Abstract
Simple Summary
In this study, we measured the plasmatic concentration of Kinase inhibitors (KI) among a population with non-small cell lung cancer (NSCLC) harboring driver genetic alterations. They received erlotinib, gefitinib, osimertinib, crizotinib, or dabrafenib (with or without trametinib) for at least three months. The results were measured by ultra-performance liquid chromatography coupled with tandem mass spectrometry and compared to previously published data. Between November 2013 and February 2019, fifty-one samples were analyzed. The main outcome was the rate of samples with suboptimal KI plasma concentrations. Suboptimal plasma concentrations were observed in 51% (26/51) of cases and might contribute to treatment failure.
Abstract
Kinase inhibitors (KI) have dramatically improved the outcome of treatment in patients with non-small cell lung cancer (NSCLC), which harbors an oncogene addiction. This study assesses KI plasma levels and their clinical relevance in patients chronically exposed to KIs. Plasma samples were collected in NSCLC patients receiving erlotinib, gefitinib, osimertinib, crizotinib, or dabrafenib (with or without trametinib) for at least three months between November 2013 and February 2019 in a single institution. KI drug concentrations were measured by ultra-performance liquid chromatography coupled with tandem mass spectrometry and compared to published data defining optimal plasma concentration. The main outcome was the rate of samples with suboptimal KI plasma concentrations. Secondary outcomes included its impact on T790M mutation emergence in patients receiving a first-generation epidermal growth factor receptor (EGFR) KI. Fifty-one samples were available from 41 patients with advanced NSCLC harboring driver genetic alterations, including EGFR, v-Raf murine sarcoma viral oncogene homolog B (BRAF), anaplastic lymphoma kinase (ALK) or ROS proto-oncogene 1 (ROS1), and who had an available evaluation of chronic KI plasma exposure. Suboptimal plasma concentrations were observed in 51% (26/51) of cases. In EGFR-mutant cases failing first-generation KIs, EGFR exon 20 p.T790M mutation emergence was detected in 31% (4/13) of samples in optimal vs. none in suboptimal concentration (0/5). Suboptimal plasma concentrations of KIs are frequent in advanced NSCLC patients treated with a KI for at least three months and might contribute to treatment failure.
Keywords: non-small cell lung cancer, oncogene addiction, kinase inhibitors, chronic plasmatic exposure, resistance mutation
1. Introduction
Kinase inhibitors (KIs) form the cornerstone of the therapeutic strategy in patients with non-small cell lung cancer (NSCLC) harboring molecular driver alterations, such as epidermal growth factor receptor (EGFR) mutations, v-Raf murine sarcoma viral oncogene homolog B (BRAF) mutations, anaplastic lymphoma kinase (ALK) fusions, ROS proto-oncogene 1 (ROS1) fusions, etc. [1]. Although an initial benefit under KIs is common, all patients ultimately experience disease progression. One cause of KI failure is the acquisition of resistance mechanisms at the molecular level. Next-generation KIs were successfully developed to overcome resistance to the previous-generation KIs. One of the best-known examples is osimertinib, which has demonstrated impressive antitumor activity against NSCLC harboring an EGFR mutation, either an exon 19 deletion (Ex19del), an exon 21 p.L858R, or an exon 20 p.T790M, the latter being acquired under first-generation kinase inhibitors (erlotinib, gefitinib) [2]. However, few KIs have been approved in NSCLC, and strategies aimed at optimizing the duration of response are needed. One such approach involves a better understanding of the pharmacology of KIs.
In oncology, suboptimal KI plasma concentrations have been associated with a lack of antitumor efficacy (Table S1) [3,4,5], and represents a plausible explanation for KI failure. The therapeutic index of this category of drugs is often narrow, and most are prescribed as a flat dose. Furthermore, KI plasma concentrations vary depending on several factors, such as body weight, smoking status [6], concomitant drug intake [7,8], and adherence [9]. Plasma concentrations of KIs can also decrease over time, due to the drug’s pharmaceutical properties, such as CYP3A5/CYP3A4 auto-induction or P-glycoprotein auto-induction, which will increase the drug’s clearance [10].
For KIs, the pharmacokinetic steady state is usually reached after two to three weeks of treatment depending on the half-life of the drug, however, data on the dynamic evolution of KI plasma concentrations are limited [5]. A retrospective study of plasma concentration of sorafenib measured every 15 days by liquid chromatography in a population of hepatocellular carcinoma patients has been reported, with sampling from initiation of treatment until progression [10]. This showed that exposure after three months of treatment was lower than after one month of treatment. In the event of a decrease in plasma concentration over time, intra-patient adaptation could be discussed within the framework of target drug monitoring (TDM) [4]. TDM involves the measurement and interpretation of drug concentrations in biological fluids to determine drug dosage for an individual patient. This strategy is used in clinical practice for various therapeutic drug classes, including antibiotics, immunosuppressors, antiepileptics, and antiarrhythmic agents [4,11]. In oncology, TDM is widely accepted for imatinib in chronic myeloid leukemia [12], and is currently being explored in oncogene-addicted NSCLC [3,4,5]. Good candidates for TDM are drugs with a narrow therapeutic window and a direct relationship between plasma concentrations and efficacy or toxicity pharmacokinetic-pharmacodynamic relationships [13]. In oncogene-addicted advanced NSCLC, chronic plasma exposure to KIs and its clinical relevance, in particular at the time of disease progression, is poorly described. We aimed to assess the clinical and molecular impact of chronic suboptimal KI plasma concentrations in patients with oncogene-addicted advanced NSCLC.
2. Patients and Methods
A monocentric observational study was performed in the context of routine clinical care.
2.1. Patients
Patients with advanced NSCLC harboring oncogenic drivers, such as an EGFR-mutation, BRAFV600E-mutation, ALK-fusion, or ROS1-fusion, treated with KI therapy for at least three months were eligible. Patients receiving erlotinib, gefitinib, osimertinib, crizotinib, or dabrafenib (with or without trametinib) in the context of a trial (academic or clinical), expanded access, or routine clinical care between November 2013 and February 2019 were screened. KI plasma concentrations were evaluated in blood samples collected during therapy, and at the time of clinical response or relapse. Chronic plasma exposure was defined as at least three months of KI therapy. Clinical and pathological data were extracted from electronic medical records. Radiological assessments were performed every 8 or 12 weeks per Response Evaluation Criteria in Solid Tumors (RECIST) v1.1 and per the treating physician’s discretion.
2.2. Assessment of Plasma Exposure
Residual plasma concentrations of drugs were measured in blood samples using ultra-performance liquid chromatography coupled with tandem mass spectrometry validated methods [10]. A residual estimate based on pharmacokinetic and population pharmacokinetic analysis parameters (Table S2) was made for samples not collected at the time of the residual sampling.
Additional information about the methodology is present in the Supplementary Materials.
Precise measurement of trough concentrations is challenging in routine practice, due to the constraints of the logistics of blood collection at a precise time and the fact that the timing of administration varies from patient to patient. We defined three situations according to the dosing time with respect to the last dose: Optimal, evaluable, and non-interpretable.
Optimal: The optimal concentration corresponds to the true residual plasma concentration at a steady state, in the blood collection performed immediately before the next administration.
- Evaluable: The residual plasma concentration is estimated by an extrapolation method from known pharmacokinetic parameters (distribution volume, half-life, clearance) and from data obtained in population pharmacokinetic models [14]. This estimate of standard trough concentration (Cmin, std) is only possible when blood samples were collected at steady state or during the terminal elimination phase of the drug, since in this phase, the elimination rate is linear [14,15].
-
-C (min, std) = C(t) * 0.5 ^ (Delta (t)/t1/2)
-
-C (min, std) = C(t) * exp (k(e) x Delta (t))
-
-
Delta t = t − tau, tau is 24 h when collecting a sample once a day, or 12 h when collecting samples twice a day, k(e) is the elimination rate constant.
Pharmacokinetic parameters and a population pharmacokinetic study are summarized in Table S2.
-
3.
Not interpretable: Extrapolation is not feasible for samples taken during the plasma peak period.
Residual plasma concentrations (optimal and evaluable) were compared to target values recommended in the literature for TDM to define the ‘optimal concentration’ for each KI (erlotinib > 500 ng/mL, gefitinib > 200 ng/mL, osimertinib > 166 ng/mL, crizotinib > 235 ng/mL, dabrafenib > 96.1 ng/mL, trametinib > 10.6 ng/mL) or ‘suboptimal concentration’ [3,4,5] (Table S1).
2.3. Somatic Molecular Analysis
ALK fusion was assessed by immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH), while ROS1 FISH was used to assessed fusions, and reverse transcriptase-polymerase chain reaction (RT-PCR) or next-generation sequencing (NGS) was used to assess mutations and/or other alterations.
Blood sample collections and ctDNA (for mutational analyses) were collected over time, including at the time of radiological disease evaluation. Plasma was isolated, and ctDNA analysis was performed centrally (Gustave Roussy, France) using a targeted panel. The panel used is described in Table 1.
Table 1.
The molecular testing panel in tissue/blood samples from 18 patients with EGFR-mutated NSCLC after failing a first-generation kinase inhibitor.
| N# | Driver Alteration | Other Alteration | Kinase Inhibitor | NGS Panel (Tissue) | NGS Panel (Blood) | EGFR T790M ddPCR Stilla® (Blood) |
|---|---|---|---|---|---|---|
| 1 | EGFR exon 21 p. L858R | No | Gefitinib | - | CHP2 *: Not detected | Not detected |
| 2 | EGFR exon 21 p. L858R | No | Gefitinib | - | - | T790M detected |
| 3 | EGFR exon 21 p. L858R | No | Gefitinib | Oncomine® Lung: T790M detected | CHP2 *: Not detected | - |
| 4 | EGFR exon 21 p. L858R | No | Gefitinib | - | CHP2 *: Not detected | Not detected |
| 5 | EGFR exon 19 deletion | TP53 | Gefitinib | MOSC4: T790M not detected | - | - |
| 6 | EGFR exon 19 deletion | No | Gefitinib | - | - | Not detected |
| 7 | EGFR exon 19 deletion | No | Gefitinib | MOSC4: T790M not detected | - | T790M detected |
| 8 | EGFR exon 21 p.L833F | TP53, CKDN2A | Erlotinib | - | - | ddPCR Not detected |
| 9 | EGFR exon 19 deletion | No | Erlotinib | - | - | Not detected |
| 10 | EGFR exon 19 deletion | No | Erlotinib | - | - | Not detected |
| 11 | EGFR exon 19 deletion | No | Erlotinib | - | - | Not detected |
| 12 | EGFR exon 19 deletion | No | Erlotinib | MOSC4: T790M detected | - | T790M detected |
| 13 | EGFR exon 21 p. L858R | No | Erlotinib | Unknown: not detected | - | - |
| 14 | EGFR exon 19 deletion | No | Erlotinib | MOSC4: T790M not detected | - | Not detected |
| 15 | EGFR exon 19 deletion | No | Erlotinib | MOSC4: T790M not detected | - | - |
| 16 | EGFR exon 19 deletion | No | Erlotinib | MOSC4: T790M not detected | CHP2 *: Not detected | - |
| 17 | EGFR exon 21 p. L858R | No | Erlotinib | OCAV3: T790M not detected | Oncomine® Lung: Not detected | - |
| 18 | EGFR exon 19 deletion | No | Erlotinib | NSCLC: T790M not detected | - | Not detected |
(-): Test not performed; ddPCR: droplet digital polymerase chain reaction, CHP2 *: Ion Ampliseq Cancer Hotspot Panel v2 targeting 50 cancer genes (Thermo Fisher Scientific), MOSC4: Gustave Roussy homemade panel targeting 82 genes, OCAV3: Oncomine Comprehensive Assay v3M (Thermo Fisher Scientific) with 161 genes and NSCLC: Sentosa SQ Non-Small Cell Lung Cancer Panel (Vela Diagnostics) targeting 11 genes.
Panels tested in blood samples (liquid biopsy):
-
-
CHP2 (Ion AmpliSeq Cancer Hotspot Panel v2 (CHP2)) designed to amplify 207 amplicons covering 50 genes (Thermo Fisher Scientific)).
-
-
Oncomine lung (Oncomine Lung ctDNA Assay contains 35 amplicons covering 11 genes (Thermo Fisher Scientific)). A unique molecular identifier is combined with each single DNA molecule. For calling the detected variants, the following parameters were applied: Allele Read count > 10; Fusion read count > 1; Variant type: Single nucleotide variant, insertion-deletion, multi-nucleotide variant, copy number variant, long deletion, fusion; Variant effect: Unknown, missense, none frameshift Insertion, none frameshift Deletion, non-sense, stop loss, frameshift insertion, frameshift deletion.
Panels used for tissue samples:
-
-
MOSC4 (Ion AmpliSeq MOSC4 designed to cover 82 genes, combining two other panels (CHP2 + Safir02)).
-
-
OCAV3 (Ion AmpliSeq Oncomine Comprehensive Assay V3 enables the detection of mutations across 161 genes, gene fusions, and copy number variations (Thermo Fisher Scientific)).
-
-
Sentosa SQ NSCLC (Sentosa SQ Non-Small Cell Lung Cancer panel targets 11 genes with 28 amplicons (Vela Diagnostics)). For calling the detected variants, following parameters were applied: 5000 Exomes Global MAF < 0.01; Allele frequency > 0.02; Allele ratio > 0.02; Allele read counts > 50; Alternate read counts > 30; Fusion read counts > 50; Variant effect: Unknown, missense, none frameshift insertion, none frameshift deletion, stop loss, non-sense, frameshift insertion, frameshift deletion; Variant type: Single nucleotide variant, insertion-deletion, multi-nucleotide variant, copy number variant, long deletion, fusion.
2.4. Statistical Analysis
Median values (interquartile range) and frequencies (percentage) were calculated for continuous and categorical variables, respectively. Medians and proportions were compared using the Student’s t-test and chi-square test (or Fisher’s exact test, if appropriate), respectively.
Time to treatment failure was defined as the time between KI initiation and progression. Overall survival (OS) was defined as the time between KI initiation and death from any cause. Time to treatment failure and OS were estimated using the Kaplan-Meier method and described using median values with their 95% confidence intervals (95% CI). Follow-up was calculated using the reverse Kaplan-Meier method. Correlation between exposure and EGFR exon 20 p.T790M mutation occurrence was evaluated with a Pearson correlation coefficient.
All statistical analyses were performed with R studio version 2.15.2, p-values < 0.05 were considered statistically significant, and all tests were two-sided.
3. Results
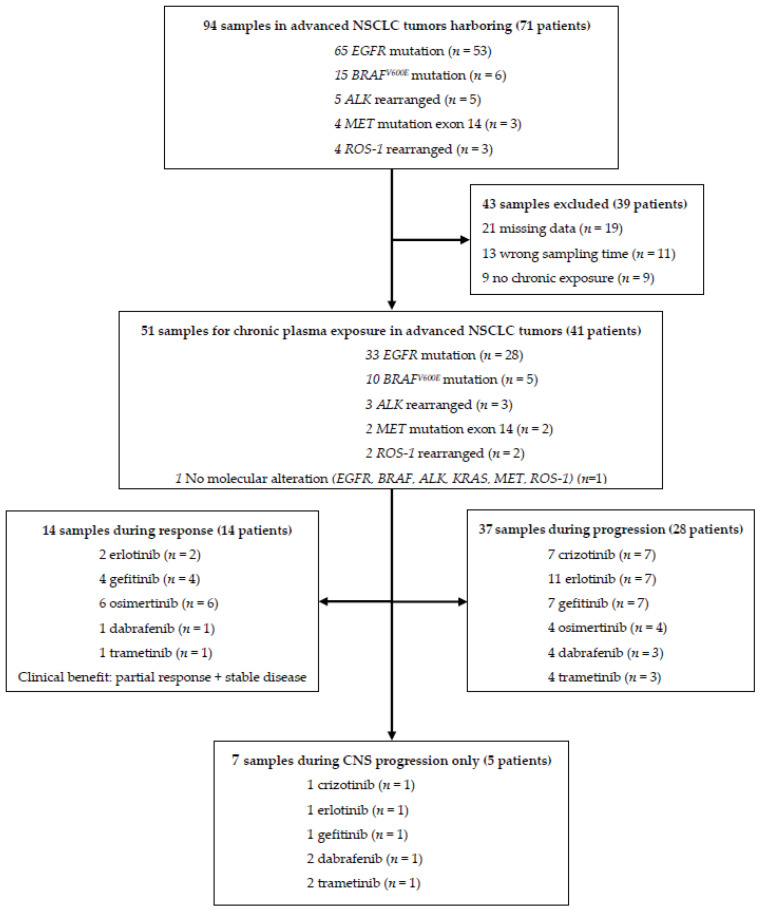
A total of 94 plasma samples from 71 patients were prospectively collected. Among them, 43 samples were excluded, due to missing data, including the time of last drug intake (n = 21), technical issues (n = 13), and treatment for less than three months (n = 9) (Figure 1). A total of 51 samples from 41 patients were eligible for evaluation. During the evaluation period, patients received treatment with erlotinib (n = 13), gefitinib (n = 11), osimertinib (n = 10), crizotinib (n = 7) and dabrafenib (n = 5) + trametinib (n = 5). Baseline characteristics are summarized in Table 2 for eligible samples and in Table S3 for patients. The 51 eligible samples were collected after a median of 20.3 months (95% CI, 6.29 to 25.5) on KI treatment.
Figure 1.
Flow diagram of samples and the study population.
Table 2.
Sample baseline characteristics and according to plasma kinase inhibitor concentration.
| Characteristics, No. (%) | All Samples (n = 51) | Optimal Concentration (n = 25) | Suboptimal Concentration (n = 26) | p-Value |
|---|---|---|---|---|
| Molecular alteration:ALK-rearranged, BRAFV600E mutation, EGFR deletion exon 19, EGFR mutation exon 21 (L858R), EGFR mutation exon 21 (L833F), ROS-1 rearranged, MET mutation exon 14, No molecular alteration (ALK, BRAF, EGFR, KRAS, MET, ROS-1) | 3 (7%), 10 (19%), 23 (45%), 9 (17%), 1 (2%), 2 (4%), 2 (4%), 1 (2%) | 0 (0%), 4 (16%), 12 (48%), 6 (24%), 1 (4%), 1 (4%), 1 (4%), 0 | 3 (12%), 6 (22%), 11 (42%), 3 (12%), 0, 1 (4%), 1 (4%), 1 (4%) | p = 0.50 |
| Kinase inhibitor: Erlotinib, Gefitinib, Osimertinib, Crizotinib, Dabrafenib, Trametinib | 13 (26%), 11 (21%), 10 (19%), 7 (14%), 5 (10%), 5 (10%) | 7 (28%), 8 (32%), 4 (16%), 2 (8%), 2 (8%), 2 (8%) | 6 (23%), 3 (11.5%), 6 (23%), 5 (19.5%), 3 (11.5%), 3 (11.5%) | p = 0.52 |
| Stage at diagnosis: I-II, III, IV | 1 (2%), 2 (4%), 48 (94%) | 0, 2 (8%), 23 (92%) | 1 (4%), 0, 25 (96%) | p = 0.24 |
| Lines of previous kinase inhibitors: ≤2, >2 | 44 (86%), 7 (14%) | 20 (80%), 5 (20%) | 24 (92%), 2 (8%) | p = 0.25 |
| Current smoker: Yes, No | 5 (10%), 46 (90%) | 1 (4%), 24 (96%) | 4 (15%), 22 (85%) | p = 0.35 |
| Concomitant proton pump inhibitor: No, Yes | 35 (69%), 16 (31%) | 15 (60%), 10 (40%) | 20 (77%), 6 (23%) | p = 0.19 |
3.1. Suboptimal Concentration and KI Response
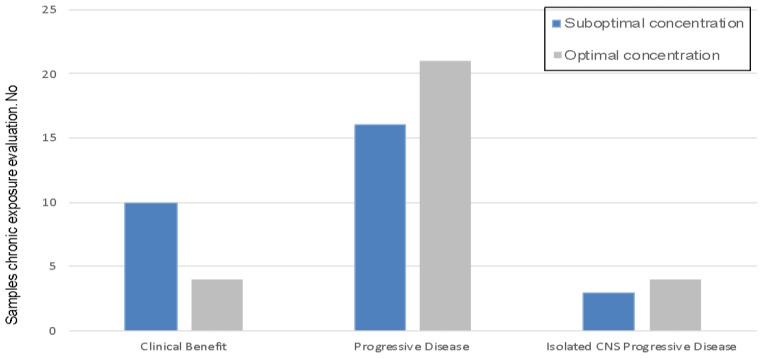
Suboptimal KI plasma concentrations were observed in 26 (51%) samples from 20 (49%) patients. Clinical characteristics, according to KI concentration (suboptimal vs. optimal) are summarized in Table 2. No significant differences were observed for any characteristics evaluated, including tobacco consumption and other drug intake. For samples collected at the time of disease progression, the suboptimal plasma concentration rate was 43% (16/37) vs. 71% (10/14) in samples from patients without progression at the time of sample collection. In cases of isolated intracranial progression, suboptimal plasma concentrations were reported in 43% (3/7) of cases (Figure 2).
Figure 2.
Distribution of plasma exposures according to clinical outcome. Clinical Benefit: Stable disease and partial response. Isolated CNS PD: Isolated central nervous system progressive disease.
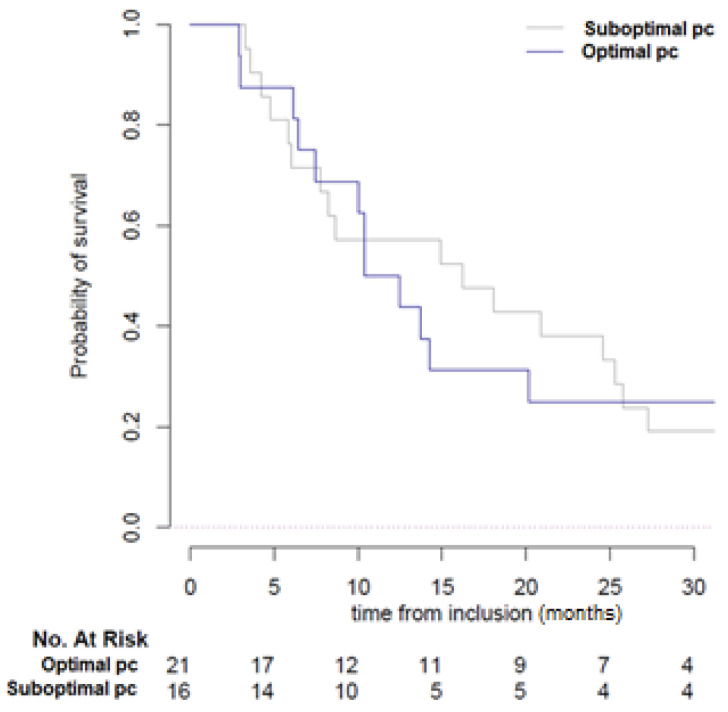
3.2. Clinical Relevance of Suboptimal Concentration
After a median follow-up of 52.4 months (95% CI 35.6 to 106.9), the median OS was 61.1 months (95% CI 30.6 to not reached). The median time to treatment failure in the overall population was 15.9 months (95% CI 13.7 to 25.8). In patients with suboptimal concentrations (n = 26), time to treatment failure was 14.2 months (95% CI 12.48 to 57.4) vs. 18.1 months (95% CI 8.65 to 58.9) in the optimal concentration group (n = 25; p = 0.9) (Figure S1). No significant difference was observed according to the type of KI administered in optimal vs. suboptimal concentration groups (log-rank test, p = 0.52) (Table 2). At the time of progression (n = 16), the median time to treatment failure in the suboptimal concentration group was 16.2 months (95% CI 7.8 to 27.2) vs. 11.4 months (95% CI 7.4 to 57.4) in the optimal concentration, which was not significantly different (log-rank test, p = 0.8) (Figure 3).
Figure 3.
Kaplan-Meier curves of time to treatment failure according to KI plasma concentration. Sub-optimal pc: Suboptimal plasma concentration, Optimal pc: Sub-optimal plasma concentration.
3.3. KI Exposure and Resistance Mechanisms
Among patients with EGFR-mutated NSCLC failing a first-generation KI (n = 24), 18 patients had a molecular evaluation to assess resistance mechanisms. The emergence of EGFR exon 20 p.T790M mutations was detected in 31% (4/13) of patients in the optimal concentration group vs. none in the suboptimal concentration group (0/5) (Spearman r = −0.33, p = 0.18) (Table 1).
4. Discussion
In our cohort of patients with oncogene-addicted NSCLC treated with a KI for at least three months, 51% of blood samples showed suboptimal KI concentrations (plasma concentration below the published recommended values). This is consistent with studies of KI concentrations for other cancers, which report suboptimal concentration rates ranging from 11% to 83% with KIs, including 11% for erlotinib, 49% for sunitinib, and 65–73% for imatinib [12,16]. Various hypotheses have been formulated to explain decreasing concentrations over time, such as a quantitative decrease, due to intrinsic pharmacological properties (CYP3A4 auto-induction, P-glycoprotein auto-induction, etc.), poor adherence, and drug–drug interactions [7,9,10]. In our cohort, 32% of patients (n = 13) received a proton pump inhibitor and 12% (n = 4) were current smokers. These two parameters had no measurable effect on plasmatic exposure. However, cigarette smoke induces CYP1A1 and significantly decreases erlotinib plasmatic exposure, but has no known effect on the exposure of KIs metabolized mostly by other cytochromes (CYP3A4, CYP3A4, CYP2C8, among others) [6]. The absorption of erlotinib and gefitinib requires gastric acidity. Proton pump inhibitors are known to interact with erlotinib and gefitinib, decreasing their bioavailability and the plasmatic exposure [7,17]. This interaction is not relevant for crizotinib, dabrafenib, osimertinib, and trametinib [7,17]. Furthermore, in our study, data were collected retrospectively, making an objective evaluation of adherence impossible, which is one of the main causes of low-plasmatic exposure [9,18].
Suboptimal concentrations could contribute to treatment failure with KIs. The median time to treatment failure was lower in the suboptimal group vs. the optimal concentration group (14.2 vs. 18.2 months), although this was not statistically significant, possibly due to the small number of cases. We also observed a 43% rate of suboptimal concentrations in patients with isolated intracranial progression, which is relevant in light of the low ability of some KIs to cross the blood-brain-barrier, resulting in even lower intracranial concentrations [19].
In patients failing a first-generation EGFR KI, the emergence of the resistance EGFR exon 20 p.T790M is expected in half of these cases [20]. In our cohort, an EGFR exon 20 p.T790M mutation was not detected in any of the five patients with suboptimal concentrations vs. 31% of patients in the optimal concentration group. Although the sample size was small, this supports the hypothesis that tumor progression is more likely with an insufficient plasma concentration of the drug before acquiring molecular resistance. Exclusion of concomitant interfering drugs or intra-patient dose escalation could be efficient strategies for overcoming this phenomenon.
This approach of including pharmacological evaluations and intra-patient dose adaptation in a TDM strategy, to restore plasmatic exposure and possibly tumor response has not been evaluated in oncogene-addicted NSCLC. However, it has been proposed in other malignancies, such as chronic myeloid leukemia with imatinib [4,12,13], thyroid cancer with sorafenib [21], and renal cancer with axitinib [22].
This study has various limitations, including missing data and incomplete adherence data, due to the retrospective nature of the clinical data collection. The sample size is limited, and the population was heterogeneous and received different KIs. In addition, there was no evaluation of the concentration evolution over time that could explain the high rate of suboptimal concentrations in the clinical benefit group (Figure 2). Thus, these findings should be validated in larger prospective studies where different molecular populations are well represented. This may confirm that low plasmatic exposure at tumor progression correlates with KI failure and the emergence of resistance mutations.
5. Conclusions
KI suboptimal concentrations were observed in approximately 50% of advanced NSCLC patients with chronic exposure in our institution; the emergence of resistance mutations was only seen in optimal concentration cases, supporting the hypothesis of suboptimal concentrations as a potential explanation for KI failure.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6694/12/12/3758/s1. Table S1. Overview of practical target drug monitoring recommendation for KIs in thoracic oncology. Table S2. Pharmacokinetics parameters of the KIs evaluated. Table S3. Patient baseline characteristics. Figure S1. Kaplan-Meier curves of time to treatment failure according to plasma concentration.
Author Contributions
Conceptualization, A.G. (Arthur Geraud), L.M., E.A., D.C., J.D., P.G., C.M., C.J., C.C., J.A., C.N., P.L., A.G. (Anas Gazzah), L.L., E.R., D.V., O.M., D.P., A.P., B.B.; methodology, E.A.; software, E.A.; validation, A.G. (Arthur Geraud), L.M., E.A., D.C., J.D., O.M., D.P., A.P. and B.B.; formal analysis, E.A.; resources, A.P. and B.B.; data curation, A.G. (Arthur Geraud), L.M.; writing—original draft preparation, Arthur Geraud and L.M. writing—review and editing, A.G. (Arthur Geraud), L.M., E.A., D.C., J.D., O.M., D.P., A.P. and B.B.; visualization, A.G. (Arthur Geraud), L.M. and B.B.; supervision, L.M., A.P., O.M. and B.B. All authors have read and agreed to the published version of the manuscript.
Funding
Laura Mezquita received support from the 2018 IASLC Research Fellowship Award, ESMO Translational Research Fellowship 2019 and SEOM Retorno de Investigadores 2019.
Conflicts of Interest
Arthur Geraud: As part of the Drug Development Department (DITEP) Principal/sub-Investigator of Clinical Trials for Abbvie, Adaptimmune, Aduro Biotech, Agios Pharmaceuticals, Amgen, Argen-X Bvba, Arno Therapeutics, Astex Pharmaceuticals, Astra Zeneca, Astra Zeneca Ab, Aveo, Bayer Healthcare Ag, Bbb Technologies Bv, Beigene, Bioalliance Pharma, Biontech Ag, Blueprint Medicines, Boehringer Ingelheim, Boston Pharmaceuticals, Bristol Myers Squibb, Bristol-Myers Squibb International Corporation, Ca, Celgene Corporation, Cephalon, Chugai Pharmaceutical Co., Clovis Oncology, Cullinan-Apollo, Daiichi Sankyo, Debiopharm S.A., Eisai, Eisai Limited, Eli Lilly, Exelixis, Forma Tharapeutics, Gamamabs, Genentech, Gilead Sciences, Glaxosmithkline, Glenmark Pharmaceuticals, H3 Biomedicine, Hoffmann La Roche Ag, Incyte Corporation, Innate Pharma, Institut De Recherche Pierre Fabre, Iris Servier, Janssen Cilag, Janssen Research Foundation, Kura Oncology, Kyowa Kirin Pharm. Dev., Lilly France, Loxo Oncology, Lytix Biopharma As, Medimmune, Menarini Ricerche, Merck Kgaa, Merck Sharp & Dohme Chibret, Merrimack Pharmaceuticals, Merus, Millennium Pharmaceuticals, Molecular Partners Ag, Nanobiotix, Nektar Therapeutics, Nerviano Medical Sciences, Novartis Pharma, Octimet Oncology Nv, Oncoethix, Oncomed, Oncopeptides, Onyx Therapeutics, Orion Pharma, Oryzon Genomics, Ose Pharma, Pfizer, Pharma Mar, Philogen S.P.A., Pierre Fabre Medicament, Plexxikon, Rigontec Gmbh, Roche, Sanofi Aventis, Sierra Oncology, Sotio A.S, Syros Pharmaceuticals, Taiho Pharma, Tesaro, Tioma Therapeutics, Wyeth Pharmaceuticals France, Xencor, Y’s Therapeutics, Research Grants from Astrazeneca, BMS, Boehringer Ingelheim, Janssen Cilag, Merck, Novartis, Pfizer, Roche, Sanofi. Non-financial support (drug supplied) from Astrazeneca, Bayer, BMS, Boringher Ingelheim, Johnson & Johnson, Lilly, Medimmune, Merck, NH TherAGuiX, Pfizer, Roche. Laura Mezquita: Sponsored Research: Bristol-Myers Squibb, Boehringer Ingelheim, Amgen. Consulting, advisory role: Roche Diagnostics, Roche, Takeda. Lectures and educational activities: Bristol-Myers Squibb, Tecnofarma, Roche. Travel, Accommodations, Expenses: Bristol-Myers Squibb, Roche. Mentorship program with key opinion leaders: funded by AstraZeneca. Edouard Auclin: Travel expenses: Mundipharma. Lectures and educational activities: Sanofi Genzymes. David Combarel: Nothing to disclose. Julia Delahousse: Nothing to disclose. Paul Gougis: Nothing to disclose. Christophe Massard: Consultant/Advisory fees: Amgen, Astellas, Astra Zeneca, Bayer, BeiGene, BMS, Celgene, Debiopharm, Genentech, Ipsen, Janssen, Lilly, MedImmune, MSD, Novartis, Pfizer, Roche, Sanofi, Orion. Principal/sub-Investigator of ClinicalTrials: Abbvie, Aduro, Agios, Amgen, Argen-x, Astex, AstraZeneca, Aveopharmaceuticals, Bayer, Beigene, Blueprint, BMS, BoeringerIngelheim, Celgene, Chugai, Clovis, DaiichiSankyo, Debiopharm, Eisai, Eos, Exelixis, Forma, Gamamabs, Genentech, Gortec, GSK, H3 biomedecine, Incyte, InnatePharma, Janssen, Kura Oncology, Kyowa, Lilly, Loxo, Lysarc, LytixBiopharma, Medimmune, Menarini, Merus, MSD, Nanobiotix, NektarTherapeutics, Novartis, Octimet, Oncoethix, OncopeptidesAB, Orion, Pfizer, Pharmamar, Pierre Fabre, Roche, Sanofi, Servier, Sierra Oncology, Taiho, Takeda, Tesaro, Xencor. Cécile Jovelet: Nothing to disclose. Caroline Caramella: Honorarium: Pfizer, BMS, MSK, Astra Zeneca. Julien Adam: Advisor/consultant for: AstraZeneca, Bayer, BMS, MSD, Roche. Charles Naltet: Travel expenses: Pfizer, Roche, AstraZeneca. Pernelle Lavaud: Travel, accommodation, congress registration expenses: Astra Zeneca, Mundi Pharma, Ipsen, Astellas, Janssen. Anas Gazzah: Travel, accommodation, congress registration expenses from Boehringer Ingelheim, Novartis, Pfizer, Roche. Consultant/Expert role for Novartis. Principal/sub-Investigator of Clinical Trials for Aduro Biotech, Agios Pharmaceuticals, Amgen, Argen-X Bvba, Arno Therapeutics, Astex Pharmaceuticals, Astra Zeneca, Aveo, Bayer Healthcare Ag, Bbb Technologies Bv, Beigene, Bioalliance Pharma, Biontech Ag, Blueprint Medicines, Boehringer Ingelheim, Bristol Myers Squibb, Ca, Celgene Corporation, Chugai Pharmaceutical Co., Clovis Oncology, Daiichi Sankyo, Debiopharm S.A., Eisai, Exelixis, Forma, Gamamabs, Genentech, Inc., Gilead Sciences, Inc, Glaxosmithkline, Glenmark Pharmaceuticals, H3 Biomedicine, Inc, Hoffmann La Roche Ag, Incyte Corporation, Innate Pharma, Iris Servier, Janssen, Kura Oncology, Kyowa Kirin Pharm, Lilly, Loxo Oncology, Lytix Biopharma As, Medimmune, Menarini Ricerche, Merck Sharp & Dohme Chibret, Merrimack Pharmaceuticals, Merus, Millennium Pharmaceuticals, Nanobiotix, Nektar Therapeutics, Novartis Pharma, Octimet Oncology Nv, Oncoethix, Oncomed, Oncopeptides, Onyx Therapeutics, Orion Pharma, Oryzon Genomics, Pfizer, Pharma Mar, Pierre Fabre, Rigontec Gmbh, Roche, Sanofi Aventis, Sierra Oncology, Taiho Pharma, Tesaro, Inc, Tioma Therapeutics, Inc., Xencor. Research Grants from Astrazeneca, BMS, Boehringer Ingelheim, Janssen Cilag, Merck, Novartis, Pfizer, Roche, Sanofi. Non-financial support (drug supplied) from Astrazeneca, Bayer, BMS, Boringher Ingelheim, Johnson & Johnson, Lilly, Medimmune, Merck, NH TherAGuiX, Pfizer, Roche. Ludovic Lacroix: Consultancy: Abbott, Astrazeneca, Boehringer Ingelheim, Bristol Myers Squibb, Ca Bayer Healthcarer, Illumina, Genomic Health, Myriad, Novartis, Pfizer, Roche, Siemens, Thermofisher, VelaDx. Etienne Rouleau: Board participations: MS, AstraZeneca, Roche. Damien Vasseur: Nothing to disclose. Olivier Mir: Consultancy: Amgen, Astra-Zeneca, Bayer, Bristol Myers-Squibb, Eli-Lilly, Ipsen, Lundbeck, MSD, Novartis, Pfizer, Roche, Servier, Vifor Pharma. Speakers bureau: Eli-Lilly, Roche, Servier. Stock ownership: Amplitude surgical, Ipsen, Transgene. David Planchard: Consulting, advisory role or lectures: AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Daiichi Sankyo, Eli Lilly, Merck, Novartis, Pfizer, prIME Oncology, Peer CME, Roche. Honoraria: AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Merck, Novartis, Pfizer, prIME Oncology, Peer CME, Roche. Clinical trials research: AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly, Merck, Novartis, Pfizer, Roche, Medimmune, Sanofi-Aventis, Taiho Pharma, Novocure, Daiichi Sankyo. Travel, Accommodations, Expenses: AstraZeneca, Roche, Novartis, prIME Oncology, Pfizer. Angelo Paci: Consulting, advisory role or lectures: Fresenius, Pierre Fabre, Pfizer, Servier. Travel, Accommodations, Expenses: Fresenius, Pierre Fabre. Benjamin Besse: Grant Abbvie, Amgen, AstraZeneca, Biogen, Blueprint Medicines, BMS, Celgene, Eli Lilly, GSK, Ignyta, IPSEN, Merck KGaA, MSD, Nektar, Onxeo, Pfizer, Pharma Mar, Sanofi, Spectrum Pharmaceuticals, Takeda, Tiziana Pharma, Investigator or co-investigator of trials: Abbvie, Amgen, AstraZeneca, Biogen, Blueprint Medicines, BMS, Celgene, Eli Lilly, GSK, Ignyta, IPSEN, Merck KGaA, MSD, Nektar, Onxeo, Pfizer, Pharma Mar, Sanofi, Spectrum Pharmaceuticals, Takeda, Tiziana Pharma. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kalemkerian G.P., Narula N., Kennedy E.B., Biermann W.A., Donington J., Leighl N.B., Lew M., Pantelas J., Ramalingam S.S., Reck M., et al. Molecular Testing Guideline for the Selection of Patients With Lung Cancer for Treatment With Targeted Tyrosine Kinase Inhibitors: American Society of Clinical Oncology Endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology Clinical Practice Guideline Update. J. Clin. Oncol. 2018;36:911–919. doi: 10.1200/jco.2017.76.7293. [DOI] [PubMed] [Google Scholar]
- 2.Soria J.-C., Ohe Y., Vansteenkiste J., Reungwetwattana T., Chewaskulyong B., Lee K.H., Dechaphunkul A., Imamura F., Nogami N., Kurata T., et al. Osimertinib in UntreatedEGFR-Mutated Advanced Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018;378:113–125. doi: 10.1056/NEJMoa1713137. [DOI] [PubMed] [Google Scholar]
- 3.Verheijen R.B., Yu H., Schellens J.H., Beijnen J.H., Steeghs N., Huitema A.D. Practical Recommendations for Therapeutic Drug Monitoring of Kinase Inhibitors in Oncology. Clin. Pharmacol. Ther. 2017;102:765–776. doi: 10.1002/cpt.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu H., Steeghs N., Nijenhuis C.M., Schellens J.H.M., Beijnen J.H., Huitema A.D.R. Practical Guidelines for Therapeutic Drug Monitoring of Anticancer Tyrosine Kinase Inhibitors: Focus on the Pharmacokinetic Targets. Clin. Pharmacokinet. 2014;53:305–325. doi: 10.1007/s40262-014-0137-2. [DOI] [PubMed] [Google Scholar]
- 5.Groenland S.L., Mathijssen R.H.J., Beijnen J.H., Huitema A.D.R., Steeghs N. Individualized dosing of oral targeted therapies in oncology is crucial in the era of precision medicine. Eur. J. Clin. Pharmacol. 2019;75:1309–1318. doi: 10.1007/s00228-019-02704-2. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton M., Wolf J.L., Rusk J., Beard S.E., Clark G.M., Witt K., Cagnoni P.J. Effects of Smoking on the Pharmacokinetics of Erlotinib. Clin. Cancer Res. 2006;12:2166–2171. doi: 10.1158/1078-0432.CCR-05-2235. [DOI] [PubMed] [Google Scholar]
- 7.Van Leeuwen R.W.F., Van Gelder T., Mathijssen R.H.J., A Jansman F.G. Drug–drug interactions with tyrosine-kinase inhibitors: A clinical perspective. Lancet Oncol. 2014;15:e315–e326. doi: 10.1016/S1470-2045(13)70579-5. [DOI] [PubMed] [Google Scholar]
- 8.Mir O., Touati N., Lia M., Litière S., Le Cesne A., Sleijfer S., Blay J.-Y., Leahy M., Young R., Mathijssen R.H., et al. Impact of Concomitant Administration of Gastric Acid–Suppressive Agents and Pazopanib on Outcomes in Soft-Tissue Sarcoma Patients Treated within the EORTC 62043/62072 Trials. Clin. Cancer Res. 2019;25:1479–1485. doi: 10.1158/1078-0432.CCR-18-2748. [DOI] [PubMed] [Google Scholar]
- 9.Marin D., Bazeos A., Mahon F.-X., Eliasson L., Milojkovic D., Bua M., Apperley J.F., Szydlo R., Desai R., Kozlowski K., et al. Adherence Is the Critical Factor for Achieving Molecular Responses in Patients With Chronic Myeloid Leukemia Who Achieve Complete Cytogenetic Responses on Imatinib. J. Clin. Oncol. 2010;28:2381–2388. doi: 10.1200/JCO.2009.26.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arrondeau J., Mir O., Boudou-Rouquette P., Coriat R., Ropert S., Dumas G., Rodrigues M.J., Rousseau B., Blanchet B., Goldwasser F. Sorafenib exposure decreases over time in patients with hepatocellular carcinoma. Investig. New Drugs. 2011;30:2046–2049. doi: 10.1007/s10637-011-9764-8. [DOI] [PubMed] [Google Scholar]
- 11.Hiemke C., Bergemann N., Clement H.W., Conca A., Deckert J., Domschke K., Eckermann G., Egberts K., Gerlach M., Greiner C., et al. Consensus Guidelines for Therapeutic Drug Monitoring in Neuropsychopharmacology: Update 2017. Pharmacopsychiatry. 2018;51:9–62. doi: 10.1055/s-0043-116492. [DOI] [PubMed] [Google Scholar]
- 12.Rousselot P., Johnson-Ansah H., Huguet F., Legros L., Escoffre-Barbe M., Gardembas M., Cony-Makhoul P., Coiteux V., Sutton L., Abarah W., et al. Personalized Daily Doses of Imatinib By Therapeutic Drug Monitoring Increase the Rates of Molecular Responses in Patients with Chronic Myeloid Leukemia. Final Results of the Randomized OPTIM Imatinib Study. Blood. 2015;126:133. doi: 10.1182/blood.V126.23.133.133. [DOI] [Google Scholar]
- 13.Widmer N., Bardin C., Chatelut E., Paci A., Beijnen J., Levêque D., Veal G., Astier A. Review of therapeutic drug monitoring of anticancer drugs part two–Targeted therapies. Eur. J. Cancer. 2014;50:2020–2036. doi: 10.1016/j.ejca.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 14.Reis R., Labat L., Allard M., Boudou-Rouquette P., Chapron J., Bellesoeur A., Thomas-Schoemann A., Arrondeau J., Giraud F., Alexandre J., et al. Liquid chromatography-tandem mass spectrometric assay for therapeutic drug monitoring of the EGFR inhibitors afatinib, erlotinib and osimertinib, the ALK inhibitor crizotinib and the VEGFR inhibitor nintedanib in human plasma from non-small cell lung cancer patients. J. Pharm. Biomed. Anal. 2018;158:174–183. doi: 10.1016/j.jpba.2018.05.052. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y., Chia Y.L., Nedelman J., Schran H., Mahon F.-X., Molimard M. A Therapeutic Drug Monitoring Algorithm for Refining the Imatinib Trough Level Obtained at Different Sampling Times. Ther. Drug Monit. 2009;31:579–584. doi: 10.1097/FTD.0b013e3181b2c8cf. [DOI] [PubMed] [Google Scholar]
- 16.Lankheet N.A.G., Knapen L.M., Schellens J.H.M., Beijnen J.H., Steeghs N., Huitema A.D.R. Plasma Concentrations of Tyrosine Kinase Inhibitors Imatinib, Erlotinib, and Sunitinib in Routine Clinical Outpatient Cancer Care. Ther. Drug Monit. 2014;36:326–334. doi: 10.1097/FTD.0000000000000004. [DOI] [PubMed] [Google Scholar]
- 17.Van Leeuwen R.W.F., Jansman F.G.A., Hunfeld N.G., Peric R., Reyners A.K.L., Imholz A.L.T., Brouwers J.R.B.J., Aerts J.G., Van Gelder T., Mathijssen R.H.J. Tyrosine Kinase Inhibitors and Proton Pump Inhibitors: An Evaluation of Treatment Options. Clin. Pharmacokinet. 2017;56:683–688. doi: 10.1007/s40262-016-0503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pistilli B., Paci A., Ferreira A.R., Di Meglio A., Poinsignon V., Bardet A., Menvielle G., Dumas A., Pinto S., Dauchy S., et al. Serum Detection of Nonadherence to Adjuvant Tamoxifen and Breast Cancer Recurrence Risk. J. Clin. Oncol. 2020;38:2762–2772. doi: 10.1200/JCO.19.01758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gougis P., Palmieri L.-J., Funck-Brentano C., Paci A., Flippot R., Mir O., Coriat R. Major pitfalls of protein kinase inhibitors prescription: A review of their clinical pharmacology for daily use. Crit. Rev. Oncol. 2019;141:112–124. doi: 10.1016/j.critrevonc.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Yu H.A., Arcila M.E., Rekhtman N., Sima C.S., Zakowski M.F., Pao W., Kris M.G., Miller V.A., Ladanyi M., Riely G.J. Analysis of Tumor Specimens at the Time of Acquired Resistance to EGFR-TKI Therapy in 155 Patients with EGFR-Mutant Lung Cancers. Clin. Cancer Res. 2013;19:2240–2247. doi: 10.1158/1078-0432.CCR-12-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huillard O., Blanchet B., Boudou-Rouquette P., Thomas-Schoemann A., Wassermann J., Goldwasser F. Sorafenib in Thyroid Cancer Patients: Learning From Toxicity. Oncol. 2014;19:e3. doi: 10.1634/theoncologist.2014-0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doherty G.J., Lynskey D., Matakidou A., Fife K., Eisen T. Dose escalation of axitinib on disease progression as a strategy in the treatment of metastatic renal cell carcinoma. ESMO Open. 2018;3:e000445. doi: 10.1136/esmoopen-2018-000445. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.