., Mansilla-Soto J., Boyer J.A., Li X., Giavridis T., et al. Senolytic CAR T cells reverse senescence-associated pathologies. Nature. 2020;583:127–132. doi: 10.1038/s41586-020-2403-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wakita M., Takahashi A., Sano O., Loo T.M., Imai Y., Narukawa M., Iwata H., Matsudaira T., Kawamoto S., Ohtani N., et al. A BET family protein degrader provokes senolysis by targeting NHEJ and autophagy in senescent cells. Nat. Commun. 2020;11:1935. doi: 10.1038/s41467-020-15719-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mariño G., Niso-Santano M., Baehrecke E.H., Kroemer G. Self-consumption: The interplay of autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 2014;15:81–94. doi: 10.1038/nrm3735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Thapa R.K., Nguyen H.T., Jeong J.-H., Kim J.R., Choi H.-G., Yong C.S., Kim J.O. Progressive slowdown/prevention of cellular senescence by CD9-targeted delivery of rapamycin using lactose-wrapped calcium carbonate nanoparticles. Sci. Rep. 2017;7:43299. doi: 10.1038/srep43299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ke S., Lai Y., Zhou T., Li L., Wang Y., Ren L., Ye S. Molybdenum Disulfide Nanoparticles Resist Oxidative Stress-Mediated Impairment of Autophagic Flux and Mitigate Endothelial Cell Senescence and Angiogenic Dysfunctions. ACS Biomater. Sci. Eng. 2018;4:663–674. doi: 10.1021/acsbiomaterials.7b00714. [DOI] [PubMed] [Google Scholar]
- 109.Muñoz-Espín D., Rovira M., Galiana I., Giménez C., Lozano-Torres B., Paez-Ribes M., Llanos S., Chaib S., Muñoz-Martín M., Ucero A.C., et al. A versatile drug delivery system targeting senescent cells. EMBO Mol. Med. 2018;10:e9355. doi: 10.15252/emmm.201809355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ekpenyong-Akiba A.E., Canfarotta F., Abd H.B., Poblocka M., Casulleras M., Castilla-Vallmanya L., Kocsis-Fodor G., Kelly M.E., Janus J., Althubiti M., et al. Detecting and targeting senescent cells using molecularly imprinted nanoparticles. Nanoscale Horiz. 2019;4:757–768. doi: 10.1039/C8NH00473K. [DOI] [Google Scholar]
- 111.Musi N., Valentine J.M., Sickora K.R., Baeuerle E., Thompson C.S., Shen Q., Orr M.E. Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell. 2018;17:e12840. doi: 10.1111/acel.12840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Riessland M., Kolisnyk B., Kim T.W., Cheng J., Ni J., Pearson J.A., Park E.J., Dam K., Acehan D., Ramos-Espiritu L.S., et al. Loss of SATB1 Induces p21-Dependent Cellular Senescence in Post-mitotic Dopaminergic Neurons. Cell Stem. Cell. 2019;25:514–530.e8. doi: 10.1016/j.stem.2019.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Salmonowicz H., Passos J.F. Detecting senescence: A new method for an old pigment. Aging Cell. 2017;16:432–434. doi: 10.1111/acel.12580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Muñoz-Espin D., Demaria M. Senolytics in Disease, Ageing and Longevity. 1st ed. Springer Nature Switzerland; Cham, Switzerland: 2020. pp. 163–180. [Google Scholar]
- 115.Xu T., Cai Y., Zhong X., Zhang L., Zheng D., Gao Z., Pan X., Wang F., Chen M., Yang Z. β-Galactosidase instructed supramolecular hydrogelation for selective identification and removal of senescent cells. Chem. Commun. 2019;55:7175–7178. doi: 10.1039/C9CC03056E. [DOI] [PubMed] [Google Scholar]
- 116.Hildebrand D., Lehle S., Borst A., Haferkamp S., Essmann F., Schulze-Osthoff K. α-Fucosidase as a novel convenient biomarker for cellular senescence. Cell Cycle. 2013;12:1922–1927. doi: 10.4161/cc.24944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lozano-Torres B., Blandez J.F., Galiana I., García-Fernández A., Alfonso M., Marcos M.D., Orzáez M., Sancenón F., Martínez-Máñez R. Real-Time In Vivo Detection of Cellular Senescence through the Controlled Release of the NIR Fluorescent Dye Nile Blue. Angew. Chem. Int. Ed. 2020;59:15152–15156. doi: 10.1002/anie.202004142. [DOI] [PubMed] [Google Scholar]
- 118.Nguyen H.T., Thapa R.K., Shin B.S., Jeong J.-H., Kim J.-R., Yong C.S., Kim J.O. CD9 monoclonal antibody-conjugated PEGylated liposomes for targeted delivery of rapamycin in the treatment of cellular senescence. Nanotechnology. 2017;28:095101. doi: 10.1088/1361-6528/aa57b3. [DOI] [PubMed] [Google Scholar]
- 119.Nagesh P.K.B., Chowdhury P., Hatami E., Kumari S., Kashyap V.K., Tripathi M.K., Wagh S., Meibohm B., Chauhan S.C., Jaggi M., et al. Cross-Linked Polyphenol-Based Drug Nano-Self-Assemblies Engineered to Blockade Prostate Cancer Senescence. ACS Appl. Mater. Interfaces. 2019;11:38537–38554. doi: 10.1021/acsami.9b14738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lewinska A., Adamczyk-Grochala J., Bloniarz D., Olszowka J., Kulpa-Greszta M., Litwinienko G., Tomaszewska A., Wnuk M., Pazik R. AMPK-mediated senolytic and senostatic activity of quercetin surface-functionalized Fe3O4 nanoparticles during oxidant-induced senescence in human fibroblasts. Redox Biol. 2020;28:101337. doi: 10.1016/j.redox.2019.101337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Galiana I., Lozano-Torres B., Sancho M., Alfonso M., Bernardos A., Bisbal V., Serrano M., Martínez-Máñez R., Orzáez M. Preclinical antitumor efficacy of senescence-inducing chemotherapy combined with a nanoSenolytic. J. Control. Release. 2020;323:624–634. doi: 10.1016/j.jconrel.2020.04.045. [DOI] [PubMed] [Google Scholar]