Abstract
Simple Summary
Research into the causes and potential treatments for cancer-related cognitive impairment has increased greatly over the past several years. Advances have been made in studies related to human neuropsychology and animal models of behavior. Findings from both types of studies implicate a role of the genetic risk factor APOE4 in cancer-related cognitive impairment. APOE4 is the strongest genetic risk factor for Alzheimer’s disease, and this convergence across disparate research approaches now provides a great opportunity for insight into mechanisms of both conditions. This review provides an overview of potential mechanisms that could account for aspects of cancer-related cognitive impairment, and how they could be affected by the APOE genotype.
Abstract
Cancer related cognitive impairment (CRCI) is a serious impairment to maintaining quality of life in cancer survivors. Cancer chemotherapy contributes to this condition through several potential mechanisms, including damage to the blood brain barrier, increases in oxidative stress and inflammation in the brain, and impaired neurogenesis, each of which lead to neuronal dysfunction. A genetic predisposition to CRCI is the E4 allele of the Apolipoprotein E gene (APOE), which is also the strongest genetic risk factor for Alzheimer’s disease. In normal brains, APOE performs essential lipid transport functions. The APOE4 isoform has been linked to altered lipid binding, increased oxidative stress and inflammation, reduced turnover of neural progenitor cells, and impairment of the blood brain barrier. As chemotherapy also affects these processes, the influence of APOE4 on CRCI takes on great significance. This review outlines the main areas where APOE genotype could play a role in CRCI. Potential therapeutics based on APOE biology could mitigate these detrimental cognitive effects for those receiving chemotherapy, emphasizing that the APOE genotype could help in developing personalized cancer treatment regimens.
Keywords: Apolipoprotein E, chemotherapy, cognitive impairment, APOE, Alzheimer’s disease, inflammation, blood brain barrier, neurogenesis
1. Introduction—Cancer Related Cognitive Impairment after Chemotherapy
While the increasing success in treating cancer improves survivorship, the detrimental effects of cancer chemotherapy on the central nervous system (CNS), including neurotoxicity and reduced cognitive ability, have been observed for decades [1,2,3,4,5]. Cancer related cognitive impairments (CRCI) affect memory, verbal ability, and executive functions [6,7]. Mitigating the CNS side effects would substantially improve prognoses by increasing quality of life [8,9,10,11]. While CRCI is a broad field that includes cognitive problems suffered by cancer patients regardless of treatment [12], this review will focus on the cognitive impairments induced after chemotherapy.
Gross CNS impacts after cancer treatments are observed in MRI scans [13]. Decreased gray matter density was found in patients one month after treatment, some of which persisted even one year later [14] and these changes to brain structures correlated with cognitive difficulties [15]. CRCI occurs in survivors of many cancers [16], although breast cancer survivors have been the most extensively characterized. Neuropsychological analyses of breast cancer survivors found that chemotherapy treatment was associated with significant reductions in verbal memory and psychomotor function persisting for up to 10 years [17]. Breast cancer survivors administered chemotherapy had significantly lower scores in visual memory and visuospatial function than survivors given local therapy and healthy controls [18]. Five to ten years post-treatment, breast cancer survivors who had completed systemic treatment with chemotherapy performed significantly worse on short term memory tasks, which correlated with reductions in the resting metabolism levels of several brain regions as measured by [F-18] fluorodeoxyglucose (FDG) positron emission tomography (PET) scans [19]. Cytostatic chemotherapies were also associated with structural changes in the white matter in regions of the brain involved in cognitive processes [20], which correlate with worse performance in verbal memory tests [20]. Over the long term, chemotherapy is associated with white matter deficiencies and reduced scores on cognitive tests, as well as gray matter alterations over nine years [21] and 21 years [22]. Overall, the cognitive impairments induced by chemotherapy are persistent and involve changes in brain structure and physiology.
Involvement of APOE in CRCI
It is unknown what factors predispose a person to CRCI, although several genetic studies have identified the APOE gene [5,23,24,25]. APOE is the strongest genetic risk factor for Alzheimer’s disease (AD) [26,27,28]. APOE encodes the apolipoprotein E protein, a 299 amino acid, secreted O-glycoprotein that transports lipids in the periphery and CNS [29]. In the CNS, APOE affects processes such as neuronal health, inflammation, oxidative stress, and clearance of the AD pathogenic protein Aβ [30,31,32]. APOE also plays important roles in the neurovascular system and the blood brain barrier [33], a structure crucial to preventing many chemotherapeutics direct access to the CNS. There are three APOE alleles that produce isoforms with single amino acid differences: APOE2 (Cys112, Cys158), APOE3 (Cys112, Arg158), and APOE4 (Arg112, Arg158). Compared to the most common APOE3 allele, APOE2 reduces risk of AD by up to 50% and APOE4 increases AD risk three-fold in heterozygotes and 14-fold in homozygotes [34]. APOE4 is common, with approximately a quarter of the US population carrying an APOE4 allele [35]. APOE4 allele frequencies differ across ethnicities around the world [36]: 14% in Caucasian Americans [35], up to 40% in African Americans [37], 10% in Japan and Italy [38,39], and up to 20% in Sweden [40].
Several studies have addressed the influence of the APOE genotype on risk of CRCI (described in Table 1). For breast cancer survivors treated with chemotherapy five years post diagnosis, APOE4 carriers had worse visual memory and spatial ability [23]. APOE4 breast cancer patients with no smoking history had significantly lower scores on measures of processing speed and working memory at 1, 6, and 18 months post-chemotherapy [24]. APOE4 carriers who received chemotherapy for testicular cancer had a significantly lower global cognitive score based on a battery of cognitive tests [25]. Finally, APOE4-positive breast cancer survivors assigned cytostatics had lower scores on tests measuring attention, processing speed and executive function, as well as learning and memory compared to controls or those given only hormone therapy, one to two years post-treatments [5]. Together, these studies show that the APOE genotype has an impact on cognitive decline following chemotherapy.
Table 1.
Clinical and pre-clinical studies showing effects of APOE4 on CRCI.
| Study | Study Design | Results |
|---|---|---|
| CLINICAL | ||
| Ahles et al., 2003 [23]. Long term survivors of breast cancer (8.8 years +/− 4.3 years post treatment) or lymphoma who had been treated with chemotherapy were given tests of cognition and stratified by the presence of at least one APOE4 allele. |
Breast cancer survivors (n = 51, age 55.9 +/− 8.8 years old), lymphoma survivors (n = 29 age 55.8 +/− 11.6). Together, 21% (n = 17) were APOE4 carriers. A neuropsychological battery of tests assessed cognition, including verbal and spatial ability, verbal and visual memory, psychomotor function, and attention. |
APOE4 carriers scored significantly lower in visual memory and spatial ability, with a trend toward lower psychomotor function. |
| Ahles et al., 2014 [24]. Breast cancer patients treated with chemotherapy were assessed with cognitive tests prior to treatment at 1, 6 and 18 months post-chemotherapy, and were compared to breast cancer patients not treated with chemotherapy as well as healthy controls. Smoking history was also evaluated. |
Chemotherapy treated breast cancer patients (n = 55, age 51.9 +/- 7.1; APOE carriers n = 14, 25%, had smoked n = 31, 56%). Non-chemotherapy treated breast cancer patients (n = 68, age 56.8+/− 8.3; APOE4 n = 18, 26%; smoked n = 43, 63%). Healthy controls (n = 43, age 53.0+/10.1; APOE4 n = 7, 16%; smoked n = 26, 60%). Individuals were evaluated for verbal ability and memory, visual and working memory, and processing speed. | Breast cancer patients who were APOE4 carriers without a smoking history had significantly lower performance on processing speed and working memory compared to smokers and healthy controls. APOE4 carriers without a smoking history who received chemotherapy had lower processing speed compared to those with a smoking history. |
| Mandleblatt et al., 2018 [5]. Newly diagnosed non-metastatic breast cancer survivors aged 60 years and older were matched controls without cancer. Cognitive measurements were collected before treatment at 12 and 24 months after treatment. |
Breast cancer survivors: Chemotherapy +/− hormone therapy n = 80; APOE4 n = 12 (15%). Hormonal Therapy alone n = 201; APOE4 n = 41 (20%). Healthy controls n = 322; APOE4 carriers n = 81 (25%). Individuals were tested for learning and memory (LM) and attention, processing speed and executive function (APE). |
Hormonal Therapy alone: APOE3 patients had no change in LM; APOE4 patients had a short term decrease. There was no change in APE with APOE genotype. Chemotherapy: There was no change in APE in APOE3 patients, but significant reduction in APOE4 carriers. |
| Amidi et al., 2017 [25]. Testicular cancer patients were assessed for cognition and grey matter (GM) morphology after surgery but prior to further treatment, and 6 months later. |
65 patients total, 22 received chemotherapy (age 31.9 +/− 9.4 years) and 43 did not (age 39.6 +/− 10.7). 20 of 61 (33%) patients with known APOE genotype were APOE4 positive. There were 25 healthy controls (age 32.8 +/− 11.1) tested for attention and working memory, processing speed, auditory learning and memory, verbal fluency and executive functions. | Testicular cancer patients had greater cognitive decline than healthy controls (p < 0.05). APOE4 carriers in cancer patients had significantly worse performance and had lower global composite score (p < 0.03) but did not have significant GM density changes. |
| PRECLINICAL | ||
| Speidell et al., 2018 [41]. Female homozygous APOE3 and APOE4 mice at 4–6 months were treated with doxorubicin or saline, and subjected to cognitive tests involving mazes that measure spatial learning and memory, as well as MRI scans to measure structural brain changes. |
APOE3 (n = 18) and APOE4 (n = 21) knock-in female C57BL/6J mice were used, most commonly used in studies of cognition based on good learning skills. Mice were treated with doxorubicin or saline, and spatial learning tests (Barnes maze) were performed 6 weeks post exposure, at 21 to 25 weeks of age. | APOE4 mice treated with doxorubicin had significantly reduced spatial and learning memory compared to APOE3 mice, which showed no impairment. There were significant MRI changes in the cortex and hippocampus after treatment, with similar patterns in both APOE genotypes, more pronounced in APOE4. |
| Demby et al., 2020 [42]. Female aged (12 months old) homozygous APOE3 or APOE4 mice were treated with doxorubicin or saline, and then subjected to cognitive and behavioral assays, and MRI scans were performed to detect regional brain volume differences. |
APOE3 (n = 30) and APOE4 (n = 31) knock-in female C57BL/6J mice were used, and measures taken at 31–35 weeks post-exposure. Spatial and memory tests were analyzed via the Barnes maze, and tissue sections stained for markers of AD pathogenesis. | APOE3 mice were unaffected but APOE4 mice had significant impairment in spatial learning after doxorubicin treatment. Doxorubicin impaired spatial memory in both genotypes. There were no changes in AD marker expression. |
In addition to these clinical studies, preclinical models from our lab using transgenic knock-in mice expressing the human APOE alleles support a role for APOE in CRCI. Such mouse models allow for a rigorous comparison of APOE3 and APOE4, controlling for variables such as diet, age, and chemotherapy regimen. Four to six-month old female APOE4 mice treated with the common breast cancer chemotherapeutic doxorubicin showed induced deficits in spatial learning and reduced grey matter volumes compared to untreated APOE4 mice, as well as treated and untreated APOE3 mice [41]. At 12 months of age, treated APOE4 mice again showed impairments in spatial memory compared to untreated APOE4 mice. APOE3 mice showed no deficits post-treatment [42]. These studies support the human genetic studies demonstrating that the APOE genotype plays a role in the detrimental CNS side effects of chemotherapy (Table 1).
2. Molecular Mechanisms of CNS Damages in CRCI
The numerous neurophysiological processes affected by APOE suggest many pathways for its influence on the mechanisms related to CRCI. Several possible CNS mechanisms for CRCI influenced by the APOE genotype are reviewed here, including blood brain barrier compromise, oxidative stress, inflammation, and deleterious effects on adult neurogenesis.
2.1. Blood Brain Barrier
The blood brain barrier (BBB) relies on tight junctions between endothelial cells, membrane-bound efflux proteins, the glia limitans, and a relative lack of endothelial fenestrations in the CNS [43]. As most chemotherapeutics do not readily cross the BBB, the cognitive effects of CRCI are not usually associated with direct CNS damage from the drugs. Rather, the effects of chemotherapy that induce peripheral damage can affect the integrity of the BBB, which could then result in CNS damage as peripheral molecules enter.
Oxidative stress from reactive oxygen species (ROS) induce membrane protein and lipid oxidation (discussed in detail below), which causes dysfunction of the BBB. ROS can impact expression of tight junction proteins [44], affect cytoskeletal structure, and activate matrix metalloproteinases (MMPs), all affecting BBB permeability [45]. The impact of ROS on in vitro models of the BBB included activation of MMPs, which reduced structural integrity, increased permeability, and allowed leukocytes to migrate through [46,47]. One cancer chemotherapeutic agent, oxaliplatin, directly affected expression of the tight junction proteins zonula occludens-1 (ZO-1) and F-actin in an in vitro model [48]. In vivo, the induction of enzymes that increase ROS production (NAPDH oxidase (NOX1) and inducible nitric oxide synthase (iNOS)) correlated with a reduction in expression of tight junction proteins [49]. Inflammatory cytokines also impact the integrity of the BBB. Tumor necrosis factor alpha (TNFα) is induced by many chemotherapeutics (also discussed below) and alters BBB integrity by upregulating MMPs [50]. Cytokines also reduce BBB integrity through effects on tight junctions and multiple components of the neuroimmune system [51].
APOE Genotype and the Blood Brain Barrier
The increased susceptibility of APOE4 carriers to CRCI may be due in part to APOE’s involvement in the health of the BBB [33]. A direct role for APOE in BBB function was initially demonstrated in APOE knockout mice, which showed an infiltration of plasma antibodies throughout the CNS [52]. In the CNS, astrocytes and microglia are the main producers of APOE, but vascular cells (smooth muscle and endothelial cells) and pericytes (cells associated with small vessels) also express APOE [33].
Mouse knock-in models of the human APOE alleles are useful for comparisons among human APOE alleles as well as for comparisons with wildtype mice. These models show levels and patterns of APOE expression similar to wildtype mice and humans [53,54]. Wildtype mice show more similarity in cerebral blood flow and neurovascular density to APOE3 than APOE4 mice [55], consistent with the idea that APOE3 mice reflect normal brain conditions. APOE4 mouse brains showed less collagen IV, an important basement membrane protein, and an increased penetration of plasma proteins [56]. APOE2 and APOE3 mouse brains were impermeable to fluorescently labeled dextran and multiple plasma proteins, while both APOE4 and APOE KO allowed leakage into the brain [57]. One mechanism identified involved the pro-inflammatory cytokine CypA, which had previously been shown to cause vascular damage in APOE KO mice [57]. Both APOE4 and APOE KO mice had five- to six-fold elevated levels of CypA in cerebral micro vessels, which was responsible for increased BBB permeability through the activation of MMP9. BBB breakdown correlated with a reduction in tight junction proteins that are MMP9 substrates. The proper regulation of CypA levels required the binding of astrocyte-derived APOE3 to low density lipoprotein receptor 1 (LRP1), of which APOE4 binding was deficient [57]. In in vitro assays, APOE4 had significantly less effect at attenuating MMP activity than APOE2 or APOE3 [58]. Postmortem analysis of human brain AD tissue showed accelerated pericyte and microvascular breakdown in APOE4 carriers, and increased presence of serum proteins in the CNS, indicative of BBB breakdown [59]. There was also a corresponding increase in CypA and MMP9 levels [57]. Finally, an APOE AD mouse model showed that APOE4 effects on BBB leakage were exacerbated by the presence of the Aβ peptide that accumulates in brains of AD patients [60].
In vitro models provide more mechanistic studies of the BBB. One model of brain endothelial cells and pericytes from wildtype mice, combined with astrocytes harvested from APOE3 and APOE4 knock-in transgenic mice, showed that APOE4 impaired BBB integrity and altered phosphorylation of the tight junction protein occludin [61]. The tight junction integrity was dependent on LRP1 binding, as treatment of the APOE3 model with an LRP1 inhibitor caused leakage of the BBB to levels similar to that of the APOE4 containing model [61]. Pericyte APOE4 reduced induction of endothelial cell extracellular matrix production and BBB formation [56].
Breakdown of the BBB correlates with cognitive decline with aging and AD in humans [62,63,64]. The APOE4 genotype was associated with a thinning of the microvascular basement membrane in AD patients [65]. The plasma protein prothrombin was present within micro vessels in the brain of AD patients, and this leakage through the BBB was more common in individuals with at least one APOE4 allele [66]. An examination of regional cerebral blood flow in healthy non-demented subjects over a period of eight years showed that the declines over this time period were more pronounced in APOE4 carriers [67]. High resolution MRI scans illustrated that APOE4 carriers had elevated BBB breakdown that was evident even in cognitively normal patients, and breakdown was further exacerbated in cognitively impaired subjects [68]. Higher levels of soluble platelet derived growth factor receptor-β (sPDGFRβ) was found in CSF of APOE4 but not APOE3 carriers [68]; PDGFRβ induces BBB restoration [69] and this shed form of PDGFRβ inhibits normal PDGFRβ signaling [70]. sPDGFRβ levels predicted cognitive decline, as well as increased BBB permeability and levels of plasma protein leakage into the CSF [68].
Thus, important components of the impact of APOE4 on BBB function and integrity have been identified and these mechanisms could underlie impairment of brain function by chemotherapy (Figure 1). BBB disruption related to APOE4 and chemotherapy could allow greater penetration of neurotoxic drugs or exacerbate the deleterious effects of processes such as oxidative stress and inflammation.
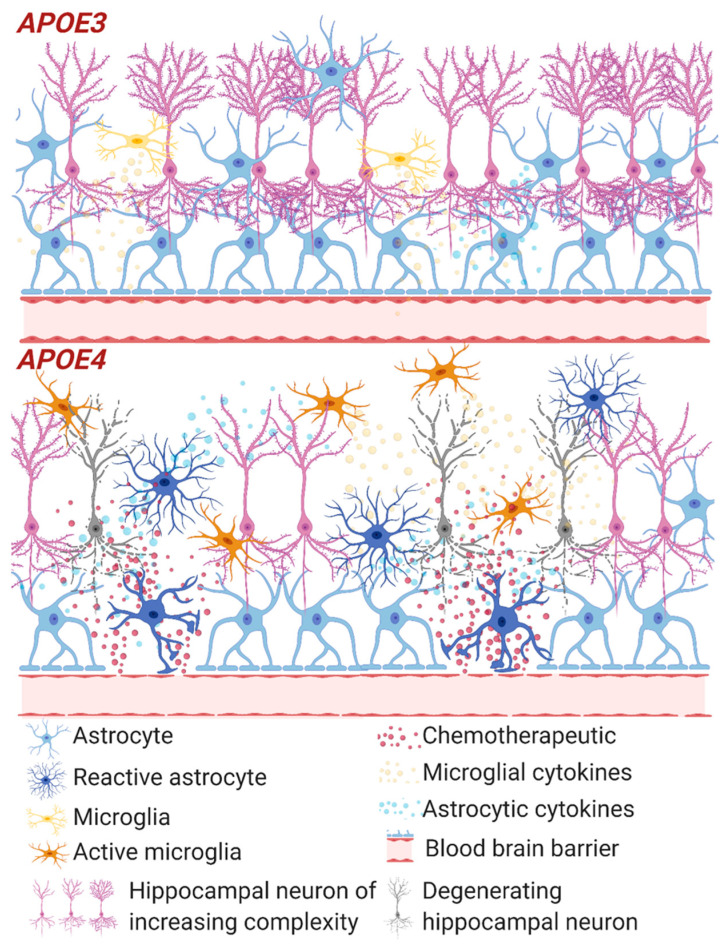
Figure 1.
Inflammation and the blood brain barrier with chemotherapy. Summary of impacts of chemotherapeutics on APOE3 and APOE4 neural tissue and the blood brain barrier (BBB). APOE4 show thinning basement membrane and impaired tight junctions leading to increased BBB permeability and release of chemotherapeutic (red particles) into the brain compartment, not apparent in APOE3. This impairment leads to increasing the already heightened immune and oxidative stress response in APOE4, increasing reactive astrocytes and active microglia, further increasing BBB breakdown. Ultimately this results in an environment that increases neurodegeneration (grey neurons). Although chemotherapeutic agents are unable to cross the secure APOE3 BBB, they are still able to induce a cytokine response close to the BBB which may damage the integrity of the tight junctions.
2.2. Oxidative Stress
Most of the cytostatic agents used to treat cancer induce oxidative stress, whether indirectly or directly, contributing to the neurotoxicity of many of these agents [71]. Cyclophosphamide (CPA) [72], doxorubicin (DOX) [73], and methotrexate (MTX) [74] generate oxidative stress in the CNS through imbalanced ROS levels, demonstrated by various markers. CPA increased cortical levels of malondialdehyde, conjugated dienes, and hydroperoxides [72,75]. In a breast cancer rodent model, CPA and DOX caused increased expression of oxidative stress related genes such as glutathione peroxidase 1 (GPX1), peroxiredoxin 1 (PRDX1), and NF-ΚB in the hippocampus [76]. An anti-oxidant compound mitigated the cognitive effects of chemotherapies [77], indicating that oxidative stress is one mechanism for CRCI. Co-administration of metformin as an antioxidant with CPA protected mice from the memory deficits associated with hippocampal damage [78]. The anti-stroke drug edavarone, which has anti-oxidant activity, blocked the reductions in superoxide dismutase, catalase and glutathione activities, and ameliorated the memory and motor coordination impairments induced by CPA [79]. A mimetic of superoxide dismutase used to reduce oxidative stress corrected cognitive behavioral deficiencies and neuronal cell changes induced by CPA, DOX, and paclitaxel in mice [80]. MTX-induced oxidative stress was relieved by co-administration of melatonin, an anti-oxidant, which resulted in restoration of spatial cognitive function in rats [81]. Finally, DOX increased protein oxidation and lipid peroxidation in the brains of mice [73], and the anti-oxidant activity of insulin reduced oxidative stress and improved cognitive function [82].
Several mechanisms could account for chemotherapy-induced oxidation. DOX increased Ca2+-mediated induction of the permeability transition pore (PTP) in brain mitochondria [83]. A PTP increase in mitochondrial membrane permeability can lead to mitochondria swelling and rupture, thereby inducing oxidative stress in the brain [83]. MTX, a folate analog, induces oxidative stress via interactions with enzymes in the folate metabolic pathway, causing elevated levels of malondialdehyde in the cerebellum in rats [84]. DOX increased TNFα production, inhibiting murine brain mitochondrial respiration and increased oxidative stress [85]. Similarly, rats injected with DOX showed increased carbonylation of brain proteins, likely mediated by increases in TNFα [86]. The involvement of TNFα in DOX-induced oxidative stress was confirmed through the use of TNFα knockout mice. In these animals the oxidative stress was alleviated, and mitochondrial activity was preserved [87]. Pro-inflammatory molecules such as TNFα thus allow certain chemotherapeutic agents to exert oxidative damage throughout the CNS, despite some of these agents being unable to cross the BBB.
In addition to animal studies, studies in human tissue show evidence of chemotherapy-related oxidative stress. Significant increases in TNFα and protein carbonyls following DOX treatment were observed in the plasma of patients [88]. CSF of acute lymphoblastic leukemia (ALL) patients showed evidence of lipid peroxidation, where the dose of MTX correlated with the levels of oxidized phosphatidylinositol [89]. While MTX allows good survival from childhood ALL, up to 40% of survivors show cognitive deterioration [89]. Polymorphisms in oxidative stress/neuroinflammation-related genes (NOS3, COMT, SLCO2A) were associated with poor neurocognitive performance on a series of behavioral tests after MTX [90]. This genomic analysis, along with the other studies mentioned, indicate that oxidative damage can contribute to the CRCI.
APOE Genotype and Oxidative Stress
APOE genotype affects susceptibility to oxidative stress, potentially exacerbating CRCI. APOE4 carriers had higher levels of certain ROS in plasma than control subjects [91]. In a postmortem study of AD patients, APOE4 brains showed greater levels of oxidative stress, including elevated lipid peroxidation in the hippocampus, and lower levels of catalase activity, glutathione peroxidase activity, and glutathione throughout the cortex [92]. Levels of thiobarbituric acid-reactive substances (TBARS), a measure of lipid peroxidation, were highest in APOE4 and lowest in APOE2 brains [93]. APOE4 carriers also had higher hydroxyl content in the blood, indicating a systemic increase in oxidative stress [94].
In a mouse model of traumatic brain injury (TBI) which induces oxidative stress, there was greater expression of anti-oxidant related genes in APOE3 and higher levels of oxidative stress markers by immunohistochemitry in APOE4 mice [95]. The APOE knock-in mice are also useful for elucidating synaptic structure and function through use of synaptosomes. Synaptosomes isolated from the APOE4 mice had the highest levels of ROS, protein and lipid oxidation, followed by APOE3 and then APOE2 [96]. The proteomes of synaptosomes from APOE4 mice had elevated oxidative stress markers compared to APOE3 mice [97].
In vitro studies showed that the three APOE isoforms provided different levels of protection against oxidative stress and toxicity caused by Aβ peptides, with APOE4 providing the least protection and APOE2 the most [98]. Several mechanisms have been proposed for the relationship between APOE4 and oxidative damage. APOE KO neurons had significantly increased levels of lactate dehydrogenase, decreased levels of SOD activity and increased intracellular Ca2+ levels when treated with APOE4 protein, compared to APOE3 [99]. APOE4 induced increased susceptibility to Ca2+-mediated neuronal apoptosis by increasing CaMKII phosphorylation and activation of caspase 3 [99]. The lack of cysteine residues (and their replacement with arginine) in the APOE4 molecule may contribute to induction of oxidative damage. Specifically, the neurotoxic 4-hydroxynonenal (HNE) molecule (which is produced as a result of lipid oxidation) can covalently bind to cysteine residues on APOE2 and APOE3 and prevent further damage to neighboring neurons [100]. APOE4 cannot bind HNE, allowing it to cause oxidative damage to neuronal proteins and eventually cell death [100].
Together, clinical and experimental findings show that common chemotherapeutic agents induce oxidative stress, as measured in a number of biological processes. APOE4 has broad impacts on oxidative stress in the brain, potentially amplifying damage introduced by chemotherapeutic treatments. These CNS damages could be mitigated by antioxidant treatments, protecting against neurotoxicity and the development of CRCI.
2.3. Inflammation
Inflammation resulting from cytostatics could be involved in promoting or exacerbating CRCI. Neuroinflammation is a critical component of neurodegeneration [101], and pro-inflammatory cytokines such as TNFα and interleukins are associated with impairments in memory and cognition. Chemotherapeutics that do not cross the BBB induce pro-inflammatory cytokines in the periphery, which could cross the BBB (by diffusion through a damaged barrier or by receptor mediated endocytosis) and elicit gliosis associated with CNS inflammation [102].
2.3.1. Inflammatory Cytokines
Cytostatics can have differing effects on the many markers of inflammation [103]. Patients receiving DOX for early stage breast cancer showed that the blood levels of cytokines IL-6, IL-8 and monocyte chemoattractant protein 1 (MCP-1) increased. These same cytokines decreased for CPA, MTX and fluorouracil. Breast cancer survivors who received surgery plus chemotherapy had significantly elevated levels of TNFα activity compared to those who had only surgery [104]. The cytokines IL-6 and TNFα were also both elevated (an average of 5 years post-surgery and chemotherapy) and associated with decreased verbal memory performance and lower hippocampal volume [105]. TNFα decreased over the first year, which correlated with a reduction in self-reported memory complaints. Brain metabolism (as measured by FDG PET) negatively correlated with TNFα in specific brain regions [104]. Cognitive response speed was negatively associated with increases in IL-1β plasma levels, but positively correlated with IL-4 (indicating a protective effect of IL-4) [106]. Higher concentrations of IL-1β and IL-6 accompanied lower self-perceived cognitive performance, while patients with higher IL-4 reported less severe cognitive disturbance. The levels of sTNF-RII (a marker of TNFα activity) and MCP-1 showed a significant association between elevated levels of sTNF-RII and reduced short term memory [106].
For B-cell non-Hodgkin lymphoma, the first line drugs rituximab and bendamustine (RB) increased serum IL-6 more than rituximab and CPA, DOX, vincristine, and prednisone (R-CHOP), and the levels of IL-6 correlated with increased fatigue three months after the end of chemotherapy [107]. Patients receiving RB had significantly lower scores in cognitive tests than a healthy cohort, while the R-CHOP trended lower than the controls [107], another example of one chemotherapy type producing varying responses. An examination of leukoencephalopathy in ALL survivors after treatment found that MTX exposure correlated with persistent increases in neuroinflammation (including astrogliosis and microglial activation) and increased neuronal damages resulting from this neuroinflammation were proposed to cause the associated cognitive problems [108]. This work across survivors of breast cancer, B-cell non-Hodgkin lymphoma, and ALL shows that chemotherapy produces strong (and varied) inflammatory responses impacting memory, cognition, and even brain structure.
Animal models allow more direct identification of mechanisms related to CRCI. Although DOX does not cross the BBB, it results in increases in peripheral and brain TNFa [85]. The elevation in brain TNFα levels was associated with reduced mitochondrial activity, and a causal connection was demonstrated by the use of anti-TNFα antibodies alleviating these effects [85]. DOX, docetaxel, and CPA treatment resulted in elevation of IL-6 and TNFα in serum and the hippocampus, as well as reductions in the anti-inflammatory cytokines IL-4 and IL-10 [109]. IL-6 and TNFα levels showed strong inverse correlations with mouse performance in water maze cognitive tests, combined with reduced signal in manganese enhance magnetic resonance imaging measuring hippocampal neuronal activity [109]. The levels of these pro-inflammatory cytokines also showed robust correlation with dendritic spine loss, a marker of reduced neuronal complexity [109]. DOX also increased TNFα levels in the brains of rats, with the robust inflammatory response further evidenced by significant increases in the levels of prostaglandin E2 and cyclooxygenase 2 (COX-2) [110].
Agents countering inflammation have been used in rodent models to alleviate behavioral effects of chemotherapy. Combined breast cancer chemotherapies of CPA, MTX, and 5-fluorouracil resulted in increased levels of TNFα, IL-1β, and COX-2 in rat brain, while levels of the anti-inflammatory cytokine IL-10 decreased [111]. Problems with inflammation, myelin levels, and cognitive scores were all alleviated by the anti-inflammatory COX-2 inhibitor NS-398 [111]. DOX treatment resulted in inflammatory responses including the activation of the NF-ΚB pathway as well as reduced spatial learning and memory [112]. DOX led to elevated TNFα, PGE-2, and COX-2 levels in the brain, which was counteracted by polydatin (PLD), an anti-inflammatory and anti-oxidant [112]. Chemotherapy induced neuronal apoptosis in the hippocampus, along with the reduced learning and memory, were alleviated by PLD which also normalized the levels of NF-ΚB pathway intermediates. Despite a different mechanism of action, paclitaxel (which works by destabilizing microtubules as opposed to damaging DNA) also impairs cognition [113]. Paclitaxel induced inflammation in the hippocampus, with increases in TNFα and IL-1β [114]. The TNFα inhibitor thalidomide reduced inflammation and neuronal apoptosis and memory and spatial learning deficits [114].
These studies show that chemotherapy effects on brain function are related to inflammation and suggest interesting directions for treatments aimed at reducing CRCI.
2.3.2. Gliosis
The primary regulators of neuroinflammation in the brain are two glial cell types, astrocytes and microglia [115]. Many brain insults induce activation and proliferation of glial cells as part of the pathways to repair damages and clear cellular debris. Importantly, glia are the main source of brain APOE.
In mouse models, DOX treatment induced widespread astrogliosis, which correlated with oxidative stress, increased IL-6 and TNFα, while reducing IL-10 and cognitive impairments [116]. Treatment of mice with the colony stimulating factor receptor 1 (CSF1R) inhibitor PLX5622, which depleted over 95% of brain microglia, caused reductions in multiple pro-inflammatory cytokines and behavioral impairments caused by DOX [117]. A role for the third type of glial cell, oligodendrocytes, was indicated by MTX treatment associated with problems with myelination and CRCI [118]. Analysis of human postmortem brain samples showed oligodendrocyte lineage cells were depleted in subjects that had undergone chemotherapy. A mouse model was developed to mimic the regimens in these patients, and it demonstrated deficits in oligodendrocyte precursor cell (OPC) numbers even 6 months after treatment cessation [118]. Reduced myelin sheath thickness corresponded to behavioral deficits similar to those that affect humans (attention, short term memory). MTX also caused activated microglia in the brain white matter, which also persisted 6 months later. Brain injury—as defined by activated astrocytes—lowered oligodendrocyte precursors, and reduced myelin sheath thickness were alleviated by depletion of the inflammatory microglia [118]. These various reports demonstrate the crucial role of glia in promoting adverse effects of chemotherapy on brain functions.
2.3.3. APOE Genotype and Neuroinflammation
Many AD genetic risk factors are directly related to processes important in neuroinflammation, including TREM2, CD33, CR1, and APOE [119]. In addition to its role in cholesterol homeostasis, APOE has profound effects on neuroinflammation, with the APOE4 protein promoting a pro-inflammatory environment, whether under normal conditions or in response to injury and disease [115]. Analyses of post-mortem AD patient brains found that APOE4 subjects had significantly increased activated microglia [120] and astrogliosis [121]. The APOE2 genotype was associated with a pattern of microglial protein expression that correlated with good cognition, while the APOE4 genotype was associated with proteins correlating with poor cognition [122]. Increased inflammatory cytokines were present in the plasma of even healthy APOE4 carriers [123], and elevated cytokines combined with the APOE4 genotype to increase risk of AD [124]. Greater cytokine production in APOE4 carriers was observed from the ex vivo stimulation of blood from patients with toll-like receptor ligands, as well as in those who had challenges with intravenous lipopolysaccharide (LPS) [125]. CCL23, a pro-inflammatory chemokine associated with cerebral damage [126], was increased in the plasma of APOE4 carriers in patients with mild cognitive impairment (MCI) and AD [127]. The CSF of APOE4 MCI and mild AD patients also had significantly increased amounts of IL-4, IL-6, and IL-8 and granulocyte colony stimulating factor [128]. A proteomic analysis of postmortem cortical samples revealed that inflammation was the biological pathway most impacted by APOE genotype in AD patients [129].
The importance of the APOE4 allele was vividly illustrated by the use of CRISPR editing technology in human induced pluripotent stem cells (iPSCs). Microglia derived from genetically identical APOE3 and APOE4 iPSCs [130] showed APOE4 microglia had elevated expression of the transcription factor IRF8 regulating multiple genes required for microglial activation [130].
The transgenic APOE knock-in mice have also provided much data on the role of APOE4 in inflammation. APOE4 mice have stronger inflammatory gene expression responses to LPS injected into the brain [131]. An increased inflammatory response to LPS injection in APOE4 mice also led to stronger gliosis and more synaptic protein loss [132]. A broad hippocampal microgliosis and astrogliosis in APOE4 mice compared in APOE3 mice was associated with accumulation of the neurotoxic intracellular Aβ [133]. LPS treatment of primary APOE4 microglial cultures led to more extensive neuron damage compared to APOE3 microglia [134], with similar experiments entailing in vitro exposure to LPS inducing significantly elevated pro-inflammatory cytokine production in APOE4 microglia [135]. The induction of acute brain injury from needle penetration resulted in greater inflammatory responses as measured by reactive astrocytes and microglia in APOE4 mice [136]. Control APOE4 mice had a lower dendritic spine density [137,138], likely a result of increased inflammation, as this phenotype was alleviated with nonsteroidal anti-inflammatory drug treatment [139].
The combination of AD-related transgenes along with APOE knock-in further demonstrated the increased inflammation in APOE4 mice. Transgenic mice containing five familial AD mutations along with APOE4 had higher cortical cytokine and microglial reactivity [140], while APOE4 mice with the P301S tau transgene had significantly higher levels of TNFα and reduced neuronal viability compared to APOE2 or APOE3 [141]. The impacts of chemotherapy on neuroinflammation, combined with the profound APOE4-dependent increase in the susceptibility to inflammation as a result of brain injuries, provide a robust link between the APOE genotype and CRCI.
2.4. Impaired Neurogenesis
Current cancer treatments are aimed at reducing atypical cell division associated with malignancy. However, they could lead to unintended impairment of neural stem cell proliferation, particularly if chemotherapeutic agents cross the blood brain barrier at times of damage by oxidative stress or inflammation.
The process of neurogenesis involves neural progenitor cells developing and maturing into new neurons. The adult brain retains two regions with prominent neurogenesis: the sub-granular zone in the dentate gyrus of the hippocampus and the subventricular zone. Cytostatics decrease neurogenesis and progenitor proliferation in these areas [142]. Cisplatin, carmustine, and AraC each decreased cell division in the dentate gyrus and the subventricular zone of mouse brains, and this pattern persisted for weeks even after treatment ceased [143]. CPA decreased the number of dentate gyrus cells expressing Ki-67 and doublecortin (DCX), markers of neurogenic cells [144]. CPA also reduced DCX levels in rats, decreased numbers of newborn granule cells, and caused less dendritic branching and shorter dendrite length, all of which correlated with reduced memory and learning capability [145]. A chronic regimen of CPA at a lower dose in rats, in contrast, did not affect neurogenesis [146]. Both CPA and DOX treatment of rats significantly reduced mature (DCX) or immature (Ki-67/NeuN) neurogenesis markers [147]. Interestingly, while both drugs affected neurogenesis, only CPA resulted in increased microglial activation [147]. The combination of DOX, CPA and 5-fluorouracil (5-FU) reduced neurogenesis and caused memory impairments in mice [148]. This same drug combination resulted in similarly reduced neurogenesis in rats and also caused changes in chromatin remodeling in the hippocampus, consistent with the observed memory and spatial learning deficits [149].
Other cytostatics, such as MTX or 5-FU, also reduced neurogenesis. MTX inhibited neurogenesis [150,151] and caused decreased white matter density in the lateral corpus callosum and memory impairments [152]. The combination of MTX and 5-FU led to significant hippocampal and frontal lobe volume changes alongside impaired neurogenesis and cognitive impairment [153]. 5-FU alone lowered levels of brain-derived neurotrophic factor and reduced spatial working memory [150]. Temozolomide, a cytostatic agent used for CNS tumors, also reduced adult hippocampal neurogenesis [154]. Unlike many of the drugs mentioned, temozolomide directly accesses the brain.
Together, these studies establish that chemotherapeutic agents can decrease neural progenitor development in critical proliferative locations. Damage to cells in these germinal areas is a key mechanism by which chemotherapy could exert long-lasting, neurotoxic effects, which in turn could impair processes such as brain plasticity and cognition [143,148,153].
APOE Genotype and Hippocampal Neurogenesis
Adult neurogenesis is important for the proper functioning of the hippocampus, a region affected early in the pathogenesis of AD [155,156]. Neural progenitor cells in the dentate gyrus require APOE expression for proper self-renewal capability. APOE knock-out resulted in loss of neural progenitor cells [157], as well as an increase in the proliferation of astrocytes [158]. In APOE4 mice there was increased proliferation of neural stem cells, but decreased neuronal maturation and neurogenesis compared to APOE3 mice, demonstrating that proper differentiation was also dependent on APOE [158]. Furthermore, dendritic development of newborn hippocampal neurons was impaired by APOE4—the dendritic length and branch number were significantly lower in APOE4 mice compared to APOE3. APOE4 knock-in mice displayed a decrease in hippocampal interneurons, resulting in learning and memory deficits [159]. Dysfunction of these neurons leads to impairment of adult hippocampal neurogenesis in mice [158]. In both transgenic APOE3 and wildtype mice, neurogenesis in the dentate gyrus is induced by environmental stimulation. In contrast, the response in APOE4 mice was the reduction of cell proliferation [160].
Analysis of the effect of the APOE genotype during aging showed that neurogenesis in young (10–12 weeks) APOE4 male and female mice was lower than in APOE2 and APOE3 mice [161] and effects in aged mice were limited to females [161]. In young mice, TBI induced neuronal proliferation in the hippocampus, but caused an attenuated response in APOE4 mice, while APOE KO mice displayed a complete lack of proliferation [162]. APOE KO and APOE4 mice also showed impaired dendritic arborization and diminished spine density in newborn granule neurons after TBI compared to APOE3 [163]. These studies show that impairment of neurogenesis in APOE4 carriers continues throughout the lifetime and after damage, particularly in females. The particular sensitivity of females may be especially significant considering the susceptibility of breast cancer survivors to CRCI [164].
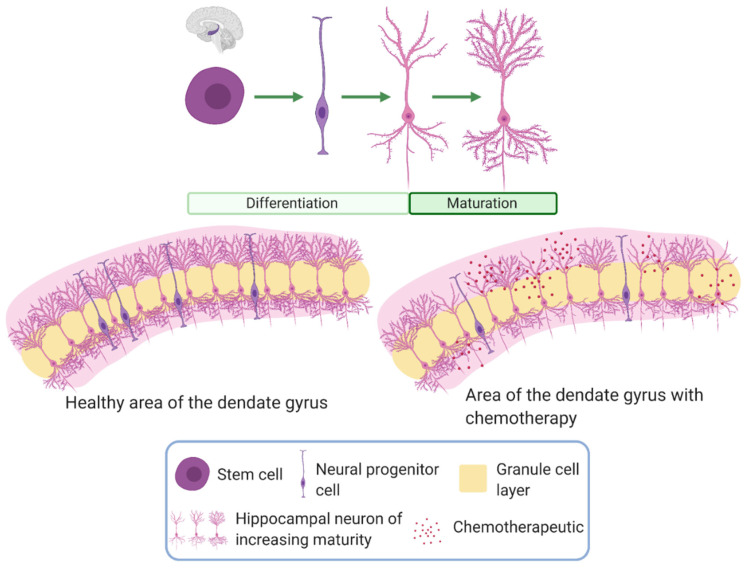
In addition to neurogenesis, synaptogenesis is also impaired in the presence of APOE4 in vivo and in primary cell cultures [165]. These findings support the well-established connection between APOE4 and progressive cognitive decline, which is often marked by abnormalities such as loss of hippocampal synapses [166,167]. The APOE-dependent regulation of neurogenesis and synaptogenesis provides a rationale for investigating a possible association between different isoforms and susceptibility to chemotherapy-induced impairment of neurogenesis. Figure 2 provides a summary of how the APOE genotype could exacerbate the detrimental effects of chemotherapy on neurogenesis.
Figure 2.
Neurogenesis and neural maturation with chemotherapy. The top image shows the progression of neurons from the stem cell to neural progenitor cell into neurons, which then mature, designated by the increase in processes and spines. The image below shows differences in neurogenesis observed in the dentate gyrus with chemotherapy. Chemotherapy results in a decrease in proliferative processes including neurogenesis and progenitor proliferations. This effect is seen through a reduction in neural progenitor cells and impaired maturation of neurons. Neurogenesis and neural maturation are reduced in APOE4 individuals compared to those carrying the APOE3 genotype. Stem cells from APOE4 individuals produce fewer neural progenitor cells compared to APOE3 individuals. Impaired neuron differentiation leads to slower maturation of neurons in APOE4 individuals, resulting in less complex neurons.
3. Interventions to Reduce the Severity of CRCI
The neurophysiological processes that are mediated by APOE would affect the risk and severity of CRCI. Table 2 reviews ways that mitigating the impact of APOE4, either reducing the detrimental influence of APOE4 or promoting the neuroprotective functions of APOE2/APOE3, may protect against CRCI. Some of these interventions are currently only being tested in vitro, while others are already being used as therapies for other diseases. APOE mimetic peptides reduce oxidative stress and inflammation by binding APOE receptors and are safe in humans in Phase I trials for spontaneous intracranial hemorrhage [168]. Agonists of the ABCA1 transporter increase APOE lipidation, which stimulates APOE function and reduces HDL inflammatory indices in high risk cardiovascular patients [169]. Several APOE-related therapeutic approaches are aimed at its effects on neuroinflammation, including cyclosporin A, non-steroidal anti-inflammatory drugs (NSAIDS) [139], and exercise [170]. Other approaches address APOE levels or APOE4 tertiary structure [171,172]. The connections between APOE biology and CRCI will aid in the development of therapeutic approaches against CRCI for the large fraction of the population who have inherited APOE4. In particular, preventative approaches before chemotherapy would be particularly promising. Furthermore, preventions that proved successful against the induced condition of CRCI may also be useful in other conditions, such as AD, which have a more prolonged onset.
Table 2.
Potential interventions to reduce the severity of cancer related cognitive impairments.
| Treatment | Mechanism | Experimental Stage | Reference |
|---|---|---|---|
| APOE mimetics | Bind APOE receptors | Pre-clinical: alleviated CNS damage induced by ischemic stroke in wildtype mice | [173] |
| Pre-clinical: reduced inflammation and oxidative stress, improved cognition in wildtype mice | [174] | ||
| Phase I human trials: completed as treatment for spontaneous intracranial hemorrhage | [168] | ||
| Pre-clinical: inhibited BBB impairment following subarachnoid hemorrhage (SAH), reduced inflammation and improved cognition in wildtype mice | [175] | ||
| ABCA1 agonists | Increase ABCA1 activity and hence APOE4 lipidation. Increase APOE levels |
Pre-clinical: alleviated synaptic impairment and improved cognition in APOE4 mice | [176] |
| In vitro: mitigated inhibition of APOE secretion by AD pathogenic protein Aβ in vitro | [177] | ||
| Clinical Trials: showed HDL inflammatory index reduced in high risk cardiovascular patients | [169,178] | ||
| Retanoic X receptor agonists |
Increase APOE levels and lipidation to increase activity | Pre-clinical: effective in reducing cognitive decline in wildtype mice | [179,180,181] |
| Clinical: Approved for use in humans as a cancer treatment | [182] | ||
| APOE4 structure correctors | Alleviate pathological intramolecular domain interactions | In vitro: increased neurite outgrowth in neurons and improved mitochondrial activity in APOE4 cells to resemble APOE3 cells | [183,184,185] |
| Cyclosporin A | Inhibits pro-inflammatory cyclophilin A to reduce BBB breakdown | Pre-clinical: reduced BBB leakage in APOE4 mice | [57] |
| Clinical: used to prevent organ rejection in humans | [186] | ||
| Exercise | Reduce rate of cognitive decline by unknown mechanism | Post hoc analysis: more beneficial for APOE4 carriers | [187] |
| APOE peptide antagonist | Disrupts interaction between APOE and Aβ and reduces inflammation and AD pathology | Pre-clinical: reduces inflammation and AD pathology induced by APOE-Aβ binding in AD mouse model | [188,189] |
| Antisense oligonucleotides | Reduce APOE levels | Pre-clinical: reduced AD pathology in an AD mouse model | [172] |
| Anti-inflammatory-NSAIDs | Reduces inflammation, increases neuronal complexity | Pre-clinical: causes APOE4 mice to more closely resemble APOE3 mice in AD model | [139] |
| CRISPR/Cas9 | Editing APOE4 to either APOE2 or APOE3, or editing APOE3 to the protective Christchurch mutation | In vitro: corrects APOE4-dependent dysfunction in neurons, astrocytes, and microglia | [130,190,191] |
4. Conclusions
There are a number of mechanisms that may play a role in the promotion of CRCI, and it is likely that a combination of these is responsible for observed debilitating effects. Each process likely varies in its impact depending on the cancer and the type of treatment. The APOE4 genotype strongly influences several aspects of brain health, and these processes provide mechanistic insight into the causes of CRCI. APOE plays important roles in the function and integrity of the blood brain barrier. These effects would profoundly modify the extent of the neurotoxicity induced by oxidative stress and inflammation resulting from chemotherapeutic drugs. APOE also has more direct effects on neuroinflammation based on its anti-inflammatory nature and is involved in the fidelity of neurogenesis, which is also detrimentally affected by chemotherapy. Recognizing its importance in the response to cancer treatments emphasizes that identifying whether a patient is an APOE4 carrier should be required before implementing a personalized regimen, as this could influence the susceptibility to, and severity of, possible neurological side effects. Moreover, there are a number of therapies that could alleviate some of the deleterious effects of chemotherapy that should be evaluated for co-administration to patients based on the impact it has on APOE function. Together, the ubiquitous roles of this essential component of many aspects of CNS health necessitates continued focus on the relationship between APOE genotype and CRCI.
Author Contributions
All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NIH R01 NS100704, R01 AG067258, R35 CA197289 and R01 AG068193.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weiss H.D., Walker M.D., Wiernik P.H. Neurotoxicity of Commonly Used Antineoplastic Agents (first of two parts) New Engl. J. Med. 1974;291:127–133. doi: 10.1056/NEJM197407182910305. [DOI] [PubMed] [Google Scholar]
- 2.Weiss H.D., Walker M.D., Wiernik P.H. Neurotoxicity of Commonly Used Antineoplastic Agents (second of two parts) New Engl. J. Med. 1974;291:75–81. doi: 10.1056/NEJM197407112910205. [DOI] [PubMed] [Google Scholar]
- 3.Silberfarb P.M., Philibert D., Levine P.M. Psychosocial aspects of neoplastic disease: II. Affective and cognitive effects of chemotherapy in cancer patients. Am. J. Psychiatry. 1980;137:597–601. doi: 10.1176/ajp.137.5.597. [DOI] [PubMed] [Google Scholar]
- 4.Silberfarb P.M. Chemotherapy and Cognitive Defects in Cancer Patients. Annu. Rev. Med. 1983;34:35–46. doi: 10.1146/annurev.me.34.020183.000343. [DOI] [PubMed] [Google Scholar]
- 5.Mandelblatt J.S., Small B.J., Luta G., Hurria A., Jim H., McDonald B.C., Graham D., Zhou X., Clapp J., Zhai W., et al. Cancer-Related Cognitive Outcomes Among Older Breast Cancer Survivors in the Thinking and Living with Cancer Study. J. Clin. Oncol. 2018;36:3211–3222. doi: 10.1200/JCO.18.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen L.D., Ehrlich B.E. Cellular mechanisms and treatments for chemobrain: Insight from aging and neurodegenerative diseases. EMBO Mol. Med. 2020;12:e12075. doi: 10.15252/emmm.202012075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bray V.J., Dhillon H., Vardy J. Systematic review of self-reported cognitive function in cancer patients following chemotherapy treatment. J. Cancer Surviv. 2018;12:537–559. doi: 10.1007/s11764-018-0692-x. [DOI] [PubMed] [Google Scholar]
- 8.Dhillon H., Bell M.L., Dhillon H.M., Vardy J.L. Baseline quality of life is associated with survival among people with advanced lung cancer. J. Psychosoc. Oncol. 2020;38:635–641. doi: 10.1080/07347332.2020.1765065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Movsas B., Hu C., Sloan J., Bradley J., Komaki R., A Masters G., Kavadi V.S., Narayan S., Michalski J.M., Johnson D.W., et al. Quality of Life Analysis of a Radiation Dose–Escalation Study of Patients with Non–Small-Cell Lung Cancer. JAMA Oncol. 2016;2:359–367. doi: 10.1001/jamaoncol.2015.3969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Movsas B., Moughan J., Sarna L., Langer C., Werner-Wasik M., Nicolaou N., Komaki R., Machtay M., Wasserman T., Bruner D.W. Quality of Life Supersedes the Classic Prognosticators for Long-Term Survival in Locally Advanced Non–Small-Cell Lung Cancer: An Analysis of RTOG 9801. J. Clin. Oncol. 2009;27:5816–5822. doi: 10.1200/JCO.2009.23.7420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noll K.R., Sullaway C.M., Wefel J.S. Depressive symptoms and executive function in relation to survival in patients with glioblastoma. J. Neuro-Oncol. 2019;142:183–191. doi: 10.1007/s11060-018-03081-z. [DOI] [PubMed] [Google Scholar]
- 12.Harrison R.A., Wefel J.S. Neurocognitive Function in Adult Cancer Patients. Neurol. Clin. 2018;36:653–674. doi: 10.1016/j.ncl.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Li M., Caeyenberghs K. Longitudinal assessment of chemotherapy-induced changes in brain and cognitive functioning: A systematic review. Neurosci. Biobehav. Rev. 2018;92:304–317. doi: 10.1016/j.neubiorev.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 14.McDonald B.C., Conroy S.K., Ahles T.A., West J.D., Saykin A.J. Gray matter reduction associated with systemic chemotherapy for breast cancer: A prospective MRI study. Breast Canc. Res. Treat. 2010;123:819–828. doi: 10.1007/s10549-010-1088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McDonald B.C., Conroy S.K., Smith D.J., West J.D., Saykin A.J. Frontal gray matter reduction after breast cancer chemotherapy and association with executive symptoms: A replication and extension study. Brain Behav. Immun. 2013;30:S117–S125. doi: 10.1016/j.bbi.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walczak P., Janowski M. Chemobrain as a Product of Growing Success in Chemotherapy—Focus on Glia as Both A Victim and A Cure. Neuropsychiatry. 2019;9:2207–2216. doi: 10.4172/Neuropsychiatry.1000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahles T.A., Saykin A.J., Furstenberg C.T., Cole B., Mott L.A., Skalla K., Whedon M.B., Bivens S., Mitchell T., Greenberg E.R., et al. Neuropsychologic Impact of Standard-Dose Systemic Chemotherapy in Long-Term Survivors of Breast Cancer and Lymphoma. J. Clin. Oncol. 2002;20:485–493. doi: 10.1200/JCO.2002.20.2.485. [DOI] [PubMed] [Google Scholar]
- 18.Castellon S.A., Ganz P.A., Bower J.E., Petersen L., Abraham L., Greendale G.A. Neurocognitive Performance in Breast Cancer Survivors Exposed to Adjuvant Chemotherapy and Tamoxifen. J. Clin. Exp. Neuropsychol. 2004;26:955–969. doi: 10.1080/13803390490510905. [DOI] [PubMed] [Google Scholar]
- 19.Silverman D.H., Dy C.J., Castellon S.A., Lai J., Pio B.S., Abraham L., Waddell K., Petersen L., Phelps M.E., Ganz P.A. Altered frontocortical, cerebellar, and basal ganglia activity in adjuvant-treated breast cancer survivors 5–10 years after chemotherapy. Breast Cancer Res. Treat. 2007;103:303–311. doi: 10.1007/s10549-006-9380-z. [DOI] [PubMed] [Google Scholar]
- 20.Deprez S., Amant F., Smeets A., Peeters R., Leemans A., van Hecke W., Verhoeven J.S., Christiaens M.-R., Vandenberghe J., Vandenbulcke M., et al. Longitudinal Assessment of Chemotherapy-Induced Structural Changes in Cerebral White Matter and Its Correlation with Impaired Cognitive Functioning. J. Clin. Oncol. 2012;30:274–281. doi: 10.1200/JCO.2011.36.8571. [DOI] [PubMed] [Google Scholar]
- 21.da Ruiter M.B., Reneman L., Boogerd W., Veltman D.J., Caan M., Douaud G., Lavini C., Linn S.C., Boven E., van Dam F.S.A.M., et al. Late effects of high-dose adjuvant chemotherapy on white and gray matter in breast cancer survivors: Converging results from multimodal magnetic resonance imaging. Hum. Brain Mapp. 2011;33:2971–2983. doi: 10.1002/hbm.21422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koppelmans V., de Ruiter M.B., van der Lijn F., Boogerd W., Seynaeve C., van der Lugt A., Vrooman H., Niessen W.J., Breteler M.M., Schagen S.B. Global and focal brain volume in long-term breast cancer survivors exposed to adjuvant chemotherapy. Breast Cancer Res. Treat. 2011;132:1099–1106. doi: 10.1007/s10549-011-1888-1. [DOI] [PubMed] [Google Scholar]
- 23.Ahles T.A., Saykin A.J., Noll W.W., Furstenberg C.T., Guerin S., Cole B., Mott L.A. The relationship of APOE genotype to neuropsychological performance in long-term cancer survivors treated with standard dose chemotherapy. Psycho-Oncology. 2003;12:612–619. doi: 10.1002/pon.742. [DOI] [PubMed] [Google Scholar]
- 24.Ahles T.A., Li Y., McDonald B.C., Schwartz G.N., Kaufman P.A., Tsongalis G.J., Moore J.H., Saykin A.J. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: The impact of APOE and smoking. Psycho-Oncology. 2014;23:1382–1390. doi: 10.1002/pon.3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amidi A., Agerbæk M., Wu L.M., Pedersen A.D., Mehlsen M., Clausen C.R., Demontis D., Børglum A.D., Harbøll A., Zachariae R. Changes in cognitive functions and cerebral grey matter and their associations with inflammatory markers, endocrine markers, and APOE genotypes in testicular cancer patients undergoing treatment. Brain Imaging Behav. 2016;11:769–783. doi: 10.1007/s11682-016-9552-3. [DOI] [PubMed] [Google Scholar]
- 26.Lambert J.C., Ibrahim-Verbaas C.A., Harold D., Naj A.C., Sims R., Bellenguez C., DeStafano A.L., Bis J.C., Beecham G.W., Grenier-Boley B., et al. Meta-Analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat. Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jansen I.E., Savage J.E., Watanabe K., Bryois J., Williams D.M., Steinberg S., Sealock J., Karlsson I.K., Hägg S., Athanasiu L., et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat. Genet. 2019;51:404–413. doi: 10.1038/s41588-018-0311-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kunkle B.W., Grenier-Boley B., Sims R., Bis J.C., Damotte V., Naj A.C., Boland A., Vronskaya M., van der Lee S.J., Amlie-Wolf A., et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 2019;51:414–430. doi: 10.1038/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flowers S.A., Grant O.C., Woods R.J., Rebeck G.W. O-glycosylation on cerebrospinal fluid and plasma apolipoprotein E differs in the lipid-binding domain. Glycobiology. 2019;30:74–85. doi: 10.1093/glycob/cwz084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dose J., Huebbe P., Nebel A., Rimbach G. APOE genotype and stress response—A mini review. Lipids Heal. Dis. 2016;15:121. doi: 10.1186/s12944-016-0288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rebeck G.W. The role of APOE on lipid homeostasis and inflammation in normal brains. J. Lipid Res. 2017;58:1493–1499. doi: 10.1194/jlr.R075408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flowers S.A., Rebeck G.W. APOE in the normal brain. Neurobiol. Dis. 2020;136:104724. doi: 10.1016/j.nbd.2019.104724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tai L., Thomas R., Marottoli F.M., Koster K.P., Kanekiyo T., Morris A.W.J., Bu G. The role of APOE in cerebrovascular dysfunction. Acta Neuropathol. 2016;131:709–723. doi: 10.1007/s00401-016-1547-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reiman E.M., Arboleda-Velasquez J.F., Quiroz Y.T., Huentelman M.J., Beach T.G., Caselli R.J., Chen Y., Su Y., Myers A.J. Exceptionally low likelihood of Alzheimer’s dementia in APOE2 homozygotes from a 5,000-person neuropathological study. Nat. Commun. 2020;11:1–11. doi: 10.1038/s41467-019-14279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jansen W.J., Ossenkoppele R., Knol D.L., Tijms B.M., Scheltens P., Verhey F.R.J., Visser P.J., Aalten P., Aarsland D., Alcolea D., et al. Prevalence of Cerebral Amyloid Pathology in Persons Without Dementia. JAMA. 2015;313:1924–1938. doi: 10.1001/jama.2015.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eisenberg D.T., Kuzawa C.W., Hayes M.G. Worldwide allele frequencies of the human apolipoprotein E gene: Climate, local adaptations, and evolutionary history. Am. J. Phys. Anthr. 2010;143:100–111. doi: 10.1002/ajpa.21298. [DOI] [PubMed] [Google Scholar]
- 37.Logue M.W. A Comprehensive Genetic Association Study of Alzheimer Disease in African Americans. Arch. Neurol. 2011;68:1569–1579. doi: 10.1001/archneurol.2011.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kobayashi S., Tateno M., Park T.W., Utsumi K., Sohma H., Ito Y.M., Kokai Y., Saito T. Apolipoprotein E4 Frequencies in a Japanese Population with Alzheimer’s Disease and Dementia with Lewy Bodies. PLoS ONE. 2011;6:e18569. doi: 10.1371/journal.pone.0018569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishimura A., Nonomura H., Tanaka S., Yoshida M., Maruyama Y., Aritomi Y., Saunders A.M., Burns D.K., Lutz M.W., Runyan G., et al. Characterization ofAPOEandTOMM40allele frequencies in the Japanese population. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2017;3:524–530. doi: 10.1016/j.trci.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eggertsen G., Tegelman R., Ericsson S., Angelin B., Berglund L. Apolipoprotein E polymorphism in a healthy Swedish population: Variation of allele frequency with age and relation to serum lipid concentrations. Clin. Chem. 1993;39:2125–2129. doi: 10.1093/clinchem/39.10.2125. [DOI] [PubMed] [Google Scholar]
- 41.Speidell A.P., Demby T., Lee Y., Rodriguez O., Albanese C., Mandelblatt J., Rebeck G.W. Development of a Human APOE Knock-in Mouse Model for Study of Cognitive Function After Cancer Chemotherapy. Neurotox. Res. 2019;35:291–303. doi: 10.1007/s12640-018-9954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Demby T.C., Rodriguez O., McCarthy C.W., Lee Y.-C., Albanese C., Mandelblatt J., Rebeck G.W. A mouse model of chemotherapy-related cognitive impairments integrating the risk factors of aging and APOE4 genotype. Behav. Brain Res. 2020;384:112534. doi: 10.1016/j.bbr.2020.112534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dias M.C., Mapunda J.A., Vladymyrov M., Engelhardt B. Structure and Junctional Complexes of Endothelial, Epithelial and Glial Brain Barriers. Int. J. Mol. Sci. 2019;20:5372. doi: 10.3390/ijms20215372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tan K.H., Harrington S., Purcell W.M., Hurst R.D. Peroxynitrite Mediates Nitric Oxide–Induced Blood–Brain Barrier Damage. Neurochem. Res. 2004;29:579–587. doi: 10.1023/B:NERE.0000014828.32200.bd. [DOI] [PubMed] [Google Scholar]
- 45.Pun P.B.L., Lu J., Moochhala S. Involvement of ROS in BBB dysfunction. Free. Radic. Res. 2009;43:348–364. doi: 10.1080/10715760902751902. [DOI] [PubMed] [Google Scholar]
- 46.Haorah J., Ramirez S.H., Schall K., Smith D., Pandya R., Persidsky Y. Oxidative stress activates protein tyrosine kinase and matrix metalloproteinases leading to blood? Brain barrier dysfunction. J. Neurochem. 2007;101:566–576. doi: 10.1111/j.1471-4159.2006.04393.x. [DOI] [PubMed] [Google Scholar]
- 47.Parathath S., Tsirka S.E. Nitric oxide mediates neurodegeneration and breakdown of the blood-brain barrier in tPA-dependent excitotoxic injury in mice. J. Cell Sci. 2006;119:339–349. doi: 10.1242/jcs.02734. [DOI] [PubMed] [Google Scholar]
- 48.Branca J.J.V., Maresca M., Morucci G., Becatti M., Paternostro F., Gulisano M., Ghelardini C., Salvemini D., Mannelli L.D.C., Pacini A. Oxaliplatin-induced blood brain barrier loosening: A new point of view on chemotherapy-induced neurotoxicity. Oncotarget. 2018;9:23426–23438. doi: 10.18632/oncotarget.25193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abdul-Muneer P.M., Schuetz H., Wang F., Skotak M., Jones J., Gorantla S., Zimmerman M.C., Chandra N., Haorah J. Induction of oxidative and nitrosative damage leads to cerebrovascular inflammation in an animal model of mild traumatic brain injury induced by primary blast. Free. Radic. Biol. Med. 2013;60:282–291. doi: 10.1016/j.freeradbiomed.2013.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Candelario-Jalil E., Taheri S., Yang Y., Sood R., Grossetete M., Estrada E.Y., Fiebich B.L., Rosenberg G.A. Cyclooxygenase Inhibition Limits Blood-Brain Barrier Disruption following Intracerebral Injection of Tumor Necrosis Factor-α in the Rat. J. Pharmacol. Exp. Ther. 2007;323:488–498. doi: 10.1124/jpet.107.127035. [DOI] [PubMed] [Google Scholar]
- 51.Banks W.A., Erickson M.A. The blood–brain barrier and immune function and dysfunction. Neurobiol. Dis. 2010;37:26–32. doi: 10.1016/j.nbd.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 52.Fullerton S.M., Shirman G.A., Strittmatter W.J., Matthew W.D. Impairment of the Blood–Nerve and Blood–Brain Barriers in Apolipoprotein E Knockout Mice. Exp. Neurol. 2001;169:13–22. doi: 10.1006/exnr.2001.7631. [DOI] [PubMed] [Google Scholar]
- 53.Sullivan P.M., Mace B., Maeda N., Schmechel D. Marked regional differences of brain human apolipoprotein e expression in targeted replacement mice. Neuroscience. 2004;124:725–733. doi: 10.1016/j.neuroscience.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 54.Riddell D.R., Zhou H., Atchison K., Warwick H.K., Atkinson P.J., Jefferson J., Xu L., Aschmies S., Kirksey Y., Hu Y., et al. Impact of Apolipoprotein E (ApoE) Polymorphism on Brain ApoE Levels. J. Neurosci. 2008;28:11445–11453. doi: 10.1523/JNEUROSCI.1972-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Koizumi K., Hattori Y., Ahn S.J., Buendia I., Ciacciarelli A., Uekawa K., Wang G., Hiller A., Zhao L., Voss H.U., et al. Apoε4 disrupts neurovascular regulation and undermines white matter integrity and cognitive function. Nat. Commun. 2018;9:1–11. doi: 10.1038/s41467-018-06301-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yamazaki Y., Shinohara M., Yamazaki A., Ren Y., Asmann Y.W., Kanekiyo T., Bu G. ApoE (Apolipoprotein E) in Brain Pericytes Regulates Endothelial Function in an Isoform-Dependent Manner by Modulating Basement Membrane Components. Arter. Thromb. Vasc. Biol. 2020;40:128–144. doi: 10.1161/ATVBAHA.119.313169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bell R.D., Winkler E.A., Singh I., Sagare A.P., Deane R., Wu Z., Holtzman D.M., Betsholtz C., Armulik A., Sallstrom J., et al. Apolipoprotein E controls cerebrovascular integrity via cyclophilin A. Nat. Cell Biol. 2012;485:512–516. doi: 10.1038/nature11087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ringland C., Schweig J.E., Paris D., Shackleton B., Lynch C.E., Eisenbaum M., Mullan M., Crawford F., Abdullah L., Bachmeier C. Apolipoprotein E isoforms differentially regulate matrix metallopeptidase 9 function in Alzheimer’s disease. Neurobiol. Aging. 2020;95:56–68. doi: 10.1016/j.neurobiolaging.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Halliday M.R., Rege S.V., Ma Q., Zhao Z., A Miller C., A Winkler E., Zlokovic B.V. Accelerated pericyte degeneration and blood–brain barrier breakdown in apolipoprotein E4 carriers with Alzheimer’s disease. Br. J. Pharmacol. 2016;36:216–227. doi: 10.1038/jcbfm.2015.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marottoli F.M., Katsumata Y., Koster K.P., Thomas R., Fardo D.W., Tai L. Peripheral Inflammation, Apolipoprotein E4, and Amyloid-β Interact to Induce Cognitive and Cerebrovascular Dysfunction. ASN Neuro. 2017;9:9. doi: 10.1177/1759091417719201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nishitsuji K., Hosono T., Nakamura T., Bu G., Michikawa M. Apolipoprotein E Regulates the Integrity of Tight Junctions in an Isoform-dependent Manner in an in Vitro Blood-Brain Barrier Model. J. Biol. Chem. 2011;286:17536–17542. doi: 10.1074/jbc.M111.225532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Montagne A., Barnes S.R., Sweeney M.D., Halliday M.R., Sagare A.P., Zhao Z., Toga A.W., Jacobs R.E., Liu C.Y., Amezcua L., et al. Blood-Brain Barrier Breakdown in the Aging Human Hippocampus. Neuron. 2015;85:296–302. doi: 10.1016/j.neuron.2014.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bowman G.L., Dayon L., Kirkland R., Wojcik J., Peyratout G., Severin I.C., Henry H., Oikonomidi A., Migliavacca E., Bacher M., et al. Blood-brain barrier breakdown, neuroinflammation, and cognitive decline in older adults. Alzheimer’s Dement. 2018;14:1640–1650. doi: 10.1016/j.jalz.2018.06.2857. [DOI] [PubMed] [Google Scholar]
- 64.Nation D.A., Sweeney M., Montagne A., Sagare A.P., D’Orazio L.M., Pachicano M., Sepehrband F., Nelson A.R., Buennagel D.P., Harrington M.G., et al. Blood–brain barrier breakdown is an early biomarker of human cognitive dysfunction. Nat. Med. 2019;25:270–276. doi: 10.1038/s41591-018-0297-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Salloway S., Gur T., Berzin T., Zipser B., Correia S., Hovanesian V., Fallon J., Kuo-Leblanc V., Glass D., Hulette C., et al. Effect of APOE genotype on microvascular basement membrane in Alzheimer’s disease. J. Neurol. Sci. 2002;203:183–187. doi: 10.1016/S0022-510X(02)00288-5. [DOI] [PubMed] [Google Scholar]
- 66.Zipser B., Johanson C., Gonzalez L., Berzin T., Tavares R., Hulette C., Vitek M., Hovanesian V., Stopa E. Microvascular injury and blood–brain barrier leakage in Alzheimer’s disease. Neurobiol. Aging. 2007;28:977–986. doi: 10.1016/j.neurobiolaging.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 67.Thambisetty M., Beasonheld L.L., An Y., Kraut M.A., Resnick S.M. APOE ε4 Genotype and Longitudinal Changes in Cerebral Blood Flow in Normal Aging. Arch. Neurol. 2010;67:93–98. doi: 10.1001/archneurol.2009.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Montagne A., Nation D.A., Sagare A.P., Barisano G., Sweeney M.D., Chakhoyan A., Pachicano M., Joe E., Nelson A.R., D’Orazio L.M., et al. APOE4 leads to blood–brain barrier dysfunction predicting cognitive decline. Nat. Cell Biol. 2020;581:71–76. doi: 10.1038/s41586-020-2247-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shen J., Xu G., Zhu R., Yuan J., Ishii Y., Hamashima T., Matsushima T., Yamamoto S., Takatsuru Y., Nabekura J., et al. PDGFR-β restores blood-brain barrier functions in a mouse model of focal cerebral ischemia. Br. J. Pharmacol. 2019;39:1501–1515. doi: 10.1177/0271678X18769515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sagare A.P., Sweeney M., Makshanoff J., Zlokovic B.V. Shedding of soluble platelet-derived growth factor receptor-β from human brain pericytes. Neurosci. Lett. 2015;607:97–101. doi: 10.1016/j.neulet.2015.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ahles T.A., Saykin A.J. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat. Rev. Cancer. 2007;7:192–201. doi: 10.1038/nrc2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Oboh G., Ogunruku O.O. Cyclophosphamide-induced oxidative stress in brain: Protective effect of hot short pepper (Capsicum frutescens L. var. abbreviatum) Exp. Toxicol. Pathol. 2010;62:227–233. doi: 10.1016/j.etp.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 73.Joshi G., Sultana R., Tangpong J., Cole M.P., Clair D.K.S., Vore M., Estus S., Butterfield D.A. Free radical mediated oxidative stress and toxic side effects in brain induced by the anti-cancer drug adriamycin: Insight into chemobrain. Free. Radic. Res. 2005;39:1147–1154. doi: 10.1080/10715760500143478. [DOI] [PubMed] [Google Scholar]
- 74.Rajamani R., Muthuvel A., Senthilvelan M., Devi R.S. Oxidative stress induced by methotrexate alone and in the presence of methanol in discrete regions of the rodent brain, retina and optic nerve. Toxicol. Lett. 2006;165:265–273. doi: 10.1016/j.toxlet.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 75.Bhatia A.L., Manda K., Patni S., Sharma A.L. Prophylactic Action of Linseed (Linum usitatissimum) Oil Against Cyclophosphamide-Induced Oxidative Stress in Mouse Brain. J. Med. Food. 2006;9:261–264. doi: 10.1089/jmf.2006.9.261. [DOI] [PubMed] [Google Scholar]
- 76.Bagnall-Moreau C., Chaudhry S., Salas-Ramirez K., Ahles T., Hubbard K. Chemotherapy-Induced Cognitive Impairment Is Associated with Increased Inflammation and Oxidative Damage in the Hippocampus. Mol. Neurobiol. 2019;56:7159–7172. doi: 10.1007/s12035-019-1589-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Konat G.W., Kraszpulski M., James I., Zhang H.-T., Abraham J. Cognitive dysfunction induced by chronic administration of common cancer chemotherapeutics in rats. Metab. Brain Dis. 2008;23:325–333. doi: 10.1007/s11011-008-9100-y. [DOI] [PubMed] [Google Scholar]
- 78.Alhowail A., Chigurupati S., Sajid S., Mani V. Ameliorative effect of metformin on cyclophosphamide-induced memory impairment in mice. Eur. Rev. Med. Pharmacol Sci. 2019;23:9660–9666. doi: 10.26355/eurrev_201911_19460. [DOI] [PubMed] [Google Scholar]
- 79.Singh S. Protective Effect of Edaravone on Cyclophosphamide Induced Oxidative Stress and Neurotoxicity in Rats. Curr. Drug Saf. 2019;14:209–216. doi: 10.2174/1574886314666190506100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McElroy T., Brown T., Kiffer F., Wang J., Byrum S.D., Oberley-Deegan R.E., Allen A.R. Assessing the Effects of Redox Modifier MnTnBuOE-2-PyP 5+ on Cognition and Hippocampal Physiology Following Doxorubicin, Cyclophosphamide, and Paclitaxel Treatment. Int. J. Mol. Sci. 2020;21:1867. doi: 10.3390/ijms21051867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen Y.-C., Sheen J.-M., Hsu M.-H., Hsiao C.-C., Wang S.-C., Huang L.-T. Melatonin rescued methotrexate-induced spatial deficit and hyperhomocysteinemia and increased asymmetric dimethylarginine in plasma and dorsal hippocampus in developing rats. Life Sci. 2019;242:116931. doi: 10.1016/j.lfs.2019.116931. [DOI] [PubMed] [Google Scholar]
- 82.Ramalingayya G.V., Sonawane V., Cheruku S.P., Kishore A., Nayak P.G., Kumar N., Shenoy R.R., Nandakumar K. Insulin Protects against Brain Oxidative Stress with an Apparent Effect on Episodic Memory in Doxorubicin-Induced Cognitive Dysfunction in Wistar Rats. J. Environ. Pathol. Toxicol. Oncol. 2017;36:121–130. doi: 10.1615/JEnvironPatholToxicolOncol.2017017087. [DOI] [PubMed] [Google Scholar]
- 83.Cardoso S., Santos R.X., Carvalho C., Correia S., Pereira G.C., Pereira S.S., Oliveira P.J., Santos M.S., Proença T., Moreira P.I. Doxorubicin increases the susceptibility of brain mitochondria to Ca2+-induced permeability transition and oxidative damage. Free. Radic. Biol. Med. 2008;45:1395–1402. doi: 10.1016/j.freeradbiomed.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 84.Uzar E., Koyuncuoglu H.R., Uz E., Yilmaz H.R., Kutluhan S., Kilbas S., Gultekin F. The Activities of Antioxidant Enzymes and the Level of Malondialdehyde in Cerebellum of Rats Subjected to Methotrexate: Protective Effect of Caffeic Acid Phenethyl Ester. Mol. Cell. Biochem. 2006;291:63–68. doi: 10.1007/s11010-006-9196-5. [DOI] [PubMed] [Google Scholar]
- 85.Tangpong J., Cole M.P., Sultana R., Joshi G., Estus S., Vore M., Clair W.S., Ratanachaiyavong S., Clair D.K.S., Butterfield D.A. Adriamycin-induced, TNF-α-mediated central nervous system toxicity. Neurobiol. Dis. 2006;23:127–139. doi: 10.1016/j.nbd.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 86.Joshi G., Aluise C.D., Cole M.P., Sultana R., Pierce W., Vore M., Clair D.K.S., Butterfield D.A. Alterations in brain antioxidant enzymes and redox proteomic identification of oxidized brain proteins induced by the anti-cancer drug adriamycin: Implications for oxidative stress-mediated chemobrain. Neuroscience. 2010;166:796–807. doi: 10.1016/j.neuroscience.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ren X., Keeney J.T., Miriyala S., Noel T., Powell D.K., Chaiswing L., Bondada S., Clair D.K.S., Butterfield D.A. The triangle of death of neurons: Oxidative damage, mitochondrial dysfunction, and loss of choline-containing biomolecules in brains of mice treated with doxorubicin. Advanced insights into mechanisms of chemotherapy induced cognitive impairment (“chemobrain”) involving TNF-α. Free. Radic. Biol. Med. 2019;134:1–8. doi: 10.1016/j.freeradbiomed.2018.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Aluise C.D., Miriyala S., Noel T., Sultana R., Jungsuwadee P., Taylor T.J., Cai J., Pierce W.M., Vore M., Moscow J.A., et al. 2-Mercaptoethane sulfonate prevents doxorubicin-induced plasma protein oxidation and TNF-α release: Implications for the reactive oxygen species-mediated mechanisms of chemobrain. Free. Radic. Biol. Med. 2011;50:1630–1638. doi: 10.1016/j.freeradbiomed.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 89.Moore I.M., Gundy P., Pasvogel A., Montgomery D.W., Taylor O.A., Koerner K.M., McCarthy K., Hockenberry M.J. Increase in Oxidative Stress as Measured by Cerebrospinal Fluid Lipid Peroxidation During Treatment for Childhood Acute Lymphoblastic Leukemia. J. Pediatr. Hematol. 2015;37:e86–e93. doi: 10.1097/MPH.0000000000000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cole P.D., Finkelstein Y., Stevenson K.E., Blonquist T.M., Vijayanathan V., Silverman L.B., Neuberg D.S., Sallan S.E., Robaey P., Waber D.P. Polymorphisms in Genes Related to Oxidative Stress Are Associated with Inferior Cognitive Function After Therapy for Childhood Acute Lymphoblastic Leukemia. J. Clin. Oncol. 2015;33:2205–2211. doi: 10.1200/JCO.2014.59.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fernandes M.A., Proença M.T., Nogueira A.J., Grazina M., Oliveira L.M., I Fernandes A., Santiago B., Santana I., Oliveira C.R. Influence of apolipoprotein E genotype on blood redox status of Alzheimer’s disease patients. Int. J. Mol. Med. 1999;4:179–265. doi: 10.3892/ijmm.4.2.179. [DOI] [PubMed] [Google Scholar]
- 92.Ramassamy C., Averill D., Beffert U., Théroux L., Lussier-Cacan S., Cohn J.S., Christen Y., Schoofs A., Davignon J., Poirier J. Oxidative Insults Are Associated with Apolipoprotein E Genotype in Alzheimer’s Disease Brain. Neurobiol. Dis. 2000;7:23–37. doi: 10.1006/nbdi.1999.0273. [DOI] [PubMed] [Google Scholar]
- 93.Tamaoka A., Miyatake F., Matsuno S., Ishii K., Nagase S., Sahara N., Ono S., Mori H., Wakabayashi K., Tsuji S., et al. Apolipoprotein E allele-dependent antioxidant activity in brains with Alzheimer’s disease. Neurology. 2000;54:2319–2321. doi: 10.1212/WNL.54.12.2319. [DOI] [PubMed] [Google Scholar]
- 94.Ihara Y., Hayabara T., Sasaki K., Kawada R., Nakashima Y., Kuroda S. Relationship between oxidative stress and apoE phenotype in Alzheimer’s disease. Acta Neurol. Scand. 2000;102:346–349. doi: 10.1034/j.1600-0404.2000.102006346.x. [DOI] [PubMed] [Google Scholar]
- 95.Ferguson S., Mouzon B., Kayihan G., Wood M., Poon F., Doore S.M., Mathura V., Humphrey J., O’Steen B., Hayes R., et al. Apolipoprotein E genotype and oxidative stress response to traumatic brain injury. Neuroscience. 2010;168:811–819. doi: 10.1016/j.neuroscience.2010.01.031. [DOI] [PubMed] [Google Scholar]
- 96.Lauderback C.M., Kanski J., Hackett J.M., Maeda N., Kindy M.S., Butterfield D. Apolipoprotein E modulates Alzheimer’s Aβ(1–42)-induced oxidative damage to synaptosomes in an allele-specific manner. Brain Res. 2002;924:90–97. doi: 10.1016/s0006-8993(01)03228-0. [DOI] [PubMed] [Google Scholar]
- 97.Shi L., Du X., Zhou H., Tao C.-L., Liu Y., Meng F., Wu G., Xiong Y., Xia C., Wang Y., et al. Cumulative effects of the ApoE genotype and gender on the synaptic proteome and oxidative stress in the mouse brain. Int. J. Neuropsychopharmacol. 2014;17:1863–1879. doi: 10.1017/S1461145714000601. [DOI] [PubMed] [Google Scholar]
- 98.Miyata M., Smith J.D. Apolipoprotein E allele–specific antioxidant activity and effects on cytotoxicity by oxidative insults and β–amyloid peptides. Nat. Genet. 1996;14:55–61. doi: 10.1038/ng0996-55. [DOI] [PubMed] [Google Scholar]
- 99.Xu D., Peng Y. Apolipoprotein E 4 triggers multiple pathway mediated Ca2+ overload, causes CaMK II phosphorylation abnormity and aggravates oxidative stress caused cerebral cortical neuron damage. Eur. Rev. Med Pharmacol. Sci. 2017;21:5717–5728. doi: 10.26355/eurrev_201712_14018. [DOI] [PubMed] [Google Scholar]
- 100.Butterfield D.A., Mattson M.P. Apolipoprotein E and oxidative stress in brain with relevance to Alzheimer’s disease. Neurobiol. Dis. 2020;138:104795. doi: 10.1016/j.nbd.2020.104795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Guzman-Martinez L., Maccioni R.B., Andrade V., Navarrete L.P., Pastor M.G., Ramos-Escobar N. Neuroinflammation as a Common Feature of Neurodegenerative Disorders. Front. Pharmacol. 2019;10:1008. doi: 10.3389/fphar.2019.01008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ren X., Clair D.K.S., Butterfield D.A. Dysregulation of cytokine mediated chemotherapy induced cognitive impairment. Pharmacol. Res. 2017;117:267–273. doi: 10.1016/j.phrs.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 103.Janelsins M.C., Mustian K.M., Palesh O.G., Mohile S.G., Peppone L.J., Sprod L.K., Heckler C.E., Roscoe J.A., Katz A.W., Williams J.P., et al. Differential expression of cytokines in breast cancer patients receiving different chemotherapies: Implications for cognitive impairment research. Support. Care Cancer. 2011;20:831–839. doi: 10.1007/s00520-011-1158-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ganz P.A., Bower J., Kwan L., Castellon S., Silverman D., Geist C., Breen E., Irwin M., Cole S. Does tumor necrosis factor-alpha (TNF-α) play a role in post-chemotherapy cerebral dysfunction? Brain Behav. Immun. 2013;30:S99–S108. doi: 10.1016/j.bbi.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kesler S.R., Janelsins M.C., Koovakkattu D., Palesh O., Mustian K.M., Morrow G.R., Dhabhar F.S. Reduced hippocampal volume and verbal memory performance associated with interleukin-6 and tumor necrosis factor-alpha levels in chemotherapy-treated breast cancer survivors. Brain Behav. Immun. 2013;30:S109–S116. doi: 10.1016/j.bbi.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Williams A.M., Shah R., Shayne M., Huston A.J., Krebs M., Murray N., Thompson B.D., Doyle K., Korotkin J., van Wijngaarden E., et al. Associations between inflammatory markers and cognitive function in breast cancer patients receiving chemotherapy. J. Neuroimmunol. 2018;314:17–23. doi: 10.1016/j.jneuroim.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zimmer P., Mierau A., Bloch W., Strüder H.K., Hülsdünker T., Schenk A., Fiebig L., Baumann F.T., Hahn M., Reinart N., et al. Post-chemotherapy cognitive impairment in patients with B-cell non-Hodgkin lymphoma: A first comprehensive approach to determine cognitive impairments after treatment with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone or rituximab and bendamustine. Leuk. Lymphoma. 2014;56:347–352. doi: 10.3109/10428194.2014.915546. [DOI] [PubMed] [Google Scholar]
- 108.Cheung Y.T., Khan R.B., Liu W., Brinkman T.M., Edelmann M.N., Reddick W.E., Pei D., Panoskaltsis-Mortari A., Srivastava D.K., Cheng C., et al. Association of Cerebrospinal Fluid Biomarkers of Central Nervous System Injury with Neurocognitive and Brain Imaging Outcomes in Children Receiving Chemotherapy for Acute Lymphoblastic Leukemia. JAMA Oncol. 2018;4:e180089. doi: 10.1001/jamaoncol.2018.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shi D.-D., Huang Y.-H., Lai C.S.W., Dong C.M., Ho L.C., Wu E.X., Li Q., Wang X.-M., Chung S.K., Sham P.C., et al. Chemotherapy-Induced Cognitive Impairment Is Associated with Cytokine Dysregulation and Disruptions in Neuroplasticity. Mol. Neurobiol. 2019;56:2234–2243. doi: 10.1007/s12035-018-1224-4. [DOI] [PubMed] [Google Scholar]
- 110.El-Agamy S.E., Abdel-Aziz A.K., Wahdan S., Esmat A., Azab S.S. Astaxanthin Ameliorates Doxorubicin-Induced Cognitive Impairment (Chemobrain) in Experimental Rat Model: Impact on Oxidative, Inflammatory, and Apoptotic Machineries. Mol. Neurobiol. 2017;55:5727–5740. doi: 10.1007/s12035-017-0797-7. [DOI] [PubMed] [Google Scholar]
- 111.Briones T.L., Woods J. Dysregulation in myelination mediated by persistent neuroinflammation: Possible mechanisms in chemotherapy-related cognitive impairment. Brain Behav. Immun. 2013;35:23–32. doi: 10.1016/j.bbi.2013.07.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tong Y., Wang K., Sheng S., Cui J. Polydatin ameliorates chemotherapy-induced cognitive impairment (chemobrain) by inhibiting oxidative stress, inflammatory response, and apoptosis in rats. Biosci. Biotechnol. Biochem. 2020;84:1201–1210. doi: 10.1080/09168451.2020.1722057. [DOI] [PubMed] [Google Scholar]
- 113.Panoz-Brown D., Carey L.M., Smith A.E., Gentry M., Sluka C.M., Corbin H.E., Wu J.-E., Hohmann A.G., Crystal J.D. The chemotherapeutic agent paclitaxel selectively impairs reversal learning while sparing prior learning, new learning and episodic memory. Neurobiol. Learn. Mem. 2017;144:259–270. doi: 10.1016/j.nlm.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Li Z., Zhao S., Zhang H.-L., Liu P., Liu F.-F., Guo Y.-X., Wang X.-L. Proinflammatory Factors Mediate Paclitaxel-Induced Impairment of Learning and Memory. Mediat. Inflamm. 2018;2018:1–9. doi: 10.1155/2018/3941840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kloske C.M., Wilcock D.M. The Important Interface Between Apolipoprotein E and Neuroinflammation in Alzheimer’s Disease. Front. Immunol. 2020;11:754. doi: 10.3389/fimmu.2020.00754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Cardoso C.V., de Barros M.P., Bachi A.L.L., Bernardi M.M., Kirsten T.B., Martins M.D.F.M., Rocha P.R.D., Rodrigues P.D.S., Bondan E.F., Vieira C. Chemobrain in rats: Behavioral, morphological, oxidative and inflammatory effects of doxorubicin administration. Behav. Brain Res. 2020;378:112233. doi: 10.1016/j.bbr.2019.112233. [DOI] [PubMed] [Google Scholar]
- 117.Allen B.D., Apodaca L.A., Syage A.R., Markarian M., Baddour A.A.D., Minasyan H., Alikhani L., Lu C., West B.L., Giedzinski E., et al. Attenuation of neuroinflammation reverses Adriamycin-induced cognitive impairments. Acta Neuropathol. Commun. 2019;7:1–15. doi: 10.1186/s40478-019-0838-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gibson E.M., Nagaraja S., Ocampo A., Tam L.T., Wood L.S., Pallegar P.N., Greene J.J., Geraghty A.C., Goldstein A.K., Ni L., et al. Methotrexate Chemotherapy Induces Persistent Tri-glial Dysregulation that Underlies Chemotherapy-Related Cognitive Impairment. Cell. 2019;176:43–55. doi: 10.1016/j.cell.2018.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Malik M., Parikh I., Vasquez J.B., Smith C., Tai L., Bu G., Ladu M.J., Fardo D.W., Rebeck G.W., Estus S. Genetics ignite focus on microglial inflammation in Alzheimer’s disease. Mol. Neurodegener. 2015;10:1–12. doi: 10.1186/s13024-015-0048-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Egensperger R., Kösel S., Eitzen U., Graeber M.B. Microglial Activation in Alzheimer Disease: Association with APOE Genotype. Brain Pathol. 2006;8:439–447. doi: 10.1111/j.1750-3639.1998.tb00166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Overmyer M., Helisalmi S., Soininen H., Laakso M., Sr P.R., Alafuzoff I. Astrogliosis and the ApoE Genotype. Dement. Geriatr. Cogn. Disord. 1999;10:252–257. doi: 10.1159/000017128. [DOI] [PubMed] [Google Scholar]
- 122.Minett T., Cfas M., Classey J., Matthews F.E., Fahrenhold M., Taga M., Brayne C., Ince P.G., Nicoll J.A.R., Boche D. Microglial immunophenotype in dementia with Alzheimer’s pathology. J. Neuroinflamm. 2016;13:1–10. doi: 10.1186/s12974-016-0601-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ringman J.M., Elashoff D., Geschwind D.H., Welsh B.T., Gylys K.H., Lee C., Cummings J.L., Cole G.M. Plasma Signaling Proteins in Persons at Genetic Risk for Alzheimer Disease. Arch. Neurol. 2012;69:757–764. doi: 10.1001/archneurol.2012.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fan Y.-Y., Cai Q.-L., Gao Z.-Y., Lin X., Huang Q., Tang W., Liu J.-H. APOE ε4 allele elevates the expressions of inflammatory factors and promotes Alzheimer’s disease progression: A comparative study based on Han and She populations in the Wenzhou area. Brain Res. Bull. 2017;132:39–43. doi: 10.1016/j.brainresbull.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 125.Gale S.C., Gao L., Mikacenic C., Coyle S.M., Rafaels N., Dudenkov T.M., Madenspacher J.H., Draper D.W., Ge W., Aloor J.J., et al. APOε4 is associated with enhanced in vivo innate immune responses in human subjects. J. Allergy Clin. Immunol. 2014;134:127–134. doi: 10.1016/j.jaci.2014.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Simats A., García-Berrocoso T., Penalba A., Giralt D., Llovera G., Jiang Y., Ramiro L., Bustamante A., Martinez-Saez E., Canals F., et al. CCL23: A newCCchemokine involved in human brain damage. J. Intern. Med. 2018;283:461–475. doi: 10.1111/joim.12738. [DOI] [PubMed] [Google Scholar]
- 127.Faura J., Bustamante A., Penalba A., Giralt D., Simats A., Martínez-Sáez E., Alcolea D., Fortea J., Lleó A., Teunissen C.E., et al. CCL23: A Chemokine Associated with Progression from Mild Cognitive Impairment to Alzheimer’s Disease. J. Alzheimer’s Dis. 2020;73:1585–1595. doi: 10.3233/JAD-190753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Motta C., Finardi A., Toniolo S., di Lorenzo F., Scaricamazza E., Loizzo S., Mercuri N.B., Furlan R., Koch G., Martorana A. Protective Role of Cerebrospinal Fluid Inflammatory Cytokines in Patients with Amnestic Mild Cognitive Impairment and Early Alzheimer’s Disease Carrying Apolipoprotein E4 Genotype. J. Alzheimer’s Dis. 2020:1–9. doi: 10.3233/JAD-191250. [DOI] [PubMed] [Google Scholar]
- 129.Dai J., Johnson E.C.B., Dammer E.B., Duong D.M., Gearing M., Lah J.J., Levey A.I., Wingo T.S., Seyfried N.T. Effects of APOE Genotype on Brain Proteomic Network and Cell Type Changes in Alzheimer’s Disease. Front. Mol. Neurosci. 2018;11:454. doi: 10.3389/fnmol.2018.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lin Y.-T., Seo J., Gao F., Feldman H.M., Wen H.-L., Penney J., Cam H.P., Gjoneska E., Raja W.K., Cheng J., et al. APOE4 Causes Widespread Molecular and Cellular Alterations Associated with Alzheimer’s Disease Phenotypes in Human iPSC-Derived Brain Cell Types. Neuron. 2018;98:1294. doi: 10.1016/j.neuron.2018.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ophir G., Amariglio N., Jacob-Hirsch J., Elkon R., Rechavi G., Michaelson D.M. Apolipoprotein E4 enhances brain inflammation by modulation of the NF-κB signaling cascade. Neurobiol. Dis. 2005;20:709–718. doi: 10.1016/j.nbd.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 132.Zhu Y., Nwabuisi-Heath E., Dumanis S.B., Tai L.M., Yu C., Rebeck G.W., Ladu M.J. APOE genotype alters glial activation and loss of synaptic markers in mice. Glia. 2012;60:559–569. doi: 10.1002/glia.22289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Belinson H., Michaelson D.M. ApoE4-dependent Aβ-mediated neurodegeneration is associated with inflammatory activation in the hippocampus but not the septum. J. Neural Transm. 2009;116:1427–1434. doi: 10.1007/s00702-009-0218-9. [DOI] [PubMed] [Google Scholar]
- 134.Maezawa I., Nivison M., Montine K.S., Maeda N., Montine T.J. Neurotoxicity from innate immune response is greatest with targeted replacement of ε4 allele of apolipoprotein E gene and is mediated by microglial p38MAPK. FASEB J. 2006;20:797–799. doi: 10.1096/fj.05-5423fje. [DOI] [PubMed] [Google Scholar]
- 135.Vitek M., Brown C.M., Colton C.A. APOE genotype-specific differences in the innate immune response. Neurobiol. Aging. 2009;30:1350–1360. doi: 10.1016/j.neurobiolaging.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ben-Moshe H., Luz I., Liraz O., Boehm-Cagan A., Salomon-Zimri S., Michaelson D.M. ApoE4 Exacerbates Hippocampal Pathology Following Acute Brain Penetration Injury in Female Mice. J. Mol. Neurosci. 2019;70:32–44. doi: 10.1007/s12031-019-01397-7. [DOI] [PubMed] [Google Scholar]
- 137.Dumanis S.B., Tesoriero J.A., Babus L.W., Nguyen M.T., Trotter J.H., Ladu M.J., Weeber E.J., Turner R.S., Xu B., Rebeck G.W., et al. ApoE4 Decreases Spine Density and Dendritic Complexity in Cortical Neurons In Vivo. J. Neurosci. 2009;29:15317–15322. doi: 10.1523/JNEUROSCI.4026-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rodriguez G.A., Burns M.P., Weeber E.J., Rebeck G.W. Young APOE4 targeted replacement mice exhibit poor spatial learning and memory, with reduced dendritic spine density in the medial entorhinal cortex. Learn. Mem. 2013;20:256–266. doi: 10.1101/lm.030031.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Dibattista A.M., Dumanis S.B., Newman J., Rebeck G.W. Identification and modification of amyloid-independent phenotypes of APOE4 mice. Exp. Neurol. 2016;280:97–105. doi: 10.1016/j.expneurol.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rodriguez G.A., Tai L., Ladu M.J., Rebeck G.W. Human APOE4 increases microglia reactivity at Aβ plaques in a mouse model of Aβ deposition. J. Neuroinflamm. 2014;11:111. doi: 10.1186/1742-2094-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Shi Y., Initiative A.D.N., Yamada K., Liddelow S.A., Ferguson-Smith A.C., Zhao L., Luo W., Tsai R.M., Spina S., Grinberg L.T., et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration in a mouse model of tauopathy. Nat. Cell Biol. 2017;549:523–527. doi: 10.1038/nature24016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Dias G.P., Hollywood R., Bevilaqua M.C.D.N., Luz A.C.D.D.S.D., Hindges R., Nardi A.E., Thuret S. Consequences of cancer treatments on adult hippocampal neurogenesis: Implications for cognitive function and depressive symptoms. Neuro-Oncology. 2014;16:476–492. doi: 10.1093/neuonc/not321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Dietrich J., Wanchang C., Yang Y., Mayer-Pröschel M., Noble M. CNS progenitor cells and oligodendrocytes are targets of chemotherapeutic agents in vitro and in vivo. J. Biol. 2006;5:22. doi: 10.1186/jbiol50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yang M., Kim J.-S., Song M.-S., Kim S.-H., Kang S.S., Bae C.-S., Kim J.-C., Wang H., Shin T., Moon C. Cyclophosphamide impairs hippocampus-dependent learning and memory in adult mice: Possible involvement of hippocampal neurogenesis in chemotherapy-induced memory deficits. Neurobiol. Learn. Mem. 2010;93:487–494. doi: 10.1016/j.nlm.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 145.Wu L., Guo D., Liu Q., Gao F., Wang X., Song X., Wang F., Zhan R.-Z. Abnormal Development of Dendrites in Adult-Born Rat Hippocampal Granule Cells Induced by Cyclophosphamide. Front. Cell. Neurosci. 2017;11:171. doi: 10.3389/fncel.2017.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lyons L., Elbeltagy M., Bennett G., Wigmore P. The Effects of Cyclophosphamide on Hippocampal Cell Proliferation and Spatial Working Memory in Rat. PLoS ONE. 2011;6:e21445. doi: 10.1371/journal.pone.0021445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Christie L.-A., Acharya M.M., Parihar V.K., Nguyen A., Martirosian V., Limoli C.L. Impaired Cognitive Function and Hippocampal Neurogenesis following Cancer Chemotherapy. Clin. Cancer Res. 2012;18:1954–1965. doi: 10.1158/1078-0432.CCR-11-2000. [DOI] [PubMed] [Google Scholar]
- 148.Rendeiro C., Sheriff A., Bhattacharya T.K., Gogola J.V., Baxter J.H., Chen H., Helferich W.G., Roy E.J., Rhodes J.S. Long-lasting impairments in adult neurogenesis, spatial learning and memory from a standard chemotherapy regimen used to treat breast cancer. Behav. Brain Res. 2016;315:10–22. doi: 10.1016/j.bbr.2016.07.043. [DOI] [PubMed] [Google Scholar]
- 149.Briones T.L., Woods J. Chemotherapy-induced cognitive impairment is associated with decreases in cell proliferation and histone modifications. BMC Neurosci. 2011;12:124. doi: 10.1186/1471-2202-12-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mustafa S., Walker A.J., Bennett G., Wigmore P. 5-Fluorouracil chemotherapy affects spatial working memory and newborn neurons in the adult rat hippocampus. Eur. J. Neurosci. 2008;28:323–330. doi: 10.1111/j.1460-9568.2008.06325.x. [DOI] [PubMed] [Google Scholar]
- 151.Elbeltagy M., Mustafa S., Umka J., Lyons L., Salman A., Dormon K., Allcock C., Bennett G., Wigmore P. The effect of 5-fluorouracil on the long term survival and proliferation of cells in the rat hippocampus. Brain Res. Bull. 2012;88:514–518. doi: 10.1016/j.brainresbull.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 152.Seigers R., Schagen S.B., Coppens C.M., van der Most P.J., van Dam F.S.A.M., Koolhaas J.M., Buwalda B. Methotrexate decreases hippocampal cell proliferation and induces memory deficits in rats. Behav. Brain Res. 2009;201:279–284. doi: 10.1016/j.bbr.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 153.Winocur G., Berman H., Nguyen M., Binns M.A., Henkelman M., van Eede M., Piquette-Miller M., Sekeres M.J., Wojtowicz J.M., Yu J., et al. Neurobiological Mechanisms of Chemotherapy-induced Cognitive Impairment in a Transgenic Model of Breast Cancer. Neuroscience. 2018;369:51–65. doi: 10.1016/j.neuroscience.2017.10.048. [DOI] [PubMed] [Google Scholar]
- 154.Nokia M.S., Anderson M.L., Shors T.J. Chemotherapy disrupts learning, neurogenesis and theta activity in the adult brain. Eur. J. Neurosci. 2012;36:3521–3530. doi: 10.1111/ejn.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Moreno-Jiménez E.P., Flor-García M., Terreros-Roncal J., Rábano A., Cafini F., Pallas-Bazarra N., Ávila J., Llorens-Martin M. Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease. Nat. Med. 2019;25:554–560. doi: 10.1038/s41591-019-0375-9. [DOI] [PubMed] [Google Scholar]
- 156.Scopa C., Marrocco F., Latina V., Ruggeri F., Corvaglia V., la Regina F., Ammassari-Teule M., Middei S., Amadoro G., Meli G., et al. Impaired adult neurogenesis is an early event in Alzheimer’s disease neurodegeneration, mediated by intracellular Aβ oligomers. Cell Death Differ. 2020;27:934–948. doi: 10.1038/s41418-019-0409-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yang C.-P., Gilley J.A., Zhang G., Kernie S.G. ApoE is required for maintenance of the dentate gyrus neural progenitor pool. Development. 2011;138:4351–4362. doi: 10.1242/dev.065540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Li G., Bien-Ly N., Andrews-Zwilling Y., Xu Q., Bernardo A., Ring K., Halabisky B., Deng C., Mahley R.W., Huang Y. GABAergic Interneuron Dysfunction Impairs Hippocampal Neurogenesis in Adult Apolipoprotein E4 Knockin Mice. Cell Stem Cell. 2009;5:634–645. doi: 10.1016/j.stem.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Andrews-Zwilling Y., Bien-Ly N., Xu Q., Li G., Bernardo A., Yoon S.Y., Zwilling D., Yan T.X., Chen L., Huang Y. Apolipoprotein E4 Causes Age- and Tau-Dependent Impairment of GABAergic Interneurons, Leading to Learning and Memory Deficits in Mice. J. Neurosci. 2010;30:13707–13717. doi: 10.1523/jneurosci.4040-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Levi O., Michaelson D.M. Environmental enrichment stimulates neurogenesis in apolipoprotein E3 and neuronal apoptosis in apolipoprotein E4 transgenic mice. J. Neurochem. 2007;100:202–210. doi: 10.1111/j.1471-4159.2006.04189.x. [DOI] [PubMed] [Google Scholar]
- 161.Koutseff A., Mittelhaeuser C., Essabri K., Auwerx J., Meziane H. Impact of the apolipoprotein E polymorphism, age and sex on neurogenesis in mice: Pathophysiological relevance for Alzheimer’s disease? Brain Res. 2014;1542:32–40. doi: 10.1016/j.brainres.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 162.Hong S., Washington P.M., Kim A., Yang C.-P., Yu T.-S., Kernie S.G. Apolipoprotein E Regulates Injury-Induced Activation of Hippocampal Neural Stem and Progenitor Cells. J. Neurotrauma. 2016;33:362–374. doi: 10.1089/neu.2014.3860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Tensaouti Y., Yu T.-S., Kernie S.G. Apolipoprotein E regulates the maturation of injury-induced adult-born hippocampal neurons following traumatic brain injury. PLoS ONE. 2020;15:e0229240. doi: 10.1371/journal.pone.0229240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Joly F., Lange M., Msc M.D.S., Vaz-Luis I., di Meglio A. Long-Term Fatigue and Cognitive Disorders in Breast Cancer Survivors. Cancers. 2019;11:1896. doi: 10.3390/cancers11121896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Najm R., Jones E.A., Huang Y. Apolipoprotein E4, inhibitory network dysfunction, and Alzheimer’s disease. Mol. Neurodegener. 2019;14:24. doi: 10.1186/s13024-019-0324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Scheff S.W., Price D.A., Schmitt F.A., Mufson E.J. Hippocampal synaptic loss in early Alzheimer’s disease and mild cognitive impairment. Neurobiol. Aging. 2006;27:1372–1384. doi: 10.1016/j.neurobiolaging.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 167.Scheff S.W., Price D.A., Schmitt F.A., DeKosky S.T., Mufson E.J. Synaptic alterations in CA1 in mild Alzheimer disease and mild cognitive impairment. Neurology. 2007;68:1501–1508. doi: 10.1212/01.wnl.0000260698.46517.8f. [DOI] [PubMed] [Google Scholar]
- 168.Guptill J.T., Raja S.M., Boakye-Agyeman F., Noveck R., Ramey S., Tu T.M., Laskowitz D.T. Phase 1 Randomized, Double-Blind, Placebo-Controlled Study to Determine the Safety, Tolerability, and Pharmacokinetics of a Single Escalating Dose and Repeated Doses of CN-105 in Healthy Adult Subjects. J. Clin. Pharmacol. 2017;57:770–776. doi: 10.1002/jcph.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Dunbar R.L., Movva R., Bloedon L.T., Duffy D., Norris R.B., Navab M., Fogelman A.M., Rader D.J. Oral Apolipoprotein A-I Mimetic D-4F Lowers HDL-Inflammatory Index in High-Risk Patients: A First-in-Human Multiple-Dose, Randomized Controlled Trial. Clin. Transl. Sci. 2017;10:455–469. doi: 10.1111/cts.12487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Williams T., Borchelt D.R., Chakrabarty P. Therapeutic approaches targeting Apolipoprotein E function in Alzheimer’s disease. Mol. Neurodegener. 2020;15:1–19. doi: 10.1186/s13024-020-0358-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lanfranco M.F., Ng C.A., Rebeck G.W. ApoE Lipidation as a Therapeutic Target in Alzheimer’s Disease. Int. J. Mol. Sci. 2020;21:6336. doi: 10.3390/ijms21176336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Huynh T.-P.V., Liao F., Francis C.M., Robinson G.O., Serrano J.R., Jiang H., Roh J., Finn M.B., Sullivan P.M., Esparza T.J., et al. Age-Dependent Effects of apoE Reduction Using Antisense Oligonucleotides in a Model of β-amyloidosis. Neuron. 2017;96:1013–1023. doi: 10.1016/j.neuron.2017.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu J., Zhou G., Kolls B.J., Tan Y., Fang C., Wang H., Laskowitz D.T. Apolipoprotein E mimetic peptide CN-105 improves outcome in a murine model of SAH. Stroke Vasc. Neurol. 2018;3:222–230. doi: 10.1136/svn-2018-000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Laskowitz D.T., Wang H., Chen T., Lubkin D.T., Cantillana V., Tu T.M., Kernagis D., Zhou G., Macy G., Kolls B.J., et al. Neuroprotective pentapeptide CN-105 is associated with reduced sterile inflammation and improved functional outcomes in a traumatic brain injury murine model. Sci. Rep. 2017;7:srep46461. doi: 10.1038/srep46461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Pang J., Chen Y., Kuai L., Yang P., Peng J., Wu Y., Chen Y., Vitek M.P., Chen L., Sun X., et al. Inhibition of Blood-Brain Barrier Disruption by an Apolipoprotein E-Mimetic Peptide Ameliorates Early Brain Injury in Experimental Subarachnoid Hemorrhage. Transl. Stroke Res. 2016;8:257–272. doi: 10.1007/s12975-016-0507-1. [DOI] [PubMed] [Google Scholar]
- 176.Boehm-Cagan A., Bar R., Liraz O., Bielicki J.K., Johansson J.O., Michaelson D.M. ABCA1 Agonist Reverses the ApoE4-Driven Cognitive and Brain Pathologies. J. Alzheimer’s Dis. 2016;54:1219–1233. doi: 10.3233/JAD-160467. [DOI] [PubMed] [Google Scholar]
- 177.Chernick D., Ortiz-Valle S., Jeong A., Swaminathan S.K., Kandimalla K.K., Rebeck G.W., Li L. High-density lipoprotein mimetic peptide 4F mitigates amyloid-β-induced inhibition of apolipoprotein E secretion and lipidation in primary astrocytes and microglia. J. Neurochem. 2018;147:647–662. doi: 10.1111/jnc.14554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Bloedon L.T., Dunbar R., Duffy D., Pinell-Salles P., Norris R., DeGroot B.J., Movva R., Navab M., Fogelman A.M., Rader D.J. Safety, pharmacokinetics, and pharmacodynamics of oral apoA-I mimetic peptide D-4F in high-risk cardiovascular patients. J. Lipid Res. 2008;49:1344–1352. doi: 10.1194/jlr.P800003-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Cramer P.E., Cirrito J.R., Wesson D.W., Lee C.Y.D., Karlo J.C., Zinn A.E., Casali B.T., Restivo J.L., Goebel W.D., James M.J., et al. ApoE-Directed Therapeutics Rapidly Clear -Amyloid and Reverse Deficits in AD Mouse Models. Science. 2012;335:1503–1506. doi: 10.1126/science.1217697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Fitz N.F., Cronican A.A., Lefterov I., Koldamova R. Comment on “ApoE-Directed Therapeutics Rapidly Clear -Amyloid and Reverse Deficits in AD Mouse Models”. Science. 2013;340:924-c. doi: 10.1126/science.1235809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Tesseur I., Lo A.C., Roberfroid A., Dietvorst S., van Broeck B., Borgers M., Gijsen H., Moechars D., Mercken M., Kemp J., et al. Comment on “ApoE-Directed Therapeutics Rapidly Clear -Amyloid and Reverse Deficits in AD Mouse Models”. Science. 2013;340:924-e. doi: 10.1126/science.1233937. [DOI] [PubMed] [Google Scholar]
- 182.Shen D., Yu X., Wu Y., Chen Y., Li G., Cheng F., Xia L. Emerging roles of bexarotene in the prevention, treatment and anti-drug resistance of cancers. Expert Rev. Anticancer. Ther. 2018;18:487–499. doi: 10.1080/14737140.2018.1449648. [DOI] [PubMed] [Google Scholar]
- 183.Chen H.-K., Ji Z.-S., Dodson S.E., Miranda R.D., Rosenblum C.I., Reynolds I.J., Freedman S.B., Weisgraber K.H., Huang Y., Mahley R.W. Apolipoprotein E4 Domain Interaction Mediates Detrimental Effects on Mitochondria and Is a Potential Therapeutic Target for Alzheimer Disease. J. Biol. Chem. 2010;286:5215–5221. doi: 10.1074/jbc.M110.151084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Chen H.-K., Liu Z., Meyer-Franke A., Brodbeck J., Miranda R.D., McGuire J.G., Pleiss M.A., Ji Z.-S., Balestra M.E., Walker D.W., et al. Small Molecule Structure Correctors Abolish Detrimental Effects of Apolipoprotein E4 in Cultured Neurons. J. Biol. Chem. 2011;287:5253–5266. doi: 10.1074/jbc.M111.276162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Brodbeck J., McGuire J., Liu Z., Meyer-Franke A., Balestra M.E., Jeong D.-E., Pleiss M., McComas C., Hess F., Witter D., et al. Structure-dependent Impairment of Intracellular Apolipoprotein E4 Trafficking and Its Detrimental Effects Are Rescued by Small-molecule Structure Correctors. J. Biol. Chem. 2011;286:17217–17226. doi: 10.1074/jbc.M110.217380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Al Mamun A., Uddin S., Bin Bashar F., Zaman S., Begum Y., Bulbul I.J., Islam S., Sarwar S., Mathew B., Amran S., et al. Molecular Insight into the Therapeutic Promise of Targeting APOE4 for Alzheimer’s Disease. Oxidative Med. Cell. Longev. 2020;2020:1–16. doi: 10.1155/2020/5086250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Jensen C.S., Simonsen A.H., Siersma V., Beyer N., Frederiksen K.S., Gottrup H., Hoffman K., Høgh P., Frikke-Schmidt R., Sobol N.A., et al. Patients with Alzheimer’s disease who carry the APOE ε4 allele benefit more from physical exercise. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2019;5:99–106. doi: 10.1016/j.trci.2019.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Sawmiller D., Habib A., Hou H., Mori T., Fan A., Tan J., Zeng J., Giunta B., Sanberg P.R., Mattson M.P. A Novel Apolipoprotein E Antagonist Functionally Blocks Apolipoprotein E Interaction With N-terminal Amyloid Precursor Protein, reduces β-Amyloid-Associated Pathology, and Improves Cognition. Biol. Psychiatry. 2019;86:208–220. doi: 10.1016/j.biopsych.2019.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 189.Potter H., Chial H.J. Targeting the Interaction Between Apolipoprotein E and Amyloid Precursor Protein: A Novel Alzheimer’s Disease Therapy. Biol. Psychiatry. 2019;86:169–170. doi: 10.1016/j.biopsych.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 190.Wang C., Najm R., Xu Q., Jeong D.-E., Walker D., Balestra M.E., Yoon S.Y., Yuan H., Li G., Miller Z., et al. Gain of toxic apolipoprotein E4 effects in human iPSC-derived neurons is ameliorated by a small-molecule structure corrector. Nat. Med. 2018;24:647–657. doi: 10.1038/s41591-018-0004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Arboleda-Velasquez J.F., Lopera F., O’Hare M., Delgado-Tirado S., Marino C., Chmielewska N., Saez-Torres K.L., Amarnani D., Schultz A.P., Sperling R.A., et al. Resistance to autosomal dominant Alzheimer’s disease in an APOE3 Christchurch homozygote: A case report. Nat. Med. 2019;25:1680–1683. doi: 10.1038/s41591-019-0611-3. [DOI] [PMC free article] [PubMed] [Google Scholar]