Abstract
Colorectal cancer (CRC) is one of the leading causes of cancer deaths worldwide. The initiation and progression of CRC is a multi-step process that proceeds via precursor lesions to carcinoma, with each stage characterized by its distinct molecular and tissue microenvironment changes. Precursor lesions of CRC, aberrant crypt foci, and adenoma exhibit drastic changes in genetic, transcriptomic, and proteomic profiles compared to normal tissue. The identification of these changes is essential and provides further validation as an initiator or promoter of CRC and, more so, as lesion-specific druggable molecular targets for the precision chemoprevention of CRC. Mutated/dysregulated signaling (adenomatous polyposis coli, β-catenin, epidermal growth factor receptor, V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog (KRAS), tumor protein53, Akt, etc.), inflammatory (cyclooxygenase-2, microsomal prostaglandin E synthase-1, inducible nitric oxide synthase, and other pro-inflammatory mediators), and metabolic/growth factor (fatty acid synthase, β-Hydroxy β-methylglutaryl-CoA reductase, and ornithine decarboxylase) related targets are some of the well-characterized molecular targets in the precision chemoprevention of CRC. In this review, we discuss precursor-lesion specific targets of CRC and the current status of pre-clinical studies regarding clinical interventions and combinations for better efficacy and safety toward future precision clinical chemoprevention. In addition, we provide a brief discussion on the usefulness of secondary precision chemopreventive targets for tertiary precision chemoprevention to improve the disease-free and overall survival of advanced stage CRC patients.
Keywords: colorectal cancer, biomarkers, precision prevention, molecular targets
1. Introduction
Colorectal cancer (CRC) is one of the leading causes of cancer-related deaths worldwide. CRC can be preventable with early diagnosis and can sometimes lead to a complete cure. CRC is a major public health issue worldwide, with an estimated 861,000 deaths and 1.8 million new cases annually [1]. In the United States (US), an estimated 147,950 cases and 53,200 people will die from CRC in 2020 [1].
Most of the CRC cases (≈55–70%) are sporadic and about 30% are linked to genetic disorders, which are mostly related to the increased risk from hereditary polyposis syndromes or hereditary nonpolyposis colon cancer (Lynch syndrome) [1]. Familial adenomatous polyposis (FAP) accounts for about 1% of all CRC [1]. The sporadic and non-hereditary CRC linked to environmental factors, including diet, weight, food-borne mutagens, intestinal commensals, and chronic intestinal inflammation [1,2]. Most of the sporadic cases are detected at advanced stages of CRC, which makes it difficult to treat them. This gained attention by clinicians and researchers to identify novel biomarkers/targets for detection as well as precision chemoprevention of CRC.
The precision prevention of CRC is tailoring treatment recommendations for each individual patient based on their genetic basis and profiling of related biomarkers. The aim of precision prevention is to either increase the efficacy of treatment or reduce the side effects by selecting the appropriate treatment based on the tumor biomarker. The identification and development of novel biomarkers/targets is crucial to the future of precision oncology.
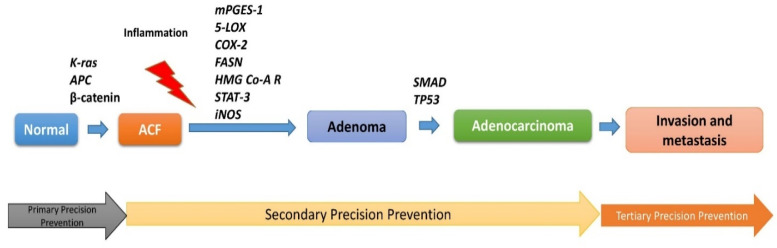
The initiation of CRC driven by loss of homeostasis of the epithelium of the intestine and mutations of key genes (for an example: APC) leads to abnormal crypt growth, leading to aberrant crypt foci (ACF) and further activation of pro-inflammatory mediators. The dysregulation of several signaling pathways within the ACF microenvironment leads to adenoma formation [2]. Furthermore, several mutations, importantly, KRAS, SMAD, and TP53, appear to be altered and promote adenoma to adenocarcinoma and metastasis. Moreover, genomic instability is a crucial feature in CRC initiation and development, which is mainly categorized into the chromosomal instability (≈85%) and microsatellite instability (≈15%) pathways. Chromosome instability is associated with several frequently mutated genes (APC, TP53, KRAS, TGF-β and others) of CRC during initiation and progression [3].
The review article updates the current knowledge in various biomarkers and molecular targets for the precision prevention/treatment of CRC. It describes the expression profile and the role of several markers at various stages of CRC development as evident from and supported by pre-clinical and clinical studies. Furthermore, the potential utility of some of the selected biomarkers and their targeted agents for personalized CRC chemoprevention/therapy are also reviewed.
2. Lesions-Specific Molecular Targets in CRC
2.1. Mutated and Dysregulated Signaling Precision-Molecular Targets
2.1.1. APC/β-Catenin
Adenomatous polyposis coli (APC), a gatekeeper tumor suppressor gene, is the most commonly mutated gene in familial adenomatous polyposis (FAP) that develops many colonic polyps and has the highest risk of developing colonic cancers at an early age (<35 years) [2,4,5]. In addition, the APC gene is mutated in more than 80% of patients with sporadic CRC. Dysregulation of the Wnt/APC/β-catenin pathway is associated with APC mutation [2,4]. One of major functions of the APC protein is the regulation of β-catenin by its degradation and maintenance of the homeostasis of normal colon epithelial cell growth. Mutations in the APC gene lead to a functionally inactive, oncogenic truncated APC protein, leading to the nuclear translocation of β-catenin and induction of genes responsible for the carcinogenesis of CRC [2,4]. Clinical data suggest that CRC correlates with increased nuclear levels of β-catenin phosphorylated at serine 552 and bound with TCF4 in nucleus (Table 1) [6]. APC/β-catenin mutations were found in precursor lesions (ACF and mucin depleted foci (MDF)) and adenoma in both humans and rodents by PCR amplification and sequencing of their DNA [7]. Some studies show that an uncontrolled nuclear accumulation of β-catenin in intestinal epithelial cells in pre-neoplastic lesions is a prerequisite for the progression of tumor growth [8]. Several small molecule agents that target the Wnt/β-catenin signaling pathway are developed, and some are in various stages of their pre-clinical and clinical development for CRC. However, no drug that targets this pathway has entered into clinical practice [9]. Overall, studies demonstrated that APC/β-catenin is a well validated target for CRC prevention and warranted detailed studies to develop inhibitors of this pathway as chemopreventive agents for CRC prevention.
Table 1.
Expression status of molecular targets at different stages from initiation to progression of colorectal cancer (CRC).
| Normal | ACF | Adenoma | Adenocarcinoma | References | |
|---|---|---|---|---|---|
| Mutant/Dysregulated Signaling | |||||
| APC | |||||
| Pre-clinical | + | − | − | − | [6] |
| Clinical | + | − | − | − | [3,4,5] |
| β-catenin | |||||
| Pre-clinical | + | ++ | ++++ | +++++ | [7,8] |
| Clinical | + | ++ | ++++ | +++++ | [6] |
| TP53 | |||||
| Pre-clinical | + | + | − | − | [24] |
| Clinical | + | + | − | − | [20,21,22,23] |
| KRAS | |||||
| Pre-clinical | − | ? | +++ | ++++ | [12,13] |
| Clinical | − | + | +++ | ++++ | [12] |
| AKT | |||||
| Pre-clinical | − | ? | +++ | +++++ | [30] |
| Clinical | − | ? | +++ | +++++ | [29] |
| SMAD4 | |||||
| Pre-clinical | + | ? | + | − | [19] |
| Clinical | + | ? | + | − | [19] |
| Inflammatory | |||||
| COX-2 | |||||
| Pre-clinical | − | + * | ++++ | +++++ | [34] |
| Clinical | ? | ++++ | +++++ | [32,35] | |
| mPGES-1 | |||||
| Pre-clinical | − | ? | ++++ | +++++ | [45,46] |
| Clinical | − | ? | ++++ | +++++ | [47,48] |
| 5-LOX | |||||
| Pre-clinical | − | ? | +++ | ++++ | [49] |
| Clinical | − | ? | +++ | ++++ | [50,51] |
| iNOS | |||||
| Pre-clinical | − | + * | +++ | ++++ | [52] |
| Clinical | − | ? | +++ | ++++ | [53,54] |
| 15-PGDH | |||||
| Pre-clinical | +++ | ? | − | − | [55] |
| Clinical | +++ | ? | − | − | [56] |
| STAT-3 | |||||
| Pre-clinical | + | ? | +++ | +++++ | [57] |
| Clinical | + | ? | +++ | +++++ | [58] |
| Prostaglandin I2 Synthase | ++ | − | − | − | |
| Pre-clinical | ++ | − | − | − | [59,60] |
| Clinical | ++ | − | − | − | [61] |
| 15-LOX | |||||
| Pre-clinical | ++ | ? | − | − | [62,63] |
| Clinical | ++ | ? | − | − | [64] |
| Growth and metabolism | |||||
| Ornithine decarboxylase | |||||
| Pre-clinical | + | ? | ++++ | +++++ | [65] |
| Clinical | + | ? | ++++ | +++++ | [66,67,68] |
| HMG Co-A-Reductase | |||||
| Pre-clinical | + | ? | ++++ | +++++ | [69,70] |
| Clinical | + | ? | ++++ | +++++ | [71] |
| Fatty acid synthase | |||||
| Pre-clinical | + | + | +++ | ++++ | [72] |
| Clinical | + | + | +++ | ++++ | [72,73] |
“−” less expression or mutation; “+, ++, +++, ++++, +++++” overexpression or upregulation; “?” unknown expression levels; * Minimally expressed in ACF.
2.1.2. KRAS/EGFR
The epidermal growth factor receptor (EGFR)/V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog (KRAS) pathway plays a key role in CRC initiation and progression [10]. The KRAS gene is the most frequently mutated gene in CRC and is associated with the modulation of several downstream effectors to include: RAF/MEK/ERK, PTEN-PI3K-AKT-mTOR, RalGDS/p38MAPK, and Rac/Rho during tumorigenesis and the tumor progression of CRC [11]. The KRAS mutation is more frequent in ACF and colon tumors (Table 1; Figure 1) [5,12,13]. Approximately 40% of colon cancers are positive for mutations in KRAS [12,13]. Takahashi et al. [14] reported that KRAS was mutated in ACF, adenoma, and adenocarcinomas in AOM-treated colons of rats. KRAS mutations are more common in female patients with CRC than in male patients with CRC [15].
Figure 1.
Important molecular targets during colorectal tumorigenesis and progression.
KRAS mutations are associated with a lack of response to anti-EGFR targeted therapies for CRC patients [15]. This is because KRAS amplification may also be responsible for primary resistance to EGFR inhibitors [16]. Therefore, oncogenic KRAS pathways are key targets for CRC prevention/therapy. However, detailed investigations are still required to demonstrate the clear role of the EGFR pathway in colorectal tumorigenesis and progression.
2.1.3. TGF-β1/SMAD
TGF-β1 plays an important role in controlling gut inflammation in relation to the continuous stimulation of the intestinal microbiota. SMAD4 is a common mediator of the TGF-1β signaling pathway. Tsushima et al. [17] reported high levels of TGF-β1 in patients with colorectal cancer compared to healthy individuals (Table 1; Figure 1). SMAD4 haploinsufficiency is associated with an increased susceptibility to bowel inflammation with variable penetrance in association with the colonic mucosal microbiota [18]. TGF-β1 suppressed the expression of pro-inflammatory markers in the colon epithelium, and the loss of its downstream mediator, SMAD4, is associated with the initiation of inflammation-driven colon cancer and is identified as a tumor suppressor. Loss of SMAD4 expression is observed in 48% of human colitis-associated carcinoma samples as compared with 19% of sporadic colorectal carcinomas [19]. Hence, these studies suggested that TGF-β1/SMAD4 is a novel biomarker and target for the prevention of CRC.
2.1.4. TP53
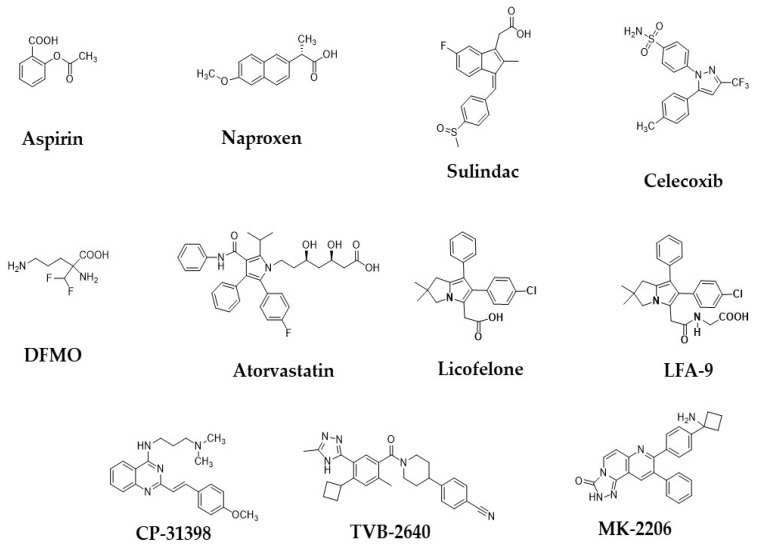
TP53 is a tumor suppressor gene, and the mutation of this gene commonly occurs in approximately 40–50% of sporadic CRC [20]. The status of p53 mutation is closely related to the progression and outcome of sporadic CRC [20]. TP53 mutations are most commonly found in adenoma to adenocarcinoma stages of CRC (Table 1; Figure 1) [21]. Previous studies suggested that p53 protein accumulation and p53 gene mutations were not found in ACF [22,23]. Chang et al. [24] reported that the loss of p53 enhanced the induction of colitis-associated CRC by dextran sulfate sodium. Recently, Alpert et al. [25] found that TP53 mutations are common in inflammatory bowel disease-associated colon cancer, while the frequency of APC and KRAS mutations was significantly lower than in sporadic CRC (Table 1) [25,26]. Hence, the authors concluded that TP53 is a novel target for IBD-CRC. Previously, we reported that CP-31398 exhibited significant chemopreventive activity in a pre-clinical animal model (Figure 2) [27]. These pre-clinical studies warranted clinical studies on the combinational use of CP-31398 and celecoxib for the prevention and therapy of CRC. Overall, studies suggest that TP53 is a promising marker for precision prevention and therapy of CRC.
Figure 2.
Chemical structures of some of the important precision chemopreventive agents for colorectal cancer prevention and treatment by inhibiting or modulating the various key targets.
2.1.5. AKT
AKT pathway has been investigated extensively in CRC initiation and progression [28,29]. The lipid product of class I PI3Ks activates the downstream kinase AKT (AKT1, AKT2, AKT3), which is further involved in the pathophysiology of CRC tumorigenesis [28,29]. Clinical and pre-clinical evidence suggests that an overexpression of AKT is found in tumors of CRC as compared to normal tissues. Phosphorylated-AKT was high adenocarcinoma compared with adenoma and normal colonic mucosa [29]. Roy et al. [30] reported that AKT is overexpressed in adenomas of sporadic CRC but not in normal colonic mucosa and/or hyperplastic polyps. A selective inhibitor of AKT MK-2206 is under clinical evaluation with combination of other drugs for treatment of the patients with CRC (Figure 2) [31]. Thus, the AKT pathway has been considered as a target in initial and later stages of CRC.
2.2. Inflammatory Targets: ACF Progression to Adenoma
2.2.1. Cyclooxygenase-2
Cyclooxygenases (COX-1/2) are key enzymes in eicosanoids biosynthesis that catalyze arachidonic acid to PHG2. COX-1 is a constitutive enzyme and involved in normal physiological functions, while COX-2 is an inducible enzyme and plays a key role in the pathophysiology of inflammation and carcinogenesis. In rodent and human colonic tumors, COX-2 is overly expressed as compared to COX-1 [32]. The role of COX-2 in CRC is well established, and it is a validated target for adenoma prevention in both pre-clinical and clinical settings [33]. COX-2 expression is associated with multi-crypt-ACF and MDF, whereas no expression in normal crypts of the colon was observed [34]. The activated COX-2 pathway in ACF may be involved in its further progression to adenoma [32]. COX-2 is predominantly overexpressed in adenoma compared to adjacent normal colorectal mucosa (Table 1 and Figure 1) [35,36]. Polymorphism in the COX-2 gene (-765G/C region) was associated with an increased risk of CRC by several folds [37]. Nonsteroidal anti-inflammatory drugs, or NSAIDs (aspirin, naproxen, sulindac) and COX-2 selective inhibitors COXibs, such as celecoxib, are widely used in the clinic for CRC prevention (Figure 2) [38,39,40,41,42,43,44]. Chan et al. [42] found that the regular use of aspirin reduced the risk of CRC patients with an overexpression of COX-2. In a prospective and case-control study, the use of aspirin/NSAID appeared to lower the risk of COX-2-positive cancers, particularly among individuals with high levels of a circulatory inflammatory biomarker macrophage inhibitory cytokine-1 [43]. Hence, COX-2 is a novel target/biomarker in CRC, and its inhibitors have been widely used for the prevention and therapy of CRC.
2.2.2. Microsomal Prostaglandin E Synthase-1
Microsomal prostaglandin E synthase-1 (mPGES-1) is an inducible enzyme in inflammatory and oncologic conditions among other constitutive isoforms i.e., cytosolic PGES and mPGES-2, which specifically acts on PGH2 released by the activity of COX-2 and converts to PGE2 (Figure 1). mPGES-1 was reported to be overexpressed in the large ACF and adenomas and more so, in the adenocarcinomas, compared to the matched normal tissues (Table 1) [45,46,47,48,74]. The genetic deletion of mPGES-1 suppresses intestinal tumorigenesis in ApcD14/+ mice [45]. The deletion of mPGES-1 reduced the size and number of pre-neoplastic aberrant crypt foci (ACF) and blocked β-catenin nuclear translocation in carcinogen-induced ACF [45]. It also caused up to an 80% decrease in tumor multiplicity and up to a 90% reduction in tumor load in the distal colon of AOM (carcinogen)-treated mice compared to wild-type mice [74]. Moreover, a mechanistically enzymatic inhibition of mPGES-1 resulted in the suppression of PGE2 production and sparing the prostacyclin I2 and thromboxane B2, which circumvent the unwanted side effects associated with the inhibition of COX-2 activity [39]. Several mPGES-1 inhibitors have been developed as chemopreventive agents, and some of them are under various stages of their pre-clinical and clinical evaluation with a better safety profile [39]. Therefore, mPGES-1 is a novel and precision target for the prevention of CRC with better safety.
2.2.3. 5-Lipoxygenase
The lipoxygenase (5-LOX) involves the chronic inflammation and carcinogenesis of CRC. Accumulating evidence suggests a potential role of 5-LOX and its products in early and advanced stages of CRC carcinogenesis [50,51,75]. 5-LOX expression levels are higher in patients with CRC than healthy individuals and have found its expression levels associated with tumor initiation and progression [49,50,51]. 5-LOX inhibitors (e.g., zileuton) exhibited a chemopreventive effect in pre-clinical models of CRC [76]. Overall, studies so far suggest that 5-LOX is a precision target in CRC.
2.2.4. Prostacyclin I2 Synthase
Prostacyclin (PG I2), products of prostacyclin synthase (PGIS), have been characterized as anti-inflammatory mediators and tumor suppressors. PGI2 levels are suppressed in CRC compared to normal colonic mucosa [61]. Cutler et al. [77] reported that the stromal production of PGI2 showed an anti-apoptotic effect in colonic epithelial cells. The genetic deletion of prostacyclin synthase (PGIS) enhanced ACF formation at the early stage of carcinogenesis [59,60]. These results suggest that PGIS and PGIS-derived PGI2 are involved in anti-carcinogenic effects. Mechanistic studies demonstrated that epigenetic inactivation of the PTGIS gene (hypermethylation of the PTGIS promoter) is associated with colorectal carcinogenesis [78]. The aforementioned studies suggested that PGIS is a biomarker for CRC.
2.2.5. 15-Hydroxyprostaglandin Dehydrogenase
15-hydroxyprostaglandin dehydrogenase (15-PGDH) is an NAD(+)-dependent enzyme, which is involved in the degradation of PGE2 in a normal colon. 15-PGDH levels are significantly down-regulated in adenoma and adenocarcinoma as compared to normal colonic mucosa (Table 1) [56]. In an AOM/DSS-promoted carcinogenesis mouse model, 15-PGDH levels are low/abolished in colonic adenocarcinoma [55]. The expressions of 15-PGDH, apart from COX-2, in pre-treatment adenomas, provides predictive information in patients treated with celecoxib for the prevention of CR adenomas based on a study by Wang et al. [79]. In addition, elevated HDAC expression is correlated with the down-regulation of 15-PGDH in human colon cancers [80]. Moreover, HDAC inhibitors enhanced 15-PGDH expression in CRC cells [80]. Hence, 15-PGDH can be a predictive biomarker of CRC, and its enhancers are needed for CRC prevention.
2.2.6. 15-Lipoxygenase-1
15-lipoxygenase-1 (ALOX15 or 15-LOX-1), a member of the AA pathway, is involved in the formation of lipoxins and resolvins to resolve inflammation and cancer of the colon [62,64,81]. The expression of ALOX15 was less in adenoma of patients with CRC as compared to that of healthy individuals (Table 1) [64]. Transgenic expression of ALOX15 in the intestine of mice inhibited DSS-induced colitis and chemical-induced CRC tumorigenesis [55,79]. ALOX15 inhibited several pro-inflammatory mediators, which have a key role in the promotion of colorectal cancer via an activation of chronic inflammation [64,82]. ALOX15 expression suppressed the invasion of CRC cells [83,84]. 15-LOX-1 exhibits anti-angiogenic effects through reduced VEGF levels in CRC cells [85]. 15-LOX-1 improved the tumor-suppressive effect of NSAIDs and celecoxib, and this effect is associated with its overexpression [86]. Previous studies suggested that 15-LOX-1 exhibited tumor-suppressive effects during CRC tumorigenesis and can be a biomarker for CRC.
2.2.7. Inducible Nitric Oxide Synthase
Inducible nitric oxide synthase (iNOS), an inducible enzyme during inflammatory conditions, plays a key role in CRC initiation and progression. Among isoforms of nitric oxide synthase (nNOS, eNOS, and iNOS), iNOS has a key role in the pathophysiology of inflammatory and oncologic diseases, including CRC [2]. iNOS expression and activity were higher than normal in cancerous tissues of the colon (Table 1 and Figure 1) [52,53,54]. iNOS is overexpressed in precursor lesions, such as MDF [34]. The expression of iNOS was increased after the transition from hyperplastic ACF to dysplastic ACF, adenoma, and carcinoma [87]. Regular exercise prevents CRC tumorigenesis, which is partly mediated through the suppression of iNOS expression-associated inflammation [88]. Previous reports suggest that chronic inflammation and iNOS-mediated NO promotes neoplastic transformation of the colorectum, which leads to the carcinogenesis of CRC [2,89,90]. Mice with mutations in both APC and iNOS showed a reduction in adenomatous polyps in the small and large intestines compared to mice with the mutation in APC alone [91]. Moreover, several iNOS inhibitors showed a significant chemopreventive efficacy of CRC [92]. Hence, iNOS is a promising target in CRC prevention.
2.2.8. STAT-3
Signal transducer and activator of transcription (STAT), a group of signaling molecules, is involved in various physiological functions of cell proliferation and survival. The activation STAT (-1, -3 and -5) signaling pathway plays a key role in CRC tumorigenesis and progression [2,58]. STAT3 is overexpressed in malignant tissues compared to normal based on experimental and clinical data [57,58]. Li et al. [58] reported the prognostic role of phospho-STAT3 in patients with cancers. The STAT-3 signaling pathway plays a key role in the pathophysiology of IBD and colorectal cancer along with other pro-inflammatory mediators [93]. The activation of STAT-3 involves in the growth of CRC cells [94]. Previously, our group reported that regulatory T cells promote intestinal tumorigenesis via the activation of IL-22 and STAT-3 [95]. Chen et al. [96] reported that black raspberry anthocyanins prevented carcinogen-induced CRC by targeting several oncogenic mediators, including STAT-3. The aforementioned finding suggested that STAT-3 can be a novel target in CRC.
2.2.9. Chemokine Receptor 5
Chemokine receptor 5 (CCR5) is a chemokine receptor for chemokine CCR3 that plays an important role in CRC progression of CRC [96,97,98]. Löfroos et al. [98] reported that infiltrating T lymphocytes in colorectal cancers showed an overexpression of CCR5 (Table 1). CCR5-deficient mice failed to develop colon tumors in DSS/AOM-treated mice compared to wild-type mice [97]. Clinical data demonstrated that CCR5 expression in CD4 T-cells is associated with an increased risk of CRC [99]. Maraviroc, an antagonist of CCR5 and a drug for AIDS, suppressed the tumor formation of a murine CRC cell line and the growth of orthotopically injected colon cancer cells [100]. CCL5 is produced by lymphocytes and promotes tumor cell growth. In a clinical study, CCL5 antagonist showed a considerable effect in blocking CRC progression [101]. Previous studies suggest that CCR5 is novel target in CRC and its antagonist, maraviroc, can be a novel agent for CRC prevention and therapy based on future studies. Further detailed studies are warranted on CCR5 to validate as novel target in CRC at pre-clinical and clinical levels.
2.3. Metabolic and Growth Factor-Related Targets
2.3.1. Fatty Acid Synthase
Fatty acid synthase (FASN), a lipogenic enzyme, plays a key role in the carcinogenesis and development of CRC [102]. The overexpression of FASN was found in ACF and tumors with sporadic CRC or FAP [73]. FASN was highly expressed in rectal biopsies from patients harboring colonic adenomas as well as colonic mucosa of both the AOM-treated and APCpirc rats as compared to that of healthy tissue (Table 1) [72]. Increased FASN activity is associated with a decreased survival of patients with CRC [103,104]. FASN levels in serum are associated with different stages of colorectal cancer patients [105]. FASN inhibitors have been developed and are currently under evaluation of various stages of pre-clinical and clinical trials for CRC [103,104,105,106]. Oral FASN inhibitor (TVB-2640) entered a Phase I clinical trial (3V2640-CLIN-002) in solid tumor patients, and the study is demonstrating a favorable tolerability profile without any significant adverse events (Figure 2) [102]. Expression levels of FASN are more frequent in patients with advanced CRC [72,73]. In vitro studies confirmed that the knockdown of FASN in various CRC cell lines hindered the invasive capability of cancer cells, and these results suggested the pro-metastatic role of FASN in CRC tumorigenesis [107]. Zaytseva et al. [108] found that the overexpression of FASN is associated with advanced stages of CRC and liver metastasis. Kuchiba et al. [109] demonstrated that cellular FASN status determines a cell’s dependence on energy balance status for the malignant transformation of CRC. Chang et al. [110] reported that the blockade of FASN is associated with an inhibition of cell proliferation and induction of apoptosis. Hence, the aforementioned suggests that FASN is a novel target in CRC and its pharmacological inhibitory agents can be novel preventive and therapeutic agents for CRC.
2.3.2. Ornithine Decarboxylase
Ornithine decarboxylase (ODC) is a key enzyme in the biosynthesis of polyamines, which is involved in the proliferation of cells in colorectum. ODC activity of cancer tissue or adenoma tissue of CRC was significantly higher than that of normal tissues based on pre-clinical and clinical studies [65,66,67,68]. ODC inhibitors have been developed as chemopreventive agents for CRC [111,112]. D, L-α-diflouromethylornithine (DFMO), a selective ODC inhibitor, suppressed APC-dependent intestinal tumorigenesis in mice and was found to be less toxic (Figure 2) [65,113]. In clinical trials, DFMO inhibited ODC enzyme activity and polyamine contents and exhibited a preventive efficacy of CRC [111,112]. In a randomized clinical trial, DFMO in combination with the NSAID sulindac reduced the adenoma recurrence rate among individuals with colonic adenomas when compared with placebos [110]. Previously, we evaluated different combinations of chemopreventive agents with DFMO for CRC prevention in a chemical carcinogen-induced rat CRC model [114]. DFMO in combination with rosuvastatin alone or a combination strategy showed a significant suppression of colon adenocarcinomas in carcinogen-induced CRC [114]. In another study from our group, piroxicam plus DFMO significantly inhibited colon adenocarcinoma incidence in carcinogen-induced CRC [115]. Kumar et al. [116] found that the oral supplementation of ellagic acid caused the transcriptional inactivation of ODC expression, reducing ACF proliferation and/or progression, thereby exhibiting the chemopreventive efficacy of EA against CRC. Pre-clinical and clinical studies demonstrated that D, L-α-diflouromethylornithine (DFMO), a selective ODC inhibitor, exhibited chemopreventive efficacy on CRC [111,112]. Hence, ODC can be a promising target, and its pharmacological inhibitor DFMO can be a potential chemopreventive agent for CRC.
2.3.3. HMG Co-A Reductase
HMG Co-A Reductase (HMG Co-A R) is an enzyme involved in cholesterol synthesis and has a key role in the tumorigenesis of colorectal cancer. HMG Co-A R is overexpressed/high activity from normal epithelium to colorectal tumors of early or advanced stages of rodents and humans (Table 1 and Figure 1) [69,70,71]. Bengtsson et al. [71] reported that the significant associations of HMG Co-A reductase expression with expressions of cell survival markers in colorectal cancer. Inhibitors of HMG CO-A reductase are called statins, which have been widely explored as preventive and therapeutic agents for CRC [69,117]. Karagkounis et al. [118] reported that the combination of radiation and simvastatin inhibited the cell growth and viability of different CRC lines. Wei et al. [69,119] found that HDAC and HMG Co-A reductase dual inhibitory statin hydroxamic acid derivatives showed significant preventive efficacy on inflammation-driven colorectal tumorigenesis in rodent models. These studies suggest that the dual targeting of HDAC and HMG Co-A reductase can be a better strategy for the prevention of CRC. Atorvastatin, an HMG-CoA R inhibitor, suppressed intestinal tumorigenesis, and its chemopreventive efficacy was increased with low doses of celecoxib or NSAIDs in an APCmin\− mice (Figure 2) [120,121]. Previously, we reported that COX inhibitors and HMG Co-A reductase inhibitors (statins) were effective in chemopreventive efficacy than alone at a low dose [121]. In a population-based case-control study by Lipkin et al. [122], a single-nucleotide polymorphism was identified in the HMG Co-A gene that significantly modified the chemopreventive protective association between statins and CRC risk. Therefore, HMG-CoA R has been proven as a promising target, and its inhibitors statins exhibited promising efficacy in CRC secondary prevention.
3. Molecular Targets and Tertiary Precision Prevention
The importance of tertiary precision prevention has grown due to the increasing mortality and morbidity of CRC. A lack of well validated surrogate biomarker(s) at the pre-clinical and clinical level has limited the development of precision preventive strategies to improve the cancer survivors. Pre-clinical and clinical studies demonstrate that several factors with a major impact on the risk of developing CRC are also related to the cancer survival, which highlights opportunities for tertiary precision prevention. In this scenario, the role of chemoprevention in tertiary precision prevention is currently an important subject to intensive research. COXs, ODC, and HMG Co-A reductase are the most validated targets for CRC tertiary prevention, and their inhibitors (NSAIDs, COXibs, and statins) showed promising efficacy in the reduction of adenocarcinoma based on pre-clinical and clinical evaluations [40,123,124,125,126,127]. Previously, our group reported that the administration of 1500 ppm celecoxib during the progression stage also significantly suppressed the incidence and multiplicity of adenocarcinomas of the colon [126]. A meta-analysis by Li et al. [127] demonstrated that the use of aspirin after diagnosis improves CRC survival. A phase III double-blind placebo-controlled randomized trial of aspirin (80 mg given orally) once daily for five years is ongoing to evaluate five-year overall survival for stage II and III colon cancer patients and recurrence (https://clinicaltrials.gov/ct2/show/NCT02301286) [124]. mPGES-1 is expressed and correlated with a significantly worse prognosis in stage I–III patients of CRC. However, more studies are required to validate the mPGES-1 as a novel target for the safer tertiary precision prevention of CRC [125]. Overall, pre-clinical and clinical studies suggested the emerging role of several molecular targets and its inhibitors in the tertiary precision prevention of CRC.
4. Pre-Clinical Rodent Animal Models for Biomarkers-Based Precision Chemoprevention
Several animal models have been developed for biomarkers-based research relevant to the chemoprevention of CRC, including chemically induced CRC and genetically modified rodent models, which are useful in pre-clinical novel biomarkers identification and target-based drug development for human CRC preventive/therapeutic intervention. Among the chemically induced CRC models, the combination of azoxymethane (AOM) with the inflammatory agent dextran sodium sulfate (DSS) in rodents has proven to dramatically shorten the latency time for the induction of CRC with ACF–adenoma–carcinoma sequence that occurs in human CRC [128]. This model has been helpful in the identification of biomarkers/agents for primary, secondary, and tertiary chemoprevention of inflammation-associated and sporadic CRC. The APCmin/+ mouse model is the most commonly used model related to the APC gene heterozygous mutation and β-catenin pathway activation, and it is helpful in the identification of biomarkers/agents for the chemoprevention of hereditary CRC [129]. Tetteh et al. [130] developed an inducible colon-specific cre enzyme mouse line for proximal tumors development with APC/KRAS mutation and aggressive carcinomas with some invasion into lymph nodes also developed upon a combined induction of oncogenic mutations of APC, Kras, p53, and SMAD4 in quadruple-mutant mice. APCpirc is a novel model in rats, which mimics the FAP of humans with pre-neoplastic polyps development in the colorectum [6,131,132]. Moreover, MDF are formed in colons of the rats during CRC initiation and associated with nuclear β-catenin accumulation (Table 1) [123,124]. The aforementioned models are widely used for the identification of novel targets and target-based agents at the pre-clinical level for the chemoprevention of CRC [131,132].
Several pre-clinical models have been developed for studies related to Lynch syndrome [133,134,135]. Homozygous Msh2, Msh6, and Mlh1 knockout mice are cancer-prone, developing tumors in different organs including the colorectum. The disadvantage of these homozygous knockout mice is they usually die by 6 to 8 months due to aggressive lymphomas [133,134]. To overcome the early death, conditional Msh2 knockout mice, in which intestine-specific gene inactivation is permitted, have been generated using Villin-Cre or Cdx2-NLS-Cre. These mice develop tumors that highly mimic the tumors developed by patients with Lynch syndrome [134]. Biallelic germ-line mutations in the MUTYH gene, which encodes for a DNA glycosylase involved in base excision repair, have been identified in patients with hereditary multiple colorectal adenoma and carcinoma. A Mutyh−/− mouse strain was developed and their response to oxidative stress in the form of exposure to dextran sulfate sodium (DSS) was assessed [135]. The mice model development has helped to understand the base–excision–repair and inflammatory response in CRC tumorigenesis.
In addition, xenografts and orthotopic rodent animal models have been developed for CRC carcinogenesis studies and therapeutic drug development [136]. CRC stem cells appeared in the tumors of the xenograft model, but the lack of active immune system in these models is the drawback for their utility in immunomodulation studies [136]. Subcutaneous xenografts are not useful for CRC local tumor invasion and CRC metastatic research, while the orthotopic model is useful for studies related to metastasis [136]. Moreover, the molecularly annotated patient-derived xenograft “Avatar” models are providing an excellent opportunity for co-clinical trials to determine the clinical decisions, including the identification of precision-targeted therapeutic agents, for patients with CRC in a real-time manner [137].
5. Conclusions and Perspectives
Biomarker analyses of CRC are important in order to diagnose and develop precise target specific agents for the precision chemoprevention of CRC. Over the last decade, tremendous progress has been made by several research groups in the identification and development of biomarkers/targets for the precision prevention of CRC, which is one of the reasons for the drop in the death rate in men and women in the US. Some of the biomarkers can be surrogate endpoint markers (APC, β-catenin, HMG-CoA R, COX-2, mPGES-1, 5-LOX, TP53, KRAS, TGF-β1, AKT, and ODC) other than ACF/adenoma, which can be useful to understand the CRC development and also to evaluate the effectiveness of the agent’s preventive/therapeutic intervention.
The mutation of the APC gene and activation of β-catenin occurs in the initiation of CRC. Therefore, the APC/β-catenin pathway is a key target in the prevention of CRC at an early stage. Several inhibitors of the APC/β-catenin pathway are under pre-clinical and clinical evaluation for prevention and/or treatment of CRC. KRAS is one of the most commonly mutated genes in CRC, and EGFR/KRAS has been considered as an important target in the prevention of CRC. Mutations of TP53 and SMAD and the activation of PI3K/AKT play an important role in the adenoma–carcinoma sequence.
There are several biomarkers of inflammation; for instance, COX-2 is the most validated target in the secondary precision prevention of CRC. The incidence of colitis and other inflammation-associated CRC has diminished from the last decades due to the use of NSAIDs. Aspirin, sulindac, naproxen, and other NSAIDs, as well as COXibs such as celecoxib, are widely used for the secondary and tertiary prevention of CRC. However, gastrointestinal, cardiovascular, and renal side effects are limiting their usage. In this scenario, combinational therapies such as COX inhibitors and other chemopreventive agents such as statins, or targeting downstream mediators of COX-2 such as mPGES-1, have been validated as a target for the safer chemoprevention of CRC. Recent findings suggest that COX-2 or mPGES-1 alone are not very effective in blockade of the inflammation due to arachidonate metabolic pathway diversion to leukotrienes production by the activation of 5-LOX. Further, COX/5-LOX inhibitors (e.g., licofelone) were developed but did not enter into the clinic due to safety concerns (Figure 2). Therefore, targeting mPGES-1/5-LOX dual inhibitors is an effective and safer strategy. Recently, mPGES-1/5-LOX inhibitor LFA-9 was designed and developed as a next-generation anti-inflammatory agent using a rational drug design strategy and exploring its pre-clinical anti-inflammatory efficacy [138] (Figure 2). ODC, FASN, and HMG COA-reductase are growth-factor/metabolic regulators, respectively, which are promising targets in obesity-mediated CRC. Statins are widely evaluated in pre-clinical and clinical levels for CRC prevention.
Over the last decade, several biomarkers/targets are identified and well characterized, and some others are under evaluation at the pre-clinical and clinical level, which have diagnostic and preventive/therapeutic importance in the precision chemoprevention of CRC. In addition, current and future efforts should focus on the identification, validation, and implementation of novel molecular biomarkers, which will achieve surrogate end point status. In turn, this may be helpful to the development of molecular targeted precision medicine with great promise in CRC prevention and treatment.
Abbreviations
| CRC | Colorectal cancer |
| ACF | Aberrant crypt foci |
| APC | Adenomatous polyposis coli |
| KRAS | V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog |
| COX-2 | Cyclooxygenase-2 |
| LOX | Lipoxygenase |
| FASN | Fatty acid synthase |
| ODC | Ornithine decarboxylase |
| iNOS | Inducible nitric oxide synthase |
| EGFR | Epidermal growth factor receptor |
| HMG Co-A-R | 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase |
| FASN | Fatty acid synthase |
| TGF-β1 | Transforming growth factor-β1 |
| 15-PGDH | 15-hydroxyprostaglandin dehydrogenase |
| STAT | Signal transducer and activator of transcription |
| NSAIDs | Nonsteroidal anti-inflammatory drugs |
| AOM | Azoxymethane |
| FAP | Familial adenomatous polyposis |
| CCR5 | Chemokine receptor 5 |
| PGI2 | Prostacyclin |
| PGE2 | Prostaglandin E2 |
| mPGES-1 | Microsomal prostaglandin E synthase-1 |
| MDF | Mucin depleted foci |
| COXibs | COX-2 inhibitors |
| CCR5 | Chemokine receptor 5 |
Author Contributions
C.V.R. supervised the conception of the work and participated in the discussion and review of the manuscript. V.M. participated in the discussion and review of the manuscript. N.S.Y. wrote the manuscript and produced the figures and tables; G.P. participated in the discussion and produced Figure 2. All authors have read and agreed to the published version of the manuscript.
Funding
The authors acknowledge NIH/NCI R01CA 213987, NIH/NCI HHSN261201500024I and VA merit for funding support.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.The American Cancer Society Journal, CA: A Cancer Journal for Clinicians Cancer Facts & Figures. [(accessed on 10 October 2020)]; Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2020-2022.pdf.
- 2.Janakiram N.B., Rao C.V. Molecular markers and targets for colorectal cancer prevention. Acta Pharmacol. Sin. 2008;29:1–20. doi: 10.1111/j.1745-7254.2008.00742.x. [DOI] [PubMed] [Google Scholar]
- 3.Müller M.F., Ibrahim A.E., Arends M.J. Molecular pathological classification of colorectal cancer. Virchows Arch. 2016;469:125–134. doi: 10.1007/s00428-016-1956-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fodde R. The APC gene in colorectal cancer. Eur. J. Cancer. 2002;38:867–871. doi: 10.1016/S0959-8049(02)00040-0. [DOI] [PubMed] [Google Scholar]
- 5.Yuan P., Sun M.H., Zhang J.S., Zhu X.Z., Shi D.R. APC and K-ras gene mutation in aberrant crypt foci of human colon. World J. Gastroenterol. 2001;7:352–356. doi: 10.3748/wjg.v7.i3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goretsky T., Bradford E.M., Ye Q., Lamping O.F., Vanagunas T., Moyer M.P., Keller P.C., Sinh P., Llovet J.M., Gao T., et al. Beta-catenin cleavage enhances transcriptional activation. Sci. Rep. 2018;8:671. doi: 10.1038/s41598-017-18421-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Femia A.P., Dolara P., Giannini A., Salvadori M., Biggeri A., Caderni G. Frequent mutation of Apc gene in rat colon tumors and mucin-depleted foci, preneoplastic lesions in experimental colon carcinogenesis. Cancer Res. 2007;67:445–449. doi: 10.1158/0008-5472.CAN-06-3861. [DOI] [PubMed] [Google Scholar]
- 8.Femia A.P., Piero D., Maddalena S., Giovanna C. Expression of LGR-5, MSI-1 and DCAMKL-1, putative stem cell markers, in the early phases of 1,2-dimethylhydrazine-induced rat colon carcinogenesis: Correlation with nuclear β-catenin. BMC Cancer. 2013;13:48. doi: 10.1186/1471-2407-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiaofei C., Xiangming X., Dong C., Feng Z., Weilin W. Therapeutic Potential of Targeting the Wnt/β-catenin Signaling Pathway in Colorectal Cancer. Biomed. Pharmacother. 2019;110:473–481. doi: 10.1016/j.biopha.2018.11.082. [DOI] [PubMed] [Google Scholar]
- 10.Markman B., Javier R.F., Capdevila J., Tabernero J. EGFR and KRAS in colorectal cancer. Adv. Clin. Chem. 2010;51:71–119. doi: 10.1016/s0065-2423(10)51004-7. [DOI] [PubMed] [Google Scholar]
- 11.Rizzo S., Bronte G., Fanale D., Corsini L., Silvestris N., Santini D., Gulotta G., Bazan V., Gebbia N., Fulfaro F., et al. Prognostic vs predictive molecular biomarkers in colorectal cancer: Is KRAS and BRAF wild type status required for anti-EGFR therapy? Cancer Treat. Rev. 2010;36:S56–S61. doi: 10.1016/S0305-7372(10)70021-9. [DOI] [PubMed] [Google Scholar]
- 12.Pretlow T.P., Pretlow T.G. Mutant KRAS in aberrant crypt foci (ACF): Initiation of colorectal cancer? Biochim. Biophys. Acta. 2005;1756:83–96. doi: 10.1016/j.bbcan.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Femia A.P., Tarquini E., Salvadori M., Ferri S., Giannini A., Dolara P., Caderni G. K-ras mutations and mucin profile in preneoplastic lesions and colon tumors induced in rats by 1,2-dimethylhydrazine. Int. J. Cancer. 2008;122:117–123. doi: 10.1002/ijc.23065. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi M., Mutoh M., Kawamori T., Sugimura T., Wakabayashi K. Altered expression of beta-catenin, inducible nitric oxide synthase and cyclooxygenase-2 in azoxymethane-induced rat colon carcinogenesis. Carcinogenesis. 2000;21:1319–1327. doi: 10.1093/carcin/21.7.1319. [DOI] [PubMed] [Google Scholar]
- 15.Kwak M.S., Cha J.M., Cho Y.H., Kim S.H., Yoon J.Y., Jeon J.W., Shin H.P., Joo K.R., Lee J.I. Clinical Predictors for KRAS Codon 13 Mutations in Patients with Colorectal Cancer. J. Clin. Gastroenterol. 2018;52:431–436. doi: 10.1097/MCG.0000000000000809. [DOI] [PubMed] [Google Scholar]
- 16.Valtorta E., Misale S., Sartore-Bianchi A., Nagtegaal I.D., Paraf F., Lauricella C., Dimartino V., Hobor S., Jacobs B., Ercolani C. KRAS gene amplification in colorectal cancer and impact on response to EGFR-targeted therapy. Int. J. Cancer. 2013;133:1259–1265. doi: 10.1002/ijc.28106. [DOI] [PubMed] [Google Scholar]
- 17.Tsushima H., Kawata S., Tamura S., Ito N., Shirai Y., Kiso S., Imai Y., Shimomukai H., Nomura Y., Matsuda Y., et al. High levels of transforming growth factor beta 1 in patients with colorectal cancer: Association with disease progression. Gastroenterology. 1996;110:375–382. doi: 10.1053/gast.1996.v110.pm8566583. [DOI] [PubMed] [Google Scholar]
- 18.Szigeti R., Pangas S.A., Nagy-Szakal D., Dowd S.E., Shulman R.J., Olive A.P., Popek E.J., Finegold M.J., Kellermayer R. SMAD4 haploinsufficiency associates with augmented colonic inflammation in select humans and mice. Ann. Clin. Lab. Sci. 2012;42:401–408. doi: 10.1097/00054725-201112002-00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Means A.L., Freeman T.J., Zhu J., Woodbury L.G., Marincola-Smith P., Wu C., Meyer A.R., Weaver C.J., Padmanabhan C., An H., et al. Epithelial Smad4 Deletion Up-Regulates Inflammation and Promotes Inflammation-Associated Cancer. Cell. Mol. Gastroenterol. Hepatol. 2018;6:257–276. doi: 10.1016/j.jcmgh.2018.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takayama T., Miyanishi K., Hayashi T., Sato Y., Niitsu Y. Colorectal cancer: Genetics of development and metastasis. J. Gastroenterol. 2006;41:185–192. doi: 10.1007/s00535-006-1801-6. [DOI] [PubMed] [Google Scholar]
- 21.Xiao L.L., Jianbiao Z., Zhi-Rong C., Wee-Joo C. p53 mutations in colorectal cancer- molecular pathogenesis and pharmacological reactivation. World J. Gastroenterol. 2015;21:84–93. doi: 10.3748/wjg.v21.i1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamashita N., Minamoto T., Ochiai A., Onda M., Esumi H. Frequent and characteristic K-ras activation and absence of p53 protein accumulation in aberrant crypt foci of the colon. Gastroenterology. 1995;108:434–440. doi: 10.1016/0016-5085(95)90071-3. [DOI] [PubMed] [Google Scholar]
- 23.Losi L., Roncucci L., Di Gregorio C., Leon M.P., Benhattar J. K-ras and p53 mutations in human colorectal aberrant crypt foci. J. Pathol. 1996;178:259–263. doi: 10.1002/(SICI)1096-9896(199603)178:3<259::AID-PATH473>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 24.Chang W.C., Coudry R.A., Clapper M.L., Zhang X., Williams K.L., Spittle C.S., Li T., Cooper H.S. Loss of p53 enhances the induction of colitis-associated neoplasia by dextran sulfate sodium. Carcinogenesis. 2007;28:2375–2381. doi: 10.1093/carcin/bgm134. [DOI] [PubMed] [Google Scholar]
- 25.Alpert L., Yassan L., Poon R., Kadri S., Niu N., Patil S.A., Mujacic I., Montes D., Galbo F., Wurst M.N., et al. Targeted mutational analysis of inflammatory bowel disease-associated colorectal cancers. Hum. Pathol. 2019;89:44–50. doi: 10.1016/j.humpath.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 26.Du L., Kim J.J., Shen J., Chen B., Dai N. KRAS and TP53 mutations in inflammatory bowel disease-associated colorectal cancer: A meta-analysis. Oncotarget. 2017;8:22175–22186. doi: 10.18632/oncotarget.14549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rao C.V., Swamy M.V., Patlolla J.M., Kopelovich L. Suppression of familial adenomatous polyposis by CP-31398, a TP53 modulator, in APCmin/+ mice. Cancer Res. 2008;68:7670–7675. doi: 10.1158/0008-5472.CAN-08-1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Narayanankutty A. PI3K/Akt/mTOR Pathway as a Therapeutic Target for Colorectal Cancer: A Review of Preclinical and Clinical Evidence. Curr. Drug Targets. 2019;20:1217–1226. doi: 10.2174/1389450120666190618123846. [DOI] [PubMed] [Google Scholar]
- 29.Saglam O., Garrett C.R., Boulware D., Sayegh Z., Shibata D., Malafa M., Yeatman T., Cheng J.Q., Sebti S., Coppola D. Activation of the serine/threonine protein kinase AKT during the progression of colorectal neoplasia. Clin. Colorectal Cancer. 2007;6:652–656. doi: 10.3816/CCC.2007.n.034. [DOI] [PubMed] [Google Scholar]
- 30.Roy H.K., Olusola B.F., Clemens D.L., Karolski W.J., Ratashak A., Lynch H.T., Smyrk T.C. AKT proto-oncogene overexpression is an early event during sporadic colon carcinogenesis. Carcinogenesis. 2002;23:201–205. doi: 10.1093/carcin/23.1.201. [DOI] [PubMed] [Google Scholar]
- 31.Lara P.N., Jr., Longmate J., Mack P.C., Kelly K., Socinski M.A., Salgia R., Gitlitz B., Li T., Koczywas M., Reckamp K.L., et al. Phase II Study of the AKT Inhibitor MK-2206 plus Erlotinib in Patients with Advanced Non-Small Cell Lung Cancer Who Previously Progressed on Erlotinib. Clin. Cancer Res. 2015;21:4321–4326. doi: 10.1158/1078-0432.CCR-14-3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sano H., Kawahito Y., Wilder R.L., Hashiramoto A., Mukai S., Asai K., Kimura S., Kato H., Kondo M., Hla T. Expression of cyclooxygenase-1 and -2 in human colorectal cancer. Cancer Res. 1995;55:3785–3789. [PubMed] [Google Scholar]
- 33.Gupta R.A., Dubois R.N. Colorectal cancer prevention and treatment by inhibition of cyclooxygenase-2. Nat. Rev. Cancer. 2001;1:11–21. doi: 10.1038/35094017. [DOI] [PubMed] [Google Scholar]
- 34.Femia A.P., Dolara P., Luceri C., Salvadori M., Caderni G. Mucin-depleted foci show strong activation of inflammatory markers in 1,2-dimethylhydrazine-induced carcinogenesis and are promoted by the inflammatory agent sodium dextran sulfate. Int. J. Cancer. 2009;125:541–547. doi: 10.1002/ijc.24417. [DOI] [PubMed] [Google Scholar]
- 35.Negi R.R., Rana S.V., Gupta V., Gupta R., Chadha V.D., Prasad K.K., Dhawan D.K. Over-Expression of Cyclooxygenase-2 in Colorectal Cancer Patients. Asian Pac. J. Cancer Prev. 2019;20:1675–1681. doi: 10.31557/APJCP.2019.20.6.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roelofs H.M., Te Morsche R.H., van Heumen B.W., Nagengast F.M., Peters W.H. Over-expression of COX-2 mRNA in colorectal cancer. BMC Gastroenterol. 2014;2:14. doi: 10.1186/1471-230X-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cossiolo D.C., Costa H.C.M., Fernandes K.B.P., Laranjeira L.L.S., Fernandes M.T.P., Poli-Frederico R.C. Polymorphism of the COX-2 gene and susceptibility to colon and rectal cancer. Arq. Bras. Cir. Dig. 2017;30:114–117. doi: 10.1590/0102-6720201700020008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Katona B.W., Weiss J.M. Chemoprevention of Colorectal Cancer. Gastroenterology. 2020;158:368–388. doi: 10.1053/j.gastro.2019.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mohammed A., Yarla N.S., Madka V., Rao C.V. Clinically Relevant Anti-Inflammatory Agents for Chemoprevention of Colorectal Cancer: New Perspectives. Int. J. Mol. Sci. 2018;19:2332. doi: 10.3390/ijms19082332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loomans-Kropp H.A., Umar A. Cancer prevention and screening: The next step in the era of precision medicine. NPJ Precis Oncol. 2019;28:3. doi: 10.1038/s41698-018-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drew D.A., Cao Y., Chan A.T. Aspirin and colorectal cancer: The promise of precision chemoprevention. Nat. Rev. Cancer. 2016;16:173–186. doi: 10.1038/nrc.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chan A.T., Ogino S., Fuchs C.S. Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N. Engl. J. Med. 2007;356:2131–2142. doi: 10.1056/NEJMoa067208. [DOI] [PubMed] [Google Scholar]
- 43.Mehta R.S., Song M., Bezawada N., Wu K., Garcia-Albeniz X., Morikawa T., Fuchs C.S., Ogino S., Giovannucci E.L., Chan A.T. A prospective study of macrophage inhibitory cytokine-1 (MIC-1/GDF15) and risk of colorectal cancer. J. Natl. Cancer Inst. 2014;106:dju016. doi: 10.1093/jnci/dju016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.JAMA United States Preventative Services Task Force Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:2564–2575. doi: 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 45.Nakanishi M., Montrose D.C., Clark P., Nambiar P.R., Belinsky G.S., Claffey K.P., Xu D., Rosenberg D.W. Genetic Deletion of mPGES-1 Suppresses Intestinal Tumorigenesis. Cancer Res. 2008;68:3251–3259. doi: 10.1158/0008-5472.CAN-07-6100. [DOI] [PubMed] [Google Scholar]
- 46.Sasaki Y., Kamei D., Ishikawa Y., Ishii T., Uematsu S., Akira S., Murakami M., Hara S. Microsomal prostaglandin E synthase-1 is involved in multiple steps of colon carcinogenesis. Oncogene. 2012;31:2943–2952. doi: 10.1038/onc.2011.472. [DOI] [PubMed] [Google Scholar]
- 47.Yang D.H., Ryu Y.M., Lee S.M., Jeong J.Y., Yoon S.M., Ye B.D., Byeon J.S., Yang S.K., Myung S.J. 15-Hydroxyprostaglandin dehydrogenase as a marker in colon carcinogenesis: Analysis of the prostaglandin pathway in human colonic tissue. Intest. Res. 2017;15:75–82. doi: 10.5217/ir.2017.15.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kamei D., Murakami M., Nakatani Y., Ishikawa Y., Ishii T., Kudo I. Potential role of microsomal prostaglandin E synthase-1 in tumorigenesis. J. Biol. Chem. 2003;278:19396–19405. doi: 10.1074/jbc.M213290200. [DOI] [PubMed] [Google Scholar]
- 49.Melstrom L.G., Bentrem D.J., Salabat M.R., Kennedy T.J., Ding X.Z., Strouch M., Rao S.M., Witt R.C., Ternent C.A., Talamonti M.S., et al. Overexpression of 5-lipoxygenase in colon polyps and cancer and the effect of 5-LOX inhibitors in vitro and in a murine model. Clin. Cancer Res. 2008;14:6525–6530. doi: 10.1158/1078-0432.CCR-07-4631. [DOI] [PubMed] [Google Scholar]
- 50.Wasilewicz M.P., Kołodziej B., Bojułko T., Kaczmarczyk M., Sulzyc-Bielicka V., Bielicki D., Ciepiela K. Overexpression of 5-lipoxygenase in sporadic colonic adenomas and a possible new aspect of colon carcinogenesis. Int. J. Colorectal Dis. 2010;25:1079–1085. doi: 10.1007/s00384-010-0980-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shureiqi I., Lippman S.M. Lipoxygenase modulation to reverse carcinogenesis. Cancer Res. 2001;61:6307–6312. [PubMed] [Google Scholar]
- 52.Takahashi M., Wakabayashi K. Gene mutations and altered gene expression in azoxymethane-induced colon carcinogenesis in rodents. Cancer Sci. 2004;95:475–480. doi: 10.1111/j.1349-7006.2004.tb03235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cianchi F., Cortesini C., Fantappiè O., Messerini L., Schiavone N., Vannacci A., Nistri S., Sardi I., Baroni G., Marzocca C., et al. Inducible nitric oxide synthase expression in human colorectal cancer: Correlation with tumor angiogenesis. Am. J. Pathol. 2003;162:793–801. doi: 10.1016/S0002-9440(10)63876-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zafirellis K., Zachaki A., Agrogiannis G., Gravani K. Inducible nitric oxide synthase expression and its prognostic significance in colorectal cancer. APMIS. 2010;118:115–124. doi: 10.1111/j.1600-0463.2009.02569.x. [DOI] [PubMed] [Google Scholar]
- 55.Kangwan N., Kim Y., Han Y.M., Jeong M., Park J.M., Hahm K.B. Concerted actions of ameliorated colitis, aberrant crypt foci inhibition and 15-hydroxyprostaglandin dehydrogenase induction by sonic hedgehog inhibitor led to prevention of colitis-associated cancer. Int. J. Cancer. 2016;138:1482–1493. doi: 10.1002/ijc.29892. [DOI] [PubMed] [Google Scholar]
- 56.Kang P.S., Kim J.H., Moon O.I., Lim S.C., Kim K.J. Prognostic implication of 15-hydroxyprostaglandin dehydrogenase down-regulation in patients with colorectal cancer. J. Korean Soc. Coloproctol. 2012;28:253–258. doi: 10.3393/jksc.2012.28.5.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dai Y., Jiao H., Teng G., Wang W., Zhang R., Wang Y., Hebbard L., George J., Qiao L. Embelin reduces colitis-associated tumorigenesis through limiting IL-6/STAT3 signaling. Mol. Cancer Ther. 2014;13:1206–1216. doi: 10.1158/1535-7163.MCT-13-0378. [DOI] [PubMed] [Google Scholar]
- 58.Li M.X., Bi X.Y., Huang Z., Zhao J.J., Han Y., Li Z.Y., Zhang Y.F., Li Y., Chen X., Hu X.H., et al. Prognostic role of phospho-STAT3 in patients with cancers of the digestive system: A systematic review and meta-analysis. PLoS ONE. 2015;10:e0127356. doi: 10.1371/journal.pone.0127356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sasaki Y., Kamiyama S., Kamiyama A., Matsumoto K., Akatsu M., Nakatani Y., Kuwata H., Ishikawa Y., Ishii T., Yokoyama C., et al. Genetic-deletion of Cyclooxygenase-2 Downstream Prostacyclin Synthase Suppresses Inflammatory Reactions but Facilitates Carcinogenesis, unlike Deletion of Microsomal Prostaglandin E Synthase-1. Sci. Rep. 2015;5:17376. doi: 10.1038/srep17376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Poole E.M., Bigler J., Whitton J., Sibert J.G., Potter J.D., Ulrich C.M. Prostacyclin synthase and arachidonate 5-lipoxygenase polymorphisms and risk of colorectal polyps. Cancer Epidemiol. Biomark. Prev. 2006;15:502–508. doi: 10.1158/1055-9965.EPI-05-0804. [DOI] [PubMed] [Google Scholar]
- 61.Rigas B., Goldman I.S., Levine L. Altered eicosanoid levels in human colon cancer. J. Lab. Clin. Med. 1993;122:518–523. [PubMed] [Google Scholar]
- 62.Zuo X., Peng Z., Wu Y., Moussalli M.J., Yang X.L., Wang Y., Parker-Thornburg J., Morris J.S., Broaddus R.R., Fischer S.M., et al. Effects of gut-targeted 15-LOX-1 transgene expression on colonic tumorigenesis in mice. J. Natl. Cancer Inst. 2012;104:709–716. doi: 10.1093/jnci/djs187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mao F., Xu M., Zuo X., Yu J., Xu W., Moussalli M.J., Elias E., Li H.S., Watowich S.S., Shureiqi I. 15-Lipoxygenase-1 suppression of colitis-associated colon cancer through inhibition of the IL-6/STAT3 signaling pathway. FASEB J. 2015;29:2359–2370. doi: 10.1096/fj.14-264515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tian R., Zuo X., Jaoude J., Mao F., Colby J., Shureiqi I. ALOX15 as a suppressor of inflammation and cancer: Lost in the link. Prostaglandins Other Lipid Mediat. 2017;132:77–83. doi: 10.1016/j.prostaglandins.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Erdman S.H., Ignatenko N.A., Powell M.B., Blohm-Mangone K.A., Holubec H., Guillén-Rodriguez J.M., Gerner E.W. APC-dependent changes in expression of genes influencing polyamine metabolism, and consequences for gastrointestinal carcinogenesis, in the Min mouse. Carcinogenesis. 1999;20:1709–1713. doi: 10.1093/carcin/20.9.1709. [DOI] [PubMed] [Google Scholar]
- 66.Hoshino Y., Terashima S., Teranishi Y., Terashima M., Kogure M., Saitoh T., Osuka F., Kashimura S., Saze Z., Gotoh M. Ornithine decarboxylase activity as a prognostic marker for colorectal cancer. Fukushima J. Med. Sci. 2007;53:1–9. doi: 10.5387/fms.53.1. [DOI] [PubMed] [Google Scholar]
- 67.Zell J.A., Ziogas A., Ignatenko N., Honda J., Qu N., Bobbs A.S., Neuhausen S.L., Gerner E.W., Anton-Culver H. Associations of a polymorphism in the ornithine decarboxylase gene with colorectal cancer survival. Clin. Cancer Res. 2009;15:6208–6216. doi: 10.1158/1078-0432.CCR-09-0592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Takami H., Koudaira H., Kodaira S. Relationship of ornithinedecarboxylase activity and human colon tumorigenesis. Jpn. J. Clin. Oncol. 1994;24:141–143. [PubMed] [Google Scholar]
- 69.Wei T.T., Lin Y.T., Chen W.S., Luo P., Lin Y.C., Shun C.T., Lin Y.H., Chen J.B., Chen N.W., Fang J.M., et al. Dual Targeting of 3-Hydroxy-3-methylglutaryl Coenzyme A Reductase and Histone Deacetylase as a Therapy for Colorectal Cancer. EBioMedicine. 2016;10:124–136. doi: 10.1016/j.ebiom.2016.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barone M., Notarnicola M., Caruso M.G., Scavo M.P., Viggiani M.T., Tutino V., Polimeno L., Pesetti B., Di Leo A., Francavilla A. Olive oil and omega-3 polyunsaturated fatty acids suppress intestinal polyp growth by modulating the apoptotic process in ApcMin/+ mice. Carcinogenesis. 2014;35:1613–1619. doi: 10.1093/carcin/bgu068. [DOI] [PubMed] [Google Scholar]
- 71.Bengtsson E., Nerjovaj P., Wangefjord S., Nodin B., Eberhard J., Uhlén M., Borgquist S., Jirström K. HMG-CoA reductase expression in primary colorectal cancer correlates with favourable clinicopathological characteristics and an improved clinical outcome. Diagn. Pathol. 2014;9:78. doi: 10.1186/1746-1596-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cruz M.D., Wali R.K., Bianchi L.K., Radosevich A.J., Crawford S.E., Jepeal L., Goldberg M.J., Weinstein J., Momi N., Roy P., et al. Colonic mucosal fatty acid synthase as an early biomarker for colorectal neoplasia: Modulation by obesity and gender. Cancer Epidemiol. Biomark. Prev. 2014;23:2413–2421. doi: 10.1158/1055-9965.EPI-14-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kearney K.E., Pretlow T.G., Pretlow T.P. Increased expression of fatty acid synthase in human aberrant crypt foci: Possible target for colorectal cancer prevention. Int. J. Cancer. 2009;125:249–252. doi: 10.1002/ijc.24356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nakanishi M., Menoret A., Tanaka T., Miyamoto S., Montrose D.C., Vella A.T., Rosenberg D.W. Selective PGE(2) suppression inhibits colon carcinogenesis and modifies local mucosal immunity. Cancer Prev. Res. 2011;4:1198–1208. doi: 10.1158/1940-6207.CAPR-11-0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li Y.C., Wang D.X., Li C.S., Ye Z.P., Wu Z.M., Chen J.H. Association of 5-lipoxygenase expression and clinicopathological factors in colorectal carcinoma. Zhonghua Wei Chang. Wai Ke Za Zhi. 2013;16:895–897. [PubMed] [Google Scholar]
- 76.Gounaris E., Heiferman M.J., Heiferman J.R., Shrivastav M., Vitello D., Blatner N.R., Knab L.M., Phillips J.D., Cheon E.C., Grippo P.J., et al. Zileuton, 5-lipoxygenase inhibitor, acts as a chemopreventive agent in intestinal polyposis, by modulating polyp and systemic inflammation. PLoS ONE. 2015;10:e0121402. doi: 10.1371/journal.pone.0121402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cutler N.S., Graves-Deal R., LaFleur B.J., Gao Z., Boman B.M., Whitehead R.H., Terry E., Morrow J.D., Coffey R.J. Stromal production of prostacyclin confers an antiapoptotic effect to colonic epithelial cells. Cancer Res. 2003;63:1748–1751. [PubMed] [Google Scholar]
- 78.Frigola J., Muñoz M., Clark S.J., Moreno V., Capellà G., Peinado M.A. Hypermethylation of the prostacyclin synthase (PTGIS) promoter is a frequent event in colorectal cancer and associated with aneuploidy. Oncogene. 2005;24:7320–7326. doi: 10.1038/sj.onc.1208883. [DOI] [PubMed] [Google Scholar]
- 79.Wang J., Cho N.L., Zauber A.G., Hsu M., Dawson D., Srivastava A., Mitchell-Richards K.A., Markowitz S.D., Bertagnolli M.M. The expression of Cox-2 and 15-PGDH in pre-treatment adenomas provides predictive information in patients treated with celecoxib for prevention of colorectal adenomas. Cancer Epidemiol. Biomark. Prev. 2018;27:728–736. doi: 10.1158/1055-9965.EPI-17-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Backlund M.G., Mann J.R., Holla V.R., Shi Q., Daikoku T., Dey S.K., DuBois R.N. Repression of 15-hydroxyprostaglandin dehydrogenase involves histone deacetylase 2 and snail in colorectal cancer. Cancer Res. 2008;68:9331–9337. doi: 10.1158/0008-5472.CAN-08-2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gilligan M.M., Gartung A., Sulciner M.L., Norris P.C., Sukhatme V.P., Bielenberg D.R., Huang S., Kieran M.W., Serhan C.N., Panigrahy D. Aspirin-triggered proresolving mediators stimulate resolution in cancer. Proc. Natl. Acad. Sci. USA. 2019;116:6292–6297. doi: 10.1073/pnas.1804000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cimen I., Astarci E., Banerjee S. 15-lipoxygenase-1 exerts its tumor suppressive role by inhibiting nuclear factor-kappa B via activation of PPAR gamma. J. Cell Biochem. 2011;112:2490–2501. doi: 10.1002/jcb.23174. [DOI] [PubMed] [Google Scholar]
- 83.Cimen I., Tunçay S., Banerjee S. 15-Lipoxygenase-1 expression suppresses the invasive properties of colorectal carcinoma cell lines HCT-116 and HT-29. Cancer Sci. 2009;100:2283–2291. doi: 10.1111/j.1349-7006.2009.01313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tunçer S., Tunçay Ç.S., Keşküş A.G., Çolakoğlu M., Konu Ö., Banerjee S. Interplay between 15-lipoxygenase-1 and metastasis-associated antigen 1 in the metastatic potential of colorectal cancer. Cell Prolif. 2016;49:448–459. doi: 10.1111/cpr.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tunçer S., Keşküş A.G., Çolakoğlu M., Çimen I., Yener C., Konu Ö., Banerjee S. 15-Lipoxygenase-1 re-expression in colorectal cancer alters endothelial cell features through enhanced expression of TSP-1 and ICAM-1. Cell. Signal. 2017;39:44–54. doi: 10.1016/j.cellsig.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 86.Yoshinaga M., Murao H., Kitamura Y., Koga K., Tsuruta S., Igarashi H., Nakamura K., Takayanagi R. The 15-lipoxygenase-1 expression may enhance the sensitivity to non-steroidal anti-inflammatory drug-induced apoptosis in colorectal cancers from patients who are treated with the compounds. J. Gastroenterol. Hepatol. 2007;22:2324–2329. doi: 10.1111/j.1440-1746.2007.04842.x. [DOI] [PubMed] [Google Scholar]
- 87.Xu M.H., Deng C.S., Zhu Y.Q., Lin J. Role of inducible nitric oxide synthase expression in aberrant crypt foci-adenoma-carcinoma sequence. World J. Gastroenterol. 2003;9:1246–1250. doi: 10.3748/wjg.v9.i6.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Aoi W., Naito Y., Takagi T., Kokura S., Mizushima K., Takanami Y., Kawai Y., Tanimura Y., Hung L.P., Koyama R., et al. Regular exercise reduces colon tumorigenesis associated with suppression of iNOS. Biochem. Biophys. Res. Commun. 2010;399:14–19. doi: 10.1016/j.bbrc.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 89.Hofseth L.J., Hussain S.P., Wogan G.N., Harris C.C. Nitric oxide in cancer and chemoprevention. Free Radic. Biol. Med. 2003;34:955–968. doi: 10.1016/S0891-5849(02)01363-1. [DOI] [PubMed] [Google Scholar]
- 90.Crowell J.A., Steele V.E., Sigman C.C., Fay J.R. Is inducible nitric oxide synthase a target for chemoprevention? Mol. Cancer Ther. 2003;2:815–823. [PubMed] [Google Scholar]
- 91.Ahn B., Ohshima H. Suppression of intestinal polyposis in ApcMin/+ mice by inhibiting nitric oxide production. Cancer Res. 2001;61:8357–8360. [PubMed] [Google Scholar]
- 92.Gao Y., Zhou S., Xu Y., Sheng S., Qian S.Y., Huo X. Nitric oxide synthase inhibitors 1400W and L-NIO inhibit angiogenesis pathway of colorectal cancer. Nitric Oxide. 2019;83:33–39. doi: 10.1016/j.niox.2018.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Atreya R., Neurath M.F. Signaling molecules: The pathogenic role of the IL-6/STAT-3 trans signaling pathway in intestinal inflammation and in colonic cancer. Curr. Drug Targets. 2008;9:369–374. doi: 10.2174/138945008784221116. [DOI] [PubMed] [Google Scholar]
- 94.Wei X., Wang G., Li W., Hu X., Huang Q., Xu K., Lou W., Wu J., Liang C., Lou Q., et al. Activation of the JAK-STAT3 pathway is associated with the growth of colorectal carcinoma cells. Oncol. Rep. 2014;31:335–341. doi: 10.3892/or.2013.2858. [DOI] [PubMed] [Google Scholar]
- 95.Janakiram N.B., Mohammed A., Bryant T., Brewer M., Biddick L., Lightfoot S., Lang M.L., Rao C.V. Adoptive transfer of regulatory T cells promotes intestinal tumorigenesis and is associated with decreased NK cells and IL-22 binding protein. Mol. Carcinog. 2015;54:986–998. doi: 10.1002/mc.22168. [DOI] [PubMed] [Google Scholar]
- 96.Chen L., Jiang B., Zhong C., Guo J., Zhang L., Mu T., Zhang Q., Bi X. Chemoprevention of colorectal cancer by black raspberry anthocyanins involved the modulation of gut microbiota and SFRP2 demethylation. Carcinogenesis. 2018;39:471–481. doi: 10.1093/carcin/bgy009. [DOI] [PubMed] [Google Scholar]
- 97.Sasaki S., Baba T., Shinagawa K., Matsushima K., Mukaida N. Crucial involvement of the CCL3-CCR5 axis-mediated fibroblast accumulation in colitis-associated carcinogenesis in mice. Int. J. Cancer. 2014;135:1297–1306. doi: 10.1002/ijc.28779. [DOI] [PubMed] [Google Scholar]
- 98.Löfroos A.B., Kadivar M., Resic L.S., Marsal J. Colorectal cancer-infiltrating T lymphocytes display a distinct chemokine receptor expression profile. Eur. J. Med. Res. 2017;22:40. doi: 10.1186/s40001-017-0283-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Xing J., Li X., Sui J., Cao G., Fu C. C-X-C chemokine receptor type 5 gene polymorphism affects gene expression in CD4+ T cells and is associated with increased risk of colorectal cancer. Tumour. Biol. 2014;35:7929–7934. doi: 10.1007/s13277-014-2069-8. [DOI] [PubMed] [Google Scholar]
- 100.Tanabe Y., Sasaki S., Mukaida N., Baba T. Blockade of the chemokine receptor, CCR5, reduces the growth of orthotopically injected colon cancer cells via limiting cancer-associated fibroblast accumulation. Oncotarget. 2016;7:48335–48345. doi: 10.18632/oncotarget.10227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Halama N., Zoernig I., Berthel A., Kahlert C., Klupp F., Suarez-Carmona M., Suetterlin T., Brand K., Krauss J., Lasitschka F., et al. Tumoral Immune Cell Exploitation in Colorectal Cancer Metastases Can Be Targeted Effectively by Anti-CCR5 Therapy in Cancer Patients. Cancer Cell. 2016;29:587–601. doi: 10.1016/j.ccell.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 102.Jafari N., Drury J., Morris A.J., Onono F.O., Stevens P.D., Gao T., Liu J., Wang C., Lee E.Y., Weiss H.L., et al. De Novo Fatty Acid Synthesis-Driven Sphingolipid Metabolism Promotes Metastatic Potential of Colorectal Cancer. Mol. Cancer Res. 2019;17:140–152. doi: 10.1158/1541-7786.MCR-18-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yekaterina Y., Piotr G.R., Tianyan G., Eun Y.L., Heidi L.W., Timothy S.H., George K., Mark B.E. Evaluation of small-molecule FASN inhibitors in preclinical models of colorectal cancer; Proceedings of the 107th Annual Meeting of the American Association for Cancer Research; New Orleans, LA, USA. 16–20 April 2016; Philadelphia, PA, USA: AACR; 2016. [Google Scholar]
- 104.Zaytseva Y.Y., Rychahou P.G., Le A.T., Scott T.L., Flight R.M., Kim J.T., Harris J., Liu J., Wang C., Morris A.J., et al. Preclinical evaluation of novel fatty acid synthase inhibitors in primary colorectal cancer cells and a patient-derived xenograft model of colorectal cancer. Oncotarget. 2018;9:24787–24800. doi: 10.18632/oncotarget.25361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Long Q.Q., Yi Y.X., Qiu J., Xu C.J., Huang P.L. Fatty acid synthase (FASN) levels in serum of colorectal cancer patients: Correlation with clinical outcomes. Tumor. Biol. 2014;35:3855–3859. doi: 10.1007/s13277-013-1510-8. [DOI] [PubMed] [Google Scholar]
- 106.Clinical Trial Identification Number. [(accessed on 10 January 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02980029.
- 107.Wang H., Xi Q., Wu G. Fatty acid synthase regulates invasion and metastasis of colorectal cancer via Wnt signaling pathway. Cancer Med. 2016;5:1599–1606. doi: 10.1002/cam4.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zaytseva Y.Y., Rychahou P.G., Gulhati P., Elliott V.A., Mustain W.C., O’Connor K., Morris A.J., Sunkara M., Weiss H.L., Lee E.Y., et al. Inhibition of fatty acid synthase attenuates CD44-associated signaling and reduces metastasis in colorectal cancer. Cancer Res. 2012;72:1504–1517. doi: 10.1158/0008-5472.CAN-11-4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kuchiba A., Morikawa T., Yamauchi M., Imamura Y., Liao X., Chan A.T., Meyerhardt J.A., Giovannucci E., Fuchs C.S., Ogino S. Body mass index and risk of colorectal cancer according to fatty acid synthase expression in the nurses’ health study. J. Natl. Cancer Inst. 2012;104:415–420. doi: 10.1093/jnci/djr542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chang L., Wu P., Senthilkumar R., Tian X., Liu H., Shen X., Tao Z., Huang P. Loss of fatty acid synthase suppresses the malignant phenotype of colorectal cancer cells by down-regulating energy metabolism and mTOR signaling pathway. J. Cancer Res. Clin. Oncol. 2016;142:59–72. doi: 10.1007/s00432-015-2000-8. [DOI] [PubMed] [Google Scholar]
- 111.Meyskens F.L., Emerson S.S., Pelot D., Meshkinpour H., Shassetz L.R., Einspahr J., Alberts D.S., Gerner E.W. Dose de-escalation chemoprevention trial of α-difluoromethylornithine in patients with colon polyps. J. Natl. Cancer Inst. 1994;86:1122–1130. doi: 10.1093/jnci/86.15.1122. [DOI] [PubMed] [Google Scholar]
- 112.Meyskens F.L., McLaren C.E., Pelot D., Fujikawa-Brooks S., Carpenter P.M., Hawk E., Kelloff G., Lawson M.J., Kidao J., McCracken J., et al. Difluoromethylornithine plus sulindac for the prevention of sporadic colorectal adenomas: A randomized placebo-controlled, double-blind trial. Cancer Prev. Res. 2008;1:32–38. doi: 10.1158/1940-6207.CAPR-08-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Danzin C., Mamont P.S. Polyamine inhibition in vivo and in organ growth and repair. In: McCann P.P., Pegg A.E., Sjoerdsma A., editors. Inhibition of Polyamine Metabolism. Academic Press; New York, NY, USA: 1987. pp. 141–164. [Google Scholar]
- 114.Janakiram N.B., Mohammed A., Bryant T., Zhang Y., Brewer M., Duff A., Biddick L., Singh A., Lightfoot S., Steele V.E., et al. Potentiating NK cell activity by combination of Rosuvastatin and Difluoromethylornithine for effective chemopreventive efficacy against Colon Cancer. Sci. Rep. 2016;6:37046. doi: 10.1038/srep37046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rao C.V., Tokumo K., Rigotty J., Zang E., Kelloff G., Reddy B.S. Chemoprevention of colon carcinogenesis by dietary administration of piroxicam, alpha-difluoromethylornithine, 16 alpha-fluoro-5-androsten-17-one, and ellagic acid individually and in combination. Cancer Res. 1991;51:4528–4534. [PubMed] [Google Scholar]
- 116.Kumar K.N., Raja S.B., Vidhya N., Devaraj S.N. Ellagic acid modulates antioxidant status, ornithine decarboxylase expression, and aberrant crypt foci progression in 1,2-dimethylhydrazine-instigated colon preneoplastic lesions in rats. J. Agric. Food Chem. 2012;60:3665–3672. doi: 10.1021/jf204128z. [DOI] [PubMed] [Google Scholar]
- 117.Li Y., He X., Ding Y., Chen H., Sun L. Statin uses and mortality in colorectal cancer patients: An updated systematic review and meta-analysis. Cancer Med. 2019;8:3305–3313. doi: 10.1002/cam4.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Karagkounis G., DeVecchio J., Ferrandon S., Kalady M.F. Simvastatin enhances radiation sensitivity of colorectal cancer cells. Surg. Endosc. 2018;32:1533–1539. doi: 10.1007/s00464-017-5841-1. [DOI] [PubMed] [Google Scholar]
- 119.Wei T.T., Lin Y.T., Tseng R.Y., Shun C.T., Lin Y.C., Wu M.S., Fang J.M., Chen C.C. Prevention of Colitis and Colitis-Associated Colorectal Cancer by a Novel Polypharmacological Histone Deacetylase Inhibitor. Clin. Cancer Res. 2018;24:499. doi: 10.1158/1078-0432.CCR-15-2379. [DOI] [PubMed] [Google Scholar]
- 120.Suh N., Reddy B.S., DeCastro A., Paul S., Lee H.J., Smolarek A.K., So J.Y., Simi B., Wang C.X., Janakiram N.B., et al. Combination of atorvastatin with sulindac or naproxen profoundly inhibits colonic adenocarcinomas by suppressing the p65/β-catenin/cyclin D1 signaling pathway in rats. Cancer Prev. Res. 2011;4:1895–1902. doi: 10.1158/1940-6207.CAPR-11-0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Swamy M.V., Patlolla J.M., Steele V.E., Kopelovich L., Reddy B.S., Rao C.V. Chemoprevention of familial adenomatous polyposis by low doses of atorvastatin and celecoxib given individually and in combination to APCMin mice. Cancer Res. 2006;66:7370–7377. doi: 10.1158/0008-5472.CAN-05-4619. [DOI] [PubMed] [Google Scholar]
- 122.Lipkin S.M., Chao E.C., Moreno V., Rozek L.S., Rennert H., Pinchev M., Dizon D., Rennert G., Kopelovich L., Gruber S.B. Genetic variation in 3-hydroxy-3-methylglutaryl CoA reductase modifies the chemopreventive activity of statins for colorectal cancer. Cancer Prev. Res. 2010;3:597–603. doi: 10.1158/1940-6207.CAPR-10-0007. [DOI] [PubMed] [Google Scholar]
- 123.Ricciardiello L., Ahnen D.J., Lynch P.M. Chemoprevention of hereditary colon cancers: Time for new strategies. Nat. Rev. Gastroenterol. Hepatol. 2016;13:352–361. doi: 10.1038/nrgastro.2016.56. [DOI] [PubMed] [Google Scholar]
- 124.Clinical Trial Identification Number. [(accessed on 10 January 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02301286.
- 125.Seo T., Tatsuguchi A., Shinji S., Yonezawa M., Mitsui K., Tanaka S., Fujimori S., Gudis K., Fukuda Y., Sakamoto C. Microsomal prostaglandin E synthase protein levels correlate with prognosis in colorectal cancer patients. Virchows Arch. 2009;454:667–676. doi: 10.1007/s00428-009-0777-z. [DOI] [PubMed] [Google Scholar]
- 126.Reddy B.S., Hirose Y., Lubet R., Steele V., Kelloff G., Paulson S., Seibert K., Rao C.V. Chemoprevention of colon cancer by specific cyclooxygenase-2 inhibitor, celecoxib, administered during different stages of carcinogenesis. Cancer Res. 2000;60:293–297. [PubMed] [Google Scholar]
- 127.Li P., Wu H., Zhang H., Shi Y., Xu J., Ye Y., Xia D., Yang J., Cai J., Wu Y. Aspirin use after diagnosis but not prediagnosis improves established colorectal cancer survival: A meta-analysis. Gut. 2015;64:1419–1425. doi: 10.1136/gutjnl-2014-308260. [DOI] [PubMed] [Google Scholar]
- 128.De Robertis M., Massi E., Poeta M.L., Carotti S., Morini S., Cecchetelli L., Signori E., Fazio V.M. The AOM/DSS murine model for the study of colon carcinogenesis: From pathways to diagnosis and therapy studies. J. Carcinog. 2011;10:9. doi: 10.4103/1477-3163.78279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zeineldin M., Neufeld K.L. More than two decades of Apc modeling in rodents. Biochim. Biophys. Acta. 2013;1836:80–89. doi: 10.1016/j.bbcan.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tetteh P.W., Kretzschmar K., Begthel H., van den Born M., Korving J., Morsink F., Farin H., van Es J.H., Offerhaus G.J., Clevers H. Generation of an inducible colon-specific Cre enzyme mouse line for colon cancer research. Proc. Natl. Acad. Sci. USA. 2016;113:11859–11864. doi: 10.1073/pnas.1614057113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Femia A.P., Luceri C., Soares P.V., Lodovici M., Caderni G. Multiple mucin depleted foci, high proliferation and low apoptotic response in the onset of colon carcinogenesis of the PIRC rat, mutated in Apc. Int. J. Cancer. 2015;136:E488–E495. doi: 10.1002/ijc.29232. [DOI] [PubMed] [Google Scholar]
- 132.Navarra M., Femia A.P., Romagnoli A., Tortora K., Luceri C., Cirmi S., Ferlazzo N., Caderni G. A flavonoid-rich extract from bergamot juice prevents carcinogenesis in a genetic model of colorectal cancer, the Pirc rat (F344/NTac-Apcam1137) Eur. J. Nutr. 2020;59:885–894. doi: 10.1007/s00394-019-01948-z. [DOI] [PubMed] [Google Scholar]
- 133.Tong Y., Yang W., Koeffler H.P. Mouse models of colorectal cancer. Chin. J. Cancer. 2011;30:450–462. doi: 10.5732/cjc.011.10041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Taketo M.M., Edelmann W. Mouse models of colon cancer. Gastroenterology. 2009;136:780–798. doi: 10.1053/j.gastro.2008.12.049. [DOI] [PubMed] [Google Scholar]
- 135.Young M., Ordonez L., Clarke A.R. What are the best routes to effectively model human colorectal cancer? Mol. Oncol. 2013;7:178–189. doi: 10.1016/j.molonc.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Oliveira R.C., Abrantes A.M., Tralhao J.G., Botelho M.F. The role of mouse models in colorectal cancer research-The need and the importance of the orthotopic models. Anim. Models Exp. Med. 2020;3:1–8. doi: 10.1002/ame2.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Inoue A., Deem A.K., Kopetz S., Heffernan T.P., Draetta G.F., Carugo A. Current and Future Horizons of Patient-Derived Xenograft Models in Colorectal Cancer Translational Research. Cancers. 2019;11:1321. doi: 10.3390/cancers11091321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yarla N.S., Pathuri G., Gali H., Panneerselvam J., Chandrakesan P., Madka V., Rao C.V. LFA-9, a Selective Inhibitor of Microsomal Prostaglandin Synthase-1 and 5-Lipoxygenase. Prev. Inflamm. Oncol. Dis. 2020;34:S1. doi: 10.1096/fasebj.2020.34.s1.00079. [DOI] [Google Scholar]