Abstract
Coronavirus disease 2019 (COVID-19) was recently declared a pandemic by the WHO. This outbreak threatens not only physical health but also has significant repercussions on mental health. In recent world history, major infectious outbreaks were associated with severe mental health sequelae, including suicide. In this study, we systematically review the literature on suicidal outcomes during major international respiratory outbreaks, including COVID-19. We reviewed descriptive and analytic articles addressing suicide during major international respiratory outbreaks. We searched PubMed, Medline, Embase, Scopus, and PsycInfo databases and then utilized an independent method for study selection by a pair of reviewers. Two reviewers completed data abstraction and conducted a narrative summary of the findings. Our search generated 2,153 articles. Nine studies (three descriptive, five analytical, and one with mixed methodology) were eligible. The included studies were heterogeneous, divergent in methods, and with a low degree of evidence. Deducing an association between pandemics, suicide, and suicide-related outcomes remains thus poorly supported. Future research with better methodological characteristics, the use of longitudinal studies, and a focus on suicide as the primary outcome would allow for an in-depth understanding and formulation of the scope of this problem.
Keywords: Suicide, Outbreak, Epidemic, Pandemic, COVID-19, Mental health.
1. Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease was first reported in December 2019 in Wuhan, central China (CDC, 2020; WHO, 2020a). It has rapidly spread since then and was declared a pandemic by WHO on March 11, 2020 (WHO, 2020b). In addition to its morbid effects on physical health, its impact on mental health might also be severe (Holmes et al., 2020).
Mental illness is a strong predictor of suicide (Gili et al., 2019; Harris and Barraclough, 1997). Most suicides worldwide are related to psychiatric diseases, depression constituting one of the most significant risk factors (Bachmann, 2018; Hawton et al., 2013). Alternatively, in recent world history, major infectious outbreaks were associated with severe mental health sequelae, including suicide. For instance, there is evidence that deaths by suicide increased in the USA during the 1918–19 influenza pandemic (Wasserman, 1992) and among older people in Hong Kong during the 2003 Severe Acute Respiratory Syndrome (SARS) epidemic (Cheung et al., 2008). Additionally, during the 2003 SARS outbreak in Singapore, almost one-quarter of medical workers reported psychiatric symptoms of depression, anxiety, and posttraumatic morbidity (Sim et al., 2004). Likewise, in 2015, Lee et al. showed that medical staff who performed tasks related to the Middle East Respiratory Syndrome (MERS) in Korea exhibited symptoms of post-traumatic stress disorder (PTSD) (Lee et al., 2018).
It can be hypothesized, in line with reports from previous respiratory outbreaks, that the current COVID-19 outbreak might cause a significant and global surge of mental health problems. Recent studies described emotional distress and psychiatric symptoms of depression and anxiety during the COVID-19 outbreak (Qiu et al., 2020; Wang et al., 2020). Some cases of suicidal acts related to the COVID-19 quarantine have also been reported (Ho et al., 2020). It is acknowledged that mental health deterioration during pandemics can stem from numerous factors. These include the constant fear of contracting the virus, contracting the virus, losing loved ones to the illness, as well as the impact of being quarantined. These factors can go on to precipitate mental illness in those without prior psychiatric history or can exacerbate the symptoms in those with a pre-existing mental illness (Ho et al., 2020).
We hypothesize that during outbreaks, including the current pandemic, individuals might be at increased risk of suicide. We set out to conduct a systematic review to test this hypothesis. Our goal was to synthesize descriptive and analytic evidence of suicide and suicide-related outcomes (ideations, intent, attempt, or completion) during major international respiratory outbreaks (COVID-19, MERS, SARS, and influenza A) in the recent history.
2. Methods
The protocol of this systematic review was registered at the International Prospective Register of Systematic Reviews PROSPERO (ID number 180977).
2.1. Eligibility criteria
Studies were considered eligible if they met the following criteria:
-
•
Population: Any individual who lived during a resolved or continuing major international respiratory outbreak, regardless of their age, gender, race, ethnicity, geographical location, profession, or other characteristics.
-
•
Exposure: Living during a major international respiratory outbreak over the past two decades (COVID-19, SARS, MERS, and Influenza A - H1N1, H2N2, and H3N2).
-
•
Outcomes: Suicide-related outcomes (suicidal ideation, intent, attempt, or completion).
-
•
Study design: Analytical (cross-sectional, case-control, or cohort) and descriptive (case report or case series) studies.
Studies assessing other outbreaks, studies having non-suicidal self-harm or self-mutilation and other-directed violence as outcomes, and studies that include reviews, letters, or correspondences were excluded. Studies not available in English or reported as abstracts for which the authors could not identify a full text after consultation with a medical librarian or contact with the corresponding author were also excluded.
2.2. Search strategy
PubMed, Medline, Embase, Scopus, and PsycInfo databases were searched from the day of inception until April 20, 2020. Filters were restricted to studies with a full text published in the English language. The search strategy and its relevant MESH terms are outlined in Supplementary Appendix 1. The search also included the references lists of reviews of interest identified during the preliminary search. The authors also hand-searched the reference lists of the final included studies and used Google Scholar to find articles that cited these studies.
2.3. Selection process
EndNote software version X9.2 was used to import all studies obtained from the literature search. After removing duplicate references, a pair of reviewers (KK and SEH) independently conducted the title and abstract screening of the obtained articles using a standardized screening guide. Any disagreement in this step was resolved by including the article in the full-text screening stage. The title and abstract screening step was followed by a full-text screening done by another pair of reviewers (MAC and SEH) using a standardized screening guide. Any disagreement was resolved by consensus and, if unsuccessful, by a discussion with a third reviewer (KK).
2.4. Data abstraction
Two reviewers (MAC and SEH) independently extracted and compared the data of interest from the full texts of the eligible studies. Studies were stratified according to their design (descriptive versus analytical). For each eligible descriptive study, the reviewers extracted the following information: design of the study, country of origin, contemporary outbreak, sample characteristics (number of cases, gender, age, and psychiatric history), and suicide characteristics (method and alleged reason). For each eligible analytical study, the reviewers extracted the following information: design of the study, country of origin, contemporary outbreak, methodology (recruitment strategy, recruitment site, and eligibility criteria), sample characteristics (number of cases, gender, and age), outcomes (suicide and suicide-related outcomes), and conflict of interest.
2.4.1. Risk of bias assessment
Two reviewers (MAC and SEH) independently assessed the risk of bias in each eligible quantitative study. They resolved any disagreement by consensus or, if unsuccessful, by a discussion with a third reviewer (KK). The criteria evaluated were based on the GRADE system for observational non-randomized studies (Guyatt et al., 2011).
2.5. Data synthesis
Although the authors planned to include a quantitative synthesis (meta-analysis) of the results from analytical studies, it was not possible to conduct it due to the heterogeneity and scarcity of the included studies. Instead, a qualitative synthesis of the study designs, populations, exposures, and outcomes was conducted.
3. Results
3.1. Search results
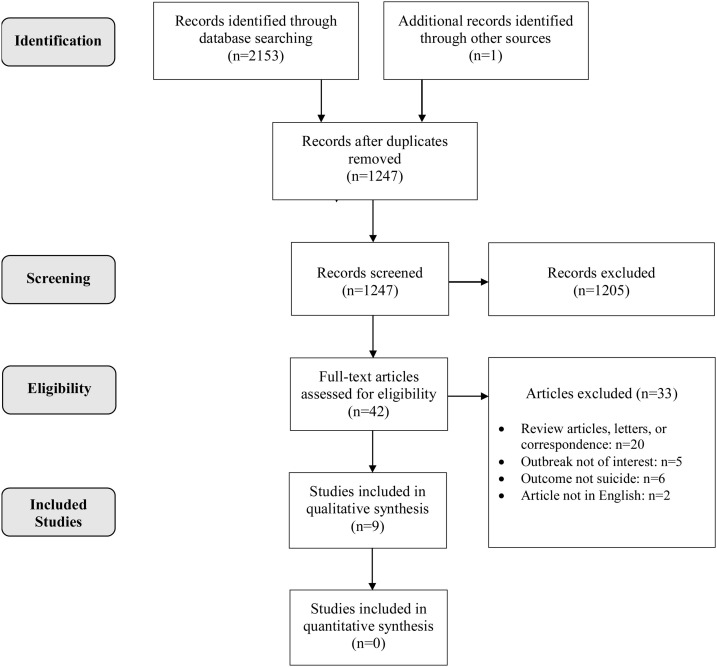
A total of 2,153 potentially eligible studies were obtained after the electronic search of the five databases. One additional record was obtained through the manual search of reference lists of included articles. After the removal of duplicates, a total of 1,247 records were processed via title and abstract screening. A total of 1,205 records were excluded. Of the remaining 42 articles, another 33 were further excluded after full-text screening for different reasons, as outlined in Fig. 1 . Nine studies remained for qualitative synthesis.
Fig. 1.
Systematic review flowchart. Nine studies were included in the qualitative synthesis.
3.2. Study characteristics
Of the included studies, three were descriptive case reports (Goyal et al., 2020; Mamun and Griffiths, 2020) and case series (Sahoo et al., 2020). Five studies were analytical with a cross-sectional design (Chan et al., 2006; Cheung et al., 2008; Huang et al., 2005; Lee, 2020; Okusaga et al., 2011) and one had both descriptive (case series) and analytical (cross-sectional) methods (Yip et al., 2010). The studies were carried out in five countries, with most of them originating from Mainland China and Hong Kong, while the remaining studies came from the USA, India, Bangladesh, and Taiwan.
3.3. Risk of bias
There was considerable bias in the methodological quality of the included non-randomized observational studies (see Supplementary Appendix 2). Based on GRADE 4 guidelines (Guyatt et al., 2011), only two out of the six quantitative studies were considered to have a low risk of bias, whereas the remaining four had moderate risk.
3.4. Synthesis of results
3.4.1. Descriptive studies
Descriptive studies tackling suicide during major international respiratory outbreaks included two major pandemics: COVID-19 and SARS. In the former, three cases from India (Goyal et al., 2020; Sahoo et al., 2020) and one from Bangladesh (Mamun and Griffiths, 2020) described middle-aged men who committed suicide either by hanging or using a gun. Three of these studies did not report on previous psychiatric history. On the other hand, in the SARS outbreak case series (Yip et al., 2010), 22 cases of suicide in older males and females occurred; three had a past psychiatric history. The major themes that emerged as alleged reasons for committing suicide included fear of contracting the infection, fear of transmitting it, fear of having a painful death secondary to it, and fear of social isolation. A summary of the descriptive studies is presented in Table 1 .
Table 1.
Summary of descriptive studies tackling suicide-related outcomes during major international outbreaks of respiratory viruses.
| Study | Type | Country | Outbreak | Number | Gender | Age (years) | Suicide method | Reason for suicide | Psychiatric history |
|---|---|---|---|---|---|---|---|---|---|
| Mamun and Griffiths (2020) | Case report | Bangladesh | COVID-19 | 1 | Male | 36 | Hanging from a tree | Moral duty of not passing the suspected COVID-19 infection to the inhabitants of the village | Not mentioned |
| Goyal et al. (2020) | Case report | India | COVID-19 | 1 | Male | 50 | Hanging from a tree | Fear and panic of having acquired COVID-19 infection | Not mentioned |
| Sahoo et al. (2020) | Case series | India | COVID-19 | 2 | Male | 52 | Shooting self in the abdomen | Worries of being infected by COVID-19 from a friend carrying the virus, followed by the development of depressive symptoms after two weeks of isolation to prevent the spread of any infection to family members, and excessive fear of having a painful death from COVID-19 | No previous psychiatric history |
| Male | 40 | Hanging with a rope | Worries of being infected by COVID-19 from foreigners, followed by the development of depressive symptoms over two weeks period, self-isolation, and excessive fear of having a painful death from COVID-19 | Not mentioned | |||||
| Yip et al. (2010) | Case series | China | SARS | 22 | 11 males 11 females |
74.9 ± 5.72 (Mean ± standard deviation) |
Jumping from a height (n = 2) Otherwise not specified |
Fear of contracting SARS (n = 12): negative news about SARS (especially the death toll among elderly) causing worries about getting infected, avoiding hospital admission due to fear of a higher risk of infection, and feelings of a burden and risk to family | Depression and anxiety (n = 2) |
| Fear of social isolation (n = 7): reduced contact with others and disruption of normal life | Schizophrenia (n = 1) | ||||||||
| Disease burden among those with long-term illnesses (n = 6): associated unpleasant emotions and feelings of burden from the chronic illness |
3.4.2. Analytical studies
Analytical studies assessing suicidal outcomes during major international respiratory outbreaks mostly addressed SARS. Three studies were based on a chart review of either death or suicide cases in Hong Kong (Chan et al., 2006; Cheung et al., 2008; Yip et al., 2010). In contrast, the fourth assessed the emergency department visits at a tertiary hospital in Taiwan (Huang et al., 2005). Both Chan et al. and Cheung et al. showed a statistically significant increase in the older adults' suicide rate in 2003, the year of the SARS outbreak, compared to prior years (Chan et al., 2006; Cheung et al., 2008). This was maintained in 2004, suggesting that the suicide rate did not return to its baseline before the SARS epidemic (Cheung et al., 2008). Along the same lines, in Taiwan, the mean numbers of patients presenting to the emergency department for a suicide attempt with drug overdose were greater, although not significantly, during the peak-outbreak stage compared to all other stages (Huang et al., 2005). While comparing SARS-related to non-SARS related suicides, Yip et al. showed no difference in psychiatric profiles. Nonetheless, higher social disconnection and fear of contracting the illness were detected in the former group (Yip et al., 2010). One study that aimed to validate a scale for anxiety towards COVID-19 reported on an individual expressing passive death wishes (Lee, 2020). Lastly, one cross-sectional study assessed for an association between seropositivity to influenza A, B, and coronaviruses and suicidality in patients with mood disorders (Okusaga et al., 2011). Results showed that a significantly greater percentage of individuals who attempted suicide were seropositive for influenza A, influenza B, and coronavirus in comparison to healthy controls. However, among individuals with a history of mood disorder, only seropositivity for influenza B was significantly associated with a history of suicide attempt (Okusaga et al., 2011). A summary of the analytical studies is presented in Table 2 a and b.
Table 2.
Summary of analytical studies tackling suicide-related outcomes during major international outbreaks of respiratory viruses.
| a. General characteristics and methodology of the included analytical studies. | |||||||
|---|---|---|---|---|---|---|---|
| Study | Type | Country | Outbreak | Methodology |
Conflict of interest | ||
| Recruitment strategy | Recruitment site | Eligibility criteria | |||||
| Lee (2020) | Cross-sectional | United States | COVID-19 | Online survey data collected from March 11 to March 13, 2020 | Participants recruited through Amazon MTurk in exchange forpayment ($0.50) | Participants were eligible if they provided consent and complete information, followed the directions to a validity item, had spent at least one hour during the past two weeks thinking about and/or watching media about COVID-19, and had experienced significant anxiety, fear, or worry about the disease outbreak. | None |
| Okusaga et al. (2011) | Cross-sectional | United States | Influenza A, B, and coronavirus | Participants recruited from two studies of environmental influences on mood disorders and suicidal behavior (studies not mentioned within the manuscript) | Participants recruited from the University of Maryland, Johns Hopkins University, and the Sheppard Pratt Health System | Patients were eligible if they met criteria for major depressive or bipolar disorder according to the Structured Clinical Interview for DSM-IV Disorders. Suicide attempts were recorded using the Columbia Suicide History Form. | None |
| Patients meeting criteria for substance dependence, cognitive disorders, or primary psychotic disorders were excluded. | |||||||
| Yip et al. (2010) | Cross-sectional | China | SARS | Chart review of death case records in the year 2003 | Death records obtained from the Coroner’s Court in Hong Kong | Case records were eligible if they contained suicide notes and witnesses’ descriptions of the suicide deaths (ICD10: X60-X84). Wherever SARS was mentioned as being crucial to the suicide act and was included in the police death investigation, the suicide death was defined as a SARS-related case. Non-SARS-related cases were then randomly selected for comparison. | Not mentioned |
| Cheung et al. (2008) | Cross-sectional | China | SARS | Chart review of suicide case records for the period 1993–2004 | Suicide records obtained from the Coroner’s Court in Hong Kong | No reported inclusion or exclusion criteria. | None |
| Case records contained sociodemographic, medical, and psychosocial data gathered from police investigations and medical institutions. Information about suicide was obtained from suicide notes, interviews, and witness reports. | |||||||
| Chan et al. (2006) | Cross-sectional | China | SARS | Chart review of suicide case records for the period 1986–2003 | Suicide records obtained from the Census and Statistics Department of the Government of Hong Kong Special Administrative Region | Deaths labeled as “of undetermined cause” were excluded from the analysis. | Not mentioned |
| Huang et al. (2005) | Cross-sectional | Taiwan | SARS | Retrospective chart review from March 14 to August 31, 2003 | Charts obtained from the emergency department of Taipei Veterans General Hospital, a tertiary referral and teaching medical center in northern Taiwan | Patients younger than 14 years were excluded. | Not mentioned |
| Patient information was reviewed and compared for different stages of the SARS epidemic (pre-epidemic, early epidemic, peak epidemic, late epidemic, and post-epidemic stages). | |||||||
| b. Outcomes of the included analytical studies. | |||||
|---|---|---|---|---|---|
| Study | Sample size | Gender | Age | Suicide-related outcomes | Other relevant outcomes |
| Lee (2020) | 775 | 446 males | Passive suicidal ideation (measured by the item: “I wished I was already dead, so I did not have to deal with the coronavirus”): | In terms of significant anxiety or worry about the coronavirus during the past two weeks, most participants spent several days feeling elevated anxiety (36.5%), followed by more than seven days feeling elevated anxiety (27.0%), less than a day or two feeling elevated anxiety (22.8%), and nearly every day feeling elevated anxiety (13.7%). | |
| 329 females | 1.58 ± 1.46 (reported as mean ± SD) | ||||
| Okusaga et al. (2011) | 257 | 95 males | 32.72 ± 9.35 18 to 65 | A more significant percentage of individuals in the suicide attempt group were seropositive for influenza A (p = 0.006), influenza B (p < 0.0001), and coronavirus (p < 0.0001) in comparison to healthy controls. | There were statistically significant associations between seropositivity for influenza A, influenza B, coronaviruses, and the diagnosis of a major depressive disorder. |
| 162 females | Among individuals with a history of mood disorder, seropositivity for influenza B, but not for influenza A or coronaviruses, was significantly associated with a history of suicide attempt (p = 0.001). The odds of having attempted suicide were increased in influenza B seropositive individuals (OR = 2.53, CI 1.33-4.80). | The odds of having a history of mood disorder were increased with seropositivity for influenza A, influenza B, and coronaviruses. | |||
| Seropositivity for influenza B, but not for influenza A or coronaviruses, was significantly associated with the presence of a history of psychotic symptoms in mood disorder patients. | |||||
| Yip et al. (2010) | 66 (SARS-related: 22, Non-SARS-related: 44) | 33 males 33 females (For each: SARS-related: 11, Non-SARS-related: 22) |
SARS-related: 74.9 ± 5.72 Non-SARS-related: 74.75 ± 6.77 |
Sociodemographic factors, employment status, and medical and psychiatric profiles were insignificantly different between the SARS and non-SARS groups. | None |
| Disconnection (p = 0.002) and fear of contracting SARS (p<0.001) were significantly more common in the SARS compared to the non-SARS group. | |||||
| Cheung et al. (2008) | Not applicable | Not applicable | 65 and above | There was a decreasing trend of elderly suicide rates from 1993 (39.19 per 100,000) to 2002 (28.44 per 100,000), whereas the rate drastically climbed up to 40.35 per 100,000 in 2003 and maintained a high in 2004 (33.95 per 100,000). | The overall severity of illness (p < 0.001), level of dependency (p < 0.013), and worrying about having sickness (p < 0.021) among the older adult suicides were found to be significantly different in the pre-SARS, peri-SARS, and post-SARS periods. |
| The monthly older adult suicide rate in April 2003 was significantly higher than those in April 1993, 1997, 1998, 2001, and 2002. It was also significantly higher than that in June 2003, which suggested the disappearance of the usual summer peak and that some of the suicides might have been brought forward. | |||||
| The annual older adult suicide rate in 2003 was significantly higher than in 1996 and 1998-2002. The annual older adult suicide rate in 2004 was also significantly higher than in 2002 (yet lower than in 2003), suggesting that the suicide rate did not return to the level before the SARS epidemic. | |||||
| Chan et al. (2006) | Not applicable | Not applicable | Stratified as below and above 65 | Suicide rates of elders aged 65 and above in 1986–1997 were significantly higher than in 2002, with an Incident Rate Ratio (IRR) of 1.34 to 1.61. Suicide rates in 1998–2001 did not differ from 2002, representing the stabilization of rates for four years after 1997. Elderly suicide rate increased to 37.46/100,000 in 2003, with an IRR of 1.32 relative to 2002 (p < 0.0019). | The peak number of suicides in elders aged 65 and above occurred in April 2003, a month after the SARS outbreak began. |
| Such a trend remained significant when female elderly (but not male elderly or the age group below 65) suicide rates in 1993–2003 were analyzed. | |||||
| Huang et al. (2005) | 17,586 | Reported percentage in males: 62.7 ± 3.8 to 65.6 ± 3.9, according to epidemic stage | 54.6 ± 3.2 to 57.0 ± 3.1, according to epidemic stage | The mean numbers of patients attending the emergency department with a principal diagnosis of suicide attempt via drug overdose were higher during the peak-epidemic stage than all other epidemic stages. However, these differences were not statistically significant. | The total percentage of patients in the “Psychiatric problem/disease” diagnostic category who attended the emergency department did not significantly change across the various stages of the epidemic. |
4. Discussion
In this systematic review, we investigated scientific literature reporting cases of suicide and suicide-related outcomes during major international respiratory outbreaks. Most of the generated studies emanated from two outbreaks: the current COVID-19 pandemic and SARS. We have postulated that, in such difficult circumstances, the risk of suicide might increase. The included studies were heterogeneous and divergent in methodologies: descriptive studies of case reports and series described instances of suicide during outbreaks; these included either middle-aged or older adults. Of the alleged reasons for suicide, fear from the infection, worries about others, and social isolation were reported. Some of the analytical studies, on the other hand, hinted towards older adults being at higher risk for suicide. However, due to the limited nature of these studies, all being cross-sectional, the evidence for this argument is rather limited. As such, deducing an association between outbreaks and suicide remains, so far, unwarranted.
A few studies have recently addressed the effect of COVID-19 on psychological distress and psychiatric symptoms. A large-scale survey was designed in China to survey peritraumatic psychological distress during the tumultuous time of the COVID-19 outbreak (Qiu et al., 2020). The COVID-19 Peritraumatic Distress Index, based on the International Classification of Disease (11th revision) and expert opinions from psychiatrists, inquired about the frequency of anxiety, depression, and specific phobias, amongst other symptoms over one week. One-third of the respondents experienced moderate to severe psychological distress. Also, psychological distress was highest among migrant workers and in regions that lacked adequate medical resources or effective governmental control measures (Qiu et al., 2020). In an online survey assessing psychological impact during the COVID-19 outbreak, half of the participants rated the psychological effect of the epidemic as moderate to severe, as per the Impact of Event Scale-Revised (IES-R) (Wang et al., 2020). Besides, about one-quarter of respondents reported moderate-to-severe depressive and anxiety symptoms, as assessed by the Depression, Anxiety and Stress Scale (Wang et al., 2020).
On the other hand, the impact of SARS on mental health has been more widely studied. Wu et al. examined the occurrence rate of PTSD, anxiety, and depression among SARS survivors one month after their discharge from the hospital (Wu et al., 2005). From the sample of 195 participants, 6% met the cutoff for PTSD as per the IES-R. Also, using the Hospital Anxiety and Depression Scale (HADS), 14 % and 18 % met the cutoff for anxiety and depression, respectively (Wu et al., 2005). In a cohort study investigating psychiatric complications among SARS survivors 30 months after the outbreak, the post-SARS cumulative incidence of DSM-IV psychiatric disorders was 58.9 %. As per the IES-R and HADS, one-fourth of the patients had PTSD and 15.6 % had depressive disorders (Mak et al., 2009).
The potential effect of the current COVID-19 outbreak on mental health is likely to be profound. A rise in symptoms of anxiety and depression is expected not only amidst the pandemic but also during the upcoming months and years. One would expect, along these lines, an upsurge in suicide rates, similar to what has been described during the SARS outbreak in Hong Kong. Indeed, both mental health symptoms and diagnoses are well-established risk factors for suicide (Too et al., 2019). Additionally, exacerbation of preexisting mental health symptoms is anticipated during outbreaks, including COVID-19. This can be attributed to anxiety and worry about the infection, prolonged social isolation, and the uncertainty created by the outbreak (Cao et al., 2020; James et al., 2019; Tucci et al., 2017; Xiang et al., 2020).
Other superimposed risk factors might lead to an increase in suicide during the COVID-19 outbreak. A major adverse consequence of this pandemic, just like other outbreaks, is social isolation. Studies have shown an association between suicide rates and social isolation. Those who are single, live alone, or endorse the subjective feeling of loneliness are the most susceptible (Calati et al., 2019; Elovainio et al., 2017; Matthews et al., 2019; Naher et al., 2019). The link between social isolation and suicide was explained by Joiner’s psychological model of suicide, in which social isolation results in feelings of thwarted belongingness (Naher et al., 2019). Moreover, social isolation is thought to omit social support stemming from interpersonal relationships, an important protective factor against suicide (Calati et al., 2019). Alternatively, interpersonal risk factors for suicide are likely to be exacerbated midst of the current outbreak. This is especially notable among vulnerable populations, namely the elderly and immunosuppressed, who may experience greater physical isolation due to concerns about contracting the infection (Leight, 2003; Letvak, 2002), as well as those at risk of domestic violence (Godin, 2020; Lanier and Maume, 2009; MacIsaac et al., 2017). Secondary consequences of social distancing may also increase the risk of suicide. These include economic stress, decreased access to community and religious support, and decreased access to appropriate medical and mental health care (Reger et al., 2020). When it comes to economic stress, one study showed a 20–30% increase in suicide risk following unemployement (Nordt et al., 2015). Following the COVID-19 outbreak, the International Labour Organization expected a worlwide increase in the rate of unemployment that would result in up to 9570 additional suicide cases per year (Kawohl and Nordt, 2020).
Alternatively, quarantine by itself may exacerbate the mental health toll on the individual. Three of the case reports of suicide during the COVID-19 outbreak were allegedly reported to be related to quarantine. Many studies have demonstrated a causal relationship between quarantine and psychological distress. It seems that community anxiety resulting from pandemics is further exacerbated by mass quarantine (Rubin and Wessely, 2020). Barbisch et al. lists incarceration as one of the two major sources of psychological distress in pandemics, alongside the fear and ambiguity of the disease (Barbisch et al., 2015). Quarantine not only contributes to increased anxiety but also feelings of anger, boredom, and loneliness (Park and Park, 2020). Being quarantined is also linked to an increased risk of depression as well as PTSD (Brooks et al., 2020). Major stressors during quarantine include longer duration of confinement, fear of infection, frustration and boredom, inadequate supplies, and insufficient information (Brooks et al., 2020). As for quarantine within the same family, restricted physical contact results in a loss of intimacy, contributing to further emotional and psychological distress (Johal, 2009). Quarantine is also considered to be an indicator of the severity of the situation; it is associated with a perceived loss of control, as well as a sense of entrapment (Rubin and Wessely, 2020). As a result, confinement creates a sense of “collective hysteria”, which can be a major driving force towards suicide (Barbisch et al., 2015). Finally, quarantine and social isolation might increase drug consumption or relapse into substance misuse, even in long-term abstainers (Ornell et al., 2020; Wei and Shah, 2020). For instance, in an online survey conducted in China, 19 % and 32 % of participants relapsed or increased their alcohol use during the pandemic, respectively (Sun et al., 2020). The misuse of substance can further accentuate the risk of suicide (Carrà et al., 2014; Vijayakumar et al., 2011).
Since the onset of the COVID-19 outbreak, cases of suicide attempts attributed to the outbreak have been reported worldwide via newspapers and social media outlets (Nabbout, 2020; Pavan, 2020; Steinbuch, 2020; Stickings, 2020). Regardless, the direct association between the two events remains overall uncertain (Betz, 2020). This systematic review, a first in the existing literature, carries an invitation for further research into the topic, through the design of evidence-based studies that use large database clinical data. This would allow a better estimation of an underlying association between worldwide outbreaks and the outcome event of suicide. At a clinical level, from the abovementioned results, caution should be particularly directed towards those who are the most vulnerable: the elderly, the immunosuppressed, the inhabitants of rural areas, and the poorly educated, amongst others. Experts and early-career psychiatrists have also called for a global action to prevent suicide amidst this outbreak (Holmes et al., 2020; Ransing et al., 2020). An immediate action that fosters improving monitoring and reporting of anxiety, depression, and suicide amongst other mental health issues has been requested. This would be followed, in the long-term, by efforts to unveil the intricate culprit mechanisms behind the increased risk of suicide during outbreaks (Holmes et al., 2020).
5. Limitations
The strengths of this study mainly lie in its design and the novelty of the topic, as this is the first systematic review addressing the relationship between suicide and major international respiratory outbreaks. Furthermore, this study was based on a thorough search of the literature, which included multiple search engines and a detailed search strategy, thereby ensuring adequate retrieval of data. However, the limitations of this systematic review stem from the sparsity of research related to the topic, particularly to the COVID-19 outbreak, and the relatively low degree of evidence of the retrieved studies. Four of the nine studies include case reports and case series, which lie at the base of the Evidence Pyramid. Besides, eligible quantitative studies were cross-sectional, as we could not find any longitudinal study that fits our inclusion criteria. Also, four out of six cross-sectional studies were found to have a moderate risk of bias, further weakening the level of evidence. Moreover, the studies lacked homogeneity, making it difficult to deduce associations or draw generalizable conclusions. Another limitation of this study involves restricting the analysis to respiratory outbreaks, therefore excluding other epidemics such as those caused by Ebola, Monkeypox, and Zika viruses. Nevertheless, there is data supporting increased suicidality during these outbreaks. In a study conducted in Guinea, suicidal ideations or attempts were documented in four out of 33 Ebola Virus Disease survivors assessed by a psychiatrist (Keita et al., 2017). Another study conducted in Nigeria documented one suicide case out of 21 individuals affected by a Monkeypox outbreak (Ogoina et al., 2018). The current review also excluded studies assessing suicide during the Human Immunodeficiency Virus (HIV) pandemic. The association between acquiring HIV infection and suicide has been well established. A systematic review of 66 studies addressing suicidal behaviors and HIV infection revealed a high suicidal burden among individuals with HIV (Catalan et al., 2011). Yet, we opted to exclude the HIV outbreak from the current analysis due to the presence of mediators in the association between the infection and suicide. One main confounder is stigma towards vulnerable populations, particularly the LGBTQI community, which can account for the heightened risk of suicidality (Ferlatte et al., 2017).
6. Conclusion
In conclusion, this is the first systematic review to analyze the evidence about suicide and suicide-related outcomes during major international respiratory outbreaks. Deducing an association between pandemics, suicide, and suicide-related outcomes remains poorly supported. Future research with better methodological characteristics, the use of longitudinal studies, and a focus on suicide as the main outcome would allow for an in-depth understanding and formulation of the scope of this problem. However, despite the limitations inherent to the reviewed studies, they still provide insight into the need to improve mental health care during the current COVID-19 outbreak, and to enhance the readiness and aptitude of health care workers in detecting and managing the psychological sequelae of pandemics.
Funding and financial disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgment
None.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ajp.2020.102509.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Public Health. 2018:15. doi: 10.3390/ijerph15071425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbisch D., Koenig K.L., Shih F.Y. Is there a case for quarantine? Perspectives from SARS to ebola. Disaster Med. Public Health Prep. 2015;9:547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- Betz E. STAT; 2020. Covid-19 And Suicide: An Uncertain Connection. [Google Scholar]
- Brooks S., Webster R., Smith L., Woodland L., Wessely S., Greenberg N., Rubin G. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calati R., Ferrari C., Brittner M., Oasi O., Olie E., Carvalho A.F., Courtet P. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J. Affect. Disord. 2019;245:653–667. doi: 10.1016/j.jad.2018.11.022. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrà G., Bartoli F., Crocamo C., Brady K.T., Clerici M. Attempted suicide in people with co-occurring bipolar and substance use disorders: systematic review and meta-analysis. J. Affect. Disord. 2014;167:125–135. doi: 10.1016/j.jad.2014.05.066. [DOI] [PubMed] [Google Scholar]
- Catalan J., Harding R., Sibley E., Clucas C., Croome N., Sherr L. HIV infection and mental health: suicidal behaviour--systematic review. Psychol. Health Med. 2011;16:588–611. doi: 10.1080/13548506.2011.582125. [DOI] [PubMed] [Google Scholar]
- CDC . Centers for Disease Control and Prevention; 2020. Coronavirus Disease 2019 (COVID-19) [Google Scholar]
- Chan S.M., Chiu F.K., Lam C.W., Leung P.Y., Conwell Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2006;21:113–118. doi: 10.1002/gps.1432. [DOI] [PubMed] [Google Scholar]
- Cheung Y.T., Chau P.H., Yip P.S. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Elovainio M., Hakulinen C., Pulkki-Raback L., Virtanen M., Josefsson K., Jokela M., Vahtera J., Kivimaki M. Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lancet Public Health. 2017;2:e260–e266. doi: 10.1016/S2468-2667(17)30075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlatte O., Salway T., Oliffe J.L., Trussler T. Stigma and suicide among gay and bisexual men living with HIV. AIDS Care. 2017;29:1346–1350. doi: 10.1080/09540121.2017.1290762. [DOI] [PubMed] [Google Scholar]
- Gili M., Castellví P., Vives M., de la Torre-Luque A., Almenara J., Blasco M.J., Cebrià A.I., Gabilondo A., Pérez-Ara M.A., A, M.M, Lagares C., Parés-Badell O., Piqueras J.A., Rodríguez-Jiménez T., Rodríguez-Marín J., Soto-Sanz V., Alonso J., Roca M. Mental disorders as risk factors for suicidal behavior in young people: a meta-analysis and systematic review of longitudinal studies. J. Affect. Disord. 2019;245:152–162. doi: 10.1016/j.jad.2018.10.115. [DOI] [PubMed] [Google Scholar]
- Godin M. Time; 2020. As Cities Around the World Go on Lockdown, Victims of Domestic Violence Look for a Way Out. [Google Scholar]
- Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: First suicidal case in India! Asian J. Psychiatr. 2020;49 doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Vist G., Kunz R., Brozek J., Alonso-Coello P., Montori V., Akl E.A., Djulbegovic B., Falck-Ytter Y., Norris S.L., Williams J.W., Jr., Atkins D., Meerpohl J., Schunemann H.J. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias) J. Clin. Epidemiol. 2011;64:407–415. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]
- Harris E.C., Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br. J. Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hawton K., Casañas i Comabella C., Haw C., Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J. Affect. Disord. 2013;147:17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020;49:1–3. [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C.C., Yen D.H., Huang H.H., Kao W.F., Wang L.M., Huang C.I., Lee C.H. Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J. Chin. Med. Assoc. 2005;68:254–259. doi: 10.1016/S1726-4901(09)70146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James P.B., Wardle J., Steel A., Adams J. Post-Ebola psychosocial experiences and coping mechanisms among Ebola survivors: a systematic review. Trop. Med. Int. Health. 2019;24:671–691. doi: 10.1111/tmi.13226. [DOI] [PubMed] [Google Scholar]
- Johal S.S. Psychosocial impacts of quarantine during disease outbreaks and interventions that may help to relieve strain. N. Z. Med. J. 2009;122:47–52. [PubMed] [Google Scholar]
- Kawohl W., Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7:389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keita M.M., Taverne B., Sy Savané S., March L., Doukoure M., Sow M.S., Touré A., Etard J.F., Barry M., Delaporte E., PostEboGui Study G. Depressive symptoms among survivors of Ebola virus disease in Conakry (Guinea): preliminary results of the PostEboGui cohort. BMC Psychiatry. 2017;17 doi: 10.1186/s12888-017-1280-8. 127-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier C., Maume M.O. Intimate partner violence and social isolation across the rural/urban divide. Violence Against Women. 2009;15:1311–1330. doi: 10.1177/1077801209346711. [DOI] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020:1–9. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leight S.B. The application of a vulnerable populations conceptual model to rural health. Public Health Nurs. 2003;20:440–448. doi: 10.1046/j.1525-1446.2003.20604.x. [DOI] [PubMed] [Google Scholar]
- Letvak S. The importance of social support for rural mental health. Issues Ment. Health Nurs. 2002;23:249–261. doi: 10.1080/016128402753542992. [DOI] [PubMed] [Google Scholar]
- MacIsaac M.B., Bugeja L.C., Jelinek G.A. The association between exposure to interpersonal violence and suicide among women: a systematic review. Aust. N. Z. J. Public Health. 2017;41:61–69. doi: 10.1111/1753-6405.12594. [DOI] [PubMed] [Google Scholar]
- Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Griffiths M.D. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J. Psychiatr. 2020:51. doi: 10.1016/j.ajp.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews T., Danese A., Caspi A., Fisher H.L., Goldman-Mellor S., Kepa A., Moffitt T.E., Odgers C.L., Arseneault L. Lonely young adults in modern Britain: findings from an epidemiological cohort study. Psychol. Med. 2019;49:268–277. doi: 10.1017/S0033291718000788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabbout M. Step Feed; 2020. Foreign Student Commits Suicide While Quarantined in Saudi Arabia. [Google Scholar]
- Naher A.F., Rummel-Kluge C., Hegerl U. Associations of suicide rates with socioeconomic status and social isolation: findings from longitudinal register and census data. Front. Psychiatry. 2019;10:898. doi: 10.3389/fpsyt.2019.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordt C., Warnke I., Seifritz E., Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000-11. Lancet Psychiatry. 2015;2:239–245. doi: 10.1016/S2215-0366(14)00118-7. [DOI] [PubMed] [Google Scholar]
- Ogoina D., Hendricks J., Aworabhi N., Yinka-Ogunleye A.F., Etebu E.N., Numbere W., Anebonam U.U. The 2017 monkeypox outbreak in Nigeria-report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. Am. J. Trop. Med. Hyg. 2018;99:72–73. [Google Scholar]
- Okusaga O., Yolken R.H., Langenberg P., Lapidus M., Arling T.A., Dickerson F.B., Scrandis D.A., Severance E., Cabassa J.A., Balis T., Postolache T.T. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J. Affect. Disord. 2011;130(1):220–225. doi: 10.1016/j.jad.2010.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F.H.P., von Diemen L. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113096. 113096-113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.C., Park Y.C. Mental health care measures in response to the 2019 novel coronavirus outbreak in Korea. Psychiatry Investig. 2020;17:85–86. doi: 10.30773/pi.2020.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavan P. Bangalore Mirror; 2020. COVID-19: Two Commit Suicide Out of Fear. [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransing R., Adiukwu F., Pereira-Sanchez V., Ramalho R., Orsolini L., Schuh Teixeira A.L., Gonzalez-Diaz J.M., da Costa M.P., Soler-Vidal J., Bytyçi D.G., El Hayek S., Larnaout A., Shalbafan M., Syarif Z., Nofal M., Kundadak G.K. Early career psychiatrists’ perspectives on the mental health impact and care of the COVID-19 pandemic across the world. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide Mortality and Coronavirus Disease 2019-A Perfect Storm? JAMA Psychiatry. 2020;77(11):1093–1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Rubin J., Wessely S. The BMJ Opinion; 2020. Coronavirus: The Psychological Effects of Quarantining a City. [DOI] [PubMed] [Google Scholar]
- Sahoo S., Rani S., Parveen S., Pal Singh A., Mehra A., Chakrabarti S., Grover S., Tandup C. Self-harm and COVID-19 Pandemic: an emerging concern - A report of 2 cases from India. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim K., Chong P.N., Chan Y.H., Soon W.S. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. J. Clin. Psychiatry. 2004;65:1120–1127. doi: 10.4088/jcp.v65n0815. [DOI] [PubMed] [Google Scholar]
- Steinbuch Y. New York Post; 2020. Italian Nurse With Coronavirus Kills Herself Over Fear of Infecting Others. [Google Scholar]
- Stickings T. Mail Online; 2020. Italian Nurse, 34, Kills Herself After Testing Positive for Coronavirus and Worrying She Had Infected Others. [Google Scholar]
- Sun Y., Li Y., Bao Y., Meng S., Sun Y., Schumann G., Kosten T., Strang J., Lu L., Shi J. Brief report: increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am. J. Addict. 2020;29:268–270. doi: 10.1111/ajad.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Too L.S., Spittal M.J., Bugeja L., Reifels L., Butterworth P., Pirkis J. The association between mental disorders and suicide: a systematic review and meta-analysis of record linkage studies. J. Affect. Disord. 2019;259:302–313. doi: 10.1016/j.jad.2019.08.054. [DOI] [PubMed] [Google Scholar]
- Tucci V., Moukaddam N., Meadows J., Shah S., Galwankar S.C., Bobby Kapur G. The forgotten plague: psychiatric manifestations of ebola, zika, and emerging infectious diseases. J. Glob. Infect. Dis. 2017;9:151–156. doi: 10.4103/jgid.jgid_66_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar L., Kumar M.S., Vijayakumar V. Substance use and suicide. Curr. Opin. Psychiatry. 2011;24:197–202. doi: 10.1097/YCO.0b013e3283459242. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020:17. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman I.M. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life‐Threat. Behav. 1992;22:240–254. [PubMed] [Google Scholar]
- Wei Y., Shah R. Substance use disorder in the COVID-19 pandemic: a systematic review of vulnerabilities and complications. Pharmaceuticals (Basel) 2020:13. doi: 10.3390/ph13070155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2020. Country & Technical Guidance - Coronavirus Disease (COVID-19) [Google Scholar]
- WHO . World Health Organization; 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J. Trauma. Stress. 2005;18:39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip P.S.F., Cheung Y.T., Chau P.H., Law Y.W. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis J. Crisis Interv. Suicide Prev. 2010;31:86–92. doi: 10.1027/0227-5910/a000015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.