Abstract
Outbreaks of an epidemic, such as coronavirus disease 2019 (COVID-19), always brings about far-ranging discrimination and stigmatization to the epicenter. This was a cross-sectional survey conducted to assess experienced discrimination, internalized stigma, shame, and mental health (anxiety, depression, distress, insomnia) among college students who merely had a perceived linkage with COVID-19, and explore the linkage between discrimination and negative mental health outcomes through the mediating effects of shame and internalized stigma. A total of 995 participants (53% female) were involved in this study, in which 40.9% of college students were reported to be discriminated against because of their experience in Wuhan. The experience of COVID-19-related discrimination is indirectly associated with anxiety, depression, and insomnia, in which shame and internalized stigma play a complete mediating effect. Meanwhile, it is both directly and indirectly associated with distress through shame and internalized stigma. The findings of this study suggest that COVID-19-related discrimination is associated with shame and internalized stigma, which in turn predict psychological symptoms over time.
Keywords: discrimination, internalized stigma, shame, mental health, college students, COVID-19
1. Introduction
At the end of December 2019, a novel pneumonia caused by coronavirus disease 2019 (COVID-19) was first identified in Wuhan; it soon escalated into a global health emergency [1,2]. The world faced an unprecedented public health crisis. Apart from physical health, mental health was equally crucial and worthy of attention. Epidemic outbreaks have been historically accompanied by stigma, discrimination, and xenophobia [3], leading to psychological harm to individuals in the epicenter [4]. Previous studies have elucidated a few interactions of these psychological issues. Moreover, the linkage between COVID-19 and racism brought about anti-Chinese activities, and these acts of discrimination occurred in social, political, and historical contexts [5]. Social media bias against Asian Americans increased, with escalated radical and abusive expressions, which incurred discrimination and adverse mental health consequences [6]. Such COVID-19-related discrimination was quite evident and omnipresent among individuals, especially those who manifested a potential linkage with Wuhan during the outbreak of COVID-19, since Wuhan was the first epicenter of this global health crisis. Consequently, those discriminated individuals became more vigilant concerning stigma-related threats, as well as more vulnerable to stigmatization [7]. However, little information is available that reveals how invisible harm caused by discrimination exerts its toll on mental health during the COVID-19 pandemic. Therefore, underlying psychological mechanisms of COVID-19-related discrimination associated with mental health needs to be further explored.
Stigma is a personal attribute that is socially devalued [8] and exists with the co-occurrence of labeling, stereotyping, social exclusion, discrimination [9]. Importantly, stigma is context-specific and not deemed to reside in the person but in a social context [10,11]. According to the theory of the stigma framework, a stigma is generally categorized into discrimination and internalized stigma [12]. Therefore, in the context of the COVID-19 pandemic, internalized stigma refers to the awareness of devaluation or a stereotype of oneself because of a perceived linkage with COVID-19 [12,13]. In an overview of outbreaks of epidemics during past decades, epidemic-related stigma unremittingly occurred in particular groups, which could be a barrier to the containment of the epidemic, leading to detrimental consequences for psychological wellbeing [14,15]. Wuhan, the initial epicenter of COVID-19, was put under an international spotlight, leading to the stigmatized label “Wuhan virus” [16]. In addition to the mandatory quarantine measures, media-driven misinformation and overloaded news reports ignited fear and uncertainty, provoking stigma and discrimination. According to the COVID-19 Health Stigma and Discrimination Framework (HSDF) [17], the experience of discrimination, along with shame, were drivers of stigmatization, and the internalized stigma can be regarded as a manifestation to exert a negative impact on mental health outcomes. Besides, internalized stigma could manifest as self-hatred, self-isolation, shame, and fear of further stigmatization [18,19,20]. The empirical study, demonstrating perceived epidemic-related discrimination, was far-ranging and increased with time. As a result, it might profoundly contribute to long-term adverse mental health outcomes [21,22]. Moreover, individuals with travel experience in the epicenter were affected by internalized stigma [23], and that could be psychologically damaging for individuals affected by COVID-19, since high levels of internalized stigma might be associated with lower levels of self-esteem and increased depression [10,24]. In addition, previous studies have shown the association between multifaceted discrimination and retention cares in HIV-positive young adolescents; this process was mediated by internalized stigma [25]. Although the repercussion of internalized stigma has been widely revealed, the psychological process was still unclear in the context of COVID-19.
Shame is a negative self-conscious emotion [26], triggered when individuals experience failure in regards to personal or social standards. Ashamed individuals might blame themselves rather than others, believing that failures reflect inadequacy in themselves. Shame often originates from incorrect perception or belief in particular events, and it may be an underlying mechanism in which stigma is enacted [27]. Concerning infectious disease-perceived discrimination, individuals may exhibit feelings of shame and stigmatization synchronously. Moreover, shame has been shown to mediate the negative mental and physical health consequences of stigmatization, both shame and stigma are directly related to mental health problems [25,28,29]. However, they probably have different manifestations. In particular, shame is a part of the experience of which individuals seek health-care services, while stigma may be a barrier in decisions to seek care [30]. Previous research indicated that individuals with sexually transmitted diseases (STD), HIV/AIDs, hepatitis C, and mental illnesses were more likely to suffer poor mental and physical health if they felt ashamed of their stigma. Often in cases where infectious disease-related shame was a strong predictor of stigma [31], previous studies demonstrated that shame mediated the relationship between stigma and depression [32]. Unfortunately, up until now, researches focused on shame in COVID-19, and the psychological effects of this process are scarce. We could not make a firm conclusion of the psychological impact so far.
To date, regarding the increasing concern about mental health during the post-COVID-19 pandemic, the present study sought to access the knowledge gap of the mental health status and address the issue related to discrimination, shame, and stigma connected with mental health.
2. Methods
2.1. Setting and Participants
This was a cross-sectional study using a web-based survey to assess the experiences of COVID-19-related discrimination, shame, internalized stigma with mental health outcomes among college students. Participants who were not exposed to the risk of COVID-19, but merely had a perceived linkage with the first epicenter of COVID-19, were invited to participate in this survey, from 31 August to 14 September, 2020. The snowball sampling method, which focused on recruiting college students in Wuhan, was used to obtain samples. The sample size should be 5–10 times the number of scale entries. Furthermore, it was expected that at least 696 participants would be required, considering a sample dispersion rate of 20%. Participants were encouraged to participate in online surveys or complete offline questionnaires. Eligibility criteria of this study included: (i) participants who were studying in Wuhan before the COVID-19 outbreak (as well as currently in Wuhan); (ii) participants aged 18 years or older; (iii) participants who volunteered to take part in this study.
2.2. Procedure
This was an anonymous survey, and data confidentiality were ensured. We developed the online questionnaires on the official website of “Questionnaire Star”, which is recognized as a professional online questionnaire survey platform. To practice social distancing and avoid large-scale gatherings, we printed the informed consent form with the attached QR code. Once the QR code (via a mobile phone) was scanned, participants could directly enter the survey page and then fill out the questionnaire. The informed consent forms from all participants were obtained before they completed the online questionnaires, and the web-based survey prompted participants to complete skipped items. Therefore, no missing item-level data were present during the process of data collection. After removing participants with dozens of consecutive identical and illogical item responses, our effective sample included 995 participants.
2.3. Measures
Internalized stigmatization: it was measured by a 12-item scale adapted from Visser and colleagues [33]. It included two dimensions, identified as “Blame and Judgement” and “Interpersonal Distancing”. Stigma is time- and context-specific [10]; therefore, the items were tailored to reflect the context of COVID-19-related internalized stigma. The Chinese version of this scale was translated in a previous study by Li et al. [23], showing adequate reliability and validity for reflecting participant levels of internalized stigma. Items were rated on a 7-point Likert-type scale, and scales with higher scores indicated a higher level of internalized stigma. The Cronbach’s α for the scale in this study was 0.806.
Shame: it was measured by a 6-item scale, adapted from Fortenberry and colleagues [34]. A bilingual researcher was recruited to perform the translation from English to Chinese, and then we conducted a backward translation for confirmation. Higher total scores reflect the higher level of shame. The Cronbach’s α for the scale in this study was 0.899.
Anxiety: it was assessed by the Chinese version [35] of Generalized Anxiety Disorder Scale-7 (GAD-7), which comprised 7 self-reported symptoms rating over the past two weeks. The GAD-7 used a Likert-type frequency scale from “0 = Not at all” to “3 = Nearly every day.” The Cronbach’s α coefficient of the Chinese version of GAD-7 is 0.898, and the test-retest reliability coefficient was 0.856, proving it had good reliability and validity in the application of evaluating anxiety. In addition, summed scores were reliable and valid [36]. We tailored this instruction to query COVID-19-related anxiety, specifying “Over the last 2 weeks, how often have you been bothered by the following problems because of the outbreak of COVID-19?”. The total score ranged from 0 to 21, with higher scores indicating a greater degree of anxiety. The Cronbach’s α for the scale in this study was 0.928.
Depression: it was measured by the Chinese version of Patient Health Questionnaire-9 (PHQ-9), which was a self-rating measurement assessing depressive symptoms over the last two weeks. The PHQ-9 used a 4-point Likert scale from 0 (never) to 3 (nearly every day), with higher scores indicating a greater severe symptom of depression. This scale has been widely used among the Chinese, indicating excellent psychometric properties [37]. The Cronbach’s α for the scale in this study was 0.917.
Insomnia: the severity of insomnia was measured by the Chinese version of the Insomnia Severity Index scale (ISI-7) [38]. It consisted of seven items, rated on a five-point Likert scale, including evaluating sleep onset and maintenance, early morning awakening, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by disturbed sleep. The total score ranged from 0 to 28, with higher scores indicating a greater severity of insomnia. The Cronbach’s α for the scale in this study was 0.903.
Distress: COVID-19-related distress was measured by the Chinese version of the Impact of Event Scale (IES-7) with a seven-item subscale [39]. The Chinese version of IES-7 used a 6-point Likert scale from 0 “never” to 5 “a high degree” with higher IES total scores, indicating participants with greater self-reported severe symptoms. The items were designedly tailored to reflect the context of COVID-19 related distress. The Cronbach’s α for the scale in this study was 0.805.
The experience of COVID-19-related discrimination: we used a “yes”/“no” binary item to query COVID-19-related discrimination [40,41] by asking, “Have you ever been discriminated against because of your experience of studying and living in Wuhan, Hubei province?”. Moreover, we subsequently used a series of multiple choice questions to query the main sources and forms of discrimination by asking, “If you are discriminated against or treated differently, what are the main sources from and in which form?”.
Covariates: the following covariates were included in this study: gender, age, and years expected to graduate.
2.4. Common Method Bias
Common method bias analysis was conducted before data analysis. The Eigenvalues of 11 factors were greater than 1. The first factor explains 29.34% of the accumulative variation, which indicated no serious common method bias deviation.
2.5. Data Analysis
The data were calculated and analyzed by SPSS version 24.0 (IBM SPSS, IBM Corp., Armonk, NY, USA). Apart from descriptive statistics and frequency analysis of demographic characteristics and the COVID-19-related information, we conducted a t-test or (F-test) and correlation test to examine relationships of potential covariates with our predictors, mediators, and outcomes. These analyses guided our covariate selections. Prior to testing for mediation, we examined the possibility that shame and internalized stigma may moderate the relationship between the experience of discrimination and detrimental consequences for psychological wellbeing. Consequently, preliminary analyses did not confirm the moderating effects. After adjusting for age, gender and, years expected to graduate, the mediation models were conducted by using the bootstrapping procedure by Preacher and Hayes, and the corresponding SPSS macro Model 6 within SPSS 24.0 to test whether COVID-19-related shame and internalized stigma mediated the relationship between discrimination and mental health problems. We utilized non-standardized coefficients and bootstrapping with 5000 samples to place 95% bias-corrected confidence intervals around estimates.
3. Results
3.1. Characteristics of Participants
The overview of sociodemographic characteristics and the experience of discrimination relative information are exhibited in Table 1. It is shown that 40.90% of college students were reported to be discriminated against because of their experiences in Wuhan. The main discrimination sources were from the community (76.66%), friends and relatives (54.30%), and social media (32.92%). The main forms of discrimination are social avoidance (68.06%), personal information leakage (54.05%), and abusive expressions (45.95%).
Table 1.
Demographic characteristics and discrimination relative information.
| Variable | Categories | n | % |
|---|---|---|---|
| Sex | Male | 463 | 46.53 |
| Female | 532 | 53.47 | |
| Age | 18–21 | 421 | 42.31 |
| 22–25 | 501 | 50.35 | |
| 26–29 | 63 | 6.33 | |
| 30 and above | 10 | 1.01 | |
| Years expected to graduate | Within 1 year | 339 | 34.07 |
| Within 2 years | 328 | 32.96 | |
| Within 3 years | 240 | 24.12 | |
| 4 years and above | 88 | 8.84 | |
| Have you ever been discriminated against because of your experience in Wuhan? | Yes | 407 | 40.90 |
| No | 588 | 59.10 | |
| Source of discrimination | Community | 312 | 76.66 |
| Friends and relatives around | 221 | 54.30 | |
| Social Media | 134 | 32.92 | |
| Restaurants, hotels, hospitals, and other facilities | 90 | 22.11 | |
| Administrative Departments and law enforcement agencies | 90 | 22.11 | |
| Railway transportation and airport department | 55 | 13.51 | |
| Form of discrimination | Social avoidance | 277 | 68.06 |
| Personal information leakage | 220 | 54.05 | |
| Abusive expressions | 187 | 45.95 | |
| Deliberately complicated examination procedure | 157 | 38.57 | |
| Others | 19 | 4.67 | |
| Body conflicts | 17 | 4.18 |
3.2. Correlation between Variables
Means, standard deviations, and bivariate correlations of variables in this study are shown in Table 2. The experience of discrimination, shame, internalized stigma, and negative mental health outcomes (anxiety, distress, depression, and insomnia) are positively correlated. In particular, the experience of discrimination is positively correlated with shame (r = 0.116, p < 0.001), internalized stigma (r = 0.390, p < 0.001), anxiety (r = 0.084, p < 0.01), distress (r = 0.175, p < 0.001), depression (r = 0.099, p < 0.01) and insomnia (r = 0.101, p < 0.01). Moreover, similar results are observed in shame and internalized stigma.
Table 2.
Means, standard deviations, and bivariate correlations among variables.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Discrimination | 1 | ||||||||
| 2. Shame | 8.24 | 4.74 | 0.116 *** | 1 | |||||
| 3. Internalized stigma | 36.37 | 12.45 | 0.390 *** | 0.406 *** | 1 | ||||
| 4. Anxiety | 11.38 | 4.30 | 0.084 ** | 0.300 ** | 0.270 *** | 1 | |||
| 5. Distress | 15.84 | 4.98 | 0.175 *** | 0.316 *** | 0.351 *** | 0.443 *** | 1 | ||
| 6. Depression | 14.21 | 5.18 | 0.099 ** | 0.334 *** | 0.279 *** | 0.716 *** | 0.454 *** | 1 | |
| 7. Insomnia | 13.80 | 5.50 | 0.101 ** | 0.282 *** | 0.265 *** | 0.518 *** | 0.441 *** | 0.641 *** | 1 |
Note: n = 995, ** p < 0.01, *** p < 0.001.
3.3. Mediating Effect Analysis
Table 3 illustrates the linear regression analysis results, and the control variables are sex, age, and year expected to graduate. Regression analysis reveals that the experience of discrimination could positively predict higher shame (β = 0.7683, p < 0.05), internalized stigma (β = 7.811, p < 0.001), and distress (β = 0.7698, p < 0.05). Moreover, as shown in Table 3, shame can positively predict internalized stigma (β = 1.1975, p < 0.001), anxiety (β = 0.2636, p < 0.001), distress (β = 0.2536, p < 0.001), depression (β = 0.3848, p < 0.001), and insomnia (β = 0.3038, p < 0.001). Internalized stigma can positively predict anxiety (β = 0.0552, p < 0.001), distress (β = 0.0787, p < 0.001), depression (β = 0.0569, p < 0.001) and insomnia (β = 0.0670, p < 0.001).
Table 3.
Regression results.
| Regression Model | Fitting Index | Significance of Coefficients | ||||
|---|---|---|---|---|---|---|
| Outcome Variable | Independent Variable | R | R2 | F | β | t |
| Shame | Sex | 0.1502 | 0.0226 | 5.712 | −1.0219 | −3.4045 |
| Age | 0.5129 | 2.1465 * | ||||
| YEG | −0.083 | −0.5266 | ||||
| Discrimination | 0.7683 | 2.5197 * | ||||
| Internalized Stigma | Sex | 0.5934 | 0.3521 | 107.515 | 0.4303 | 0.6666 |
| Age | 2.0311 | 3.9665 *** | ||||
| YEG | −0.0816 | −0.2421 | ||||
| Discrimination | 7.811 | 11.9435 *** | ||||
| Shame | 1.1975 | 17.6241 *** | ||||
| Anxiety | Sex | 0.3969 | 0.1575 | 30.795 | 0.359 | 1.4108 |
| Age | −0.2052 | −1.0089 | ||||
| YEG | −0.2428 | −1.8277 | ||||
| Discrimination | 0.0391 | 0.1418 | ||||
| Shame | 0.2636 | 8.5866 *** | ||||
| Internalized sigma | 0.0552 | 4.4006 *** | ||||
| Distress | Sex | 0.4207 | 0.177 | 35.408 | 0.1259 | 0.4321 |
| Age | 0.0476 | 0.2045 | ||||
| YEG | −0.4952 | −3.2545 ** | ||||
| Discrimination | 0.7698 | 2.4375 * | ||||
| Shame | 0.2536 | 7.2125 *** | ||||
| Internalized stigma | 0.0787 | 5.4841 *** | ||||
| Depression | Sex | 0.4487 | 0.2014 | 41.518 | 0.8699 | 2.9115 ** |
| Age | 0.1959 | 0.82 | ||||
| YEG | −0.3077 | −1.973 * | ||||
| Discrimination | 0.0594 | 0.1836 | ||||
| Shame | 0.3848 | 10.6758 *** | ||||
| Internalized stigma | 0.0569 | 3.8697 *** | ||||
| Insomnia | Sex | 0.4036 | 0.1629 | 32.042 | 0.561 | 1.7289 |
| Age | 1.0709 | 4.1285 *** | ||||
| YEG | −0.0996 | −0.588 | ||||
| Discrimination | 0.1528 | 0.4347 | ||||
| Shame | 0.3038 | 7.7609 *** | ||||
| Internalized stigma | 0.067 | 4.1921 *** | ||||
Note: n = 995, * p < 0.05, ** p < 0.01, *** p < 0.001. YEG, years expected to graduate.
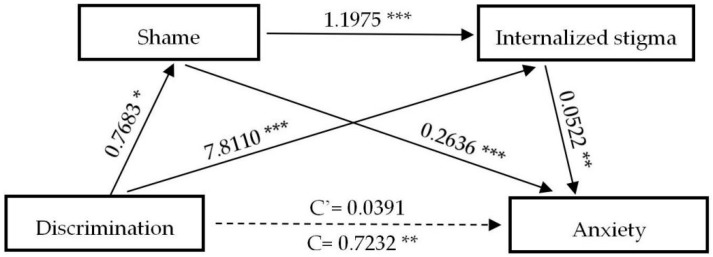
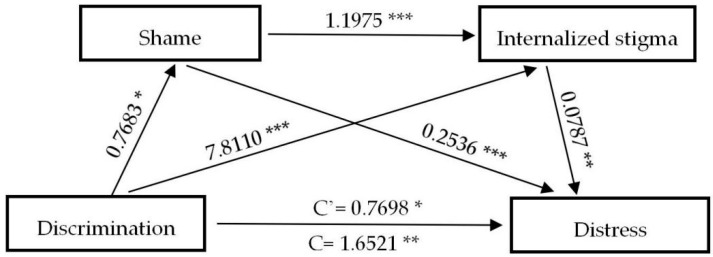
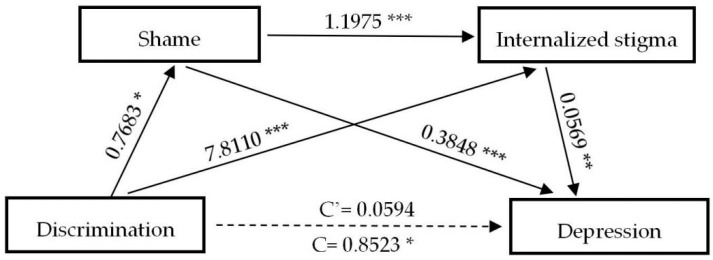
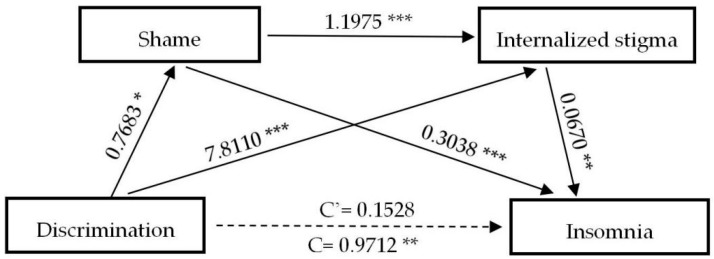
Table 4 exhibits the results of direct and indirect paths and effects of the experience of discrimination on the negative psychological outcomes, respectively. Notably, the bootstrap method indicates that except distress (β = 0.7689, (CI: 0.1501, 1.3896)), the experience of discrimination does not exert direct effects (C’) on psychological outcomes assessed, while none of the direct effects of anxiety (β = 0.0391, (CI: −0.5020, 0.5802)), depression (β = 0.0594, (CI: −0.5759, 0.6948)) and insomnia (β = 0.1528, (CI: −0.5372, 0.8428)) are statistically significant. However, the total indirect effect of discrimination on anxiety (β = 0.6841, (CI: 0.3889, 0.9918)), distress (β = 0.8822, (CI: 0.5511, 1.2642)), depression (β = 0.7929, (CI: 0.4261, 1.1704)) and insomnia (β = 0.8184, (CI: 0.4580, 1.2168)) are significantly observed. Specifically, shame and internalized stigma have played complete mediating roles in predicting anxiety, depression, and insomnia; three indirect paths between the experience of discrimination and negative mental health outcomes (NMHO) are significant: (a) D→S→NMHO, (b) D→IS→NMHO, (c) D→S→IS→NMHO, and total indirect effects overwhelmingly accounted for 94.59%, 93.03%, and 84.27% of the total effect, respectively. After controlling for shame and internalized stigma, the experience of discrimination can significantly predict distress, indicating that shame and internalized stigma are partial mediators between the experience of discrimination and distress. The total indirect effect accounts for 53.40% of the total effect. To better understand the associations between the experience of discrimination and negative mental health outcomes, Figure 1, Figure 2, Figure 3 and Figure 4 are plotted to depict the indirect and their chain mediation paths.
Table 4.
Direct and indirect effects of coronavirus disease 2019 (COVID-19)-related discrimination on anxiety, distress, depression, and insomnia through the mediating effects of shame and internalized stigma.
| Model | Path | Effect | Boot SE | Boot 95%CI | Effect Size |
|---|---|---|---|---|---|
| D on anxiety | Direct effect | 0.0391 | 0.2757 | −0.5020, 0.5802 | 5.41% |
| Indirect effect | |||||
| Total | 0.6841 | 0.1529 | 0.3889, 0.9918 | 94.59% | |
| D→S→Anxiety | 0.2025 | 0.0887 | 0.0361, 0.3899 | 28.00% | |
| D→IS→Anxiety | 0.4308 | 0.1127 | 0.2204, 0.6633 | 59.57% | |
| D→S→IS→Anxiety | 0.0507 | 0.0254 | 0.008, 0.1077 | 7.01% | |
| D on distress | Direct effect | 0.7689 | 0.3158 | 0.1501, 1.3896 | 46.54% |
| Indirect effect | |||||
| Total | 0.8822 | 0.1795 | 0.5511, 1.2642 | 53.40% | |
| D→S→Distress | 0.1949 | 0.0822 | 0.0411, 0.3669 | 11.80% | |
| D→IS→Distress | 0.6149 | 0.132 | 0.3761, 0.8908 | 37.22% | |
| D→S→IS→Distress | 0.0724 | 0.0366 | 0.0141, 0.1597 | 4.38% | |
| D on depression | Direct effect | 0.0594 | 0.3238 | −0.5759, 0.6948 | 6.97% |
| Indirect effect | |||||
| Total | 0.7929 | 0.1904 | 0.4261, 1.1704 | 93.03% | |
| D→S→Depression | 0.2957 | 0.1266 | 0.0516, 0.5541 | 34.69% | |
| D→IS→Depression | 0.4448 | 0.126 | 0.2046, 0.7034 | 52.19% | |
| D→S→IS→Depression | 0.0524 | 0.0272 | 0.0077, 0.1135 | 6.15% | |
| D on insomnia | Direct effect | 0.1528 | 0.3516 | −0.5372, 0.8428 | 15.73% |
| Indirect effect | |||||
| Total | 0.8184 | 0.1954 | 0.458, 1.2168 | 84.27% | |
| D→S→Insomnia | 0.2334 | 0.1025 | 0.0482, 0.4457 | 24.03% | |
| D→IS→Insomnia | 0.5233 | 0.1435 | 0.2567, 0.8183 | 53.88% | |
| D→S→IS→Insomnia | 0.0616 | 0.0325 | 0.0107, 0.1367 | 6.34% |
Note: D, the experience of discrimination; S, shame; IS, internalized stigma. Models were adjusted for sex, age, and years expected to graduate.
Figure 1.
A serial mediation analysis of shame and internalized stigma on discrimination to anxiety. * p < 0.05, ** p < 0.01, *** p < 0.001. C: direct effect without mediators; C’: direct effect with the mediators of shame and internalized stigma.
Figure 2.
A serial mediation analysis of shame and internalized stigma on discrimination to distress. * p < 0.05, ** p < 0.01, *** p < 0.001.
Figure 3.
A serial mediation analysis of shame and internalized stigma on discrimination to depression. * p < 0.05, ** p < 0.01, *** p < 0.001.
Figure 4.
A serial mediation analysis of shame and internalized stigma on discrimination to insomnia. * p < 0.05, ** p < 0.01, *** p < 0.001.
The coefficients shown above are non-standardized. Shame and internalized stigma in sequence mediated the relationship between discrimination and anxiety, distress, depression, and insomnia.
4. Discussion
Epidemic outbreaks have been historically accompanied by stigma, discrimination, and xenophobia, leading to psychological harm to individuals in the epicenter [4]. Such stigma and discrimination were quite evident among college students in Wuhan since China was the first country afflicted by the COVID-19 pandemic, and Wuhan was the first epicenter of the unprecedented global health crisis [1,2]. However, it was quite challenging to uncover the underlying mechanisms of the toll on mental health outcomes and reveal certain invisible harm caused by discrimination and stigma. The focus of this cross-sectional study is twofold: (1) to investigate the experience of COVID-19-related discrimination among returning college students in Wuhan and explore the linkage between discrimination and negative mental health outcomes; and (2) to assess the mediating role of shame and internalized stigma between the experiences of COVID-19-related discrimination and negative mental health outcomes.
To our knowledge, this is the first quantitative study to examine COVID-19-related discrimination experienced by Chinese back-to-school (returning) college students. Our study demonstrates nearly 41% of them were reported to have encountered different kinds of discrimination because of their experience in Wuhan, which is in line with a study conducted among Hong Kong residents during the outbreak of Severe Acute Respiratory Syndrome (SARS) [42]. Additionally, 76.7%, 54.3%, and 32.9% of them were discriminated against in various ways (e.g., social avoidance, personal information leakage, abusive expressions, deliberately complicated examination procedures, body conflict, etc.) by their local communities, friends, relatives, and social media, respectively. This might be associated with uncertainty from the public towards infectious diseases and Chinese nationwide over-mobilization [16], which, turned out to be useful in the containment of COVID-19. Likewise, during the COVID-19 pandemic in China, those who had experiences in Wuhan were urged to quarantine for 14 days in designated facilities or homes. Therefore, those returning individuals might have regarded the quarantine as a discrimination signal. Furthermore, media-driven labeling of the unprecedented risk of COVID-19 in Wuhan, to some extent, had fueled discrimination toward these individuals, who had a similar experience with the residents in Hong Kong and Dallas during the SARS [43] and Ebola crises [44,45]. Consequently, they were prone to experience discrimination and stigmatization related to COVID-19, as they might have been blamed as potential “sources of infection”.
A significant association between the experience of discrimination and adverse psychological consequences were observed in this study. We found that the negative mental health outcomes were positively associated with COVID-19-related discrimination among returning college students in Wuhan. This finding is consistent with numerous previous studies revealing that individuals with perceived discrimination showed increased morbidity rates of negative mental health outcomes [46], especially a study conducted during the COVID-19 pandemic [40]. The experience of discrimination implied rejection, as well as the exclusion of targeted groups, and a threat of self-concept, thus spontaneously prompting detrimental psychological outcomes and lower quality of life [47].
Research had linked experiences of discrimination with detrimental psychological consequences, but less was known about the role of shame and internalized stigma as mediators. To this end, our study was sequentially targeted at exploring, prospectively, whether the linkage between discrimination and psychological wellbeing was accounted for by shame and internalized stigma. In this study, direct and indirect effects of the experience of discrimination, shame, and internalized stigma on negative mental health outcomes among participants were explored. Corroborating previous studies [40], the experience of discrimination was directly associated with high levels of negative mental health outcomes, and the effect sizes were substantial without considering the mediating effects of COVID-19-related shame and internalized stigma. However, further meditational path analyses surprisingly indicated that, except for an individual’s COVID-19-related distress, the experience of discrimination demonstrated a total indirect influence on mental health outcomes (anxiety, depression, insomnia), with shame and internalized stigma playing important mediating roles. In particular, several potential mechanisms, by which the experience of discrimination could affect the negative mental health outcomes, were observed. Shame and internalized stigma could separately mediate the impact of the experience of discrimination on negative mental health outcomes. This was consistent with previous studies [48,49] that internalized stigma could take a toll on mental health as a mediator. Meanwhile, our findings suggested that shame could directly influence the internalized stigma, thus, affecting negative mental health outcomes through their chain mediating path. This was in line with previous studies linking shame and internalized stigma to increased risks for negative mental health outcomes [20,50,51,52,53,54,55,56,57,58] in the context of HIV, obesity, schizophrenia, and marginalized groups. Multiple mediating analyses further revealed the underlying mechanisms and explained why discrimination could increase negative mental health outcomes. Previous studies confirmed the constructive role of coping with stigma on maintaining a positive self-concept [10] and self-esteem [59]. However, the discriminated individuals tended to experience higher shame and internalized stigma, which in turn implied the malfunction of coping strategies with stigma and discrimination. Consequently, negative mental health outcomes increased when low self-concept and self-esteem were shaped as a result of shame and internalized stigma. Taken together, we argued that a higher level of shame and internalized stigma appeared to occur successively without detecting when individuals were discriminated against in various ways, and became aware of the potential link, along with stereotypes with COVID-19, then directly affected the negative mental health outcomes.
The experience of discrimination could both directly and indirectly impact COVID-19-related distress, considering the mediator of shame and internalized stigma, since the COVID-19 pandemic had created an unprecedented panic [60], and the discrimination encountered by individuals could be profoundly impressed and enduringly related. However, it seemed to be unsuccessful in directly predicting a higher level of anxiety, depression, and insomnia since there were no significant direct effects observed, supporting the notion that shame and internalized stigma play an important role in determining the individual’s negative emotions [61]. To be more specific, being discriminated against—momently regarded as an unpleasant experience by individuals—did not necessarily prompt a higher level of anxiety, depression, and insomnia, unless shame and internalized stigma were perceived during the process in the long-term.
The study is not exempt from limitations. First, this study is exploratory, as the cross-sectional design prohibits inferring causal relationships among variables. Further research should utilize longitudinal data to explore causality. In addition, a single item was used to assess the experience of discrimination, and both internalized stigmatization and shame scales are short compared with other studies. Therefore, psychometric properties could not be fully established, although similar items and scales [40,41] had been used in previous studies. Future studies should use multi-item and context-specific instruments to access the experience of discrimination. Second, large-scale gatherings and dispensable mobilization were strictly prohibited due to the stern restrictions and sealed management implemented by universities in Wuhan. For this reason, we adopted the convenience sampling method, which may restrict the representativeness of our samples. Third, the findings of this study may not generally apply to other groups as the sample was non-randomly selected and limited to university students. Hence, further research can carry out among different groups suffering the stigma, especially in those areas with a weak medical system. Furthermore, follow-up qualitative studies, and a more sophisticated questionnaire design, are urgently needed to explore more specific effects of COVID-19-related discrimination in the future.
5. Conclusions
Our findings extended previous cross-sectional research and demonstrated that the experience of COVID-19-related discrimination was positively associated with shame and internalized stigma, which in turn predicted negative mental health outcomes over time. First, these findings suggested that there was a trade-off between the merits of mandatory measures and the risk of pervasive social tensions. Hence, policymakers were supposed to balance tensions between discrimination as well as stigma mitigation and the COVID-19 containment so as to eliminate discrimination. Second, misinformation and negative stereotypes are key drivers of fear and stigma. The implication of this mediation analysis is that inclusive language and less stigmatizing terminology are urgently needed to prevent stigmatization, and an emerging disease should not be attached to location or ethnicity. Meanwhile, it would be important for social influencers and community leaders to create public awareness of fighting the pandemic, without stigma, through social media or the online community, and construct a supportive and tolerant environment to help subdue unverified rumors and alleviate stigmatization among individuals who exhibit a potential and perceived linkage with COVID-19. Third, college students who have been affected by COVID-19 should not be reckoned with. Tailored intervention strategies, such as large-scale COVID-19-related psychoeducation programs and accessible psychological counseling, were needed to mitigate individual negative mental health outcomes on an intrapersonal level in college settings.
Acknowledgments
The authors would like to thank Li Jiannan for her willingness to provide the Chinese version scales of internalized stigma and shame in this study. We also want to thank the administrative staff in HUST for their effort in collecting the data.
Author Contributions
Conceptualization, H.L. (Hao Li); data curation, H.L. (Hao Li); formal analysis, L.Z. (Ling Zheng); funding acquisition, H.T.; investigation, L.Z. (Ling Zheng), L.Z. (Lijun Zhuo), Q.W., and G.M.; methodology, H.L. (Hao Li) and L.Z. (Ling Zheng); project administration, G.M. and H.T.; software, L.Z. (Ling Zheng); supervision, H.L. (Hong Le); validation, L.Z. (Ling Zheng); writing—original draft, H.L. (Hao Li) and L.Z. (Ling Zheng); writing—review and editing, L.Z. (Ling Zheng), H.L. (Hong Le), and L.Z. (Lijun Zhuo). All authors have read and agreed to the published version of the manuscript.
Funding
The research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White A.I.R. Historical linkages: Epidemic threat, economic risk, and xenophobia. Lancet. 2020;395:1250–1251. doi: 10.1016/S0140-6736(20)30737-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villa S., Jaramillo E., Mangioni D., Bandera A., Gori A., Raviglione M.C. Stigma at the time of the COVID-19 pandemic. Clin. Microbiol. Infect. 2020;11:1450–1452. doi: 10.1016/j.cmi.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devakumar D., Shannon G., Bhopal S.S., Abubakar I. Racism and discrimination in COVID-19 responses. Lancet. 2020;395:1194. doi: 10.1016/S0140-6736(20)30792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anwar A., Malik M., Raees V., Anwar A. Role of Mass Media and Public Health Communications in the COVID-19 Pandemic. Cureus. 2020;12:e10453. doi: 10.7759/cureus.10453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mendoza-Denton R., Downey G., Purdie V.J., Davis A., Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. J. Pers. Soc. Psychol. 2002;83:896–918. doi: 10.1037/0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- 8.Bos A.E.R., Pryor J.B., Reeder G.D., Stutterheim S.E. Stigma: Advances in Theory and Research. Basic Appl. Soc. Psychol. 2013;35:1–9. doi: 10.1080/01973533.2012.746147. [DOI] [Google Scholar]
- 9.Link B.G., Phelan J.C. Conceptualizing Stigma. Annu. Rev. Sociol. 2001;27:363–385. doi: 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- 10.Major B., O’Brien L.T. The social psychology of stigma. Annu. Rev. Psychol. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- 11.Hebl M.R., Dovidio J.F. Promoting the “Social” in the Examination of Social Stigmas. Personal. Soc. Psychol. Rev. 2005;9:156–182. doi: 10.1207/s15327957pspr0902_4. [DOI] [PubMed] [Google Scholar]
- 12.Earnshaw V.A., Chaudoir S.R. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav. 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mumin A.A., Gyasi R.M., Segbefia A.Y., Forkuor D., Ganle J.K. Internalised and Social Experiences of HIV-Induced Stigma and Discrimination in Urban Ghana. Glob. Soc. Welfare. 2018;5:83–93. doi: 10.1007/s40609-018-0111-2. [DOI] [Google Scholar]
- 14.Baldassarre A., Giorgi G., Alessio F., Lulli L.G., Arcangeli G., Mucci N. Stigma and Discrimination (SAD) at the Time of the SARS-CoV-2 Pandemic. Int. J. Environ. Res. Public Health. 2020;17:6341. doi: 10.3390/ijerph17176341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fischer L.S., Mansergh G., Lynch J., Santibanez S. Addressing Disease-Related Stigma During Infectious Disease Outbreaks. Disaster Med. Public Health Prep. 2019;13:989–994. doi: 10.1017/dmp.2018.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang H., Bin P., He A.J. Opinions from the epicenter: An online survey of university students in Wuhan amidst the COVID-19 outbreak1. J. Chin. Gov. 2020;5:234–248. doi: 10.1080/23812346.2020.1745411. [DOI] [Google Scholar]
- 17.Ransing R., Ramalho R., de Filippis R., Ojeahere M.I., Karaliuniene R., Orsolini L., Pinto da Costa M., Ullah I., Grandinetti P., Gashi Bytyci D., et al. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: Drivers, facilitators, manifestations, and outcomes across the world. Brain Behav. Immun. 2020;89:555–558. doi: 10.1016/j.bbi.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu I.H.C., Tsai W., McNeill L.H., Lu Q. The associations of self-stigma, social constraints, and sleep among Chinese American breast cancer survivors. Support. Care Cancer. 2020;28:3935–3944. doi: 10.1007/s00520-019-05233-x. [DOI] [PubMed] [Google Scholar]
- 19.Emlet C.A. A Comparison of HIV Stigma and Disclosure Patterns Between Older and Younger Adults Living with HIV/AIDS. AIDS Patient Care STDs. 2006;20:350–358. doi: 10.1089/apc.2006.20.350. [DOI] [PubMed] [Google Scholar]
- 20.Angelo A., Alonzo N.R.R. Stigma, HIV and AIDS: An exploration and elaboration of a stigma trajectory. Soc. Sci. Med. 1995;41:303–315. doi: 10.1016/0277-9536(94)00384-6. [DOI] [PubMed] [Google Scholar]
- 21.Liu Y., Finch B.K., Brenneke S.G., Thomas K., Le P.D. Perceived Discrimination and Mental Distress Amid the COVID-19 Pandemic: Evidence From the Understanding America Study. Am. J. Prev. Med. 2020;59:481–492. doi: 10.1016/j.amepre.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan B.T., Pradeep A., Prasad L., Murugesan V., Chandrasekaran E., Kumarasamy N., Mayer K.H., Tsai A.C. Association between internalized stigma and depression among HIV-positive persons entering into care in Southern India. J. Glob. Health. 2017;7:020403. doi: 10.7189/jogh.07.020403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li J., Liang W., Yuan B., Zeng G. Internalized Stigmatization, Social Support, and Individual Mental Health Problems in the Public Health Crisis. Int. J. Environ. Res. Public Health. 2020;17:4507. doi: 10.3390/ijerph17124507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Postgrad. Med. J. 1969;45:642. doi: 10.1136/pgmj.45.527.642. [DOI] [Google Scholar]
- 25.Pantelic M., Casale M., Cluver L., Toska E., Moshabela M. Multiple forms of discrimination and internalized stigma compromise retention in HIV care among adolescents: Findings from a South African cohort. J. Int. AIDS Soc. 2020;23:e25488. doi: 10.1002/jia2.25488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tracy J.L., Robins R.W. TARGET ARTICLE: “Putting the Self into Self-Conscious Emotions: A Theoretical Model”. Psychol. Inq. 2004;15:103–125. doi: 10.1207/s15327965pli1502_01. [DOI] [Google Scholar]
- 27.Lopez-Pelayo H., Aubin H.J., Drummond C., Dom G., Pascual F., Rehm J., Saitz R., Scafato E., Gual A. “The post-COVID era”: Challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Med. 2020;18:241. doi: 10.1186/s12916-020-01693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sahoo S., Mehra A., Suri V., Malhotra P., Yaddanapudi L.N., Dutt Puri G., Grover S. Lived experiences of the corona survivors (patients admitted in COVID wards): A narrative real-life documented summaries of internalized guilt, shame, stigma, anger. Asian J. Psychiatr. 2020;53:102187. doi: 10.1016/j.ajp.2020.102187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abadia-Barrero C.E., Castro A. Experiences of stigma and access to HAART in children and adolescents living with HIV/AIDS in Brazil. Soc. Sci. Med. 2006;62:1219–1228. doi: 10.1016/j.socscimed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 30.Northrop J.M. A dirty little secret: Stigma, shame and hepatitis C in the health setting. Med. Humanit. 2017;43:218–224. doi: 10.1136/medhum-2016-011099. [DOI] [PubMed] [Google Scholar]
- 31.Badahdah A.M., Foote C.E. Role of shame in the stigmatization of people with human immunodeficiency virus: A survey of female college students in 3 Arab countries. East. Mediterr. Health J. 2010;16:982–987. doi: 10.26719/2010.16.9.982. [DOI] [PubMed] [Google Scholar]
- 32.Wood L., Byrne R., Burke E., Enache G., Morrison A.P. The impact of stigma on emotional distress and recovery from psychosis: The mediatory role of internalised shame and self-esteem. Psychiatry Res. 2017;255:94–100. doi: 10.1016/j.psychres.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 33.Visser M.J., Kershaw T., Makin J.D., Forsyth B.W. Development of parallel scales to measure HIV-related stigma. AIDS Behav. 2008;12:759–771. doi: 10.1007/s10461-008-9363-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fortenberry J.D., McFarlane M., Bleakley A., Bull S., Fishbein M., Grimley D.M., Malotte C.K., Stoner B.P. Relationships of Stigma and Shame to Gonorrhea and HIV Screening. Am. J. Public Health. 2002;92:378–381. doi: 10.2105/AJPH.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jie H.x.L.C.Q. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch. Psychiatry. 2010;22:200–203. doi: 10.3969/j.issn.1002-0829.2010.04.002. [DOI] [Google Scholar]
- 36.Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y.L., Liang W., Chen Z.M., Zhang H.M., Zhang J.H., Weng X.Q., Yang S.C., Zhang L., Shen L.J., Zhang Y.L. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia Pac. Psychiatry. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 38.Yu D.S. Insomnia Severity Index: Psychometric properties with Chinese community-dwelling older people. J. Adv. Nurs. 2010;66:2350–2359. doi: 10.1111/j.1365-2648.2010.05394.x. [DOI] [PubMed] [Google Scholar]
- 39.Wu K.K., Chan K.S. The development of the Chinese version of Impact of Event Scale--Revised (CIES-R) Soc. Psychiatry Psychiatr. Epidemiol. 2003;38:94–98. doi: 10.1007/s00127-003-0611-x. [DOI] [PubMed] [Google Scholar]
- 40.Xin M., Luo S., She R., Yu Y., Li L., Wang S., Ma L., Tao F., Zhang J., Zhao J., et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am. Psychol. 2020;75:607–617. doi: 10.1037/amp0000692. [DOI] [PubMed] [Google Scholar]
- 41.Turan B., Rogers A.J., Rice W.S., Atkins G.C., Cohen M.H., Wilson T.E., Adimora A.A., Merenstein D., Adedimeji A., Wentz E.L., et al. Association between Perceived Discrimination in Healthcare Settings and HIV Medication Adherence: Mediating Psychosocial Mechanisms. AIDS Behav. 2017;21:3431–3439. doi: 10.1007/s10461-017-1957-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee S., Chan L.Y., Chau A.M., Kwok K.P., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61:2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Person B.P., Sy F., Holton K., Govert B., Liang A. Fear and Stigma: The Epidemic within the SARS Outbreak. Emerg. Infect. Dis. 2004;10:358–363. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tenkorang E.Y. Ebola-related stigma in Ghana: Individual and community level determinants. Soc. Sci. Med. 2017;182:142–149. doi: 10.1016/j.socscimed.2017.03.060. [DOI] [PubMed] [Google Scholar]
- 45.Smith-Morris C. Epidemiological placism in public health emergencies: Ebola in two Dallas neighborhoods. Soc. Sci. Med. 2017;179:106–114. doi: 10.1016/j.socscimed.2017.02.036. [DOI] [PubMed] [Google Scholar]
- 46.Schmitt M.T., Branscombe N.R., Postmes T., Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychol. Bull. 2014;140:921–948. doi: 10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- 47.Silvan-Ferrero P., Recio P., Molero F., Nouvilas-Palleja E. Psychological Quality of Life in People with Physical Disability: The Effect of Internalized Stigma, Collective Action and Resilience. Int. J. Environ. Res. Public. Health. 2020;17:1802. doi: 10.3390/ijerph17051802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mak W.W., Cheung R.Y., Law R.W., Woo J., Li P.C., Chung R.W. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc. Sci. Med. 2007;64:1549–1559. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 49.Rinehart R., Rao D., Amico R.K., Ruiz E., Brandes P., Correa C., Pasalar S., Lama J.R., Duerr A., Molina Y. Experienced HIV-Related Stigma and Psychological Distress in Peruvian Sexual and Gender Minorities: A Longitudinal Study to Explore Mediating Roles of Internalized HIV-Related Stigma and Coping Styles. AIDS Behav. 2019;23:661–674. doi: 10.1007/s10461-018-2348-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lin C.Y., Tsang H.W.H. Stigma, Health and Well-Being. Int. J. Environ. Res. Public Health. 2020;17:7615. doi: 10.3390/ijerph17207615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garrido-Hernansaiz H., Alonso-Tapia J. Predictors of anxiety and depression among newly diagnosed people living with HIV: A longitudinal study. Scand. J. Psychol. 2020;61:616–624. doi: 10.1111/sjop.12621. [DOI] [PubMed] [Google Scholar]
- 52.Boyes M.E., Pantelic M., Casale M., Toska E., Newnham E., Cluver L.D. Prospective associations between bullying victimisation, internalised stigma, and mental health in South African adolescents living with HIV. J. Affect. Disord. 2020;276:418–423. doi: 10.1016/j.jad.2020.07.101. [DOI] [PubMed] [Google Scholar]
- 53.Lin C.Y., Tsai M.C., Liu C.H., Lin Y.C., Hsieh Y.P., Strong C. Psychological Pathway from Obesity-Related Stigma to Depression via Internalized Stigma and Self-Esteem among Adolescents in Taiwan. Int. J. Environ. Res. Public Health. 2019;16:4410. doi: 10.3390/ijerph16224410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chan K.K.S., Fung W.T.W. The impact of experienced discrimination and self-stigma on sleep and health-related quality of life among individuals with mental disorders in Hong Kong. Qual. Life Res. 2019;28:2171–2182. doi: 10.1007/s11136-019-02181-1. [DOI] [PubMed] [Google Scholar]
- 55.Murphy P.J., Garrido-Hernansaiz H., Mulcahy F., Hevey D. HIV-related stigma and optimism as predictors of anxiety and depression among HIV-positive men who have sex with men in the United Kingdom and Ireland. AIDS Care. 2018;30:1173–1179. doi: 10.1080/09540121.2018.1445827. [DOI] [PubMed] [Google Scholar]
- 56.Picco L., Lau Y.W., Pang S., Abdin E., Vaingankar J.A., Chong S.A., Subramaniam M. Mediating effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes among psychiatric outpatients: Findings from a cross-sectional survey in Singapore. BMJ Open. 2017;7:e018228. doi: 10.1136/bmjopen-2017-018228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adewuya A.O., Afolabi M.O., Ola B.A., Ogundele O.A., Ajibare A.O., Oladipo B.F., Fakande I. Post-traumatic stress disorder (PTSD) after stigma related events in HIV infected individuals in Nigeria. Soc. Psychiatry Psychiatr. Epidemiol. 2009;44:761–766. doi: 10.1007/s00127-009-0493-7. [DOI] [PubMed] [Google Scholar]
- 58.Birchwood M., Trower P., Brunet K., Gilbert P., Iqbal Z., Jackson C. Social anxiety and the shame of psychosis: A study in first episode psychosis. Behav. Res. Ther. 2007;45:1025–1037. doi: 10.1016/j.brat.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 59.Ilic M., Reinecke J., Bohner G., Rottgers H.O., Beblo T., Driessen M., Frommberger U., Corrigan P.W. Protecting self-esteem from stigma: A test of different strategies for coping with the stigma of mental illness. Int. J. Soc. Psychiatry. 2012;58:246–257. doi: 10.1177/0020764010392058. [DOI] [PubMed] [Google Scholar]
- 60.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Herek G.M., Saha S., Burack J. Stigma and Psychological Distress in People With HIV/AIDS. Basic Appl. Soc. Psychol. 2013;35:41–54. doi: 10.1080/01973533.2012.746606. [DOI] [Google Scholar]