Abstract
Regulatory T cells (Tregs) express the lineage-defining transcription factor FoxP3 and play crucial roles in self-tolerance and immune homeostasis. Thymic tTregs are selected based on affinity for self-antigens and are stable under most conditions. Peripheral pTregs differentiate from conventional CD4 T cells under the influence of TGF-β and other cytokines and are less stable. Treg plasticity refers to their ability to inducibly express molecules characteristic of helper CD4 T cell lineages like T-helper (Th)1, Th2, Th17 or follicular helper T cells. Plastic Tregs retain FoxP3 and are thought to be specialized regulators for “their” lineage. Unstable Tregs lose FoxP3 and switch to become exTregs, which acquire pro-inflammatory T-helper cell programs. Atherosclerosis with systemic hyperlipidemia, hypercholesterolemia, inflammatory cytokines, and local hypoxia provides an environment that is likely conducive to Tregs switching to exTregs.
Keywords: atherosclerosis, Tregs, stability
1. Introduction
Atherosclerosis is the leading cause of death globally, with about 610,000 deaths in the US annually. Atherosclerosis is a chronic progressive inflammatory disease with an autoimmune component [1]. Two recent clinical trials (CANTOS and COLCOT) show that anti-inflammatory therapies can have beneficial effects for outcomes of atherosclerosis, including myocardial infarction, cardiovascular death, and stroke [2,3]. Inflammation in the atherosclerotic vessel wall is driven by both the adaptive and innate immune responses [4,5,6,7], and regulatory T cells (Tregs) have attracted considerable attention as immune modulators in cardiovascular disease [8].
CD4 T cells help with killing and interferon-γ-driven type 1 inflammation (T-helper Th1); IL-4-, 5- and 13-driven type 2 inflammation (Th2); IL-17-driven inflammation (Th17), maturation of germinal centers; isotype switching; and affinity maturation of B cells (follicular helper Tfh) and other subsets. Tregs are a subset of CD4 T cells that maintain immunological homeostasis by suppressing the functional activity of conventional effector T cells (Tcons). The majority of CD4+ Tregs are generated in the thymus (tTregs), and others can be generated from peripheral Tcon cells (pTregs). tTregs arise from CD4+CD25+ cells upon engagement of their high-affinity, self-reactive T-cell receptors (TCRs) [9]. tTregs are found primarily in lymphoid tissues and blood [10] and can migrate to inflamed non-lymphoid tissues. pTregs, on the other hand, arise when peripheral CD4+CD25− Tcons are exposed to IL-2 and TGF-β in vitro or to an unknown cytokine mix in vivo. pTregs are typically found in mucosal tissues and are responsible for damping local inflammation elicited by foreign antigens [11,12,13,14]. Both tTregs and pTregs maintain self-tolerance and suppress the activity of CD4+CD25− Tcons via IL-10 and TGF-β production and through cell–cell interactions. Another subset of peripherally induced CD4+ Tregs, termed T-helper 3 (Th3) [15] cells, suppress the proliferation and cytokine secretion by Th1 and Th2 cells in a TGF-β-dependent, but not an IL-10-dependent, manner. A fourth subset are Tr1 cells, a cell type that mainly suppresses immune responses by secreting IL-10 and TGF-β [16]. In human Tregs, IL-7R(CD127) expression is negatively correlated with Foxp3 expression; thus, the common phenotype of human Tregs is CD4+CD25hiFoxp3+CD127low [16].
tTregs and pTregs, but not Th3 or Tr1 cells, express the Forkhead box P3 (Foxp3) transcription factor. In mice, their phenotype is CD4+CD25+Foxp3+. Foxp3 is the only Treg-defining transcription factor that has been identified to date. Loss of Foxp3 results in defective Treg development and causes fatal autoimmune diseases in mice and humans [17,18,19]. Nonetheless, the hypothesis that Foxp3 is the sole defining factor for the Treg lineage has been challenged by several studies. On one hand, Foxp3 transduction into CD4+CD25− is not sufficient to fully recapitulate the transcriptional landscape of Tregs [20,21]. On the other hand, in mice in which a stop codon was introduced into Foxp3 and no FoxP3 protein was made, Foxp3-deficient T cells still expressed some of the Treg cell signature genes [22]. Unknown transcriptional regulator(s) may be upstream of Foxp3 [23]. Tr1 cells arise from CD4+CD25−/low when the immune system is experiencing a chronic inflammatory response in the presence of IL-10 [24]. Although Tr1 cells lack Foxp3, they dampen cytokine secretion and proliferation of naive CD4+CD25−T cells, including Th1 and Th2 cells in an IL-10- and TGF-β-dependent manner.
Given that Foxp3 is considered the master regulator of Tregs and its absence can result in severe autoimmunity, it is reasonable to assume that the long-term lineage stability of Tregs is highly dependent on the stability of Foxp3 expression. Foxp3 imposes a unique transcriptional signature on Tregs by interacting, directly or indirectly, with cell surface proteins, signaling molecules, transcription factors, non-coding RNAs, and epigenetic regulators [22,25,26]. The Foxp3 locus encodes three evolutionarily conserved non-coding sequences (CNS1–3) that determine the size and stability of the Treg pool [27]. CNS3 is the main inducer of Foxp3 expression in tTregs and pTregs. The maintenance of Foxp3 expression in tTregs is epigenetically regulated by CNS2, also known as Treg-specific demethylated region (TSDR) [27,28,29]. During early stages of thymic Treg development, signaling through IL-2 and other γ-chain cytokines initiates TSDR demethylation and thereby regulates Foxp3 expression [30,31]. Moreover, loss of CNS2 inhibits the heritable expression of Foxp3 when mature Tregs divide under inflammatory conditions or in an IL-2-limited environment [32]. Epigenetic profiling of Tregs showed that most tTregs exhibit completely demethylated TSDR, whereas pTregs exhibit partially demethylated TSDR [33,34]. CNS1, on the other hand, is dispensable for the development of tTregs, but imperative for pTregs, which are strongly dependent on TGF-β signaling. CNS1 contains a TGF-β-NFAT response element [27]. The stability of pTreg and in vitro–derived Tregs (iTreg) may be dependent on acquiring both Foxp3 expression and Treg-specific DNA hypomethylated regions [35,36]. tTregs possess unique DNA hypomethylated features that are acquired during thymic Treg development and start before Foxp3 induction [20,21,33,37]. These features are imprinted in genes that are normally upregulated in unstimulated tTregs, such as Foxp3, Ctla4, Tnfrsf18, and Ikzf2 [21].
Tregs can become dysregulated, and this has been linked to some autoimmune diseases. Tregs adoptively transferred into lymphopenic mice lose the expression of Foxp3 and gain effector characteristics [38]. Moreover, a subset of Tregs can lose the expression of Foxp3 under inflammatory settings, which can impact their immunosuppressive function [39,40]. Other Tregs expressing Tcon-lineage transcription factors and cytokines can still dampen the immune response and maintain immunological homeostasis [41]. In this review, we summarize the literature documenting the Tregs stability and plasticity, mostly based on mouse models, and we discuss the mechanisms underlying Treg instability and how this may apply to atherosclerosis.
2. Phenotypic and Functional Adaptability of Tregs
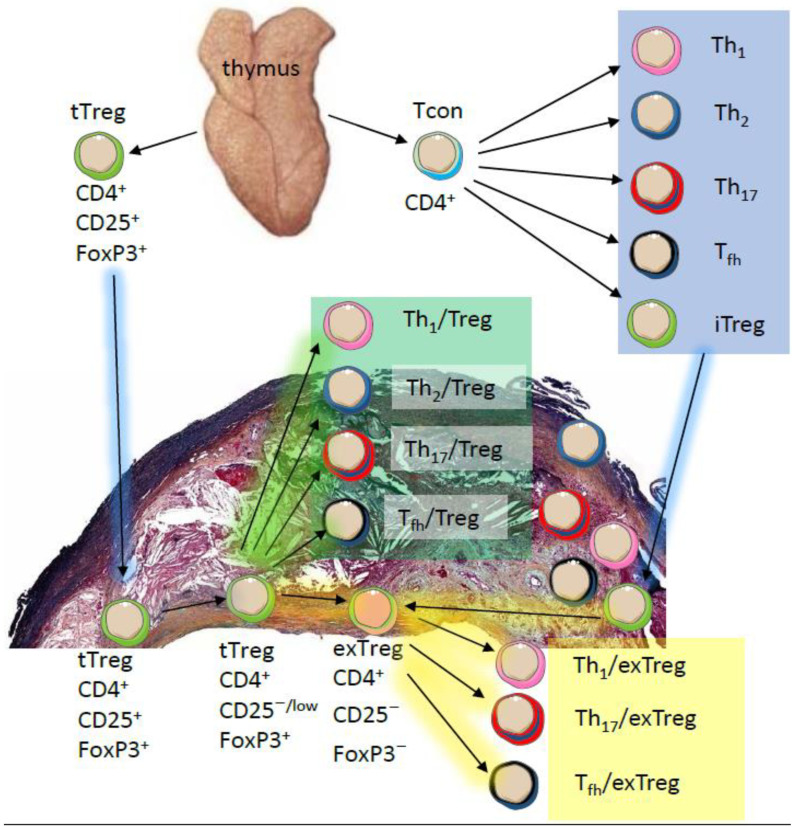
It is well established that most Tregs are stable and long-lasting under physiological conditions. However, several studies have challenged this notion and showed that prolonged exposure to inflammatory cues can promote Treg functional plasticity or affect Tregs stability [39,42,43]. Furthermore, IL-2 deprivation can create dysfunctional Tregs [44,45]. Moreover, metabolites and metabolic programs were shown to control Treg fate [46]. Instability and plasticity describe two distinct fates of Tregs. Instability describes the state at which Tregs lose Foxp3 expression and become so-called exTregs. This loss impairs the suppressive capacity (functionality) of these cells and allows them to acquire an effector-like phenotype. Loss of Foxp3 expression and gain of Th1, Tfh, or Th17 effector phenotypes have been reported in different diseases such as rheumatoid arthritis [47] and atherosclerosis [42,48] (Figure 1). Moreover, the presence of “latent” Tregs among exTregs has been observed by one group [49,50]. These cells were shown to maintain the epigenetic Treg memory by retaining the demethylated status of CNS2 region and were shown to be able to revert to Foxp3+ Tregs upon TCR stimulation [49].
Figure 1.
The thymus produces CD4+CD25+FoxP3+ tTregs (green), CD4+ conventional T cells (Tconv, blue) and many other cells (not shown). tTregs can migrate (blue arrows) into atherosclerotic lesions and the adventitia and maintain their phenotype. CD4+ Tconv differentiate into T-helper (Th)1, 2, and 17; Tfh; and induced iTregs. All of these (blue box) can also migrate into atherosclerotic lesions and the adventitia. In the lesion environment or in secondary lymphoid organs (not shown), both tTregs and iTregs can gain expression of T-bet for Th1, GATA3 for Th2, RORγt for Th17 or Bcl6 for Tfh, while maintaining expression of FoxP3 (Treg plasticity, green box). tTreg and iTregs can lose CD25 and FoxP3 expression and become exTregs that have a Th1, Th17, or Tfh phenotype (Treg instability, yellow box).
The term “plasticity” refers to the capacity of Tregs to acquire the migratory and functional characteristics of effector T cells while maintaining Foxp3 expression, so-called Th-like Tregs [44]. It can be envisioned that Treg plasticity is driving Treg heterogeneity in which multiple subsets of Th-like Tregs were reported. For example, IFNγ+ T-bet+CXCR3+ Th1-like Tregs, IL4+IL5+IL13+GATA3+ Th2-like Tregs, IL17A+RORγt+ Th17-like Tregs, and CXCR5+Bcl6+ICOS+PD1+ follicular Tregs have been identified under both physiological and pathological conditions [51,52,53,54,55]. It should be noted that, while instability is detrimental for Treg functionality, plasticity can be beneficial. It is thought that plasticity allows Tregs to adapt the transcriptional and migratory features of effector T cells, thus becoming more effective suppressors. For example, in response to IFNγ or IL-27 Tregs acquire Th1 characteristics by expressing T-bet and CXCR3, preferentially accumulate in Th1 inflammatory niches, and render Th1 cells more susceptible to suppression [41,56]. The same is true when Tregs acquire IRF4 expression and gain higher control over Th2 [55], or when Tregs acquire Bcl6 expression to control germinal center responses [57,58].
To evaluate Treg stability, multiple Treg-fate reporter mouse models have been generated [40,44,49] (Table 1). In all of these models, the Foxp3 promoter drives expression of a fluorescent protein (GFP) and/or Cre recombinase, using bacterial artificial chromosome (BAC)-derived transgenic or targeted knock-in mice. These mice were bred to reporter mice that harbor a transgene encoding loxP site-flanked stop codons in front of a reporter fluorescent protein (RFP) inserted into the Rosa26 locus. Thus, Foxp3 drives GFP and Cre, which removes the loxP sites, resulting in expression of RFP in cells that once expressed Foxp3, even if Foxp3-GFP-Cre expression is later lost. In such mice, current Tregs are yellow (GFP+RFP+), and ex-Tregs are red (GFP−RFP+). In a further refinement, GFP and Cre expression was made inducible by using a mutated form of human estrogen receptor (CreERT2; Foxp3GFP−CreERT2) [44]. In this system, in the absence of the ERT2 ligand tamoxifen, CreERT2 is sequestered in the cytoplasm. Ligand administration activates CreERT2, leading to its translocation to the nucleus, where Cre recombines the loxP sites. Endogenous mouse 17β-estradiol does not activate this form of ER mutant (ERT2); hereby, it eliminates the possibility of artifacts due to “leakiness” in expression [59].
Table 1.
Foxp3 lineage tracking mouse models.
| Foxp3 Allele | IRES for Reporter/Cre | Allele Type | ROSA-Locus | Inducible | Advantages | Limitations | References |
|---|---|---|---|---|---|---|---|
| Foxp3-EGFP-Cre | No | Transgenic (BAC), Recombinase-expressing, Reporter | Rosa26-loxP-Stop-loxP-YFP | No | Natural FoxP3 locus intact | May overestimate the switched population. BAC transgene inactivation in some Foxp3+ cells has been reported. Promoter may be incomplete. Enhancers may be missing. | [31] |
| Foxp3-IRES-GFP-iCre | Yes | Targeted (knock-in), Recombinase-expressing, Reporter | Rosa26-loxP-Stop-loxP-RFP | No | Reporter expressed under the natural FoxP3 promoter with enhancers intact. | May overestimate the switched population. Foxp3 activation can occur early during development in non-Treg cells. In this mouse, Cre activity was reported in CD8 T cells, B cells, and myeloid cells. | [40] |
| Foxp3-IRES-EGFP-Cre-ERT2 | Yes | Targeted (knock-in), Recombinase-expressing, Reporter, Inducible | Rosa26-loxP-Stop-loxP-YFP | Yes, with Tamoxifen | Reporter expressed under the natural FoxP3 promoter with enhancers intact. | May underestimate the switched population. This mouse tracks only the Tregs that were labeled during Tamoxifen injection. If the switched subset developed after tamoxifen injection, it will not be visible. | [35] |
| Foxp3-dCNS1-hCre-2A-eqFP650-2A-Thy1.1 | No | Transgenic (BAC), Recombinase-expressing, Reporter | Rosa26-loxP-Stop-loxP-YFP | No | This mouse detects the fate of tTregs but not pTregs. In YFP+ cells Thy1.1 is lost before Foxp3, making Thy1.1 a marker for cells that are about to lose Foxp3 expression. | In this model, to define exTregs, researchers need to stain for intracellular Foxp3. | [60] |
BAC, bacterial artificial chromosome
Two of these models showed that 10–20% (depending on the lymphoid tissue) of the total Tregs were unstable and switched to form exTregs [40,49]. Moreover, the propensity of Treg switching increased in response to (chronic) inflammatory insults in these models. In the inducible model, the total Treg lineage was shown to be remarkably stable with less than 5% of unstable peripheral Treg (exTregs). In this model, exposing Tregs to inflammatory insults did not undermine their stability. However, this model may underestimate the switched population, because only the Tregs that had been labeled during Tamoxifen injection are tracked. The cells that switched after tamoxifen injection are not labeled.
The reason for these divergent observations is likely, at least in part, technical. In the first two models, Tregs are labeled from birth to the time of data collection. In the inducible model, Tregs are labeled at the time of induction with Tamoxifen. This resembles taking a snapshot within a limited time period during Treg development. Indeed, the model proposed by Miyao and colleagues showed that exTregs appeared during ontogeny and accumulated through adulthood. In addition, pTregs contain an unstable pool of Tregs [50,60]. Thus, it is possible that the labeling system in the Rubstov et al. model is less representative of the unstable pTreg pool, which could have been accumulated from childhood through adulthood. Indeed, in a recent tTreg tracing model, in which CNS-1 was deleted from Foxp3 locus to limit the tracing to mature tTregs, only ~1% of tTregs lost Foxp3 expression under physiological conditions [61]. In this model, it has been shown that activated tTregs (CD62LloCD44hiCCR7lo) are more likely to lose Foxp3 activity than resting/central Tregs (CD62LhiCD44loCCR7hi). Another factor to consider when comparing Treg-fate reporter models is the type/intensity of inflammatory triggers that were utilized to challenge Treg stability. It appears that IL-2 and TCR engagement provide stability signals, while pro-inflammatory cytokines like IL-6, IL-4, and IL-12 can render Tregs unstable [39,62,63,64]. Collectively, despite the discrepancies in the percentage of the observed exTregs, the lineage tracing models portray the Treg pool as a stable cell-type of CD4 T cells, with a minor unstable subset, at least under the conditions studied so far.
3. Possible Mechanisms of Treg Instability
Both cell-intrinsic (TCR) and extrinsic (pro-inflammatory cues) factors modulate the Treg program. However, to what extent each is correlated to Treg stability is unknown. Two leading hypotheses may explain Treg instability. The first suggests that TCR stimulation may prime the epigenome of developing thymocytes to develop toward Tregs. The second hypothesis suggests that proinflammatory cytokines such as IL-6 and IL-4 may be major instability-inducing factors in mature Tregs.
Optimal Treg development depends on both TCR signal intensity and duration. The strength of TCR signal during positive and negative selection may follow the Goldilocks principle: Too strong results in clonal deletion, and too weak prevents Foxp3 induction [9,65,66]. Phosphoinositol 3′-kinase (PI(3)K)/Akt signaling downstream of TCR activation is less active in Tregs than Tcons [67,68]. Activation of Akt strongly represses Foxp3 induction during tTreg development as well as during iTreg formation [68]. The duration of TCR signaling along with the right co-stimulators appears to control the Treg-specific DNA hypomethylation. For example, constitutive or repetitive TCR stimulation downregulates Foxp3 in both mature activated tTregs and iTregs [67,69]. Premature termination of TCR signaling and PI3k and mTOR inhibition induces Foxp3 expression from CD4+CD25−CD62Lhi cells by changing the methylation status of the Foxp3 locus [67]. In a recent study, the absence of anti-CD28 during the induction of iTregs from CD4+CD25−CD62Lhi resulted in more epigenetically stable Tregs [37]. Overall, stably committed Tregs require a precise amount of TCR strength (for Foxp3 induction) and duration (for DNA-hypomethylation). Thus, effector Tregs may lose their suppressive functionality by interacting with ligand(s) similar to their cognate self-antigen that binds the TCR with higher affinity. Such interactions may lead to strong ICOS signaling that activates the PI3k/AKT signaling pathway, thus potentiating Treg instability [70]. Although both effector and resting Tregs receive continuous TCR signaling, the signal intensity skews the Treg phenotype: With a strong TCR signal, Tregs adopt an activated phenotype in which Treg homeostasis and function depend on ICOS signaling rather than IL-2 [71,72]. Supporting this hypothesis, a recent study has shown that highly self-reactive Tregs are more susceptible to upregulate T-bet and CXCR3 in response to TCR signaling rather than environmental cues [73]. However, in this study, the Tregs were stable, maintained their DNA-hypomethylation and did not express IFNγ. It is unclear how TCR signal duration and the type of co-stimulators maintain the epigenetic features of Tregs.
Under inflammatory conditions, the imbalance between local pro-inflammatory cytokines and Treg survival factors like IL-2 could impair Treg stability. Several studies have shown that IL-6, IL-4, IL-12, and IL-32 drive the inactivation of Foxp3 expression [39,74,75,76,77]. On the other hand, lack of IL-2 in diabetic islets [78] and under highly polarized Th1 immune responses [43] reduced Treg numbers and compromised their function. Treatment with IL-2 and anti-IL-2 complexes stabilized Foxp3 expression during EAE and expanded the Treg population in clinical trials [79,80].
Recent studies have demonstrated crucial roles for nutrients, metabolites, and cellular metabolism in modulating Treg functions. Vitamins such as A, D, and C can promote Foxp3 expression mainly by enhancing CNS demethylation [28,81,82,83]. Metabolites such as tryptophan induce Foxp3 expression by decreasing IL-6 production and increasing TGF-β expression in dendritic cells [84]. Other metabolites such as extracellular NAD+ and ATP can induce Treg conversion to Th17 cells by stimulating purinergic 2X receptor signaling, which induces T-cell activation, proliferation, and apoptosis [85,86]. Cellular metabolism can also modulate Foxp3 expression. The metabolic status is affected by the type of activated signaling pathway(s). Activation of the PI3K and Akt and mammalian target of rapamycin (mTOR) pathway promotes glycolysis. The AMP-activated protein kinase (AMPK) pathway promotes oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO) [87]. Unlike Tcons, Tregs prefer OXPHOS and FAO to glycolysis [88]. Studies have shown that Foxp3 induction promotes OXPHOS over glycolysis by suppressing the transcription of Myc and the glucose transporter Glut-1, and by inhibiting the PI(3)K and Akt and mTOR pathway [89,90]. Conversely, unrestrained glycolysis induces destabilization of Tregs [91,92,93]. Treg-specific deletion of PTEN (phosphatase and tensin homolog), a negative regulator of the glycolysis-promoting PI(3)K-Akt-mTORC2 pathway, promotes phenotypic transition of Tregs, which is characterized by a loss of their surface marker interleukin-2 receptor α subunit (CD25) and, ultimately, their lineage defining factor, Foxp3. Concomitantly, PTEN-deficient Tregs lose their suppressive capacity and the resulting overactivation of Th1 and Tfh responses gives rise to an autoimmune-lymphoproliferative disease [93]. Tregs of transgenic mice harboring T-cell-specific expression of constitutively active Glut1, likewise, lose Foxp3 expression, as well as their suppressive capacity [90].
On the other hand, disrupting OXPHOS by ablation of mitochondrial transcription factor A or mitochondrial complex III impairs Treg suppressive function without altering Foxp3 stability [94,95]. Lipid metabolism can also enhance Treg functionality. LKB-1, a key player in lipid metabolism in T cells, stabilizes Foxp3 expression by inhibiting STAT4-mediated CNS2 methylation [96]. Additionally, LKB-1 regulates the mevalonate pathway, related to intracellular cholesterol homeostasis, and thereby inhibits inflammatory cytokine production in Tregs and maintains their suppressiveness [97]. The mevalonate pathway can also be regulated by raptor, an essential component of mTORC1. Deletion of raptor impairs Treg function without affecting Foxp3 expression [98]. Interestingly, the mevalonate pathway is strongly inhibited by statins, a class of cholesterol-lowering drugs [99]. A recent study showed that the mTOR pathway can promote Treg stability [100], possibly because mTOR deficiency upregulates the levels of glutaminolysis and α-ketoglutarate, resulting in partial remethylation of the CNS2 region of Foxp3 [100,101,102].
4. Treg Adaptability in Atherosclerosis
In atherosclerosis, both Treg instability and Treg plasticity were reported (Figure 1). In 2016, Li et al. fed Apoe−/− mice on a Western diet (WD) for 12–20 weeks, to report the presence of plastic Tregs in aortas. These cells expressed IFNγ, T-bet, and Foxp3, were CD25low or negative, and accounted for 80% of all CCR5+ αβ T cells. The percentage of this population in the para-aortic lymph nodes (paLN) was significantly less (~15% of all CCR5+ αβ T cells) [48], and these cells were undetectable in the spleen. A similar population was observed by Butcher at al. [42]. In their study, IFNγ-producing Foxp3+ cells (Th1/Tregs) were evident in aortas (15% of total CD4 T cells) of aged Apoe−/− mice after two weeks of WD. This population was observed in both spleen and paLNs although at lower percentages (~12% in spleen and ~4% in paLNs). This work established CCR5 as an extracellular marker for Th1/Tregs. Previous studies have shown IFNγ to be important in generating atheroprotective CXCR3+ Tregs [41]. The authors tested the suppressive capacity of atherosclerotic Th1/Tregs and found them to be non-suppressive. In their efforts to track the source of Th1/Tregs, the authors injected Tregs from fate-reporter mice, Foxp3yfp-cre/yfp-creRosa26RtdTomato/tdTomato, into aged Apoe−/− mice. After two weeks of a Western diet, 30% of the injected cells were Foxp3+ CCR5+, suggesting that plastic Tregs arise from Tregs. In this system, however, none of the transferred Tregs lost the Foxp3-YFP signal, suggesting that two weeks of a WD is not enough to abolish Foxp3 expression and cause Treg instability.
In vitro, prolonged exposure to inflammatory cytokines like IL-12, IL-27, and IFNγ promoted Treg plasticity, suggesting that such cytokines could drive Treg plasticity in atherosclerosis. Indeed, IL-12 induces the formation of IFNγ+-Tregs by directly activating the PI(3)-AKT and Foxo1/3 pathway [103]. Foxo1/3 phosphorylation by AKT results in their cytoplasmic sequestration, preventing the interaction with their transcriptional targets. Foxo1 upregulates Foxp3 and Ctla4 gene expression and dampens Ifng expression [104,105,106]. In addition, decreased Foxo1 activity correlates with decreased glycolysis. This induce Tregs to acquire Th1-like program. As mentioned earlier, the activation of PI(3)K and AKT metabolic pathway can upregulate Glut-1, which can promote glycolysis and induce Treg plasticity [93,107]. To further support the atherogenic role of Th1/Treg in atherosclerosis, the authors used a Th1/Treg-prone mouse model (Mir146a−/− mice). Moreover, miR-146a regulates the activation of Stat1 in Treg cells, which maintains efficient control of a spontaneous IFNγ-dependent Th1 response and prevents the conversion of activated Tregs to IFNγ-producing Th1-like cells [108]. When Mir146a−/− Tregs (CD4+CD25+) were transferred into 27-week-old Apoe−/− mice for eight weeks, these mice developed more plaques than the mice receiving Mir146 sufficient Tregs. However, the lesion percentage was similar between mice that received Tregs from Mir146a−/− and sham-treated mice (baseline). This suggests that Th1/Treg-prone cells do not cause inflammation per se; instead, they fail to suppress atherogenic adaptive immune responses. Overall, this study reported, for the first time, non-suppressive plastic Th1/Tregs in atherosclerosis and proved their atherogenicity.
In another study, Treg-fate reporter mice (Foxp3YFP-CreRosa26RFPApoE−/−) showed Treg instability and exTreg formation in atherosclerosis [109]. In this study, exTregs were evident in the paLNs, spleen, and aorta of mice fed either chow diet or WD (15 weeks), but the proportion was higher under WD. Interrogation of exTreg phenotype(s) by using intracellular cytokine staining (ICS) suggested that Tregs can switch to Th1 and atherogenic Tfh under atherosclerotic conditions. Moreover, flow cytometry analysis showed that exTregs display low CD25 expression and increased IL-6Rα when compared with Tregs. The conversion of Tregs to Tfh may be caused by the disruption of intracellular cholesterol homeostasis in WD-fed ApoE−/− mice, because subcutaneous injections of ApoAI, a necessary component for the formation of nascent HDL particles, prompted cholesterol efflux, and sustained Treg stability. Interestingly, ApoAI treatment reduced Tfh exTregs, but not Th1 exTregs, suggesting different mechanisms underlying Treg conversion to Th1. Overall, this work illustrates how the hypercholesterolemic environment may shape the Tregs fate.
Recent work from our lab demonstrated that prolonged exposure to a hypercholesterolemic environment promotes the conversion of apolipoprotein B (ApoB) antigen-specific Tregs to atherogenic Th17 and Th1-like cells [110]. Time course scRNA-seq data analysis of ApoB-specific T cells demonstrated a phenotypic switch from Foxp3 expression toward a novel subpopulation of T-bet+RORγt+ cells in chow diet (CD)- fed ApoE−/− mice. Moreover, Tregs transferred into old ApoE−/− mice lost Foxp3 expression and gained T-bet or RORγt. These results were supported by an increase of Th1 and Th17 cells in WD-fed ApoE−/− mice in comparison to CD fed ApoE−/− mice. Gain of RORγt expression in Foxp3+ cells appears to be driven by Treg exposure to proinflammatory cytokines such as IL-6 and IL-1β. Indeed, we observed an upregulation of these cytokines in 20-week-old ApoE−/− mice. Moreover, IL-6, along with TGF-β, induces c-Maf in Th17 cells [111]. Indeed, c-Maf was upregulated in Th17 cells. Interestingly, in the intestinal niche, c-Maf promotes RORγt+ transcription in protective Foxp3+ cells in response to microbiota [112]. Another player in Treg conversion toward RORγt+ is continuous antigen exposure. Moreover, oxLDL, a known autoantigen in atherosclerosis that contains ApoB, is known to accumulate in atherosclerotic plaques, where it may reduce Treg stability and function [113,114]. A recent study showed that hypercholesterolemia induces hepatic iTreg/Th17 formation. These cells were shown to be home to aortas [115]. These cells may lose Foxp3 under atherosclerotic conditions and become atherogenic. Hypoxia is common in atherosclerotic plaques [116]. Previous studies have shown that hypoxia-inducible factor-1α (HIF-1α) induces RORγt expression and prevents iTreg formation by inducing Foxp3 proteasomal degradation [117]. Augmented HIF-1α activity in Tregs can promote glycolysis and induce the formation of IFN-γ+ Th1-like Tregs [118]. CNS2 demethylation is dependent on oxygen availability. The ten-eleven translocases TET2 and TET3 that mediate CNS2 demethylation require molecular oxygen (O2) for their activity [119]. How hypoxia affects the fate of Tregs in atherosclerosis is not known.
Taken together, the functional and phenotypic reprogramming of Tregs in atherosclerosis is not fully understood. Some results point to a loss of Treg stability, while others point to Treg plasticity. The discrepancies could be due to different time windows during which the Tregs were under inflammatory pressure. In the Butcher et al. study, the Treg-fate tracer mice were on a wild-type (ApoE+/+) background; thus; exTreg formation during atherogenesis was not investigated. The Treg fate was assessed two weeks after adoptive transfer to atherosclerotic ApoE−/− mice. On the other side, Gaddis et al. had Treg-fate tracer mice crossed into the ApoE−/− background. Thereby, Tregs were under inflammatory conditions during the entire study. It is noteworthy to mention that the study by Gaddis et al. does not rule out the availability of plastic Treg in atherosclerosis. The percentage of IFNγ+ -producing Tregs, which contain Th1/Tregs, was not reported.
5. Conclusions
Although Tregs are a largely stable lineage, recent studies have shown that the Treg program is mutable and that Tregs can lose their function, along with their lineage-marker (Foxp3), to form pathogenic exTregs. Emerging evidence indicates that atherosclerotic Apoe−/− mice have non-suppressive Th1-like Tregs [42] and that Tregs can convert to pathogenic Tfh and Th1 and Th17-like cells under atherosclerotic conditions [109,110]. However, the impact of naturally formed exTreg (from pTregs or tTregs) on the development of atherosclerosis remains to be elucidated. To date, the proatherogenic properties of exTregs have not been tested in rigorous adoptive transfer experiments. It remains unclear whether the exTregs formed in atherosclerotic mice are “latent” Tregs and can revert to fully functional Tregs when appropriately stimulated, in the absence of proinflammatory cytokines and the presence of a cognate self-antigen such as ApoB. Tolerogenic vaccines against atherosclerosis can expand atheroprotective Tregs and prevent atherosclerosis [120,121], but there is no evidence that a tolerogenic vaccine works in mice with established atherosclerosis (therapeutic vaccine). Since Treg function and stability is dependent on TCR signaling, metabolic processes, and cytokine signaling, the atherosclerotic environment has a lot to offer to drive Treg instability. Hypercholesterolemia, hypoxia, and enrichment of proinflammatory cytokines are all candidates for disrupting the Treg program and promote their conversion to exTregs.
Acknowledgments
We wish to acknowledge Andreas Schober, LMU Munich, Germany, for the histological image of a human carotid artery with severe atherosclerosis in Figure 1 and Servier, http://smart.servier.com/, for digital artwork used for the immune cells.
Author Contributions
A.J.A. and K.L. wrote the manuscript. J.M. read and edited the manuscript. A.J.A. compiled the table. K.L. drew the figure. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gistera A., Hansson G.K. The immunology of atherosclerosis. Nat. Rev. Nephrol. 2017;13:368–380. doi: 10.1038/nrneph.2017.51. [DOI] [PubMed] [Google Scholar]
- 2.Ridker P.M., Everett B.M., Thuren T., MacFadyen J.G., Chang W.H., Ballantyne C., Fonseca F., Nicolau J., Koenig W., Anker S.D., et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 3.Tardif J.C., Kouz S., Waters D.D., Bertrand O.F., Diaz R., Maggioni A.P., Pinto F.J., Ibrahim R., Gamra H., Kiwan G.S., et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N. Engl. J. Med. 2019;381:2497–2505. doi: 10.1056/NEJMoa1912388. [DOI] [PubMed] [Google Scholar]
- 4.Glass C.K., Witztum J.L. Atherosclerosis. The road ahead. Cell. 2001;104:503–516. doi: 10.1016/S0092-8674(01)00238-0. [DOI] [PubMed] [Google Scholar]
- 5.Wolf D., Ley K. Immunity and Inflammation in Atherosclerosis. Circ. Res. 2019;124:315–327. doi: 10.1161/CIRCRESAHA.118.313591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ley K. Role of the adaptive immune system in atherosclerosis. Biochem. Soc. Trans. 2020;48:2273–2281. doi: 10.1042/BST20200602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saigusa R., Winkels H., Ley K. T cell subsets and functions in atherosclerosis. Nat. Rev. Cardiol. 2020;17:387–401. doi: 10.1038/s41569-020-0352-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ou H.X., Guo B.B., Liu Q., Li Y.K., Yang Z., Feng W.J., Mo Z.C. Regulatory T cells as a new therapeutic target for atherosclerosis. Acta Pharm. Sin. 2018;39:1249–1258. doi: 10.1038/aps.2017.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jordan M.S., Boesteanu A., Reed A.J., Petrone A.L., Holenbeck A.E., Lerman M.A., Naji A., Caton A.J. Thymic selection of CD4+CD25+ regulatory T cells induced by an agonist self-peptide. Nat. Immunol. 2001;2:301–306. doi: 10.1038/86302. [DOI] [PubMed] [Google Scholar]
- 10.Wei S., Kryczek I., Zou W. Regulatory T-cell compartmentalization and trafficking. Blood. 2006;108:426–431. doi: 10.1182/blood-2006-01-0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng S.G., Wang J.H., Gray J.D., Soucier H., Horwitz D.A. Natural and induced CD4+CD25+ cells educate CD4+CD25− cells to develop suppressive activity: The role of IL-2, TGF-beta, and IL-10. J. Immunol. 2004;172:5213–5221. doi: 10.4049/jimmunol.172.9.5213. [DOI] [PubMed] [Google Scholar]
- 12.Yamagiwa S., Gray J.D., Hashimoto S., Horwitz D.A. A role for TGF-beta in the generation and expansion of CD4+CD25+ regulatory T cells from human peripheral blood. J. Immunol. 2001;166:7282–7289. doi: 10.4049/jimmunol.166.12.7282. [DOI] [PubMed] [Google Scholar]
- 13.Zheng S.G., Wang J., Wang P., Gray J.D., Horwitz D.A. IL-2 is essential for TGF-beta to convert naive CD4+CD25− cells to CD25+Foxp3+ regulatory T cells and for expansion of these cells. J. Immunol. 2007;178:2018–2027. doi: 10.4049/jimmunol.178.4.2018. [DOI] [PubMed] [Google Scholar]
- 14.Chen W., Jin W., Hardegen N., Lei K.J., Li L., Marinos N., McGrady G., Wahl S.M. Conversion of peripheral CD4+CD25− naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J. Exp. Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carrier Y., Yuan J., Kuchroo V.K., Weiner H.L. Th3 cells in peripheral tolerance. I. Induction of Foxp3-positive regulatory T cells by Th3 cells derived from TGF-beta T cell-transgenic mice. J. Immunol. 2007;178:179–185. doi: 10.4049/jimmunol.178.1.179. [DOI] [PubMed] [Google Scholar]
- 16.Seddiki N., Santner-Nanan B., Martinson J., Zaunders J., Sasson S., Landay A., Solomon M., Selby W., Alexander S.I., Nanan R., et al. Expression of interleukin (IL)-2 and IL-7 receptors discriminates between human regulatory and activated T cells. J. Exp. Med. 2006;203:1693–1700. doi: 10.1084/jem.20060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khattri R., Cox T., Yasayko S.A., Ramsdell F. Pillars Article: An Essential Role for Scurfin in CD4+CD25+ T Regulatory Cells. J. Immunol. 2017;198:993–998. [PubMed] [Google Scholar]
- 18.Fontenot J.D., Gavin M.A., Rudensky A.Y. Pillars Article: Foxp3 Programs the Development and Function of CD4+CD25+ Regulatory T Cells. J. Immunol. 2017;198:986–992. [PubMed] [Google Scholar]
- 19.Wildin R.S., Smyk-Pearson S., Filipovich A.H. Clinical and molecular features of the immunodysregulation, polyendocrinopathy, enteropathy, X linked (IPEX) syndrome. J. Med. Genet. 2002;39:537–545. doi: 10.1136/jmg.39.8.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sugimoto N., Oida T., Hirota K., Nakamura K., Nomura T., Uchiyama T., Sakaguchi S. Foxp3-dependent and -independent molecules specific for CD25+CD4+ natural regulatory T cells revealed by DNA microarray analysis. Int. Immunol. 2006;18:1197–1209. doi: 10.1093/intimm/dxl060. [DOI] [PubMed] [Google Scholar]
- 21.Ohkura N., Hamaguchi M., Morikawa H., Sugimura K., Tanaka A., Ito Y., Osaki M., Tanaka Y., Yamashita R., Nakano N., et al. T cell receptor stimulation-induced epigenetic changes and Foxp3 expression are independent and complementary events required for Treg cell development. Immunity. 2012;37:785–799. doi: 10.1016/j.immuni.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Gavin M.A., Rasmussen J.P., Fontenot J.D., Vasta V., Manganiello V.C., Beavo J.A., Rudensky A.Y. Foxp3-dependent programme of regulatory T-cell differentiation. Nature. 2007;445:771–775. doi: 10.1038/nature05543. [DOI] [PubMed] [Google Scholar]
- 23.Hill J.A., Feuerer M., Tash K., Haxhinasto S., Perez J., Melamed R., Mathis D., Benoist C. Foxp3 transcription-factor-dependent and -independent regulation of the regulatory T cell transcriptional signature. Immunity. 2007;27:786–800. doi: 10.1016/j.immuni.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Groux H., O’Garra A., Bigler M., Rouleau M., Antonenko S., de Vries J.E., Roncarolo M.G. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 1997;389:737–742. doi: 10.1038/39614. [DOI] [PubMed] [Google Scholar]
- 25.Zheng Y., Josefowicz S.Z., Kas A., Chu T.T., Gavin M.A., Rudensky A.Y. Genome-wide analysis of Foxp3 target genes in developing and mature regulatory T cells. Nature. 2007;445:936–940. doi: 10.1038/nature05563. [DOI] [PubMed] [Google Scholar]
- 26.Williams L.M., Rudensky A.Y. Maintenance of the Foxp3-dependent developmental program in mature regulatory T cells requires continued expression of Foxp3. Nat. Immunol. 2007;8:277–284. doi: 10.1038/ni1437. [DOI] [PubMed] [Google Scholar]
- 27.Zheng Y., Josefowicz S., Chaudhry A., Peng X.P., Forbush K., Rudensky A.Y. Role of conserved non-coding DNA elements in the Foxp3 gene in regulatory T-cell fate. Nature. 2010;463:808–812. doi: 10.1038/nature08750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yue X., Trifari S., Aijo T., Tsagaratou A., Pastor W.A., Zepeda-Martinez J.A., Lio C.W., Li X., Huang Y., Vijayanand P., et al. Control of Foxp3 stability through modulation of TET activity. J. Exp. Med. 2016;213:377–397. doi: 10.1084/jem.20151438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li X., Liang Y., LeBlanc M., Benner C., Zheng Y. Function of a Foxp3 cis-element in protecting regulatory T cell identity. Cell. 2014;158:734–748. doi: 10.1016/j.cell.2014.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soper D.M., Kasprowicz D.J., Ziegler S.F. IL-2Rbeta links IL-2R signaling with Foxp3 expression. Eur. J. Immunol. 2007;37:1817–1826. doi: 10.1002/eji.200737101. [DOI] [PubMed] [Google Scholar]
- 31.Burchill M.A., Yang J., Vogtenhuber C., Blazar B.R., Farrar M.A. IL-2 receptor beta-dependent STAT5 activation is required for the development of Foxp3+ regulatory T cells. J. Immunol. 2007;178:280–290. doi: 10.4049/jimmunol.178.1.280. [DOI] [PubMed] [Google Scholar]
- 32.Feng Y., Arvey A., Chinen T., van der Veeken J., Gasteiger G., Rudensky A.Y. Control of the inheritance of regulatory T cell identity by a cis element in the Foxp3 locus. Cell. 2014;158:749–763. doi: 10.1016/j.cell.2014.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Floess S., Freyer J., Siewert C., Baron U., Olek S., Polansky J., Schlawe K., Chang H.D., Bopp T., Schmitt E., et al. Epigenetic control of the foxp3 locus in regulatory T cells. PLoS Biol. 2007;5:e38. doi: 10.1371/journal.pbio.0050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baron U., Floess S., Wieczorek G., Baumann K., Grutzkau A., Dong J., Thiel A., Boeld T.J., Hoffmann P., Edinger M., et al. DNA demethylation in the human FOXP3 locus discriminates regulatory T cells from activated FOXP3+ conventional T cells. Eur. J. Immunol. 2007;37:2378–2389. doi: 10.1002/eji.200737594. [DOI] [PubMed] [Google Scholar]
- 35.Ohkura N., Sakaguchi S. Transcriptional and epigenetic basis of Treg cell development and function: Its genetic anomalies or variations in autoimmune diseases. Cell Res. 2020;30:465–474. doi: 10.1038/s41422-020-0324-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helmin K.A., Morales-Nebreda L., Torres Acosta M.A., Anekalla K.R., Chen S.Y., Abdala-Valencia H., Politanska Y., Cheresh P., Akbarpour M., Steinert E.M., et al. Maintenance DNA methylation is essential for regulatory T cell development and stability of suppressive function. J. Clin. Investig. 2020;130:6571–6587. doi: 10.1172/JCI137712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mikami N., Kawakami R., Chen K.Y., Sugimoto A., Ohkura N., Sakaguchi S. Epigenetic conversion of conventional T cells into regulatory T cells by CD28 signal deprivation. Proc. Natl. Acad. Sci. USA. 2020;117:12258–12268. doi: 10.1073/pnas.1922600117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duarte J.H., Zelenay S., Bergman M.L., Martins A.C., Demengeot J. Natural Treg cells spontaneously differentiate into pathogenic helper cells in lymphopenic conditions. Eur. J. Immunol. 2009;39:948–955. doi: 10.1002/eji.200839196. [DOI] [PubMed] [Google Scholar]
- 39.Kastner L., Dwyer D., Qin F.X. Synergistic effect of IL-6 and IL-4 in driving fate revision of natural Foxp3+ regulatory T cells. J. Immunol. 2010;185:5778–5786. doi: 10.4049/jimmunol.0901948. [DOI] [PubMed] [Google Scholar]
- 40.Zhou X., Bailey-Bucktrout S.L., Jeker L.T., Penaranda C., Martinez-Llordella M., Ashby M., Nakayama M., Rosenthal W., Bluestone J.A. Instability of the transcription factor Foxp3 leads to the generation of pathogenic memory T cells in vivo. Nat. Immunol. 2009;10:1000–1007. doi: 10.1038/ni.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koch M.A., Tucker-Heard G., Perdue N.R., Killebrew J.R., Urdahl K.B., Campbell D.J. The transcription factor T-bet controls regulatory T cell homeostasis and function during type 1 inflammation. Nat. Immunol. 2009;10:595–602. doi: 10.1038/ni.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Butcher M.J., Filipowicz A.R., Waseem T.C., McGary C.M., Crow K.J., Magilnick N., Boldin M., Lundberg P.S., Galkina E.V. Atherosclerosis-Driven Treg Plasticity Results in Formation of a Dysfunctional Subset of Plastic IFNgamma+ Th1/Tregs. Circ. Res. 2016;119:1190–1203. doi: 10.1161/CIRCRESAHA.116.309764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oldenhove G., Bouladoux N., Wohlfert E.A., Hall J.A., Chou D., Dos Santos L., O’Brien S., Blank R., Lamb E., Natarajan S., et al. Decrease of Foxp3+ Treg cell number and acquisition of effector cell phenotype during lethal infection. Immunity. 2009;31:772–786. doi: 10.1016/j.immuni.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rubtsov Y.P., Niec R.E., Josefowicz S., Li L., Darce J., Mathis D., Benoist C., Rudensky A.Y. Stability of the regulatory T cell lineage in vivo. Science. 2010;329:1667–1671. doi: 10.1126/science.1191996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Setoguchi R., Hori S., Takahashi T., Sakaguchi S. Homeostatic maintenance of natural Foxp3+ CD25+ CD4+ regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J. Exp. Med. 2005;201:723–735. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shi H., Chi H. Metabolic Control of Treg Cell Stability, Plasticity, and Tissue-Specific Heterogeneity. Front. Immunol. 2019;10:2716. doi: 10.3389/fimmu.2019.02716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Komatsu N., Okamoto K., Sawa S., Nakashima T., Oh-hora M., Kodama T., Tanaka S., Bluestone J.A., Takayanagi H. Pathogenic conversion of Foxp3+ T cells into TH17 cells in autoimmune arthritis. Nat. Med. 2014;20:62–68. doi: 10.1038/nm.3432. [DOI] [PubMed] [Google Scholar]
- 48.Li J., McArdle S., Gholami A., Kimura T., Wolf D., Gerhardt T., Miller J., Weber C., Ley K. CCR5+T-bet+FoxP3+ Effector CD4 T Cells Drive Atherosclerosis. Circ. Res. 2016;118:1540–1552. doi: 10.1161/CIRCRESAHA.116.308648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miyao T., Floess S., Setoguchi R., Luche H., Fehling H.J., Waldmann H., Huehn J., Hori S. Plasticity of Foxp3+ T cells reflects promiscuous Foxp3 expression in conventional T cells but not reprogramming of regulatory T cells. Immunity. 2012;36:262–275. doi: 10.1016/j.immuni.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 50.Komatsu N., Mariotti-Ferrandiz M.E., Wang Y., Malissen B., Waldmann H., Hori S. Heterogeneity of natural Foxp3+ T cells: A committed regulatory T-cell lineage and an uncommitted minor population retaining plasticity. Proc. Natl. Acad. Sci. USA. 2009;106:1903–1908. doi: 10.1073/pnas.0811556106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tan T.G., Mathis D., Benoist C. Singular role for T-BET+CXCR3+ regulatory T cells in protection from autoimmune diabetes. Proc. Natl. Acad. Sci. USA. 2016;113:14103–14108. doi: 10.1073/pnas.1616710113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bovenschen H.J., van de Kerkhof P.C., van Erp P.E., Woestenenk R., Joosten I., Koenen H.J. Foxp3+ regulatory T cells of psoriasis patients easily differentiate into IL-17A-producing cells and are found in lesional skin. J. Investig. Derm. 2011;131:1853–1860. doi: 10.1038/jid.2011.139. [DOI] [PubMed] [Google Scholar]
- 53.Qiu R., Zhou L., Ma Y., Zhou L., Liang T., Shi L., Long J., Yuan D. Regulatory T Cell Plasticity and Stability and Autoimmune Diseases. Clin. Rev. Allergy Immunol. 2020;58:52–70. doi: 10.1007/s12016-018-8721-0. [DOI] [PubMed] [Google Scholar]
- 54.Wollenberg I., Agua-Doce A., Hernandez A., Almeida C., Oliveira V.G., Faro J., Graca L. Regulation of the germinal center reaction by Foxp3+ follicular regulatory T cells. J. Immunol. 2011;187:4553–4560. doi: 10.4049/jimmunol.1101328. [DOI] [PubMed] [Google Scholar]
- 55.Zheng Y., Chaudhry A., Kas A., deRoos P., Kim J.M., Chu T.T., Corcoran L., Treuting P., Klein U., Rudensky A.Y. Regulatory T-cell suppressor program co-opts transcription factor IRF4 to control T(H)2 responses. Nature. 2009;458:351–356. doi: 10.1038/nature07674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hall A.O., Beiting D.P., Tato C., John B., Oldenhove G., Lombana C.G., Pritchard G.H., Silver J.S., Bouladoux N., Stumhofer J.S., et al. The cytokines interleukin 27 and interferon-gamma promote distinct Treg cell populations required to limit infection-induced pathology. Immunity. 2012;37:511–523. doi: 10.1016/j.immuni.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Linterman M.A., Pierson W., Lee S.K., Kallies A., Kawamoto S., Rayner T.F., Srivastava M., Divekar D.P., Beaton L., Hogan J.J., et al. Foxp3+ follicular regulatory T cells control the germinal center response. Nat. Med. 2011;17:975–982. doi: 10.1038/nm.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chung Y., Tanaka S., Chu F., Nurieva R.I., Martinez G.J., Rawal S., Wang Y.H., Lim H., Reynolds J.M., Zhou X.H., et al. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat. Med. 2011;17:983–988. doi: 10.1038/nm.2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Feil R., Wagner J., Metzger D., Chambon P. Regulation of Cre recombinase activity by mutated estrogen receptor ligand-binding domains. Biochem. Biophys. Res. Commun. 1997;237:752–757. doi: 10.1006/bbrc.1997.7124. [DOI] [PubMed] [Google Scholar]
- 60.Josefowicz S.Z., Niec R.E., Kim H.Y., Treuting P., Chinen T., Zheng Y., Umetsu D.T., Rudensky A.Y. Extrathymically generated regulatory T cells control mucosal TH2 inflammation. Nature. 2012;482:395–399. doi: 10.1038/nature10772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang Z., Zhang W., Guo J., Gu Q., Zhu X., Zhou X. Activation and Functional Specialization of Regulatory T Cells Lead to the Generation of Foxp3 Instability. J. Immunol. 2017;198:2612–2625. doi: 10.4049/jimmunol.1601409. [DOI] [PubMed] [Google Scholar]
- 62.Barbi J., Pardoll D., Pan F. Treg functional stability and its responsiveness to the microenvironment. Immunol. Rev. 2014;259:115–139. doi: 10.1111/imr.12172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Guo H., Xun L., Zhang R., Hu F., Luan J., Lao K., Wang X., Gou X. Stability and inhibitory function of Treg cells under inflammatory conditions in vitro. Exp. Ther. Med. 2019;18:2443–2450. doi: 10.3892/etm.2019.7873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhao J., Zhao J., Perlman S. Differential effects of IL-12 on Tregs and non-Treg T cells: Roles of IFN-gamma, IL-2 and IL-2R. PLoS ONE. 2012;7:e46241. doi: 10.1371/journal.pone.0046241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kawahata K., Misaki Y., Yamauchi M., Tsunekawa S., Setoguchi K., Miyazaki J., Yamamoto K. Generation of CD4+CD25+ regulatory T cells from autoreactive T cells simultaneously with their negative selection in the thymus and from nonautoreactive T cells by endogenous TCR expression. J. Immunol. 2002;168:4399–4405. doi: 10.4049/jimmunol.168.9.4399. [DOI] [PubMed] [Google Scholar]
- 66.Gabrysova L., Christensen J.R., Wu X., Kissenpfennig A., Malissen B., O’Garra A. Integrated T-cell receptor and costimulatory signals determine TGF-beta-dependent differentiation and maintenance of Foxp3+ regulatory T cells. Eur. J. Immunol. 2011;41:1242–1248. doi: 10.1002/eji.201041073. [DOI] [PubMed] [Google Scholar]
- 67.Sauer S., Bruno L., Hertweck A., Finlay D., Leleu M., Spivakov M., Knight Z.A., Cobb B.S., Cantrell D., O’Connor E., et al. T cell receptor signaling controls Foxp3 expression via PI3K, Akt, and mTOR. Proc. Natl. Acad. Sci. USA. 2008;105:7797–7802. doi: 10.1073/pnas.0800928105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haxhinasto S., Mathis D., Benoist C. The AKT-mTOR axis regulates de novo differentiation of CD4+Foxp3+ cells. J. Exp. Med. 2008;205:565–574. doi: 10.1084/jem.20071477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hoffmann P., Boeld T.J., Eder R., Huehn J., Floess S., Wieczorek G., Olek S., Dietmaier W., Andreesen R., Edinger M. Loss of FOXP3 expression in natural human CD4+CD25+ regulatory T cells upon repetitive in vitro stimulation. Eur. J. Immunol. 2009;39:1088–1097. doi: 10.1002/eji.200838904. [DOI] [PubMed] [Google Scholar]
- 70.Zhang Z., Zhou X. Foxp3 Instability Helps tTregs Distinguish Self and Non-self. Front. Immunol. 2019;10:2226. doi: 10.3389/fimmu.2019.02226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Smigiel K.S., Richards E., Srivastava S., Thomas K.R., Dudda J.C., Klonowski K.D., Campbell D.J. CCR7 provides localized access to IL-2 and defines homeostatically distinct regulatory T cell subsets. J. Exp. Med. 2014;211:121–136. doi: 10.1084/jem.20131142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zemmour D., Zilionis R., Kiner E., Klein A.M., Mathis D., Benoist C. Single-cell gene expression reveals a landscape of regulatory T cell phenotypes shaped by the TCR. Nat. Immunol. 2018;19:291–301. doi: 10.1038/s41590-018-0051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sprouse M.L., Scavuzzo M.A., Blum S., Shevchenko I., Lee T., Makedonas G., Borowiak M., Bettini M.L., Bettini M. High self-reactivity drives T-bet and potentiates Treg function in tissue-specific autoimmunity. JCI Insight. 2018;3:e97322. doi: 10.1172/jci.insight.97322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bettelli E., Carrier Y., Gao W., Korn T., Strom T.B., Oukka M., Weiner H.L., Kuchroo V.K. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 75.Zheng S.G., Wang J., Horwitz D.A. Cutting edge: Foxp3+CD4+CD25+ regulatory T cells induced by IL-2 and TGF-beta are resistant to Th17 conversion by IL-6. J. Immunol. 2008;180:7112–7116. doi: 10.4049/jimmunol.180.11.7112. [DOI] [PubMed] [Google Scholar]
- 76.Massoud A.H., Charbonnier L.M., Lopez D., Pellegrini M., Phipatanakul W., Chatila T.A. An asthma-associated IL4R variant exacerbates airway inflammation by promoting conversion of regulatory T cells to TH17-like cells. Nat. Med. 2016;22:1013–1022. doi: 10.1038/nm.4147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tarique M., Saini C., Naqvi R.A., Khanna N., Sharma A., Rao D.N. IL-12 and IL-23 modulate plasticity of FoxP3+ regulatory T cells in human Leprosy. Mol. Immunol. 2017;83:72–81. doi: 10.1016/j.molimm.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 78.Tang Q., Adams J.Y., Penaranda C., Melli K., Piaggio E., Sgouroudis E., Piccirillo C.A., Salomon B.L., Bluestone J.A. Central role of defective interleukin-2 production in the triggering of islet autoimmune destruction. Immunity. 2008;28:687–697. doi: 10.1016/j.immuni.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bailey-Bucktrout S.L., Martinez-Llordella M., Zhou X., Anthony B., Rosenthal W., Luche H., Fehling H.J., Bluestone J.A. Self-antigen-driven activation induces instability of regulatory T cells during an inflammatory autoimmune response. Immunity. 2013;39:949–962. doi: 10.1016/j.immuni.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ye C., Brand D., Zheng S.G. Targeting IL-2: An unexpected effect in treating immunological diseases. Signal. Transduct Target. Ther. 2018;3:2. doi: 10.1038/s41392-017-0002-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chambers E.S., Suwannasaen D., Mann E.H., Urry Z., Richards D.F., Lertmemongkolchai G., Hawrylowicz C.M. 1alpha,25-dihydroxyvitamin D3 in combination with transforming growth factor-beta increases the frequency of Foxp3+ regulatory T cells through preferential expansion and usage of interleukin-2. Immunology. 2014;143:52–60. doi: 10.1111/imm.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Urry Z., Chambers E.S., Xystrakis E., Dimeloe S., Richards D.F., Gabrysova L., Christensen J., Gupta A., Saglani S., Bush A., et al. The role of 1alpha, 25-dihydroxyvitamin D3 and cytokines in the promotion of distinct Foxp3+ and IL-10+ CD4+ T cells. Eur. J. Immunol. 2012;42:2697–2708. doi: 10.1002/eji.201242370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lu L., Lan Q., Li Z., Zhou X., Gu J., Li Q., Wang J., Chen M., Liu Y., Shen Y., et al. Critical role of all-trans retinoic acid in stabilizing human natural regulatory T cells under inflammatory conditions. Proc. Natl. Acad. Sci. USA. 2014;111:E3432–E3440. doi: 10.1073/pnas.1408780111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Puccetti P., Fallarino F. Generation of T cell regulatory activity by plasmacytoid dendritic cells and tryptophan catabolism. Blood Cells Mol. Dis. 2008;40:101–105. doi: 10.1016/j.bcmd.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 85.Schenk U., Frascoli M., Proietti M., Geffers R., Traggiai E., Buer J., Ricordi C., Westendorf A.M., Grassi F. ATP inhibits the generation and function of regulatory T cells through the activation of purinergic P2X receptors. Sci. Signal. 2011;4:ra12. doi: 10.1126/scisignal.2001270. [DOI] [PubMed] [Google Scholar]
- 86.Grassi F. The P2X7 Receptor as Regulator of T Cell Development and Function. Front. Immunol. 2020;11:1179. doi: 10.3389/fimmu.2020.01179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.DeBerardinis R.J., Thompson C.B. Cellular metabolism and disease: What do metabolic outliers teach us? Cell. 2012;148:1132–1144. doi: 10.1016/j.cell.2012.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Michalek R.D., Gerriets V.A., Jacobs S.R., Macintyre A.N., MacIver N.J., Mason E.F., Sullivan S.A., Nichols A.G., Rathmell J.C. Cutting edge: Distinct glycolytic and lipid oxidative metabolic programs are essential for effector and regulatory CD4+ T cell subsets. J. Immunol. 2011;186:3299–3303. doi: 10.4049/jimmunol.1003613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Angelin A., Gil-de-Gomez L., Dahiya S., Jiao J., Guo L., Levine M.H., Wang Z., Quinn W.J., 3rd, Kopinski P.K., Wang L., et al. Foxp3 Reprograms T Cell Metabolism to Function in Low-Glucose, High-Lactate Environments. Cell Metab. 2017;25:1282–1293.e1287. doi: 10.1016/j.cmet.2016.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gerriets V.A., Kishton R.J., Johnson M.O., Cohen S., Siska P.J., Nichols A.G., Warmoes M.O., de Cubas A.A., MacIver N.J., Locasale J.W., et al. Foxp3 and Toll-like receptor signaling balance Treg cell anabolic metabolism for suppression. Nat. Immunol. 2016;17:1459–1466. doi: 10.1038/ni.3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Huynh A., DuPage M., Priyadharshini B., Sage P.T., Quiros J., Borges C.M., Townamchai N., Gerriets V.A., Rathmell J.C., Sharpe A.H., et al. Control of PI(3) kinase in Treg cells maintains homeostasis and lineage stability. Nat. Immunol. 2015;16:188–196. doi: 10.1038/ni.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wei J., Long L., Yang K., Guy C., Shrestha S., Chen Z., Wu C., Vogel P., Neale G., Green D.R., et al. Autophagy enforces functional integrity of regulatory T cells by coupling environmental cues and metabolic homeostasis. Nat. Immunol. 2016;17:277–285. doi: 10.1038/ni.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shrestha S., Yang K., Guy C., Vogel P., Neale G., Chi H. Treg cells require the phosphatase PTEN to restrain TH1 and TFH cell responses. Nat. Immunol. 2015;16:178–187. doi: 10.1038/ni.3076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Weinberg S.E., Singer B.D., Steinert E.M., Martinez C.A., Mehta M.M., Martinez-Reyes I., Gao P., Helmin K.A., Abdala-Valencia H., Sena L.A., et al. Mitochondrial complex III is essential for suppressive function of regulatory T cells. Nature. 2019;565:495–499. doi: 10.1038/s41586-018-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chapman N.M., Zeng H., Nguyen T.M., Wang Y., Vogel P., Dhungana Y., Liu X., Neale G., Locasale J.W., Chi H. mTOR coordinates transcriptional programs and mitochondrial metabolism of activated Treg subsets to protect tissue homeostasis. Nat. Commun. 2018;9:2095. doi: 10.1038/s41467-018-04392-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wu D., Luo Y., Guo W., Niu Q., Xue T., Yang F., Sun X., Chen S., Liu Y., Liu J., et al. Lkb1 maintains Treg cell lineage identity. Nat. Commun. 2017;8:15876. doi: 10.1038/ncomms15876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Timilshina M., You Z., Lacher S.M., Acharya S., Jiang L., Kang Y., Kim J.A., Chang H.W., Kim K.J., Park B., et al. Activation of Mevalonate Pathway via LKB1 Is Essential for Stability of Treg Cells. Cell Rep. 2019;27:2948–2961.e7. doi: 10.1016/j.celrep.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 98.Zeng H., Yang K., Cloer C., Neale G., Vogel P., Chi H. mTORC1 couples immune signals and metabolic programming to establish T(reg)-cell function. Nature. 2013;499:485–490. doi: 10.1038/nature12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stancu C., Sima A. Statins: Mechanism of action and effects. J. Cell Mol. Med. 2001;5:378–387. doi: 10.1111/j.1582-4934.2001.tb00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Vallion R., Divoux J., Glauzy S., Ronin E., Lombardi Y., Lubrano di Ricco M., Gregoire S., Nemazanyy I., Durand A., Fradin D., et al. Regulatory T Cell Stability and Migration Are Dependent on mTOR. J. Immunol. 2020;205:1799–1809. doi: 10.4049/jimmunol.1901480. [DOI] [PubMed] [Google Scholar]
- 101.Xu T., Stewart K.M., Wang X., Liu K., Xie M., Ryu J.K., Li K., Ma T., Wang H., Ni L., et al. Metabolic control of TH17 and induced Treg cell balance by an epigenetic mechanism. Nature. 2017;548:228–233. doi: 10.1038/nature23475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Klysz D., Tai X., Robert P.A., Craveiro M., Cretenet G., Oburoglu L., Mongellaz C., Floess S., Fritz V., Matias M.I., et al. Glutamine-dependent alpha-ketoglutarate production regulates the balance between T helper 1 cell and regulatory T cell generation. Sci. Signal. 2015;8:ra97. doi: 10.1126/scisignal.aab2610. [DOI] [PubMed] [Google Scholar]
- 103.Kitz A., de Marcken M., Gautron A.S., Mitrovic M., Hafler D.A., Dominguez-Villar M. AKT isoforms modulate Th1-like Treg generation and function in human autoimmune disease. EMBO Rep. 2016;17:1169–1183. doi: 10.15252/embr.201541905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kerdiles Y.M., Stone E.L., Beisner D.R., McGargill M.A., Ch’en I.L., Stockmann C., Katayama C.D., Hedrick S.M. Foxo transcription factors control regulatory T cell development and function. Immunity. 2010;33:890–904. doi: 10.1016/j.immuni.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ouyang W., Beckett O., Ma Q., Paik J.H., DePinho R.A., Li M.O. Foxo proteins cooperatively control the differentiation of Foxp3+ regulatory T cells. Nat. Immunol. 2010;11:618–627. doi: 10.1038/ni.1884. [DOI] [PubMed] [Google Scholar]
- 106.Harada Y., Harada Y., Elly C., Ying G., Paik J.H., DePinho R.A., Liu Y.C. Transcription factors Foxo3a and Foxo1 couple the E3 ligase Cbl-b to the induction of Foxp3 expression in induced regulatory T cells. J. Exp. Med. 2010;207:1381–1391. doi: 10.1084/jem.20100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Peng M., Yin N., Chhangawala S., Xu K., Leslie C.S., Li M.O. Aerobic glycolysis promotes T helper 1 cell differentiation through an epigenetic mechanism. Science. 2016;354:481–484. doi: 10.1126/science.aaf6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lu L.F., Boldin M.P., Chaudhry A., Lin L.L., Taganov K.D., Hanada T., Yoshimura A., Baltimore D., Rudensky A.Y. Function of miR-146a in controlling Treg cell-mediated regulation of Th1 responses. Cell. 2010;142:914–929. doi: 10.1016/j.cell.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gaddis D.E., Padgett L.E., Wu R., McSkimming C., Romines V., Taylor A.M., McNamara C.A., Kronenberg M., Crotty S., Thomas M.J., et al. Apolipoprotein AI prevents regulatory to follicular helper T cell switching during atherosclerosis. Nat. Commun. 2018;9:1095. doi: 10.1038/s41467-018-03493-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wolf D., Gerhardt T., Winkels H., Anto Michel N., Pramod A.B., Ghosheh Y., Brunel S., Buscher K., Miller J., McArdle S., et al. Pathogenic Autoimmunity in Atherosclerosis Evolves from Initially Protective ApoB-Reactive CD4+ T-Regulatory Cells. Circulation. 2020;142:1279–1293. doi: 10.1161/CIRCULATIONAHA.119.042863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xu J., Yang Y., Qiu G., Lal G., Wu Z., Levy D.E., Ochando J.C., Bromberg J.S., Ding Y. c-Maf regulates IL-10 expression during Th17 polarization. J. Immunol. 2009;182:6226–6236. doi: 10.4049/jimmunol.0900123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Neumann C., Blume J., Roy U., Teh P.P., Vasanthakumar A., Beller A., Liao Y., Heinrich F., Arenzana T.L., Hackney J.A., et al. c-Maf-dependent Treg cell control of intestinal TH17 cells and IgA establishes host-microbiota homeostasis. Nat. Immunol. 2019;20:471–481. doi: 10.1038/s41590-019-0316-2. [DOI] [PubMed] [Google Scholar]
- 113.Mor A., Planer D., Luboshits G., Afek A., Metzger S., Chajek-Shaul T., Keren G., George J. Role of naturally occurring CD4+ CD25+ regulatory T cells in experimental atherosclerosis. Arter. Thromb. Vasc. Biol. 2007;27:893–900. doi: 10.1161/01.ATV.0000259365.31469.89. [DOI] [PubMed] [Google Scholar]
- 114.Mor A., Luboshits G., Planer D., Keren G., George J. Altered status of CD4+CD25+ regulatory T cells in patients with acute coronary syndromes. Eur. Heart J. 2006;27:2530–2537. doi: 10.1093/eurheartj/ehl222. [DOI] [PubMed] [Google Scholar]
- 115.Mailer R.K.W., Gistera A., Polyzos K.A., Ketelhuth D.F.J., Hansson G.K. Hypercholesterolemia Induces Differentiation of Regulatory T Cells in the Liver. Circ. Res. 2017;120:1740–1753. doi: 10.1161/CIRCRESAHA.116.310054. [DOI] [PubMed] [Google Scholar]
- 116.Parathath S., Mick S.L., Feig J.E., Joaquin V., Grauer L., Habiel D.M., Gassmann M., Gardner L.B., Fisher E.A. Hypoxia is present in murine atherosclerotic plaques and has multiple adverse effects on macrophage lipid metabolism. Circ. Res. 2011;109:1141–1152. doi: 10.1161/CIRCRESAHA.111.246363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dang E.V., Barbi J., Yang H.Y., Jinasena D., Yu H., Zheng Y., Bordman Z., Fu J., Kim Y., Yen H.R., et al. Control of T(H)17/T(reg) balance by hypoxia-inducible factor 1. Cell. 2011;146:772–784. doi: 10.1016/j.cell.2011.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lee J.H., Elly C., Park Y., Liu Y.C. E3 Ubiquitin Ligase VHL Regulates Hypoxia-Inducible Factor-1alpha to Maintain Regulatory T Cell Stability and Suppressive Capacity. Immunity. 2015;42:1062–1074. doi: 10.1016/j.immuni.2015.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Salminen A., Kauppinen A., Kaarniranta K. 2-Oxoglutarate-dependent dioxygenases are sensors of energy metabolism, oxygen availability, and iron homeostasis: Potential role in the regulation of aging process. Cell Mol. Life Sci. 2015;72:3897–3914. doi: 10.1007/s00018-015-1978-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kimura T., Kobiyama K., Winkels H., Tse K., Miller J., Vassallo M., Wolf D., Ryden C., Orecchioni M., Dileepan T., et al. Regulatory CD4+ T Cells Recognize MHC-II-Restricted Peptide Epitopes of Apolipoprotein B. Circulation. 2018;138:1130–1143. doi: 10.1161/CIRCULATIONAHA.117.031420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kimura T., Tse K., McArdle S., Gerhardt T., Miller J., Mikulski Z., Sidney J., Sette A., Wolf D., Ley K. Atheroprotective vaccination with MHC-II-restricted ApoB peptides induces peritoneal IL-10-producing CD4 T cells. Am. J. Physiol. Heart Circ. Physiol. 2017;312:H781–H790. doi: 10.1152/ajpheart.00798.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]