Abstract
Primary hypertension (HTN) and obesity are associated with a worse health-related quality of life (QoL). This research was carried out to analyze the health-related QoL measurements in a physically inactive and obese population with HTN (n = 253) in comparison to a HEALTHY sample (n = 30), to determine the HTN sample changes in QoL following different (high-volume moderate-intensity continuous training, high-volume high-intensity interval training (HIIT), low-volume HIIT) 16-week supervised aerobic exercise training (ExT) programs compared to attention control, and to assess the differences in QoL variables between the different ExT programs. The SF-36 questionnaire was used to assess health-related QoL. At baseline, HTN showed lower scores (p < 0.05) in physical function (88.6 vs. 99.2), general health (63.3 vs. 82.4), vitality (58.2 vs. 68.7), social functioning (88.5 vs. 95.2), and mental health (76.1 vs. 81.8) compared to HEALTHY. Following intervention, all HTN subgroups showed higher (p < 0.05) vitality, but physical functioning and general health significantly improved only in the ExT groups, with even better values in general health for both HIIT subgroups. Only the low-volume HIIT showed positive changes (p < 0.05) in social functioning (∆ = 6.9%) and mental health (∆ = 6.4%) domains after the intervention. These results highlight the important role of supervised exercise in improving physical and psychological health.
Keywords: SF-36 questionnaire, supervised exercise, physical health, mental health, high-intensity interval training, low-volume training
1. Introduction
Primary hypertension (HTN), with an overall prevalence in adults around 30–45%, is recognized as a major risk factor for cardiovascular disease; chronic kidney disease; peripheral artery disease; and cognitive decline disease [1]. A previous systematic review and observational studies concluded that the quality of life (QoL) of individuals with HTN is worse than that of normotensive ones, with better values in the physically active population compared to sedentary ones [2,3,4]. Therefore, a non-pharmacological treatment of HTN is recommended, involving lifestyle interventions that might result in lower blood pressure (BP) and avoid the need for medication to improve the health status of this population [1,5].
Exercise training (ExT) contributes to the management of HTN, with health promotion, greater cardiorespiratory fitness, decreasing mortality and cardiovascular morbidity, and reduced BP values [6]. Experimental studies indicate that high-intensity interval training (HIIT) produces superior benefits than moderate-intensity continuous training (MICT) in cardiorespiratory fitness improvement, but similar enhanced control of BP [6,7]. Adding to that, the low-volume HIIT (i.e., ≤10 min of high-intensity effort in one exercise session) has emerged as a time-efficient and effective training method for improving health [7].
It is well known that regular physical activity improves health-related QoL contributing to perceived well-being [8], with greater improvements in interventions supervised by exercise specialists [9]. In a recent study, comparing the effects of HIIT and MICT in patients with fibromyalgia, both exercise groups showed significant and similar improvements for pain, functional capacity and QoL compared to the control group [10].
Many questionnaires have been developed to assess population health, but finding a generic questionnaire that is easy to administer, acceptable, valid, and short has been a difficult task. One of the most used questionnaires has been the Nottingham health profile due its acceptability and shortness [11]. However, it has been criticized for its inability to detect low levels of disability that are important not only clinically but also for respondents [12]. The 36-item short-form health survey questionnaire (SF-36) is not just a potentially valuable tool for medical research, it has also served to assess the QoL in different populations with diseases, such as fibromyalgia, knee osteoarthritis, and chronic low back pain [13], cancer [14], psoriasis [15], and chronic kidney disease [16]. On the other hand, in individuals with HTN, while the beneficial effects of MICT [17] and a walking program [18] on QoL assessed with the SF-36 have been confirmed, the relationship in response to HIIT programs, differing in volume, has not been examined in this population.
Therefore, the main purposes of this study were: (1) to compare the health-related QoL in physically inactive individuals with obesity/overweight and HTN with that of HEALTHY ones; (2) to determine changes in QoL following different (high-volume MICT, high-volume HIIT, low-volume HIIT) 16-week supervised aerobic ExT programs compared to attention control (AC) in inactive individuals with obesity/overweight and HTN; and (3) to analyze the possible differences in QoL variables between the different ExT programs.
2. Methods
2.1. Study Design
Data from the present study were taken from the EXERDIET-HTA research including two sub-studies: (1) a cross-sectional analyzing the health-related QoL measurements in physically inactive and obese population with HTN in comparison to a HEALTHY sample, and (2) a multi-arm parallel, randomized, single-blind controlled experimental trial comparing the effects of different 16-week aerobic ExT programs (performed 2 days/week) combined with dietary intervention in physically inactive, overweight/obese individuals with HTN (www.clinicaltrials.gov, number NCT02283047). The study protocol was approved by the ethics committee of the University of the Basque Country (UPV/EHU, CEISH/279/2014) and clinical investigation of Araba University Hospital (2015-030), and all participants provided written informed consent before any data collection. The medical staff was blinded to the participant randomization process. Examinations at baseline and follow-up were performed in the same laboratory setting and by the same researchers. The design, selection criteria, and procedures for the EXERDIET-HTA study have been detailed previously [19].
2.2. Participants
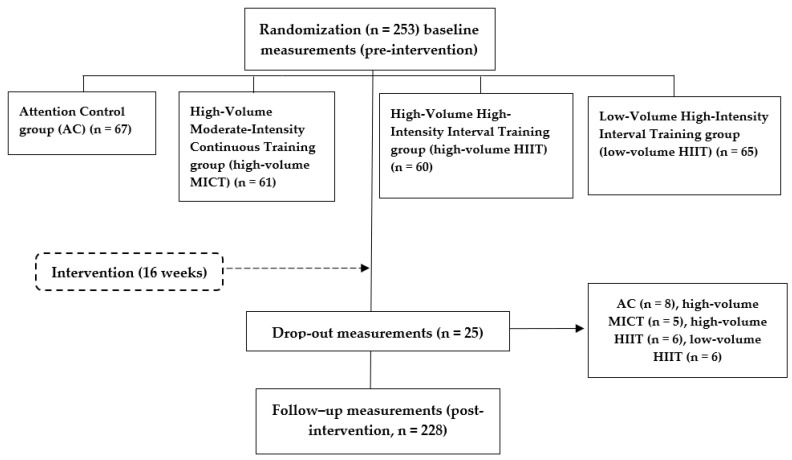
A flow chart of the participants in this study is shown in Figure 1. Participants were recruited from the medical services (cardiology) and local media (university media, newspapers, radio, and television). Interested individuals were invited to contact the research team. A sample of 253 individuals aged between 24 and 69 years (53.7 ± 7.9 years) took part in the study, 161 men and 92 women. All participants were physically inactive (i.e., they were below the Global Recommendations of Physical Activity for health set by the World Health Organization) [20], overweight/obese (i.e., body mass index ≥25 kg/m2 or 30 kg/m2, respectively), and had the diagnosis of HTN (i.e., mean systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg or under antihypertensive pharmacological treatment) [21]. Participants with no diagnosis of HTN were assessed with ambulatory BP monitoring (ABPM) to confirm the HTN status by a cardiologist. All other inclusion and exclusion criteria were specified in the study protocol [19]. Data were retained from those participants who had measurements in anthropometry, ABPM, and cardiorespiratory fitness using the metabolic gas analysis system.
Figure 1.
Flow diagram of the EXERDIET-HTA study from recruitment to the follow-up measurements post intervention.
In addition to the EXERDIET-HTA study participants, another group was created to allow for comparison to a healthy control population (HEALTHY, n = 30, 40.0 ± 9.0 years), who did not receive any type of intervention. Only baseline measurements were assessed for comparison to the EXERDIET-HTA study participants. HEALTHY participants were recruited from the community through university media. Inclusion for HEALTHY criteria was to be 25–55 years of age and exclusion criteria were being pregnant, currently breastfeeding, taking regular medication, or having any known medical conditions, had abnormal findings on physical examination (including blood pressure ≥140/90 mmHg, or overweight ≥25 kg/m2), or had abnormal results on screening test (rest and exercise electrocardiogram).
2.3. Measurements
A full description of the study protocol was previously presented elsewhere [19]. A brief explanation of the main measures is presented below.
Anthropometry measurements for the assessment of body composition included stature (SECA 213, Hamburg, Germany), total body mass, and body mass index (BMI) (Tanita, BF 350, Arlington Heights, IL, USA), and waist circumferences (SECA 200, Hamburg, Germany).
Ambulatory BP monitoring was measured with an oscillometric ABPM (6100 and 7100 recorders, Welch Allyn, New York, NY, USA). The device measured BP an entire day, at 30-min intervals during the daytime, and at 60-min intervals during nighttime. The variables registered from the ABPM were mean values of systolic BP and diastolic BP during the day and night periods.
Physical fitness was determined by performing a symptom-limited cardiopulmonary exercise test on an electronically braked Lode Excalibur Sport cycle ergometer (Groningen, The Netherlands). The test started at 40 W with a gradual increment of 10 W every minute applied until volitional exhaustion. The expired gas was analyzed using a commercially available metabolic cart (Ergo Card, Medi-soft S.S, Belgium Ref. USM001 V1.0). Achievement of peak oxygen uptake criteria has previously been defined [22] and was assumed with the presence of two or more of the following criteria: volitional fatigue (>18 on Borg Scale), peak respiratory exchange ratio ≥1.1, achieving >85% of age-predicted maximum heart rate, and failure of oxygen uptake and/or heart rate to increase with further increases in work rate. Absolute and relative indications for terminating the exercise test were taken into account [23].
The health-related QoL was assessed using the Spanish version of the SF-36 questionnaire [24]. The items of the questionnaire report both positive and negative states of “physical component summary” and “mental component summary”, identifying eight dimensions of health: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. For each dimension of the SF-36, the items are coded, added, and transformed into a scale with a path from 0 to 100 (higher scores indicating higher levels of health-related QoL) using the algorithms and indications that the scoring and interpretation manual of the questionnaire offers [25]. Psychometric evaluation of instruments targeting two independent constructs of physical and mental health has been recently published and validated [26]. Once the SF-36 questionnaire was explained, each participant answered it on their own.
2.4. Intervention
After baseline measurements, EXERDIET-HTA participants were randomly allocated into one of the four intervention subgroups stratified by sex, systolic BP, BMI, and age using a time-blocked computerized randomization program. The medical staff was blinded to participant randomization assignment. The four intervention subgroups were: three supervised ExT groups (i.e., high-volume MICT, high-volume HIIT, low-volume HIIT) on two non-consecutive days per week under supervision by exercise specialists for 16 weeks; and one attention AC, with only physical activity advice participating in at least 30 min of moderate-intensity aerobic exercise (walking, jogging, cycling, or swimming) for 5–7 days per week blended with some dynamic resistance exercises [19]. The high-volume MICT group performed 45 min of aerobic continuous exercise at moderate intensity, whereas the high- and low-volume HIIT groups performed 45 and 20 min, respectively. In the HIIT groups, they alternated high- and moderate-intensities performing protocols previously published [19]. All participants underwent a hypocaloric DASH diet. The diet was designed to provide 25% less energy than their daily energy expenditure and to achieve a weekly loss in body mass of between 0.5 and 1.0 kg in accordance with the recommendations of the American Diabetes Association and the Spanish Society for the Study of Obesity [27]. The diet contained approximately 30% fat, 15% protein, and 55% carbohydrates and was designed following the DASH diet. To ensure participant compliance with the DASH diet every two weeks participants were weighed and received encouragement and advice alongside nutritional counseling to aid compliance [7].
2.5. Statistical Analysis
The values of each variable were obtained considering the mean and standard deviation (SD). Data were considered for the entire sample and presented in groups. Analysis of variance (ANOVA) was used to determine if there were significant pre-intervention differences between groups. In contrast, the differences between pre-intervention (T0) and post-intervention (T1) were analyzed using a Student-t test related to the sample in each variable. Analysis of covariance (ANCOVA) was used to examine the delta (∆) score for each group (AC, high-volume MICT, high-volume HIIT, low-volume HIIT) and Bonferroni correction was used to determine the level of significance when a significant main effect was found. Furthermore, the differences between AC vs. ExT were analyzed using the Helmert contrast. Data were analyzed according to the intention-to-treat principle. Statistical significance was set at p < 0.05. The statistical analyses were performed with the SPSS version 25.0 software package. The power calculation was completed using the G*Power 3 analysis program [28]. The required sample size was determined for the primary outcome variable (systolic BP) of the EXERDIET-HTA study. It was identified that adequate power (0.80) to evaluate differences in the current design consisting of four experimental groups would be achieved with 164 people (41 each group, α = 0.05, effect size f = 0.27) based on the pilot study with an SD of 9 mmHg.
3. Results
At baseline, answering the first goal of the study (a cross-sectional analysis), significant differences were presented in participants’ characteristics between the two samples (i.e., HEALTHY vs. EXERDIET-HTA) (Table 1). Thus, whereas HEALTHY were classified as normal body composition and BP values, as well as good cardiorespiratory fitness, EXERDIET-HTA individuals showed obesity values in addition to low cardiorespiratory fitness. These results have been previously presented and further explained [29]. In contrast, analyzing the domains of health-related QoL, EXERDIET-HTA participants showed lower scores in physical function (88.6 vs. 99.2, p < 0.001), general health (63.3 vs. 82.4, p < 0.001), vitality (58.2 vs. 68.7, p < 0.001), social functioning (88.5 vs. 95.2, p = 0.002), and mental health (76.1 vs. 81.8, p = 0.001) in comparison with the HEALTHY population (Table 1). Adding to that, the physical and mental component summaries were also lower (50.3 vs. 54.9, p < 0.001, 50.9 vs. 53.1, p = 0.036, respectively) in the EXERDIET-HTA compared to the HEALTHY group. Further, there were no significant differences between EXERDIET-HTA subgroups (p > 0.05).
Table 1.
Characteristics of the studied population and scores for eight variables of SF36 by group and subgroups at baseline.
| EXERDIET-HTA SUBGROUPS | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | HEALTHY (n = 30) |
EXERDIET-HTA (n = 253) |
p HEALTHY vs. EXERDIET-HTA | AC (n = 67) |
High-Volume MICT (n = 61) |
High-Volume HIIT (n = 60) |
Low-Volume HIIT (n = 65) |
p Value Subgroups |
| Sex (men/women) | 12/18 | 161/92 | <0.001 | 41/26 | 38/23 | 39/21 | 43/22 | 0.934 |
| Age (yrs) | 40.0 ± 9.0 | 53.7 ± 7.9 | <0.001 | 52.7 ± 8.4 | 54.2 ± 7.2 | 53.0 ± 8.6 | 54.7 ± 7.2 | 0.339 |
| Body mass (kg) | 66.1 ± 10.5 | 91.5 ± 15.2 | <0.001 | 91.3 ± 15.2 | 92.5 ± 16.8 | 90.1 ± 15.1 | 91.3 ± 14.0 | 0.826 |
| BMI (kg/m2) | 23.1 ± 2.6 | 32.1 ± 4.2 | <0.001 | 32.3 ± 4.4 | 32.3 ± 4.4 | 31.7 ± 3.7 | 32.0 ± 4.3 | 0.799 |
| Waist (cm) | 74.7 ± 8.1 | 103.2 ± 11.2 | <0.001 | 103.3 ± 11.1 | 104.1 ± 12.8 | 101.8± 11.0 | 103.1 ± 10,1 | 0.667 |
| SBP (mmHg) | 114.0 ± 6.6 | 135.8 ± 12.1 | <0.001 | 138.2 ± 13.4 | 133.9 ± 11.1 | 134.3 ± 10.0 | 136.5 ± 13.2 | 0.167 |
| DBP (mmHg) | 68.1 ± 7.2 | 78.0 ± 8.1 | <0.001 | 79.0 ± 8.3 | 75.8 ± 8.1 | 78.9 ± 7.6 | 78.5 ± 8.5 | 0.077 |
| V̇O2peak (mL·kg−1·min−1) | 48.1 ± 8.1 | 22.6 ± 5.5 | <0.001 | 23.3 ± 6.3 | 21.8 ± 5.2 | 22.7 ± 4.9 | 22.6 ± 5.5 | 0.451 |
| Physical Functioning | 99.2 ± 2.3 | 88.6 ± 12.2 | <0.001 | 89.2 ± 11.8 | 88.6 ± 12.5 | 89.3 ± 11.2 | 87.2 ± 13.3 | 0.757 |
| Role-Physical | 96.0 ± 18.4 | 90.8 ± 25.0 | 0.165 | 92.5 ± 21.8 | 86.5 ± 28.7 | 94.6 ± 21.6 | 89.6 ± 27.2 | 0.228 |
| Bodily Pain | 81.3 ± 11.2 | 78.2 ± 19.7 | 0.189 | 75.3 ± 19.2 | 78.5 ± 18.7 | 80.9 ± 18.5 | 78.4 ± 22.3 | 0.482 |
| General Health | 82.4 ± 13.0 | 63.3 ± 16.6 | <0.001 | 65.0 ± 18.1 | 63.9 ± 15.2 | 62.4 ± 15.1 | 62.1 ± 17.9 | 0.735 |
| Vitality | 68.7 ± 9.9 | 58.2 ± 15.0 | <0.001 | 58.1 ± 15.6 | 57.6 ± 14.8 | 60.1 ± 14.4 | 56.9± 15.2 | 0.704 |
| Social Functioning | 95.2 ± 10.0 | 88.5 ± 17.2 | 0.002 | 88.8 ± 17.3 | 87.9 ± 16.8 | 89.0 ± 17.1 | 88.3 ± 17.8 | 0.991 |
| Role-Emotional | 91.4 ± 21.0 | 89.5 ± 27.4 | 0.704 | 92.0 ± 24.7 | 85.8 ± 30.7 | 91.7 ± 24.3 | 88.2 ± 29.7 | 0.576 |
| Mental Health | 81.8 ± 7.3 | 76.1 ± 14.2 | <0.001 | 75.0 ± 14.1 | 78.2 ± 12.9 | 76.1 ± 15 | 75.5 ± 14.7 | 0.592 |
| Physical Component Summary | 54.9 ± 4.2 | 50.3 ± 6.6 | <0.001 | 50.4 ± 6.2 | 50.0 ± 7.1 | 51.0 ± 5.8 | 50.0 ± 7.3 | 0.698 |
| Mental Component Summary | 53.1 ± 5.0 | 50.9 ± 8.3 | 0.036 | 50.9± 7.6 | 50.9 ± 8.7 | 51.1 ± 8.5 | 50.5 ± 8.8 | 0.970 |
Values are mean ± standard deviation or number. HEALTHY: healthy control; AC: attention control group; MICT: moderate-intensity continuous training group; HIIT: high-intensity interval training group; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; V̇O2peak: peak oxygen uptake. p < 0.05.
Following 16 weeks of intervention, answering the second and third goals of the study (controlled experimental trial), positive changes (T0 vs. T1, p < 0.05) were observed in the total EXERDIET-HTA sample in some of the domains of the SF-36 questionnaire (Table 2), such as physical functioning (difference %, ∆ = 4.9%), general health (∆ = 10.8%), vitality (∆ = 12%), social functioning (∆ = 4.4%), and mental health (∆ = 3.5%). Vitality was the unique domain improving with higher (p < 0.05) values in each of the four groups. Further, physical functioning (p = 0.011), and general health (p = 0.001) differed when AC vs. ExT subgroups were compared, with higher values in ExT groups (“Physical functioning”: high-volume MICT, mean difference 4.189, 95% confidence interval (CI) −1.184–9.563; high-volume HIIT, mean difference 5.169, 95% CI −0.109–10.448; low-volume HIIT, mean difference 3.007, 95% CI −2.366–8.382. “General health”: high-volume MICT, mean difference 5.319, 95% CI −2.531–13.171; high-volume HIIT, mean difference 9.237, 95% CI 1.525–16.949; low-volume HIIT, mean difference 9.829, 95% CI 1.977–17.680). Further, a favorable effect of the intervention was also observed in “general health” in high-volume HIIT (p < 0.001, mean difference -10.135, 95% CI −14.801 + 5.470), and low-volume HIIT (p < 0.001, mean difference −6.218, 95% CI −10.261 + 2.174) vs. AC, with higher values in both ExT subgroups. Likewise, the “vitality” domain in low-volume HIIT showed higher (p = 0.043) values than AC. Interestingly, after intervention positive differences (p < 0.05) in “social functioning” (∆ = 6.9%) and “mental health” (∆ = 6.4%) domains were only found in the low-volume HIIT subgroup, leading consequently to higher (∆ = 6.3%, p < 0.05) “mental component summary” (Table 2).
Table 2.
Health-related Quality of Life outcomes before and after a 16-week intervention program in the EXERDIET-HTA group.
| Variables | ALL (n = 253) |
AC (n = 67) |
High-Volume MICT (n = 61) |
High-Volume HIIT (n = 60) |
Low-VolumeHIIT (n = 65) |
p AC vs. ExT |
p Value Intergroups |
|---|---|---|---|---|---|---|---|
| Physical Functioning | |||||||
| T0 | 88.9 ± 11.8 | 90.0 ± 10.3 | 88.5 ± 12.6 | 90.0 ± 10.8 | 87.3 ± 13.5 | 0.011 | 0.057 |
| T1 | 93.3 ± 7.9 *× | 91.4 ± 9.9 | 94.1 ± 6.9 * | 94.4 ± 7.5 * | 93.8 ± 6.6 * | ||
| Role-Physical | |||||||
| T0 | 91.8 ± 23.2 | 93.6 ± 20.5 | 89.1 ± 25.8 | 95.4 ± 18.1 | 90.2 ± 25.8 | 0.145 | 0.292 |
| T1 | 93.6 ± 22.2 | 90.2 ± 28.6 | 95.0 ± 18.2 | 94.5 ± 17.8 | 94.5 ± 22.3 | ||
| Bodily Pain | |||||||
| T0 | 78.8 ± 19.1 | 75.4 ± 19.8 | 79.2 ± 17.9 | 82.4 ± 16.4 | 77.8 ± 21.4 | 0.984 | 0.312 |
| T1 | 81.4 ± 20.1 | 78.1 ± 23.5 | 85.5 ± 19.9 | 79.8 ± 19.2 | 82.2 ± 18.4 | ||
| General Health | |||||||
| T0 | 64.1 ± 16.6 | 65.9 ± 18.3 | 64.4 ± 15.1 | 63.5 ± 14.7 | 62.4 ± 17.9 | 0.001 | 0.003 |
| T1 | 71.0 ±17.1 *× | 66.8 ± 21.3 | 70.6 ± 14.6 * | 74.3 ± 15.5 *× | 72.5 ± 15.5 *× | ||
| Vitality | |||||||
| T0 | 59.0 ± 14.9 | 58.5 ± 15.8 | 57.9 ± 15.1 | 61.8 ± 13.5 | 58.0 ± 15.2 | 0.101 | 0.043 |
| T1 | 66.2 ± 13.8 *× | 63.0 ± 15.9 * | 66.3 ± 13.4 * | 66.5 ± 13.5 * | 69.1 ± 11.8 * | ||
| Social Functioning | |||||||
| T0 | 88.9 ± 17.0 | 89.2 ± 17.0 | 88.6 ± 16.7 | 90.0 ± 16.4 | 87.7 ± 18.0 | 0.951 | 0.769 |
| T1 | 92.8 ± 14.6 * | 93.0 ± 13.2 | 91.8 ± 19.6 | 92.5 ± 11.7 | 93.8 ± 13.2 * | ||
| Role-Emotional | |||||||
| T0 | 90.5 ± 26.7 | 93.2 ± 23.8 | 87.3 ± 29.0 | 93.3 ± 23.5 | 88.1 ± 30.2 | 0.100 | 0.157 |
| T1 | 92.0 ± 23.5 | 89.8 ± 26.4 | 92.7 ± 21.9 | 92.1 ± 24.0 | 94.9 ± 18.4 | ||
| Mental Health | |||||||
| T0 | 76.8 ± 14.1 | 76.1 ± 13.7 | 78.6 ± 13.3 | 76.6 ± 15.4 | 76.0 ± 14.2 | 0.287 | 0.509 |
| T1 | 79.5 ± 12.9 * | 77.1 ± 13.5 | 81.3 ± 12.7 | 78.8 ± 14.1 | 80.9 ± 11.3 * | ||
| Physical Component Summary | |||||||
| T0 | 50.6 ± 6.4 | 50.6 ± 6.1 | 50.3 ± 6.8 | 51.4 ± 5.5 | 50.0 ± 7.2 | 0.098 | 0.309 |
| T1 | 52.3 ± 6.1 | 51.1 ± 7.4 | 52.9 ± 5.6* | 53.0 ±5.0 | 52.6 ± 5.8 * | ||
| Mental Component Summary | |||||||
| T0 | 51.2 ± 8.3 | 51.3 ± 7.4 | 51.2 ± 8.8 | 51.6 ± 8.5 | 50.7 ± 8.7 | 0.329 | 0.396 |
| T1 | 52.8 ± 7.3 | 52.0 ± 8.2 | 53.0 ± 8.1 | 52.5 ± 7.2 | 53.9 ± 5.3 * |
Values are mean ± SD. AC: attention control group; MICT: moderate-intensity continuous training group; HIIT: high-intensity interval training group; ExT: Exercise Training Groups; T0: pre intervention; T1: post-intervention. * p-value < 0.05 from T0; *× p-value < 0.001 from T0.
4. Discussion
This research was carried out to analyze the health-related QoL measures in a physically inactive and obese population with HTN in comparison to a HEALTHY sample, and to determine the effects, after a 16-week ExT intervention period, on the hypertensive and physically inactive sample with obesity both as a whole and also on each of the subgroups of the study. The main findings of the present study were: (1) the HEALTHY group showed higher scores in physical function, general health, vitality, social functioning, and mental health in comparison with the HTN participants; (2) after a 16-week intervention period “vitality” showed higher values in all HTN groups; (3) “physical functioning” and “general health” scores improved more in the supervised ExT groups compared with the AC, with better values in general health in both HIIT groups; and (4) only the low-volume HIIT subgroup showed positive changes in “social functioning” and “mental health” domains after the intervention.
As one might expect, the scores of health-related QoL in HEALTHY individuals were higher (better) than those of participants with HTN, obesity, and physical inactivity. These results coincide with those by previous studies with a significant impact of chronic conditions [30] and HTN [3] on physical and mental health, and consequently the added burden associated with comorbidity. Thus, according to the SF-36 Health Survey [25], EXERDIET-HTA participants were represented in the low-medium range (i.e., 25–50th percentile) related to general health, vitality, and mental health, with a general medium-high perception of physical component summary (50–75th percentile), and low-medium perception of mental component summary (25–50th percentile).
European guidelines for the management of arterial HTN [1] claim that healthy lifestyle choices, including a healthy diet and physical activity, can prevent or delay the onset of HTN and reduce cardiovascular risk. In the present study, the 16-week intervention program showed the benefits of health-related QoL in some domains, such as “vitality” in all groups, reinforcing the power of a healthy lifestyle to make you feel strong, active, and energized. Therefore, the potential mechanism of physical activity for improving cognitive processes, antidepressant effects, and even inducing a sense of well-being has been previously discussed [31]. At a physiological level, acute exercise appears to improve mood by activating specific cortical areas and inducing the release of neurotransmitters (i.e., serotonin, dopamine, or norepinephrine) and trophic factors that contribute to adherence to a regular physical activity program by increasing the feeling of well-being and also inhibiting the nerve fibers that transmit pain [32].
Moreover, the supervised ExT groups did demonstrate greater improvements in the physical area (physical functioning and general health) compared to AC. These results are concomitant with the improvements in body composition, cardiorespiratory fitness, BP, and cardiovascular risk previously published in the studied sample [7,33]. This is the effect of multiple physiological adaptations that translate into a better physical functioning with fewer limitations in performing all types of physical activities and increase personal evaluation in general health [25]. It is well recognized that good cardiorespiratory fitness has become a key vital sign, accepting the role of exercise in cardiovascular medicine and the molecular mechanisms underlying the benefits of exercise [34]. Further, a growing body of evidence suggests that exercise involving HIIT induces larger benefits and is more effective for improving cardiovascular and metabolic health compared to MICT [35]. In the present study, this favorable effect is also presented in the “general health” item, when both HIIT groups showed higher positive values compared to the AC group, showing the safety and efficacy of this exercise design also in physically inactive people with obesity and HTN. Likewise, it was important to observe that supervised ExT programs by exercise specialists, as in previous studies [9,18,36] had better results compared to only physical activity advice reporting a positive relationship with health-related QoL. These results reinforce the general guidelines and put aside the idea of “one size fits all” recommending an exercise program designed in a systematic and individualized manner in terms of the frequency, intensity, time, and type (i.e., FITT principle) [37]. Additionally, it has also been observed that group interventions favor the development of bonds among individuals through the exchange of experiences and feelings during these activities, improving the individual’s well-being and mental health [38]. Likewise, participation in regular group classes seems to lead to a significant decrease in perceived stress and an increase in physical, mental, and emotional QoL [39].
After analyzing the health-related mental domain, the low-volume HIIT program was the only group improving the “social functioning” (↑6.9%) and “mental health” (↑6.4%) items at follow-up. Recent investigation has shown very good results in individuals with severe obesity after performing a low-volume HIIT program for 12 weeks inducing significant improvements in QoL [40]. Thus, low-volume HIIT programs are emerging as a high level of acceptance, as long as feasible, time-efficient, effective, and enjoyable exercise programs in overweight/obese and inactive populations [41]. The aforementioned results underpin the final improvement of the mental component summary in the present study as a demonstration of the efficacy of low-volume HIIT.
The current study has several strengths, including a relatively large (n = 253), carefully screened, well-characterized group of non-physically active adults with obesity and HTN. There are, however, some limitations of this study that should be considered. First, the current study had only 36.4% of women, which does not represent a division by equal sex. In addition, the perspective between the sexes could be different when highlighting the questionnaire, since women usually present lower values in all multi-items compared to men [25]. As this raises statistical problems, future studies, particularly those using interventions and questionnaires, should seek to recruit equal numbers. Second, as the SF-36 is a subjective questionnaire, it is difficult to assess all its results accurately. Furthermore, future studies with a larger sample should seek to determine whether the different training programs have greater benefits in the different sections.
5. Conclusions
Physically inactive adults with obesity and HTN showed a worse health-related QoL profile compared to a HEALTHY population. A 16-week supervised aerobic ExT and nutritional intervention program for hypertensive individuals with obesity and physically inactive was effective in increasing vitality, with better scores in the physical area in the supervised ExT groups compared to AC. Low-volume HIIT may induce more relevant positive effects on social functioning and mental health compared to high-volume programs. These results highlight the important role of supervised exercise in improving physical and psychological health.
Acknowledgments
Our special thanks to Javier Pérez-Asenjo and G. Rodrigo Aispuru, the medical doctors performing the medical assessments in this project. Thanks to the Department of Physical Education and Sport; and to the Faculty of Education and Sport (Physical Activity and Sport Sciences Section) of the University of the Basque Country (UPV/EHU) for believing in our project and providing the materials and facilities to carry it out. Also, thanks to Exercycle S.L. (BH Fitness Company) for the machines donated to conduct the exercise intervention. Last but not least to all the participants for their willingness which made this project possible, and all undergraduate and postgraduate students who collaborated in this project (2011–2018 academic years).
Author Contributions
Conception and design of the experiment: M.T.-E., I.G.-A., P.C., and S.M.-M. Data collection and analysis: M.T.-E., I.G.-A., P.C., A.M.-B., and S.M.-M. Data interpretation and drafting of the manuscript: M.T.-E., I.G.-A., P.C., A.M.-B., and S.M.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the University of the Basque Country (EHU14/08, PPGA18/15). MTE was supported by the University of the Basque Country (UPV/EHU). IGA, PC, and AMAB were supported by the Basque Government with predoctoral grants.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Williams B., Mancia G., Spiering W., Rosei E.A., Azizi M., Burnier M., Clement D.L., Coca A., de Simone G., Dominiczak A., et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Kardiol. Pol. 2019;77:71–159. doi: 10.5603/KP.2019.0018. [DOI] [PubMed] [Google Scholar]
- 2.Trevisol D.J., Moreira L.B., Fuchs F.D., Fuchs S.C. Health-Related Quality of Life is Worse in Individuals with Hypertension Under Drug Treatment: Results of Population-Based Study. J. Hum. Hypertens. 2012;26:374–380. doi: 10.1038/jhh.2011.48. [DOI] [PubMed] [Google Scholar]
- 3.Kitaoka M., Mitoma J., Asakura H., Anyenda O.E., Nguyen T.T., Hamagishi T., Hori D., Suzuki F., Shibata A., Horii M., et al. The Relationship between Hypertension and Health-Related Quality of Life: Adjusted by Chronic Pain, Chronic Diseases, and Life Habits in the General Middle-Aged Population in Japan. Environ. Health Prev. Med. 2016;21:193–214. doi: 10.1007/s12199-016-0514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pariente Rodrigo E., Garcia-Garrido A.B., Lara Torres M., Garcia Martinez A., Montes Perez M., Andino Lopez J., Otero Cabanillas N., Ramos Barron M.C. Health-Related Quality of Life in Hypertension: A Gender-Differentiated Analysis in Population of Cantabria. Rev. Esp. Salud Publica. 2020;94:e202010139. [PMC free article] [PubMed] [Google Scholar]
- 5.Cuspidi C., Tadic M., Grassi G., Mancia G. Treatment of Hypertension: The ESH/ESC Guidelines Recommendations. Pharmacol. Res. 2018;128:315–321. doi: 10.1016/j.phrs.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Leal J.M., Galliano L.M., Del Vecchio F.B. Effectiveness of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training in Hypertensive Patients: A Systematic Review and Meta-Analysis. Curr. Hypertens. Rep. 2020;22:26. doi: 10.1007/s11906-020-1030-z. [DOI] [PubMed] [Google Scholar]
- 7.Gorostegi-Anduaga I., Corres P., MartinezAguirre-Betolaza A., Perez-Asenjo J., Aispuru G.R., Fryer S.M., Maldonado-Martin S. Effects of Different Aerobic Exercise Programmes with Nutritional Intervention in Sedentary Adults with Overweight/Obesity and Hypertension: EXERDIET-HTA Study. Eur. J. Prev. Cardiol. 2018;25:343–353. doi: 10.1177/2047487317749956. [DOI] [PubMed] [Google Scholar]
- 8.Vagetti G.C., Barbosa Filho V.C., Moreira N.B., Oliveira V., Mazzardo O., Campos W. Association between Physical Activity and Quality of Life in the Elderly: A Systematic Review, 2000–2012. Braz. J. Psychiatry. 2014;36:76–88. doi: 10.1590/1516-4446-2012-0895. [DOI] [PubMed] [Google Scholar]
- 9.Dechamps A., Diolez P., Thiaudiere E., Tulon A., Onifade C., Vuong T., Helmer C., Bourdel-Marchasson I. Effects of Exercise Programs to Prevent Decline in Health-Related Quality of Life in Highly Deconditioned Institutionalized Elderly Persons: A Randomized Controlled Trial. Arch. Intern. Med. 2010;170:162–169. doi: 10.1001/archinternmed.2009.489. [DOI] [PubMed] [Google Scholar]
- 10.Atan T., Karavelioglu Y. Effectiveness of High-Intensity Interval Training Vs Moderate-Intensity Continuous Training in Patients with Fibromyalgia: A Pilot Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020;101:1865–1876. doi: 10.1016/j.apmr.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 11.Hunt S.M., McEwen J., McKenna S.P. Measuring Health Status: A New Tool for Clinicians and Epidemiologists. J. R. Coll. Gen. Pract. 1985;35:185–188. [PMC free article] [PubMed] [Google Scholar]
- 12.Kind P., Carr-Hill R. The Nottingham Health Profile: A Useful Tool for Epidemiologists? Soc. Sci. Med. 1987;25:905–910. doi: 10.1016/0277-9536(87)90260-7. [DOI] [PubMed] [Google Scholar]
- 13.De Oliveira Paes Leme M., Yuan S.L.K., Oliveira Magalhaes M., Ferreira de Meneses S.R., Marques A.P. Pain and Quality of Life in Knee Osteoarthritis, Chronic Low Back Pain and Fibromyalgia: A Comparative Cross-Sectional Study. Reumatismo. 2019;71:68–74. doi: 10.4081/reumatismo.2019.1104. [DOI] [PubMed] [Google Scholar]
- 14.George S.M., Alfano C.M., Groves J., Karabulut Z., Haman K.L., Murphy B.A., Matthews C.E. Objectively Measured Sedentary Time is Related to Quality of Life among Cancer Survivors. PLoS ONE. 2014;9:e87937. doi: 10.1371/journal.pone.0087937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanchez-Carazo J.L., Lopez-Estebaranz J.L., Guisado C. Comorbidities and Health-Related Quality of Life in Spanish Patients with Moderate to Severe Psoriasis: A Cross-Sectional Study (Arizona Study) J. Dermatol. 2014;41:673–678. doi: 10.1111/1346-8138.12465. [DOI] [PubMed] [Google Scholar]
- 16.Rebollo-Rubio A., Morales-Asencio J.M., Pons-Raventos M.E., Mansilla-Francisco J.J. Review of Studies on Health Related Quality of Life in Patients with Advanced Chronic Kidney Disease in Spain. Nefrologia. 2015;35:92–109. doi: 10.3265/Nefrologia.pre2014.Jul.12133. [DOI] [PubMed] [Google Scholar]
- 17.Tsai J.C., Yang H.Y., Wang W.H., Hsieh M.H., Chen P.T., Kao C.C., Kao P.F., Wang C.H., Chan P. The Beneficial Effect of Regular Endurance Exercise Training on Blood Pressure and Quality of Life in Patients with Hypertension. Clin. Exp. Hypertens. 2004;26:255–265. doi: 10.1081/CEH-120030234. [DOI] [PubMed] [Google Scholar]
- 18.Arija V., Villalobos F., Pedret R., Vinuesa A., Jovani D., Pascual G., Basora J. Physical Activity, Cardiovascular Health, Quality of Life and Blood Pressure Control in Hypertensive Subjects: Randomized Clinical Trial. Health Qual. Life Outcomes. 2018;16:184. doi: 10.1186/s12955-018-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maldonado-Martín S., Gorostegi-Anduaga I., Aispuru R., Illera-Villas M., Jurio-Iriarte B., Francisco-Terreros S., Pérez-Asenjo J. Effects of Different Aerobic Exercise Programs with Nutritional Intervention in Primary Hypertensive and Overweight/Obese Adults: EXERDIET-HTA Controlled Trial. J. Clin. Trials. 2016;6:1–10. doi: 10.4172/2167-0870.1000252. [DOI] [Google Scholar]
- 20.Bull F.C., Al-Ansari S.S., Biddle S., Borodulin K., Buman M.P., Cardon G., Carty C., Chaput J.P., Chastin S., Chou R., et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mancia G., Fagard R., Narkiewicz K., Redon J., Zanchetti A., Bohm M., Christiaens T., Cifkova R., De Backer G., Dominiczak A., et al. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J. Hypertens. 2013;31:1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 22.Mezzani A., Hamm L.F., Jones A.M., McBride P.E., Moholdt T., Stone J.A., Urhausen A., Williams M.A., European Association for Cardiovascular Prevention and Rehabilitation. American Association of Cardiovascular and Pulmonary Rehabilitation et al. Aerobic Exercise Intensity Assessment and Prescription in Cardiac Rehabilitation: A Joint Position Statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the Canadian Association of Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2012;32:327–350. doi: 10.1097/HCR.0b013e3182757050. [DOI] [PubMed] [Google Scholar]
- 23.Task Force of the Italian Working Group on Cardiac Rehabilitation Prevention. Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology. Piepoli M.F., Corra U., Agostoni P.G., Belardinelli R., Cohen-Solal A., Hambrecht R., Vanhees L. Statement on Cardiopulmonary Exercise Testing in Chronic Heart Failure due to Left Ventricular Dysfunction: Recommendations for Performance and Interpretation. Part I: Definition of Cardiopulmonary Exercise Testing Parameters for Appropriate use in Chronic Heart Failure. Eur. J. Cardiovasc. Prev. Rehabil. 2006;13:150–164. doi: 10.1097/01.hjr.0000209812.05573.04. [DOI] [PubMed] [Google Scholar]
- 24.Alonso J., Prieto L., Antó J. La Versión Española Del SF-36 Health Survey (Cuestionario De Salud SF-36): Un Instrumento Para La Medida De Los Resultados Clínicos. Med. Clin. 1995;104:771–776. [PubMed] [Google Scholar]
- 25.Ware J.E., Snow K., Kosinski M., Gandek B. SF-36 Health Survey. Manual and Interpretation Guide. The Health Institute, New England Medical Center; Boston, MA, USA: 1993. [Google Scholar]
- 26.LoMartire R., Ang B.O., Gerdle B., Vixner L. Psychometric Properties of Short Form-36 Health Survey, EuroQol 5-Dimensions, and Hospital Anxiety and Depression Scale in Patients with Chronic Pain. Pain. 2020;161:83–95. doi: 10.1097/j.pain.0000000000001700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gargallo Fernandez M., Quiles Izquierdo J., Basulto Marset J., Breton Lesmes I., Formiguera Sala X., Salas-Salvado J., FESNAD-SEEDO Consensus Group Evidence-Based Nutritional Recommendations for the Prevention and Treatment of Overweight and Obesity in Adults (FESNAD-SEEDO Consensus Document). the Role of Diet in Obesity Prevention (II/III) Nutr. Hosp. 2012;27:800–832. doi: 10.3305/nh.2012.27.3.5679. [DOI] [PubMed] [Google Scholar]
- 28.Faul F., Erdfelder E., Lang A.G., Buchner A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 29.Corres P., Fryer S.M., Aguirre-Betolaza A.M., Gorostegi-Anduaga I., Arratibel-Imaz I., Perez-Asenjo J., Francisco-Terreros S., Saracho R., Maldonado-Martin S. A Metabolically Healthy Profile is a Transient Stage when Exercise and Diet are Not Supervised: Long-Term Effects in the EXERDIET-HTA Study. Int. J. Environ. Res. Public. Health. 2020;17:2830. doi: 10.3390/ijerph17082830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alonso J., Ferrer M., Gandek B., Ware J.E., Jr., Aaronson N.K., Mosconi P., Rasmussen N.K., Bullinger M., Fukuhara S., Kaasa S., et al. Health-Related Quality of Life Associated with Chronic Conditions in Eight Countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual. Life Res. 2004;13:283–298. doi: 10.1023/B:QURE.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 31.Di Liegro C.M., Schiera G., Proia P., Di Liegro I. Physical Activity and Brain Health. Genes. 2019;10:720. doi: 10.3390/genes10090720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matta Mello Portugal E., Cevada T., Sobral Monteiro-Junior R., Teixeira Guimaraes T., da Cruz Rubini E., Lattari E., Blois C., Camaz Deslandes A. Neuroscience of Exercise: From Neurobiology Mechanisms to Mental Health. Neuropsychobiology. 2013;68:1–14. doi: 10.1159/000350946. [DOI] [PubMed] [Google Scholar]
- 33.Gorostegi-Anduaga I., Maldonado-Martin S., MartinezAguirre-Betolaza A., Corres P., Romaratezabala E., Whittaker A.C., Francisco-Terreros S., Perez-Asenjo J. Effects on Cardiovascular Risk Scores and Vascular Age After Aerobic Exercise and Nutritional Intervention in Sedentary and Overweight/Obese Adults with Primary Hypertension: The EXERDIET-HTA Randomized Trial Study. High. Blood Press Cardiovasc. Prev. 2018;25:361–368. doi: 10.1007/s40292-018-0281-0. [DOI] [PubMed] [Google Scholar]
- 34.Moreira J.B.N., Wohlwend M., Wisloff U. Exercise and Cardiac Health: Physiological and Molecular Insights. Nat. Metab. 2020;2:829–839. doi: 10.1038/s42255-020-0262-1. [DOI] [PubMed] [Google Scholar]
- 35.Karlsen T., Aamot I.L., Haykowsky M., Rognmo O. High-Intensity Interval Training for Maximizing Health Outcomes. Prog. Cardiovasc. Dis. 2017;60:67–77. doi: 10.1016/j.pcad.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 36.Battaglia G., Bellafiore M., Alesi M., Paoli A., Bianco A., Palma A. Effects of an Adapted Physical Activity Program on Psychophysical Health in Elderly Women. Clin. Interv. Aging. 2016;11:1009–1015. doi: 10.2147/CIA.S109591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pescatello L.S., MacDonald H.V., Ash G.I., Lamberti L.M., Farquhar W.B., Arena R., Johnson B.T. Assessing the Existing Professional Exercise Recommendations for Hypertension: A Review and Recommendations for Future Research Priorities. Mayo Clin. Proc. 2015;90:801–812. doi: 10.1016/j.mayocp.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Guallar-Castillón P., Santa-Olalla P., Ramón J., López E., Rodríguez-Artalejo F. Actividad Física Y Calidad De Vida De La Población Adulta Mayor En España. Med. Clin. 2004;123:606–610. doi: 10.1016/S0025-7753(04)74616-3. [DOI] [PubMed] [Google Scholar]
- 39.Yorks D.M., Frothingham C.A., Schuenke M.D. Effects of Group Fitness Classes on Stress and Quality of Life of Medical Students. J. Am. Osteopath. Assoc. 2017;117:e17–e25. doi: 10.7556/jaoa.2017.140. [DOI] [PubMed] [Google Scholar]
- 40.Reljic D., Frenk F., Herrmann H.J., Neurath M.F., Zopf Y. Low-Volume High-Intensity Interval Training Improves Cardiometabolic Health, Work Ability and Well-being in Severely Obese Individuals: A Randomized-Controlled Trial Sub-Study. J. Transl. Med. 2020;18:419. doi: 10.1186/s12967-020-02592-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jung M.E., Bourne J.E., Little J.P. Where does HIT Fit? An Examination of the Affective Response to High-Intensity Intervals in Comparison to Continuous Moderate- and Continuous Vigorous-Intensity Exercise in the Exercise Intensity-Affect Continuum. PLoS ONE. 2014;9:e114541. doi: 10.1371/journal.pone.0114541. [DOI] [PMC free article] [PubMed] [Google Scholar]